Introduction
Laparoscopic inguinal hernia repair is now used as
an alternative to conventional open herniotomy in children.
Although there is ongoing debate regarding the preferred method of
inguinal hernia repair, the laparoscopic approach is gaining
popularity because of the potential advantages of faster recovery,
attenuated pain, improved cosmetics, and low recurrence rates
(1,2). Among various laparoscopic techniques,
laparoscopic percutaneous extraperitoneal closure (LPEC) of the
hernia is a recently well-developed technique (3). A previous study evaluated the safety,
efficacy, and reliability of LPEC in children (4). However, because this technique involves
percutaneous closure of inguinal hernias, the inclusion of tissues
between the skin and hernial sac, including nerves and muscles, may
cause injury and increase the postoperative morbidity in the
long-term (5).
The present study described a novel and effective
technique to close inguinal hernias with transumbilical endoscopic
surgery in girls.
Materials and methods
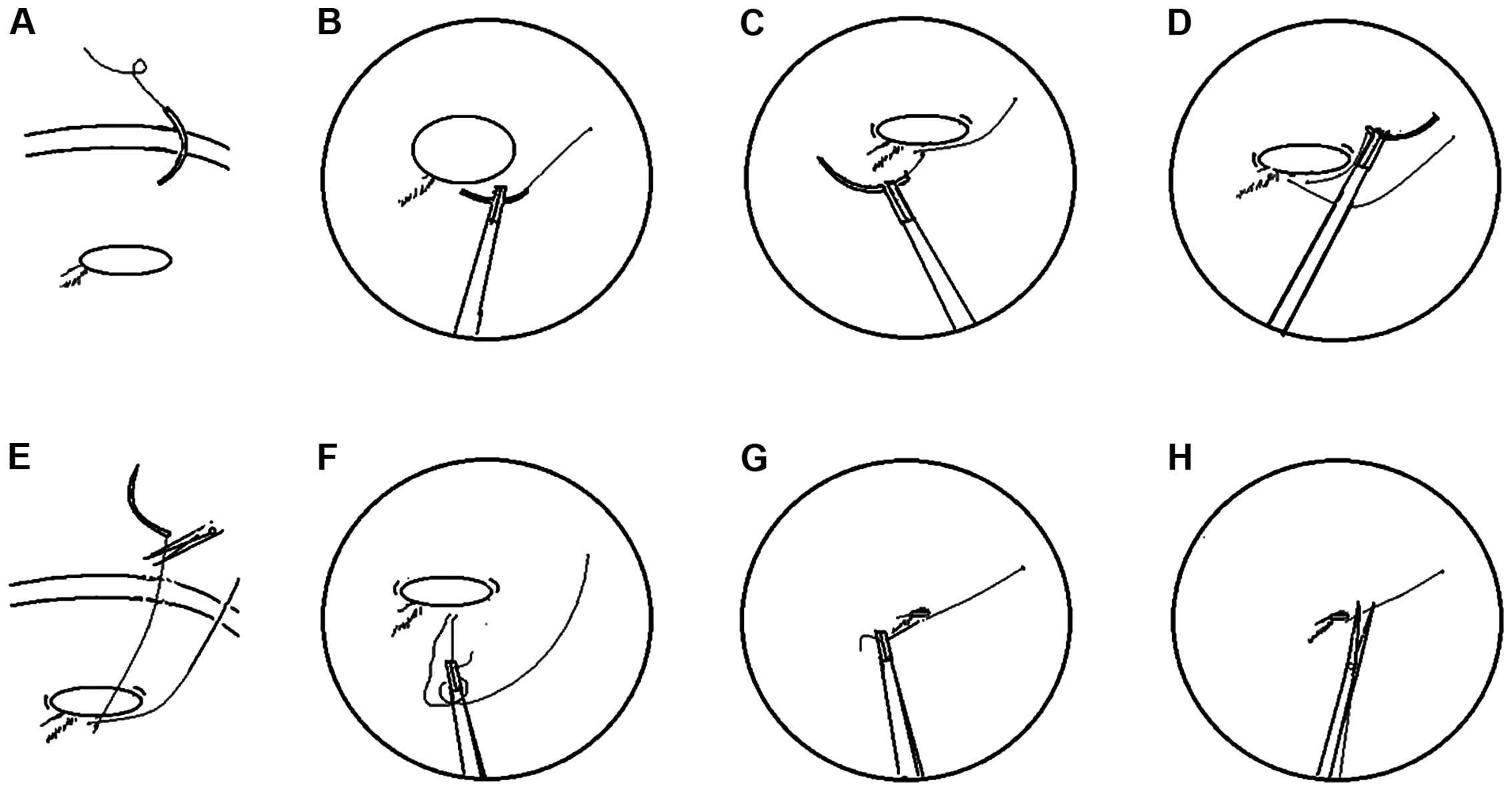
The surgical technique was modified according to our
previous study (5). Under general
anesthesia, patients were laid supine in the Trendelenburg position
at a 15° tilt. The monitor was placed at the patient's feet. The
surgeon performed the operation standing on the patient's left
side, and the camera assistant stood on the right side. Two 3- or
5-mm curvilinear intraumbilical skin incisions were made. A Veress
needle was inserted into the abdomen, and pneumoperitoneum was
established at 8 to 12 mmHg. One 3-mm trocar and one 5-mm trocar
were inserted through the umbilicus, and a 4.5-mm 0° laparoscope
(Karl Storz GmbH & Co., Tuttlingen, Germany) and a 3-mm needle
holder were placed through the umbilical incision (Fig. 1).
