Introduction
The acromioclavicular (AC) joint injury is a common
orthopedic problem that accounts for 12% of shoulder injuries
(1). Despite its prevalence, the
lack of consensus regarding its diagnosis and treatment makes it
one of the most controversial shoulder injuries (2,3).
Firstly, Tossy et al (4)
classified AC joint injury into types I, II, and III. Then,
Rockwood et al (5) expanded
the classification to types IV, V, and VI. The expanded
classification recognized a variety of complete AC dislocation
(ACD). According to the Rockwood classification, ACD is classified
into types I–VI (6). The Rockwood
classification system is very important for surgeons to accurately
diagnose AC joint injuries and is used in the literature to guide
nonoperative vs. operative management (7–10).
Rockwood type I, II could be cured by expectant treatment, while
the ACD of Rockwood types IV, V, and VI always requires surgical
intervention. However, it remains controversial for type III injury
whether to take operative treatment or not. Numerous biomechanical
studies in recent years have led to the development of surgical
techniques that stabilize the AC joint complex with fixation that
more closely approximates the natural anatomic structure (11–14).
Currently, many operative treatments for type III injury are
effective, such as clavicular hook plate fixation (CHPF), kirschner
wires tension band fixation, reconstruction of coracoclavicular
ligaments, and so on (15–18). However, the complications of surgery,
including looseness of internal fixation, postoperative pain of
shoulder, restricted joint motion and recrudescence of joint
dislocation after removing internal fixation, is still an important
issue (19–24).
Treatment of the ACD of Rockwood type III is
particularly challenging for surgeons (25–29). The
endobutton technique has been used for patients and is worthy of
popularization (30–32). At present, the hook plate is
currently used by 44% of all surgeons (33). But injury to the shoulder was worse.
Compared with hook plate in the treatment of the ACD of Rockwood
type III, the endobutton technique showed better short-term results
with regard to complications and could be used effectively in the
treatment. Biomechanical studies in recent years have demanded
stabilization of the AC joint complex with fixation that more
closely approximates the natural anatomic structure (34–36), and
the double-endobutton technique could be compatible with anatomic
structure. In a clinical study, there were no significant
differences in the mean incision length, blood loss, the operative
and radiation time, length of hospitalization, the Constant and VAS
scores, and ability to return to previous work between a double
endobutton group and triple endobutton group, and the triple
endobutton treatment had higher hospital costs (37). Hu et al (38) explored the clinical efficacy of
double endobutton reconstitution of the coracoclavicular ligament
combined with repair of the acromioclavicular ligament in stage I
in treating ACD with Rockwood type III–V, which suggested good
early results. In fresh-frozen cadaveric upper extremeties, Struhl
et al (39) compared the
stability of a novel closed-loop double-endobutton construct with a
commercially available cortical button system in both the axial and
superior directions and they suggested closed-loop
double-endobutton construct provided good stability. In addition,
Struhl and Wolfson (40) made a mean
follow-up of 5.2 years for 35 patients who got a closed-loop
double-endobutton technique to reconstruct both acute and chronic
dislocations (Rockwood type III) and they suggested that this
technique was a low-profile, durable fixation device that
maintained a stable AC joint, which allowing enough time for strong
soft tissue healing to develop. It was reported that arthroscopy
seem to have a lower rate of residual postoperative pain and
postoperative recurrence (40). We
modified common closed-loop double-endobutton technique by shoulder
arthroscopy, which would provide a better treatment for ACD
patients.
The application of double-endobutton reconstruction
in patients with ACD has significantly reduced the postoperative
complications (35,41). Also, the effect on Rockwood type III
has been confirmed (42–44). At the same time, the improvement of
double-endobutton reconstruction is always ongoing, aiming at
simplifying the surgical procedures, strengthening the internal
fixation, and reducing the complications. With the rapid
development of arthroscopic technique, we modified common
closed-loop double-endobutton technique (CCDT) to treat ACD by
shoulder arthroscopy. Based on replacement and stabilization of the
AC joint, the modified closed-loop double-endobutton technique
(MCDT) was more simple, convenient and efficient than CCDT, and was
worth popularizing.
The ACD of Rockwood type III, the coracoclavicular
ligament is ruptured completely, the stability of the
acromioclavicular joint on the vertical direction is lost, and the
distal clavicle is shifted upwards, that causes shoulder joint
pain, swelling, and even restricted movement. In the present study,
MCDT was used to treat the ACD of Rockwood type III, two endobutton
with loops were prepared, two loops were tied together, making a
closed-loop slipknot between two endobuttons. The total length of
the loops that was made before procedure, was approximately equal
to CC-interval in uninjured side shoulder. The modified closed-loop
double-endobutton was implanted in injured side by arthroscopy
technique, so the ACD of Rockwood type III was restored, and it
provided a stable environment, which was beneficial to early
activities and recovery.
The present study still had some limitations. For
example: Firstly, all cases enrolled were from the same hospital
but not a multi-center study. Secondly, the length of the loops was
be determined by CC-interval in uninjured side shoulder, which
maybe ignore the difference between the left and right side.
Thirdly, the radiographic distance maybe were little erroneous.
In order to evaluate the clinical efficacy and
recovery of the MCDT, we conducted a study in comparison with other
surgical procedures, including CCDT and CHPF. By comparing the
three groups, the advantages of MCDT were known, and it provided
evidence and support for clinical extensive application.
Materials and methods
Inclusion standards
Cases were enrolled according to such inclusion
criteria: i) Patients were diagnosed as acute ACD without course of
exceeding 7 days before surgical treatment. ii) The shoulder was
injuried with one side. iii) It was confirmed that injury belonged
to Rockwood type III by CT or MRI. iv) Patients completely
understood operation and expectant treatment and signed operative
informed consent, doctor-patient communication consent and
implantable informed consent. v) Patients had a follow-up of more
than 1 year.
Exclusion standards
Other cases would be excluded with such criteria: i)
Patients had an injury longer than 7 days before surgery. ii)
Patients had serious associated injuries, such as clavicular
fracture, coracoid fracture, or other fracture in shoulder. iii)
Patients suffered from open shoulder injuries that would be
infected easily. iv) Patients had anatomic variation of coracoid in
shoulder. v) Patients had associated injuries of brachial plexus.
vi) Patients had serious shoulder swelling or other injuries that
affected operations. vii) Patients had special diseases of tumor,
poisoning, infection and visceral organ failure. viii) Patients had
a follow-up of less than 1 year. ix)Patients who were attending
other project would not be enrolled.
Patients and ethic
All procedures were approved by the Ethical
Committee of Affiliated Traditional Chinese Medicine Hospital of
Southwest Medical University (no. 2016060518) and registry of
clinical trial (ChiCTR-ORC-16008438), and performed in accordance
with the 1964 Helsinki declaration and its later amendments or
comparable ethical standards. Informed consent was obtained from
all individual participants included in the present study. A total
of 61 cases were enrolled from January 2010 to December 2014 in
affiliated Traditional Chinese Medicine Hospital of Southwest
Medical University.
Grouping
There were 3 kinds of operation methods chosen by
patients, in terms of 3 kinds of operation methods, the enrolled
patients were divided into 3 groups, MCDT group (n=20), CCDT group
(n=21), CHPF group (n=20). Each group underwent surgical treatment
by one of three types of operations separately. All surgeries were
completed by the same senior surgeons in our hospital. In addition,
the main injury reasons contained traffic accident (22 cases),
tension injury during exercise (20 cases), falling injury (10
cases) and heavy pound injury (3 cases).
