Introduction
Paraquat (PQ) is one of the most widely used
herbicides worldwide, especially in developing countries (1). It was reported that 5–15 ml of 20%
concentration of PQ can lead to moderate or severe poisoning. There
are thousands of case reports on accidental or deliberate poisoning
of PQ each year (2). PQ has been
classified as moderately hazardous by the World Health Organization
(WHO) due to the lack of antidotes or effective strategies for the
toxicity. The toxicity of PQ is mainly mediated by its redox
activity (3). PQ interacts with a
variety of enzymes, such as cytochrome P450 reductase, cytochrome
oxidase and nitric oxide synthase. PQ is an electron receptor that
acts on the intracellular redox reactions, producing large amounts
of reactive oxygen species (ROS) and reactive free radicals and
cause severe cell damage (4,5). A previous study has shown that the main
organs of PQ distribution are the lung and the kidney (6). PQ has a structure similar to MPP, which
is a metabolite of 1-methyl-4-phenylpyridine (MPTP), indicating
that PQ is neurotoxic (7). For these
reasons, previous studies focused on the lung, kidney and brain.
Therefore, there is little information on the toxic effects of PQ
on other organs. The liver is the main organ of detoxification.
Recently, Kral et al confirmed that the liver is an
important target organ for PQ (8).
Curcumin, as a Chinese medicine extract, is well studied and
confirmed to have anti-inflammatory and antioxidant effects and
extensive biological functions in regulating the nervous system,
cardiovascular disease, lung disease, immune system, and tumor
development (9). However, there is
no systematic study on the protective mechanism of curcumin on
liver injury, especially PQ-induced liver injury. Therefore, the
purpose of this study was to investigate the effect of curcumin on
the dynamic processes of PQ-induced liver injury and pathological
changes and its intrinsic regulatory molecules with an expectation
of providing a theoretical basis for the clinical treatment of
PQ.
Materials and methods
Experimental animal grouping
Forty-eight male SPF grade SD rats were provided by
Nanjing Animal Experimental Center (Nanjing, China) (experimental
animal license no. SYXK2017-084). Rats were 6–9 weeks old and
weighed 180–300 g. They were fed for a week at room temperature of
26°C, under regular lighting, and environmental noise <45 dB.
Rats were divided into three groups: control group, PQ group, and
PQ + curcumin group, with 16 rats in each group. Based on our
preliminary data and the findings of Ishrat et al (10), rats in the control group were treated
with gavage using 0.2 ml normal saline every day. The rats in the
PQ group were treated with 50 mg/kg PQ every day. The PQ + curcumin
group was given 200 mg/kg curcumin on the basis of PQ group. The
weight of rats was recorded daily. All animal experiments were in
strict accordance with the National Animal Ethics Association
guidelines on the use and care of laboratory animals. The study was
approved by the Ethics Committee of Gansu Provincial People's
Hospital (Lanzhou, China).
Sample collection and processing
On the 1st, 3rd and 7th day after treatment, 6 rats
were randomly selected from each group and were sacrificed by
CO2 inhalation followed by spinal dislocation. Rats were
anesthetized with 10% chloral hydrate (300 µl/g) with endotracheal
intubation. From each rat 10 ml of apical blood was taken, liver
tissue was collected and placed in 4% formalin buffer and stored in
liquid nitrogen. All samples were collected and used for RT-qPCR
and western blot analysis. Blood samples were kept at room
temperature for 30 min, followed by centrifugation at 1,000 × g,
4°C for 10 min. Serum samples were sent to our laboratory for
determination of alanine aminotransferase (ALT) and aspartate
aminotransferase (AST) levels using the Beckman DxC 800 automated
biochemical analyzer (Beckman Coulter, Inc., Shanghai, China). The
rest of the serum was assayed to measure malondialdehyde (MDA) by
thiobarbital colorimetric assay (cat. no. A003-1) and superoxide
dismutase (SOD) by xanthine oxidation assay (cat. no. A001-3) (both
from Nanjing Jiancheng Bio-Engineering Institute Co., Ltd.,
Nanjing, China). Liver tissue homogenate was made, and the level of
ROS was measured by an active oxygen detection kit (cat. no.
CA1410-100T; Beijing Solarbio Science & Technology Co., Ltd.,
Beijing, China). With distilled water as control, the absorbance
value of each sample was measured at 550 nm. ROS concentration was
calculated according to the formula, and ROS was expressed as U/mg
(11–13).
Hematoxylin and eosin (H&E)
staining
Rat liver tissue was cut into 1–2 mm thick pieces,
placed in 4% formalin buffer overnight, dehydrated gradient ethanol
and n-butanol, and then waxed and embedded in wax. The wax pieces
were sliced at a thickness of 4 µm and baked in a 60°C oven for 3
h. After dimethyl dewaxing, ethanol rehydration and H&E
staining, the slices were examined under a Philips microscope (EM
300, Philips Healthcare, Amsterdam, The Netherlands).