The needle holder was placed on the identical side
for the convenience of suturing. Under laparoscopic monitoring, a
round needle with 2–0 non-absorbable suture material was introduced
into the peritoneal cavity through the anterior abdominal wall near
the internal inguinal ring. The suture inside the peritoneal cavity
was 5 to 8 cm long, and the end of the suture was left outside the
peritoneal cavity in favor of ligation. The needle was passed
through the peritoneum to place an extraperitoneal purse-string
suture around the internal inguinal ring (Fig. 2), counterclockwise on the left and
clockwise on the right. The needle was then passed back into the
peritoneal cavity and out through the abdominal wall, and the
needle ends of the stitch were cut. The ends of the suture were
tied intraperitoneally with a one-hand tie. The operating assistant
maintained tension on the end of the suture outside the abdominal
cavity, and a 3- or 5-mm needle holder was used to manipulate the
end of the suture inside the peritoneal cavity (Fig. 3). Before the knot of the purse-string
stitch was tied, the hernia sac was compressed to expel the gas and
liquid within the sac. A triple knot was then performed.
Airtightness was confirmed by the absence of hernial sac
enlargement when the intraperitoneal pressure was increased. The
same procedure was performed on the contralateral side if the
processus vaginalis was patent. No stitching was required for the
needle and trocar puncture wound. The operative port sites were
covered with sterile aseptic absorbent gauze and not sutured. A
total of 96 female pediatric patients (age range, 8 months to 8
years; median, 3.4 years) with inguinal hernias (25 left-sided, 53
right-sided and 18 bilateral) were included in this study.
Results
From December, 2009 to August, 2015, 114 procedures
were performed in 96 female pediatric patients using the
transumbilical laparoscopic intraperitoneal closure technique. The
mean operating time was 15 min (range, 10–20 min) for the
unilateral and 24 min (range, 18–28 min) for the bilateral lesions.
All the operations were carried out by senior registrars. The
patients did well during the procedure. The findings showed less
operative bleeding, no major complications, and no secondary injury
for all the groups. The postoperative course was uneventful for all
the patients, and no severe perioperative complications were
observed. All 96 patients were admitted for day surgery and
discharged the same day. The mean follow-up period was 28 months
(range, 6–74 months). There were no cases of recurrence or
postoperative hydrocele.
Discussion
Inguinal hernia repair is the most frequently
performed procedure in children. Conventional open hernia repair is
still the gold standard for children. Laparoscopic inguinal hernia
repair in children has recently become an alternative to
conventional open herniotomy. Various single-incision laparoscopic
surgeries have been reported (5–7).
However, given the fact that laparoscopic inguinal hernia repair
technique involves percutaneous closure of inguinal hernias,
tissues between the skin and hernial sac, including nerves and
muscles, may be injured by their inclusion in the suture line,
which potentially increases postoperative morbidity in the
long-term. To preserve the advantages and overcome the limitations
of the single-port technique, we designed a novel technique with
which to close inguinal hernias with transumbilical laparoscopic
intraperitoneal closure in female pediatric patients.
This technique involves transumbilical laparoscopic
closure of inguinal hernias without the use of special instruments.
It requires one 3-mm trocar and one 5-mm trocar with a 4.5-mm 0°
laparoscope and a 3-mm needle holder. The direction of the
purse-string suture is circular, counterclockwise on the left and
clockwise on the right to avoid injury to the inferior epigastric
artery. Purse-string suturing is easier to perform in female
patients because there is no vas deferens or spermatic cord; thus,
the operator is less concerned about causing injury. After
purse-string suturing, the needle is passed out through the
abdominal wall and knots are tied intraperitoneally with a one-hand
tie to avoid injury. This technique is simple and can be performed
quickly.
