Introduction
Postoperative cognitive dysfunction (POCD) describes
the memory and intellectual impairment that occurs in certain
individuals during the perioperative period (1,2). A major
risk factor for POCD is age; therefore, it is particularly
prevalent in the elderly (2). Pain
is also considered to be a risk factor for POCD as the areas of the
brain involved in pain perception and cognitive control overlap
(2,3). Total knee arthroplasty (TKA) has been
reported to be one of the most painful orthopedic surgeries
(4).
Postoperative pain is intensified by sensitization
of the pain receptors in the spinal cord and brain (5). This sensitization may be due to a
perioperative inflammatory response, in which inflammatory
mediators released at the operative site sensitize peripheral pain
receptors (6). The ensuing increased
nociceptive input to the spinal cord sensitizes the pain receptors
there and this sensitization, in turn, sensitizes the pain
receptors in the brain.
If pain impulses from the operative site were
interrupted throughout as well as following surgery, both intra-
and postoperative peripheral pain stimuli could be blocked from
transmitting to the central nervous system, thus reducing
sensitization of pain receptors in the brain. If the occurrence of
POCD is associated with the development of this sensitization, as
has been suggested previously (6),
initiating a blockade of pain transmission prior to, rather than
following, surgery may decrease the incidence of POCD.
Femoral nerve block (FNB) reduces pain transmission
from the TKA operative area (7) and
when FNB is administered during TKA, following spinal anesthesia
postoperative pain is reduced (4).
In tendon graft repair, the use of postoperative femoral nerve
infusion of ropivacaine reduces early postoperative pain (2 h
following surgery) more effectively when administered pre-emptively
rather than when administered at the end of surgery (8). It has been demonstrated that femoral
nerve infusion of ropivacaine improves pain control for one day
after TKA treatment, compared with epidural ropivacaine infusion,
which continues for 6 h (9).
Studies of POCD have been conducted at a later time
post-surgery; however, to the best of our knowledge, not during the
initial days following surgery (6,10–12).
Furthermore, to the best of our knowledge, no studies have yet
investigated the effect of pre-emptively blocking pain transmission
on acute POCD in the first days following surgery. In the present
study the effect of a femoral nerve infusion of ropivacaine on TKA
initiated prior to surgery and at the end of surgery was compared,
with regard to the incidence of POCD and pain in the initial seven
days following surgery.
Patients and methods
Patients
The present study is a prospective, randomized,
double blind, controlled study. A total of 60 patients (13 males
and 47 females) aged >65 years who underwent primary TKA under
intravenous anesthesia at the General Hospital of Ningxia Medical
University (Ningxia, China) between April and September 2014 were
enrolled in the current study. All patients were examined in
accordance with the American Society of Anesthesiologists (ASA)
physical status classification and belonged to an ASA grade II or
I. Exclusion criteria were as follows: A mini mental state
examination (MMSE) score lower than the minimum score for each
education level (illiterate, ≤17 points; primary school, ≤20
points; secondary school, ≤22 points; college, ≤23 points), nervous
system disease, serious visual disorders and inability to
communicate normally, a history of mental disease or of having
received relevant medication, coagulation disorders, opioid abuse,
inability to carry out effective oral communication with doctors,
inability to complete the MMSE, inability to undergo surgery due to
various reasons, including pulmonary infection, high blood pressure
and disturbance of blood coagulation, voluntarily withdrawal from
the study and refusal to take the MMSE. The current study was
approved by the Ethics Committee of the General Hospital of Ningxia
Medical University. Informed consent was obtained from each
participant.
Patient grouping
Patients were randomly divided into two groups: A
pre-emptive analgesia group and a control group (n=30 in each).
Continuous FNB (CFNB) was performed in the pre-emptive and control
groups, but initiated prior to surgery in the pre-emptive analgesia
group and following surgery in the control group. The same
anesthesiologist was responsible for the management of anesthesia
for all patients and the same group of orthopedic surgeons
performed TKA on all patients. The individuals collecting data and
the patients were blinded to the grouping.
