Introduction
Stress-induced cardiomyopathy (SIC), also known as
takotsubo cardiomyopathy (TTC), is a type of nonischemic
cardiomyopathy that has been described in recent decades (1). Cases of SIC are increasingly reported
in the literature. This condition is characterized by acute onset
of symptoms, such as chest pain and shortness of breath, and
electrocardiogram (ECG) changes mimicking myocardial infarction
(MI), with transient but completely reversible left ventricular
(LV) dysfunction (2). SIC commonly
occurs following physical or emotional stress (3). The prevalence of TTC in the USA is
~0.02% (4), and 90% of cases occur
in women with an average age of onset between 58 and 75 years, and
only 3% of cases occurring in women <50 years of age (5). The most common presenting symptoms
include chest pain, shortness of breath and syncope. A number of
patients present with signs and symptoms of heart failure, and up
to 10% of patients may present with the signs and symptoms
characteristic of cardiogenic shock (6). Although SIC generally has a good
prognosis, intensive heart failure therapy is required for
successful convalescence (7). The
present study reports a rare case of SIC that resulted from an
infection of the upper respiratory tract in an elderly female
patient, with the aim to increase the understanding of the
characteristics of SIC due to infection.
Case report
A 68-year-old female was admitted to The First
Affiliated Hospital of Dalian Medical University (Dalian, China) in
February 2015, with symptoms of chest stuffiness and dyspnea that
persisted for 2 days. The patient did not suffer from hypertension,
diabetes or chronic kidney disease, and did not have a history of
smoking. Approximately 10 days prior to admission, the patient
presented with fever, cough and expectoration, and was diagnosed
with an infection of the upper respiratory tract. The patient's
symptoms improved after receiving antibiotic and anti-inflammatory
therapy with cefuroxime sodium (2.0 g per day, for 7 days). Upon
physical examination, the body temperature of the patient was
36.4°C, the blood pressure was 110/70 mmHg and the heart rate was
76 bpm. No rales were identified in the lungs upon auscultation.
Written informed consent was obtained from the patient prior to
publication of this study.
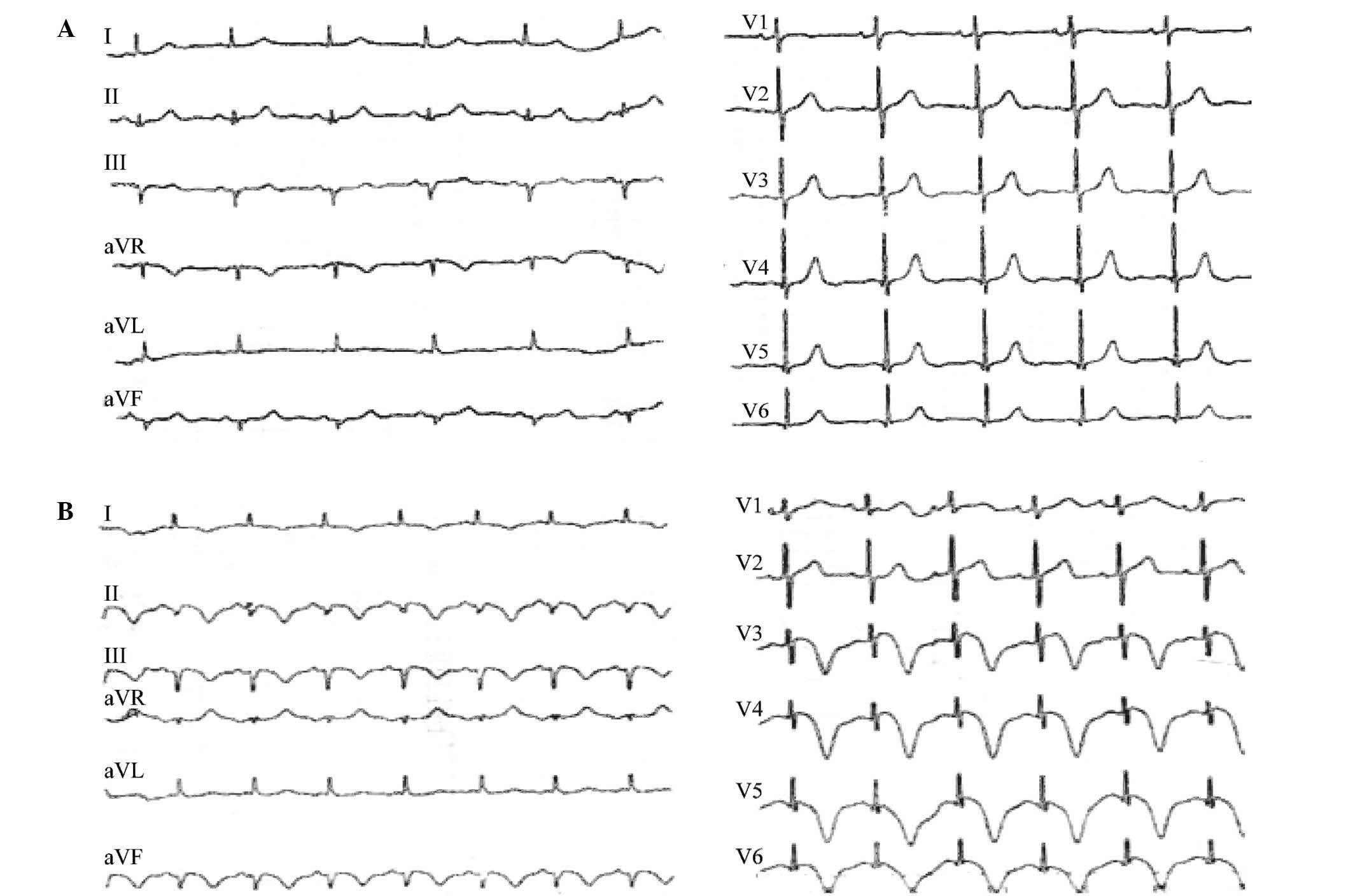
An ECG performed 10 days prior to admission appeared
to be normal, and showed negative T-waves in the leads II, III, aVF
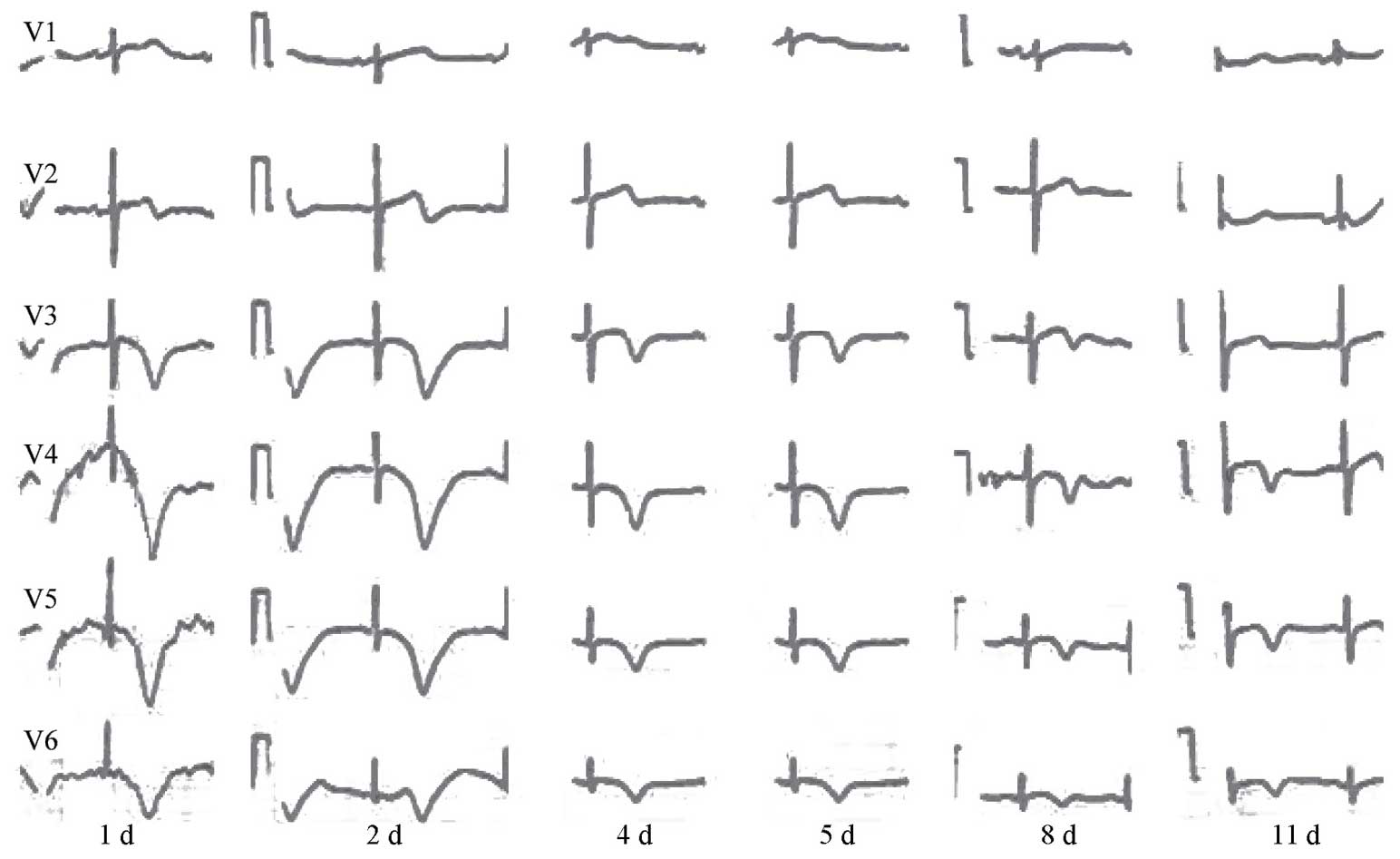
and V3-V6 and QT-prolongation upon admission (Fig. 1). Continuous ECG recording between
days 1 and 11 after admission demonstrated negative T-waves in the
