Introduction
In recent years, with the rapid development of
social economy in China, the incidence rate of finger disability
due to a variety of reasons has shown an increasing trend,
seriously affecting the patient's labor ability and normal life,
and increasing economic and psychological pressure on patients and
their families (1). At present, the
clinical treatment method of finger disability is mainly the early
replantation, and with the progress and improvement of clinical
micro-technique level, the survival rate of replanted finger has
been significantly improved. Studies have found that the key to
successful severed finger replantation is the connection of blood
vessels. However, there is no appropriate venous anastomosis in the
severed finger of patients with distal severed finger without
venous anastomosis, so the survival rate after severed finger
replantation is lower, and patients are prone to vascular crisis
after operation (2). Unilateral
digital arterial ligation, as a new surgical method, can
effectively improve the survival rate of severed finger without
venous anastomosis, but its specific mechanism of treatment is not
fully clear yet in clinical medicine, and needs further study
(3). Low-molecular weight heparin,
as a kind of common anticoagulant, can prevent and treat venous
thrombosis, and has been widely used in clinical treatment
(4). On this basis, the severed
finger without venous anastomosis was treated with unilateral
digital arterial ligation combined with low molecular weight
heparin in this study, and its clinical effect and influence on
venous crisis were analyzed.
Patients and methods
Inclusion criteria
i) Patients diagnosed as severed finger without
venous anastomosis via clinical examination; the severed finger
refers to the abruption of arterial arch from the distal severed
interphalangeal joint to the digital arterial arch; ii) patients
without coagulation dysfunction; iii) patients without drug allergy
history or allergic constitution; iv) patients without malignant
tumor, nervous system diseases or endocrine system diseases
(5); v) this study was approved by
Ethics Committee of Wuxi No. 9 People's Hospital (Jiangsu, China);
vi) all patients and their families were informed of this study,
and signed the informed consent.
Exclusion criteria
i) Patients with severe organ diseases in heart,
liver or kidney (6); ii) pregnant or
lactating women; iii) patients allergic to anesthesia and low
molecular weight heparin or who could not tolerate operation; and
iv) patients who did not participate voluntarily.
Demographic data
A total of 80 patients with distal severed finger
(98 fingers) treated in our hospital from May 2014 to July 2016
were selected as the subjects of study and they all conformed to
the inclusion criteria. According to the random number table, they
were divided into control group (n=40) and research group (n=40).
In control group, there were 22 males (25 fingers) and 18 females
(23 fingers) aged 20–60 years with an average age of 35.4±5.5
years. In terms of injury cause, there were 4 cases of machine
cutting injury, 19 cases of saw injury and 17 cases of machine
run-over injury. In research group, there were 24 males (28
fingers) and 16 females (22 fingers) aged 20–60 years with an
average age of 35.9±4.7 years. In terms of injury cause, there were
5 cases of machine cutting injury, 20 cases of saw injury and 15
cases of machine run-over injury. There were no statistically
significant differences in the basic data between the two groups
(p>0.05), and the data were comparable.
Surgical procedures
Patients in both groups were treated with unilateral
digital arterial ligation. Under the local infiltration anesthesia
or brachial plexus block anesthesia, the operation was performed
with hemostasis by compression using the pneumatic tourniquet on
upper arm or rubber strip at the root of the finger. After the
conventional cleaning of injured hand and severed fingers, the free
necrotic tissue and foreign bodies on the two cross sections were
carefully removed, followed by routine disinfection with 0.1%
povidone iodine disinfectant and draping. The operator protected
the nerves and blood vessels carefully under the microscope,
completely removed the necrotic tissue and checked the proximal
severed end. Moreover, the digital arteries and severed nerve ends
were observed and marked, followed by the bandage and release of
the tourniquet. After that, the distal severed end was checked
using the same method, but no anastomotic vein could be detected;
the digital arteries and severed nerve ends were also observed and
marked. According to the vascular conditions, if necessary, the
finger bone was appropriately shortened, the marrow cavity was
penetrated using the Kirschner wire and the severed end was fixed.
