Introduction
Adult-onset Still's disease (AOSD) is a
multisystemic inflammatory disorder characterized by a high spiking
fever, a transient rash and arthritis/arthralgia (1). Other clinical symptoms include sore
throat, myalgia, lymphadenopathies, splenomegaly and neutrophilic
leukocytosis (2). The etiology of
AOSD remains unclear, but an autoimmune pathogenesis has been
suggested (3). The most common
pulmonary manifestations associated with AOSD are pulmonary
infiltrates and pleural effusion (4). However, acute respiratory distress
syndrome (ARDS) accompanied by AOSD has rarely been reported
(5–7). ARDS is a form of acute diffuse lung
injury characterized by severe inflammation, increased pulmonary
vascular permeability and a loss of aerated lung tissue (8). ARDS occurs in 7.2–38.9/100,000
individuals (9,10), and has a mortality rate of ~40%
(11). Patient mortality varies
based on numerous factors, including age, etiology of the lung
injury and non-pulmonary organ dysfunction. The most common risk
factors for ARDS are pneumonia, sepsis, aspiration and trauma
(11). Multiple predisposing risk
factors, in addition to some secondary factors such as alcohol
abuse and obesity, also increase the risk (4). In addition to patient support provided
by improving oxygen delivery to the tissues and preventing
multiorgan system failure, early recognition and correction of the
underlying cause is important in ARDS treatment. A thorough patient
assessment searching for the underlying cause should be undertaken;
once identified, it should be managed appropriately. Potential
sources of infection should also be sought to initiate timely and
appropriate antibiotic therapy to improve sepsis-associatted
outcomes (4,11). ARDS accompanied by AOSD is sensitive
to high dose corticosteroid therapy. The present study reports the
case of a 40-year old male diagnosed with AOSD accompanied by
ARDS.
Case report
A 40-year-old Chinese male was admitted to The
Second Affiliated Hospital of Guangzhou University of Chinese
Medicine (Guangzhou, China) with a four-day history of intermittent
fever accompanied by with shortness of breath for one day. The
patient was a driver who did not smoke or drink, and had no recent
travel or contact history of infectious diseases. On June 3, 2014,
the patient had a temperature of 39°C and developed fever, cough, a
stuffy, runny nose and sore throat. On June 5, 2014, the patient
was admitted to the Emergency Department at The Second Affiliated
Hospital of Guangzhou University Chinese Hospital where laboratory
analyses was performed. The patient had an initial white blood cell
(WBC) count of 33.25×109 cells/l (normal range,
4–10×109 cells/l) with 92.1% neutrophils (normal range,
50–70%), and a routine urine test revealed positive urine protein
(1–2 g, 2+) and leukocyte esterase (+). From these results, the
patient was diagnosed with a urinary tract infection, and was
treated with levofloxacin [100 ml (0.5 g), q.d.; Daiichi Sankyo,
Co., Ltd., Shanghai, China] and antipyretic therapy (ibuprofen
suspension; 20 ml, p.o., t.i.d.; Jiangsu Hengrui Medicine Co.,
Ltd., Jiangsu, China). However, the body temperature of the patient
continued to fluctuate between 38.9 and 39.2°C, accompanied by mild
shortness of breath and headache.
