Introduction
Laryngeal cancer is a kind of malignant tumor
derived from the laryngeal mucosal epithelial tissues (1), and its incidence rate accounts for 5%
in the incidence rate of systemic tumor and 14.2% in the incidence
rate of head-neck tumors (2). In the
ear-nose-throat filed, laryngeal cancer ranks third following
nasopharynx cancer and nasal cancer, and its incidence rate shows
an increasing trend, seriously threatening the health and life of
patients (3,4). Laryngeal cancer often occurs in people
aged 50–70 years, more frequently in males than in females; the
proportion of female patients with laryngeal cancer in the
Northeast China is higher than that in official reports in China
and worldwide. With the rapid development of head-neck tumor
surgery, the clinical treatment techniques have been constantly
developed and improved, but the prognosis is still not satisfactory
(5). In order to investigate the
related factors affecting the postoperative curative effect on
patients with laryngeal cancer, and to develop effective
therapeutic regimen and improve the survival rate of patients with
laryngeal cancer, the clinical data of 215 patients with laryngeal
cancer in the Central Hospital of Wuhan were retrospectively
analyzed.
Patients and methods
General materials
A total of 215 patients with laryngeal cancer
admitted in The Central Hospital of Wuhan from May 2010 to May 2017
were selected into the study strictly according to the inclusion
and exclusion criteria. Inclusion criteria: patients without
radiotherapy and chemotherapy before surgery; patients confirmed as
squamous cell carcinoma via cell biopsy; patients with complete
data; patients with first-onset cancer and treated in our hospital
for the first time. Exclusion criteria: patients with postoperative
recurrence of laryngeal cancer; patients who could not receive
surgical treatment due to distant metastasis; patient who refused
surgical treatment. In the 215 patients with laryngeal cancer,
there were 203 males and 12 females aged 41–80 years with an
average of 57.2±3.5 years. The vast majority of patients (n=175)
had a smoking history, accounting for 81.4%, and approximately
62.3% patients consumed alcohol frequently. Cancer type, there were
95 cases of supraglottic laryngeal cancer, 72 cases of glottic
laryngeal cancer and 48 cases of subglottic laryngeal cancer. In
terms of tumor differentiation degree, there were 78 cases of high
differentiation, 86 cases of moderate differentiation and 51 cases
of poor differentiation. According to the latest Union for
International Cancer Control (UICC) tumor lymph nodes metastasis
(TNM) staging criteria, there were 48 cases of T1 stage, 56 cases
of T2 stage, 68 cases of T3 stage and 43 cases of T4 stage. The
lymph node (N) stages were 101 cases of N0 stage, 63 cases of N1
stage and 51 cases of N2 stage. The study was approved by the
Ethics Committee of The Central Hospital of Wuhan and informed
consent was signed by the patients or the guardians.
Treatment methods
With surgical treatment as the basic treatment
measure, all patients received clinical examinations before
operation, and underwent total or partial laryngectomy through
laryngoscopy and computed tomography/magnetic resonance imaging
(CT/MRI) combined with the specific intraoperative situations. Of
215 patients, 148 underwent total laryngectomy, while 67 patients
underwent partial laryngectomy. One hundred and forty-four patients
received cervical lymph node dissection, while 71 patients did
not.
Follow-up
All patients were followed up via telephone,
outpatient return visit, letters, medical data and health insurance
card, with the date of operation as the starting point. The
survival time began from the date of operation to the date of
death, date of loss to follow-up or the last follow-up date.
Statistical analysis
SPSS 23.0 software (SPSS Inc., Chicago, IL, USA) was
used for the data processing and analysis. The survival rate was
calculated using Kaplan-Meier method, and the survival curve was
drawn. Log-rank test was used for single-factor analysis, while Cox
proportional hazard regression model was used for multiple-factor
analysis. P<0.05 was considered to indicate a statistically
significant difference.
