Introduction
Rheumatoid arthritis (RA) is a kind of systemic
autoimmune disease, which is mainly characterized by multiple joint
synovitis. Due to the combined action of environment and genetic
factors, the pathogenesis of the disease is becoming more complex.
Data have shown that the prevalence of RA in China is approximately
0.38%, but that in European and American countries can reach nearly
2.0% (1). Since the most important
complication of RA is disability, which severely influences the
patient's quality of life and causes great economic pressure to
society, RA has attracted the attention of scientific researchers
over the last decade (2). The
pathological characteristics of RA include abnormal hyperplasia of
synovial tissues, aggregation of infiltrating inflammatory cells
and pannus in the synovial membrane which even involves cartilage
and lower-layer bone, leading to joint deformity combined with
function loss.
It has been shown that the aggregation of
infiltrating inflammatory cells and decompensation of synovial cell
hyperplasia are closely related to the pathology of RA (3). The mechanism involved is that the
aggregation of multiple inflammatory cells in the synovial tissue
can induce the proliferation and thickening of synovial cells,
which is involved in the injury of cartilage and lower-layer bone.
Currently, the clinical medication for RA treatment mainly consists
of i) non-steroidal anti-inflammatory drugs which can relieve the
acute symptoms but have great side effects on the gastrointestinal
tract; ii) anti-inflammatory and immunosuppressive drugs with
strong efficacy, which can fundamentally treat the disease but have
the shortcoming of apparent adverse reactions; thus the medication
duration should not be too long and iii) biological medicine,
including specific receptor antagonist and monoclonal antibody,
which has obvious specificity and targeting. However, biological
medicine can be degraded rapidly and have antigenicity in the body,
so that the long-term outcomes are not ideal. Therefore, it is
crucial to explore the complicated mechanism of RA and seek new
efficient drugs (4).
Salvianolic acid is an active ingredient of
salvia miltiorrhiza Bge, which has multiple pharmacological
activities, such as improving microcirculation and eliminating free
radicals, exerting significant anti-atherosclerotic effects
(5–7). However, there are few studies on the
effects of salvianolic acid on collagen-induced RA. In this study,
the rat collagen-induced arthritis (CIA) was taken as the model to
investigate the impact of salvianolic acid on the arthritis of CIA
rats and to preliminarily discuss its influence on relevant
inflammatory mediators in rats.
Materials and methods
Materials and reagents
Salvianolic acid, bovine type II collagen, Freund's
complete adjuvant (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany);
enzyme-linked immunosorbent assay (ELISA) kit for tumor necrosis
factor-α (TNF-α), interleukin-6 (IL-6) and prostaglandin E2 (PGE2)
(Nanjing Jiancheng Bioengineering Institute, Nanjing, China);
bicinchoninic acid (BCA) protein assay kit and cell lysis buffer
(Beyotime Institute of Biotechnology, Nantong City, China);
hematoxylin and eosin (H&E) staining kit (Proteintech Group,
Wuhan, China); synthesis of TNF-α, IL-6 and PGE2 primers, reverse
transcription (RT) kit and quantitative polymerase chain reaction
(qPCR) kit (Takara, Dalian, China) were used in the present
study.
Preparation of collagen emulsion
Bovine type II collagen (5 mg) was dissolved in 25
ml acetic acid with a concentration of 0.1 mol/l, which was
prepared into solution with a concentration of 2 mg/ml, followed by
preservation in a refrigerator at 4°C overnight. After that, 2.5 ml
Freund's complete adjuvant was added to prepare the collagen
emulsion, which was stored in the refrigerator at 4°C until
use.
