Introduction
Haemophilia is a rare hereditary disease. The knee
joint is a frequent bleeding site for patients with haemophilia.
The most important treatment to prevent knee joint bleeding among
patients with haemophilia is coagulation factor replacement therapy
(1,2). For patients who do not respond well to
conservative treatment and have recurrent bleeding, arthroscopic
synovectomy is an important treatment option (3,4). In
general, arthroscopic synovectomy is suitable for early haemophilic
arthropathy (3,4); however, in underdeveloped regions in
developing countries, it remains difficult to ensure early regular
continuous coagulation factor replacement therapy for patients with
haemophilia (5,6). Instead, the majority of adolescent or
young adult patients already have advanced haemophilic arthropathy
when they consult an orthopaedic surgeon for the first time
(6). For these patients, the most
important therapeutic goals are to decrease the frequency of joint
bleeding, relieve symptoms and delay knee joint arthroplasty as
much as possible.
Arthroscopic synovectomies performed at the
Department of Orthopaedic Surgery in The Second Affiliated Hospital
of Xi'an Jiaotong University (Xi'an, China) in 11 adolescent or
young adult patients with advanced haemophilic arthropathy between
January 2009 and January 2012. The present study retrospectively
evaluated the clinical outcomes of these cases and attempted to
determine whether arthroscopic synovectomy was effective for these
patients with advanced haemophilic arthropathy.
Materials and methods
Patients
The present study was approved by the Ethics
Committee of the Second Affiliated Hospital of Xi'an Jiaotong
University (approval no. 2008067). Written informed consent was
obtained from each patient prior to each surgical procedure as
wells as for the use of personal information for research purposes.
Clinical data was retrospectively collected from adolescent or
young adult patients with advanced haemophilic arthropathy who
underwent arthroscopic synovectomy between January 2009 and January
2012. A total of 11 patients were included in the present study
with a mean age of 18.73±5.55 years. Inclusion criteria were as
follows: i) Stage III or IV advanced haemophiliac arthritis; ii)
patients who had repeated joint bleeding and chronic pain following
conservative treatment; and iii) patients aged 12–34 years.
Exclusion criteria were as follows: i) Patients who had haemophilic
arthritis at early stages (I and II) or stage V; ii) patients aged
<12 or >34 years; and iii) patients who had contradictions
for this surgery. In this cohort, all patients were male. All
patients were negative for inhibitors. None of the patients had
concomitant diseases such as hepatitis B, hepatitis C, or other
viruses. X-ray staging of haemophilic arthropathy was based on
Arnold and Hilgartner's recommendations (7). Stage I did not exhibit skeletal
lesions, with only soft tissue swelling. Stage II exhibited
osteoporosis and overgrowth of the metaphysis of the joint. The
subchondral bone was intact, and the joint space was not invaded.
Stage III exhibited subchondral bone cyst formation, with a mild
narrowing of joint space. Stage IV exhibited more serious lesions,
with a disordered structure of subchondral bone, and a severely
narrowed joint space. Stage V had lost the joint space, and the
articular surface was severely damaged.
Surgical indications included: i) Repeated joint
bleeding that had no response following 3–6 months of conservative
treatment, including coagulation factor supplementation, physical
therapy, and rehabilitation; and ii) chronic pain caused by
haemophilic arthropathy which had no response to conservative
treatment.
Surgical contraindications included: Knee joint
infection, apparent axial malalignment (up to 5° varus or valgus)
(8), patellar subluxation, flexion
deformity >30°, active knee flexion <90° or severe knee joint
adhesions, particularly. when the patella was fixed on the
femur.
