Introduction
Primary pulmonary histoplasmosis is a lung disease
caused by the dimorphic fungus Histoplasma capsulatum, with
a worldwide incidence. It is endemic in certain areas of North
America, and was first reported in China in 1958 (1). The severity of this mycosis is
dependent upon the number of inhaled fungal particles and the
immune status of the host (2). The
morbidity and mortality rates of pulmonary histoplasmosis are low
among immunocompetent patients. However, the morbidity and
mortality rates of this mycosis are greater among immunocompromised
individuals. In China, pulmonary histoplasmosis is sporadic. By
2015, only 76 cases with complete clinical data had been reported
in the literature (3–20). Clinical presentations may include
protean symptoms of fevers, chills, malaise, weight loss, cough and
wheezing, symptoms. These are non-specific symptoms that may also
occur with multiple other diseases. The majority of affected
individuals present clinically silent manifestations and display no
apparent symptoms (3). Therefore,
misdiagnosis of pulmonary histoplasmosis as other pulmonary
diseases, including tuberculosis, is highly likely. Misdiagnosis
may delay the treatment, and the disease is fatal if left untreated
(4).
Therefore, the present study reports the case of a
patient diagnosed with pulmonary histoplasmosis. The study aimed to
increase the understanding on the disease characteristics in order
to facilitate the diagnosis and treatment of pulmonary
histoplasmosis. The patient provided written informed consent for
this case report.
Case report
A 54-year-old male patient was admitted to the
Xiangya Hospital (Changsha, China) in June 2011 with a persistent
cough that had appeared 1 week earlier due to contracting a cold.
No signs of fever, sweating, chest pain, sputum, hemoptysis or
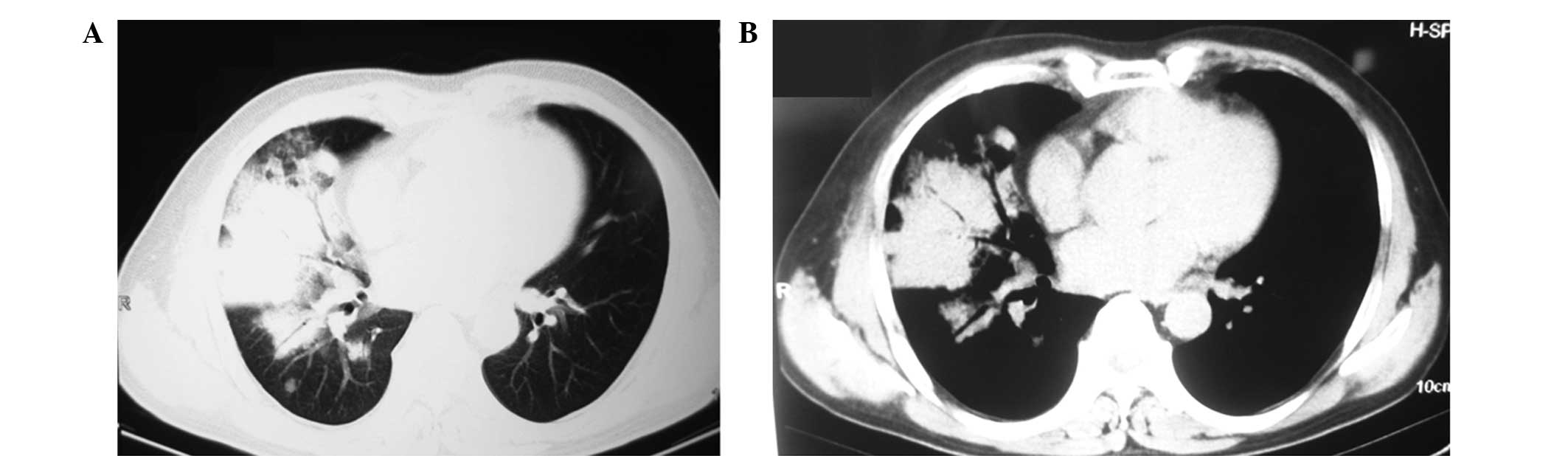
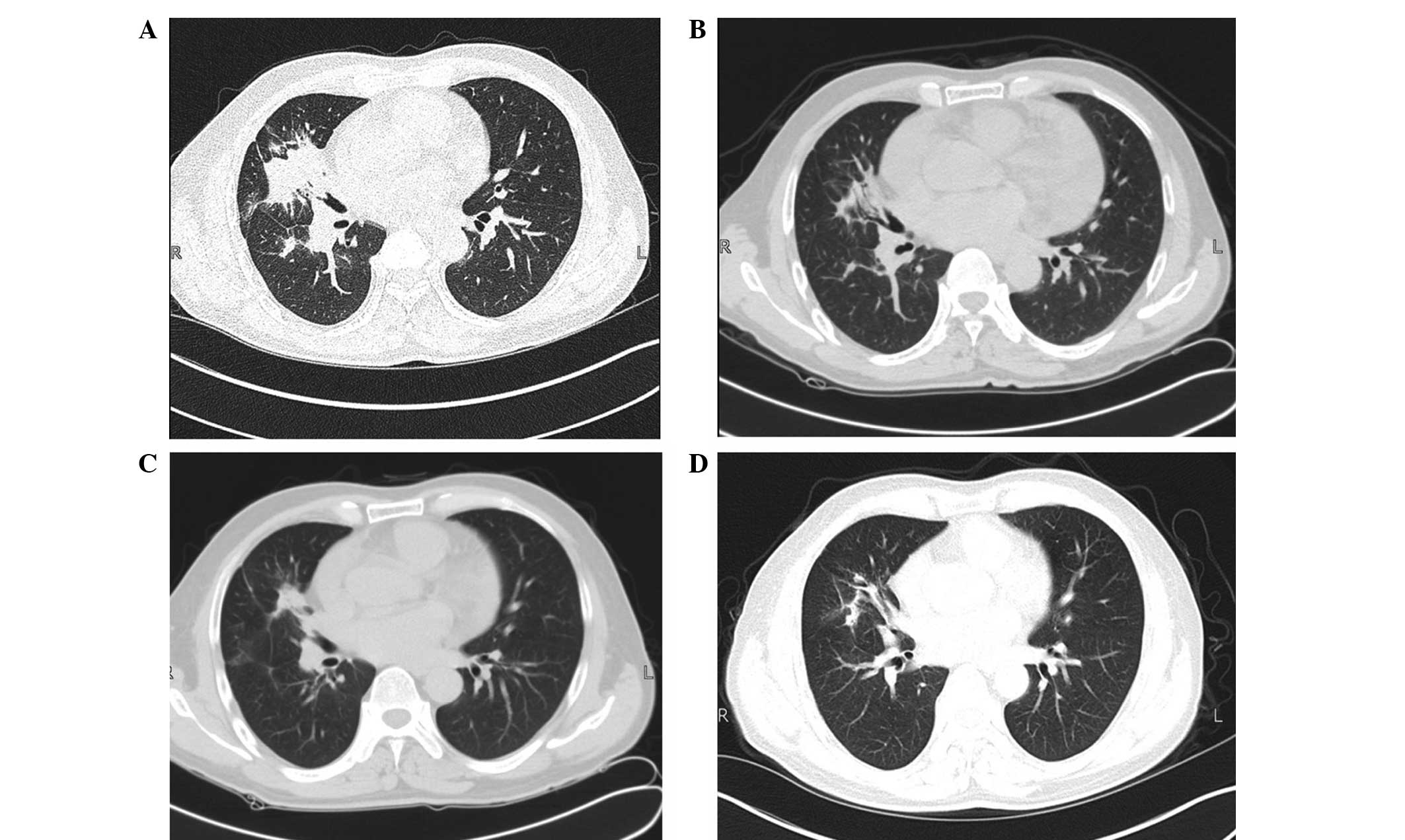
other discomfort were noted. Pulmonary computed tomography (CT)
scans conducted 2 days prior to admission detected a lump with
enhanced intensity in the upper right lung and a large mass of high
intensity in the right middle lobe with a pattern of air
bronchogram observed in the mass (Fig.