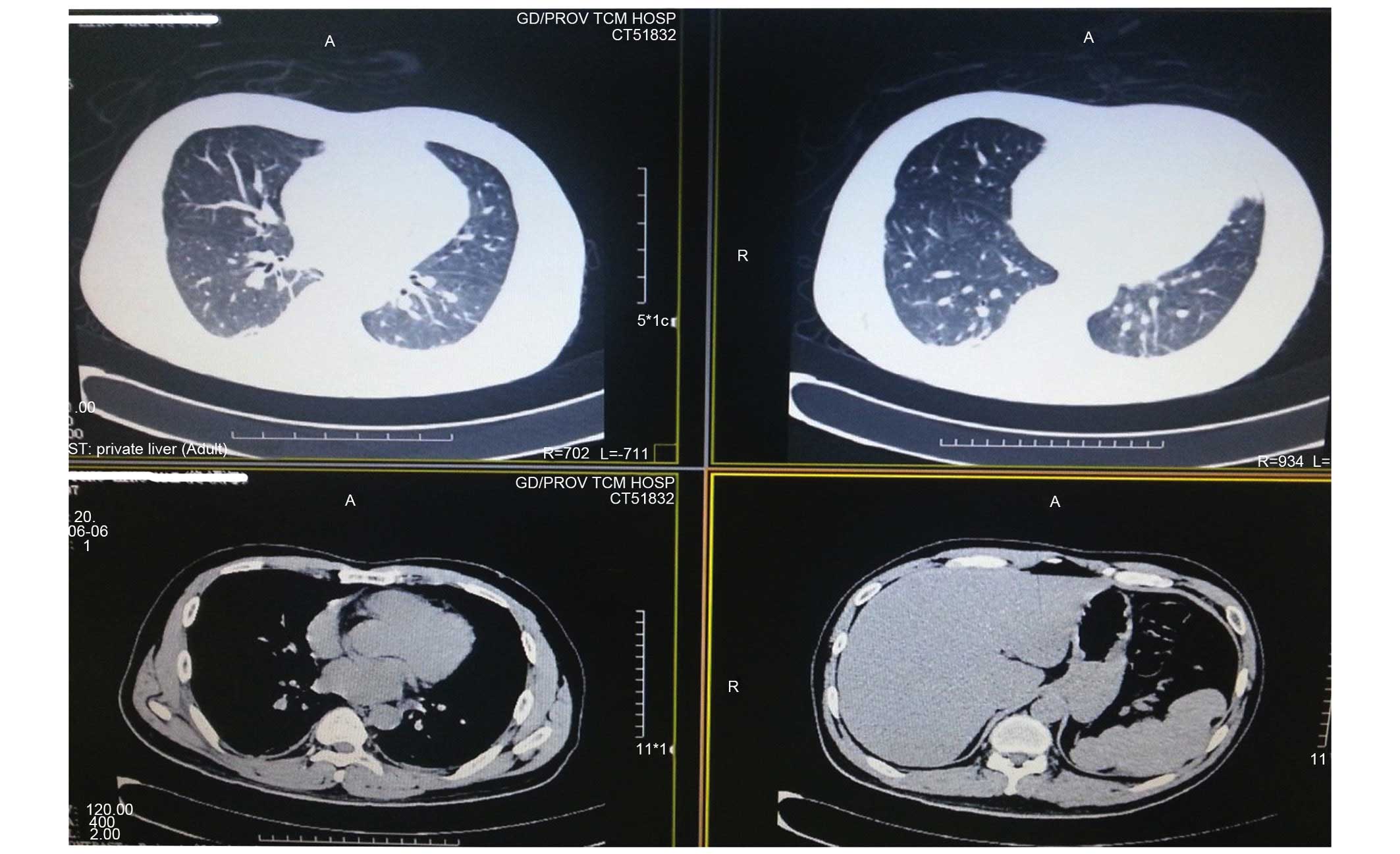
On June 6, 2014, further examination was performed
and results indicated that the respiratory status of the patient
had worsened (Table I). Computerized
axial tomography (CT) scanning of the abdomen showed splenomegaly
and bilateral kidney inflammatory effusions (Fig. 1). As a result, the patient was
diagnosed with sepsis, acute respiratory distress syndrome (ARDS),
multiple organ dysfunction syndrome (including the heart, lungs and
liver), infective fever (perirenal infection), fatty liver and
splenomegaly. The patient was subsequently treated with tienam
(1,000 mg, b.i.d.; EMD Millipore, Billerica, MA, USA), polyene
phosphatidylcholine (456 mg, t.i.d.; Sanofi S.A., Paris, France),
plavix (75 mg, q.d.; Sanofi S.A.), aspirin (100 mg, q.d.; Bayer AG,
Leverkusen, Germany) and lipitor. However, the results obtained on
the following day suggested that the patient's condition was
deteriorating; therefore, the patient was immediately admitted to
the Intensive Care Unit (ICU).
 | Table I.Laboratory analysis results prior to
admission to patient admission to intensive care. |
Table I.