Preoperative preparation
Prior to surgery, patients underwent examinations of
their coagulation factor activity, prothrombin time, activated
partial thromboplastin time and inhibitor concentration. At 30 min
prior to surgery, coagulation factors were supplemented based on
patient body weight so that their activity was at 80–100%. In the
first week following the surgery, the concentration of the
coagulation factors was maintained at 60–80%. In the second week
following the surgery, the concentration of the coagulation factors
was maintained at 20–40%. Coagulation factor VIII (Hualan
Biological Engineering, Inc., Xinxiang, China) was intravenously
injected 2–3 times daily, and coagulation factor IX (Hualan
Biological Engineering, Inc.) was intravenously injected 1–2 times
daily according to the Expert Consensus in Perioperative Management
in Haemophilia Patients Undergoing Orthopaedic Surgery in China
(9). The perioperatively
administered volumes of coagulation factor VIII or IX for each
patient are summarised in Table
I.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Patient | Age (years) | Sex | Concomitant
disease | Factor
deficiency | Follow-up duration
(months) | Perioperative
administered factor volume (U) | Involved side |
|---|
| 1 | 13 | Male | No | IX | 70 | 29,000 | L |
| 2 | 22 | Male | No | VIII | 60 | 39,000 | R |
| 3 | 28 | Male | No | VIII | 80 | 37,800 | L |
| 4 | 23 | Male | No | IX | 76 | 25,400 | L |
| 5 | 12 | Male | No | VIII | 68 | 30,700 | L |
| 6 | 13 | Male | No | VIII | 70 | 38,000 | R |
| 7 | 16 | Male | No | VIII | 72 | 33,200 | R |
| 8 | 26 | Male | No | IX | 71 | 40,000 | L |
| 9 | 17 | Male | No | VIII | 74 | 32,500 | L |
| 10 | 21 | Male | No | VIII | 77 | 39,000 | R |