Administration of anesthesia
All patients underwent surgery under intravenous
anesthesia alone. Prior to anesthetic, 1 mg penehyclidine
hydrochloride (Chengdu List Pharmaceutical Co., Ltd., Chengdu,
China) was injected intramuscularly. The patients were then taken
to surgery where the basilic vein was percutaneously cannulated
with 20 gauge intravascular catheters, and non-invasive blood
pressure, electrocardiogram, peripheral capillary oxygen
saturation, partial pressure of exhaled carbon dioxide
(PETCO2) and bispectral index (BIS) were
monitored routinely. Midazolam (0.05–0.1 mg/kg, Nhwa Pharmaceutical
Co., Ltd., Jiangsu, China), sufentanil (0.3–0.4 µg/kg, Yichang
Humanwell Pharmaceutical Co., Ltd., Yichang, China), etomidate
(0.1–0.2 mg/kg, Nhwa Pharmaceutical Co., Ltd.) and cis-atracurium
(0.15–0.2 mg/kg, Shanghai Pharmaceuticals Holding Co., Ltd.,
Shanghai, China) were injected intravenously for induction of
anesthesia. A laryngeal mask airway was applied 3 min later. Oxygen
flow was set to 1.5 l/min, tidal volume 6–8 ml/kg, respiratory rate
12–14 times/min and PETCO2 35–45 mmHg.
Anesthesia was maintained by continuous intravenous infusion of
propofol (4–8 mg/kg/h, Corden Pharma, Caponago, Italy) and
remifentanil (0.1–0.2 µg/kg/min, Yichang Humanwell Pharmaceutical
Co., Ltd., Yichang, China). Muscle relaxation was maintained by
intermittent (40–60 min) injection of cis-atracurium (0.05 mg/kg,
Shanghai Pharmaceuticals Holding Co., Ltd.). The intraoperative BIS
value was maintained at 40–60. A mean arterial pressure 20% lower
than the basal value or a systolic blood pressure <90 mmHg (1
mmHg=0.133 kPa) was considered to represent hypotension, and 3–6 mg
of ephedrine (Northeast Pharmaceutical Group, Shenyang, China) was
injected intravenously. A heart rate of <60 beats/min was
considered to indicate bradycardia and 0.25–0.5 mg atropine
(Tianjin Pharmaceutical Group Co., Ltd., Tianjin, China) was
injected intravenously. No additional cis-atracurium was injected
30 min prior to the end of surgery. Infusion of propofol and
remifentanil was stopped at the end of surgery and neostigmine
(0.02 mg/kg, Runhong Pharmaceutical Co., Ltd., Xinzheng, China) and
atropine (0.01 mg/kg, Tianjin Pharmaceutical Group Co., Ltd.) were
injected intravenously to antagonize the residual effect of the
muscle relaxants. The laryngeal mask was removed and the patient
was transferred to post-anesthesia care unit until the recovery of
consciousness, determined by the patient being able to open their
eyes upon instruction, tidal volume of unassisted respiration ≥6
ml/kg and a respiratory rate ≥10 times/min. When completely awake,
patients returned to the orthopedic ward and were discharged after
7–10 days of recovery.
FNB and perioperative pain
control
For the FNB procedure, patients were placed in the
supine position with the affected leg slightly abducted. The
femoral artery was palpated under the inguinal ligament and the
entry point was marked: 1 cm lateral to the femoral artery parallel
to the upper part of the pubic symphysis. A Braun nerve stimulator
(B. Braun Medical, Ltd., Melsungen, Germany) with a pulse duration
of 0.1 msec and a stimulation frequency of 2 Hz was used to assist
with positioning of the entry point. The initial current was 1 mA
and the threshold current at the time of local anesthetic injection
was 0.3 mA. A needle was inserted vertically into the previously
marked entry point and if a current <0.3 mA could still induce
quadricep contraction and patella fluctuation, 15 ml of a 1:1
mixture of 2% lidocaine (Shiyao Yinhu Pharmaceutical Co., Ltd.,
Yunchen, China) and 0.75% ropivacaine (AstraZeneca AB, Sodertalje,
Sweden) was injected. The needle was inserted slowly, 2 mm into the
entry point at a cephalic angle of 30° and the core was withdrawn.
A 20G cannula for arterial puncture was placed into the core and 5
ml 1:1 lidocaine/ropivacaine mixture was injected again. A
disposable patient controlled analgesia pump was connected (0.75%
ropivacaine 20 ml + sufentanil 40 µg) and used for 50 h with
self-controlled femoral nerve analgesia following surgery.
