Introduction
Associating liver partition and portal vein ligation
for staged hepatectomy (ALPPS) is a novel strategy for liver
resection that was originally established in 2007 by the German
surgeon Hans Schlitt (1,2), and was first reported in 2012 by
Schnitzbauer et al (3). The
original method utilizing laparotomy surgery has been improved by a
completely laparoscopic surgery (4).
However, the potential postoperative complications and mortality
subsequent to ALPPS remains high, and limited long-term follow-up
data exists to date. The most common postoperative complications of
ALPPS include biliary fistula (10.2–24%) and infection (7.7–20%)
(5). To the best of our knowledge,
postoperative acute kidney injury following ALPPS in patients with
posthepatitic cirrhosis has not yet been reported.
The present study reported the case of a patient
with hepatitis B-induced cirrhosis who experienced postoperative
acute kidney injury after the first stage of the ALPPS procedure.
The current case report aimed to analyze the potential causes of
this complication and suggests measures that can be employed in
clinical practice to prevent postoperative acute kidney injury,
thereby improving the patient outcome.
Case report
In May 2015, a 63-year-old man was admitted to the
Department of Hepatobiliary Surgery at the First Hospital of Jilin
University (Changchun, China), because of abdominal pain and
faintness for 2 months. The patient provided informed consent for
selective surgery, and the protocol was approved by the
Institutional Review Board of our hospital. The patient's medical
history revealed that he suffered from chronic hepatitis B for
>30 years, diabetes for 7 years (with regular injection of
insulin; fasting blood-glucose was controlled under ~7.3 mmol/l),
and hypertension for 10 years (blood pressure, 150/90 mmHg). There
were no positive signs of kidney disease, with blood levels of
creatinine of 60.6 µmol/l (normal range, 41–73 µmol/l) and
glomerular filtration rate of 95 ml/min (normal range, 80–120
ml/min) during the physical examination.
Computed tomography examination (Fig. 1A and B) displayed multiple low
density nodules of 0.8–6.8 cm in diameter in the anterior segment
of the right lobe of the cirrhotic liver, which presented
significantly heterogeneous enhancement at the arterial phase and
washout in the portal venous and delayed phases. In addition,
ultrasonography (Fig. 1C) revealed a
large solid tumor in the right lobe of the liver, with a size of
7.0×5.8 cm.
Various laboratory tests were also performed. The
results of the liver function test were as follows: Elevated
aspartate aminotransferase, 118.0 U/l (normal range, 0–31 U/l);
elevated alanine aminotransferase, 156.1 U/l (normal range, 0–32
U/l); elevated γ-glutamyl transpeptidase, 75.9 U/l (normal range,
7–45 U/l); elevated total bilirubin, 30.4 µmol/l (normal range,
<17.1 µmol/l); and elevated indirect bilirubin, 22.2 µmol/l
(normal range, 0–15 µmol/l). In addition, the renal function
examination demonstrated normal blood urea nitrogen (BUN) at 2.93
mmol/l (normal range, 2.86–7.14 µmol/l) and normal creatinine level
at 60.6 µmol/l (normal range, 41–73 µmol/l). A routine urine
culture was negative for urine protein. Hepatitis B virus (HBV)
quantitative test revealed an elevated level of 5.4×107
IU/ml (normal range, <500 IU/ml), while the serum
alphafetoprotein level was elevated at 25.34 ng/ml (normal range,
0.89–8.78 ng/ml) and carbohydrate antigen was elevated at 19,978.97
U/ml (normal range, 0–6.9 U/ml). The indocyanine green retention
rate at 15 min was normal at 8.4% (normal range, <10%).
Furthermore, the preoperative liver volume measurements indicated
that the volume of the left lobe in the liver was 520 ml, the
volume of the left external lobe in the liver was 300 ml and the
standard liver volume (SLV) was 1,420 ml. These results indicated a
dysfunction of the liver.
The preoperative clinical diagnosis was primary
liver cancer with decompensated hepatitis B-induced cirrhosis.