| 11 | 15 | Male | No | VIII | 73 | 34,000 | R |
Surgical procedures
The surgery was performed under general anaesthesia
via six arthroscopic approaches: Anterolateral, anteromedial,
lateral suprapatellar, medial suprapatellar, posterolateral and
posteromedial portal (10). A
complete total synovectomy was performed. In particular, it is
important to emphasise that the synovium of the posterior
compartment had to be resected. The surgery technique is the same
as that for routine total arthroscopic synovectomy. When necessary,
meniscus resection, articular cartilage debridement and adhesion
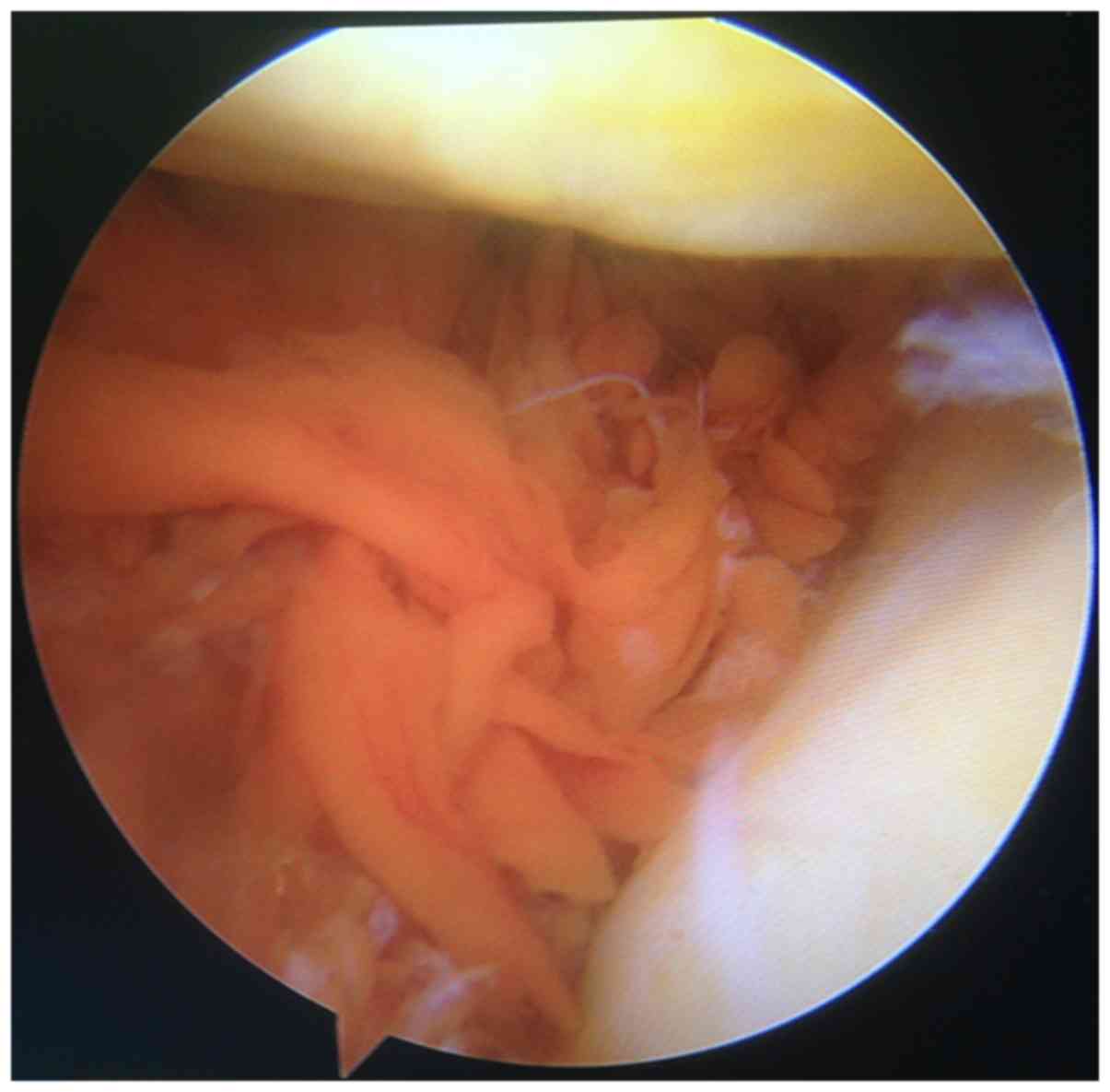
release could be simultaneously performed. For all 11 patients,
extensive synovial hyperplasia accompanied with the deposition of
iron-containing hemosiderin was visible via arthroscopy, and the
synovial hyperplasia even exhibited a nodular shape (Fig. 1). The suprapatellar bursa of 3
patients expanded abnormally to 2–3 times the normal volume due to
repeated bleeding in the joint cavity. In all patients, extensive
articular cartilage softening or even articular cartilage
full-thickness defects and subchondral bone exposure were visible.
In 2 cases, iron-containing hemosiderin deposition was observed on
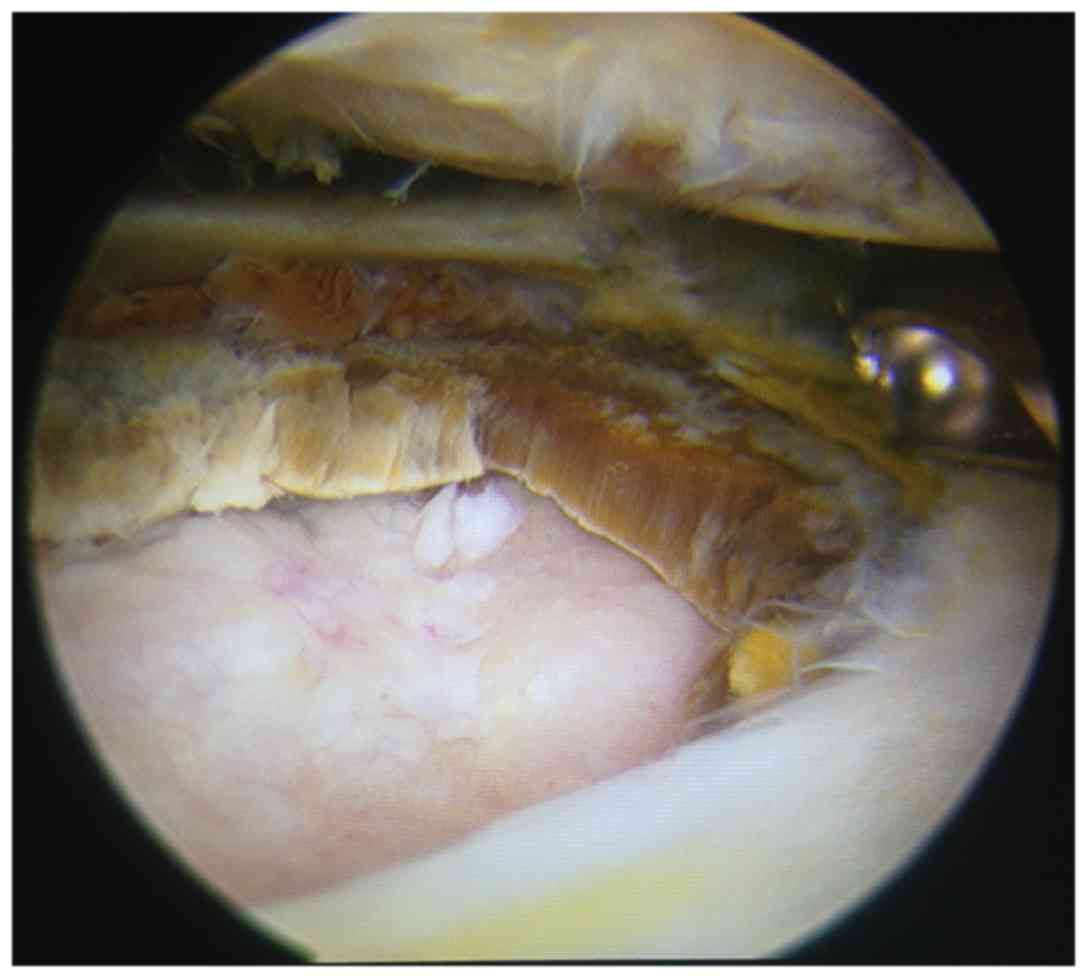
the surface of the damaged articular cartilage (Fig. 1). In 1 case, the articular cartilage
exhibited a brown colour and a brittle texture, appearing similar
to sugar cubes (Fig. 2). Obvious
adhesions in the joint cavity were not detected in any case. Prior
to the wound closure, a radiofrequency device was used to vaporise
the bleeding sites. A negative pressure drainage tube was placed
for 24–48 h. The knee was covered with ice and a bulky compression
dressing was applied.