RT-qPCR
TRIzol reagent (Invitrogen; Thermo Fisher
Scientific, Inc., Waltham, MA, USA) was used to extract total RNA
from rats. cDNA was synthesized from 1 µg of RNA using one-step
reverse transcription kit (no. 639505; Takara Bio, Inc., Otsu,
Japan). The mRNA levels of each index were measured using a
fluorescence quantitative PCR kit (FSQ-101; Toyobo Life Science,
Osaka, Japan). GAPDH was taken as an internal reference. TGF-β1
gene localization: NC_000019.10. Primers were designed and
synthesized by Shanghai Sangon Biotechnology Co., Ltd. (Shanghai,
China). Sequence: upstream, 5′-GGCCAGATCCTGTCCAAGC-3′ and
downstream, 5′-GTGGGTTTCCACCATTAGCAC-3′; internal reference GAPDH:
upstream, 5′-TGGCCTTCCGTGTTCCTAC-3′ and downstream,
5′-GAGTTGCTGTTGAAGTCGCA-3′. The relative expression level of each
index was calculated by 2−ΔCq [ΔCq = Cq (target gene) -
Cq (GAPDH)] (14–16).
Western blot analysis
The liver of SD rats was removed from liquid
nitrogen and cut. The mixture was homogenized with 500 µl of RIPA
(tissue lysate, Beyotime Biotechnology, Guangzhou, China) and 1%
cocktail (protease inhibitor; ProteinTech Group, Inc., Chicago, IL,
USA) and centrifuged at 13,000 × g, 4°C for 30 min. The supernatant
was measured for its protein concentration using an automatic
microplate reader (PerkinElmer, Inc., Waltham, MA, USA). Protein
sample (40 µg) was taken and separated with 12% sodium dodecyl
sulfate-polyacrylamide gel (SDS-PAGE). The total protein was
transferred onto nitrocellulose membrane (NC) and the band at 25
kDa was incubated with TGF-β1 primary antibody (1:1,000, cat. no.
E-CL-H0109c; Cell Signaling Technology, Inc., Danvers, MA, USA).
The abundance of the target protein was measured under the ECL
chemiluminescence system (Merck KGaA, Darmstadt, Germany) using
ultra-sensitive chemiluminescent (Merck KGaA) and the grey value
was analyzed with ImageJ software (V2.1.4.7; National Institutes of
Health, Bethesda, MD, USA).
Statistical methods
The results were analyzed using GraphPad Prism
software (version 5.01; GraphPad Software, Inc., La Jolla, CA,
USA). The single factor analysis of variance and SNK-q test were
used to compare the measurement data. P<0.05 was considered to
indicate a statistically significant difference.
Results
Effects of curcumin on body weight in
rats
Table I shows that
the body weight of the rats in the PQ group decreased significantly
after poisoning (P<0.05), while the weight of the rats in the PQ
+ curcumin group was at the lowest level on the 3rd day and then
increased. On the 1st, 3rd and 7th day, the weight of rats in PQ +
curcumin group was heavier than that in PQ group, and the
difference was statistically significant (P<0.05).
 | Table I.Weight changes in three groups (mean ±
SD, g). |
Table I.
Weight changes in three groups (mean ±
SD, g).