Intraoperative multi-point intraarticular injection
of ropivacaine (150 mg/100 ml) was also conducted. The injection
sites were the posterior and medial sides of the knee joint, medial
and lateral sides of the articular capsule, origin and insertion
sites of the collateral ligaments, extensor apparatus and
infrapatellar fat pad and subcutaneous tissue. Other perioperative
pain control managements included cyclooxygenase 2 (COX-2)
inhibitors (parecoxib sodium or celecoxib; Pharmacia and Upjohn
LLC, Kalamazoo, MI, USA) administered following surgery twice a day
for all patients.
Patient clinicopathological
characteristics
Age, gender, education level, body mass index (BMI),
comorbidities, anesthesia duration, operative time, anesthetic
dosage, tourniquet time and perioperative analgesic use were
recorded (Table I).
 | Table I.Baseline characteristics of study
population. |
Table I.
Baseline characteristics of study
population.
| Parameter | Pre-emptive
(n=30) | Control (n=30) |
|---|
| Age, years | 68.6±5.6 | 67.8±4.3 |
| Male (%) | 7 (23.3) | 6 (20.0) |
| BMI,
kg/m2 | 25.3±3.4 | 26.1±3.6 |
| Anesthesia time,
min | 128.2±24.4 | 123.2±22.5 |
| Operative time,
min | 90.2±17.4 | 92.3±15.6 |
| Tourniquet time,
min | 60.9±17.9 | 60.6±12 |
| ASA grade (%) |
|
|
| I | 5 (16.7) | 6 (20.0) |
| II | 25 (83.3) | 24 (80.0) |
| Education (%) |
|
|
|
Illiteracy | 12 (40) | 10 (33.3) |
|
Elementary school | 8 (26.7) | 7 (23.3) |
| High school or
above | 10 (33.3) | 13 (43.3) |
| Comorbidity (%) |
|
|
|
Cardiovascular disease | 3 (10.0) | 3 (10.0) |
|
Hypertension | 12 (40.0) | 12 (40.0) |
|
Diabetes | 4 (13.3) | 4 (13.3) |
Pain ratings
The Visual Analog Score (VAS) at rest and during
exercise was used to estimate pain strength. In this system, the
patient rates pain on a score of 0–10, 0 representing no pain and
10 representing the worst pain imaginable. VAS scores were recorded
at rest and during activity for patients in both groups prior to
surgery and 1, 3, 5 and 7 days following surgery. For these
ratings, pain during rest refers to the severity of pain after 30
min rest following joint movement; pain during exercise refers to
pain when the knee joint performs maximum flexion. Functional
exercise of the knee joint was started day 1 postoperation. The
patients were asked to stand for 3–5 min and the exercise training
included quadricep and tibialis anterior muscle isometric
contraction. From day 2 postoperation, exercise training included
knee extension and flexion exercises to straight leg raising, 4–5
times (at least 15 min per leg raising) a day.
Cognitive function and
dysfunction
The MMSE was used to evaluate cognitive function
prior to surgery to provide a baseline value and was measured 1, 3,
5 and 7 days following surgery (13). A decrease in the MMSE scale was used
to determine the presence of POCD. Previous studies have used a
postoperative MMSE score >1 standard deviation below the
preoperative score to define POCD (14). In the present study, 1 standard
deviation of preoperative MMSE score is 2 points, so a
postoperative MMSE score ≥2 points lower than the preoperative
score was defined as POCD.
Statistical analysis
Data regarding patient age, BMI, anesthesia time,
surgery time and tourniquet-bearing time were presented as mean ±
standard deviation and an independent t-test was used for
statistical examination. Due to the skewed distribution of the
data, data for drug administration are presented as median and
interquartile ranges, and the Wilcoxon rank-sum test was used for
statistical examinations. Categorical variables were expressed by
count (%) and examined statistically using the χ2 test.