1). Based on the characteristics observed in Fig. 1, the patient was suspected of having
an infectious lung disease. Physical examination indicated the
following: Body temperature, 36.5°C; heart rate, 76 beats/min;
blood pressure, 140/80 mmHg. In addition, no superficial
lymphadenopathy was noted, while bilateral symmetry was observed in
thoracic cage. No abnormalities were identified in the bilateral
lung on percussion. Laboratory examination was also performed and
revealed the following results: White blood cell count,
9.4×109/l (normal range, 4–10×109/l); red
blood cell count, 4.5×1012/l (normal range,
3.5–5.5×1012/l); hemoglobin level, 134 g/l (normal
range, 110–150 g/l); blood platelet count, 237×109/l
(normal range, 100–300×109/l); an elevated erythrocyte
sedimentation rate, 70 mm/l (normal range, <20 mm/l); and
negativity for tuberculosis antibody. In addition, the result of a
G-test (for the detection of (1,3)-β-D-glucan, a fungal cell wall
components) was abnormal at 57.0 pg/ml (normal range, <20
pg/ml). Bronchoscopy conducted 5 days after admission detected
signs of inflammation of the bronchi, particularly the presence of
severe inflammation in the right middle lobe. Negative acid-fast
staining of the bronchus secretion was observed. Pathological
examination under bronchoscopy revealed chronic mucosal