In the absence of tension, the tendon, nerves and blood vessels
were anastomosed, and the wound was sutured. At the same time, the
tourniquet and rubber strip at the root of finger were released,
and the replanted finger became ruddy slowly. After the unilateral
digital arterial ligation in the proximal end of replanted finger
and wound dressing, the functional position of injured hand was
fixed with plaster support. After operation, patients in the two
groups received the anti-coagulation, anti-infection, anti-spasm
and other symptomatic treatment. If the patient suffered from be
finger darkening and swelling, cyanosis and venous return
obstruction, the nails should be removed, and a longitudinal
incision on nail bed and a side incision on fingertip were made to
discharge appropriate amount of blood. The patients in the research
group were injected subcutaneously with 0.4 ml low molecular weight
heparin (NMPN H20060191; Shenzhen Saibaoer Biopharmaceutical Co.,
Ltd., Shenzhen, China) 1 time/12 h for consecutive 3 days. Patients
in the two groups were followed up for 6 months after
operation.
Observation indexes
The wound healing time after operation,
hospitalization time and hemorheology detection results were
observed and compared between the two groups. The temperature of
fingertip, the fullness of finger pulp, skin color and capillary
response of patients were observed at 7 days after operation, thus
determining the survival rate and necrosis rate of replanted finger
and incidence rate of venous crisis after operation. At the same
time, the nail length, sensory level, two-point discrimination
(2-PD) and mobility of distal interphalangeal joint (DIPJ) of the
replanted finger were evaluated according to the follow-up results.
i) Venous crisis: The skin temperature of replanted finger was
observed; if it declined suddenly, the finger turned from red to
pale, the filling of capillaries in fingertip and nail disappeared,
finger pulp shrunk, and there was no bleeding in the side incision
of fingertip and dark purple blood sometimes slowly overflowed, and
it was deemed as venous crisis (7).
ii) Hemorheology: The platelet adhesion rate, whole blood
viscosity, whole blood low-shear viscosity, hematocrit and
fibrinogen, in patients were detected at 72 h after operation using
a capillary viscometer (8).
Statistical analysis
Statistical Product and Service Solutions (SPSS,
version X; SPSS, Inc., Chicago, IL, USA) 20.0 statistical software
was used for data analysis. Enumeration data are presented as
percentage and case (n, %). Chi-square test was used for comparison
of survival rate and necrosis rate. Measurement data are presented
as mean ± SD, and t-test was used for intergroup comparison.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Wound healing time and hospitalization
time after operation
After operation, the wound healing time and
hospitalization time of patients in the research group were lower
than those in control group, and the differences were statistically
significant (p<0.05) (Table
I).
 | Table I.Comparisons of wound healing time and
hospitalization time after operation of patients between the two
groups (mean ± SD, min). |
Table I.
Comparisons of wound healing time and
hospitalization time after operation of patients between the two
groups (mean ± SD, min).
| Groups | Wound healing time
after operation | Hospitalization time
after operation |
|---|
| Control (n=40) | 8.7±2.3 | 15.8±2.7 |
| Research (n=40) | 6.3±1.4 | 11.2±2.5 |
| t-test | 5.637 | 7.906 |
| P-value | 0.000? | 0.000? |
Hemorheology detection results
At 72 h after operation, the platelet adhesion rate,
whole blood viscosity, whole blood low-shear viscosity, hematocrit
and fibrinogen level in patients in research group were lower than
those in control group, and the differences were statistically
significant (p<0.05) (Table
II).
 | Table II.Comparison of hemorheology detection
results of severed finger of patients between the two groups at 72
h after operation (mean ± SD). |
Table II.
