Introduction
The primary goal when treating epilepsy is to
prevent seizures with minimal side effects to increase patients;
quality of life (1,2). In China, there are ~9 million people
with epilepsy, 6 million of which are diagnosed with active
epilepsy. Each year, 0.4 million new cases are reported (3). Mortality risk for epilepsy patients is
2–3 times higher than that of the normal population. Although
multiple drug therapies exist for epilepsy, anti-epilepsy drugs are
not effective for one-third of patients (4). These drugs only try to control the
symptoms of epilepsy, and do not affect the occurrence or
pathological processes of the disease (5).
Previous studies have indicated that autoimmune
disorders, such as systemic lupus erythematosus and vasculitis, are
important causes of epilepsy (6).
Invasion of activated microglial cells, inflammatory media and
lymphocytes in infant brains can trigger autoimmune disorders,
which can lead to catastrophic epilepsy in children (7). In addition, patients with autoimmune
diseases of the central nervous system or N-methyl-D-aspartate
receptor encephalitis are at a high risk of epilepsy (8). Inflammation is a key factor in the
occurrence and recurrence of epilepsy and has been associated with
its pathological severity (9).
Epilepsy is a disease of the nervous system.
Repeated attacks can result in brain neuron injuries or patient
fatality (10). The
phosphatidylinositol-3-kinase (PI3K)/protein kinase B (Akt) signal
transduction pathway is a key intra-cellular survival pathway
(11). Whether cell apoptosis occurs
or not largely depends on activation of the PI3K/Akt signal
transduction pathway and a cascade of downstream signals (12).
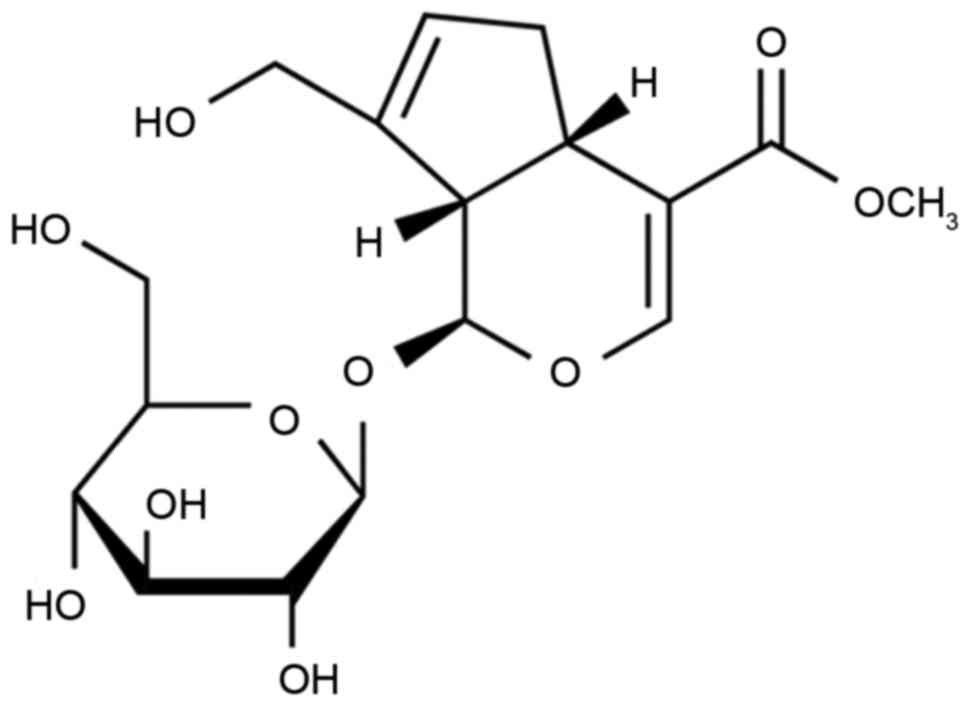
Gardenia jasminoides Ellis is principally
grown in Zhejiang, Fujian, Jiangxi, Hunan and Guangdong in China.
Geniposide is derived from G. jasminoides Ellis and previous
studies have suggested that it can be used to reduce fever, acute
icteric hepatitis, cystitis and upper gastrointestinal hemorrhage
(13–15). The present study aimed to investigate
whether geniposide treatment could reduce epilepsy symptoms in a
mouse model through the PI3K/Akt/glycogen synthase kinase-3β
(GSK-3β) signaling pathway.
Materials and methods
Animals
All experimental protocols were performed in
accordance with the guidelines of the Institutional Animal Care and
Use Committee of The Second People's Hospital of Gansu Province
(Lanzhou, China). Ethical approval was granted by the Ethics
Committee of the Second People's Hospital of Gansu Province. A
total of 38 C57Bl/6 mice aged 11–12 weeks (20–23 g, male) obtained
from Medical Experimental Center of Lanzhou University (Lanzhou,
China) were used in the present study and housed in an animal
laboratory (temperature, 22±1°C; humidity, 55±5%) on a 12 h
light/dark cycle.
Mouse model of epilepsy and
grouping
A mouse model of epilepsy was induced by maximal
electric shock (50 mA, 50 Hz, 1 sec) through ear clip electrodes
using a stimulator apparatus, as previously described (16). Mice were randomly assigned into the
following groups: Sham (10 ml/kg saline, n=6), epilepsy model (10
ml/kg saline, n=8), 5 Gen group (5 mg/kg geniposide, n=8), 10 Gen
group (10 mg/kg geniposide, n=8) and 20 Gen group (20 mg/kg
geniposide, n=8). Saline and geniposide were administered
intragastrically. Geniposide was purchased from Sigma-Aldrich
(Merck KGaA, Darmstadt, Germany) and its chemical structure is
shown in Fig. 1.
