Introduction
Talc (Mg3(Si2O5)2(OH)2) is the most commonly used
pleurodesis agent worldwide due to its reported success rate
especially for malignant pleural effusion (1). Prior to this, talc powder underwent an
evolution over the decades in terms of depuration, particle size
selection and production refining (2,3). Despite
this, the safety of talc remains debatable in terms of local
reactions and systemic syndromes such as ARDS. Being so, there is
no consensus on whether it should be used for pleurodesis,
especially in benign disease (4,5).
To date, most studies on humans have focused on
assessing the clinical outcome exclusively, therein reporting only
on short-term complications (often in severely symptomatic patients
from a respiratory disease) while investigations on long-term
complications have been few and mostly describing single cases
(6–8). Limited available data on possible long
term complications associated with talc pleurodesis are available
in the Literature (2,3,5,6).
For the above, since experimental talc pleurodesis
series were performed in rabbit and porcine models, belonging to
independent experimental comparative studies, carried out by the
same research group and using medical talc in different animal
models, different dosages and distinctive surgical techniques, an
observational model series review was performed to report the
findings after this extended experience with talc. The aim of this
analysis was to generate hypothesis regarding the functional
profile of talc for pleurodesis. Therefore, talc biocompatibility,
pleural reaction to talc deposition on the mesothelium,
intrapulmonary and lymphatic spread are observed to highlight
possible unknown events.
Materials and methods
This analysis of talc pleurodesis was performed as a
secondary investigation (opportunistic study) analysing animal
models series undergoing talc pleurodesis and belonging to already
performed experimental research protocols (9–11). Talc
slurry was performed in rabbits in different dosages with the aim
to compare talc to antibiotic both at increasing concentration and
administered via chest tube. The chosen dosages of talc were
therefore arbitrary and sought to see differences in performance of
talc at marked dose variation at different postoperative time.
Besides, talc poudrage was performed at standard dosage in pigs for
the impossibility to simulate an appropriate surgical surrogate for
medical thoracoscopy in a smaller animal model. Moreover, some
differences in the experimental techniques between the rabbit and
the swine series depend on the study aims and designs.
Animal management was carried out following
recommended practices pertaining to animal laboratory research
(12,13). The protocol was approved by central
and local authorities for animal care. Talc poudrage and slurry
were tested using a commonly available depurated, calibrated
preparation (Sterital, La Ciotat, France) in the following
models/methodology.
Rabbit model-talc slurry: Twenty New Zealand White
rabbits (Oryctolagus cuniculi), 7 weeks old, mean 2,450 g,
(range: 2,100–2,450 g) were submitted to talc slurry and divided
into 4 groups according to the following scheme: 200 mg/kg, checked
at postoperative day 14 (5 models); 200 mg/kg, checked at
postoperative day 28 (5 models); 40 mg/kg, checked at postoperative
day 14 (5 models); 40 mg/kg, checked at postoperative day 28 (5
models).
The procedure was performed under general
anaesthesia. A 10fr intrapleural catheter was placed time of
surgery. Talc suspended in 2 ml saline was administered through the
chest tube; pneumothorax was eliminated by syringe suction. The
drain was locked for 24 h then left open until post-operative day
4, when it was removed.
Swine model-talc poudrage: Eighteen Landrance ×
Large White pigs (Sus Scrofa domesticus), 4 months old, mean
42.7 kg, (range: 40–45 kg), were submitted to uniportal
videothoracoscopy (VATS) using the same procedure for human care in
each technical detail. Talc was sprayed and checked for homogenous
deposit all over the pleural surface before ending the procedure.
Complete resolution of pneumothorax was achieved under monitor
view. No chest tube was left in place. Talc poudrage was performed
according to the following design: 55 mg/kg, checked at
postoperative day 60 (18 models).
All models were analyzed post-mortem after painless
euthanasia. Autopsy was carried out according to the current
medical technique with inspection of all anatomical spaces and
cavities, systematically carried out following a standardized and
repeatable procedure. Description of findings and pictures were
performed by circulating members of the team. Autopsy operator
followed a predetermined routine in dissection and samples
collection, did not analyze the findings and was not involved in
interpretation of data. Observation sought to estimate the extent
of adhesions, pleural granulomas, intraprenchymal granulomas, and
severe spotted inflammation without pleurodesis. After autoptic
assessment, the pathologist and the surgeon evaluated the specimens
with a teamwork approach. Macroscopic examination and microscopic
assessment were systematically carried out according to the current
clinical surgical pathology methodology. Considering the
descriptive objective of the paper, no statistical analysis was
applied to the numerical variables.