Comparison of hemorheology detection
results of severed finger of patients between the two groups at 72
h after operation (mean ± SD).
| Groups | Platelet adhesion
rate (%) | Whole blood viscosity
(15 | Whole blood low-shear
viscosity (150 | Hematocrit (%) | Fibrinogen (g/l) |
|---|
| Control (n=40) | 41.8±5.2 | 8.4±0.2 | 7.5±0.3 | 47.1±4.2 | 5.0±1.5 |
| Research (n=40) | 32.8±2.7 | 7.8±0.1 | 6.3±0.2 | 31.6±3.3 | 3.1±1.0 |
| t-test | 9.715 | 16.971 | 21.049 | 18.353 | 6.666 |
| P-value | <0.000 | <0.000 | <0.000 | <0.000 | <0.000 |
Recovery condition of replanted
finger
At 7 days after operation, the survival rate of
replanted finger in the research group was higher than that in
control group, but the necrosis rate of replanted finger and
incidence rate of venous crisis were lower than those in control
group, and the differences were statistically significant
(p<0.05) (Table III).
 | Table III.Comparison of survival rate and
necrosis rate of replanted finger, and incidence rate of venous
crisis of patients between the two groups at 7 days after operation
(n, %). |
Table III.
Comparison of survival rate and
necrosis rate of replanted finger, and incidence rate of venous
crisis of patients between the two groups at 7 days after operation
(n, %).
| Groups | Survival of replanted
finger | Necrosis of replanted
finger | Venous crisis |
|---|
| Control (n=40) | 30 (75.0) | 10 (25.0) | 12 (30.0) |
| Research (n=40) | 37 (92.5) | 3 (7.5) | 3 (7.5) |
| χ2 | 4.501 | 4.501 | 6.951 |
| P-value | 0.034 | 0.034 | 0.008 |
Functional recovery effect of
replanted finger
At 6 months after operation, the nail length,
sensation, 2-PD and mobility of DIPJ of patients in the research
group were superior to those in control group, and the differences
were statistically significant (p<0.05) (Table IV).
 | Table IV.Comparison of recovery effects of
replanted finger between the two groups at 6 months after operation
(mean ± SD). |
Table IV.
Comparison of recovery effects of
replanted finger between the two groups at 6 months after operation