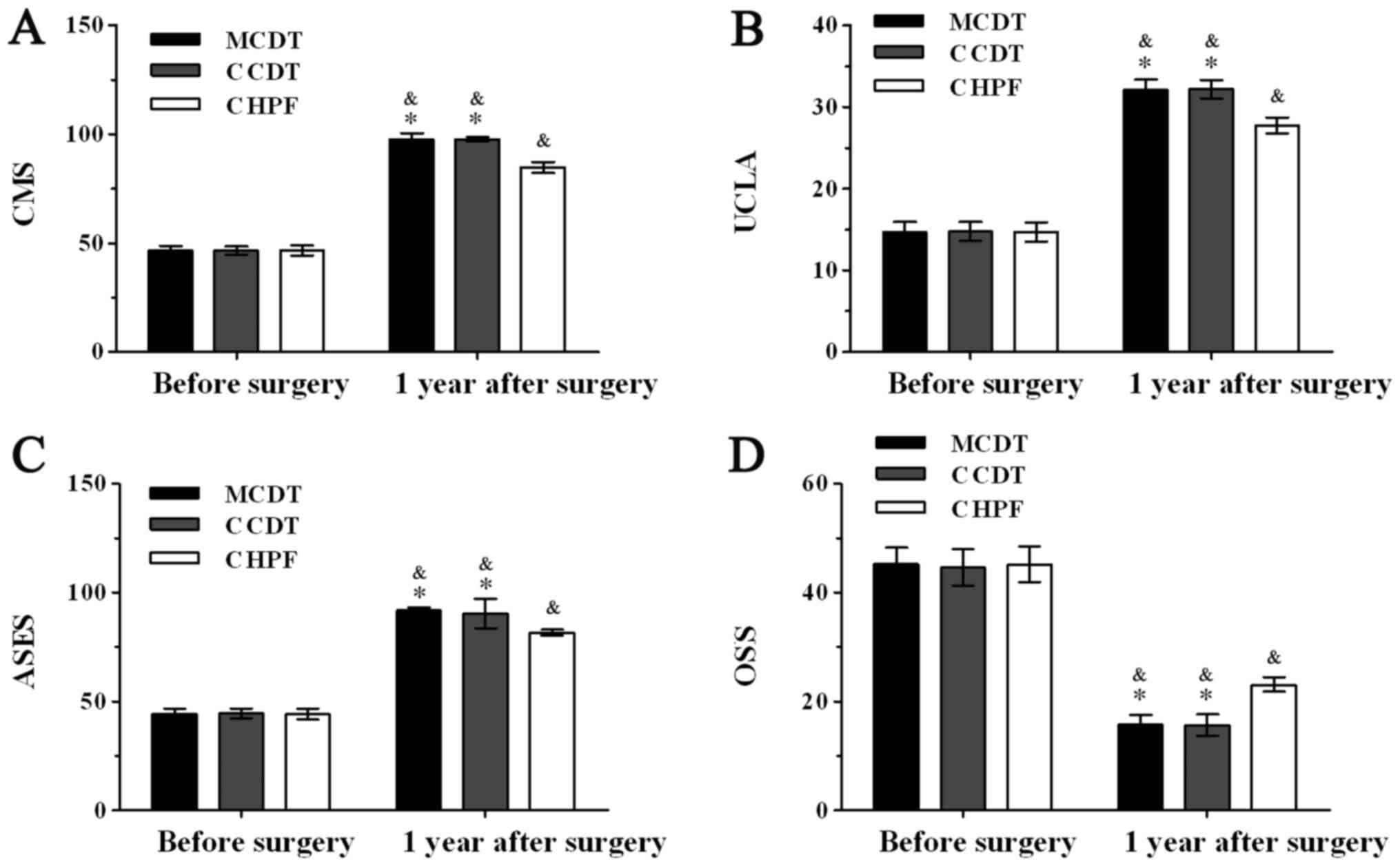
Detection index and methods
Before operation, there was no significant
difference in general data of sex, age, injured side, arm
dominance, time interval from injury to surgery and shoulder
functional scores, including Constant-Murley Score (CMS),
University of California at Los Angeles shoulder rating scale
(UCLA), rating scale of the American Shoulder and Elbow Surgeons
(ASES), Oxford Shoulder Score (OSS) (45–48) and
coracoclavicular interval (CC-interval) before surgery was noticed
among three groups (P>0.05) (Tables
I and II). Meanwhile, operative
time, incision lengths and intraoperative hemorrhage were observed
as surgical index. And multiple validated measures were collected
before and after 1 years, including CMS, UCLA, ASES, OSS, and
CC-interval.
 | Table I.Baseline data of all patients. |
Table I.
Baseline data of all patients.
| Characteristic | MCDT | CCDT | CHPF |
|---|
| Sex |
| Male
(N) | 12 | 13 | 13 |
| Female
(N) | 8 | 8 | 7 |
| Age (years) | 30.25±7.41 | 29.90±6.98 | 30.55±8.04 |
| Injured side |