Laboratory analysis results prior to
admission to patient admission to intensive care.
|
| Date |
|---|
|
|
|
|---|
| Parameter | June 5th | June 6th | June 7th |
|---|
| White blood cell |
33.25×109/l | – |
25.88×109/l |
| Neutrophil | 92.10% | – | 94% |
| Urine protein | 2+ (moderate) | – | – |
| Urine leukocyte
esterase | + (positive) | – | – |
| Procalcitonin | – | 3.49 ng/ml | 3.07 ng/ml |
| Total bilirubin | – | 53.8 µmol/l | 0.431 g/l |
| Bilirubin
conjugated | – | 7.2 µmol/l | – |
| Blood urea
nitrogen | – | 21.5 µmol/l | – |
| Arterial blood gas,
pO2 | – | 72 mmHg | 70 mmHg |
| Arterial blood gas,
pCO2 | – | 29.9 mmHg | 30.6 mmHg |
| Cardiac troponin
I | – | 1.98 g/l | – |
| N-terminal of the
pro-hormone brain natriuretic peptide | – | 1763 pg/l | – |
| β2-microglobulin | – | – | 2.35 mg/l |
| C reactive
protein | – | – | 200 mg/l |
| Erythrocyte
sedimentation rate | – | – | 100 mm/h |
Following admission to ICU (June 7, 2014), the vital
signs of the patient were as follows: Body temperature, 38.6°C
(normal range, 36.0–37.0°C); pulse rate, 121 beats/min (normal
range, 60–100 beats/min); respiratory rate, 32 breaths/min (normal
range, 70–75 breaths/min); and blood pressure, 131/72 mmHg (normal
range, 90–139/60–89 mmHg). Physical examination revealed bilateral
coarse breath sounds over the lung fields without dry or wet rale,
mild yellow dye of the systemic skin mucous membrane and sclera,
pharyngeal hyperemia, and 121 beats/min heart rate with the cardiac
dull field expanded, a sign of pericardial effusion. The abdomen
was soft, while the spleen could be touched below the left rib with
~2 fingers in width. In addition, the spleen felt tough with smooth
edges with no haphalgesia. Laboratory test results are presented in
Table II. The results of chest
radiography were as follows: Pulmonary congestion, heart
enlargement and a small quantity of pleural effusion on both sides.
This led to a diagnosis of cardiac insufficiency and infection in
the lower right lung. The therapeutic strategy comprised of
ventilation using a non-invasive ventilator, anti-infection therapy
using imipenem (1,000 mg, b.i.d.; EMD Millipore), stomach
protection using pantoprazole, phlegm control using ambroxol,
myocardial nutrition with creatine phosphate sodium, liver
protection using a combination of transmetil and glycyrrhizin, and
a number of other add-on treatments, such as traditional Chinese
Medicine and nutritional treatments.
 | Table II.Laboratory analysis results during
patient hospitalization in the Intensive Care Unit. |
Table II.
Laboratory analysis results during
patient hospitalization in the Intensive Care Unit.