(mean ± SD).
| Groups | Nail length | Sensation | 2-PD | Mobility of DIPJ |
|---|
| Control (n=40) | 11.3±0.8 | 2.5±0.2 | 7.5±0.4 | 44.8±3.2 |
| Research (n=40) | 15.8±4.3 | 3.7±0.4 | 5.0±0.7 | 59.7±5.3 |
| t-test | 6.507 | 16.971 | 19.612 | 15.221 |
| P-value | 0.000? | 0.000? | 0.000? | 0.000? |
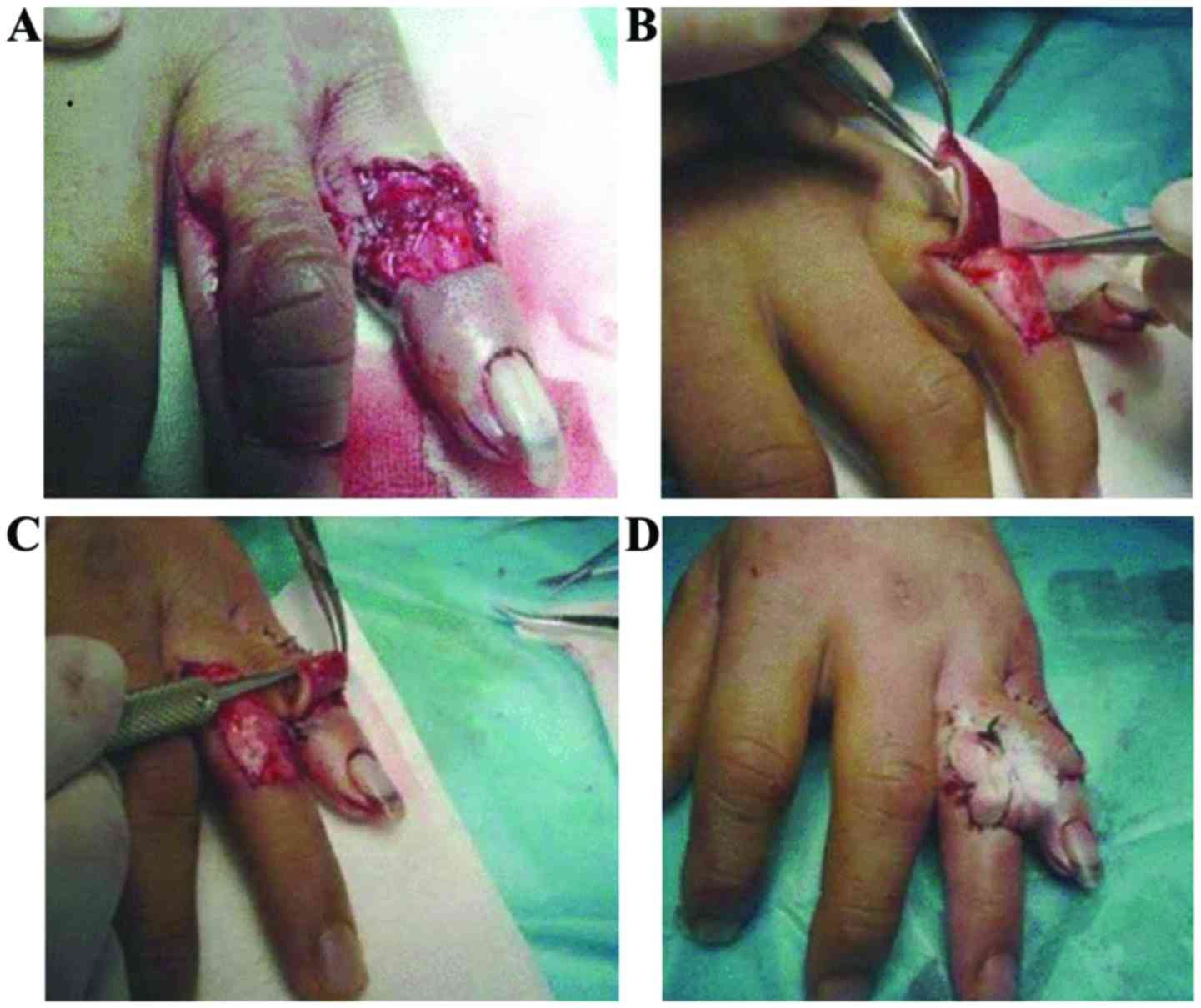
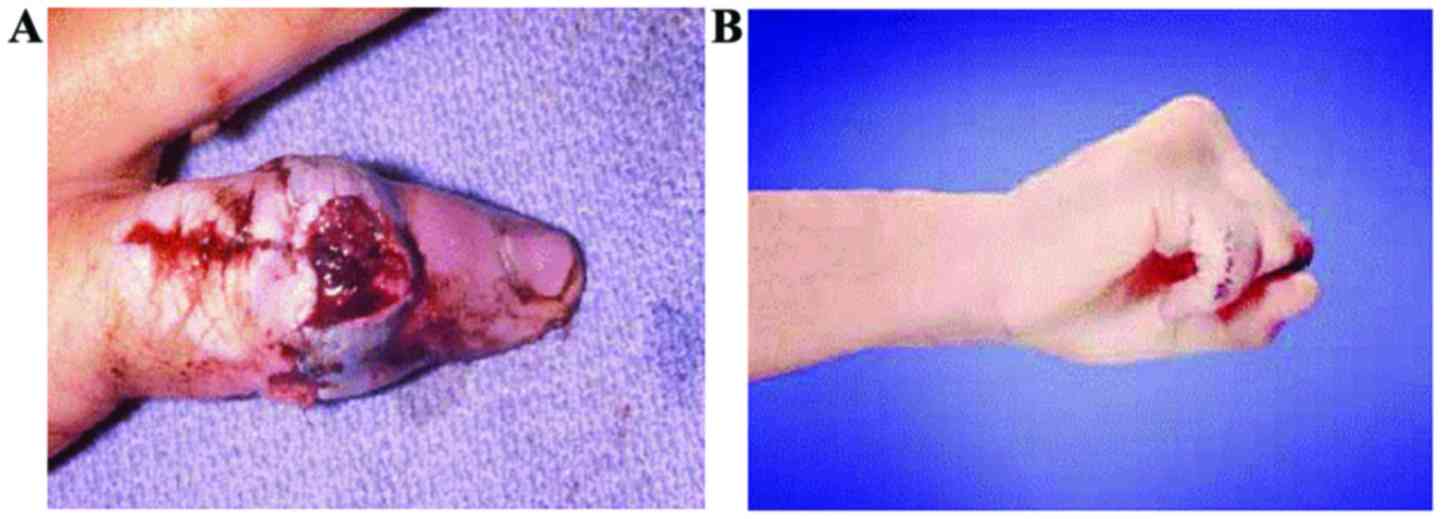
Surgical procedure and recovery
condition of severed finger without venous anastomosis
Unilateral digital arterial ligation does not reduce
the arterial blood supply of fingers in the treatment of severed
finger without venous anastomosis, which is characterized by high
survival rate and good postoperative recovery (Figs. 1 and 2).
Discussion
With the rapid development and perfection of
microsurgical technique, gradual maturity of small vascular
anastomosis technique in clinical medicine and the increasingly
higher requirement of people for modern life quality, people have
had higher and higher requirements of severed finger replantation
due to the serious impact of severed finger on the appearance,
function, psychology and normal communication of patients (9,10).
Therefore, it was found in clinical medicine on the basis of body
anatomy that there are direct communicating branches between the
branch and vein of dorsal digital artery, and it is difficult for
the corresponding supply of finger blood to return through the vein
when the physiological reflux veins disappear (11); but the proximal digital arterial
ligation after one-side anastomosis can reduce the arterial blood
perfusion of the replanted finger to a certain extent, buffer the
venous return load, and form a new blood circulation from the
dorsal digital arterial branches to the dorsal digital veins
(12).
Studies have shown that in the bilateral digital
arterial anastomosis in the unilateral digital arterial ligation,
the digital arterial section was ligated at 2–4 cm, so that the
venous return of replanted finger can be promoted to shunt towards