V3-V6 leads (Fig. 2). In addition,
the troponin-I level increased to 1.66 g/l (normal value, <0.1
g/l) and the blood concentration of B-type natriuretic peptide
(BNP) level was 776 pg/ml (normal value, <100 pg/ml).
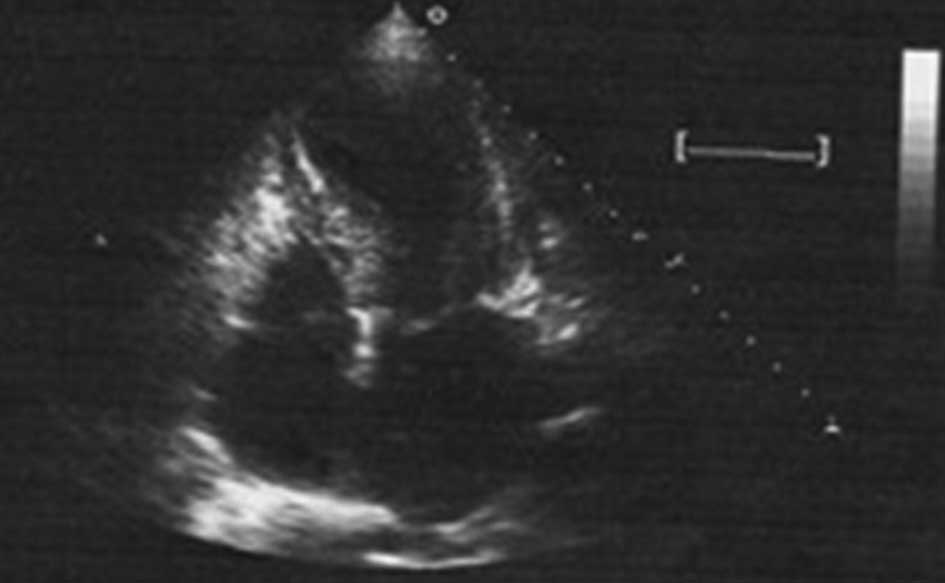
Trans-thoracic echocardiography examination
performed 3 days after admission revealed systolic dysfunction, as
observed by the LV ejection fraction (LVEF) that was 43% (normal
range, 50–70%), while apical dyskinesis and basal hyperkinesis were
also reported. These observations resembled apical ballooning,
which is a typical characteristic of SIC. Prior to diagnosis, the
patient was treated with aspirin (100 mg orally qd), clopidogrel
(75 mg orally qd,), fondaparinux (2.5 mg by subcutaneous injection
qd) and isosorbide dinitrate (20 mg by intravenous infusion qd)
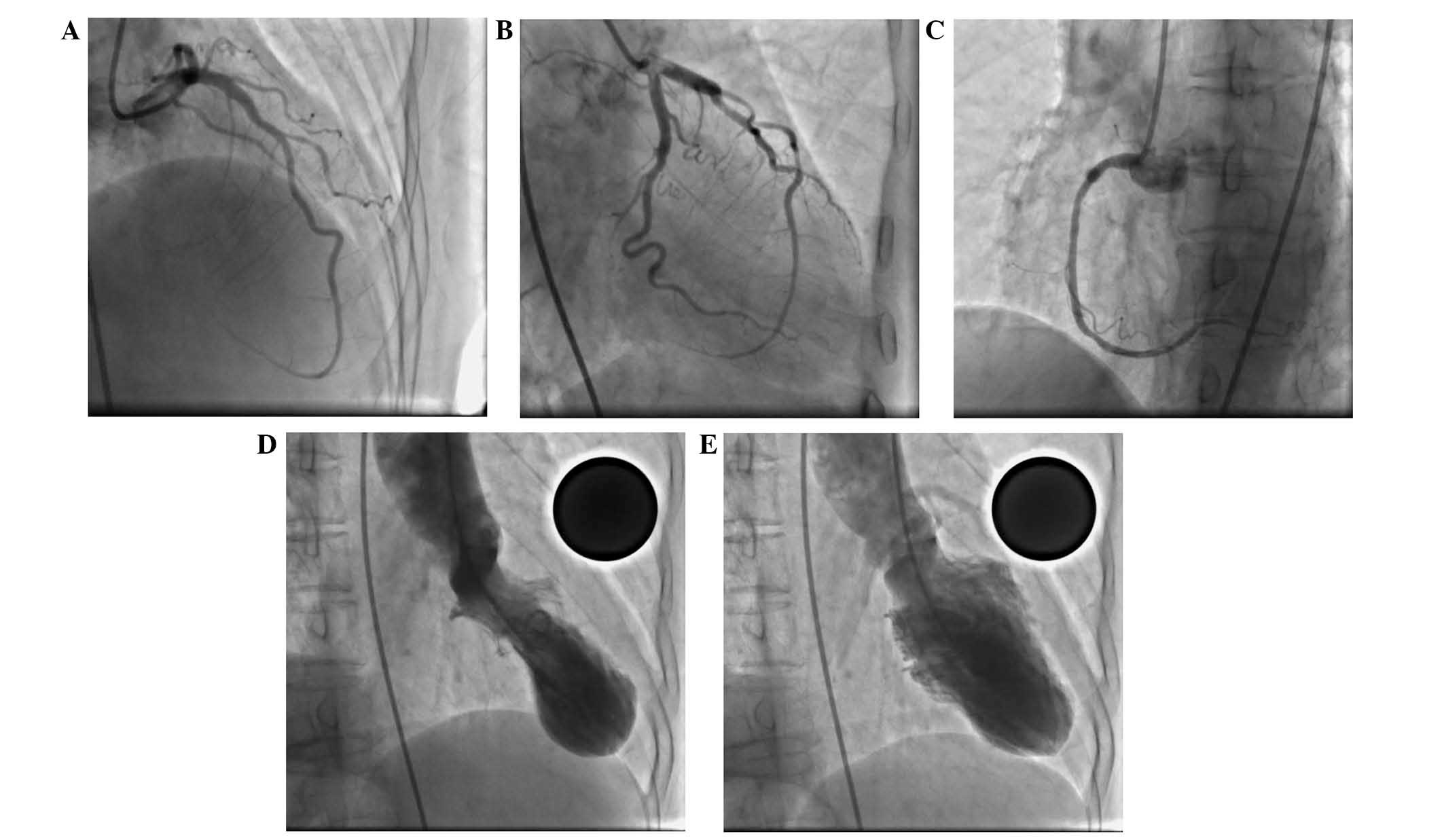
during the initial days after admission. After 2 days, coronary
angiography was performed, which showed normal coronary arteries
(Fig. 3A-C), followed by LV
angiography, which confirmed LV apical ballooning (Fig. 3D and E). Due to the limited
availability of instruments, it was not possible to conduct a
cardiac magnetic resonance imaging scan.
Based on the aforementioned characteristics, the
patient was diagnosed with SIC. Medical treatment with furosemide