| Right
(N) | 11 | 12 | 10 |
| Left
(N) | 9 | 9 | 10 |
| Arm dominance |
| Right
(N) | 19 | 19 | 19 |
| Left
(N) | 1 | 2 | 1 |
| Injured time
(days) | 3.85±0.81 | 3.86±0.79 | 3.95±0.76 |
 | Table II.Functional rating and CC-interval
before surgery. |
Table II.
Functional rating and CC-interval
before surgery.
| Group | Case(N) | CMS | UCLA | ASES | OSS | CC-interval
(mm) |
|---|
| MCDT | 20 |
46.50±2.16 |
14.65±1.31 |
44.15±2.54 |
45.25±3.01 |
16.77±0.91 |
| CCDT | 21 |
46.52±1.94 |
14.76±1.18 |
44.57±2.29 |
44.62±3.37 |
16.70±0.77 |
| CHPF | 20 |
46.55±2.31 |
14.70±1.17 |
44.25±2.55 |
45.20±3.25 |
16.83±0.75 |
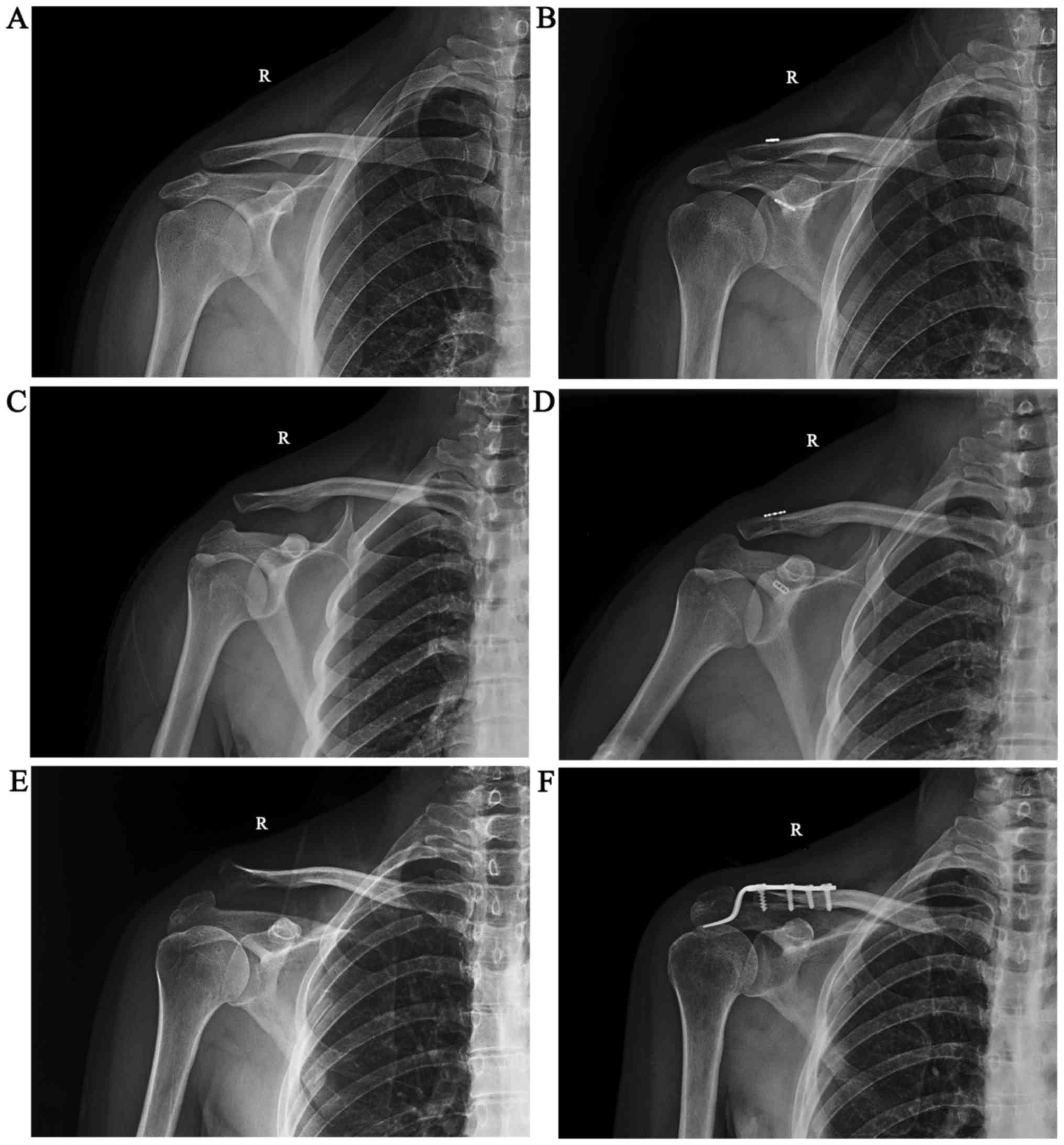
Preoperative preparation
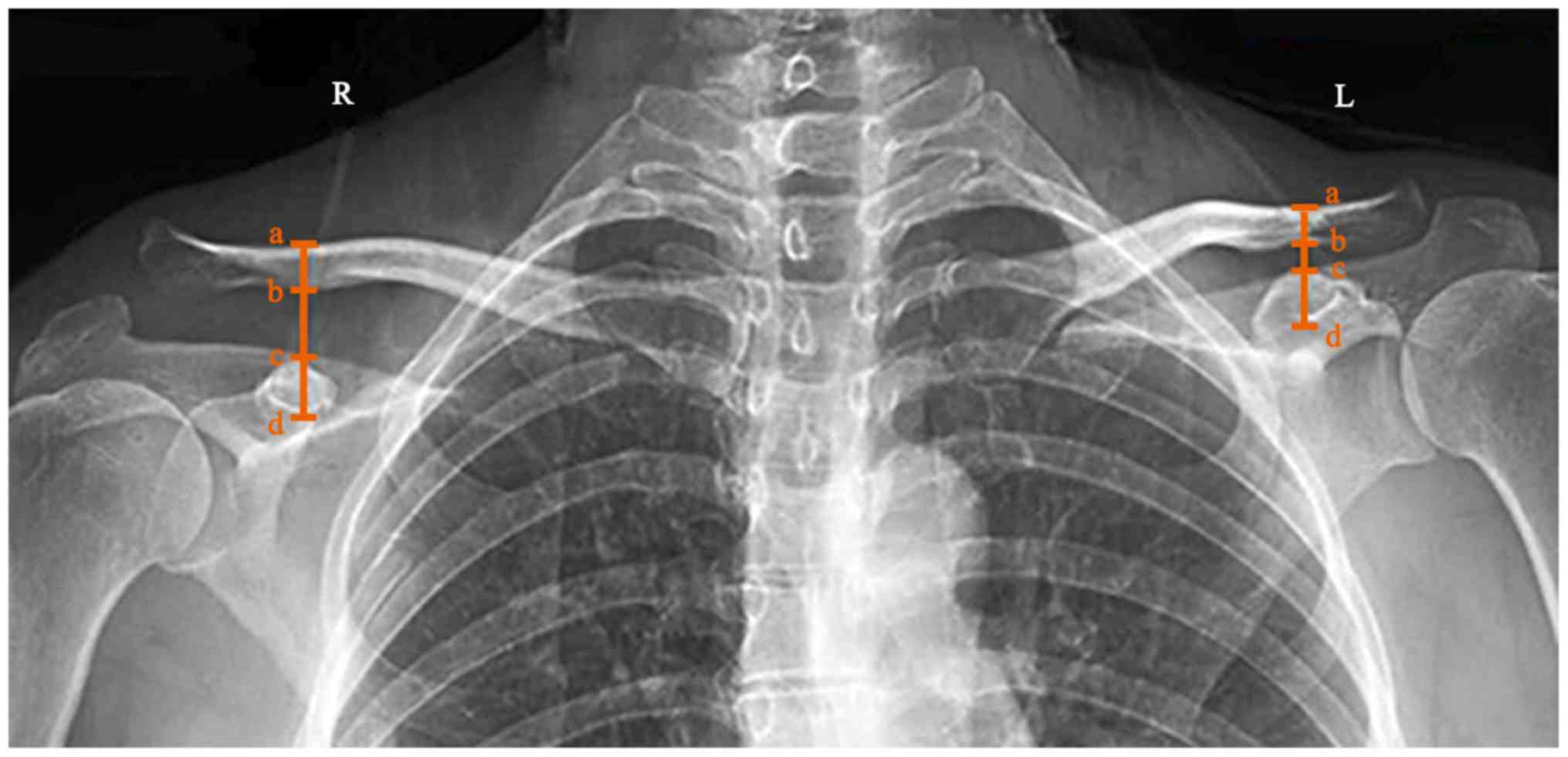
First of all, CC-interval of all patients in both
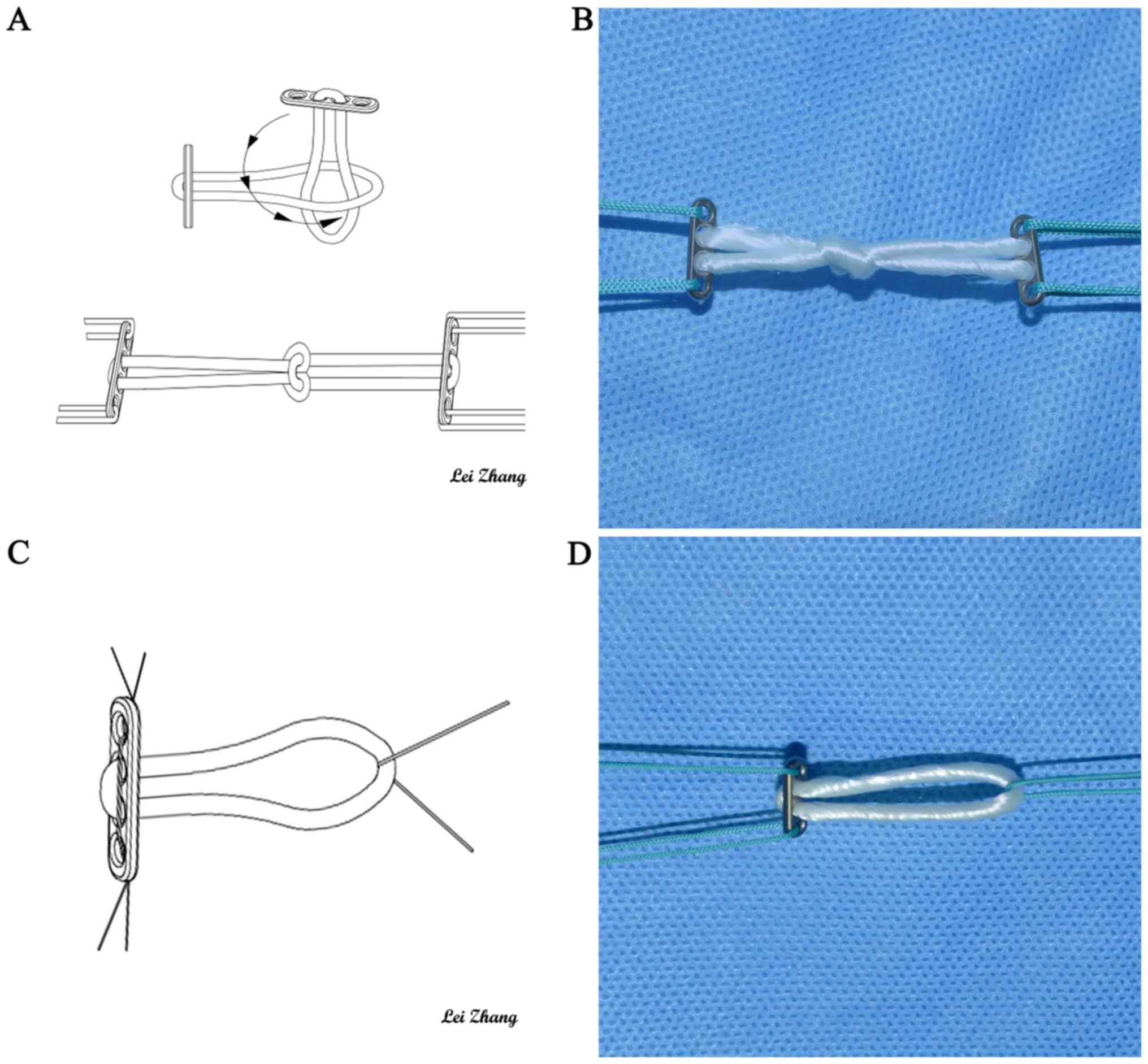
shoulders were measured under radiographs (Fig. 1). In MCDT group, two endobutton
(titanium alloy, 4×12 mm, Smith&Nephew, USA) with loops were
prepared (Fig. 2). Then, one of
endobuttons' loop was penetrated into another endobutton's loop.