Results
The outcome of talc pleurodesis in rabbits (talc
slurry) is reported in Tables I and
II; the outcome of talc pleurodesis
in pigs (talc poudrage) is summarized in Table III. The extent of the adhesions
observed in rabbits after 14 days from 40 mg/kg talc slurry ranged
from 0 to 30% of the pleural surface with no intraparenchymal
granulomas, but frequent parietal pleura granulomas. Pleural
granulomas were observed in all rabbits, whereas severe florid
inflammation without pleurodesis was recorded in one case after 14
days. When this talc dosage was tested at 28 days, the range of
pleurodesis extent resulted being between 0 and 10% of the pleural
cavity with no intraperinchymal granuloma and only one case of
florid inflammatory event of the pleura without pleurodesis. In the
series of rabbits undergoing 200 mg/kg talc slurry, the extent of
pleurodesis did not appear to increase dramatically (range from 0
to 10% at postoperative day 14, and 0 to 20% at postoperative day
28) with no intraparenchymal granuloma and no florid spotted
pleural inflammation. For this series of rabbits, granulomas on the
outer pericardium (seen on postoperative day 14), an isolated
mediastinal lymphadenopathy below the main carina and an isolated
parathymic granuloma (seen on postoperative day 28) were observed.
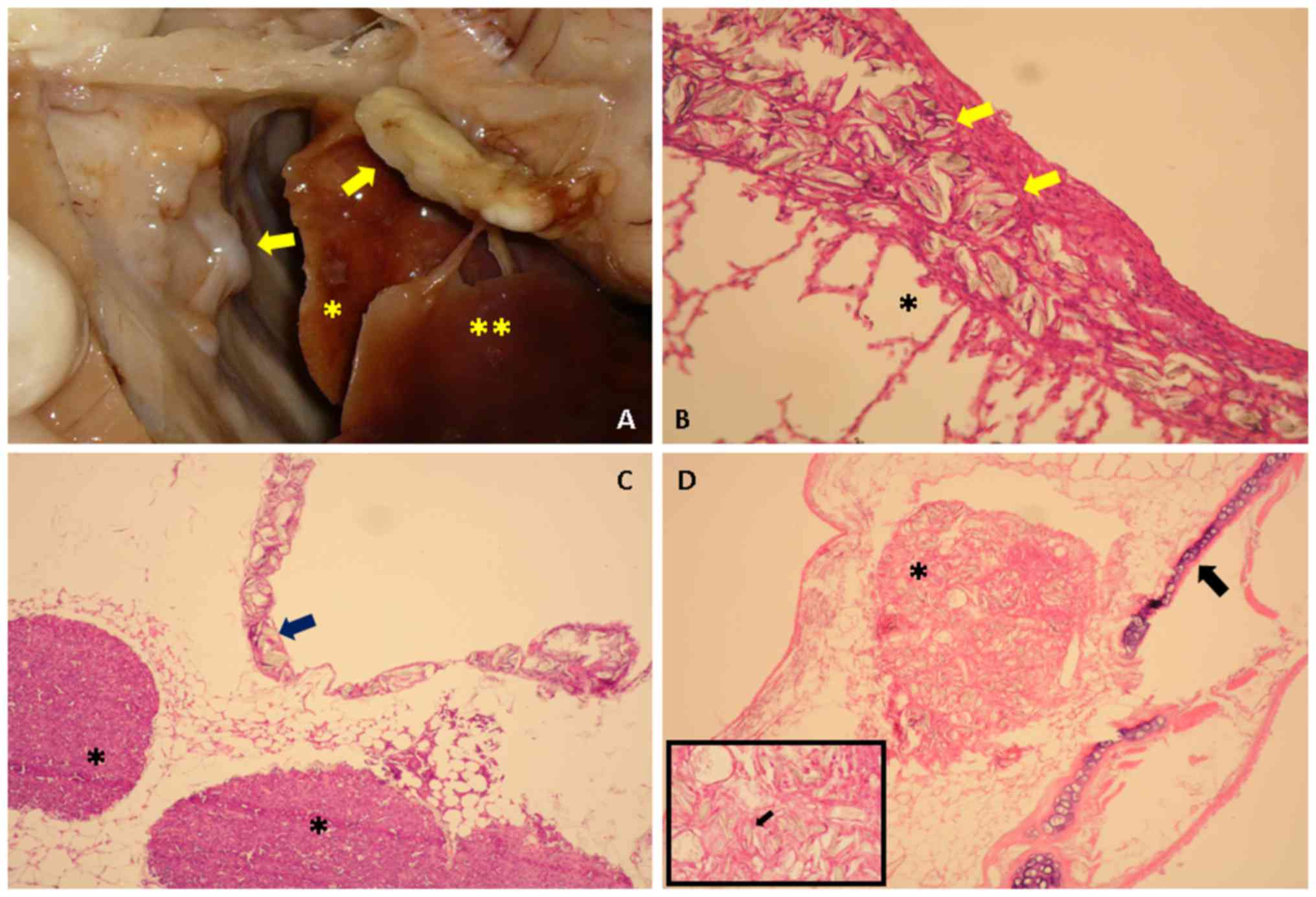
Representative findings are shown in Fig. 1.