Entecavir (0.5 mg/day; Sino American Shanghai Squibb
Pharmaceuticals Ltd., Shanghai, China) was administered for
antiviral treatment following admission. Blood glucose levels under
fasting conditions and subsequent to meals were monitored, and the
dose of insulin was adjusted accordingly. As the nodules were
predominately located in the right lobe of the liver and closely
connected to the middle and right hepatic veins, right
hemihepatectomy or right hepatictrisegmentectomy was required to
achieve an R0 resection in the patient. However, as the patient
suffered from hepatitis B-induced cirrhosis, for which the
postoperative future liver remnant size would be <40% of the SLV
(5) and he could not tolerate
one-stage complete resection of the tumor, laparoscopic ALPPS was
selected.
Intraoperative probe examination detected moderate
cirrhosis of the liver with a firm, pale mass with a diameter of 7
cm in the right anterior lobe, which was closely connected to the
middle and right hepatic veins. In addition, there were several
nodules of 0.5–1.5 cm in diameter in the right posterior lobe and
left internal lobe, while another 0.8-cm nodule was located on the
surface of the left external lobe of the liver. These lesions are
typically observed in patients with primary liver cancer. ALPPS was
performed (6), during which the
lesion that was 1.5 cm in diameter in the left external lobe of the
liver was locally resected. The right branch of the hepatic vein
and the right hepatic artery were ligated, and preset lines were
identified for the secondary surgery. Postoperative pathology
confirmed the diagnosis of primary hepatocellular carcinoma (HCC)
with moderate differentiation.
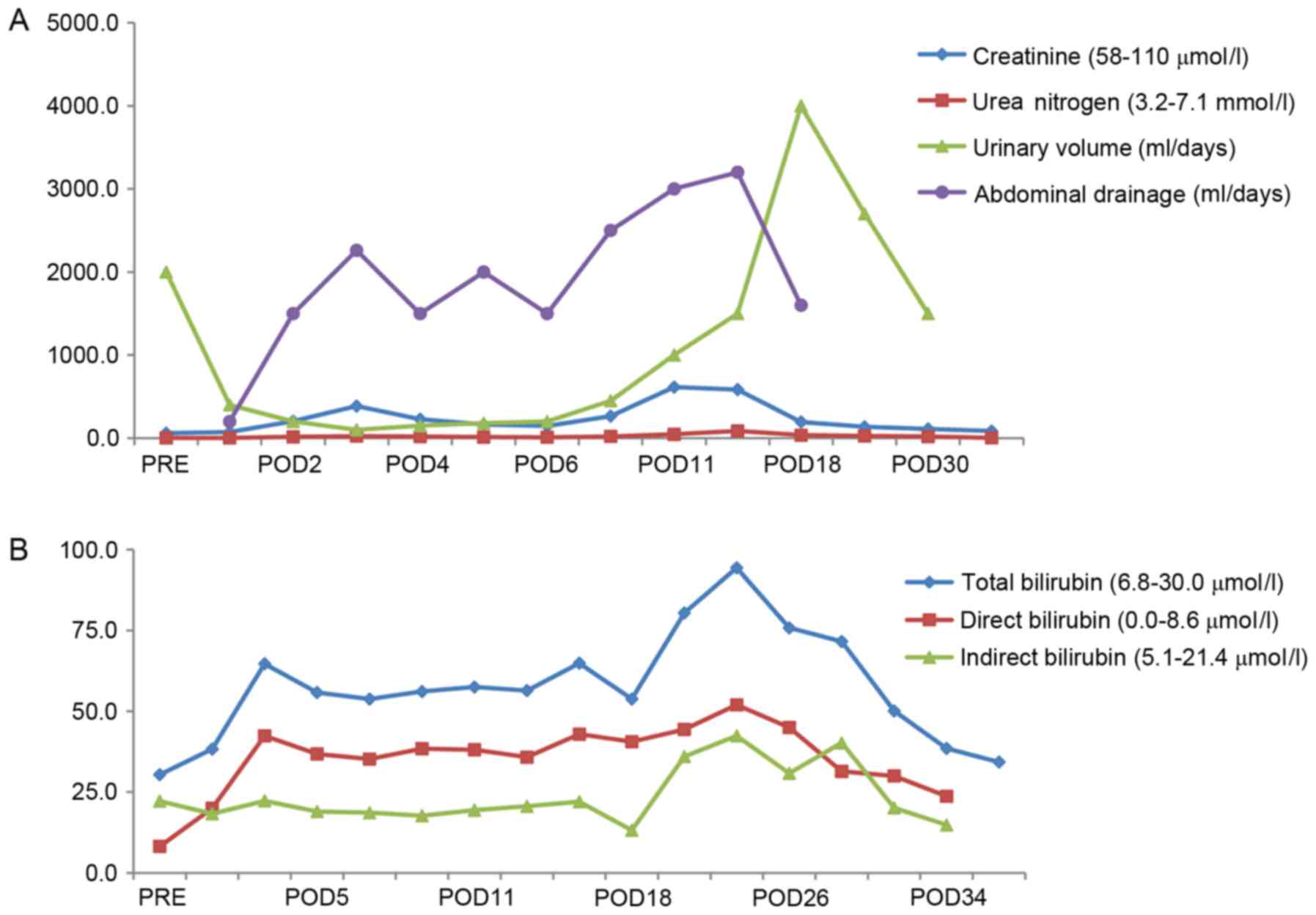
Postoperatively, the patient's urine output
gradually decreased from the first day following surgery, with
blood levels of creatinine and BUN continuously increasing. On the
third day following ALPPS, the levels of creatinine and BUN in the
patient's blood were elevated, at 386.4 µmol/l (normal range, 41–73
µmol/l) and 24.58 mmol/l (normal range, 2.86–7.14 mmol/l),
respectively, which are considerably higher than the normal values.
All these tests (urine output, creatinine and BUN) indicated a
decline in kidney function, and therefore, the patient was