inflammation in the branches of the right middle lobe. In
combination with clinical data, the patient was preliminarily
diagnosed with bacterial pneumonia. This diagnosis was made on the
basis that lung infection is most commonly bacterial, whereas
fungal infections often occur in immunodeficient patients and the
present patient was an immunocompetent individual. Furthermore,
G-tests may produce false positive results..
The patient was treated with levofloxacin (0.6 g
once daily, intravenously; Daiichi Sankyo, Tokyo, Japan) for 2
weeks, starting from day 1 after admission; however, the symptoms
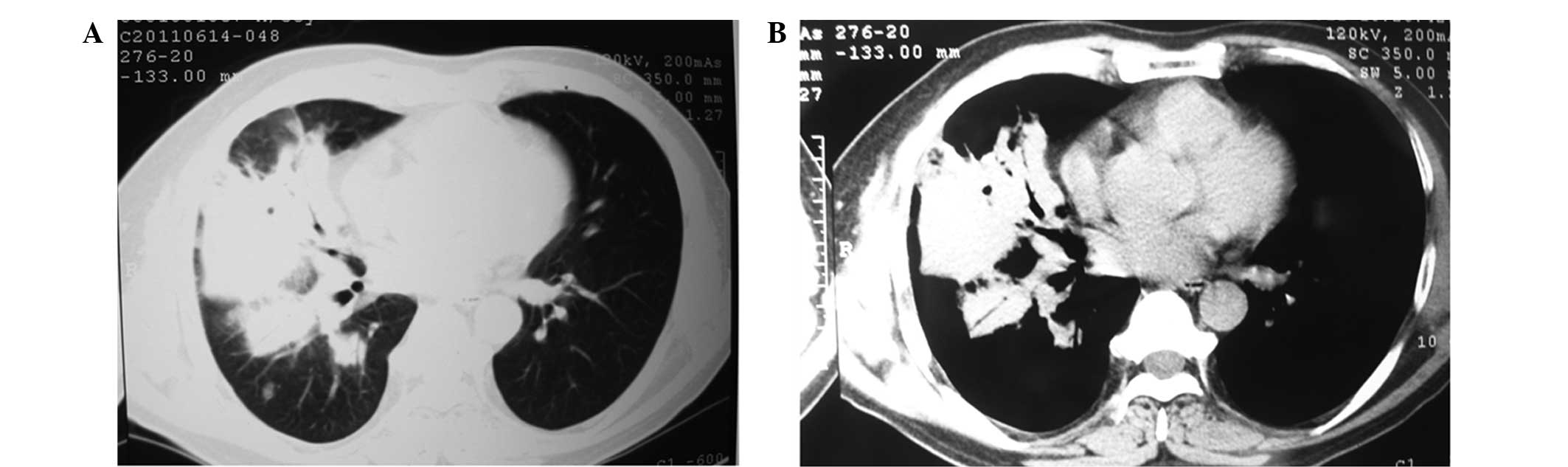
were not alleviated. Lung CT scans 12 days after admission revealed
that the infectious lesions increased in number and in size, as
shown in Fig. 2. CT-guided needle
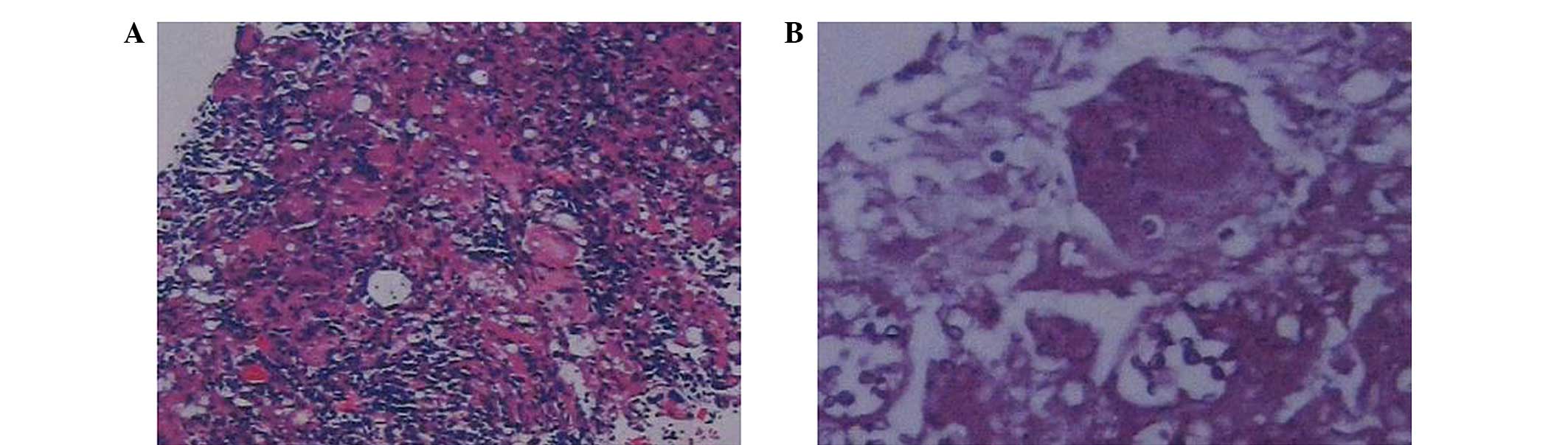
lung aspiration biopsy was then performed. Subsequent pathological
examination revealed signs of granulomatous inflammation in the
right middle lung, as shown in Fig.
3. Based on the findings of CT scans and hematoxylin-eosin
staining, the patient was suspected with histoplasmosis.
Subsequently, the patient was diagnosed with pulmonary
histoplasmosis, which was confirmed by the aforementioned imaging
and pathological findings.