 | Table I.Talc slurry (40 mg/kg) in rabbits (10
Fr pleural catheter). |
Table I.
Talc slurry (40 mg/kg) in rabbits (10
Fr pleural catheter).
|
|---|
| 14 days postoperative
observation |
|---|
|
|---|
| No. | Adhesions | Pleural
granuloma | Intraparenchymal
granuloma | Severe spotted
inflammation without pleurodesis | Note |
|---|
| 1 | YES <5% | YES parietal | NO | NO | None |
| 2 | YES
<30% | YES parietal | NO | NO | None |
| 3 | YES
<10% | YES parietal | NO | NO | Parasplenic
Fibrosis |
| 4 | NO | YES parietal | NO | YES | None |
| 5 | NO | YES parietal | NO | NO | None |
|
| 28 days
postoperative observation |
|
| No. | Adhesions | Pleural
granuloma | Intraparenchymal
granuloma | Severe spotted
inflammation without pleurodesis | Note |
|
| 1 | NO | NO | NO | YES | None |
| 2 | YES
<10% | NO | NO | NO | None |
| 3 | YES
<10% | NO | NO | NO | None |
| 4 | YES <5% | YES visceral | NO | NO | None |
| 5 | YES <5% | YES parietal | NO | NO | None |
 | Table II.Talc slurry (200 mg/kg) in rabbits (10
Fr pleural catheter). |
Table II.
Talc slurry (200 mg/kg) in rabbits (10
Fr pleural catheter).
|
|---|
| 14 days postoperative
observation |
|---|
|
|---|
| No. | Adhesions | Pleural
granuloma | Intraparenchymal
granuloma | Severe spotted
inflammation without pleurodesis | Note |
|---|
| 1 | YES <5% | YES
visceral/parietal | NO | NO | None |
| 2 | YES
<10% | YES visceral | NO | NO | None |
| 3 | YES <5% | YES
visceral/parietal | NO | NO | Pericardium
granulomas |
| 4 | NO | YES visceral | NO | NO | None |
| 5 | NO | YES visceral | NO | NO | None |
|
| 28 days
postoperative observation |
|
| No. |
Adhesions | Pleural
granuloma | Intraparenchymal
granuloma | Severe spotted
inflammation without pleurodesis | Note |
|
| 1 | NO | YES
visceral/parietal | NO | NO | Lymphadenopathy
(main carina) |
| 2 | YES <5% | YES
visceral/parietal | NO | NO | None |
| 3 | YES <5% | YES
visceral/parietal | NO | NO | None |
| 4 | YES
<20% | YES visceral | NO | NO | None |
| 5 | YES
<20% | YES parietal | NO | NO | Parathymic
granuloma |
 | Table III.Talc poudrage (55 mg/kg) in pigs
(single-port videothoracoscopy). |
Table III.