Group differences for time trends among VAS at rest and during
activity, and the MMSE were examined by generalized estimation
equation. Interactions within each corresponding time and group
were included in the models. If a significant interaction item was
revealed followed by a Bonferroni post-hoc test. All statistical
assessments were evaluated using SPSS software, version 22 (IBM
SPSS, Armonk, NY, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
Case selection
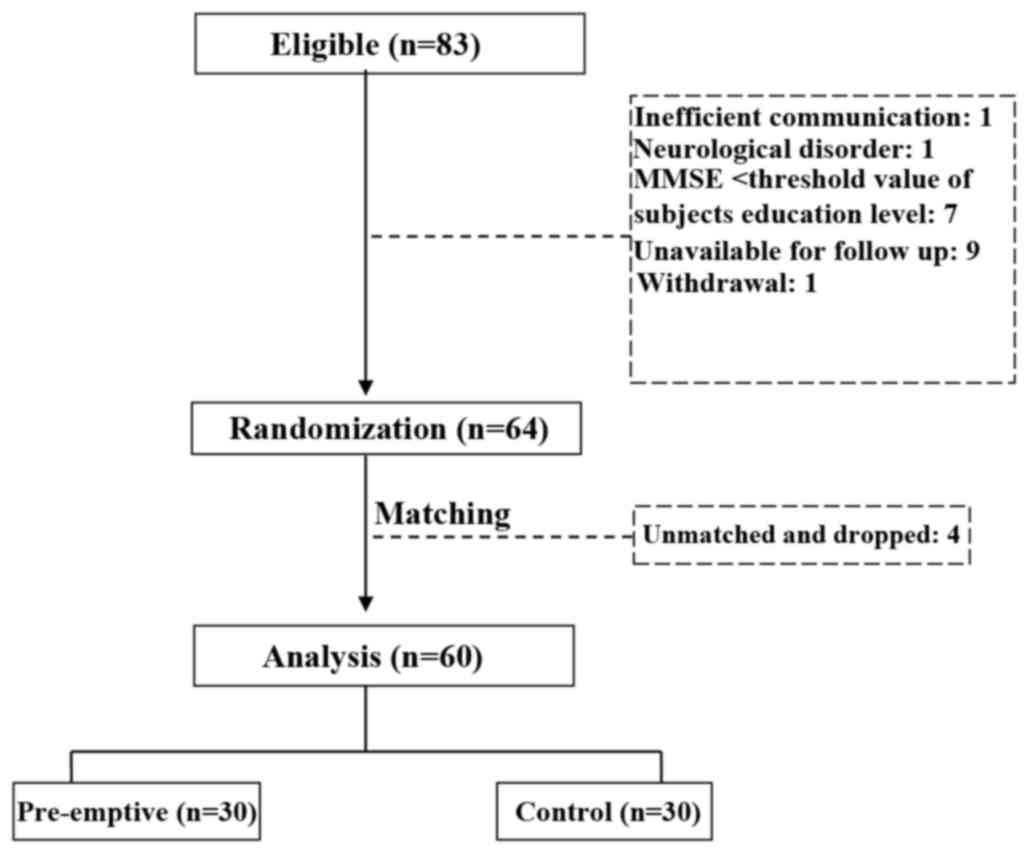
A total of 83 patients were initially enrolled.
Patients were excluded due to an inability to communicate normally
(one case), MMSE score lower than the threshold value of the
individual's education level (seven cases) and the presence of
neurological disorder (one case). In addition, nine patients were
excluded because they could not cooperate on the follow-up survey
and one patient voluntarily withdrew from the study. Finally, four
patients were dropped following frequency matching with three
comorbidities (cardiovascular disease, hypertension and diabetes).
Therefore, a total of 60 patients were included in the final
analysis of the results and 30 patients were included in each group
(Fig. 1).
Patient demographics
Patients' baseline characteristics are summarized in
Table I. There were no significant
differences between the two groups in any baseline characteristics.
Among all patients, 21.7% were males, 81.7% had ASA at II and 61.7%
had an education level of elementary school or below. In the study
population, the prevalence of cardiovascular disease was 10%,
hypertension was 40% and diabetes was 13.3%. The mean age, BMI,
anesthesia time, surgery time and tourniquet-bearing time were
68.2±5.0 years, 25.7±3.5 kg/m2, 125.7±23.4, 91.3±16.4
and 60.7±15.1 min, respectively.
Medicine administration between study
populations
Midazolam, sufentanil, cis-atracurium, etomidate,
propofol, remifentanil, celecoxib and parecoxib sodium were used in
the present study (Table II).