Stereotaxic surgery and kindling
procedure
Mice were anesthetized with intravenous injection of
60 mg/kg ketamine and 10 mg/kg xylazine (Sigma-Aldrich; Merck KGaA)
and then stereotaxically implanted with bipolar stimulating and
monopolar recording stainless-steel Teflon-coated electrodes (A-M
Systems, Sequim, WA, USA; −2.5 mm from bregma, 4.8 mm lateral and
7.4 mm ventral to dura). An additional electrode was attached to a
skull screw and fixed to the left cortical surface with dental
acrylic. At four weeks after treatment with geniposide, the after
discharge (AD) threshold was recorded in the amygdala using a 2-sec
stimulus (100 Hz, 1 msec/pulse). Stimulation was initially
delivered at 50 µA with 5-min intervals. Then stimulus intensity
was increased by 50 µA, which was delivered until at least 5 sec of
AD threshold was recorded. AD threshold was measured once a day
until three consecutive stage 5 seizures were observed. The seizure
stages were defined as follows: Stage 1, facial clonus; stage 2,
head nodding; stage 3, forelimb clonus; stage 4, rearing and
bilateral forelimb clonus; stage 5, rearing, loss of balance and
falling (17). In the sham group,
mice were anesthetized as above and no surgical procedures were
performed. Following induction of the AD model, all mice were
immediately weighed and were subsequently weighed at weeks 1, 2, 3
and 4.
Clonic seizures or generalized
seizures
Mice that appeared less active and exhibited
fremitus, mutation, scratching, face twitching or disequilibrium
were considered to experience clonic seizures. Mice were scored as
follows; 0 seizures, stage 1; 1 seizure, stage 2; 2 seizures, stage
3; 3 seizures, stage 4; >3 seizures, stage 5. The incidence (%)
of clonic seizures was calculated using the following formula:
(number of clonic seizures/total number of mice) ×100. The number
of mice exhibiting each seizure stage (1–5 stages) was expressed as
S. The incidence (%) of generalized seizures as calculated using
the following formula: (S/total number ×5) ×100.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Following 4 weeks of treatment with geniposide, mice
were sacrificed by decapitation under anesthetization (intravenous
injection of 35 mg/kg pentobarbital sodium (Sigma-Aldrich; Merck
KGaA). Total RNA was extracted from blood using an Easy Total RNA
Extraction kit (Tiangen Biotech Co., Ltd., Beijing, China). Total
RNA (1 µg) was converted to cDNA using the ReverTra ACE-α-RNAeasy
kit (Toyobo Co., Ltd., Osaka, Japan). The Bio-Rad CFX96 Real-Time
system (Bio-Rad Laboratories, Inc., Hercules, CA, USA) was
performed to analyze the mRNA expression of inducible nitric oxide
synthase (iNOS) and cyclooxygenase-2 (COX-2). The primers used were
as follows: iNOS forward, 5′-GCTCGCTTTGCCACGGACGA-3′ and reverse,
5′-AAGGCAGCGGGCACATGCAA-3′; COX-2 forward,
5′-GGGCTCAGCCAGGCAGCAAAT-3′ and reverse,
5′-GCACTGTGTTTGGGGTGGGCT-3′; β-actin forward,
5′-CTGTCCCTGTATGCCTCTG-3′ and reverse, 5′-ATGTCACGCACGATTTCC-3′. A
custom PCR master mix (Tiangen Biotech Co., Ltd., Beijing, China)
was used. The reaction conditions were as follows: 95°C for 45 sec,
followed by 40 cycles of 95°C for 30 sec, 55°C for 40 sec and 72°C
for 30 sec.
Western blot analysis
Hippocampus tissue samples were homogenized using
radioimmunoprecipitation assay buffer (Beyotime Institute of
Biotechnology) and protease/phosphatase inhibitor cocktail (EMD
Millipore, Billerica, MA, USA). The cell lysate was centrifuged at
12,000 × g for 10 min at 4°C and the supernatant was collected.
Protein concentrations were determined using a bicinchoninic acid
protein assay kit (Beyotime Institute of Biotechnology). Proteins
(20 µg) were separated by 8–12% SDS-PAGE and transferred to
polyvinylidene difluoride membranes. The membranes were blocked
with 5% bovine serum albumin (NanJing SunShine Biotechnology Co.,
Ltd., Nanjing, China) for 1 h at room temperature and probed with
anti-AP-1 (1:3,000), anti-PI3K (sc-7174; 1:2,000), anti-Akt
(sc-8312; 1:2,000) and anti-phosphorylated (p)-Akt (sc-7985-R;
1:5,000; all Genetimes Technology, Inc., Shanghai, China),
anti-GSK-3β (sc-7879; 1:2,000; Santa Cruz Biotechnology, Inc.,
Dallas, TX, USA) and anti-β-actin (sc-7210; 1:5,000; Genetimes
Technology, Inc.) overnight at 4°C. The membranes were then washed
with TBS with Tween-20 and incubated with horseradish
peroxidase-conjugated secondary antibody (sc-2004; 1:5,000; Santa
Cruz Biotechnology, Inc.) at 37°C for 1 h. The results were
visualized using an enhanced chemiluminescence substrate reagent
kit (EMD Millipore). Protein expression was measured using the
ChemiDoc™ XRS luminescent image analyzer and Image Lab version
2.0.1 software (both Bio-Rad Laboratories, Inc.).
Statistical analysis
All values are presented as the mean ± standard
error of the mean. Statistical analysis was performed using SPSS
17.0 software (SPSS, Inc., Chicago, IL, USA) and the two-tailed
Student's t-test or one-way analysis of variance. P<0.05 was
considered to indicate a statistically significant difference.