Laboratory animals and grouping
Thirty female rats (4 months old, 180–200g) were
randomly divided into the normal control group (n=10), CIA model
group (n=10) and Salvianolic Acid-CIA group (n=10). The models were
established in the endothelium of the right posterior toes from the
first day of model establishment. Rats in the normal control group
were injected with 0.1 ml normal saline, and rats in the CIA model
and Salvianolic Acid-CIA groups received injection of 0.1 ml
collagen emulsion. At 7 days after the model establishment,
equivalent dose of normal saline and collagen emulsion were
injected via the tail vein, respectively. At 21 days after the
model establishment, grouped drug administration was conducted, of
which 20 mg/kg salvianolic acid was administered by gavage to rats
in the Salvianolic Acid-CIA group, and 5 ml/kg normal saline was
given to rats in the normal control and CIA model groups. The
duration was 3 consecutive weeks. Rats were kept in cages with
controlled temperature and light cycles (24°C and 12/12 light
cycles) and with free access to water and water. The humidity was
60±10%.
The study was approved by the Ethics Committee of
The Second Affiliated Hospital of Harbin Medical University
(Harbin, China).
Detection of joint swelling degree of
CIA rats via water capacity method
A toe volumetric measuring instrument (YLS-7A, Shan-
dong Academy of Medical Science Device Station, Jinan, China) was
used to detect the swelling degree of the left posterior foot,
which was also known as secondary swelling; the detection was
conducted before model establishment and at 21, 28, 35 and 42 days
after the model establishment, and the swelling degrees were
calculated.
Measurement of contents of TNF-α, IL-6
and PGE2 via ELISA
The contents of TNF-α, IL-6 and PGE2 in the serum of
each group of rats were detected using ELISA. Experiments were
performed in strict accordance with the manufacturers protocol.
During the experiments, each sample was detected 3 times, and the
operation processes were repeated twice.
Detection of messenger RNA (mRNA)
expression levels of TNF-α, IL-6 and PGE2 via RT-PCR
The synovial tissue of the rat's joint in each group
was taken to extract total RNA. Viable total RNA was selected as
the template for synthesis of complementary DNA (cDNA) via reverse
transcription. Detailed PCR reaction conditions are: incubation at
42°C for 15 min and incubation at 95°C for 3 min, followed by
cooling on ice. The samples were then frozen in the refrigerator at
−80°C for use in subsequent experiments. Routine amplification was
conducted according to the primer sequences shown in Table I.
 | Table I.Primer sequences for RT-PCR of TNF-α,
IL-6 and PGE2 mRNAs. |
Table I.
Primer sequences for RT-PCR of TNF-α,
IL-6 and PGE2 mRNAs.
| Gene name | Primer sequences |
|---|
| TNF-α | F:
5′-TTTCGGGAACTAGACCTCTCACC-3′ |
|
| R:
5′-CTTCATGTCAGGCTTTCTGGATT-3′ |
| IL-6 | F: 5′-3′
CCCCCGAGACCTGAAAACCT |
|
| R: 3′-5′
AGTTCACCGTGGTAGTATTGTAGT |
| PGE2 | F:
5′-CCCACTCACCTGCTGCTACTC-3′ |
|
| R:
5′-AGAAGTGCTTGAGGTGGTTGTG-3′ |
Observation of synovial tissue
pathology via H&E staining
At the end of drug administration in the Salvianolic
Acid-CIA group, the rats were sacrificed after the blood was
collected from the orbit. The synovial tissue at the end of tibial
joint was taken out and fixed in neutral formalin with a volume
fraction of 4% for 48 h, followed by hydration, slicing and
staining in accordance with the H&E staining procedures.
H&E staining results of the rat synovial tissues in each group
were observed under an ordinary light microscope (Olympus, Tokyo,
Japan).
Statistical analysis
Data were presented as mean ± standard deviation and
processed using Statistical Product and Service Solutions (SPSS)
17.0 (SPSS, Inc., Chicago, IL, USA), and one-way analysis (ANOVA)
of variance with SNK post hoc test was conducted for statistical
analysis. P<0.05 was considered to indicate a statistically
significant difference.