Postoperative treatment
On the first postoperative day, the patient began
active knee joint exercise. If pain prevented active movement,
continuous passive motion machine functional exercise was
completed. Within 1 week following surgery, partial weight bearing
was permitted. The aim of postoperative rehabilitation exercise was
to maintain the range of motion of the knee to prevent stiffness
and maintain muscle strength.
Outcome measurements
The evaluated indicators included the frequency of
joint bleeding, range of motion (ROM), X-ray staging (11), hospital for special surgery (HSS)
knee score and HSS pain scores (12)
(Table II). A higher HSS pain score
suggested a lower level of pain. Clinical efficacy based on HSS
knee score was defined as the following: Excellent=≥85 points;
good=70–84 points; fair=60–69 points; or poor=≤59 points.
 | Table II.Effect of arthroscopic synovectomy on
ROM, radiographic stage, HSS pain score, HSS knee score and
frequency of joint bleeding. |
Table II.
Effect of arthroscopic synovectomy on
ROM, radiographic stage, HSS pain score, HSS knee score and
frequency of joint bleeding.
|
| ROM | Radiographic
stage | HSS pain score | HSS knee score | Frequency of joint
bleeding |
|---|
|
|
|
|
|
|
|
|---|
| Patient | Pre | Final | Pre | Final | Pre | Final | Pre | Final | Pre (n/month) | Final
(n/month) |
|---|
| 1 | 0/110 | 0/110 | IV | IV | 10 | 30 | 31 | 60 | 5 | 1 |
| 2 | 0/100 | 0/100 | IV | IV | 15 | 15 | 44 | 55 | 3 | 0 |
| 3 | 5/95 | 5/100 | IV | IV | 10 | 25 | 37 | 70 | 6 | 2 |
| 4 | 0/120 | 0/120 | IV | V | 20 | 25 | 62 | 80 | 6 | 3 |
| 5 | 0/120 | 0/120 | IV | IV | 15 | 30 | 47 | 79 | 4 | 2 |
| 6 | 0/90 | 0/100 | IV | IV | 15 | 25 | 50 | 75 | 2 | 0 |
| 7 | 5/110 | 5/110 | IV | V | 20 | 25 | 66 | 78 | 7 | 1 |
| 8 | 0/150 | 0/150 | IV | IV | 20 | 20 | 61 | 68 | 3 | 0 |
| 9 | 10/110 | 20/110 | IV | IV | 15 | 25 | 63 | 81 | 5 | 2 |
| 10 | 0/130 | 0/130 | IV | IV | 10 | 15 | 58 | 68 | 7 | 3 |
| 11 | 10/100 | 0/100 | IV | IV | 5 | 20 | 35 | 71 | 4 | 1 |
Statistical analysis
Qualitative data are expressed as numbers or
percentages. The normality of the data was assessed using the
Kolmogorov-Smirnov test. Normally distributed continuous data were
presented as means ± standard deviation and were compared using
paired Student's t-test. Non-normally distributed continuous data
were presented as the median and interquartile range and were
compared using the paired-sample Wilcoxon test. SPSS (version 11.0;
SPSS, Inc., Chicago, IL, USA) was used to analyse the data.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Patient characteristics
Of these 11 patients, 9 had haemophilia A with a
factor VIII level of <1%, and 2 patients had haemophilia B with
a factor IX level of <1%. All patients were negative for
inhibitors, and none of the patients were carriers of hepatitis B,
hepatitis C or other viruses. The X-ray staging of all cases
indicated a stage IV joint lesion (joint space narrowed severely)
and no patients exhibited apparent malalignment. The mean follow-up
time was 71.91 months (range, 60–80 months).