During the perianesthesia period, the dose of remifentanil used in
the pre-emptive analgesia group was significantly lower, compared
with the control group (P=0.019). No significant differences
between groups were observed in the doses of any other
medication.
 | Table II.Medication administered to individuals
in the present study. |
Table II.
Medication administered to individuals
in the present study.
| Parameter | Pre-emptive
(n=30) | Control (n=30) | P-value |
|---|
| Midazolam, mg | 4 (3–4) | 4 (3–4) | 0.893 |
| Sufentanil, mg | 25 (20–30) | 25 (20–30) | 0.464 |
| Cisatracurium
besylate, mg | 20 (15–20) | 20 (15–20) | 0.804 |
| Etomidate, mg | 18 (10–20) | 20 (10–20) | 0.107 |
| Propofol, mg | 400 (350–500) | 480 (400–500) | 0.124 |
| Celecoxib, g | 6 (4.8–6) | 6 (5.4–6) | 0.499 |
| Parecoxib sodium,
mg | 40 (40–40) | 40 (40–80) | 0.299 |
| Remifentanil, mg | 1.8 (1.5–2.0) | 2.0 (1.8–2.0) |
0.019a |
Differences in the incidence of
POCD
In each group, the incidence of POCD was similar on
day 1 (Table III) and then
decreased with time. This decrease was faster in the group
administered a pre-emptive FNB: By day 3 the incidence in this
group was significantly lower than in the control group (6.7 vs.
26.7%, P=0.038; Table III). By day
5, there were no cases of POCD in the pre-emptive analgesia group
and no cases of POCD in the control group by day 7.
 | Table III.Occurrence of POCD in patients
following surgery. |
Table III.
Occurrence of POCD in patients
following surgery.
| P-value | Time and group | Pre-emptive
(n=30) | Control (n=30) |
|---|
| Day 1 |
|
| 0.999 |
| No
POCD | 19 (63.3) | 19 (63.3) |
|
| POCD | 11 (36.7) | 11 (36.7) |
|
| Day 3 |
|
| 0.038a |
| No
POCD | 28 (93.3) | 22 (73.3) |
|
| POCD | 2 (6.7) | 8 (26.7) |
|
| Day 5 |
|
| 0.313 |
| No
POCD | 30 (100.0) | 29 (96.7) |
|
| POCD | 0 (0.0) | 1 (3.3) |
|
| Day 7 |
|
| NA |
| No
POCD | 30 (100.0) | 30 (100.0) |
|
|
POCD | 0 (0.0) | 0 (0.0) |
|
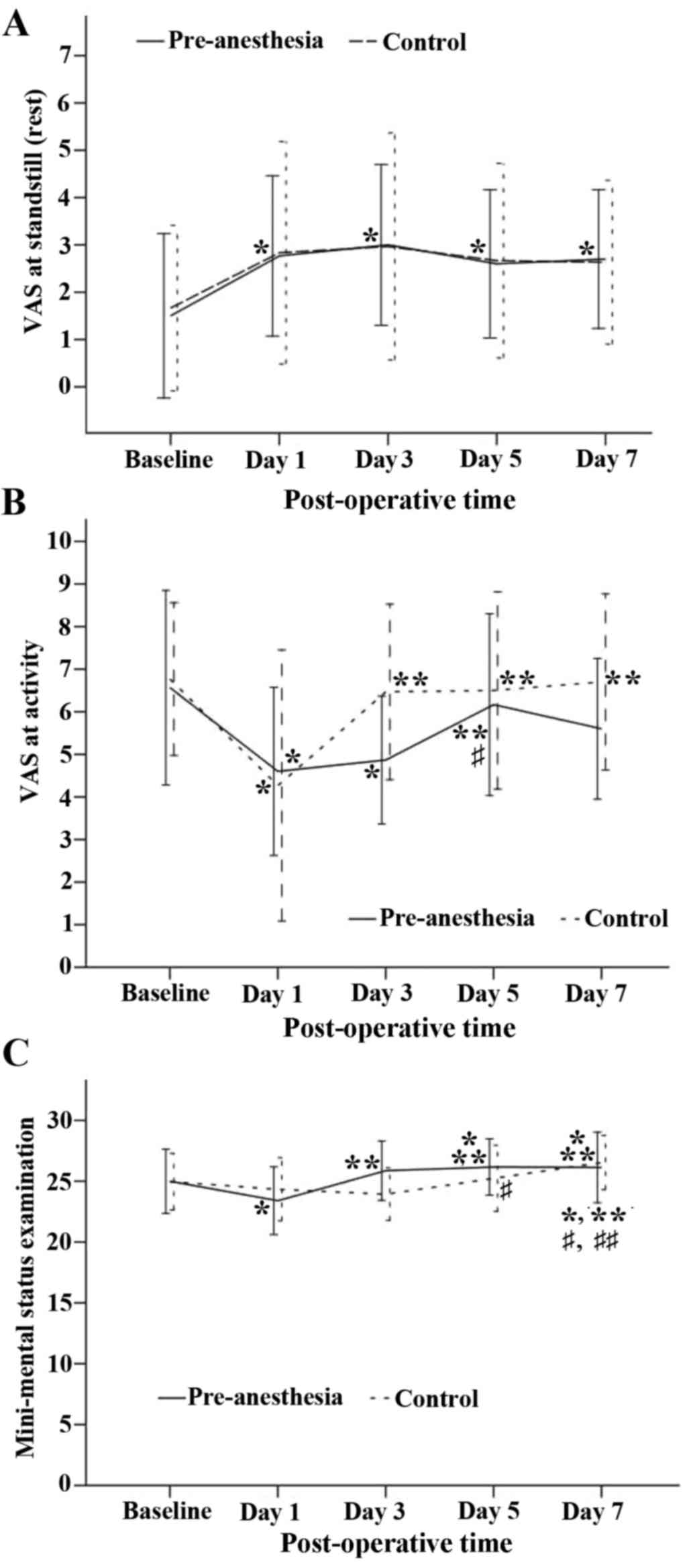
Differences in the VAS score
Pain (based on the VAS score) at rest and during
exercise for the pre-emptive and control groups is presented in
Fig. 2A and B. Pain at rest
(standstill) increased significantly following surgery in both
groups (P<0.05) and remained at stable levels in subsequent days
(Fig. 2A). However, differences in