Results
Measurement of swelling degree of
toes
At 21 days after the model establishment, there was
a significant difference in joint swelling degree in the rats' left
feet between the CIA model group as well as the Salvianolic
Acid-CIA and control groups (P<0.01), indicating that the models
were established successfully. Salvianolic acid was given at 21
days after the model establishment. The left foot joint swelling
degrees of the rats in the normal control, CIA model and
Salvianolic Acid-CIA groups were detected at 21 days after drug
administration. The results showed that there was significant
difference between the Salvianolic Acid-CIA group and CIA model
group (P<0.01) (Table II).
 | Table II.Comparison of joint swelling degrees
of the left posterior foot of three groups of rats (n=10). |
Table II.
Comparison of joint swelling degrees
of the left posterior foot of three groups of rats (n=10).
|
|
| Swelling degree of
the rats' left posterior foot after drug administration/ml |
|---|
|
|
|
|
|---|
| Groups | Swelling degree of
the left posterior foot at 21 days after model
establishment/ml | 7 days | 14 days | 21 days |
|---|
| Normal control
group | 0.12±0.05 | 0.16±0.07 | 0.19±0.09 | 0.21±0.08 |
| CIA model group |
1.20±0.18a |
1.28±0.16a |
1.32±0.17a |
1.33±0.19a |
| Salvianolic Acid-CIA
group |
1.19±0.20a |
0.97±0.19a,b |
0.89±0.20a,b |
0.77±0.18a,b |
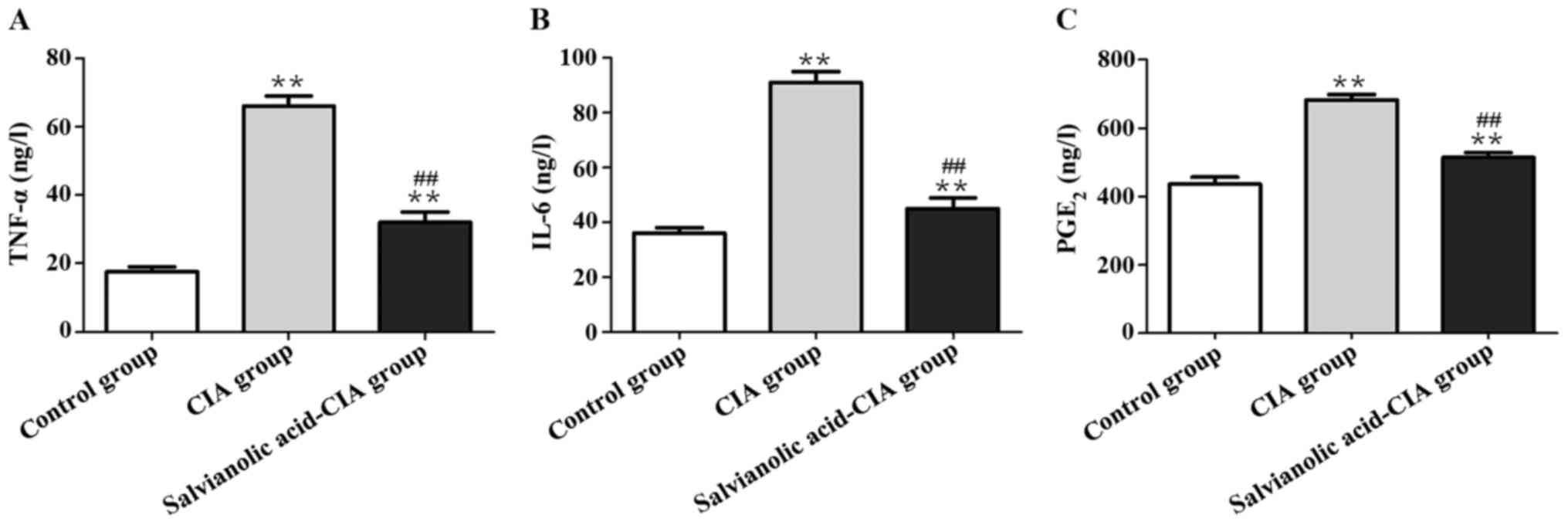
Effect of salvianolic acid on serum
TNF-α, IL-6 and PGE2 of CIA rats
As shown in Fig. 1,
the contents of TNF-α, IL-6 and PGE2 in the serum in the CIA model
group were significantly increased compared with those in the
control group (P<0.01). Contents of serum TNF-α, IL-6 and PGE2
in the Salvianolic Acid-CIA group were obviously lower than those
in the model group (P<0.01).