Results
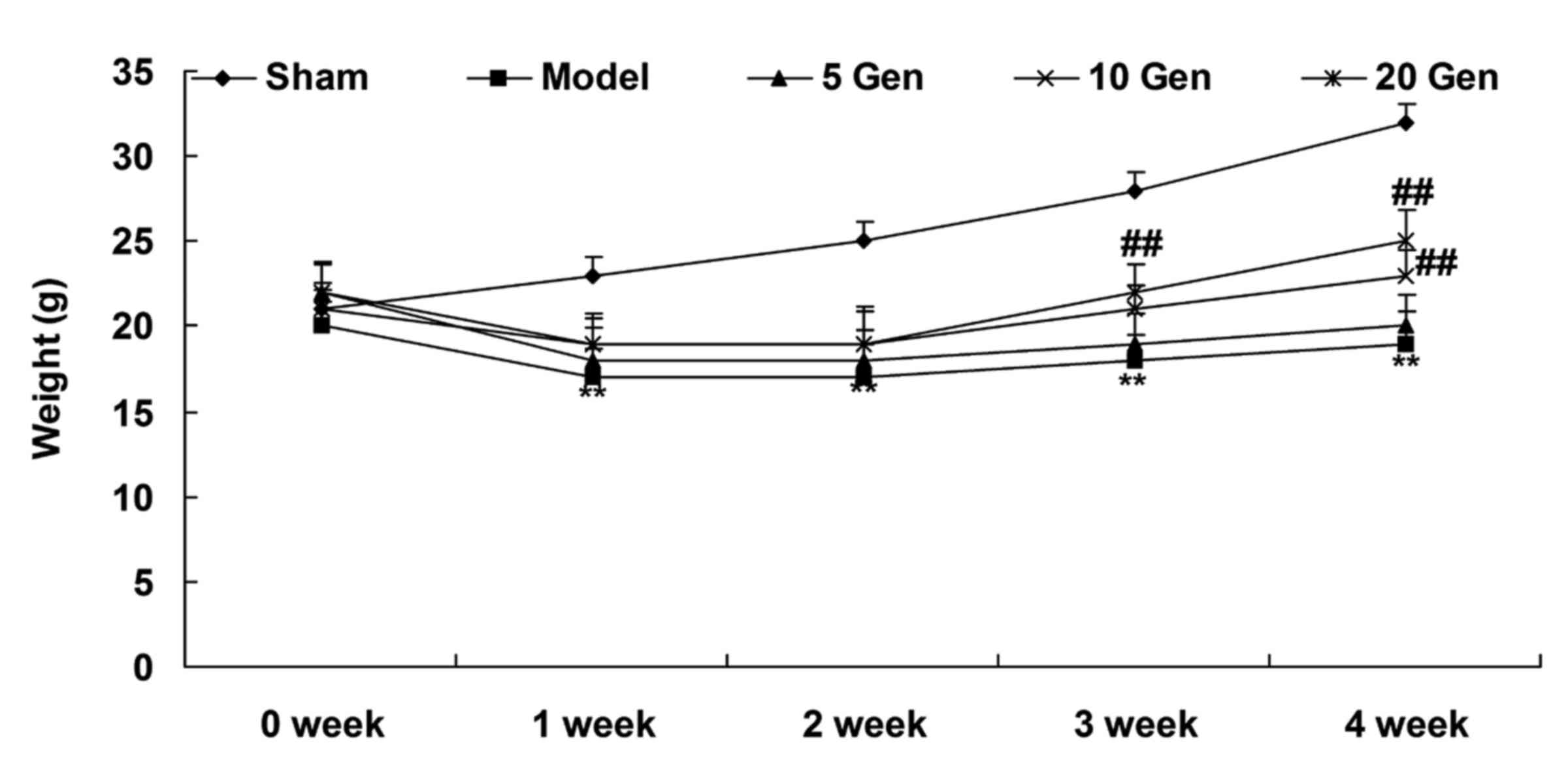
Effect of epilepsy and geniposide
treatment on mouse weight
At one week after geniposide treatment, the epilepsy
model mice weighed less than the Sham group (P<0.01; Fig. 2). The weights of the epilepsy model
mice increased from week 2 to 4, but remained lower than the Sham
group throughout the experimental period (P<0.01; Fig. 2).
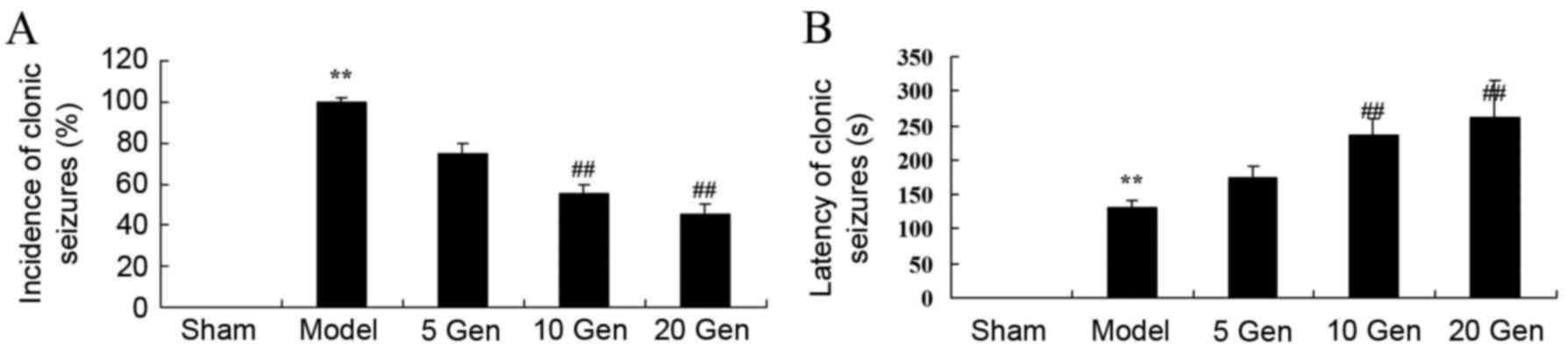
Effect of geniposide on clonic
seizures in mouse epilepsy
In the current study, the effects of geniposide
treatment on the incidence and latency of clonic seizures in mice
epilepsy were evaluated. The incidence of clonic seizures was
significantly higher in the epilepsy model control group compared
with the sham group (P<0.01; Fig.
3A). The latency of clonic seizures was significantly reduced
in the epilepsy model control group compared with the sham group
(P<0.01; Fig. 3B). However,
geniposide treatment (10 or 20 mg/kg) significantly reduced the
incidence and significantly increased the latency of clonic
seizures compared with the epileptic model control group (both
P<0.01; Fig. 3A and B).