Later, the former endobutton was reflected into its own loop which
had passed through another endobutton's loop before. Finally, two
endobuttons were strained from two opposite direction, making a
closed-loop slipknot between two endobuttons, which was the
modified closed-loop double-endobutton (Fig. 2A and C). The total length of the
loops that was made before was approximately equal to CC-interval
in uninjured side shoulder of the same patient. After that,
non-absorption braided tendon sutures (Johnson, USA) were loaded
into the first and fourth holes on plates separately as lead
wires.
In CCDT group, single-endonbutton with a loop was
prepared at first. Then non-absorption tendon sutures (Johnson,
USA) were pierced into the first and fourth holes on plates
separately as lead wires, which was single-endobutton with a loop
(Fig. 2B and D). At the same time,
the other sutures fixed on the loop. Also another endonbutton
without loops was prepared. The diameter of loops was 4.5 mm and
the length of loops was equal to CC-interval in uninjured shoulder
at the same patient.
In CHPF group, the clavicular hook plate (titanium
alloy, AO, Switzerland) was chosen before surgery.
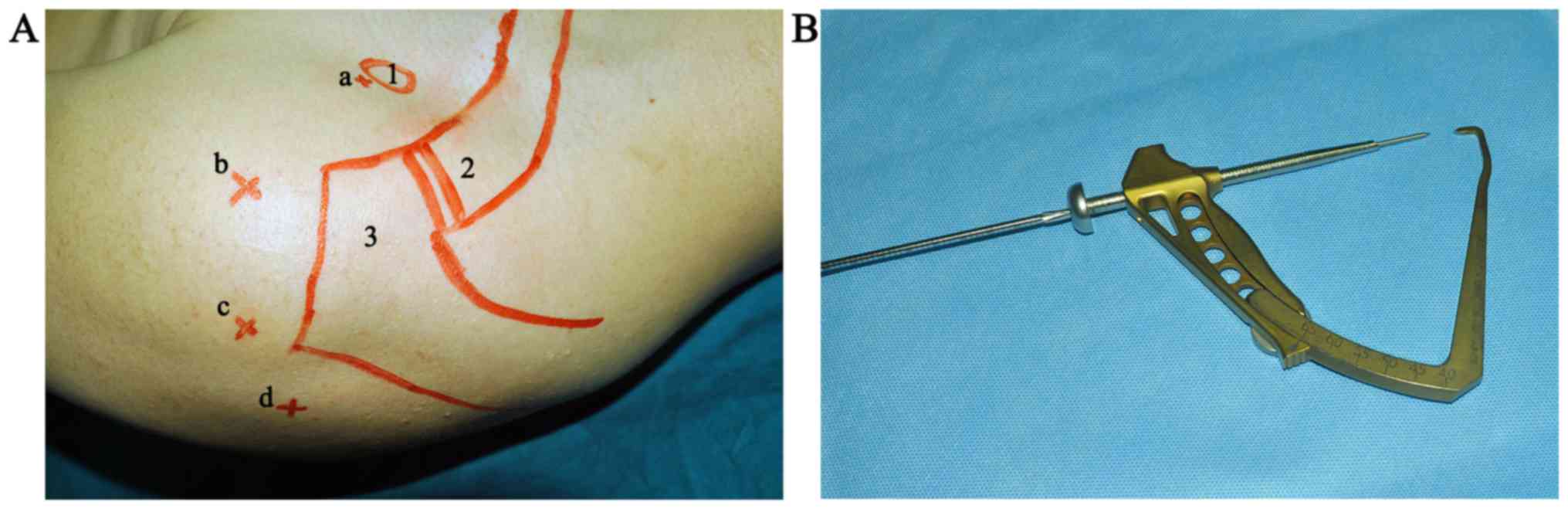
Surgical process of MCDT
Under general anesthesia in beach chair position,
almost with angle of 70 degree between horizontal line and the
upper part of the body. Trunk, limbs and head were fixed and
surgical incisions were marked before the procedure (Fig. 3A). The arthroscopic instruments
(72200616, Smith & Nephew, USA) were prepared before operation,
the instruments were strictly sterilized by operators. Then, the
patients were anesthetized and were sterilized on surgical area.