Results
Follow-up results and survival
rates
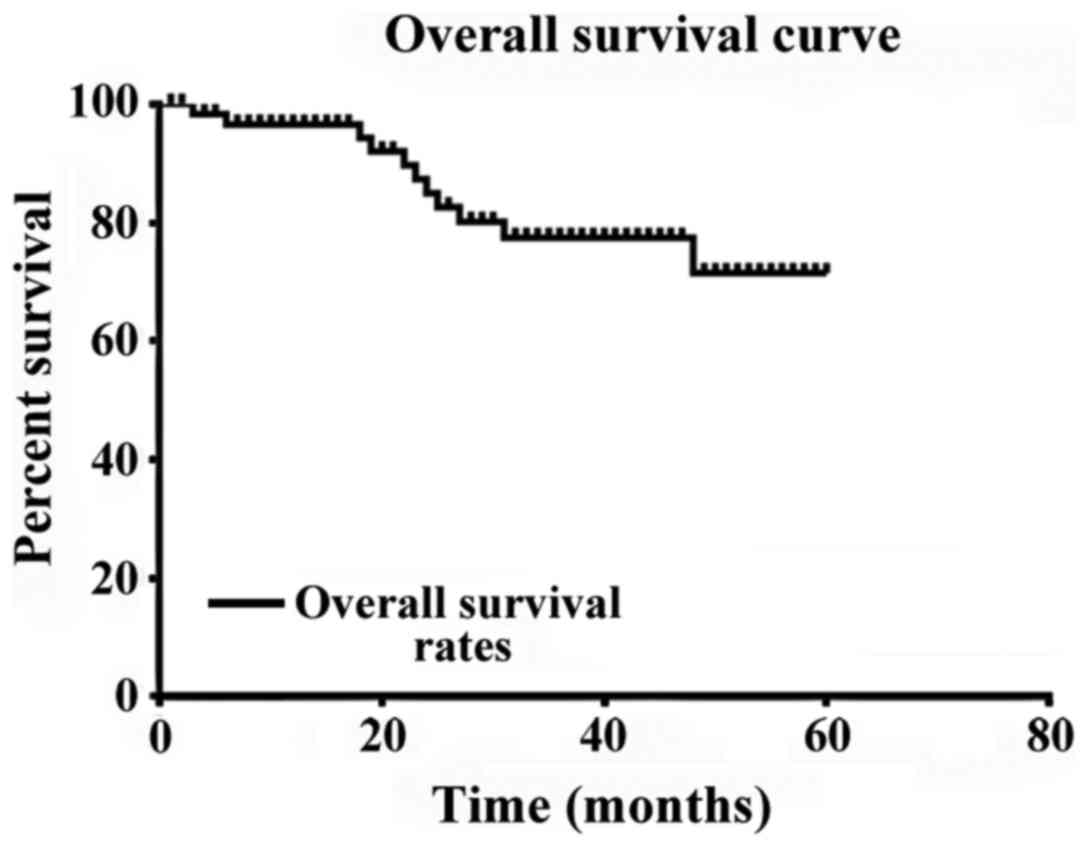
All of the 215 patients were followed up, and the
5-year follow-up rate was 100%. There were 16 cases of survival
without tumor, 10 cases of survival with tumor and 41 cases of
death, among which 21 cases died of laryngeal cancer recurrence, 2
cases died of lung metastasis, 1 case died of cervical metastasis,
4 cases died of heart disease and 13 cases died due to unknown
causes. The 1-, 3- and 5-year survival rates were 96.2, 78.0 and
72.5%, respectively, and the survival curve is shown in Fig. 1.
Single-factor analysis of
postoperative curative effect on patients with laryngeal
cancer
The results of single-factor analysis showed that
the age, primary tumor site, tumor differentiation degree, T stage,
N stage, smoking index, tumor diameter and lymph node metastasis
had significant influences on the postoperative curative effect on
patients (P<0.05), but the patient's age, drinking habit and
surgical method had no significant correlation with the
postoperative curative effect (P>0.05) (Table I).
 | Table I.Single-factor analysis of
postoperative curative effect on 215 patients with laryngeal
cancer. |
Table I.