diagnosed with postoperative acute kidney injury, according to the
evaluation criteria for acute kidney injury from the Acute Kidney
Injury Work Group (7). Thus, the
patient was treated with continuous dialysis for 3 days, beginning
on postoperative day 3, resulting in improvement in the renal
function. However, higher blood levels of creatinine (707.9 µmol/l)
and BUN (81.9 mmol/l) were detected in the patient when dialysis
was stopped, while even volume expansion and fluid supplement
therapy failed to decrease these levels. The patient was
recommenced on dialysis for 2 days, beginning on postoperative day
16, and the levels of creatinine and BUN decreased to 136.4 µmol/l
(normal range, 41–73 µmol/l) and 26.44 mmol/l (normal range,
2.86–7.14 mmol/l), respectively (Fig.
2). Subsequent to symptomatic treatments, such as liver and
kidney protection and fluid therapy (reduced glutathione, 1,200
mg/day, i.v.; magnesium isoglycyrrhizinate, 100 mg/day, i.v.;
spironolactone, 60 mg/day, orally administered), renal function
improved and the 24-h urine volume gradually returned to normal.
Other complications were also observed, such as refractory ascites
and bacterial peritonitis, although the symptoms of peritonitis
were gradually improved after abdominal drainage, hemofiltration
and administration of antibiotics (vancomycin, 2 g/day, i.v.)
effective against Enterococcus faecium. However, the patient
refused further treatment due to financial reasons, and selected to
be discharged from hospital care.
The patient attended scheduled follow-up
appointments until October 2015. The final results of the liver
function test were as follows: Aspartate aminotransferase, 200.0
U/l (normal range, 0–31 U/l); alanine aminotransferase, 250.5 U/l
(normal range, 0–32 U/l); γ-glutamyl transpeptidase, 100 U/l
(normal range, 7–45 U/l); total bilirubin, 120.6 µmol/l (normal
range, <17.1 µmol/l); and indirect bilirubin, 80.3 µmol/l
(normal range, 0–15 µmol/l). In addition, the renal function
examination demonstrated BUN at 30.23 mmol/l (normal range,
2.86–7.14 µmol/l) and creatinine level at 180.6 µmol/l (normal
range, 41–73 µmol/l). As the patient only underwent the first stage
of the ALPSS procedure, the liver tumor was still present. Liver
and kidney function appeared to be worse than when he was first
admitted.