|
| Date |
|---|
|
|
|
|---|
| Parameter | June 7th | June 14th | June 23rd |
|---|
| White blood cell |
27.33×109/l | − | − |
| Neutrophil | 93% | − | − |
| Prothrombin time | 15.3 sec | − | − |
| International
Normalised Ratio | 1.21 | − | − |
| Fibrinogen | 9.23 g/l | − | − |
| D-dimer | >8,000 µg/l | − | − |
| Ferritin | 3,364 mg/l | − | − |
| Arterial blood gas,
pO2 | 98.6 mmHg | − | − |
| Arterial blood gas,
pCO2 | 27 mmHg | − | − |
| Cardiad troponin
I | 0.342 µg/l | − | − |
| Vasculitis related
antibodies | Negative | − | − |
| Rheumatoid
factor | Negative | − | − |
| Urinary leukocyte
esterase | Negative | − | − |
| Urobilinogen | 4+ (severe) | − | − |
| Urine bilirubin | 2+ (moderate) | − | − |
| Leptospira
antibody | − | Positive (+, 1:100),
indicating Jaundice hemorrhagic fever | − |
| Epstein-Barr viral
nucleic acid | − | + (positive) | − |
| Liver fluke
antibody | − | − | + |
| Paragonimiasis
antibody | − | − | + |
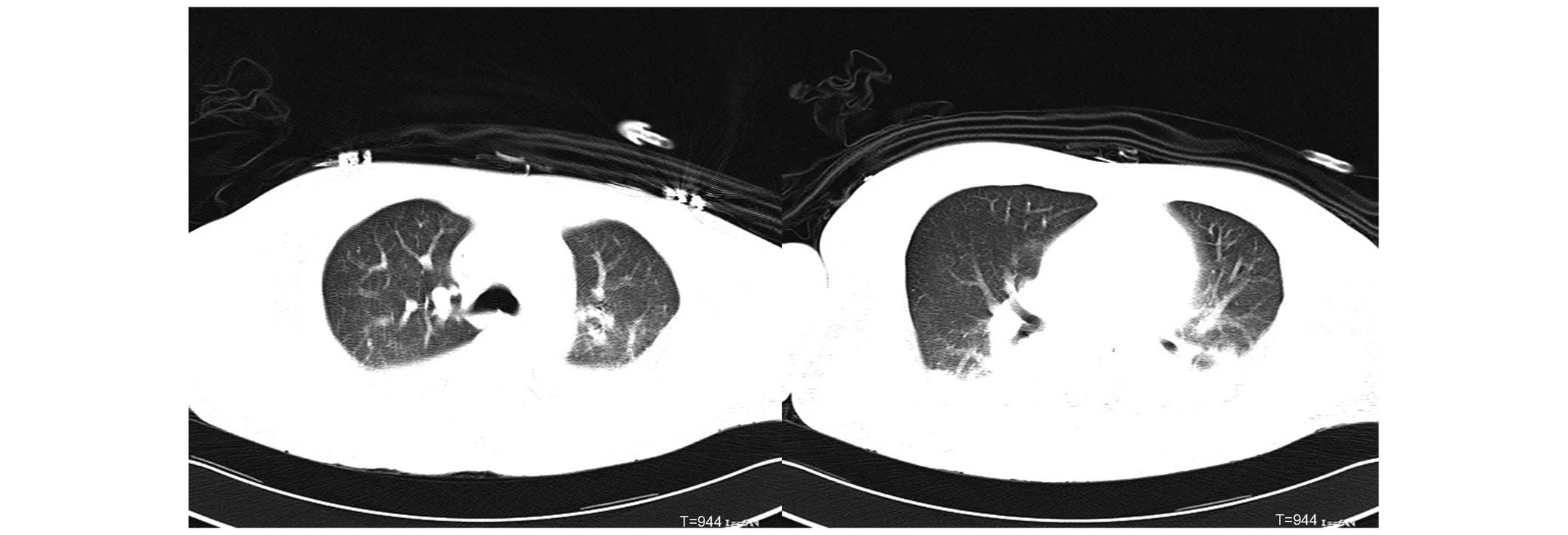
On the night of June 8th, 2014, the patient still
felt short of breath, despite the ventilation using a non-invasive
ventilator. Physical examination revealed the following: Body
temperature, 39.5°C; pulse rate, 135 beats/min; respiratory rate,
40 breaths/min; blood pressure, 122/73 mmHg; and peripheral blood
oxygen, 93%. The breathing of the patient was weak and scattered
moist rales were observed over lung fields. A chest and abdomen CT
was performed and the following results (Fig. 2) were obtained: i) Inflammation was
present in the inferior lingular segment of the upper left lung and
the dorsal and basal segments of both lungs; and ii) bilateral
pleural effusion was observed. These results were severe compared
with the results obtained on June 6th, 2014. In addition, segmental
compression and hypoventilation were observed in the lower lungs.