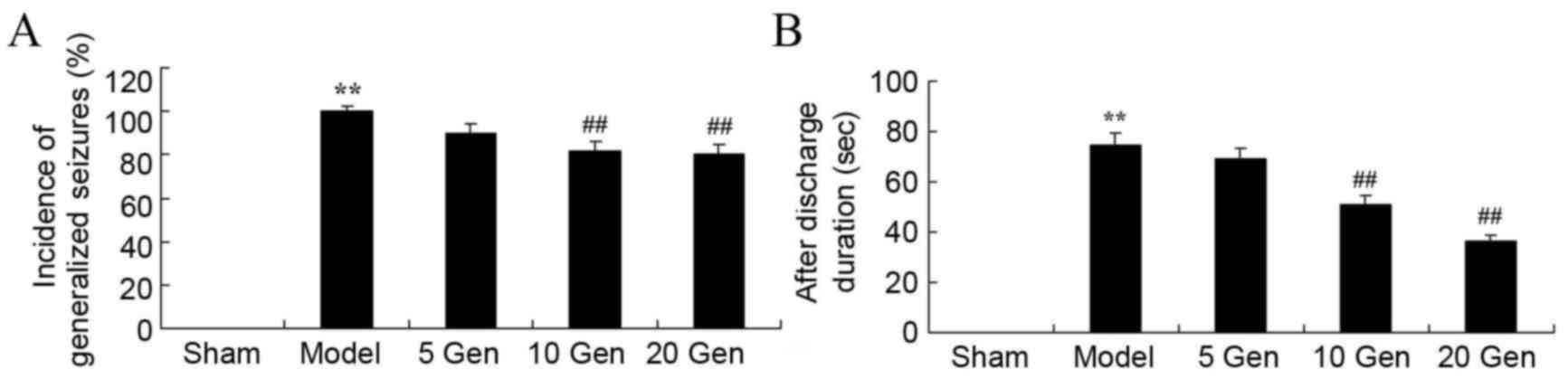
Effect of geniposide on generalized
seizures in mouse epilepsy
The epileptic model control group showed a
significant increase in the incidence of generalized seizures
compared with the sham group (P<0.01; Fig. 4A). A significant reduction was
observed in the incidence of generalized seizures after geniposide
treatment. However, there was a significant increase in AD duration
in the epilepsy model control group compared with the sham group
(P<0.01; Fig. 4B) and geniposide
treatment (10 or 20 mg/kg) significantly attenuated AD duration
compared with the epilepsy model control group (P<0.01; Fig. 4B).
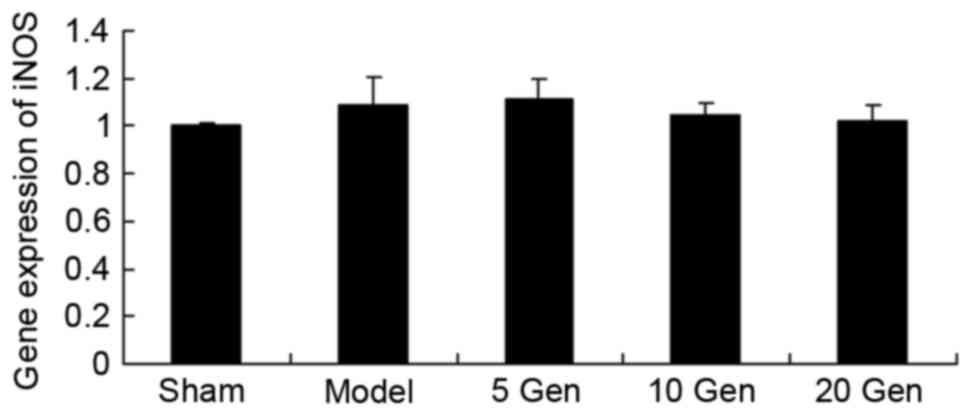
Effect of geniposide on iNOS mRNA
expression in mouse epilepsy
The level of iNOS mRNA expression in epileptic mice
was analyzed using RT-qPCR. As shown in Fig. 5, there was no significant difference
in iNOS mRNA expression between the sham group and the epileptic
model control, or between the epileptic model control and the
geniposide-treated epileptic groups.
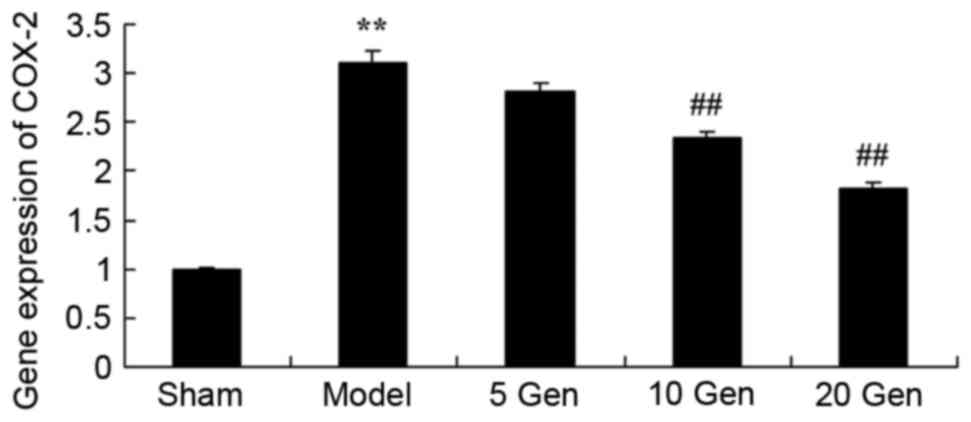
Effect of geniposide on COX-2 mRNA
expression in mouse epilepsy
The level of COX-2 mRNA expression in epileptic mice
was analyzed using RT-qPCR. As shown in Fig. 6, COX-2 mRNA expression was
significantly higher in the epilepsy model control group compared
with the sham group (P<0.01). Furthermore, treatment with
geniposide (10 or 20 mg/kg) significantly inhibited the
epilepsy-induced COX-2 mRNA expression compared with the epileptic
model control (P<0.01).