Talc poudrage (55 mg/kg) in pigs
(single-port videothoracoscopy).
|
| 60 days
postoperative observation |
|---|
|
|
|
|---|
| No. | Adhesions (%) | Pleural
granuloma | Intraparenchymal
granuloma | Severe spotted
inflammation without pleurodesis | Note |
|---|
| 1 | YES <5 | Yes
visceral/parietal | NO | YES | None |
| 2 | YES
<15 | Yes
visceral/parietal | NO | NO | None |
| 3 | YES <5 | Yes
visceral/parietal | YES | YES | None |
| 4 | YES
<50 | Yes
visceral/parietal | NO | YES | None |
| 5 | YES
<50 | Yes
visceral/parietal | NO | YES | None |
| 6 | YES <5 | Yes
visceral/parietal | YES | YES | None |
| 7 | YES>
50 | Yes
visceral/parietal | YES | NO | None |
| 8 | YES
<20 | Yes
visceral/parietal | YES | YES | None |
| 9 | YES
<20 | Yes
visceral/parietal | NO | YES | None |
| 10 | YES
<25 | Yes
visceral/parietal | YES | YES | None |
| 11 | YES <5 | Yes
visceral/parietal | YES | YES | None |
| 12 | YES
<15 | Yes
visceral/parietal | NO | YES | None |
| 13 | YES
<20 | Yes
visceral/parietal | NO | YES | None |
| 14 | YES
<20 | Yes
visceral/parietal | YES | YES | None |
| 15 | YES
<25 | Yes
visceral/parietal | NO | YES | None |
| 16 | YES
<25 | Yes
visceral/parietal | NO | NO | None |
| 17 | YES
<50 | Yes
visceral/parietal | YES | YES | None |
| 18 | YES
<15 | Yes
visceral/parietal | YES | YES | None |
The series of pigs undergoing 55 mg/kg talc poudrage
(uniportal VATS) had a wide range of outcomes regarding the extent
of pleurodesis achieved after a post-operative period of 60 days.
The outcome ranged from rare adhesions with no symphysis to a
single case with a complete pleurodesis characterized by a fully
extended pleural cavity obliteration. Pleural granulomas were
observed in the entire series of the swine models, both visceral
and parietal. Autopsies revealed severe spotted inflammation in
sites of the pleural surface without pleurodesis in 15/18 pigs.
Systematic sampling was performed at the bench and intraparenchymal