iii) Heart shadow was increased, primarily due to left ventricular
enlargement. Furthermore, a small quantity of pericardial effusion
was demonstrated; iv) splenauxe; v) increased exudation around both
kidneys compared with the results of the CT scan on June 6, 2014,
and a small quantity of effusion was observed in the bilateral
paracolic sulci the abdomen; and vi) pelvic effusion. Furthermore,
blood gas analyses (PaO2, 66.5 mmHg; PaCO2,
32.1 mmHg) indicated that the breathing problem was severe. The
patient was diagnosed with ARDS, and symptomatic treatments,
including morphine and propofol treatment, were immediately
performed.
Over a number of days, laboratory test results were
obtained (Table II) and the
therapeutic strategy was subsequently modified. Propofol and
morphine were administered for sedation and analgesia, and esmolol
was used to reduce the heart rate. In addition, anti-infection
therapy was expanded and a number of antibiotics were administered,
including imipenem, vancomycin (500 mg, q. 8 h; Eli Lilly Japan
K.K., Kobe, Japan), fluconazole (400 mg, q.d.; Pfizer, Inc., New
York, NY, USA), moxifloxacin (400 mg, q.d.; Bayer AG), penicillin,
doxycycline (200 mg, q.d.; Guangdong Weilun Biological Co., Ltd.,
Guangdong, China) and meropenem (1,000 mg, q. 8 h; Sumitomo
Dainippon Pharma Co., Ltd., Osaka, Japan). Other symptomatic
treatments, such as protecting the liver and stomach, nourishing
the myocardium, correcting anemia and improving the immune system
were administered. On June 14th, 2014, the oxygenation index was
improved (>200), therefore, the trachea intubation was removed
and a non-invasive ventilator for assisted ventilation was adopted.
Hydrocortisone (100 mg i.v.d. b.i.d.; Tianjin Biochemical
Pharmaceutical Co., Ltd., Tianjin, China) was administered for two
days as the result of recurrent fever on June 20, 2014. As a result
of the fever, all antibiotic treatment was discontinued on June 24,
2014. The breathing and liver function of the patient were
improved, although pyrexia remained. The patient was, therefore,
moved to the general inpatient area for further treatment.
Following transfer to the general inpatient area, a
number of examinations were performed, and the results were as
follows: Epstein-Barr virus (EBV)-DNA, 7.50×103 IU/ml;
EBV-DNA, <13 IU/ml (re-checked at Sun Yat-sen Memorial Hospital,
Sun Yat-sen University, Guangdong, China); tuberculosis T-spot
check was negative; antibodies for auto-immune diseases were
re-tested and were positive (1:100) for antinuclear antibodies,
whereas the remaining items were negative; ferritin, 2,823 mg/l.
The state of illness was improved following the administration of
various treatments (morphine and propofol); however, the recurrent
fever did not improve. The patient's condition was confusing, as he
did not respond to anti-infection treatment, and no signs of tumors
or rheumatoid-associated features were observed during the disease
process. Furthermore, the high fever could not be explained.
Notably, it was determined that the patient
experienced a fever 10 years previously (July 19th, 1997) and had
been diagnosed with allergic subsepticemia syndrome at The Second
Affiliated Hospital of Guangzhou University of Chinese Medicine;
the previous medical records of the patient was obtained from the
medical record library. Following a careful review of the medical
records, it was identified that the patient had a high fever with
no response to antibiotic therapy 10 years previously; however, the
fever was relieved following treatment with dexamethasone. The
patient was diagnosed with AOSD according to the Yamaguchi criteria
(11) in 2014. The patient in the
current study met the following criteria: Fevers lasting >1
week; leukocytosis with neutrophilia; sore throat; temporal rash;
transient arthralgia; abnormal liver enzymes; polyserositis; liver
functional abnormality; splenomegaly; and negative rheumatoid
factor (12). A hormone therapy
program (prednisone acetate tablets administered at 40, 35, 30, 25,
20, 15 and 10 mg p.o. q.d. on weeks 1–8, 9, 10, 11, 12–13, 14–15
and 16, respectively) was therefore applied for further treatment.