The shoulder joint was examined under anesthesia, and small
incisions were made around the joint, the scope and surgical
instruments would go into these incisions. The scope was inserted
into the shoulder joint, saline solution flowed through a tube and
into the shoulder capsule to expand the joint and to improve
visualization. The image was sent to a video monitor where the
surgeon could see inside the joint. Planer tool was inserted from
anterior-lateral approach, with the scope was inserted from lateral
approach, in order to remove partial plica that could cause pain
and to expose clearly coracoid base, the guiding locator (Fig. 3B) was inserted from the
anterior-medial approach and located on the center of base of the
coracoid and the center of upper surface of clavicle, passing 2-mm
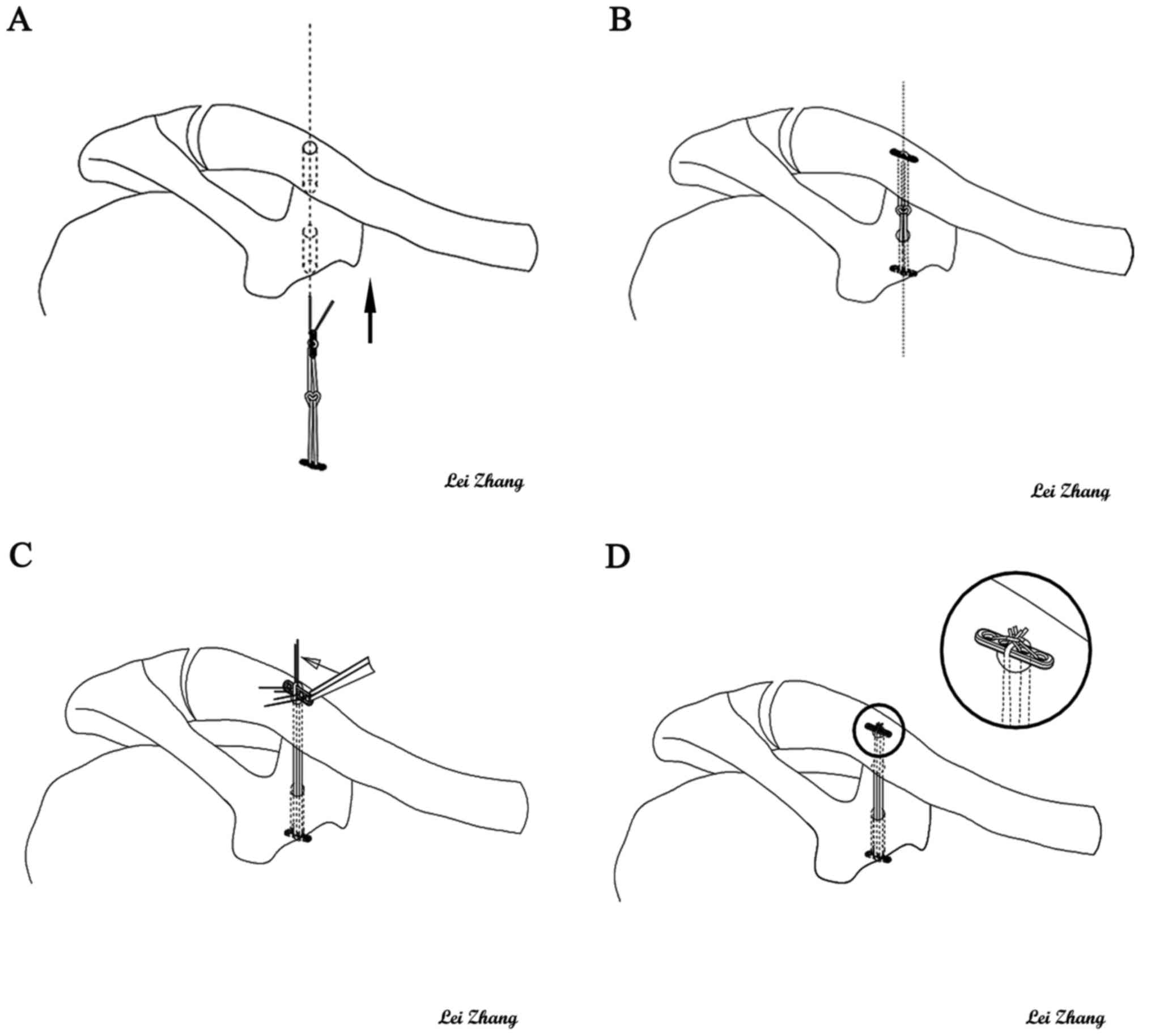
kirschner wires between these two point. A hole was drilled in the
top of the clavicle midway between the anterior and posterior
borders and directly in line with the base of the coracoid, the
tunnel was drilled over guide wire with the same diameter as the
loop. By using a grasper, the lead wires were inserted from
coracoid tunnel into clavicle tunnel and penetrated out the top of
clavicle tunnel finally. Then the modified closed-loop
double-endobutton would be inserted. One of endobuttons was taken
from clavicle tunnel to the base of coracoid tunnel. While pushing
the distal clavicle downwards, the lower endobutton was fixed on
the base of coracoid, and the upper endobutton was fixed on the top
of clavicle. Finally ACD was repaired (Fig. 4A and B). After that, the lead sutures
on endobutton were drawn out, the surgical instruments were removed
and the procedure was completed, the proper location of AC joint
was confirmed through arthroscopy, the incision was cleaned and
sutured finally.
Surgical process of CCDT
The selection of body position and process of
arthroscopic examination and establishing bone tunnel were same as
MCDT. Prepared single-endobutton with a loop was taken into base of
coracoid tunnel and was fixed on the base of coracoid. And the loop
on the single-endobutton was pulled out clavicle tunnel at the same
time, leaving empty place for the single-endobutton without loops.
After pushing distal clavicle downwards for qualified
reconstruction, the single-endobutton without loops was placed in
the loop on top of the clavicle. Then the loop was locked by two
knotted sutures from the second to third and the first to fourth
holes on the single-endobutton without loops and the lead sutures
from the single-endobutton with a loop was also drawn out (Fig. 4C and D). At the end, the proper
location of AC joint was confirmed through arthroscopy, the
incisions were cleaned and sutured by layers finally.
Surgical process of CHPF
In supine position, after general anesthesia,
patients were made an arc incision from middle part of clavicle to
acromion with 7–9 cm, exposing AC joint. Intervening soft tissues
were removed in the AC joint and the operative vision were cleared
completely later. Then the prepared plate was moulded as the shape
of clavicle, and was inserted on the top of the AC joint. The holes
were drilled and the screws were inserted. Finally, the incisions
were cleaned and sutured.
Postoperative treatment
Operated shoulder was rested in a sling for 4 weeks.
Functional exercises were started 3 days after operation. Passive
exercises began in 4 weeks. Active movement of the shoulder and
resistant exercises were allowed after 4 to 12 weeks. Strenuous
exercises were avoided during first three months following surgery.
The time of using injury-side sling and functional exercise were
extended for patients whose healing was slow. At first, all
patients reviewed clinical postoperative examination at 2, 3, 6
months. Afterwards, they were required to get follow-up examination
every 6 months. Removal of the internal fixations was not necessary
in MCDT and CCDT group, while it was essential to remove internal
fixations in CHPF group 1 year after surgery depending on the
process of recovery.
Statistical analysis
The Pearson chi-square test and Fisher exact test
were used to compare categorical outcomes. The paired t test was
used to compare the functional scores and CC-interval after the
operation with those before operation. And the one-way ANOVA was
used to compare the functional scores and CC-interval among three
groups. The level of statistical significance was set at P<0.05.
All data were analyzed with the use of SPSS software (version 20,
IBM Corp). Results are expressed as the mean ± SD unless otherwise
specified.
Results
Surgical index
Firstly, the operative time of MCDT or CHPF group
was significantly shorter than that of CCDT group (P<0.05). But
no significant difference between MCDT and CHPF group (P>0.05).
Secondly, the incision lengths of MCDT or CCDT group was
significantly shorter than that of CHPF group (P<0.05). And no
significant difference was noted between MCDT and CCDT group
(P>0.05). Thirdly, the hemorrhage of MCDT or CCDT group was
significantly less than that of CHPF group (P<0.05). And
significant difference was noted between MCDT and CCDT group
(P<0.05) (Table III).
 | Table III.Comparison in surgical index among 3
groups. |
Table III.
Comparison in surgical index among 3
groups.
| Group | Case (N) | Operation time
(min) | Length of cut
(cm) | Hemorrhage
(ml) |
|---|
| MCDT | 20 |
77.00±8.18a |
1.55±0.26b |
52.00±8.18b |
| CCDT | 21 |
101.19±7.89 |
1.54±0.25b |
75.24±11.23b |
| CHPF | 20 |
76.50±8.13a |
8.98±0.65 |
140.00±18.64 |
Follow-up outcome measurements
One year after surgery, the CMS, UCLA, ASES, OSS,
CC-interval were superior to those before surgery in three groups
(P<0.05). Secondly, all post-operation functional scores of MCDT
or CCDT group were better than those of CHPF group (P<0.05). And
no significant difference in mean functional scores was noted
between MCDT and CCDT group (P>0.05). In addition, radiographic
findings confirmed that no significant difference in CC-interval
was visible among three groups after surgery (P>0.05). And the
radiography of patients in three group showed satisfying operative
effect after one year (Figs.