granulomas were observed in 9/18 lungs. Patterns of disease
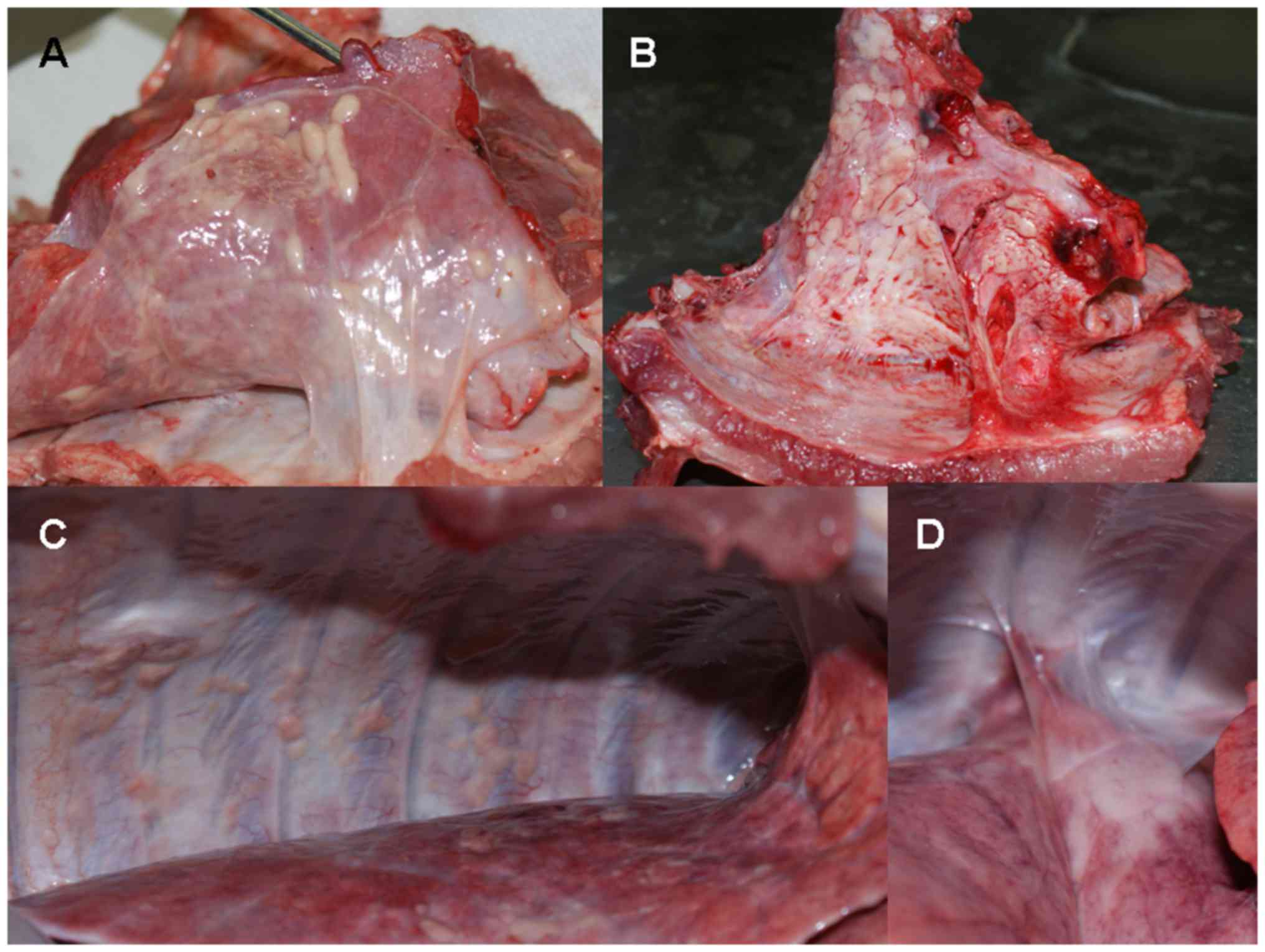
post-talcing are shown in Fig. 2.
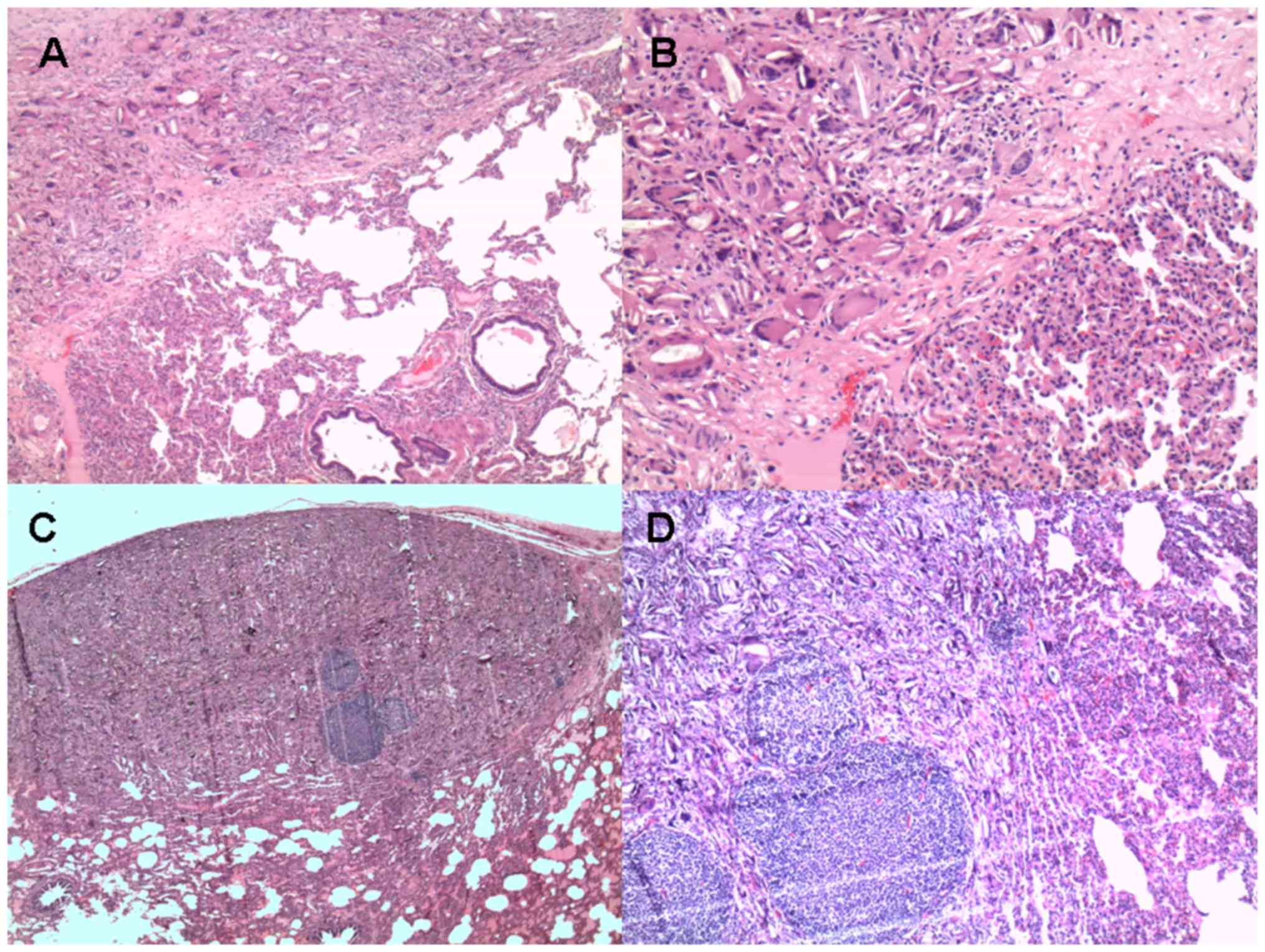
Histologies of exemplifying findings are provided in Fig. 3.
Discussion
Talc is the most used sclerosing agent worldwide for
achieving pleural space obliteration. Though its efficacy has been
widely reported especially in neoplastic effusion, severe
inflammatory reactions have been described both acute and long-term
(14–16). For this, an analysis in animal models
was carried out to investigate for the local reaction following the
contact of talc powder on the pleura. The materials under
investigation show interesting potentials considering that talc
pleurodesis was performed in different animal models, alternative
techniques and dosages. The available dataset represents a unique
source of information for a single research group according to
accessible Literature.
Talc pleurodesis is generally a technique supporting
another procedure such as videothoracoscopy or chest drainage with
several aspects of perfectibility (17). Any assessment of talc-related effects
is complex in clinical research, so an experimental setting appears
to be the only currently available way to evaluate
biocompatibility, pleural reaction and any subsequent damage. For
this animal series review, talc was administered either poudrage or
slurry in two different well-established animal models, pigs and
rabbits, respectively.
When talc was administered slurry in rabbit pleural
cavities, the obliteration of space never exceeded 30% of the
entire pleural cavity surface. Whereas, poudrage outcome in the
swine models varied from 0 to 100%, so that the effect of talc
poudrage cannot have allowed for an accurate prediction of outcome
after a videothoracoscopic administration of depurated, dry,
sterilized talc. In rabbits, intrapulmonary granulomas were