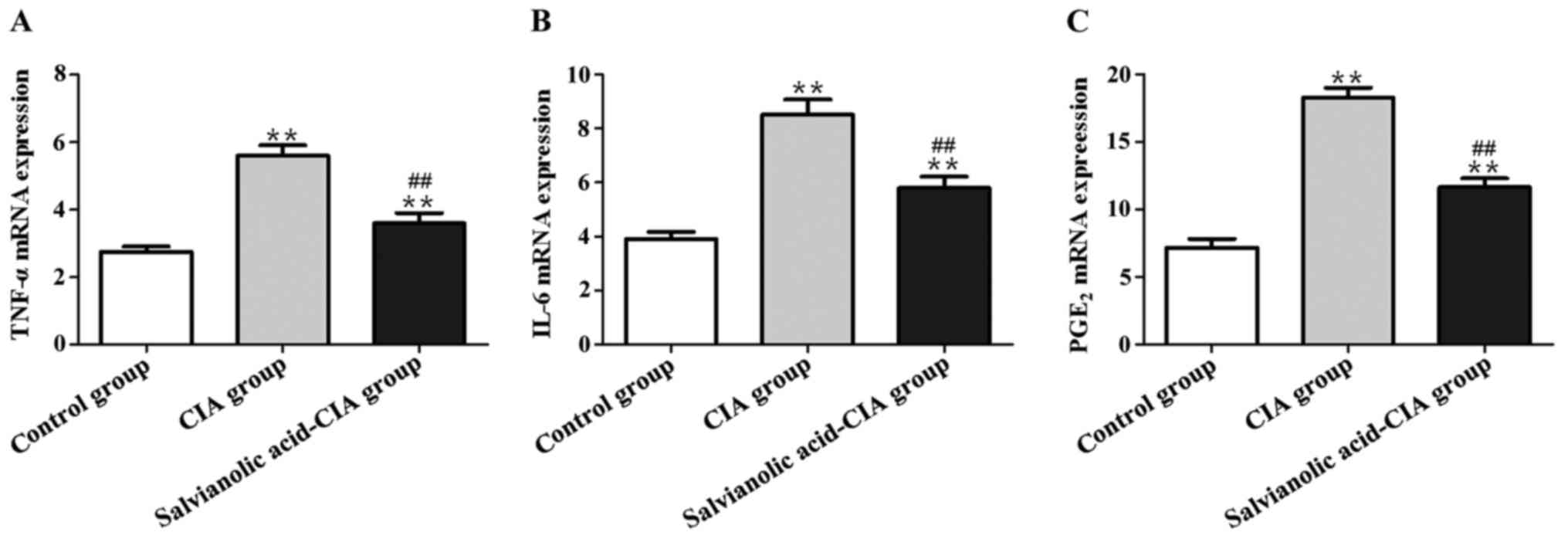
Effect of salvianolic acid on mRNA
expression levels of TNF-α, IL-6 and PGE2 in the synovial membrane
of CIA rats
As shown in Fig. 2,
the mRNA expression levels of TNF-α, IL-6 and PGE2 in the CIA model
group were notably elevated compared with those in the normal
control group (P<0.01). The mRNA expression levels of TNF-α,
IL-6 and PGE2 in the Salvianolic Acid-CIA group were obviously
decreased (P<0.01).