5–7).
Discussion
It had basically been obtained a consensus that the
Rockwood type IV, V and VI injury should be treated with operation.
However, the treatment of type III was still controversial
(25,49–52).
Nowadays, it had been put forward more and more high demands to the
range of shoulder motion and its flexibility, but there were so
much uncertainty and instability about conservative treatment. As a
consequence, great emphases were put on the operational treatments
(53–55). In addition, at present, the CHPF was
the commonly recognized operation method with many advantages
(56–59), for example, the great
histocompatibility, the anatomic design, attaching with distal
clavicular, stable fixation, continuously pressurizing distal
clavicular, keeping slight activity of AC joint and noninterference
in the normal physiological structure of AC joint. Nevertheless,
studies had been reported that the CHPF also showed many
complications, including shoulder pain, subacromial inpingement,
redislocation after extracting the internal fixation, even a stress
fracture, and so on (60–62). Moreover, the CHPF provided healing
condition for the AC ligament, the AC ligament and the surrounding
soft tissue, even though the healing scar could not ensure the
stability of the activity after shoulder surgery. With the
application of arthroscopy and double-endobutton, treatment of ACD
of the Rockwood type III has entered into a new period.
The MCDT was to be improved on the basis of CCDT,
making fixation more solid, simple, convenient and faster. Thus, it
not only inherited the advantages of CCDT, but also had its own new
superiority: ① The MCDT was in advance of making a closed-loop
between two endobuttons, it could not only keep the integrity of
the double-endobutton with loops, but also save the redundant steps
of CCDT such as resetting, knoting and so on. The MCDT could
achieve firm fixation to avoid the slip of sutures in CCDT, at the
same time, reduce the operation time and blood loss effectively.
ii) The minimally invasive surgical procedure was adopted, without
exposing the AC joint in surgery, and the operation did not involve
the rotator cuff, only 1.5-cm invasive incision was made minimally,
and the incisions of arthroscopic conventional approach were no
more than 1 cm, so it reduced blood loss and postoperative
complications. Furthermore, it could deal with the associated
injuries (rotator cuff injury, SLAP injury, Bankart injury, etc),
and help patients with more satisfied recovery. iii) The AC joint
was slightly movable joint attached with the surrounding ligaments
and other soft tissue, in the procedure, the ACD was restored and
AC ligament was reconstructed by the loop, the clavicle was fixed
in the original anatomical position, that ensured the stability of
shoulder joint. The AC joint was not used rigid fixation, so it
could maintain a certain fretting, which ensured the soft tissue to
heal in a stable environment, without any impingement-like pain and
other complications in future and early postoperative functional
exercise could be carried out. iv) When the bone tunnel of distal
clavicle and coracoid was established in surgery, we applied the
guiding locator which could accurately locate on the insertion of
the coracoid base of AC ligament, avoiding the situation such as
the iatrogenic fracture, the injury of nerves and vessels (63). v) The loop was provided by Pfizer,
and it was said that the strength of the device was more than 40%
of the body's ligaments (48).
Meanwhile, it was an implantable material with advantageous
biocompatibility, no degradation and long-term retention in the
body, without removing internal fixation surgery and avoiding the
possibility of recurrence of dislocation. Additionally, the
following matters should also be payed attention to in the MCDT: i)
Operators should control the contralateral the accurate measurement
of CC-interval, to determine the length of the loop, and a few
loops that were different lengths should be prepared before the
surgery. ii) When coracoid tunnel was established, an optimal view
should be found by arthroscopy in order to avoid the injury of
brachial plexus and axillary arteries. Meanwhile, bone tunnel
should be drilled an appropriate depth to keep the surrounding
tissues from injury.
Firstly, CHPF for ACD had been applied for many
years, which was a mature technology with widely application
(64). In CHPF group, as a reference
to compare with the MCDT group, any difference could not be found
in statistically significant in operative time, but both the CHPF
and MCDT group were better than the CCDT group, which indicated
that surgical procedure of CCDT was relatively cumbersome,
especially in resetting and fixing the endobutton on the top of
clavicle, it was difficult for manipulation and took so much time.
Secondly, in incision length, the MCDT and CCDT group were better
than the CHPF group, because the arthroscopic incisions was
minimally invasive. Thirdly, in intraoperative hemorrhage, the MCDT
and CCDT group were better than CHPF group, Moreover, the MCDT
group took less operation time than the CCDT group. mainly because
that the MCDT and CCDT used minimally invasive surgery which
reduced intraoperative hemorrhage, meanwhile the MCDT was to be
improved on the basis of CCDT, making more convenient and faster.
On the other hand, in the postoperative follow-up indicators, all
groups were better than before surgery, and comparing the
CC-interval value of the three groups after 1 year of follow-up,
the difference was not statistically significant, which indicated
three kinds of surgical methods were clinically effective. However,
after 1 year follow-up, the MCDT and CCDT group were better than
CHPF group, it associated with that large incision, soft tissue
damage, the poor attachment of plate caused the limitation of
shoulder mobility and the acromion impingement. On the contrary,
few tissue damage was found around the shoulder joint with the
MCDT, which was better for rehabilitating the shoulder joint at
early stage.
However, the present study still has limitations.
Firstly, all cases enrolled were from the same hospital but not
multi-center study. Secondly, the total length of the loops was
approximately equal to CC-interval in uninjured side shoulder,
which maybe lead to ignore the physiological difference between the
left and right side. Additionally, radiographic results were only
measured in the vertical direction and did not account for
displacement in the anteroposterior direction. In the following
study, we will explore some more about it, consider some ways to
modify the surgery. Moreover, related anatomic variation in AC
joint also remained to be further studied. Only in these ways can
we make a better contribution to clinical treatment for shoulder
injury. Finally, in the present study, Rockwood type III ACD was
suggested to receive the early surgical treatment, so we hadn't set
up blank control group.
In conclusion, three kinds of surgeries to treat
Rockwood type III ACD all were clinical effective. Although the
MCDT in treating Rockwood type III ACD performed a remarkable
effect and it had been widely used, there is still so much room for
improvement. The MCDT group had advantages in operative time,
incision length, intraoperative hemorrhage and the score of CMS,
UCLA, ASES, OSS and CC-interval. In brief, the MCDT, which was
improved on the basis of the CCDT, the operative time,
intraoperative hemorrhage had been significantly improved, that
made the reduction and fixation more solid, simple, convenient and
fast.
Acknowledgements
The present study was supported by the National
Natural Science Fund of China, grant no. 81674095, Science and
Research Project of Education Department of Sichuan Province, grant
no. 17ZB0472, the Science and Technology Project of Office of
Science and Technology of Luzhou, grant no. 2016-176-13. We thank
all patients and their family members, as well as all orthopedics
from Affiliated Traditional Chinese Medicine Hospital of Southwest
Medical University.