the dorsal digital veins via the dorsal digital arterial branches,
thus completing the new blood circulation. In early stage, new
collateral venous return can be formed at 3–7 days after the
low-level blood supply, promoting the survival of severed fingers
(13,14). Therefore, it is speculated that no
venous return is found in the severed finger after the connection
of bilateral arteries, so the incidence rate of venous crisis after
operation gradually increases under the sufficient arterial supply
but no venous return. There are distal arterial arches in the
digital arteries, combined with a large number of branches, so the
simple ligation of one-side artery has no significant threat to the
blood supply of finger tips, but can effectively reduce the
pressure of relevant tissue in finger tips after the replantation
of the severed finger; and the blood return can fully flow back to
veins via collateral circulation of non-severed end, promoting the
blood circulation (15). But we need
to pay attention in the unilateral digital arterial ligation: i)
The surgical operation should be gentle to avoid damage to the
blood vessels; ii) whether patients meet the surgical indications
should be assessed before surgery (16); iii) the non-invasive and
micro-operation principles should be followed; iv) in the arterial
anastomosis under the microscope, thicker blood vessels should be
anastomosed furthest, the operation should be gentle, and the
anastomotic blood vessels should be smooth enough; and v) the
digital arterial ligation should be implemented gently, the
integrity of soft tissue around the ligated arteries should be
guaranteed to the utmost and the digital arteries should be ligated
in case of good blood supply in the severed end.
Venous crisis as a kind of common clinical
complication, which is related to the poor quality of anastomosis,
incomplete debridement in injured veins and postoperative tissue
edema; if the patients do not receive timely treatment after venous
crisis, it will be detrimental to postoperative recovery (17).