infrequent, while they were a common finding in the pig series.
According to published case reports, the intraparenchymal deposit
of talc could even provoke a high metabolic activity (18). The results from our model series
analysis evidenced that talc-related events were common. Likewise,
the exploration of the pleural cavities post-mortem evidenced that
severe inflammation often afflicted the pleural layer without
pleurodesis: noxa without effects.
The observation surprisingly evidenced some possible
differences between models or surgical techniques. Specifically,
there is no gross evidence of intraparenchymal granulomas after
slurry in rabbits while it is a common finding in porcine poudrage.
Besides, there is no particular mediastinal involvement after
poudrage in pigs while high dose of talc slurry was associated with
possible mediastinal migration and deposition of talc in extended
granulomas. The study design is not able to explain these
differences and does not allow for a fine comparison between
techniques but supports some hypothesis regarding different outcome
due to pleurodesis procedure as already suggested after clinical
research (19). Many questions on
what these differences are dependent on arise but they necessitate
further specific studies with comparative design to experimentally
test different dosages, slurry vs. poudrage, differences between
the animal models and model-dependent variability for the procedure
outcome. Nevertheless, the pleurodesis outcome is associated with
very variable results independently in all the animal series
reviewed in this analysis.
Past controversies concerned the safety and severity
of this procedure, specifically its possible reaction to dose, type
of management and the particle size (20). The marked variations among these
preparations were claimed to produce systemic inflammatory
complications, molecule migration modalities and other effects such
as acute lung injuries (21).