| Group | Before poisoning | 1st day | 3rd day | 7th day |
|---|
| Control | 217.83±15.27 | 223.53±16.34 | 231.04±16.92 | 243.55±16.88 |
| PQ | 216.42±15.76 |
202.17±17.90a |
185.54±19.48b |
165.06±21.87c |
| PQ + curcumin |
218.59±21.87a |
216.67±15.26d |
210.41±16.86d |
238.77±18.85e |
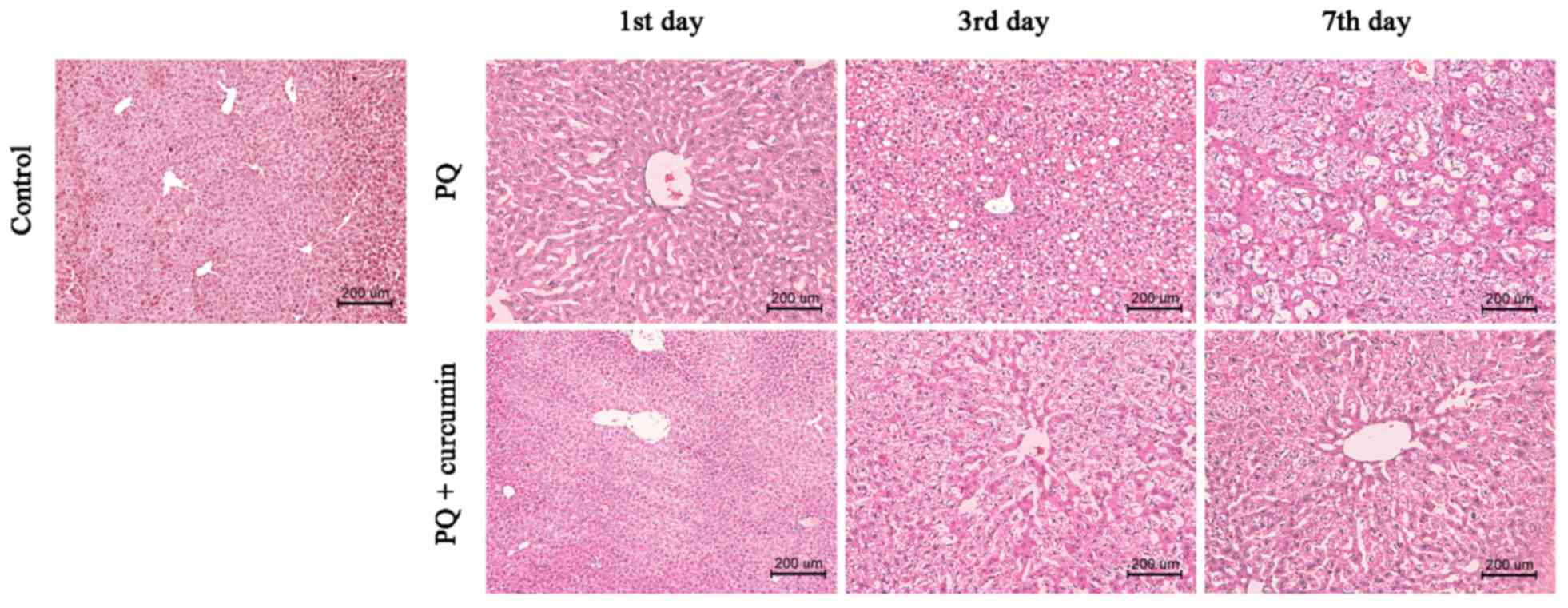
Observation of the liver tissue
morphology by H&E staining
It can be seen from Fig.
1 that on the 1st day after poisoning, the rats in PQ group
showed significant edema of liver cells, obvious fatty degeneration
was observed on the 3rd day; and large number of cavities appeared
on the 7th day due to necrosis. For the PQ + curcumin group, the
rats showed no obvious change on the 1st day, while liver cell
edema appeared on the 3rd day, and mild swelling of liver cells was
observed on the 7th day. It is suggested that curcumin treatment
can protect from liver injury caused by PQ.
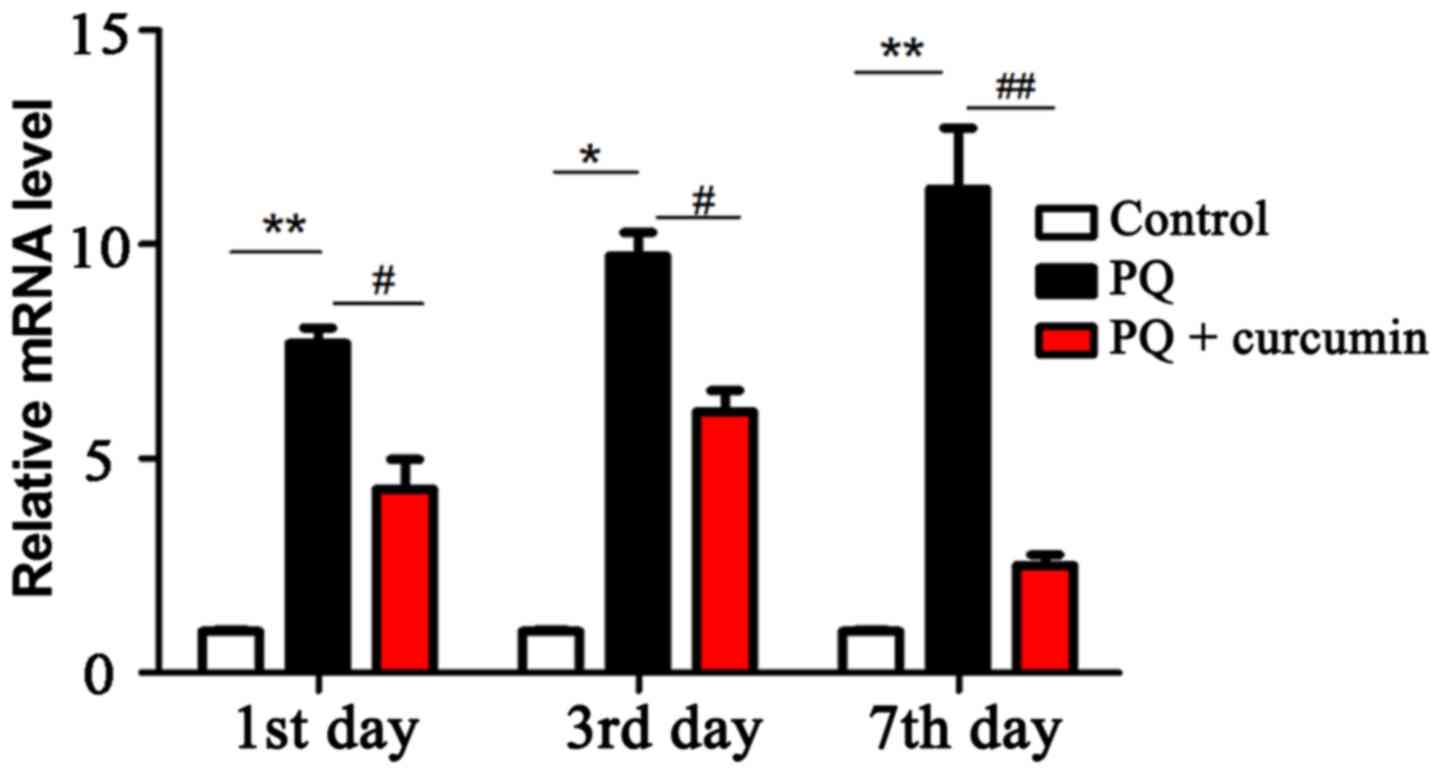
RT-qPCR detection of liver tissue