Low molecular weight heparin, as a kind of
commonly-used anticoagulant, can effectively inhibit the thrombin
and coagulation factor Xa, and it can reach the peak in plasma at 3
h after subcutaneous injection and then decline, its half-life is
~3.5 h (18); at the same time, a
certain anticoagulant effect can be detected at 24 h after
medication, and the activity of anticoagulant factor IIa in the
course of medication is lower than that of anticoagulant factor Xa.
Low molecular weight heparin is metabolized a little and removed in
prototype via liver, and its half-life in the elderly patients is
slightly extended (19). Studies
have shown that the activity of anticoagulant factor Xa of low
molecular weight heparin is significant, and the anticoagulant
factor IIa and antithrombin activity is lower, so the low molecular
weight heparin can effectively inhibit the in vivo and in
vitro thrombosis and arteriovenous thrombosis in patients, nd
has no significant effect on the platelet aggregation, fibrinogen
and platelet binding and can play the anti-thrombus effect without
higher risk of hemorrhage (20).
The results of this study showed that the healing
time and hospitalization time of patients in the research group
after treatment were lower than those in control group, the
stability of hemorheology was higher than that in control group,
the recovery effect of replanted finger after operation was
superior to that of control group, and the incidence rate of venous
crisis was lower than that in control group, indicating that
unilateral digital arterial ligation combined with low molecular
weight heparin has a significant effect in the treatment of severed
finger without venous anastomosis, which can reduce the risk of
venous crisis and improve the recovery of replanted finger. Lee
et al study (21) showed that
controlled systemic continuous heparinization improved the
replantation success rate of artery-only anastomosis replantation
in single distal digit amputation, indicated that the use of the
anticoagulation is a safe and effective method in severed finger
replantation, which coincide with our result. Compared with
systemic continuous heparinization, low molecular weight heparin is
safer, more effective, more durable and more stable. However, the
sample size in this study was small, it was not a double-blind
study, the observation time was shorter, and the safety of patients
after surgery and medication was not analyzed. In addition, this
was a single-center clinical study. To get more valid and credible
results, the sample size can be expanded and a randomized,
double-blind, placebo controlled, multicenter study should be
conducted for in-depth study later.
In conclusion, unilateral digital arterial ligation
combined with low molecular weight heparin has a significant effect
in the treatment of severed finger without venous anastomosis,
which can effectively reduce or prevent the occurrence of venous
crisis, shorten the hospitalization time of patients, improve the
survival rate of replanted finger and promote the function recovery
of replanted finger, so it is worthy of clinical promotion.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
XC designed the study, ZC was for data collection,
XC and YX were for data analysis, ZC and JZ did the follow-up, XC
and YX prepared the manuscript. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Wuxi No. 9 People's Hospital (Jiangsu, China). Signed informed
consents were obtained from the patients and/or guardians.
Consent for publication
Patients or their guardians provided written
informed consents for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lee BI, Chung HY, Kim WK, Kim SW and Dhong
ES: The effects of the number and ratio of repaired arteries and
veins on the survival rate in digital replantation. Ann Plast Surg.
44:288–294. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Doi K, Hattori Y, Ikeda K and Dhawan V:
Significance of shoulder function in the reconstruction of
prehension with double free-muscle transfer after complete
paralysis of the brachial plexus. Plast Reconstr Surg.
112:1596–1603. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hasuo T, Nishi G, Tsuchiya D and Otsuka T:
Fingertip replantations: Importance of venous anastomosis and the
clinical results. Hand Surg. 14:1–6. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koshima I, Yamashita S, Sugiyama N, Ushio
S, Tsutsui T and Nanba Y: Successful delayed venous drainage in 16
consecutive distal phalangeal replantations. Plast Reconstr Surg.