Single-factor analysis of
postoperative curative effect on 215 patients with laryngeal
cancer.
| Characteristics | n | 3-year survival
rate | 5-year survival
rate | Log-rank value | P-value |
|---|
| Sex |
|
|
| 1.265 | 0.495 |
| Male | 203 (94.4%) | 81.4% | 73.1% |
|
|
|
Female | 12 (5.6%) | 79.6% | 71.2% |
|
|
| Age |
|
|
| 7.518 | 0.038 |
|
>57 | 139 (64.7%) | 65.5% | 35.2% |
|
|
| ≤57 | 76
(35.3%) | 82.5% | 73.0% |
|
|
| Smoking index
(pcs/year) |
|
|
| 7.658 | 0.029 |
|
<400 | 32
(14.9%) | 85.5% | 79.4% |
|
|
| ≥400,
<800 | 101 (47.0%) | 72.0% | 53.5% |
|
|
| ≥800 | 82
(38.1%) | 64.6% | 43.6% |
|
|
| Primary tumor
site |
|
|
| 19.587 | >0.05 |
|
Supraglottic type | 95
(44.2%) | 89.5% | 72.6% |
|
|
| Glottic
type | 72
(33.5%) | 88.9% | 58.3% |
|
|
|
Subglottic type | 48
(22.3%) | 70.8% | 22.9% |
|
|
| Tumor differentiation
degree |
|
|
| 18.594 | 0.002 |
| High
differentiation | 78
(36.3%) | 88.5% | 81.2% |
|
|
| Moderate
differentiation | 86
(40.0%) | 75.6% | 67.5% |
|
|
| Poor
differentiation | 51
(23.7%) | 45.1% | 43.7% |
|
|
| T stage |
|
|
| 17.613 | 0.013 |
| T1 | 48
(22.3%) | 91.7% | 88.4% |
|
|
| T2 | 56
(26.0%) | 82.1% | 79.6% |
|
|
| T3 | 68
(31.6%) | 61.8% | 42.1% |
|
|
| T4 | 43
(20.0%) | 60.5% | 40.7% |
|
|
| N stage |
|
|
| 19.142 | >0.05 |
| N0 | 101 (47.0%) | 87.1% | 76.5% |
|
|
| N1 | 63
(29.3%) | 58.7% | 49.4% |
|
|
| N2 | 51
(23.7%) | 45.1% | 31.0% |
|
|
| Drinking |
|
|
| 1.505 | 0.220 |
| Never or
occasionally | 81
(37.7%) | 82.7% | 75.9% |