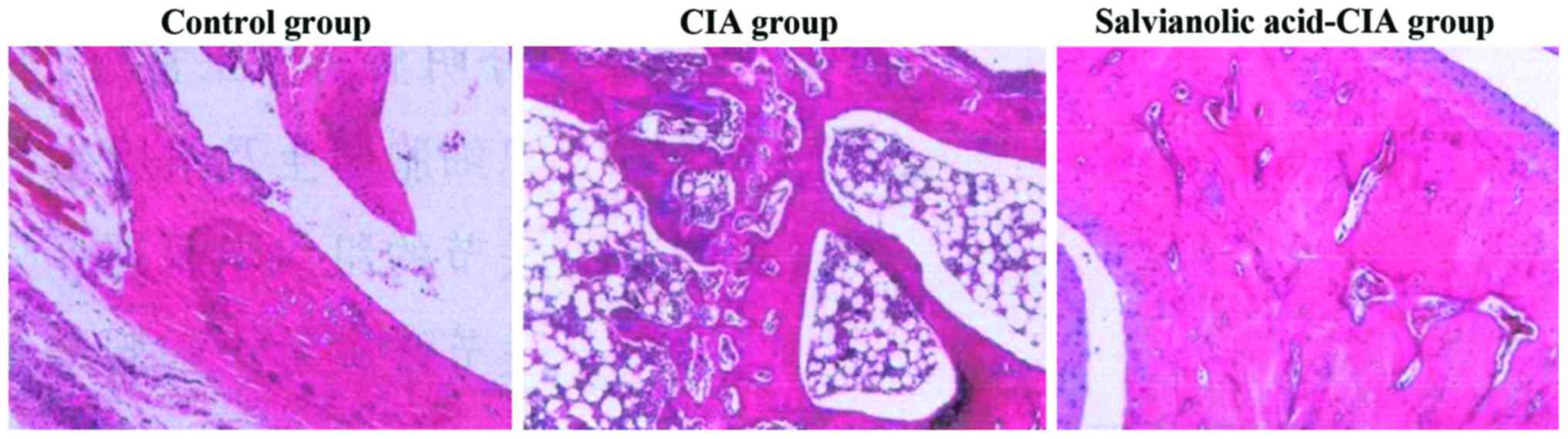
Effect of salvianolic acid on
pathology of joint synovial membrane of CIA rats
As shown in Fig. 3,
the H&E staining results showed that the synovial tissues in
the normal control group were arranged neatly, without hyperemia
and infiltration of inflammatory cells. However, the synovial
tissues in the CIA model group were arranged irregularly, with
infiltrating inflammatory cells. The hyperemia and infiltration of
inflammatory cells in the synovial tissues in the Salvianolic
Acid-CIA group were improved significantly.
Discussion
RA is a type of autoimmune disease, whose major
characteristic is chronic inflammation in the joint synovial
tissue, and the main pathological manifestations are pathological
hyperplasia of synovial cells associated with aggregation of
infiltrating inflammatory cells, of which the cartilage and its
lower-layer bone covered by the synovial membrane are involved
(8); therefore, the patients'
quality of life and even life are greatly threatened.
Inflammatory factors play vital roles in the
occurrence and progression of RA (9). Mainly secreted by the macrophages,
TNF-α is a crucial inflammatory factor for the inflammation of
synovial tissues. It is also a master switch for the activation of
inflammatory cascades in the body during the network regulation on
the occurrence of RA, which, not only triggers the mononuclear
macrophage to generate IL-l, IL-6 and other inflammatory factors
(10,11), but also causes a high expression of
chemokines by the vascular endothelial cells, thus leading to the
aggregation of inflammatory cells in the inflammatory sites of
synovial tissues (12). The
inflammatory factor IL-6 has complex functions and diversified
targets, which can induce the formation of pannus and bone
resorption in the progression of inflammation of the joints. In
osteoporosis, IL-6 can also promote inflammation, stimulate high
expression of acute phase proteins, induce anemia after the
formation of hemagglutinin, cause lassitude of the
hypothalamic-pituitary-adrenal (HPA) axis regulatory mechanisms and
finally lead to osteoporosis. In RA, the mechanism of action of
IL-6 is that it strengthens the activities of IL-1 and TNF-α and
induces the high expression levels of rheumatoid factor (RF) and
acute phase protein in the liver. Therefore, IL-6 is crucial to the
occurrence and development of RA (13). As a result, inhibiting the activity
and expression of IL-6 is the key to treating RA. The activity and
expression of PGE2, which is an important inflammatory mediator,
play vital roles in RA. Collagenase, PGE2 and other inflammatory
mediators can be synthesized and secreted by synovial fibroblasts
under the stimulation of TNF-α. However, the high expression of
PGE2 can damage the cartilage and its substratum (14,15).