Frequency of joint bleeding and
ROM
At the end of the follow-up period, the mean
frequency of joint bleeding incidents per month decreased from 4.73
times preoperatively to 1.36 times postoperatively (P<0.05;
Table II). The ROM did not
significantly change (Table II).
The mean 2.7° of extension prior to surgery did not significantly
change by the final follow-up (data not shown). Prior to surgery,
the mean flexion was 112.3°, and the mean flexion was 113.6° at the
final follow-up (data not shown).
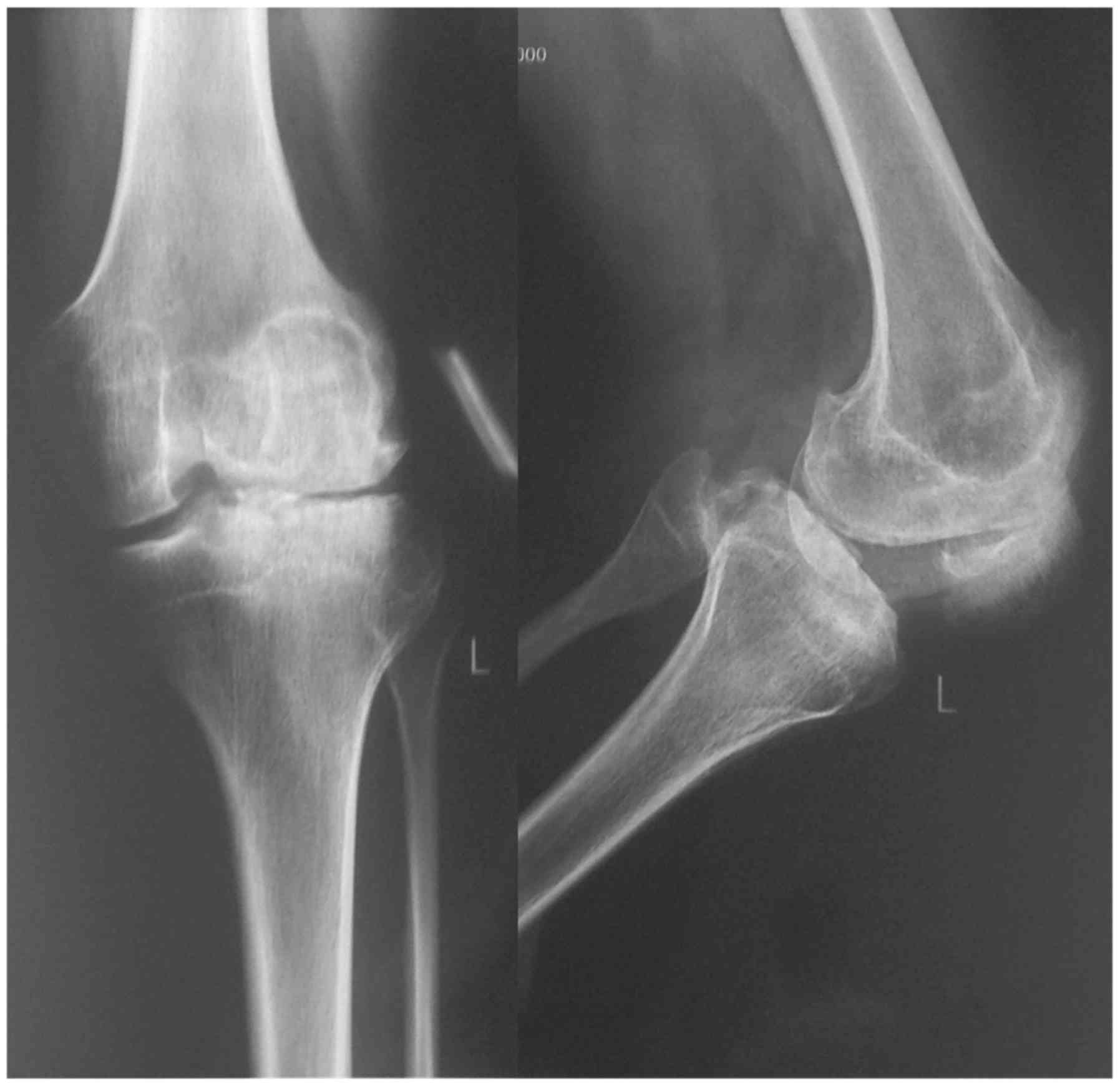
Radiographic outcomes
At the final follow-up visit, the radiographic stage
remained unchanged in 9 patients, whereas the remaining 2 cases
progressed from stage IV to stage V (Table II). No patients required total knee
arthroplasty through the end of follow-up. No joint infection,
delayed wound healing or non-healing was observed. Preoperative and
postoperative radiographs at the final follow up of a
representative case are presented in Figs. 3 and 4. The preoperative and postoperative
radiographs of this representative case are both stage IV based on
Arnold and Hilgartner's recommendations (11) and thus are similar, which suggest a
lack of joint lesion progress following surgery.