|
|
|
Often | 134 (62.3%) | 73.1% | 65.7% |
|
|
| Tumor diameter
(cm) |
|
|
| 19.783 | >0.05 |
| ≤2 | 106 (49.3%) | 82.1% | 76.1% |
|
|
| >2,
≤4 | 68
(31.6%) | 77.9% | 49.8% |
|
|
|
>4 | 41
(19.1%) | 70.7% | 35.7% |
|
|
| Surgical method |
|
|
| 6.121 | 0.059 |
| Total
laryngectomy | 148 (68.8%) | 84.5% | 60.9% |
|
|
| Partial
laryngectomy | 67
(31.2%) | 76.1% | 68.4% |
|
|
| Lymph node
metastasis |
|
|
| 25.105 | >0.05 |
|
Positive | 46
(21.4%) | 68.8% | 24.5% |
|
|
|
Negative | 169 (78.6%) | 95.3% | 79.6% |
|
|
| Cervical lymph node
dissection |
|
|
| 3.172 | 0.17 |
| No | 71
(33.0%) | 75.9% | 58.5% |
|
|
|
Functional | 63
(29.3%) | 85.7% | 64.9% |
|
|
|
Radical | 81
(37.7%) | 93.8% | 76.8% |
|
|
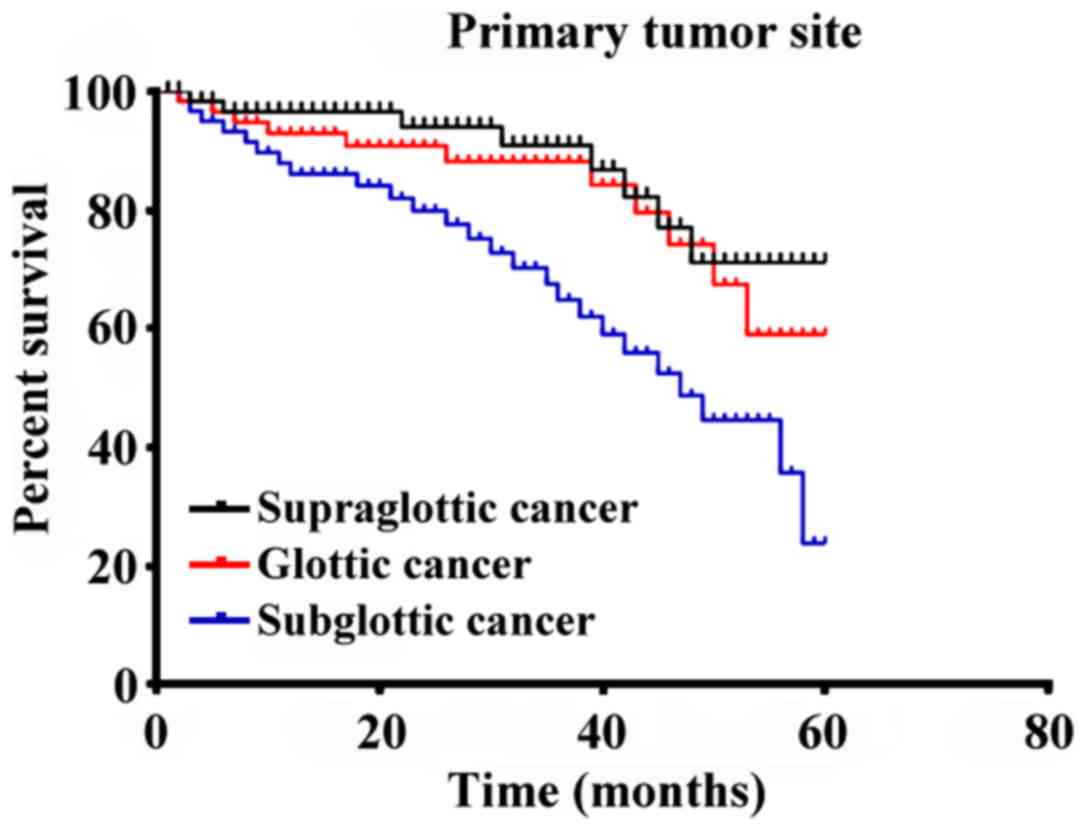
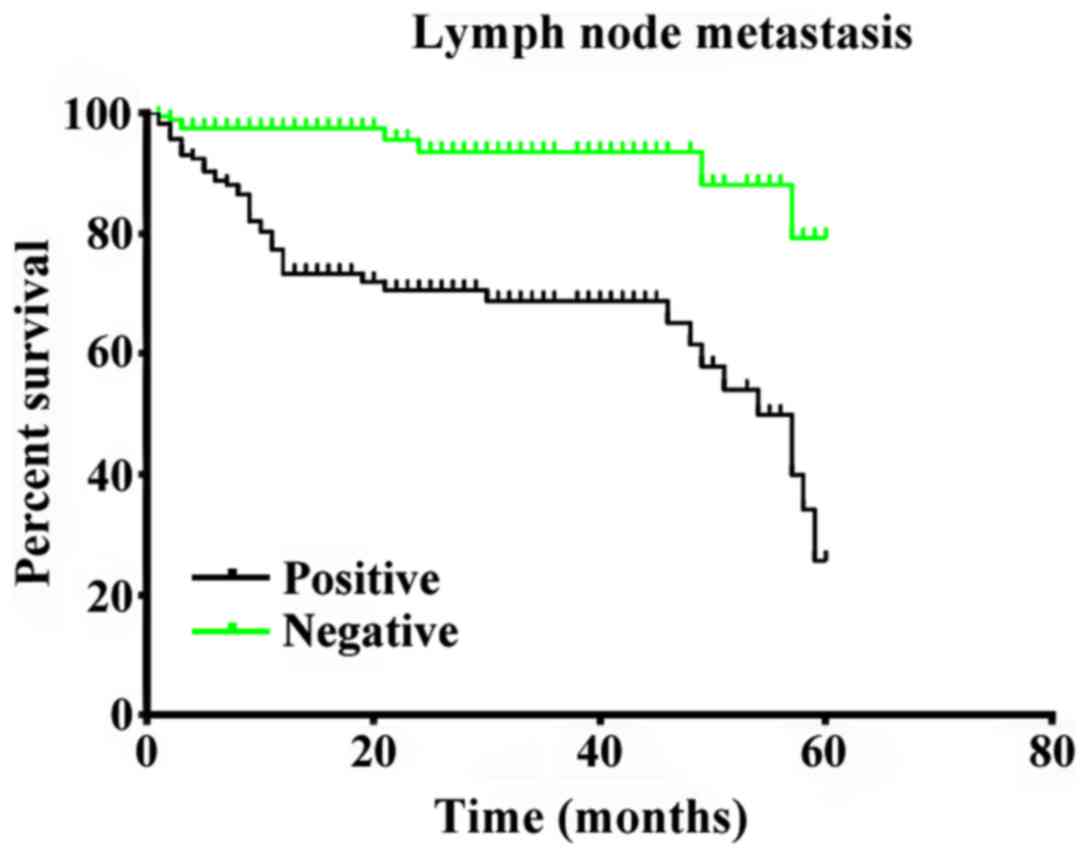
Multiple-factor analysis of surgical
effect on patients with laryngeal cancer
Cox proportional hazard regression model was used
for multiple-factor analysis with the age, primary tumor site,
tumor differentiation degree, T stage, N stage, smoking index,
tumor diameter and lymph node metastasis in the single-factor
analysis were included, and the results showed that the primary
tumor site, T stage, N stage and lymph node metastasis were the
independent risk factors affecting the surgical effect on patients
with laryngeal cancer (P<0.05) (Table II). In order to show the difference
in survival rate among the four independent prognostic factors, the
survival curves were drawn (Figs.