Discussion
Patients with multiple intrahepatic tumors or a
large liver tumor, regardless of the functional residual liver
volume, are usually treated with liver resection. However, concerns
have been raised regarding the small liver remnants and the
development of postoperative complications in these patients
(2). Portal vein embolization
(7) and portal vein ligation
(8,9)
are two conventional techniques, which are widely used prior to
liver resection to maintain sufficient liver volumes following
surgery. Recently, ALPPS has emerged as a novel procedure to
rapidly increase the residual liver volume with a 74–99% increase
in the remnant liver in the short term (9 days). In addition, the
ALPPS technique meets the safe liver resection criteria (3), while it reduces the surgery duration
and the incidence of postoperative hepatic failure. As of September
2015, 553 patients were registered as having undergone ALPSS from
84 medical centers worldwide (www.alpps.net)
(10). However, ALPPS has certain
limitations, including high morbidity and mortality rates, and
postoperative complications. In the present case report, a patient
who underwent the first stage of the ALPSS procedure without
completion of the second stage was reported. The patient
experienced acute kidney injury following ALPPS, a rare
postoperative complication.
To date, a limited number of published case reports
exist on postoperative complications following ALPPS, and acute
kidney injury has not previously been reported as a postoperative
complication of ALPPS. Therefore, there is no predictive guidlines
that can be followed in order to avoid postoperative renal damage
following ALPPS. Schadde et al (10) analyzed the early postoperative
survival rates and safety of the procedure in 202 registered ALPPS
patients. In their report, the independent risk factors associated
with postoperative complications were as follows: Intraoperative
erythrocyte transfusion, surgery duration of the first stage ALPPS
of >300 min, patient age of >60 years, and liver metastasis
other than colorectal liver metastasis. In the present case study,
the patient was 63 years old with a history of hypertension and
diabetes, which are known to induce chronic renal damage. The
patient was, therefore, at risk of acute kidney injury (10). Furthermore, the long surgery duration
of ~380 min during the first stage of ALPPS, along with the adverse
effects of anesthesia and surgical stress on renal function
possibly increased the risk and contributed to the development of
acute kidney injury. Of patients undergoing the ALPPS procedure,
70% of cases presented liver metastasis from colorectal cancer,
~17% of patients presented primary liver cancer (2,10,11), and
a small number of patients had liver cancer secondary to
hepatitis-induced cirrhosis. The latter group of patients are more
likely to suffer with viral nephropathy and are at a high risk of
postoperative acute kidney injury.
Suggestions of the present study for measures that
can be performed in clinical practice in order to reduce the risk
of postoperative acute renal injury and improve patient outcomes
also merit attention. Firstly, when the postoperative urine volume
or renal function are decreased, an insufficient circulating blood
volume should be considered. Therefore, the first step is to
replenish the circulating volume, and subsequent diuretics should
increase the daily urine output with an adequate fluid intake.
Secondly, if patients are diagnosed with HBV infection, antiviral
drug therapy should be used prior to liver resection (12) in order to avoid impairment in kidney
function caused by HBV infection. Antibiotics with less adverse
effects on renal function should be selected when spontaneous
bacterial peritonitis occurs. Abdominal drainage should be
performed if refractory ascites are suspected. Finally, if no
improvement in renal function is reported or the patient develops
metabolic acidosis and severe hyperkalemia, then renal replacement
therapy should be considered to remove toxins (13). Hemofiltration therapy can also help
to restore liver function. In the present study, the hepatic
function of the patient was improved subsequent to the second
hemofiltration treatment. Overall, when renal insufficiency occurs
following ALPPS, the patient should be treated as soon as possible
to avoid further deterioration of potential acute kidney injury or
failure.
In conclusion, the use of ALPPS in patients at risk
of chronic renal damage should be carefully considered in order to
avoid the development of postoperative acute kidney injury
following ALPPS. Furthermore, improvement in surgical techniques
and skills are required to reduce the surgical duration and improve
the clinical outcomes of patients.