Whereas, the most currently used talc preparations are
standardized. In published studies to date on talc safety,
especially those carried out over the 20th century, the preparation
of talc was not usually well described and there was a lack of
information regarding particles size, as well as degree of
contamination (16).
As talc can cause damage when inhaled or after
intravenous administration leading to granulomatosis, organ
consolidation, deposition in parenchyma and diffuse pulmonary
diseases (22,23), its use has been associated with acute
lung injuries and its systemic absorption (24). Predictors of acute responses to talc
pleurodesis have been hypothesised and different procedures for a
safer administration have been developed (19,20).
Acute events have been reported following pleurodesis including:
fever, chest pain, hypoxemia, dyspnea, hypotension, lipothymia and
less commonly hypercalcemia along with acute respiratory distress
syndrome (25). As well, chronic
events have also been reported including granulomas, pleural
thickening, mesotheliod reaction and pulmonary nodules (6–8,26).
Despite concerns regarding the long-term
consequences of talc in young patients, its use is on the rise,
even for benign diseases as primary spontaneous pneumothorax
(27). Nonetheless, recent
experimental research in a mouse model, although reporting
decreased effusion, concluded that there was an observed limited
pleurodesis surface with marked pleural thickening following this
procedure (28).
Our animal model series review had limitations.
First, there was no comparative set up, unless for dosages in talc
slurry, and it was based upon simple observation. Second, the
animal series were extracted out of different protocols for a
secondary scientific purpose; two different animal models and two
different talc pleurodesis procedures were used and this might have
led to a bias in the final results regarding the evaluation of
effectiveness and reliability of talc action.
In conclusion, despite pleurodesis being one of the
most requested procedures for the treatment of many systemic and
thoracic diseases, there is still no consensus on which situation
it is best suited for. Our study assessed for inflammatory
stimulus, biocompatibility and tissue reaction in animal models and
found that talc pleurodesis led to pleuropulmonary granulomas
especially after poudrage in pigs, intrathoracic migration and
diffuse pleural thickening. These findings suggest that talc was
not an ‘ideal’ agent due to the observed chronic inflammatory
patterns following the procedure, which could potentially have long
term effects. In this regard, research must focus on biomedical
properties of existing products to extend indications for use once
they are tested for reliability, safety and risk/effectiveness
while experimental research should aim at creating a new sclerosing
agent with all those biochemical and functional traits to perform
the ideal pleurodesis.
Acknowledgements
The study was reviewed for language editing by
English language Service.
References
|
1
|
Janssen JP, Collier G, Astoul P, Tassi GF,
Noppen M, Rodriguez-Panadero F, Loddenkemper R, Herth FJ, Gasparini
S, Marquette CH, et al: Safety of pleurodesis with talc poudrage in
malignant pleural effusion: A prospective cohort study. Lancet.
369:1535–1539. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Baron RD, Milton R and Thorpe JA:
Pleurodesis using small talc particles results in an unacceptably
high rate of acute lung injury and hypoxia. Ann Thorac Surg.
84:21362007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Genofre EH, Vargas FS, Acencio MM,
Antonangelo L, Texweira LR and Marchi E: Talc pleurodesis: Evidence
of sistemic inflammatory response to small size particles. Respir
Med. 103:91–97. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sahn SA: Talc should be used for
pleurodesis. Am J Respir Crit Care Med. 162:2023–2049. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Light RW: Talc should not be used for
pleurodesis. Am J Respir Crit Care Med. 162:2024–2026. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vandemoortele T, Laroumagne S, Roca E,
Bylicki O, Dales JP, Dutau H and Astoul P: Positive FDG-PET/CT of
the pleura twenty years after talc pleurodesis: Three cases of
benign talcoma. Respiration. 87:243–248. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ergönül AG, Çakan A, Çağirici U and Nart
D: Talc granulomatosis with multiple parenchymal and pleural
nodules. Eur J Cardiothorac Surg. 44:e3082013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tenconi S, Luzzi L, Paladini P, Voltolini
L, Gallazzi MS, Granato F and Gotti G: Pleural granuloma mimicking
malignancy 42 years after slurry talc injection for primary
spontaneous pneumothorax. Eur Surg Res. 44:201–203. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Daddi N, Vannucci J, Maggio C, Giontella
A, Bravi I, Marziani F, Capozzi R, Ragusa M, Bufalari A and Puma F:
Efficacy of tigecycline pleurodesis: A comparative experimental
study. J Surg Res. 169:e109–e118. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Droghetti A, Vannucci J, Bufalari A,
Bellezza G, De Monte V, Marulli G, Bottoli MC, Giovanardi M, Daddi
N, De Angelis V, et al: Pleurodesis with Thulium Cyber Laser versus
talc poudrage: A comparative experimental study. Lasers Med Sci.