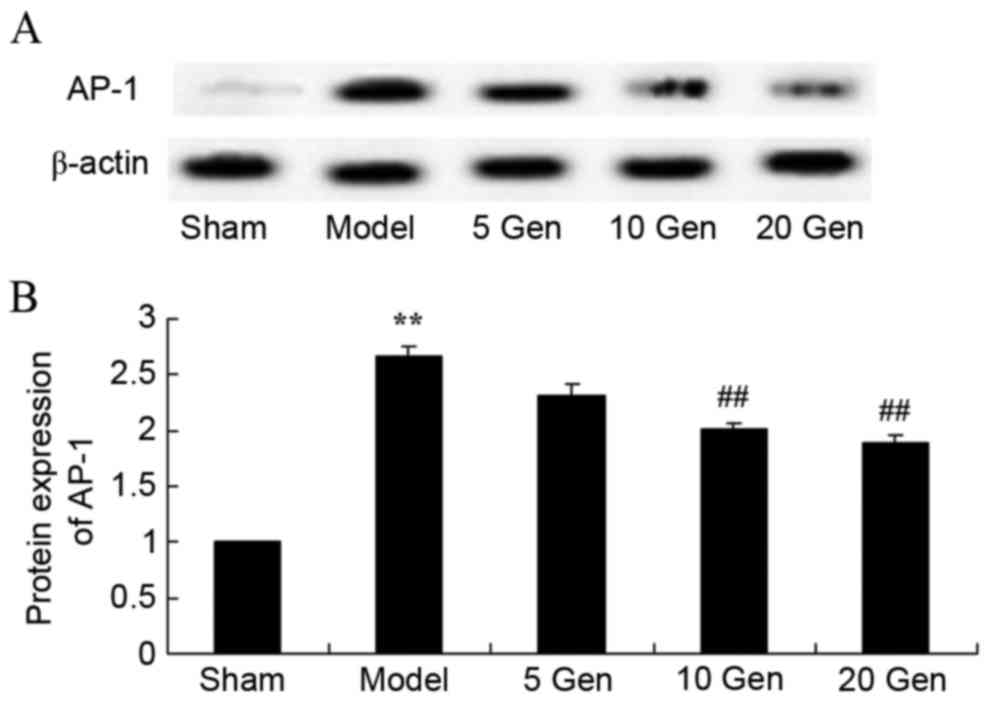
Effect of geniposide on AP-1 protein
expression in mouse epilepsy
The level of AP-1 protein expression was evaluated
by western blot analysis. As shown in Fig. 7, AP-1 protein expression was
significantly higher in the epilepsy model control group compared
with the sham group (P<0.01). Furthermore, treatment with
geniposide (10 or 20 mg/kg) significantly suppressed AP-1 protein
expression compared with the epileptic model control
(P<0.01).
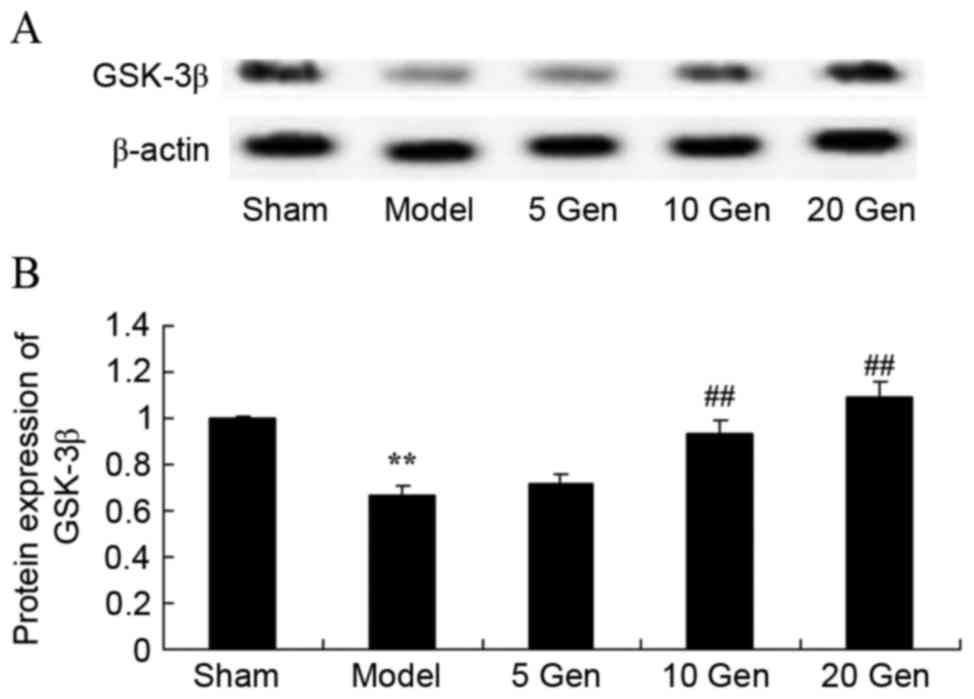
Effect of geniposide on GSK-3β protein
expression in mouse epilepsy
The level of GSK-3β protein expression was evaluated
by western blot analysis. As shown in Fig. 8, GSK-3β protein expression was
significantly lower in the epilepsy model control group compared
with the sham group (P<0.01). Furthermore, geniposide treatment
(10 or 20 mg/kg) significantly promoted GSK-3β protein expression
compared with the epileptic model control (P<0.01).
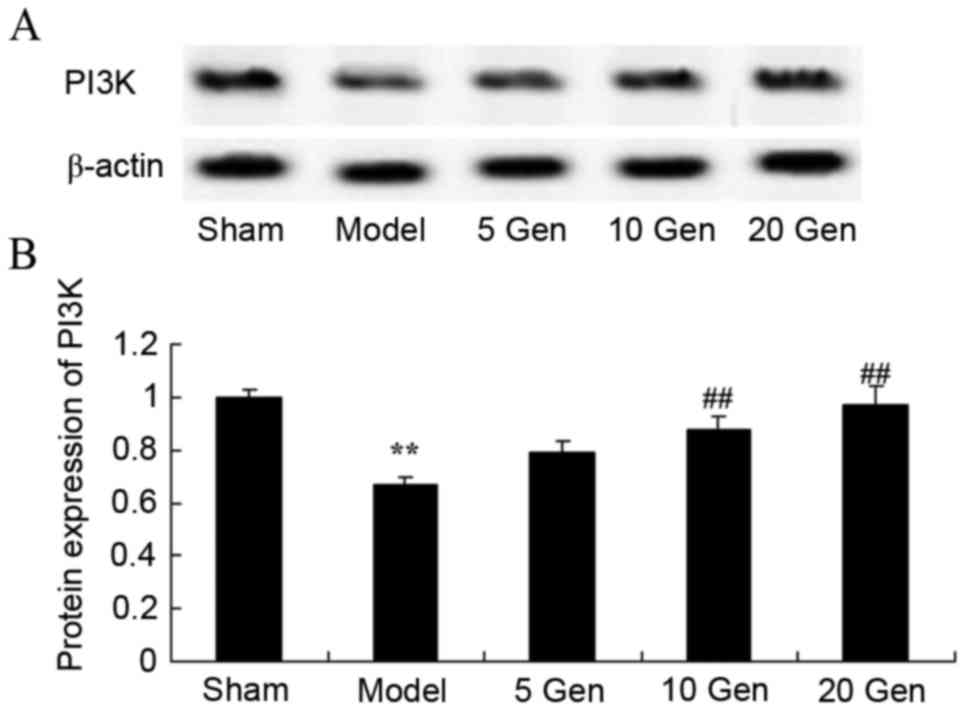
Effect of geniposide on PI3K protein
expression in mouse epilepsy
The level of PI3K protein expression was evaluated
by western blot analysis. As shown in Fig. 9, PI3K protein expression was
significantly lower in the epilepsy model control group compared
with the sham group (P<0.01). Furthermore, geniposide treatment
(10 or 20 mg/kg) significantly promoted PI3K protein expression
compared with the epileptic model control (P<0.01).