pain intensity between the groups at each time point were not
significant (Fig. 2A). Average pain
intensity during days 1–7 in the two groups was scored as ~3, a
level considered moderate. By contrast, pain during activity
decreased from a relatively high preoperative level (6–7) to a
level near 4 on day 1, then increased significantly in the control
group from day 3 onward, but did not exhibit a significant increase
in the pre-emptive FNB group until day 5 (Fig. 2B).
Differences in MMSE
Changes in the MMSE over time for the two groups are
presented in Fig. 2C. The time trend
for the two groups was similar (P=0.568), but the MMSE scores
differed significantly by group (P<0.05). Both groups
demonstrated a decrease from baseline on day 1, but the pre-emptive
FNB group exhibited recovery from this decrease by day 3, while it
took the control group until day 7 to achieve recovery from the day
1 value (Fig. 2C).
Discussion
The present study demonstrated that in TKA, the
pre-emptive infusion of remifentanil to the femoral nerve decreased
VAS scores during activity more than femoral nerve infusion
initiated at the end of surgery. These results suggest that a
pre-emptive femoral blockade of pain impulse transmission during
surgery prevented CNS hypersensitization.
Throughout the present study, patients in the
pre-emptive analgesia group had a lower VAS score (postoperative
pain sensitivity) during activity than patients in the control
group with the exception of day 1. The incidence of POCD at day 1
following TKA surgery was similar in both groups. However, at day 3
following surgery, the incidence of POCD was decreased in the
pre-emptive analgesia group compared with the post-surgery
analgesia group. This difference was not significant; however, it
suggests that the pain control of pre-emptive analgesia may promote
an early recovery of postoperative cognitive function. This mild
improvement in early postoperative cognitive function recovery may
therefore reduce duration of hospitalization and total medical
expenses of the individual. The present study used a short time
period following surgery to measure POCD; this allowed the
observation of a short-term phenomenon that studies at a later time
period may not detect. An advantage of using this early time period
is that there is a low rate of patients lost to follow-up (15).