TGF-β1 mRNA content
It can be seen from Fig.
2 that compared with the control group, liver TGF-β1 of the
rats in PQ group was increased on the 1st, 3rd and 7th day after
poisoning (P<0.05), while for the rats in PQ + curcumin group
mRNA level reached the peak on the 3rd day and then decreased. It
should be noted that the levels of TGF-β1 in PQ + curcumin group
were lower than those in PQ group at these three time-points
(P<0.05).
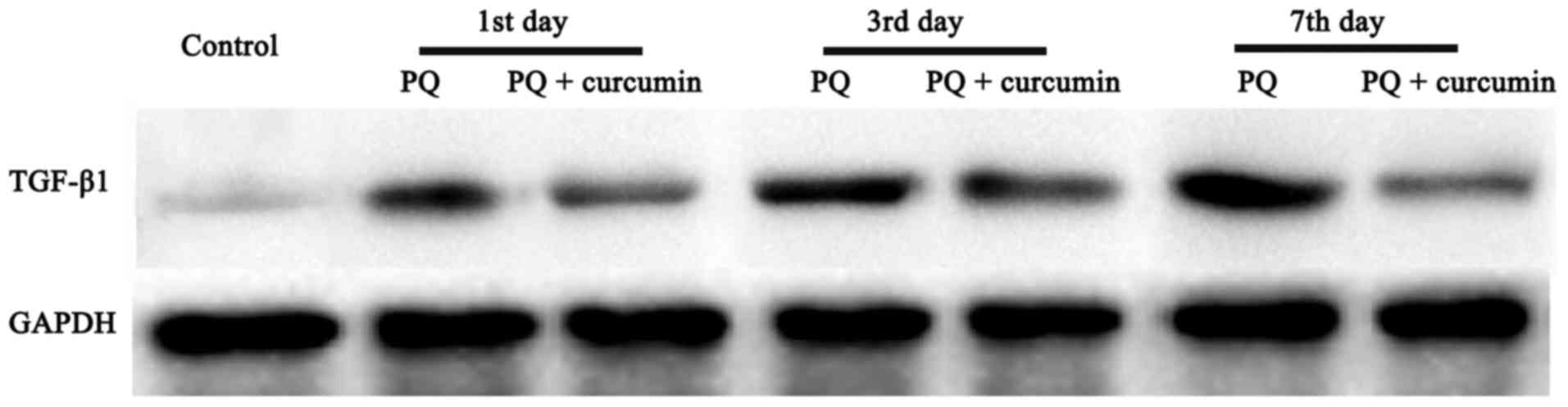
Detection of TGF-β1 protein content in
liver tissue by western blot analysis
It can be seen from Fig.
3 that, compared with the control group, liver TGF-β1 protein
of PQ rats increased on the 1st, 3rd and 7th day after poisoning,
which was consistent with the results of RT-qPCR. While in the PQ +
curcumin group, TGF-β1 protein peaked on day 3 and subsequently
decreased. At all three time-points, the content of TGF-β1 protein
in PQ + curcumin group was lower than that in PQ group.