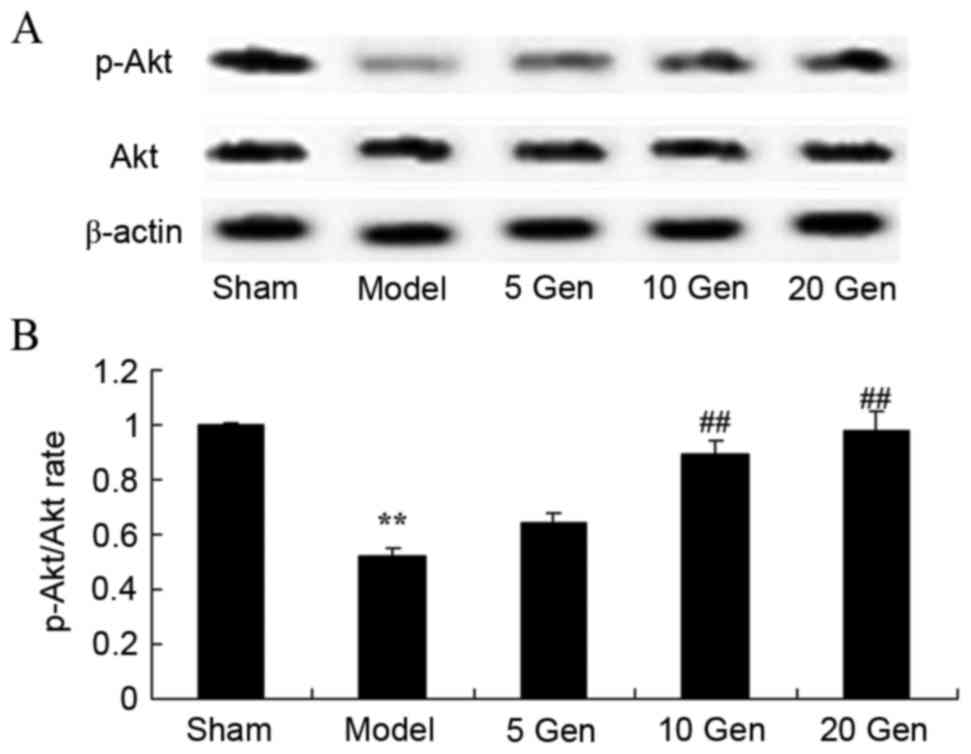
Effect of geniposide on Akt protein
expression in mouse epilepsy
In order to investigate the anti-apoptosis effects
of geniposide on Akt protein expression in mice epilepsy, Akt and
p-Akt protein expression was evaluated by western blot analysis
(Fig. 10). The p-Akt/Akt rate was
significantly reduced in the epilepsy model control group compared
with the sham group (P<0.01). Furthermore, treatment with
geniposide (10 or 20 mg/kg) significantly increased the p-Akt/Akt
rate compared with the epileptic model control (P<0.01).
Discussion
As a paroxysmal minimal brain dysfunction, epilepsy
is characterized by acute spasms. The morbidity rate of epilepsy is
24–53/100,000 in developed countries and 77–114/100,000 in
developing countries (18). The
morbidity rate in children is 151/10,000 (19). To the best of our knowledge, the
present study is the first to demonstrate a protective effect of
geniposide in mouse epilepsy, through a reduction in clonic.
Nitric oxide (NO) has a dual function of
neuroprotection and neurovirulence in the central nervous system
(20). Previous results indicated
that NO and NO synthase were significantly elevated in the brains
of epilepsy patients, which may be related to cell damages after an
attack of epilepsy (21). Previous
research also confirmed that cell apoptosis after epilepsy was
related to overexpression of NO, which demonstrated that iNOS was
more closely related with apoptosis (22). Another study demonstrated that a
selective iNOS inhibitor could significantly reduce the expression
of caspase-3 (23). The results of
the current study suggested that geniposide treatment did not
significantly affect iNOS mRNA expression in mouse epilepsy. Zhang
et al proposed that geniposide inhibits LPS-induced iNOS
expression in N9 microglial cells (24).
COX-2 participates in pathological processes such as
inflammation and tumor invasion (25). It has been found that multiple
stimuli, including cytokines, hormones, ischemia, hypoxemia,
epilepsy and phorbol ester can increase the expression of COX-2
(26). In the majority of cells,
COX-2 expression can increase rapidly after an attack of epilepsy
or cerebral ischemia and can be inhibited by corticosteroids
(27). Therefore, it is dynamically
regulated. The results of the current study indicated that
geniposide reduces COX-2 mRNA expression in mouse epilepsy. Shi
et al reported that geniposide suppresses lipopolysaccharide
(LPS)-induced iNOS and COX-2 signaling pathways in macrophages
(28).
Previous results have indicated that activated AP-1
is a key transcription factor for inflammatory responses and causes
severe inflammatory reactions, disturbs neural pathways, influences
nerve conduction and impairs tissues (29). A previous study confirmed that the
majority of inflammatory mediators are regulated by transcription
factors (29). AP-1 may regulate the
expression of inflammatory factors and therefore affect the
severity of inflammation and the efficacy of therapeutic strategies
(29). AP-1 is a homodimer or
heterodimer of c-fos and c-jun. Under basal conditions, the
concentration and activity of AP-1 are relatively low (30). When cells are stimulated, AP-1
expression increases (30). The
results of the current study indicated that geniposide reduces AP-1
protein expression in mouse epilepsy. Shi et al demonstrated
that geniposide suppresses the LPS-induced inflammatory cytokine,
prostaglandin E2, and NO through inhibition of AP-1 signaling
pathways in macrophages (28).
Akt has been demonstrated to be the direct
downstream substrate of PI3K (10).