2–5).
 | Table II.Multiple-factor analysis of surgical
effect on 215 patients with laryngeal cancer. |
Table II.
Multiple-factor analysis of surgical
effect on 215 patients with laryngeal cancer.
| Influencing
factor | β value | SE | Wald | P-value | Hazard ratio
(HR) | 95% confidence
interval (CI) |
|---|
| Primary tumor
site | 1.315 | 0.368 | 10.526 | 0.001 | 3.618 | 1.592–7.925 |
| T stage | 1.259 | 0.540 | 5.426 | 0.019 | 3.522 |
1.221–10.159 |
| N stage | 0.699 | 0.321 | 3.200 | 0.040 | 2.012 | 1.031–3.926 |
| Lymph node
metastasis | 1.152 | 0.358 | 4.125 | 0.028 | 2.916 | 1.151–4.581 |
Discussion
Laryngeal cancer is one of the common malignant
tumors in the head and neck, and its incidence rate still shows an
upward trend. Although progress has been made constantly in the
clinical comprehensive treatment, surgery, biotherapy and genetic
research, and the diagnosis and treatment of patients with
laryngeal cancer are improved, its survival rate shows a downward
trend (6); therefore, the
understanding of factors affecting the prognosis of patients, and
appropriate prognosis estimation and clinical treatment are of
great significance in improving the survival rate of patients with
laryngeal cancer. Compared with other studies, the subjects were
selected in this study in strict accordance with the inclusion and
exclusion criteria for seven years, thus ensuring the credibility
of results.
The results of single-factor analysis showed that
the age was an important factor affecting the patient's
postoperative efficacy. This study revealed that the survival rate
was 35.2% in patients with laryngeal cancer aged over 57 years and
73.0% in patients aged 57 years and below. The poorer prognosis in
elderly patients than that in middle-aged patients may be caused by
the following factors: the human natural resistance and the
function of various organs are weakened with age; the failure of
various organs lead to other types of disease and increase the
mortality rate; after surgery and a series of treatment, the body
function of the elderly patients is damaged, and the absorption and
recovery rates are slow.
Swisher-McClure et al (7) reported that the body function declines
with the age in patients with laryngeal cancer, resulting in poorer
prognosis than those in the middle-aged patients than those in the
middle-aged patients, and it is a potential risk factor of poor
prognosis. The sex has no significant correlation with the
postoperative efficacy on patients, the middle-aged men are
dominant in patients with laryngeal cancer, and the incidence rate
of laryngeal cancer in men is much higher than that in women, which
is consistent with our research (203 male patients and 12 female
patients, 17:1). The study of Guo et al (8) showed that the sex is one of the
important factors affecting the prognosis of laryngeal cancer, but
there was no significant correlation between sex and prognosis of
laryngeal cancer in this study, and the specific influencing
mechanism needs to be further explored. The smoking index is also
associated with the postoperative efficacy on patients. The smoke
in tobacco and tobacco burning contains many carcinogenic
substances, and smoking has always been recognized as the most
important risk factor of lung cancer (9). In the single-factor analysis, smoking
also had a statistically significant effect on the postoperative
efficacy on patients with laryngeal cancer.