Some studies have confirmed that the occurrence and progression of
RA is accompanied by the high expression of PGE2 in the serum and
partial inflammatory joint cavity, causing different degrees of
edema, pain and other inflammatory reactions (8,16).
Moreover, previous findings have indicated that whether PGE2 is
highly expressed is correlated with the extent of damage to the
articular cartilage and its substratum. Therefore, PGE2 plays a
promoting role in stimulating damage to articular cartilage
(17).
In this study, the CIA rats were taken as the model
to investigate the inhibitory effect of salvianolic acid on
inflammatory mediators of rats with collagen-induced RA. During the
experiments, the ankle joint swelling of rats in the model group
was obvious. After 3 weeks of drug administration, the ankle joint
swelling degree of rats in the Salvianolic Acid-CIA group was
alleviated compared with that in the model group. The ELISA results
showed that the contents of serum TNF-α, IL-6 and PGE2 in the
Salvianolic Acid-CIA group were obviously lower than those in the
model group. The RT-qPCR detection results indicated that the mRNA
expression levels of TNF-α, IL-6 and PGE2 in the Salvianolic
Acid-CIA group were markedly lower than those in the model group.
The H&E pathological sections showed that the hyperemia of rat
synovial tissues in the Salvianolic Acid-CIA group was obviously
relieved compared with that in the CIA model group, and the
infiltration of inflammatory cells was decreased. In similar
studies, it was found that mangiferin can ameliorate rats'
inflammations of the joints in the CIA model group, and the
inflammations can be alleviated by decreasing the expression levels
of TNF-α, IL-6, PGE2 and other inflammatory factors in the
articular tissues (18). Kamebaaurin
can lower the levels of nuclear factor kappa-light-chain-enhancer
of activated B cells (NF-κB), TNF-α, PGE2 and other inflammatory
factors in a dose-dependent manner to improve the status of rat
arthritis (19).
In conclusion, the models of CIA rats are
successfully replicated. Moreover, salvianolic acid has an
inhibitory effect on the RA of CIA model rats and can significantly
inhibit the expression levels of relevant inflammatory mediators,
such as TNF-α, IL-6 and PGE2.
Acknowledgements
Not applicable.
Funding
The present study was funded by the National Natural
Science Fund Project (grant no. 81202339) and Educating General
Projects of Heilongjiang Province (grant no. 11511238).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YS prepared collagen emulsion. DZ and ZL were
responsible fro animal preparation and grouping. XS and YL
performed ELISA. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Second Affiliated Hospital of Harbin Medical University
(Harbin, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nakayama H, Yaguchi T, Yoshiya S and
Nishizaki T: Resveratrol induces apoptosis MH7A human rheumatoid
arthritis synovial cells in a sirtuin 1-dependent manner. Rheumatol
Int. 32:151–157. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cha HS, Bae EK, Ahn JK, Lee J, Ahn KS and
Koh EM: Slug suppression induces apoptosis via Puma transactivation
in rheumatoid arthritis fibroblast-like synoviocytes treated with
hydrogen peroxide. Exp Mol Med. 42:428–436. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Firestein GS: Evolving concepts of
rheumatoid arthritis. Nature. 423:356–361. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen YH, Du GH and Zhang JT: Salvianolic
acid B protects brain against injuries caused by
ischemia-reperfusion in rats. Acta Pharmacol Sin. 21:463–466.