Effects of curcumin on liver
function
Table II shows that
ALT and AST in the blood of PQ rats continued to increase after
poisoning (P<0.05), and reached the highest value on the 7th
day: 87.31±13.72, 106.34±25.82. ALT and AST in the PQ + curcumin
group reached the peak on the 3rd day and then decreased. The ALT
and AST levels of the PQ + curcumin group were lower than those of
PQ group at the three time-points on day 1, 3 and 7, and the
difference was statistically significant (P<0.05).
 | Table II.Liver function of rats (mean ± SD,
U/l). |
Table II.
Liver function of rats (mean ± SD,
U/l).
| Group | Time | ALT | AST |
|---|
| Control | 1st | 26.86±2.59 | 33.36±3.06 |
|
| 3rd | 27.37±2.36 | 32.51±4.76 |
|
| 7th | 26.04±2.94 | 36.24±5.33 |
| PQ | 1st |
37.50±5.72a |
57.36±6.45a |
|
| 3rd |
63.88±12.67b |
83.45±18.39b |
|
| 7th |
87.31±13.72b |
106.34±25.82c |
| PQ + curcumin | 1st |
33.49±7.45d |
40.66±25.82d |
|
| 3rd |
47.04±15.36d |
57.81±11.05e |
|
| 7th |
36.52±12.32e |
46.34±8.37f |
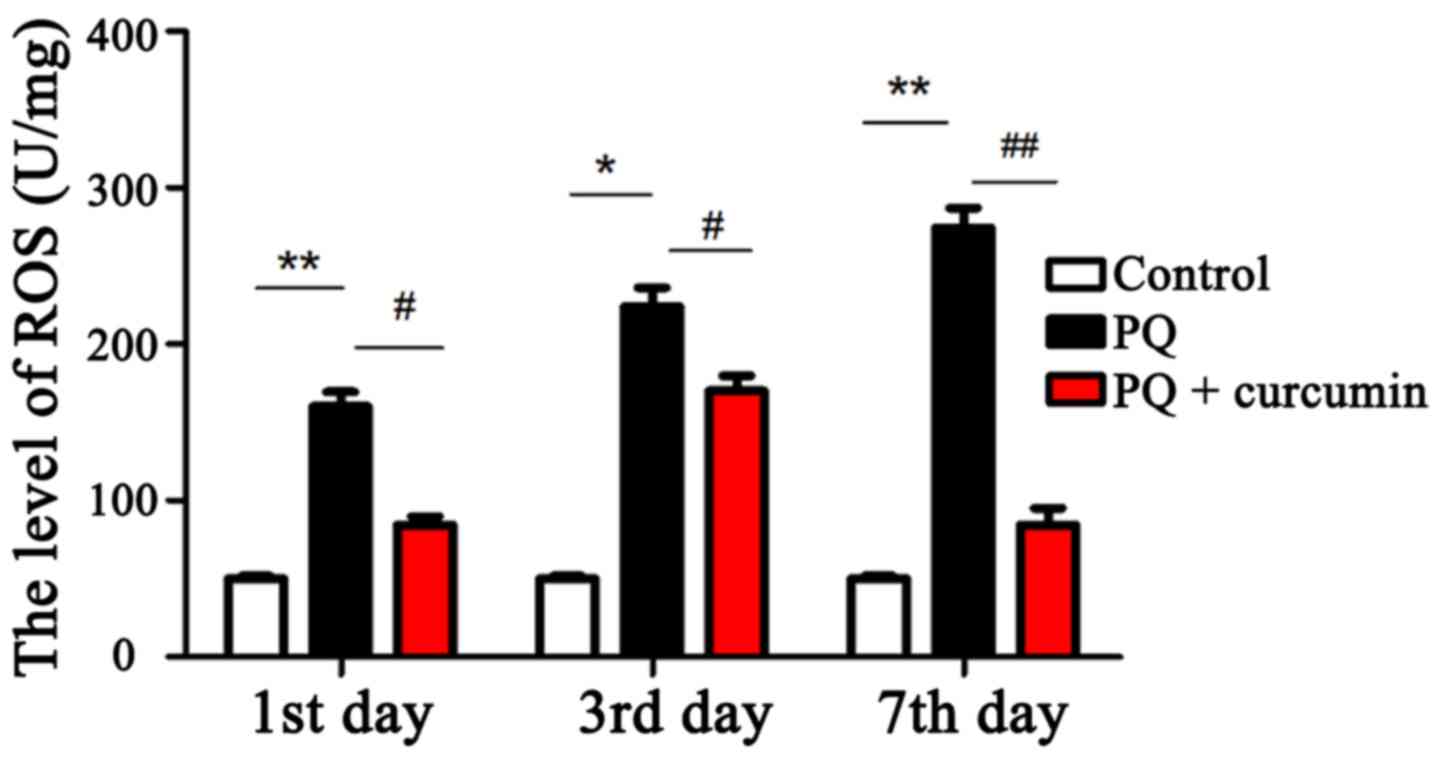
ROS level in the liver
The level of ROS was an indicator of oxidative
stress and liver injury in rats. The results showed that compared
with the control group, ROS in the liver of PQ rats continued to
increase after poisoning (P<0.05). ROS in the PQ + curcumin
group reached the peak on the 3rd day, and then decreased. Curcumin
treatment significantly reduced the level of ROS (P<0.05)
(Fig. 4).