HSS score
The mean HSS score improved from 50.36 to 71.36
points at the final follow-up (P<0.05). The HSS pain scores for
the 11 patients significantly increased. The mean pain score prior
to treatment improved from 14.09 to 23.18 points at the final
follow-up visit (P<0.05; Table
II).
Complications
In 1 case, joint bleeding occurred in the week
following the surgery. Following joint aspiration followed by
pressure and bandage application, the symptoms were relieved.
Discussion
Arthroscopic synovectomy is an effective treatment
option for repeated joint bleeding that does not respond to
conservative treatment (12–16). This technique effectively reduces the
frequency of joint bleeding, improves pain, and even increases the
range of joint motion (3,8). For patients who are able to undergo
arthroscopic synovectomy, it is generally believed that their joint
lesions are mild and that the Arnold and Hilgartner X-ray staging
of haemophilic arthropathy should be stage I or II (3,17). In
addition, the current consensus is that arthroscopic synovectomy is
inappropriate for delaying the progression of joint lesions
(3,10,17).
However, arthroscopic synovectomy is not the gold standard for
haemophilic synovectomy. If radionuclides can be provided, then
radiosynovectomy is the first choice for haemophilic synovectomy
(8). However, when radiosynovectomy
treatment is ineffective or the supply of radionuclide is limited,
then arthroscopic synovectomy is a treatment option that should be
considered. A previous study has suggested that surgical resection
of the synovium should be considered when three consecutive
radiosynovectomies have failed (1).
Arthroscopic synovectomy for advanced haemophilic
knee joint arthropathy is controversial. In general, its efficacy
is considered poor for severe haemophilic arthropathy (8,17).
Instead, knee joint arthroplasty is generally recommended (4,10,13). The
efficacy of knee joint arthroplasty is certain; in fact, it can
greatly improve the quality of life of patients with haemophilic
knee arthropathy. For specific patient populations, however, the
final selection of the treatment strategy may differ following
comprehensively considering all the various factors (9,10).
At present, it is suggested that the only effective
method to prevent joint bleeding is to develop a systematic,
persistent coagulation factor supplementation programme soon
following birth of the haemophilic patient but prior to joint
bleeding occurs (3,5,6). Such a
programme would be expensive, and on-demand coagulation factor
treatment cannot be guaranteed in many parts of the world (5,6). For
example, in underdeveloped areas of western China, the prevention
and treatment of haemophilia remains far from perfect due to
economic, social and other factors (9,10). As
many patients do not obtain sufficient early supplementation of
coagulation factors, their knee joints have already suffered severe
damage during adolescence and young adulthood. The risk of bleeding
and infection associated with knee joint arthroplasty for
haemophilic arthropathy is greater than the corresponding risk for
knee joint arthroplasty among patients with osteoarthritis
(18–21). Furthermore, prosthetic survival of
knee joint prostheses for haemophilic arthropathy is worse than
that of prostheses for osteoarthritis (18–21).
Adolescent or young adult patients with advanced haemophilic knee
arthropathy may face complications associated with knee joint
arthroplasty, necessitating more than one revision arthroplasty in
their lifetimes if primary arthroplasty procedures are performed at
a younger age (18,20,22). If
arthroscopic synovectomy for advanced knee arthropathy can achieve
similar improvement in clinical manifestations as that of
arthroscopic synovectomy for early arthropathy, then patients may
have a few pain-free years with less bleeding, and primary knee
arthroplasty can also be delayed for these patients (22,23). For
such patients, this procedure would be of great value and worth
attempting, particularly for those who are considered to be too
young to undergo knee arthroplasty surgery.