2000.PubMed/NCBI
|
|
5
|
Tang M, Feng W, Zhang Y, Zhong J and Zhang
J: Salvianolic acid B improves motor function after cerebral
ischemia in rats. Behav Pharmacol. 17:493–498. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tang MK and Zhang JT: Salvianolic acid B
inhibits fibril formation and neurotoxicity of amyloid beta-protein
in vitro. Acta Pharmacol Sin. 22:380–384. 2001.PubMed/NCBI
|
|
7
|
Cagnol S, Mansour A, Van
Obberghen-Schilling E and Chambard JC: Raf-1 activation prevents
caspase 9 processing downstream of apoptosome formation. J Signal
Transduct. 2011:8349482011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Funk JL, Oyarzo JN, Frye JB, Chen G, Lantz
RC, Jolad SD, Sólyom AM and Timmermann BN: Turmeric extracts
containing curcuminoids prevent experimental rheumatoid arthritis.
J Nat Prod. 69:351–355. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kiener HP, Watts GF, Cui Y, Wright J,
Thornhill TS, Sköld M, Behar SM, Niederreiter B, Lu J, Cernadas M,
et al: Synovial fibroblasts self-direct multicellular lining
architecture and synthetic function in three-dimensional organ
culture. Arthritis Rheum. 62:742–752. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ferreiro E, Baldeiras I, Ferreira IL,
Costa RO, Rego AC, Pereira CF and Oliveira CR: Mitochondrial- and
endoplasmic reticulum-associated oxidative stress in Alzheimer's
disease: From pathogenesis to biomarkers. Int J Cell Biol.
2012:7352062012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Car H, Zendzian-Piotrowska M, Fiedorowicz
A, Prokopiuk S, Sadowska A and Kurek K: The role of ceramides in
selected brain pathologies: Ischemia/hypoxia, Alzheimer disease.
Postepy Hig Med Dosw (Online). 66:295–303. 2012.(In Polish).
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang Y, Karakhanova S, Soltek S, Werner J,
Philippov PP and Bazhin AV: In vivo immunoregulatory properties of
the novel mitochondria-targeted antioxidant SkQ1. Mol Immunol.
52:19–29. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kehlen A, Thiele K, Riemann D and Langner
J: Expression, modulation and signalling of IL-17 receptor in
fibroblast-like synoviocytes of patients with rheumatoid arthritis.
Clin Exp Immunol. 127:539–546. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Elkholi R, Floros KV and Chipuk JE: The
role of BH3-only proteins in tumor cell development, signaling, and
treatment. Genes Cancer. 2:523–537. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
D'Orazio N, Gammone MA, Gemello E, De
Girolamo M, Cusenza S and Riccioni G: Marine bioactives:
Pharmacological properties and potential applications against
inflammatory diseases. Mar Drugs. 10:812–833. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ahmed S, Kwan K, Marotte H and Koch AE:
Regulation of prostaglandin E2 (PGE2)-induced
IL-6 production by epigallocatechin-3-gallate (EGCG) in rheumatoid
arthritis synovial fibroblasts. FASEB J. 22:2982008.http://www.fasebj.org/doi/abs/10.1096/fasebj.22.1_supplement.298.2
|
|
17
|
Akaogi J, Nozaki T, Satoh M and Yamada H:
Role of PGE2 and EP receptors in the pathogenesis of rheumatoid
arthritis and as a novel therapeutic strategy. Endocr Metab Immune
Disord Drug Targets. 6:383–394. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kumar IV, Paul BN, Asthana R, Saxena A,
Mehrotra S and Rajan G: Swertia chirayita mediated modulation of
interleukin-1beta, interleukin-6, interleukin-10, interferon-gamma,
and tumor necrosis factor-alpha in arthritic mice. Immunopharmacol
Immunotoxicol. 25:573–583. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lee JH, Choi JK, Noh MS, Hwang BY, Hong YS
and Lee JJ: Anti-inflammatory effect of kamebakaurin in in vivo
animal models. Planta Med. 70:526–530. 2004. View Article : Google Scholar : PubMed/NCBI
|