In the present study, other factors that may affect
POCD were controlled; these include demographic risk factors
including age, hypertension, diabetes and coronary heart disease
(16). The same anesthesiologist
managed the anesthesia for all patients in the present study and
the same group of orthopedic surgeons performed TKA on all
patients. The depth of anesthesia, doses of preanesthetic
anesthetics (with the exception of remifentanil), development of
hypotension and bradycardia (changes in the circulatory function)
were similar in the two groups. Anesthesia time, operative time and
tourniquet time were also similar. Thus, the severity of
intraoperative tissue injury was generally consistent, avoiding any
differences in the degree of inflammation caused by tissue injury
between the two groups. The current study assessed potentially
confounding factors, suggesting that the decrease in VAS and POCD
incidence observed in the pre-emptive analgesia group may be solely
due to the pre-emptive timing of the analgesia.
However, the dose of remifentanil used in the
pre-emptive analgesia group was significantly lower (P<0.05)
than the dose used in the control group. It has previously been
demonstrated that remifentanil may induce hyperalgesia in a
dose-dependent manner (17). Due to
the dose of intraoperative remifentanil in the pre-emptive group
being lower compared with the control group, the incidence and
severity of remifentanil-induced hyperalgesia may have been lower.
This may be an additional reason, along with the timing of
analgesia, for the relatively low VAS score during exercise in the
pre-emptive group.
The incidence of early POCD in the pre-emptive
analgesia group was lower than previously reported by Rodriguez
et al (10), but the
incidence of early POCD in the control group was higher in the
present study. This comparison indirectly confirms that pre-emptive
analgesia by CFNB may reduce the incidence of postoperative early
POCD following TKA.
All patients in the present study underwent
multimodal analgesia including preoperative and postoperative
regular application of COX-2 inhibitors, intraoperative multipoint
local injection of 0.15% ropivacaine around the knee joint and the
application of 0.15% ropivacaine and low-dose opioids for
patient-controlled nerve analgesia (PCNA). Therefore, there was no
significant difference in the VAS score at rest between the two
groups, which indicates that multimodal analgesia achieved
satisfactory postoperative analgesia for patients in the two
groups. The VAS score during exercise was relatively low in the
pre-emptive analgesia group, suggesting that pre-emptive analgesia
may reduce pain during exercise. This may be one reason for the
slightly lower incidence of POCD in the pre-emptive analgesia group
compared with the control group. Restlessness following general
anesthesia is an independent risk factor in the development of POCD
(18) and pre-emptive analgesia may
prevent the occurrence of agitation during the period of recovery
(19). This further indicates that
pre-emptive analgesia may promote an early recovery of
postoperative cognitive function.
One limitation of the present study is that patients
had to be tested a number of times within a short period and
individuals became familiar with the content of the cognitive test
and thus may have learned the appropriate responses. However, this
type of learning cannot be avoided in studies associated with POCD.
The results collected suggest that the incidence of POCD at day 3
after TKA is a temporary condition in the acute postoperative
period, regardless of whether analgesia was administered pre- or
postoperation. Furthermore, when patients were at standstill, pain
was not a substantial risk factor of POCD. As the incidence of POCD
did not steadily increase by day 7 after TKA in the post-analgesia
group, the doctor was unable to predict long-term cognitive
dysfunction using the results of the current study. It has been
suggested that the early cognitive function may predict long-term
cognitive dysfunction (20).
Therefore, the impact of relevant interventions on long-term POCD
should be further studied.
In conclusion, pre-emptive analgesia by CFNB may
promote recovery from early POCD in elderly patients who have
undergone TKA. This effect may be associated with reduced pain
experienced during postoperative exercise by individuals
pre-emptively treated with analgesia.
References
|
1
|
Dodds C and Allison J: Postoperative
cognitive deficit in the elderly surgical patient. Br J Anaesth.
81:449–462. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cohendy R, Brougere A and Cuvillon P:
Anesthesia in the older patient. Curr Opin Clin Nutr Metab Care.
8:17–21. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shackman AJ, Salomons TV, Slagter HA, Fox
AS, Winter JJ and Davidson RJ: The integration of negative effect,
pain and cognitive control in the cingulated cortex. Nat Rev
Neurosci. 12:154–167. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Allen HW, Liu SS, Ware PD, Nairn CS and
Owens BD: Peripheral nerve blocks improve analgesia after total
knee replacement surgery. Anesth Analg. 87:93–97. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Meftah M, Wong AC, Nawabi DH, Yun RJ,
Ranawat AS and Ranawat CS: Pain management after total knee
arthroplasty using a multimodal approach. Orthopedics.