A number of studies regarding arthroscopic
synovectomy for haemophilic arthropathy have also included some
cases of stage IV arthropathy. Yoon et al reported 28 cases
of arthroscopic synovectomy for haemophilic knee joints (24). Of these cases, the staging of six
knee joints was stage IV; however, the clinical results for the
stage IV arthropathy were not listed separately. In 1984, Wiedel
reported 5 cases of haemophilic arthroscopic synovectomy (including
2 cases of stage IV arthropathy) and suggested that all patients
achieved encouraging clinical results (6). For 1 case of stage IV arthropathy,
however, the postoperative range of motion did not meet
expectations, and manipulation was performed. In 1996, Wiedel
reported 9 cases of haemophilic arthroscopic synovectomy, and
patients were followed up for 10–15 years (17). These patients included 3 cases of
stage IV arthropathy, and 1 case of stage IV arthropathy that
progressed to stage V by the end of the follow up period. Of these
cases of stage IV arthropathy, 2 did not exhibit postoperative
recurrent bleeding events, but 1 case occasionally had recurrent
bleeding events. In addition, 1 patient with stage IV arthropathy
underwent total knee arthroplasty 8 years following synovectomy. Of
the 2 cases of stage IV arthropathy reported by Journeycake
(7), the postoperative range of
motion of 1 case was improved, whereas that of the other case did
not change. At present, no report has clinically studied
arthroscopic synovectomy to specifically focus on advanced
haemophilic arthropathy, to the best of our knowledge. In the
present study, a follow-up evaluation of arthroscopic synovectomies
was performed among adolescent or young adult patients with
haemophilic advanced knee arthropathy. The present study was
notable as it specifically focused on the arthroscopic synovectomy
of adolescent or young adult patients with advanced haemophilic
knee arthropathy, and the therapeutic significance and value of
arthroscopic synovectomy were primarily evaluated for these
patients with advanced joint lesions.
The present findings demonstrated that even among
patients with advanced haemophilic arthropathy, joint bleeding
frequency, pain degree and HSS scores significantly improved
following the arthroscopic synovectomy at the end of follow-up, and
a significant difference was identified compared with that prior to
the surgery. The frequency of joint bleeding was markedly decreased
in all cases. However, in case 10, joint bleeding occurred in the
week following the surgery. This may be due to surgical trauma and
inadequate intraoperative haemostasis. For this case, the symptoms
were relieved following joint aspiration followed by pressure and
bandage application. All patients exhibited improvement on HSS
scores. It was also noted that the pain degree of 2 cases remained
unchanged at the final follow-up visit, which is likely associated
with advanced joint lesions. The improvement in ROM was not
significant, which is likely because preoperative limitations in
ROM were not severe, and more aggressive postoperative
rehabilitation were not conducted to avoid early postoperative
joint bleeding. The results also demonstrated that the radiographic
staging of advanced haemophilic arthropathy was not improved
following synovectomy and that the staging of 2 cases even
progressed, which is consistent with the findings of Wiedel
(3,17). However, the deterioration of joint
radiographic staging is not necessarily associated with worsening
of clinical manifestations; the improvement of clinical
manifestation remains beneficial to patients.
X-ray imaging cannot assess changes in joint
effusion, or synovitis, nor can X-ray directly identify articular
cartilage, which can only be speculated indirectly based on the
narrowing of the joint space. Therefore, X-ray examination and
scoring are more suitable for haemophilic joints that have existing
bone changes (11,25). Magnetic resonance imaging (MRI) is
currently recognised as the gold standard for comprehensive
radiologic evaluation of joint changes. MRI, especially an MRI
scoring system for haemophilic arthropathy, allows us to observe
and record the degree of soft tissue involvement and osteochondral
involvement (25). However, for
patients with severe haemophilic knee arthropathy, it is not
necessary to have an overly detailed MRI evaluation, as a detailed
scoring difference cannot be associated with differences in
treatment strategy or therapeutic effect (25). Therefore, X-ray imaging is suitable
for assessing joint involvement among patients with previously
described severe haemophilic knee arthropathy with bone
changes.
The present study has several limitations. First, as
haemophilia is a rare disease, there were a small number of
patients recruited. Second, the follow-up period was relatively
short. A longer follow-up period is warranted to identify the mean
time from arthroscopic synovectomy to knee arthropathy, if knee
arthropathy is required.
In conclusion, the present findings suggest that
arthroscopic synovectomy is an effective treatment option to
decrease the frequency of bleeding and knee pain, improve knee
function and delay knee joint arthroplasty to a certain extent for
advanced haemophilic knee arthropathy in adolescent or young adult
patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TZ and XH conceived the study. TZ performed the
literature search and writing of the manuscript. SH and SX analysed
and interpreted the data. XH submitted the manuscript. HL and FZ
collected and assembled the data. All the authors have read and
approved the final submitted manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Second Affiliated Hospital of Xi'an Jiaotong
University (2008067; Xi'an, China). Written informed consent was
obtained from each patient prior to the surgical procedures and for
the use of personal information for research purposes.