Postoperative hernia recurrence is a complication of
inguinal hernias. Transumbilical laparoscopic intraperitoneal
closure in female patients provides a true high ligation analogous
to that performed in the open technique. We observed no recurrence
in the patients of the present study during our limited follow-up
period.
Scarless endoscopic abdominal surgery has become an
important concern in recent years with the development of minimally
invasive surgery. A new concept known as natural orifice
transluminal endoscopic surgery appeared with the publication of
the first experimental study by Kalloo et al (8); however, few clinical studies explaining
this method exist in the literature. The major limiting barriers
for its clinical application include access, closure, infection,
suturing technology, and orientation (9). Compared to natural orifice transluminal
endoscopic surgery, transumbilical endoscopic surgery is a less
complicated and safer method. Transumbilical endoscopic surgery
produce scarless outcome and theoretically has the same advantage
of rapid recovery. Undoubtedly, transumbilical endoscopic surgery
is an option for scarless abdominal surgery.
Compared to the current single-incision laparoscopic
extraperitoneal closure techniques, our method is easy to perform
and the instruments are readily available. Intraperitoneal ligation
may enclose the internal ring without a peritoneal gap. Our
preliminary experience showed satisfactory outcomes with the
transumbilical laparoscopic intraperitoneal closure technique for
complete endoscopic closure of inguinal hernias in female pediatric
patients. Cosmetic result and the ability to simultaneously detect
and repair contralateral patent processus vaginalis are the two
main advantages of laparoscopic surgery over open surgery. Our
results suggest that transumbilical endoscopic surgery for inguinal
hernias in female pediatric patients is safe, effective, and
reliable.
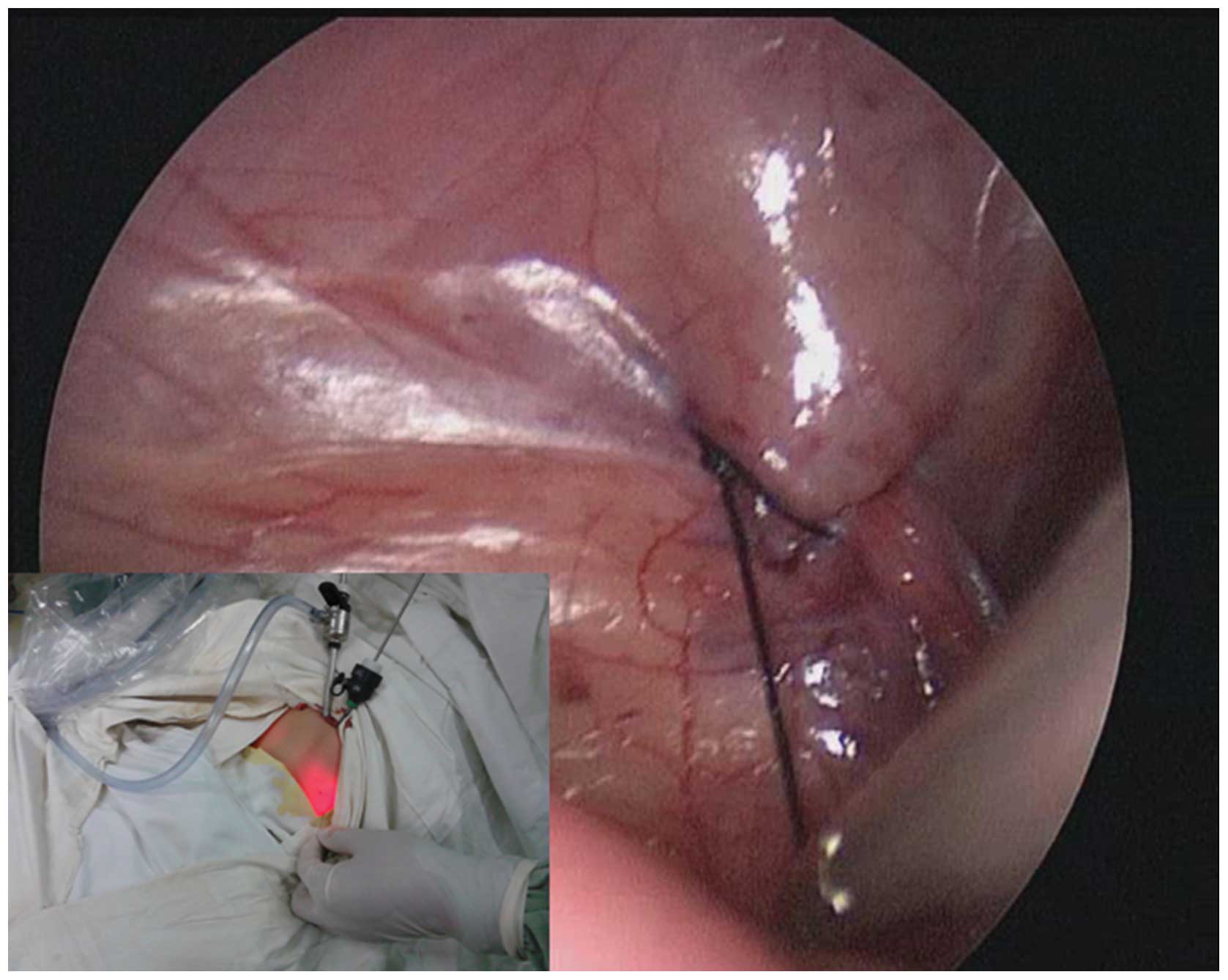
Two-port transumbilical laparoscopic intraperitoneal
closure of inguinal hernias is an effective technique in
minimal-access surgery for pediatric patients. The cosmetic results
of transumbilical laparoscopic intraperitoneal closure in the
present study were excellent because of the presence of only two
umbilical wounds for the unilateral and bilateral hernias. The
wound scar associated with the laparoscopic port was hidden in the
umbilicus, and the puncture wounds made by the devices were
minimal. This technique is more suitable for female patients with
bilateral hernias (Fig. 4).