35:e660–e664. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Xie G, Zhang W, Chang Y and Chu Q:
Relationship between perioperative inflammatory response and
postoperative cognitive dysfunction in the elderly. Med Hypotheses.
73:402–403. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Paul JE, Arya A, Hurlburt L, Cheng J,
Thabane L, Tidy A and Murthy Y: Femoral nerve block improves
analgesia outcomes after total knee arthroplasty: A meta-analysis
of randomized controlled trials. Anesthesiology. 113:1144–1162.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Roseag OP, Krepski B, Cicutti N, Dennehy
KC, Liu AC and Johnson DH: Effect of preemptive multimodal
analgesia for arthroscopic knee repair. Reg Anesth Pain Med.
26:125–130. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Qian X, Qu YX, Jiang T, Xu JD and Zheng C:
Patient-controlled femoral nerve analgesia and epidural analgesia
for postoperative pain after total knee arthroplasty. Zhongguo
Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 15:3053–3056. 2011.(In
Chinese).
|
|
10
|
Rodriguez RA, Tellier A, Grabowski J,
Fazekas A, Turek M, Miller D, Wherrett C, Villeneuve PJ and
Glachino A: Cognitive dysfunction after total knee arthroplasty:
Effects of intraoperative cerebral embolization and postoperative
complications. J Arthroplasty. 20:763–771. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shoair OA, Ii MP Grasso, Lahaye LA, Daniel
R, Biddle CJ and Slattum PW: Incidence and risk fastors for
postoperative cognitive dysfuntion in older adults undergoing major
noncardiac surgery: A prospective study. J Anaesthesiol Clin
Pharmacol. 31:30–36. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tsai TL, Sands LP and Leung JM: An update
on postoperative cognitive dysfunction. Adv Anesth. 28:269–284.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Portet F, Ousset PJ, Visser PJ, Frisoni
GB, Nobili F, Scheltens P, Vellas B and Touchon J: MCI Working
Group of the European Consortium on Alzheimer's Disease (EADC):
Mild cognitive impairment (MCI) in medical practice: A critical
review of the concept and new diagnostic procedure. Report of the
MCI Working Group of the European Consortium on Alzheimer's
Disease. J Neurol Neurosurg Psychiatry. 77:714–718. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shaw PJ, Bates D, Cartlidge NE, French JM,
Heaviside D, Julian DG and Shaw DA: Neurologic and
neuropsychological morbidity following major surgery: Comparison of
coronary artery bypass and peripheral vascular surgery. Stroke.
18:700–707. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen Z, Ding S and Zhang L: Risk factors
for developing postoperative cognitive dysfunction in elderly
patients after general anesthesia. Zhonghua Mazuixue Zazhi.
33:31–33. 2013.(In Chinese).
|
|
16
|
Newman S, Stygall J, Hirani S, Shaefi S
and Maze M: Postoperative cognitive dysfunction after noncardiac
surgery: A systematic review. Anesthesiology. 106:572–590. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cabañero D, Campillo A, Célérier E, Romero
A and Puig MM: Pronociceptive effects of remifentanil in a mouse
model of postsurgical pain: Effect of a second surgery.
Anesthesiology. 111:1334–1345. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen Y, Wei CW, Yu YG, Ni XL and Xiong LZ:
Correlation between the agitation during the anesthesia recovery
period and the postoperative cognitive dysfunction after general
anesthesia. Zhonghua Mazuixue Zazhi. 33:34–36. 2013.(In
Chinese).
|
|
19
|
Wang Q, Yu YW and Yao SL: Preemptive
analgesia effects of flurbiprofen axetil or tramadol in patients
undergoing sevoflurane general anesthesia. Guoji Mazuixue Yu Fusu
Zazhi. 34:1079–1082. 2013.(In Chinese).
|
|
20
|
Van Dijk D, Moons KG, Keizer AM, Jansen
EW, Hijman R, Diephius JC, Borst C, de Jaegere PP, Grobbee DE and
Kalkman CJ: Octopus Study Group: Association between early and
three month cognitive outcome after off-pump and on-pump coronary
bypass surgery. Heart. 90:431–434. 2004. View Article : Google Scholar : PubMed/NCBI
|