Following diagnosis, the patient was treated with
itraconazole (Janssen Pharmaceuticals, Inc., Titusville, NJ, USA)
for 2 weeks, starting from 15 days after admission. The dosage was
200 mg, by intravenous infusion, twice daily for the first 2 days
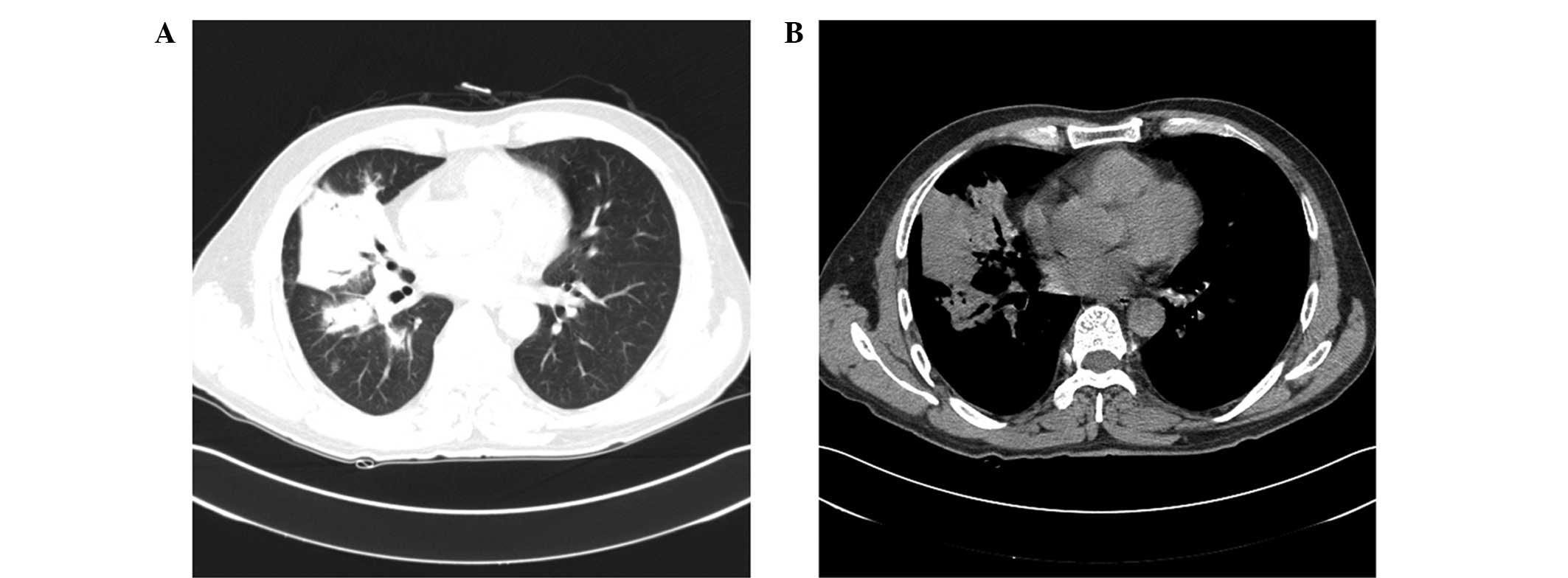
and 200 mg once daily thereafter. Subsequent lung CT scans
conducted 4 weeks after admission revealed that the pulmonary
infection was alleviated (Fig. 4),
and the symptom of cough disappeared; thus, the patient was
discharged from hospital. Subsequent to discharge, the treatment
was altered to oral administration of itraconazole only (200 mg,
twice daily, orally).
A further three rounds of lung CT scans performed in
September 2011, November 2011 and February 2012 demonstrated that
the pulmonary lesions were gradually adsorbed, as illustrated in
Fig. 5A-C, respectively. A second CT
examination scan in February 2012, 10 days after the previous one,
revealed that all the lesions in the lung had almost disappeared
(Fig. 5D); therefore, oral use of
itraconazole was discontinued.
Discussion
Primary pulmonary histoplasmosFis is a primary lung
disease caused by infection with fungus Histoplasma
capsulatum. Histoplasma capsulatum is a thermally
dimorphic fungus, found in soil, caves and abandoned constructions
that are enriched in bat or bird excrement. .Infection with
Histoplasma capsulatum occurs by the inhalation of
microconidia or mycelial fragments, which then settle in the host's
lungs and convert to yeast forms. The invasion of this fungus is
intimately associated with the host immunity. If the patient has
strong cellular immunity, then macrophages, epithelial cells and
lymphocytes can eliminate the fungi. However, in immunocompromised
individuals, Histoplasma capsulatum disseminates to a
variety of organs, including the bones, spleen, liver, adrenal
glands and mucocutaneous membranes, resulting in progressive
disseminated histoplasmosis (21).