In the present study, because the hernia sac was
closed intracorporeally, the risk of intra-abdominal complications
was not totally eliminated. Although serious complications such as
unintentional puncturing of the iliac vein and intra-abdominal
viscus did not occur, future studies with greater numbers of
patients and long-term follow-ups should be conducted.
References
|
1
|
Niyogi A, Tahim AS, Sherwood WJ, De Caluwe
D, Madden NP, Abel RM, Haddad MJ and Clarke SA: A comparative study
examining open inguinal herniotomy with and without hernioscopy to
laparoscopic inguinal hernia repair in a pediatric population.
Pediatr Surg Int. 26:387–392. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Endo M, Watanabe T, Nakano M, Yoshida F
and Ukiyama E: Laparoscopic completely extraperitoneal repair of
inguinal hernia in children: a single-institute experience with
1,257 repairs compared with cut-down herniorrhaphy. Surg Endosc.
23:1706–1712. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Li S, Li M, Wong KK, Liu L and Tam PK:
Laparoscopically assisted simple suturing obliteration (LASSO) of
the internal ring using an epidural needle: a handy single-port
laparoscopic herniorrhaphy in children. J Pediatr Surg.
49:1818–1820. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Takehara H, Yakabe S and Kameoka K:
Laparoscopic percutaneous extraperitoneal closure for inguinal
hernia in children: clinical outcome of 972 repairs done in 3
pediatric surgical institutions. J Pediatr Surg. 41:1999–2003.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chang YT: Technical refinements in
single-port laparoscopic surgery of inguinal hernia in infants and
children. Diagn Ther Endosc. 392847:1–6. 2010. View Article : Google Scholar
|
|
6
|
Wen XQ, Huang WT, Situ J, et al:
Single-port laparoscopic radical prostatectomy: initial experience
and technical points to reduce its difficulties. Chin Med J.
124:4092–4095. 2011.PubMed/NCBI
|
|
7
|
Chang Y-T, Wang J-Y, Lee J-Y and Chiou
C-S: A simple single-port laparoscopic-assisted technique for
completely enclosing inguinal hernia in children. Am J S.
198:e164–e167. 2009.
|
|
8
|
Kalloo AN, Singh VK, Jagannath SB, Niiyama
H, Hill SL, Vaughn CA, Magee CA and Kantsevoy SV: Flexible
transgastric peritoneoscopy: a novel approach to diagnostic and
therapeutic interventions in the peritoneal cavity. Gastrointest
Endosc. 60:114–117. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhu JF, Hu H, Ma YZ, Xu MZ and Li F:
Transumbilical endoscopic surgery: a preliminary clinical report.
Surg Endosc. 23:813–817. 2009. View Article : Google Scholar : PubMed/NCBI
|