115:149–154. 2005.PubMed/NCBI
|
|
5
|
Hsu CC, Lin YT, Moran SL and Lin CH, Wei
FC and Lin CH: Arterial and venous revascularization with
bifurcation of a single central artery: A reliable strategy for
Tamai Zone I replantation. Plast Reconstr Surg. 126:2043–2051.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gustafsson M and Ahlström G: Emotional
distress and coping in the early stage of recovery following acute
traumatic hand injury: A questionnaire survey. Int J Nurs Stud.
43:557–565. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Whitaker IS, Josty IC, Hawkins S,
Azzopardi E, Naderi N, Graf J, Damaris L, Lineaweaver WC and Kon M:
Medicinal leeches and the microsurgeon: A four-year study, clinical
series and risk benefit review. Microsurgery. 31:281–287. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
van Alphen NA, Gonzalez A, McKenna MC,
McKenna TK, Carlsen BT and Moran SL: Ciprofloxacin-resistant
Aeromonas infection following leech therapy for digit
replantation: Report of 2 cases. J Hand Surg Am. 39:499–502. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhao J, Abdullah S, Li WJ, Appukuttan A
and Tien HY: A novel solution for venous congestion following
digital replantation: A proximally based cross-finger flap. J Hand
Surg Am. 36:1224–1230. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang GL, Chen KM, Zhang JH and Wang SY:
Hand reconstruction using heterotopic replantation of amputated
index and little fingers. Chin J Traumatol. 14:316–318.
2011.PubMed/NCBI
|
|
11
|
Yabe T, Tsuda T, Hirose S and Ozawa T:
Treatment of fingertip amputation: Comparison of results between
microsurgical replantation and pocket principle. J Reconstr
Microsurg. 28:221–226. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
McClain DA, Abuelgasim KA, Nouraie M,
Salomon-Andonie J, Niu X, Miasnikova G, Polyakova LA, Sergueeva A,
Okhotin DJ, Cherqaoui R, et al: Decreased serum glucose and
glycosylated hemoglobin levels in patients with Chuvash
polycythemia: A role for HIF in glucose metabolism. J Mol Med
(Berl). 91:59–67. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Martini M, Teofili L, Cenci T, Giona F,
Torti L, Rea M, Foà R, Leone G and Larocca LM: A novel heterozygous
HIF2AM535I mutation reinforces the role of oxygen
sensing pathway disturbances in the pathogenesis of familial
erythrocytosis. Haematologica. 93:1068–1071. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Richalet JP, Rivera-Ch M, Maignan M,
Privat C, Pham I, Macarlupu JL, Petitjean O and León-Velarde F:
Acetazolamide for Monge's disease: Efficiency and tolerance of
6-month treatment. Am J Respir Crit Care Med. 177:1370–1376. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Delton-Vandenbroucke I, Grammas P and
Anderson RE: Regulation of n-3 and n-6 fatty acid metabolism in
retinal and cerebral microvascular endothelial cells by high
glucose. J Neurochem. 70:841–849. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tang YB, Simchon S and Chen HC:
Microcirculation of a venous flap: An experimental study with
microspheres in rabbits. Scand J Plast Reconstr Surg Hand Surg.
34:207–212. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang L, Fu J, Li M, Han D and Yang L:
Repair of hand defects by transfer of free tissue flaps from toes.
Arch Orthop Trauma Surg. 133:141–146. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Siminerio L, Ruppert KM and Gabbay RA: Who
can provide diabetes self-management support in primary care?
Findings from a randomized controlled trial. Diabetes Educ.
39:705–713. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Beacham BL and Deatrick JA: Health care
autonomy in children with chronic conditions: Implications for
self-care and family management. Nurs Clin North Am. 48:305–317.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cicutto L, Brooks D and Henderson K:
Self-care issues from the perspective of individuals with chronic
obstructive pulmonary disease. Patient Educ Couns. 55:168–176.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lee JY, Kim HS, Heo ST, Kwon H and Jung
SN: Controlled continuous systemic heparinization increases success
rate of artery-only anastomosis replantation in single distal digit
amputation: A retrospective cohort study. Medicine (Baltimore).
95:e39792016. View Article : Google Scholar : PubMed/NCBI
|