MDA and SOD levels in the liver
MDA and SOD were used as indicators of oxidative
stress. The results (Table III)
showed that compared with the control group, the levels of MDA in
the PQ group were increased and the levels of SOD were decreased
(P<0.05). The levels of MDA in PQ + curcumin group increased
first and then decreased, and the level of SOD decreased first and
then increased. For the PQ + curcumin group, the level of MDA was
lower than that in PQ group at the three time-points (P<0.05),
and the level of SOD was higher than that in PQ group
(P<0.05).
 | Table III.Rat oxidative stress (mean ± SD). |
Table III.
Rat oxidative stress (mean ± SD).
| Group | Time | MDA (mmol/l) | SOD
(×103 U/l) |
|---|
| Control | 1st | 0.42±0.07 | 167.03±11.42 |
|
| 3rd | 0.41±0.06 | 168.71±10.85 |
|
| 7th | 0.47±0.09 | 165.33±11.97 |
| PQ | 1st |
2.58±0.83a |
123.50±21.86a |
|
| 3rd |
4.57±2.74b |
105.36±26.63b |
|
| 7th |
7.76±3.12b |
94.43±37.74b |
| PQ + curcumin | 1st |
1.04±0.72c |
138.72±12.94c |
|
| 3rd |
2.12±0.87c |
117.40±28.08c |
|
| 7th |
1.45±0.39c |
146.31±21.65d |
Discussion
The important mechanism of PQ toxicity in different
experimental models (including plants, bacteria and animals) is
oxidative stress (17). Antioxidants
have become potential therapeutic agents. In the rat model,
antioxidants were able to prevent oxidative stress-induced lipid
peroxidation cell damage caused by PQ, interstitial edema and
inflammatory cell infiltration (18). In this experiment, the extract of
turmeric rhizome-curcumin, a low molecular weight polyphenol
substance, was selected. It is the most active component of
turmeric (19). It is reported that
it has good anti-inflammatory, antitumor and antioxidant
properties. Jha and Mishra found that curcumin nasal administration
can effectively remove free radicals and inhibit lipid peroxidation
(20).
SOD is the scavenger for various oxygen free
radicals in the body; it can act by catalyzing the disproportional
free radicals in organisms, including superoxide radicals, hydroxyl
radicals and lipid peroxides (21).
MDA is the terminal product of lipid peroxidation (22). The oxidative stress markers were
measured at different time-points to evaluate the antioxidant
activity of curcumin. The results showed that curcumin treatment
significantly increased SOD activity in rats and significantly
decreased MDA levels. TGF-β1, as an important member of the
transforming growth factor superfamily, plays an important role in
promoting hepatic steatosis, hepatocyte injury, inflammatory cell
infiltration, inflammatory cytokine production, HSC activation and
fibrosis (23,24). More importantly, literature
demonstrates that TGF-β1 signaling is involved in ROS production
and lipid accumulation (25). TGF-β
signaling pathway is involved in the expression of fat and fatty
acid β antioxidant genes, leading to the synthesis of triglycerides
and the accumulation of hepatocyte lipids (26). In the case of further accumulation of
lipids, TGF-β1 induces cell death through NF-κB/TAK1 pathway and
mediates the production of reactive oxygen species (27). In addition, TGF-β1 affects the
expression of various inflammatory factors through the oxidative
stress pathway (28). Li et
al found that oxidative stress and cell membrane lipid
peroxidation are one of the mechanisms by which PQ causes lung
injury. Curcumin reduces the extent of lung injury by preventing
this process (29). Li et al
studied the effects of different concentrations of PQ on serum
inflammation-related cytokines, and they found that curcumin could
reduce the level of serum inflammatory response in rats to improve
lung pathological changes (30). Han
et al reported that curcumin increased the activity of HO-1,
NQO-1, SOD and CAT and induced the antioxidant capacity of liver
cells by inducing the expression of Nrf2 (31). However, these studies were mainly
focused on the mechanism of PQ-induced lung injury. The protective
effects of curcumin on liver injury induced by PQ, and the
involvement of TGF-β1 in this process remains to be further
studied.