In the present study, ‘pulmonary histoplasmosis’ was
selected as the keyword to search the literature for relevant
studies published between 1990 and 2015. The CNKI, VIP and Wanfang
databases were searched for relevant studies. In addition, the
PubMed database was searched with ‘pulmonary histoplasmosis’ and
‘China’ as search terms. Exclusion criteria were as follows: i)
Cases who were repeatedly reported; ii) cases with pulmonary
histoplasmosis evolving into disseminated histoplasmosis; and iii)
cases with incomplete clinical data. In total, 18 eligible studies
reporting 76 cases were identified and included for systematic
review (3–20). Complete clinical data, including age,
gender, risk factors, primary disease, clinical manifestation,
misdiagnosis, confirmed diagnosis, treatment and prognosis were
pooled and evaluated. Exclusion criteria were as follows: i) Cases
who were repeatedly reported; ii) cases with pulmonary
histoplasmosis evolving into disseminated histoplasmosis; and iii)
cases with incomplete clinical data. Subsequent to case screening,
a total of 76 patients, including 40 male and 36 female aged 27–69
years, were eventually recruited for subsequent analysis.
Among these patients, 52 cases were found to present
increased risk factors or primary diseases, 5 cases were treated
with glucocorticoid therapy or chemotherapy, and 1 case was orally
treated with immunosuppressive agents for an immunodeficiency
disease. In total, 46 patients were complicated with alternative
diseases or high risk factors, including diabetes mellitus, viral
hepatitis, tuberculosis, history of surgery and contact with
poultry. However, the case reported in the present study had seldom
contacted with duck, swine, cattle and other poultry, and had no
history of any systemic disorders or use of immunosuppressive drugs
prior to onset. The environment in which the present patient worked
was not likely to have caused infection with Histoplasma
capsulatum spore, suggesting that not all cases of pulmonary
histoplasmosis have contact with the fungal spore or exposure to
high risk factors.
Previous studies demonstrated that the symptoms of
pulmonary histoplasmosis greatly vary, and ~95% of patients
diagnosed with pulmonary histoplasmosis present with atypical
clinical manifestations (3–15). Common symptoms observed in the
eligible studies mainly included fever in 11 cases, chest pain in 6
cases and other respiratory symptoms in 13 cases. However, in the
current report, the patient solely presented with cough without
apparent pulmonary infection.
The imaging manifestations of patients with
pulmonary histoplasmosis are significantly diverse. Among the 77
cases, which included the 76 previous cases (3–20) and
the patient in the present study, nodular or lump lesions were
noted in 50 patients (64.9%), pneumonia-like exudative lesions were
noted in 19 patients (24.7%) and different shapes of lung lesions
were detected in 8 patients (10.4%) (22). Based on the findings of the present
literature review, the following lung CT manifestations can be
summarized for cases of pulmonary histoplasmosis: i) Cases with a
short medical history of the disease are predominantly manifested
as multiple sporadic exudative lesions of varying sizes and
indistinct boundary. By contrast, cases with a long history of
pulmonary histoplasmosis present with nodular lesions with an
explicit boundary or Histoplasma capsulatum-infected tumors,
or both; ii) sporadic or multiple lesions are frequently noted in
the middle upper lobe of bilateral lungs; iii) pneumonia-like
lesions, nodular lesions or both are observed; iv) exudates
surround the pathological changes; v) the intensity enhancement is
not evident; vi) pleural thickening is noted rather than pleural
traction; and vii) the disease has a slow course. In the current
study case report, the patient was found to have lump lesions in
the right middle lung and exudates surrounding the lesions with
insignificant enhancement. Initially, the present patient was
misdiagnosed with bacterial pneumonia.
Lung tissue biopsy and fungal culture have been
widely recognized as the gold standards for diagnosing pulmonary
histoplasmosis (23,24). Among the 77 cases enrolled in the
present study, 74 cases were diagnosed by lung tissue biopsy, while
the remaining 3 cases were diagnosed by fungal culture. However,
the fungal culture endured for at least 3 weeks and the positive
rate was not adequately high; therefore, it has limited application
in clinical practice (3–20). Similarly, the patient in the present
case study was misdiagnosed with infectious pneumonia and showed no
improvement following anti-infectious medication therapy.