To date, the general condition of the patient is healthy and no
further episodes of fever have been experienced.
Discussion
AOSD is difficult to diagnose, particularly when it
presents with a number of severe systemic manifestations. In the
present study, when the patient was admitted, it was difficult to
obtain an accurate diagnosis; this raises two issues. First is the
acute onset of dyspnea. ARDS is a severe complication associated
with high morbidity and mortality (9). Saving lives is the priority in patients
with acute severe ARDS. In the current study, various treatment
strategies were performed to maintain the vital signs of the
patient. As the clinicians focused on improving the dyspnea and
preventing mortality, the diagnosis of the primary disease was
initially overlooked. Secondly, the patient experienced atypical
symptoms. To date, there are no specific clinical, serological
and/or instrumental diagnostic markers for AOSD diagnosis (13). AOSD is an inflammatory disorder with
unknown etiology, and is characterized by typical but
non-pathognomonic clinical and laboratory features, which are
commonly used to classify the disease after the exclusion of
infectious, neoplastic or autoimmune disorders (14). In the current case, the clinical
manifestations of the patient were not typical, and the sore
throat, rash and joint pains did not persist for long periods of
time. The disease developed rapidly and ARDS was induced
immediately; therefore, it was difficult to obtain a diagnosis of
AOSD.
To the best of our knowledge, the association
between lung diseases and AOSD has been reported numerous times
(5,15,16), and
pleuritis associated with AOSD has been widely reported, ranging
between 12 and 53% in various studies (17,18).
Pleuritis is usually followed by pleural effusion (12). ARDS is a type of acute diffuse lung
injury characterized by severe inflammation, increased pulmonary
vascular permeability and a loss of aerated lung tissue (10). There is currently no effective
treatment for ARDS, and management of the disease is focused on
supportive therapy, avoiding complications and identifying/treating
the underlying cause (19). A
previous study reviewed numerous cases of ARDS in AOSD, and
identified that the majority of cases studied have similar clinical
and serologic symptoms (20).
Similar to the case presented in the current study, those cases
were initially misdiagnosed as infectious pneumonia, and
broad-spectrum antibiotics were initially used to treat the
patients (20); all cases showed a
good response to high dose methylprednisolone therapy (20).
In conclusion, the case in the present study is
similar to that experienced by other clinicians. It is important to
recognize that reviewing the past medical history of a patient is
required, as it can provide important information for diagnosis. In
addition, although there are a number of laboratory methods
available for providing clinical diagnoses, it is important to
differentiate false positive data and to combine laboratory data
and symptoms in order to analyze the condition of a patient
carefully. Finally, to diagnose ASOD, the possibility of tumors and
infectious diseases must be excluded. When a patient is not
responding to anti-infectious therapy, a diagnosis of AOSD can be
considered, accompanied by ARDS.
Acknowledgements
The authors are grateful to staff at the Radiology
Department at The Second Affiliated Hospital of Guangzhou
University of Chinese Medicine for their review of the imaging
diagnosis. The authors also thank Dr Yong-Liang Chu for his
assistance in the decision of the diagnosis.
References
|
1
|
Gerfaud-Valentin M, Jamilloux Y, Iwaz J
and Sève P: Adult-onset Still's disease. Autoimmun Rev. 13:708–722.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim YJ, Koo BS, Kim YG, Lee CK and Yoo B:
Clinical features and prognosis in 82 patients with adult-onset
Still's disease. Clin Exp Rheumatol. 32:28–33. 2014.PubMed/NCBI
|
|
3
|
Jamilloux Y, Gerfaud-Valentin M, Martinon
F, Belot A, Henry T and Sève P: Pathogenesis of adult-onset Still's
disease: New insights from the juvenile counterpart. Immunol Res.