The study of Kim et al (10) showed that the survival rate of
smokers with laryngeal cancer is only one third of that of
non-smokers, so smoking is an important factor affecting the
prognosis of patients. In this study, both single-factor analysis
and multiple-factor analysis revealed that the primary tumor site,
T stage, N stage and lymph node metastasis were independent risk
factors for the prognosis of patients with laryngeal cancer. Our
data showed that the prognosis of patients with supraglottic cancer
was superior to that of patients with glottic cancer and subglottic
cancer; however, de Miguel-Luken et al (11) stated that the prognosis of patients
with glottic cancer is better than that of patients with
supraglottic cancer, because there are rich lymphatic vessels above
the vocal cords, and lymphatic metastasis occurs easily in the
tumor in this site with high occult metastasis (12). It is thought that the early symptoms
of supraglottic cancer can affect the throat and pharynx, and
patients will seek medical treatment once uncomfortable, which has
no significant correlation with its prognosis (P>0.05); the
different conclusions need further study.
It is believed that the higher the T stage and N
stage are, the lower the survival rate of patients will be. The
higher T stage indicates larger tumor size and involved range,
increased lymph node metastasis rate, more damaged sites, difficult
combined cure and decreased survival rate. However, Han and Ge
(13) reported that the higher T
stage decreases the survival rate of patients with laryngeal
cancer, but it is not an independent influencing factor of
prognosis. The N stage represents the lymph node metastasis staging
of tumor, and the survival rate of patients with lymph node
metastasis-positive laryngeal cancer is significantly lower than
that of patients with lymph node metastasis-negative laryngeal
cancer; moreover, the higher the N stage is, the lower the survival
rate will be. The higher the tumor differentiation degree is, the
malignant degree will be, reducing the survival rate of patients.
Besides, the tumor diameter can reflect the tumor development time
and deterioration degree indirectly, which has a significant impact
on the survival rate of patients.
The study of Liu et al (14) came to the same conclusion as our
study. In this study, the treatment method was not an influencing
factor of prognosis, which was different from the conclusion made
by Zhang et al (15), maybe
because the different types of patients affect the experimental
results. Zhang et al (15)
thought that the correct treatment method is important for the
recurrence of laryngeal cancer, the survival rate of patients
receiving comprehensive treatment is higher than that of patients
receiving simple surgical treatment, and the tumor can be radically
cured via the combined application of radiotherapy and chemotherapy
after surgical resection, greatly increasing the survival rate of
patients.
In the latest study, the research on the
pathogenesis and prognosis of laryngeal cancer has been developed
to the levels of gene and blood type. Choe et al (16) reported that the STAT3 gene expression
in laryngeal cancer cells is related to the prognosis of patients.
Jin et al (17) considered
that the ABO blood type can predict the survival rate of patients
with laryngeal cancer, and the survival rate of patients with O
blood type is lower than that with other types. Moreover, Dang
et al (18) argued that
mitochondrial DNA (mtDNA) can predict the prognosis of patients
with early laryngeal cancer. These cutting-edge research directions
may guide the researchers to obtain different diagnosis and quality
treatment methods of laryngeal cancer.
In conclusion, we believe that the age, primary
tumor site, tumor differentiation degree, T stage, N stage, smoking
index, tumor diameter and lymph node metastasis are the factors
affecting the surgical treatment effect on patients with laryngeal
cancer. The independent factors affecting the prognosis of patients
with laryngeal cancer are the primary tumor site, T stage, N stage
and lymph node metastasis. Patients with laryngeal cancer should be
diagnosed and treated in time, the laryngeal function should be
retained as far as possible in the case of complete resection of
tumor, and the surgical treatment should be combined with other
treatment means, so as to improve the survival rate of patients
with laryngeal cancer.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yu X and Li Z: The role of microRNAs
expression in laryngeal cancer. Oncotarget. 6:23297–23305. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Du L, Li H, Zhu C, Zheng R, Zhang S and
Chen W: Incidence and mortality of laryngeal cancer in China, 2011.
Chin J Cancer Res. 27:52–58. 2015.PubMed/NCBI
|
|
3
|
Li X, Wang H, Lu X and Di B: STAT3
blockade with shRNA enhances radiosensitivity in Hep-2 human
laryngeal squamous carcinoma cells. Oncol Rep. 23:345–353.