Subsequently, CT-guided percutaneous lung aspiration biopsy was
conducted, which confirmed the diagnosis of pulmonary
histoplasmosis. Consequently, bronchoscopy or CT-guided
percutaneous lung aspiration biopsy is recommended to obtain
histopathologic evidence and enhance the diagnostic accuracy when
the diagnosis is ambiguous and undetermined.
According to the practice guidelines for
histoplasmosis updated by the Infectious Diseases Society of
America (25), different therapies
should be delivered for acute or chronic pulmonary and disseminated
histoplasmosis. Following literature analysis, 45 patients with
histoplasmosis were surgically treated, 20 were treated with
antifungal medication, 4 received itraconazole, 3 received triazole
and 1 received with amphotericin B. In the present study, the
patient fully recovered following the use of levofloxacin combined
with itraconazole for 2 weeks during hospitalization and oral
liquid of itraconazole for 10 months after discharge. Among the 77
cases, 38 patients were subject to follow-up for as long as >20
years. The majority of these patients were successfully treated or
improved, whereas a minority of cases progressed into disseminated
histoplasmosis or succumbed to the disease. In the current study,
the patient was followed-up for >10 months and fully recovered
following effective antifungal medication therapy.
In conclusion, the present study reported a case of
pulmonary histoplasmosis that was initially misdiagnosed as
bacterial pneumonia, and later successfully treated with antifungal
therapy. For suspicious cases based on medical history and imaging
manifestations, bronchoscopy or CT-guided lung needle aspiration
biopsy should be actively performed to facilitate the differential
diagnosis of pulmonary infection. After the diagnosis is confirmed,
effective and proper antifungal treatment should be timely
delivered upon the individual situations, aiming to enhance the
clinical efficacy.
References
|
1
|
Li Y and Chen BQ: Histoplasmosis: One case
report. Chin Med J. 44:3011958.(In Chinese).
|
|
2
|
Kauffman CA: Histoplasmosis: A clinical
and laboratory update. Clin Microbiol Rev. 20:115–132. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu XL, Shi YF and Wang HY: One case of
pulmonary histoplasmosis. Zhejiang Lin Chuang Yi Xue. 10:105–106.
2008.(In Chinese).
|
|
4
|
Chen YB, Ji C, Ling CH, Huang J and Tao
YD: Pulmonary histoplasmosis: One case report and literature
analysis. Zhonghua Jie He He Hu Xi Za Zhi. 31:941–943. 2008.(In
Chinese).
|
|
5
|
Zhu DQ, An SJ, Chen CJ and Wang SX: Two
cases of pulmonary histoplasmosis. Linyi Yi Xue Zhuan Ke Xue Xiao
Xue Bao. 13:2571991.(In Chinese).
|
|
6
|
Xie ZB, Zhong MH and Peng QZ: One case of
pulmonary histoplasmosis. Lin Chuang Nei Ke Za Zhi. 25:702–703.
2008.(In Chinese).
|
|
7
|
Cai RZ, Li G and Cai YQ: Misdiagnosis of
pulmonary histoplasmosis: One case report and literature review.
Lin Chuang Hui Cui. 27:1912–1913. 2012.(In Chinese).
|
|
8
|
Wan P, Yan QH, Gao C, Xie YS, Yin QT, Li
PL and Cao Y: Primary pulmonary histoplasmosis: One case report and
literature review. Zhonghua Jie He He Hu Xi Za Zhi. 17:232–234.
1994.(In Chinese). PubMed/NCBI
|
|
9
|
Li Q, Liu ZD, Huang Y and Hong XP: Chronic
pulmonary histoplasmosis: One case report. Zhejiang Yi Xue.