(20 mg, oral twice daily), perindopril (2 mg, oral once daily) and
metoprolol (25 mg, oral twice daily) was therefore administered.
The patient gradually recovered and was discharged 11 days after
admission, when echocardiography demonstrated an improvement in
LVEF from 43 to 60% (Fig. 4).
However, the ECG still showed negative T-waves in the leads II,
III, aVF and V3-V6 on day 11 (Fig.
2). The patient was followed-up for a final time 3 months after
discharge in February 2015, and presented a normal ECG and
echocardiogram. Treatment with the above drugs was then
stopped.
Discussion
SIC, also known as TTC, is a recently-described
cause of reversible LV dysfunction, which commonly occurs following
physical or emotional stress (8). A
characteristic, non-coronary regional wall motion abnormality is
typically observed in SIC patients. Although the mechanism of SIC
remains unclear, sympathetic activity may serve a pathogenic role
in SIC, which is characterized with excessive catecholamine release
(a). Myocardial ischemia is also considered to be associated with
SIC (b). Other common characteristics of SIC at the tissue level
include myocardial edema as a sign of acute but reversible injury,
as well as diffuse inflammation in the absence of significant
necrosis or fibrosis (c). Furthermore, previous histological
analyses of the heart in SIC patients demonstrated sparse foci of
myocardial necrosis with contraction bands in the akinetic area
(d). Initial reports of SIC cases described an association with
psychological stress; however, further triggers were also
identified in later studies (9).
Prior studies have linked SIC to various other
conditions, including pulmonary infection (10), chronic obstructive pulmonary disease
(11), antitumor drug administration
(12) and even anaphylactic reaction
(13). However, to the best of our
knowledge, the present study is the first report of SIC associated
with infection of the upper respiratory tract. The association of
infection with SIC has not been previously reported in the
literature, and the mechanism through which infection induced SIC
remains unclear. It is possible that pathogenic microbes, such as
bacteria or viruses, along with an inflammatory reaction induced
sympathovagal imbalance towards adrenergic predominance. This
hypothesis is consistent with the suggestion of a previous study
that increased catecholamine levels may be responsible for SIC
(14). In addition, allergic
reactions induced by upper respiratory tract infection may be
involved in the occurrence of SIC, which may result in a delay
between infection and SIC symptoms, as observed in the current
patient.