31:1407–1413. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vannucci J, Droghetti A, Bufalari A, De
Monte V, Bellezza G, Bianconi F, Pecoriello R, Daddi N, Moriconi F
and Puma F: Effectiveness and predictability of pleurodesis with
the Tachosil® surgical patch compared with talc
poudrage: An experimental study. Eur J Cardiothorac Surg.
50:668–9674. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Suckow MA, Schroeder V and Douglas FA: The
Laboratory Rabbit. 2nd. CRC Press, Taylor, Francis Group; London:
2010
|
|
13
|
Bufalari A, De Monte V, Pecoriello R,
Donati L, Ceccarelli S, Cagini L, Ragusa M and Vannucci J:
Experimental left pneumonectomy in pigs: Procedure and management.
J Surg Res. 198:208–216. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Genofre HG, Marchi E and Vargas FS:
Inflammation and clinical repercussions of pleurodesis induced by
intrapleural talc administration. Clinics (Sao Paulo). 62:627–634.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
West SD, Davies RJ and Lee YC: Pleurodesis
for malignant pleural effusions: Current controversies and
variations in practices. Curr Opin Pulm Med. 10:305–310. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aelony Y: Talc pleurodesis and acute
respiratory distress syndrome. Lancet. 369:1494–1496. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Porcel JM, Lui MM, Lerner AD, Davies HE,
Feller-Kopman D and Lee YC: Comparing approaches to the management
of malignant pleural effusions. Expert Rev Respir Med. 11:273–284.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kurian EM: Lung nodule with increasing
fluorodeoxyglucose uptake in a patient with a history of lung
carcinoma and talc pleurodesis evaluated by EBUS-TBNA on-site
assessment. Acta Cytol. 61:84–86. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Stefani A, Natali P, Casali C and Morandi
U: Talc poudrage versus talc slurry in the treatment of malignant
pleural effusion. A prospective comparative study. Eur J
Cardiothoracic Surg. 30:827–832. 2006. View Article : Google Scholar
|
|
20
|
Light RW: Talc for Pleurodesis? Chest.
122:1506–1508. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Baron RD, Milton R and Thorpe JAC:
Pleurodesis using small talc particles results in an unacceptably
high rate of acute lung injury and hypoxia. Ann Thorac Surg.
84:21362007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Iqbal A, Aggarwal B, Menon B and
Kulshreshtha R: Talc granulomatosis mimicking sarcoidosis.
Singapore Med J. 49:e168–e170. 2008.PubMed/NCBI
|
|
23
|
Fiorelli A, Accardo M, Rossi F and Santini
M: Spontaneous pneumothorax associated with talc pulmonary
granulomatosis after cocaine inhalation. Gen Thorac Cardiovasc
Surg. 64:174–176. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lee YC and Light RW: Management of
malignant pleural effusions. Respirology. 9:148–156. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Aujila SJ, Michelson P, Langman CB,
Shapiro R, Ellis D and Moritz ML: Refractory hypercalcemia in an
infant secondary to talc pleurodesis resolving after renal
transplantation. Am J Transplant. 8:1329–1333. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Faynberg T, Patel N, Nayar AP and
Shienbaum AJ: Mesothelioid reaction following talc pleurodesis: A
case report. Gen Thorac Cardiovasc Surg. Mar 7–2017.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cardillo G, Bintcliffe OJ, Carleo F,
Carbone L, Di Martino M, Kahan BC and Maskell NA: Primary
spontaneous pneumothorax: A cohort study of VATS with talc
poudrage. Thorax. 71:847–853. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Iwasaki Y, Takamori S, Mitsuoka M,
Kashihara M, Nishi T, Murakami D, Matsumoto R, Mifune H, Tajiri Y
and Akagi Y: Experimental validation of talc pleurodesis for
carcinomatous pleuritis in an animal model. Gen Thorac Cardiovasc
Surg. 64:409–413. 2016. View Article : Google Scholar : PubMed/NCBI
|