In the present study, we used RT-qPCR and western
blot analysis to detect the dynamic changes of TGF-β1 in rat liver
tissue after PQ exposure. The results showed that mRNA and protein
levels of TGF-β1 in the liver of PQ poisoned rats tended to
increase continuously. However, the mRNA and protein levels of
TGF-β1 in liver decreased significantly after a 3-day intervention
with curcumin. H&E staining was used to detect the changes of
liver histomorphology at different time-points after PQ treatment
in rats. H&E staining showed that for the PQ-poisoned rats,
obvious fatty degeneration was observed in the liver on the 3rd
day; and large number of cavities appeared on the 7th day due to
necrosis. In PQ + curcumin group, there was no significant change
in liver on the 1st day, hepatocyte edema appeared on the 3rd day,
and mild hepatocyte edema appeared on the 7th day. In addition,
curcumin can improve acute liver injury caused by PQ poisoning, by
reducing AST and ALT activity.
These results indicate that TGF-β1 plays an
important role in PQ-induced liver injury. Curcumin can effectively
inhibit the expression of TGF-β1, prevent PQ-induced oxidative
damage of liver cells and protect liver function.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HC conceived and designed the study, and drafted the
manuscript. HC and XF collected the data and were responsible for
RT-qPCR and western blot analysis. Both authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Gansu Provincial People's Hospital (Lanzhou, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wesseling C, van Wendel de Joode B,
Ruepert C, León C, Monge P, Hermosillo H and Partanen TJ: Paraquat
in developing countries. Int J Occup Environ Health. 7:275–286.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Baltazar T, Dinis-Oliveira RJ, Duarte JA,
de Lourdes Bastos M and Carvalho F: Paraquat research: Do recent
advances in limiting its toxicity make its use safer? Br J
Pharmacol. 168:44–45. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ortiz-Ortiz MA, Morán JM, Ruiz-Mesa LM,
Bonmatty RG and Fuentes JM: Protective effect of the glial cell
line-derived neurotrophic factor (GDNF) on human mesencephalic
neuron-derived cells against neurotoxicity induced by paraquat.
Environ Toxicol Pharmacol. 31:129–136. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Djukic MM, Jovanovic MD, Ninkovic M,
Stevanovic I, Ilic K, Curcic M and Vekic J: Protective role of
glutathione reductase in paraquat induced neurotoxicity. Chem Biol
Interact. 199:74–86. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dinis-Oliveira RJ, Remião F, Carmo H,
Duarte JA, Navarro AS, Bastos ML and Carvalho F: Paraquat exposure
as an etiological factor of Parkinson's disease. Neurotoxicology.
27:1110–1122. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Suntres ZE: Role of antioxidants in
paraquat toxicity. Toxicology. 180:65–77. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Berry C, La Vecchia C and Nicotera P:
Paraquat and Parkinson's disease. Cell Death Differ. 17:1115–1125.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kral AH, Malekinejad M, Vaudrey J,
Martinez AN, Lorvick J, McFarland W and Raymond HF: Comparing
respondent-driven sampling and targeted sampling methods of
recruiting injection drug users in San Francisco. J Urban Health.
87:839–850. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Aggarwal BB and Harikumar KB: Potential
therapeutic effects of curcumin, the anti-inflammatory agent,
against neurodegenerative, cardiovascular, pulmonary, metabolic,
autoimmune and neoplastic diseases. Int J Biochem Cell Biol.
41:40–59. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ishrat T, Hoda MN, Khan MB, Yousuf S,
Ahmad M, Khan MM, Ahmad A and Islam F: Amelioration of cognitive
deficits and neurodegeneration by curcumin in rat model of sporadic
dementia of Alzheimer's type (SDAT). Eur Neuropsychopharmacol.
19:636–647. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Abdesselem M, Ramodiharilafy R, Devys L,
Gacoin T, Alexandrou A and Bouzigues CI: Fast quantitative ROS
detection based on dual-color single rare-earth nanoparticle
imaging reveals signaling pathway kinetics in living cells.
Nanoscale. 9:656–665. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim JY, Choi WI, Kim YH and Tae G: Highly
selective in-vivo imaging of tumor as an inflammation site by ROS
detection using hydrocyanine-conjugated, functional nano-carriers.
J Control Release. 156:398–405. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chan MS, Xu D, Guo L, Tam DY, Liu LS, Chen
Y, Wong MS and Lo PK: Cyanine fluorophores for cellular protection
against ROS in stimulated macrophages and two-photon ROS detection.
Org Biomol Chem. 13:7307–7312. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang H, Cao Y, Chen Y, Li G and Yu H:
Apatinib promotes apoptosis of the SMMC-7721 hepatocellular
carcinoma cell line via the PI3K/Akt pathway. Oncol Lett.