As an inhibitor of PI3K can block the activation of Akt, the
activation status of PI3K/Akt pathways can be predicted by
observing the expression of p-Akt (10). Previous results have suggested that
apoptosis plays an important role in cerebral neuron death after
epilepsy (31). As a key component
of survival signal, Akt is necessary to cellular survival triggered
by growth factors, extra-cellular matrix and other stimulus
(31). Activated Akt is a cellular
survival factor that can help cells escape from programmed cell
death by inactivating multiple effector molecules of apoptosis
(32). In the present study, it was
demonstrated that geniposide induces PI3K/Akt pathways in mice
epilepsy. Guo et al reported that geniposide increases
insulin secretion in pancreatic β-cells through involvement of PI3K
(33). Park et al suggested
that geniposide may suppress transforming growth
factor-β1/epithelial-mesenchymal transition and activate Akt
signaling pathways in AML12 hepatocytes (34).
Composed of 23 sub-units of GSK-3α and GSK-3β, GSK-3
is a serine/threonine kinase (35).
It is a key component of multiple signal transduction pathways and
is closely associated with cell differentiation, proliferation and
apoptosis, and diseases such as diabetes, cancer and
neurodegenerative disease (36).
GSK-3β has been indicated to be extensively distributed in rat
cerebral tissues, with high levels of expression in the hippocampus
(36). A previous study on epilepsy
reported that GSK-3β could hyperphosphorylate
microtubule-associated protein tau. P-tau proteins are key
components of neurofibrillary tangles in epilepsy (35). Previous research has also reported
that excessive p-tau protein is related to cognitive impairment in
Alzheimer's disease (37). In the
present study, it was demonstrated that geniposide attenuates
GSK-3β protein expression in mice epilepsy. Collectively, Zhang
et al reported that insulin-deficient APP/PS1 transgenic and
GSK-3β protein expression in mouse model of Alzheimer's disease
(38).
In conclusion, the present study demonstrated that
geniposide attenuates clonic seizures and generalized seizures in
mice epilepsy. Furthermore, the current results indicate that
geniposide reduces COX-2 and AP-1 expression, and that the
underlying mechanism of geniposide involves the PI3K/Akt/GSK-3β
signaling pathway to adjust neurocyte apoptosis. These findings may
be beneficial for developing effective treatment strategies for
epilepsy.
Acknowledgements
The present study was supported by the Health
Industry Scientific Research Projects in Gansu Province (grant no.
GSWST2012-07).
References
|
1
|
Velez FF, Bond TC, Anastassopoulos KP,
Wang X, Sousa R, Blum D and Cramer JA: Impact of seizure frequency
reduction on health-related quality of life among clinical trial
subjects with refractory partial-onset seizures: A pooled analysis
of phase III clinical trials of eslicarbazepine acetate. Epilepsy
Behav. 68:203–207. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Anderson WS, Kossoff EH, Bergey GK and
Jallo GI: Implantation of a responsive neurostimulator device in
patients with refractory epilepsy. Neurosurg Focus. 25:E122008.
View Article : Google Scholar
|
|
3
|
Liu J, Liu Z, Zhang Z, Dong S, Zhen Z, Man
L and Xu R: Internet usage for health information by patients with
epilepsy in China. Seizure. 22:787–790. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tseng CH, Huang WS, Muo CH and Kao CH:
Increased risk of epilepsy among patients diagnosed with chronic
osteomyelitis. Epilepsy Res. 108:1427–1434. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aliasgharpour M, Dehgahn Nayeri N,
Yadegary MA and Haghani H: Effects of an educational program on
self-management in patients with epilepsy. Seizure. 22:48–52. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhu H, Zhu J, Zhao T, Wu Y, Liu H, Wu T,
Yang L, Zou Y, Zhang R and Zheng G: Alteration of interictal brain
activity in patients with temporal lobe epilepsy in the left
dominant hemisphere: A resting-state MEG study. Biomed Res Int.
2014:1714872014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yeh CC, Wang HH, Chou YC, Hu CJ, Chou WH,
Chen TL and Liao CC: High risk of gastrointestinal hemorrhage in
patients with epilepsy: A nationwide cohort study. Mayo Clin Proc.
88:pp. 1091–1098. 2013; View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yao BZ, Yu SQ, Yuan H, Zhang HJ, Niu P and
Ye JP: The role and effects of ANXA1 in temporal lobe epilepsy: A
protection mechanism? Med Sci Monit Basic Res. 21:241–246. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Huang WX, Yu F, Sanchez RM, Liu YQ, Min
JW, Hu JJ, Bsoul NB, Han S, Yin J, Liu WH, et al: TRPV1 promotes
repetitive febrile seizures by pro-inflammatory cytokines in
immature brain. Brain Behav Immun. 48:68–77. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shetty AK and Hattiangady B: Concise
review: Prospects of stem cell therapy for temporal lobe epilepsy.
Stem Cells. 25:2396–2407. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xiao Z, Peng J, Yang L, Kong H and Yin F:
Interleukin-1β plays a role in the pathogenesis of mesial temporal
lobe epilepsy through the PI3K/Akt/mTOR signaling pathway in
hippocampal neurons. J Neuroimmunol. 282:110–117. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zheng H, Wang X, Tang Z, Zheng W and Li Z:
The PI3K/Akt and ERK1/2 signaling pathways mediate the
erythropoietin-modulated calcium influx in kainic acid-induced
epilepsy. Neuroreport. 24:335–341. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Peng CH, Huang CN and Wang CJ: The
anti-tumor effect and mechanisms of action of penta-acetyl
geniposide. Curr Cancer Drug Targets. 5:299–305. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yue PF, Zheng Q, Wu B, Yang M, Wang MS,
Zhang HY, Hu PY and Wu ZF: Process optimization by response surface
design and characterization study on geniposide pharmacosomes.
Pharm Dev Technol. 17:94–102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Song X, Zhang W, Wang T, Jiang H, Zhang Z,
Fu Y, Yang Z, Cao Y and Zhang N: Geniposide plays an
anti-inflammatory role via regulating TLR4 and downstream signaling
pathways in lipopolysaccharide-induced mastitis in mice.
Inflammation. 37:1588–1598. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sardari S, Amiri M, Rahimi H, Kamalinejad
M, Narenjkar J and Sayyah M: Anticonvulsant effect of Cicer
arietinum seed in animal models of epilepsy: Introduction of an
active molecule with novel chemical structure. Iran Biomed J.