27:4482005.(In Chinese).
|
|
10
|
Sun XY and Hong Z: Imaging manifestation
of one case of pulmonary histoplasmosis. Zhonghua Fang She Xue Za
Zhi. 48:782–783. 2014.(In Chinese).
|
|
11
|
Guo M, Zheng M, Xu Y and Chen Z: One case
of pulmonary histoplasmosis suspected with lung cancer. Qiuyi
Wenyao (Xueshuban). 9:402–403. 2011.(In Chinese).
|
|
12
|
Ruan MJ, Zhu DZ, Wang XN and Wang JP:
Pulmonary histoplasmosis with clinical characteristics similar to
lung cancer. Zhong Guo Lin Chuang Yi Xue. 9:706–707. 2002.(In
Chinese).
|
|
13
|
Zheng JX and Jia YM: Clinical analysis of
four cases of reclusive pulmonary histoplasmosis. Zhenjiang Yi Xue
Yuan Xue Bao. 5:303–304. 1995.(In Chinese).
|
|
14
|
Jiang CS, Luo XR, Qiu L, Zhang QH and Wang
XS: One senior case of pulmonary histoplasmosis. Shi Yong Yi Xue Za
Zhi. 25:3012009.(In Chinese).
|
|
15
|
Zhu ST: Pulmonary histoplasmosis with
clinical characteristics similar to tuberculosis. Lin Chuang Wu
Zhen Wu Zhi. 14:1972001.(In Chinese).
|
|
16
|
Gu YH, Zhou QY, Hou X, Xu YC, Tao JQ, Yang
B, Yi J and Xu JR: Study on diagnosis and treatment of two cases of
pulmonary infections caused by histoplasma. Zhonghua Yi Yuan Gan
Ran Xue Za Zhi. 24:2477–2479. 2014.(In Chinese).
|
|
17
|
Wang LF, Guo L and Zhu M: CT features of
primary pulmonary histoplasmosis. Lin Chuang Fang She Xue Za Zhi.
31:1727–1729. 2012.(In Chinese).
|
|
18
|
Zhang F and Xu Q: One misdiagnosis case of
pulmonary histoplasmosis. Zhong Guo Wu Zhen Xue Za Zhi.
2:11172002.(In Chinese).
|
|
19
|
Shen G, Chai K, Zhang GF, Wei HQ and Yue
L: Diagnosis and treatment of pulmonary histoplasmoma: Report of 3
cases. Zhonghua Yi Xue Za Zhi. 87:760–762. 2007.(In Chinese).
PubMed/NCBI
|
|
20
|
Xu C, Ma HT, Zhao J, Ni B and Li C:
Surgical treatment of 22 cases with pulmonary histoplasmosis. Zhong
Guo Wu Zhen Xue Za Zhi. 10:6005–6006. 2010.(In Chinese).
|
|
21
|
Garfoot AL, Zemska O and Rappleye CA:
Histoplasma capsulatum depends on de novo vitamin biosynthesis for
intraphagosomal proliferation. Infect Immun. 82:393–404. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jin LL and Yang GZ: CT appearances of
primary pulmonary histoplasmosis. Zhonghua Fang She Xue Za Zhi.
43:23–26. 2009.(In Chinese).
|
|
23
|
Cuellar-Rodriguez J, Avery RK, Lard M,
Budev M, Gordon SM, Shrestha NK, van Duin D, Oethinger M and
Mawhorter SD: Histoplasmosis in solid organ transplant recipients:
10 years of experience at a large transplant center in an endemic
area. Clin Infect Dis. 49:710–716. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Grim SA, Proia L, Miller R, Alhyraba M,
Costas-Chavarri A, Oberholzer J and Clark NM: A multicenter study
of histoplasmosis and blastomycosis after solid organ
transplantation. Transpl Infect Dis. 14:17–23. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wheat LJ, Freifeld AG, Kleiman MB, Baddley
JW, McKinsey DS, Loyd JE and Kauffman CA: Clinical practice
guidelines for the management of patients with histoplasmosis: 2007
update by the infectious diseases society of America. Clin Infect
Dis. 45:807–825. 2007. View
Article : Google Scholar : PubMed/NCBI
|