15:5739–5743. 2018.PubMed/NCBI
|
|
15
|
Li S and Wei Y: Association of HMGB1,
BRCA1 and P62 expression in ovarian cancer and chemotherapy
sensitivity. Oncol Lett. 15:9572–9576. 2018.PubMed/NCBI
|
|
16
|
Zhang C, Wang YQ, Jin G, Wu S, Cui J and
Wang RF: Selection of reference genes for gene expression studies
in human bladder cancer using SYBR-Green quantitative polymerase
chain reaction. Oncol Lett. 14:6001–6011. 2017.PubMed/NCBI
|
|
17
|
Soares JJ, Rodrigues DT, Gonçalves MB,
Lemos MC, Gallarreta MS, Bianchini MC, Gayer MC, Puntel RL, Roehrs
R and Denardin ELG: Paraquat exposure-induced Parkinson's
disease-like symptoms and oxidative stress in Drosophila
melanogaster: Neuroprotective effect of Bougainvillea glabra
Choisy. Biomed Pharmacother. 95:245–251. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Singh S and Aggarwal BB: Activation of
transcription factor NF-κB is suppressed by curcumin
(diferuloylmethane) [corrected]. J Biol Chem. 270:24995–25000.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Anand P, Kunnumakkara AB, Newman RA and
Aggarwal BB: Bioavailability of curcumin: Problems and promises.
Mol Pharm. 4:807–818. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jha NS and Mishra S: Antioxidant activity
and electrochemical elucidation of the enigmatic redox behavior of
curcumin and its structurally modified analogues. Electrochim Acta.
151:5742015. View Article : Google Scholar
|
|
21
|
Su X, He Y, Yang W and Wang Y, Zhang W and
Wang Y: Effect of Dan Hong injection on PON1, SOD activity and MDA
levels in elderly patients with coronary heart disease. Int J Clin
Exp Med. 7:5886–5889. 2014.PubMed/NCBI
|
|
22
|
Kassim SK, Kamal S, Shehata HH, Salib MM,
Louka M, Sallam M and Nabegh LM: Evaluation of serum fibrotic
markers; CTGF, IL-17 and TGF-β1 versus liver biopsy for detection
of hepatic fibrosis in Egyptian patients with chronic hepatitis.
Meta Gene. 13:63–69. 2017. View Article : Google Scholar
|
|
23
|
Xu MY, Hu JJ, Shen J, Wang ML, Zhang QQ,
Qu Y and Lu LG: Stat3 signaling activation crosslinking of TGF-β1
in hepatic stellate cell exacerbates liver injury and fibrosis.
Biochim Biophys Acta. 1842:2237–2245. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li Y, Kim BG, Qian S, Letterio JJ, Fung
JJ, Lu L and Lin F: Hepatic stellate cells inhibit T cells through
active TGF-β1 from a cell surface-bound latent TGF-β1/GARP complex.
J Immunol. 195:2648–2656. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu YN, Zha WJ, Ma Y, Chen FF, Zhu W, Ge
A, Zeng XN and Huang M: Galangin attenuates airway remodelling by
inhibiting TGF-β1-mediated ROS generation and MAPK/Akt
phosphorylation in asthma. Sci Rep. 5:117582015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wu J, Niu J, Li X, Wang X, Guo Z and Zhang
F: TGF-β1 induces senescence of bone marrow mesenchymal stem cells
via increase of mitochondrial ROS production. BMC Dev Biol.
14:212014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tang H, Gao L, Mao J, He H, Liu J, Cai X,
Lin H and Wu T: Salidroside protects against bleomycin-induced
pulmonary fibrosis: Activation of Nrf2-antioxidant signaling, and
inhibition of NF-κB and TGF-β1/Smad-2/-3 pathways. Cell Stress
Chaperones. 21:239–249. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wang JZ, Fang XT, Lv E, Yu F, Wang ZW and
Song HX: TGF-β1 related inflammation in the posterior longitudinal
ligament of cervical spondylotic myelopathy patients. Int J Clin
Exp Med. 8:2233–2239. 2015.PubMed/NCBI
|
|
29
|
Li H, Liu B, Li P, Feng L, Ma H, Xuan S
and Cao Y: Inhibitory effects of curcumin on inflammatory cytokines
in rats with paraquat poisoning. Zhonghua Lao Dong Wei Sheng Zhi Ye
Bing Za Zhi. 33:689–692. 2015.(In Chinese). PubMed/NCBI
|
|
30
|
Li H, Cao Y, Liu B, Feng L and Li P:
Antagonistic effect of curcumin on lipid peroxidation of rats
poisoned by paraquat. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za
Zhi. 33:609–611. 2015.(In Chinese). PubMed/NCBI
|
|
31
|
Han W, Wu D, Liu H, Lu Y, Wang L, Hong G,
Qiu Q and Lu Z: Curcumin alleviated liver oxidative stress injury
of rat induced by paraquat. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing
Za Zhi. 32:352–356. 2014.(In Chinese). PubMed/NCBI
|