Glossary
Abbreviations
Abbreviations:
|
AC
|
acromioclavicular
|
|
ACD
|
acromioclavicular dislocation
|
|
MCDT
|
modified closed-loop double-endobutton
technique
|
|
CCDT
|
common closed-loop double-endobutton
technique
|
|
CHPF
|
clavicular hook plate fixation
|
|
CMS
|
Constant-Murley Score
|
|
UCLA
|
University of California at Los
Angeles shoulder rating scale
|
|
ASES
|
rating scale of the American Shoulder
and Elbow Surgeons
|
|
OSS
|
Oxford Shoulder Score
|
|
CC-interval
|
coracoclavicular interval
|
References
|
1
|
Kim AC, Matcuk G, Patel D, Itamura J,
Forrester D, White E and Gottsegen CJ: Acromioclavicular joint
injuries and reconstructions: A review of expected imaging findings
and potential complications. Emerg Radiol. 19:399–413. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gstettner C, Tauber M, Hitzl W and Resch
H: Rockwood type III acromioclavicular dislocation: Surgical versus
conservative treatment. J Shoulder Elbow Surg. 17:220–225. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tauber M: Management of acute
acromioclavicular joint dislocations: Current concepts. Arch Orthop
Trauma Surg. 133:985–995. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tossy JD, Mead NC and Sigmond HM:
Acromioclavicular separations: Useful and practical classification
for treatment. Clin Orthop Relat Res. 28:111–119. 1963.PubMed/NCBI
|
|
5
|
Rockwood CJ, Williams G and Young D:
Disorders of the acromioclavicular jointThe Shoulder. 2nd. Rockwood
CJ and Matsen FA III: Philadelphia: WB Saunders; pp. 483–553.
1998
|
|
6
|
Guy DK, Wirth MA, Griffin JL and Rockwood
CA Jr: Reconstruction of chronic and complete dislocations of the
acromioclavicular joint. Clin Orthop Relat Res. 1–149.
1998.PubMed/NCBI
|
|
7
|
Pallis M, Cameron KL, Svoboda SJ and Owens
BD: Epidemiology of acromioclavicular joint injury in young
athletes. Am J Sports Med. 40:2072–2077. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kongmalai P, Apivatgaroon A and
Chernchujit B: Morphological classification of acromial spur:
Correlation between Rockwood tilt view and arthroscopic finding.
SICOT J. 3:42017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McNeil JW, Beaulieu-Jones BR, Bernhardson
AS, LeClere LE, Dewing CB, Lynch JR, Golijanin P, Sanchez G and
Provencher MT: Classification and analysis of attritional glenoid
bone loss in recurrent anterior shoulder instability. Am J Sports
Med. 45:767–774. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gorbaty JD, Hsu JE and Gee AO:
Classifications in brief: Rockwood classification of
acromioclavicular joint separations. Clin Orthop Relat Res.
475:283–287. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
von Heideken J, Bostrȍm Windhamre H,
Une-Larsson V and Ekelund A: Acute Surgical treatment of
acromioclavicular dislocation type V with a hook plate: Superiority
to late reconstruction. J Shoulder Elbow Surg. 22:9–17. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wellmann M, da Silva G, Lichtenberg S,
Magosch P and Habermeyer P: Instability pattern of
acromioclavicular joint dislocations type Rockwood III: Relevance
of horizontal instability. Orthopade. 42:271–277. 2013.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kezunović M, Bjelica D and Popović S:
Comparative study of surgical treatment of acromioclavicular
luxation. Vojnosanit Pregl. 70:292–297. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Virtanen KJ, Remes VM, Tulikoura IT,
Pajarinen JT, Savolainen VT, Björkenheim JM and Paavola MP:
Surgical treatment of Rockwood grade-V acromioclavicular joint
dislocations: 50 patients followed for 15–22 years. Acta Orthop.
84:191–195. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kienast B, Thietje R, Queitsch C, Gille J,
Schulz AP and Meiners J: Mid-term results after operative treatment
of Rockwood grade III–V Acromioclavicular joint dislocations with
an AC-hook-plate. Eur J MedRes. 16:52–56. 2011.
|
|
16
|
Kovilazhikathu Sugathan H and Dodenhoff
RM: Management of type 3 acromioclavicular joint dislocation:
Comparison long-term functional results of two operative methods.
ISRN Surg. 2012:5805042012.PubMed/NCBI
|
|
17
|
Gille J, Heinrichs G, Unger A, Riepenhof
H, Herzog J, Kienast B and Oheim R: Arthroscopic-assisted hook
plate fixation for acromioclavicular joint dislocation. Int Orthop.
37:377–382. 2013. View Article : Google Scholar
|
|
18
|
Struhl S: Double endobutton technique for
repair of complete acromioclavicular joint dislocations. Tech
Shoulder Elbow Surg. 8:175–179. 2007. View Article : Google Scholar
|
|
19
|
Di Francesco A, Zoccali C, Colafarina O,
Pizzoferrato R and Flamini S: The use of hook plate in type III and
V acromio-clavicular Rockwood dislocations: Clinical and
radiological midterm results and MRI evaluation in 42 patients.
Injury. 43:147–152. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sandmann GH, Martetschläger F, Mey L,
Kraus TM, Buchholz A, Ahrens P, Stöckle U, Freude T and Siebenlist
S: Reconstruction of displaced acromio-clavicular joint
dislocations using a triple suture-cerclage: Description of a safe
and efficient surgical technique. Patient Saf Surg. 6:252012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ranne JO, Sarimo JJ, Rawlins MI, Heinonen
OJ and Orava SY: All-arthroscopic double-bundle coracoclavicular
ligament reconstruction using autogenous semitendinosus graft: A
new technique. Arthrosc Tech. 1:e11–e14. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Choi NH, Lim SM, Lee SY and Lim TK: Loss
of reduction and complications of coracoclavicular ligament
reconstruction with autogenous tendon graft in acute
acromioclavicular dislocations. J Shoulder Elbow Surg. 26:692–698.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Clavert P, Meyer A, Boyer P, Gastaud O,
Barth J and Duparc F: SFA: Complication rates and types of failure
after arthroscopic acute acromioclavicular dislocation fixation.
Prospective multicenter study of 116 cases. Orthop Traumatol Surg
Res. 101 8 Suppl:S313–S316. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Helfen T, Siebenbürger G, Ockert B and
Haasters F: Therapy of acute acromioclavicular joint instability.
Meta-analysis of arthroscopic/minimally invasive versus open
procedures. Unfallchirurg. 118:415–426. 2015.(In German).
|
|
25
|
Longo UG, Ciuffreda M, Rizzello G,
Mannering N, Maffulli N and Denaro V: Surgical versus conservative
management of Type III acromioclavicular dislocation: A systematic
review. Br Med Bull. 122:31–49. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zumstein MA, Schiessl P, Ambuehl B,
Bolliger L, Weihs J, Maurer MH, Moor BK, Schaer M and Raniga S: New
quantitative radiographic parameters for vertical and horizontal
instability in acromioclavicular joint dislocations. Knee Surg
Sports Traumatol Arthrosc. May 25–2017.(Epub ahead of print).
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Porschke F, Schnetzke M, Aytac S,
Studier-Fischer S, Gruetzner PA and Guehring T: Sports activity
after anatomic acromioclavicular joint stabilisation with
flip-button technique. Knee Surg Sports Traumatol Arthrosc.
25:1995–2003. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Faggiani M, Vasario GP, Mattei L, Calò MJ
and Castoldi F: Comparing mini-open and arthroscopic
acromioclavicular joint repair: Functional results and return to
sport. Musculoskelet Surg. 100:187–191. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Biz C, Berizzi A, Cappellari A, Crimì A,
Tamburin S and Iacobellis C: The treatment of acute Rockwood type
III acromio-clavicular joint dislocations by two different surgical
techniques. Acta Biomed. 86:251–259. 2015.PubMed/NCBI
|
|
30
|
Struhl S and Wolfson TS: Closed-loop
double endobutton technique for repair of unstable distal clavicle
fractures. Orthop J Sports Med. 4:23259671166578102016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ye G, Peng CA, Sun HB, Xiao J and Zhu K:
Treatment of Rockwood type III acromioclavicular joint dislocation
usingautogenous semitendinosus tendon graft and endobutton
technique. Ther Clin Risk Manag. 12:47–51. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Horst K, Garving C, Thometzki T, Lichte P,
Knobe M, Dienstknecht T, Hofman M and Pape HC: Comparative study on
the treatment of Rockwood type III acuteacromioclavicular
dislocation: Clinical results from the TightRope®
technique vs. K-wire fixation. Orthop Traumatol Surg Res.