References
|
1
|
de Santibañes E and Clavien PA: Playing
Play-Doh to prevent postoperative liver failure: The ‘ALPPS’
approach. Ann Surg. 255:415–417. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bertens KA, Hawel J, Lung K, Buac S,
Pineda-Solis K and Hernandez-Alejandro R: ALPPS: Challenging the
concept of unresectability-a systematic review. Int J Surg.
13:280–287. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schnitzbauer AA, Lang SA, Goessmann H,
Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T,
Goralcyk A, Hörbelt R, et al: Right portal vein ligation combined
with in situ splitting induces rapid left lateral liver lobe
hypertrophy enabling 2-staged extended right hepatic resection in
small-for-size settings. Ann Surg. 255:405–414. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Machado MA, Makdissi FF and Surjan RC:
Totally laparoscopic ALPPS is feasible and may be worthwhile. Ann
Surg. 256:e13; author reply e16–e19. 2012. View Article : Google Scholar
|
|
5
|
Zhang GQ, Zhang ZW, Lau WY and Chen XP:
Associating liver partition and portal vein ligation for staged
hepatectomy (ALPPS): A new strategy to increase resectability in
liver surgery. Int J Surg. 12:437–441. 2014. View Article : Google Scholar
|
|
6
|
Torres OJ, Fernandes Ede S, Oliveira CV,
Lima CX, Waechter FL, Moraes-Junior JM, Linhares MM, Pinto RD,
Herman P and Machado MA: Associating liver partition and portal
vein ligation for staged hepatectomy (ALPPS): The Brazilian
experience. Arq Bras Cir Dig. 26:40–43. 2013.(In English,
Portuguese). View Article : Google Scholar
|
|
7
|
Kidney Disease Improving Global Outcomes
(KDIGO) Acute Kidney Injury Work Group, . KDIGO clinical practice
guideline for acute kidney injury. Kidney Inter. 2 Suppl:1–138.
2012.
|
|
8
|
Clavien PA, Petrowsky H, DeOliveira ML and
Graf R: Strategies for safer liver surgery and partial liver
transplantation. N Engl J Med. 356:1545–1559. 2007. View Article : Google Scholar
|
|
9
|
Kianmanesh R, Farges O, Abdalla EK,
Sauvanet A, Ruszniewski P and Belghiti J: Right portal vein
ligation: A new planned two-step all-surgical approach for complete
resection of primary gastrointestinal tumors with multiple
bilateral liver metastases. J Am Coll Surg. 197:164–170. 2003.
View Article : Google Scholar
|
|
10
|
Schadde E, Ardiles V, Robles-Campos R,
Malago M, Machado M, Hernandez-Alejandro R, Soubrane O,
Schnitzbauer AA, Raptis D, Tschuor C, et al: Early survival and
safety of ALPPS: First report of the international ALPPS registry.
Ann Surg. 260:829–836; discussion 836–838. 2014. View Article : Google Scholar
|
|
11
|
Correa-Gallego C, Berman A, Denis SC,
Langdon-Embry L, O'Connor D, Arslan-Carlon V, Kingham TP,
D'Angelica MI, Allen PJ, Fong Y, et al: Renal function after low
central venous pressure-assisted liver resection: Assessment of
2116 cases. HPB (Oxford). 17:258–264. 2015. View Article : Google Scholar
|
|
12
|
Zhang B, Xu D, Wang R, Zhu P, Mei B, Wei
G, Xiao H, Zhang B and Chen X: Perioperative antiviral therapy
improves safety in patients with hepatitis B related HCC following
hepatectomy. Int J Surg. 15:1–5. 2015. View Article : Google Scholar
|
|
13
|
Sourianarayanane A, Raina R, Garg G,
McCullough AJ and O'Shea RS: Management and outcome in hepatorenal
syndrome: Need for renal replacement therapy in non-transplanted
patients. Int Urol Nephrol. 46:793–800. 2014. View Article : Google Scholar
|