2010.PubMed/NCBI
|
|
4
|
Kim JS, Chang JW, Park JK and Hwang SG:
Increased aldehyde reductase expression mediates acquired
radioresistance of laryngeal cancer cells via modulating p53.
Cancer Biol Ther. 13:638–646. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Min JW, Kim KI, Kim HA, Kim EK, Noh WC,
Jeon HB, Cho DH, Oh JS, Park IC, Hwang SG, et al: INPP4B-mediated
tumor resistance is associated with modulation of glucose
metabolism via hexokinase 2 regulation in laryngeal cancer cells.
Biochem Biophys Res Commun. 440:137–142. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Oancea AL, Popescu CR and Bordei P:
Anatomo-surgical correlations in larynx cancer. J Med Life.
5:198–202. 2012.PubMed/NCBI
|
|
7
|
Swisher-McClure S, Mitra N, Lin A, Ahn P,
Wan F, O'Malley B, Weinstein GS and Bekelman JE: Risk of fatal
cerebrovascular accidents after external beam radiation therapy for
early-stage glottic laryngeal cancer. Head Neck. 36:611–616. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guo W, Yang D, Xu H, Zhang Y, Huang J,
Yang Z, Chen X and Huang Z: Mutations in the D-loop region and
increased copy number of mitochondrial DNA in human laryngeal
squamous cell carcinoma. Mol Biol Rep. 40:13–20. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
He FY, Liu HJ, Guo Q and Sheng JL: Reduced
miR-300 expression predicts poor prognosis in patients with
laryngeal squamous cell carcinoma. Eur Rev Med Pharmacol Sci.
21:760–764. 2017.PubMed/NCBI
|
|
10
|
Kim JS, Kim SY, Lee M, Kim SH, Kim SM and
Kim EJ: Radioresistance in a human laryngeal squamous cell
carcinoma cell line is associated with DNA methylation changes and
topoisomerase II α. Cancer Biol Ther. 16:558–566. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
de Miguel-Luken MJ, Chaves-Conde M and
Carnero A: A genetic view of laryngeal cancer heterogeneity. Cell
Cycle. 15:1202–1212. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
de Miguel-Luken MJ, Chaves-Conde M, de
Miguel-Luken V, Muñoz-Galván S, López-Guerra JL, Mateos JC, Pachón
J, Chinchón D, Suarez V and Carnero A: MAP17 (PDZKIP1) as a novel
prognostic biomarker for laryngeal cancer. Oncotarget.
6:12625–12636. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Han CD and Ge WS: Up-regulation of
angiotensin-converting enzyme (ace) enhances cell proliferation and
predicts poor prognosis in laryngeal cancer. Med Sci Monit.
22:4132–4138. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu RR, Li MD, Li T, Tan Y, Zhang M and
Chen JC: Matrix metalloproteinase 2 (MMP2) protein expression and
laryngeal cancer prognosis: A meta analysis. Int J Clin Exp Med.
8:2261–2266. 2015.PubMed/NCBI
|
|
15
|
Zhang C, Guan Z and Peng J: The
correlation between stanniocalcin 2 expression and prognosis in
laryngeal squamous cell cancer. Lin Chung Er Bi Yan Hou Tou Jing
Wai Ke Za Zhi. 29:102–107. 2015.(In Chinese). PubMed/NCBI
|
|
16
|
Choe MH, Min JW, Jeon HB, Cho DH, Oh JS,
Lee HG, Hwang SG, An S, Han YH and Kim JS: ERp57 modulates STAT3
activity in radioresistant laryngeal cancer cells and serves as a
prognostic marker for laryngeal cancer. Oncotarget. 6:2654–2666.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jin T, Li PJ, Chen XZ and Hu WH: ABO blood
group is a predictor of survival in patients with laryngeal cancer.
Chin J Cancer. 35:902016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dang S, Qu Y, Wei J, Shao Y, Yang Q, Ji M,
Shi B and Hou P: Low copy number of mitochondrial DNA (mtDNA)
predicts worse prognosis in early-stage laryngeal cancer patients.
Diagn Pathol. 9:282014. View Article : Google Scholar : PubMed/NCBI
|