103:171–176. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Thomas K, Litsky A, Jones G and Bishop JY:
Biomechanical comparison of coracoclavicular reconstructive
techniques. Am J Sports Med. 39:804–810. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Groh GI, Mighell MA, Basamania CJ and
Kibler WB: All things clavicle: From acromioclavicular to
sternoclavicular and all points in between. Instr Course Lect.
65:181–196. 2016.PubMed/NCBI
|
|
35
|
Grantham C, Heckmann N, Wang L, Tibone JE,
Struhl S and Lee TQ: A biomechanical assessment of a novel double
endobutton technique versus a coracoid cerclage sling for
acromioclavicular and coracoclavicular injuries. Knee Surg Sports
Traumatol Arthrosc. 24:1918–1924. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kumar N and Sharma V: Hook plate fixation
for acute acromioclavicular dislocations without coracoclavicular
ligament reconstruction: A functional outcome study in military
personnel. Strategies Trauma Limb Reconstr. 10:79–85. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lu D, Wang T, Chen H and Sun LJ: A
comparison of double Endobutton and triple Endobutton techniques
for acute acromioclavicular joint dislocation. Orthop Traumatol
Surg Res. 102:891–895. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hu WY, Yu C, Huang ZM and Han L: Double
Endobutton reconstituting coracoclavicular ligament combined with
repairing acromioclavicular ligament at stage I for the treatment
of acromioclavicular dislocation with Rockwood type III–V. Zhongguo
Gu Shang. 28:500–503. 2015.(In Chinese). PubMed/NCBI
|
|
39
|
Struhl S, Wolfson TS and Kummer F:
Axial-plane biomechanical evaluation of 2 suspensory cortical
button fixation constructs for acromioclavicular joint
reconstruction: Orthop. J Sports Med. 16:23259671166746682016.
|
|
40
|
Struhl S and Wolfson TS: Continuous loop
double endobutton reconstruction for acromioclavicular joint
dislocation. Am J Sports Med. 43:2437–2444. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Beris A, Lykissas M, Kostas-Agnantis I,
Vekris M, Mitsionis G and Korompilias A: Management of acute
acromioclavicular joint dislocation with a double-button fixation
system. Injury. 44:288–292. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Li H, Wang C, Wang J, Wu K and Hang D:
Restoration of horizontal stability in complete acromioclavicular
joint separations: Surgical technique and preliminary results. Eur
J Med Res. 18:422013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Constant CR and Murley AH: A clinical
method of functional assessment of the shoulder. Clin Orthop Relat
Res. 1–164. 1987.
|
|
44
|
Amstutz HC, Sew Hoy AL and Clarke IC: UCLA
anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1–20.
1981.
|
|
45
|
Richards RR, An KN, Bigliani LU, Friedman
RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA and
Zuckerman JD: A standardized method for the assessment of shoulder
function. J Shoulder Elbow Surg. 3:347–352. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Dawson J, Fitzpatrick R and Carr A: The
assessment of shoulder instability: The development and validation
of a questionnaire. J Bone Joint surg Br. 81:420–426. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Beitzel K, Cote MP, Apostolakos J,
Solovyova O, Judson CH, Ziegler CG, Edgar CM, Imhoff AB, Arciero RA
and Mazzocca AD: Current concepts in the treatment of
acromioclavicular joint dislocations. Arthroscopy. 29:387–397.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Takase K and Yamamoto K: Changes in
surgical procedures for acromioclavicular joint dislocation over
the past 30 years. Orthopedics. 36:e1277–e1282. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Arirachakaran A, Boonard M, Piyapittayanun
P, Kanchanatawan W, Chaijenkij K, Prommahachai A and
Kongtharvonskul J: Post-operative outcomes and complications of
suspensory loop fixation device versus hook plate in acute unstable
acromioclavicular joint dislocation: A systematic review and
meta-analysis. J Orthop Traumatol. Feb 25–2017.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Murena L, Vulcano E, Ratti C, Cecconello
L, Rolla PR and Surace MF: Arthroscopic treatment of acute
acromioclavicular joint dislocation with double flip button. Knee
Surg Sports Traumatol Arthrosc. 17:1511–1515. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Korsten K, Gunning AC and Leenen LP:
Operative or conservative treatment in patients with Rockwood type
III acromioclavicular dislocation: A systematic review and update
of current literature. Int Orthop. 38:831–838. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Balke M, Schneider MM, Akoto R, Bähis H,
Bouillon B and Banerjee M: Acute acromioclavicular joint injuries:
Changes in diagnosis and therapy over the last 10 years.
Unfallchirurg. 118:851–857. 2014. View Article : Google Scholar
|
|
53
|
González-Erreguín V and Morales-Villanueva
J: Surgical treatment of acute acromioclavicular dislocation
Preliminary report. Acta Ortop Mex. 29:203–206. 2015.(In Spanish).
PubMed/NCBI
|
|
54
|
Ejam S, Lind T and Falkenberg B: Surgical
treatment of acute and chronic acromioclavicular dislocation Tossy
type III and V using the Hookplate. Acta Orthop Belg. 74:441–445.
2008.PubMed/NCBI
|
|
55
|
Nühtern JV, Sellenschloh K, Bishop N,
Jauch S, Briem D, Hoffmann M, Lehmann W, Pueschel K, Morlock MM,
Rueger JM and Großterlinden LG: Biomechanical evaluation of 3
stabilization methods on acromioclavicular joint dislocations. Am J
Sports Med. 41:1387–1394. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
McKee MD: Operative fixation of chronic
acromioclavicular joint dislocation with hook plate and modified
ligament transfer. J Orthop Trauma. 30 Suppl 2:S7–S8. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Lee CH, Shih CM, Huang KC, Chen KH, Hung
LK and Su KC: Biomechanical analysis of implanted clavicle hook
plates with different implant depths and materials in the
acromioclavicular joint: A finite element analysis study. Artif
Organs. 40:1062–1070. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lin HY, Wong PK, Ho WP, Chuang TY, Liao YS
and Wong CC: Clavicular hook plate may induce subacromial shoulder
impingement and rotator cuff lesion-dynamic sonographic evaluation.
J Orthop Surg Res. 9:62014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Sun S, Gan M, Sun H, Wu G, Yang H and Zhou
F: Does subacromial osteolysis affect shoulder function after
clavicle hook plating? Biomed Res Int. 2016:40853052016. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Shih CM, Huang KC, Pan CC, Lee CH and Su
KC: Biomechanical analysis of acromioclavicular joint dislocation
treated with clavicle hook plates in different lengths. Int Orthop.
39:2239–2244. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Coale RM, Hollister SJ, Dines JS, Allen AA
and Bedi A: Anatomic considerations of
transclavicular-transcoracoid drilling for coracoclavicular
ligament reconstruction. J Shoulder Surg. 22:137–144. 2013.
View Article : Google Scholar
|
|
62
|
Chaudry SN and Waseem M: Clavicular hook
plate: Complications of retaining the implant. Injury. 37:6652006.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Steinbacher G, Sallent A, Seijas R, Boffa
JM, Espinosa W and Cugat R: Clavicular hook plate for grade-III
acromioclavicular dislocation. J Orthop Surg (Hong Kong).
22:329–332. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Jafary D, Keihan Shokouh H, Najd Mazhar F,
Shariat Zadeh H and Mochtary T: Clinical and radiological results
of fixation of acromioclavicular joint dislocation by hook plates
retained for more than five months. Trauma Mon. 19:e137282014.
View Article : Google Scholar : PubMed/NCBI
|