61:53–62. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cheema GS and Quismorio FP Jr: Pulmonary
involvement in adult-onset Still's disease. Curr Opin Pulm Med.
5:305–309. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dua AB, Manadan AM and Case JP: Adult
onset Still's disease presenting with acute respiratory distress
syndrome: Case report and review of the literature. Open Rheumatol
J. 7:125–128. 2013.PubMed/NCBI
|
|
6
|
Hagiyama H, Koike R, Nagasaka K, Nonomura
Y, Nishio J, Nanki T, Kohsaka H, Kubota T and Miyasaka N: Two cases
of acute respiratory distress syndrome resulting from adult-onset
Still's disease. Mod Rheumatol. 13:76–80. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Suleiman M, Wolfovitz E, Boulman N and
Levy Y: Adult onset Still's disease as a cause of ARDS and acute
respiratory failure. Scand J Rheumatol. 31:181–183. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
ARDS Definition Task Force. Ranieri VM,
Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E,
Camporota L and Slutsky AS: Acute respiratory distress syndrome:
The berlin definition. JAMA. 307:2526–2533. 2012.PubMed/NCBI
|
|
9
|
Carlucci M, Graf N, Simmons JQ and
Corbridge SJ: Effective management of ARDS. Nurse Pract. 39:35–40.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ware LB: Pathophysiology of acute lung
injury and the acute respiratory distress syndrome. Semin Respir
Crit Care Med. 27:337–349. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yamaguchi M, Ohta A, Tsunematsu T,
Kasukawa R, Mizushima Y, Kashiwagi H, Kashiwazaki S, Tanimoto K,
Matsumoto Y, Ota T, et al: Preliminary criteria for classification
of adult Still's disease. J Rheumatol. 19:424–430. 1992.PubMed/NCBI
|
|
12
|
Yamaguchi M, Ohta A, Tsunematsu T,
Kasukawa R, Mizushima Y, Kashiwagi H, Kashiwazaki S, Tanimoto K,
Matsumoto Y, Ota T, et al: Preliminary criteria for classification
of adult Still's disease. J Rheumatol. 19:424–430. 1992.PubMed/NCBI
|
|
13
|
Manzini CU, Brugioni L, Colaci M, Tognetti
M, Spinella A, Sebastiani M, Giuggioli D and Ferri C: Elevated
troponin serum levels in adult onset Still's disease. Case Rep
Rheumatol. 2015:7320952015.PubMed/NCBI
|
|
14
|
Hu Q, Yan Z and Zhong J: Adult-onset
Still's disease: How to make a diagnosis in an atypical case.
Rheumatol Int. 32:3299–3302. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Qi H, Yin C, Xiao H and Duan T: A rare
case of diffuse pulmonary nodules in a patient with adult-onset
Still's disease. Intern Med. 53:1869–1872. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sato H, Yokoe I, Nishio S, Onishi T, Takao
T, Kobayashi Y and Haraoka H: A case of adult onset Still's disease
complicated with cryptogenic organizing pneumonia. Intern Med.
50:247–251. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zeng T, Zou YQ, Wu MF and Yang CD:
Clinical features and prognosis of adult-onset still's disease: 61
cases from China. J Rheumatol. 36:1026–1031. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ikeue T, Fukuhara A, Watanabe S, Sugita T,
Horikawa S, Suzuki Y, Nishiyama H and Maekawa N: A case of severe
adult-onset Still's disease presenting with pleuropericarditis.
Nihon Kokyuki Gakkai Zasshi. 44:389–393. 2006.(In Japanese).
PubMed/NCBI
|
|
19
|
Erickson SE, Martin GS, Davis JL, Matthay
MA and Eisner MD: NIH NHLBI ARDS Network: Recent trends in acute
lung injury mortality: 1996–2005. Crit Care Med. 37:1574–1579.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hu Y, Wang H and Deng J: Adult-Onset
Still's disease associated with thyroid dysfunction: Case report
and review of the literature. Open Rheumatol J. 8:9–12. 2014.
View Article : Google Scholar : PubMed/NCBI
|