In conclusion, the present study reported for the
first time a rare case of SIC subsequent to an infection of the
upper respiratory tract, observed in an elderly female patient.
This case will help further the understanding of SIC.
References
|
1
|
Dote K, Sato H, Tateishi H, Uchida T and
Ishihara M: Myocardial stunning due to simultaneous multivessel
coronary spasms: A review of 5 cases. J Cardiol. 21:203–214.
1991.PubMed/NCBI
|
|
2
|
Hurst RT, Prasad A, Askew JW, Sengupta PP
and Tajik AJ: Takotsubo cardiomyopathy: A unique cardiomyopathy
with variable ventricular morphology. JACC Cardiovasc Imaging.
3:641–649. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Angelini P: Reverse, or inverted,
transient Takotsubo cardiomyopathy. Tex Heart Inst J. 40:60–63.
2013.PubMed/NCBI
|
|
4
|
Deshmukh A, Kumar G, Pant S, Rihal C,
Murugiah K and Mehta JL: Prevalence of Takotsubo cardiomyopathy in
the United States. Am Heart J. 164:66–71. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
5. Prasad A, Lerman A and Rihal CS: Apical
ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): A mimic
of acute myocardial infarction. Am Heart J. 155:408–17. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Templin C, Ghadri JR, Diekmann J, Napp LC,
Bataiosu R, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann
CA, et al: Clinical features and outcomes of Takotsubo (stress)
cardiomyopathy. N Engl J Med. 373:929–938. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ledakowicz-Polak A, Bartodziej J, Majos A
and Zielińska M: Inverted stress-induced cardiomyopathy as a
unusual variant of acute heart failure after cesarean delivery - a
case report. BMC Cardiovasc Disord. 16:762016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tsuchihashi K, Ueshima K, Uchida T,
Oh-mura N, Kimura K, Owa M, Yoshiyama M, Miyazaki S, Haze K, Ogawa
H, et al: Angina Pectoris-Myocardial Infarction Investigations in
Japan: Transient left ventricular apical ballooning without
coronary artery stenosis: A novel heart syndrome mimicking acute
myocardial infarction. J Am Coll Cardiol. 38:11–18. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bybee KA, Kara T, Prasad A, Lerman A,
Barsness GW, Wright RS and Rihal CS: Systematic review: Transient
left ventricular apical ballooning: A syndrome that mimics ST
segment elevation myocardial infarction. Ann Intern Med.
141:858–865. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Brunetti ND, Leva R, Passero T, Correale
M, Dioguardi E, Montrone D, De Gennaro L and Di Biase M: Transient
apical ballooning accompanying respiratory infection. Acute Card
Care. 14:96–98. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
White JM and Stewart RA: Troponin
elevation during exacerbations of chronic obstructive airways
disease due to stress cardiomyopathy. Int J Cardiol. 160:206–207.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Khanji M, Nolan S, Gwynne S, Pudney D and
Ionescu A: Tako-Tsubo syndrome after trastuzumab - an unusual
complication of chemotherapy for breast cancer. Clin Oncol (R Coll
Radiol). 25:3292013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Santoro F, Correale M, Ieva R, Caiaffa MF,
Pappalardo I, Di Biase M and Brunetti ND: Tako-Tsubo cardiomyopathy
following an allergic asthma attack after cephalosporin
administration. Int J Cardiol. 159:e20–e21. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brunetti ND, Ieva R, Correale M, De
Gennaro L, Pellegrino PL, Dioguardi E, D'Arienzo G, Ziccardi L and
Di Biase M: Combined exogenous and endogenous catecholamine release
associated with Tako-Tsubo like syndrome in a patient with
atrio-ventricular block undergoing pace-maker implantation. Acute
Card Care. 13:112–114. 2011. View Article : Google Scholar : PubMed/NCBI
|