19:45–50. 2015.PubMed/NCBI
|
|
17
|
Szelenyi A, Joksimovic B and Seifert V:
Intraoperative risk of seizures associated with transient direct
cortical stimulation in patients with symptomatic epilepsy. J Clin
Neurophysiol. 24:39–43. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kibar AE, Unver O, Oflaz MB, Güven AS,
Balli S, Ece I, Erdem S and Içağasıoğlu FD: Effect of antiepilepsy
drug therapy on ventricular function in children with epilepsy: A
tissue Doppler imaging study. Pediatr Cardiol. 35:280–288. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chamberlain JM, Okada P, Holsti M, Mahajan
P, Brown KM, Vance C, Gonzalez V, Lichenstein R, Stanley R,
Brousseau DC, et al: Lorazepam vs diazepam for pediatric status
epilepticus: A randomized clinical trial. JAMA. 311:1652–1660.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Solla DF, Paiva TS, André M and Paiva WS:
Potential toxicity of dental nanomaterials to the central nervous
system. Int J Nanomedicine. 10:5593–5594. 2015.PubMed/NCBI
|
|
21
|
Payandemehr B, Khoshneviszadeh M,
Varastehmoradi B, Gholizadeh R, Bahremand T, Attar H, Bahremand A
and Dehpour AR: A COX/5-LOX inhibitor licofelone revealed
anticonvulsant properties through iNOS diminution in mice.
Neurochem Res. 40:1819–1828. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Per S, Tasdemir A, Yildirim M, Ayyildiz M,
Ayyildiz N and Agar E: The involvement of iNOS activity in the
anticonvulsant effect of grape seed extract on the
penicillin-induced epileptiform activity in rats. Acta Physiol
Hung. 100:224–236. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cetin F, Yazihan N, Dincer S and Akbulut
G: The effect of intracerebroventricular injection of beta amyloid
peptide (1–42) on caspase-3 activity, lipid peroxidation, nitric
oxide and NOS expression in young adult and aged rat brain. Turk
Neurosurg. 23:144–150. 2013.PubMed/NCBI
|
|
24
|
Zhang G, He JL, Xie XY and Yu C:
LPS-induced iNOS expression in N9 microglial cells is suppressed by
geniposide via ERK, p38 and nuclear factor-κB signaling pathways.
Int J Mol Med. 30:561–568. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
McCown TJ, Knapp DJ and Crews FT: Inferior
collicular seizure generalization produces site-selective cortical
induction of cyclooxygenase 2 (COX-2). Brain Res. 767:370–374.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tocco G, Freire-Moar J, Schreiber SS,
Sakhi SH, Aisen PS and Pasinetti GM: Maturational regulation and
regional induction of cyclooxygenase-2 in rat brain: Implications
for Alzheimer's disease. Exp Neurol. 144:339–349. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Polascheck N, Bankstahl M and Löscher W:
The COX-2 inhibitor parecoxib is neuroprotective but not
antiepileptogenic in the pilocarpine model of temporal lobe
epilepsy. Exp Neurol. 224:219–233. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shi Q, Cao J, Fang L, Zhao H, Liu Z, Ran
J, Zheng X, Li X, Zhou Y, Ge D, et al: Geniposide suppresses
LPS-induced nitric oxide, PGE2 and inflammatory cytokine by
downregulating NF-κB, MAPK and AP-1 signaling pathways in
macrophages. Int Immunopharmacol. 20:298–306. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Li DD, Feng ZH, Zhang WQ and Hong JS: The
changes of AP-1 DNA binding activity and components in hippocampus
of seizure-sensitive rat induced by kainate. Sheng Li Xue Bao.
50:385–391. 1998.PubMed/NCBI
|
|
30
|
Gan AM, Butoi ED, Manea A, Simion V, Stan
D, Parvulescu MM, Calin M, Manduteanu I and Simionescu M:
Inflammatory effects of resistin on human smooth muscle cells:
Up-regulation of fractalkine and its receptor, CX3CR1 expression by
TLR4 and Gi-protein pathways. Cell Tissue Res. 351:161–174. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Dong M, Yang G, Liu H, Liu X, Lin S, Sun D
and Wang Y: Aged black garlic extract inhibits HT29 colon cancer
cell growth via the PI3K/Akt signaling pathway. Biomed Rep.
2:250–254. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lee SH, Chun W, Kong PJ, Han JA, Cho BP,
Kwon OY, Lee HJ and Kim SS: Sustained activation of Akt by
melatonin contributes to the protection against kainic acid-induced
neuronal death in hippocampus. J Pineal Res. 40:79–85. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Guo LX, Liu JH and Yin F: Regulation of
insulin secretion by geniposide: Possible involvement of
phosphatidylinositol 3-phosphate kinase. Eur Rev Med Pharmacol Sci.
18:1287–1294. 2014.PubMed/NCBI
|
|
34
|
Park JH, Yoon J, Lee KY and Park B:
Effects of geniposide on hepatocytes undergoing
epithelial-mesenchymal transition in hepatic fibrosis by targeting
TGFbeta/Smad and ERK-MAPK signaling pathways. Biochimie. 113:26–34.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tong Z, Jiang B, Wu Y, Liu Y, Li Y, Gao M,
Jiang Y, Lv Q and Xiao X: MiR-21 protected cardiomyocytes against
doxorubicin-induced apoptosis by targeting BTG2. Int J Mol Sci.
16:14511–14525. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chen Y, Chen H, Wu X, Wang X, Lin W and
Yuan W: Comparative analysis of clinical outcomes between
zero-profile implant and cages with plate fixation in treating
multilevel cervical spondilotic myelopathy: A three-year follow-up.
Clin Neurol Neurosurg. 144:72–76. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Jackson RJ, Davis RJ, Hoffman GA, Bae HW,
Hisey MS, Kim KD, Gaede SE and Nunley PD: Subsequent surgery rates
after cervical total disc replacement using a Mobi-C Cervical Disc
Prosthesis versus anterior cervical discectomy and fusion: a
prospective randomized clinical trial with 5-year follow-up. J
Neurosurg Spine. 24:734–745. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhang Y, Yin F, Liu J and Liu Z:
Geniposide attenuates the phosphorylation of tau protein in
cellular and insulin-deficient APP/PS1 transgenic mouse model of
Alzheimer's disease. Chem Biol Drug Des. 87:409–418. 2016.
View Article : Google Scholar : PubMed/NCBI
|