Patient consent for publication
The subjects provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests
References
|
1
|
Rodriguez-Merchan EC: Prevention of the
musculoskeletal complications of hemophilia. Adv Prev Med.
2012:2012712012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Acharya SS: Exploration of the
pathogenesis of haemophilic joint arthropathy: Understanding
implications for optimal clinical management. Br J Haematol.
156:13–23. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wiedel JD: Arthroscopic synovectomy: State
of the art. Haemophilia. 8:372–374. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
De Kleijn P, Odent T, Berntorp E, Hilliard
P, Pasta G, Srivastava A, Iliescu A and Mohanty S: Differences
between developed and developing countries in paediatric care in
haemophilia. Haemophilia. 18 Suppl 4:S94–S100. 2012. View Article : Google Scholar
|
|
5
|
Kim HC, Klein K, Hirsch S, Seibold JR,
Eisele J and Saidi P: Arthroscopic synovectomy in the treatment of
hemophilic synovitis. Scand J Haematol Suppl. 40:271–279.
1984.PubMed/NCBI
|
|
6
|
Wiedel JD: Arthroscopic synovectomy in
hemophilic arthropathy of the knee. Scand J Haematol Suppl.
40:263–270. 1984.PubMed/NCBI
|
|
7
|
Journeycake JM, Miller KL, Anderson AM,
Buchanan GR and Finnegan M: Arthroscopic synovectomy in children
and adolescents with hemophilia. J Pediatr Hematol Oncol.
25:726–731. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Verma N, Valentino LA and Chawla A:
Arthroscopic synovectomy in haemophilia: Indications, technique and
results. Haemophilia. 13 Suppl 3:S38–S44. 2007. View Article : Google Scholar
|
|
9
|
Wang XF, Feng JM, Sun J, Hua BL, Chen L,
Chen F, Chen B, Zhao YQ, Weng X, Guo JF, et al: Expert consensus in
perioperative management in hemophilia patients undergoing
orthopedic surgery in China. Chin J Bone Joint Surg. 9:361–370.
2016.(In Chinese).
|
|
10
|
Ghosh K and Ghosh K: Management of
haemophilia in developing countries: Challenges and options. Indian
J Hematol Blood Transfus. 32:347–355. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Arnold WD and Hilgartner MW: Hemophilic
arthropathy. Current concepts of pathogenesis and management. J
Bone Joint Surg Am. 59:287–305. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Insall JN, Ranawat CS, Aglietti P and
Shine J: A comparison of four models of total knee-replacement
prostheses. J Bone Joint Surg Am. 58:754–765. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dunn AL, Busch MT, Wyly JB, Sullivan KM
and Abshire TC: Arthroscopic synovectomy for hemophilic joint
disease in a pediatric population. J Pediatr Orthop. 24:414–426.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rampal V, Odent T, Torchet MF, Rothschild
C, Elie C, Glorion C and Padovani JP: Surgical synovectomy of the
knee in young haemophiliacs: Long-term results of a monocentric
series of 23 patients. J Child Orthop. 4:33–37. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
de Almeida AM, de Rezende MU, Cordeiro FG,
Villaça PR, D'Amico EA, Hernandez AJ and Camanho GL: Arthroscopic
partial anterior synovectomy of the knee on patients with
haemophilia. Knee Surg Sports Traumatol Arthrosc. 23:785–791. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Triantafyllou SJ, Hanks GA, Handal JA and
Greer RB III: Open and arthroscopic synovectomy in hemophilic
arthropathy of the knee. Clin Orthop Relat Res. 196–204.
1992.PubMed/NCBI
|
|
17
|
Wiedel JD: Arthroscopic synovectomy of the
knee in hemophilia: 10-to-15 year followup. Clin Orthop Relat Res.
46–53. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rodriguez-Merchan EC: Special features of
total knee replacement in hemophilia. Expert Rev Hematol.
6:637–642. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Poenaru DV, Patrascu JM, Andor BC and Popa
I: Orthopaedic and surgical features in the management of patients
with haemophilia. Eur J Orthop Surg Traumatol. 24:685–692. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Norian JM, Ries MD, Karp S and Hambleton
J: Total knee arthroplasty in hemophilic arthropathy. J Bone Joint
Surg Am. 84-A:1138–1141. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cohen I, Heim M, Martinowitz U and
Chechick A: Orthopaedic outcome of total knee replacement in
haemophilia A. Haemophilia. 6:104–109. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rodriguez-Merchan EC and Gomez-Cardero P:
Arthroscopic knee debridement can delay total knee replacement in
painful moderate haemophilic arthropathy of the knee in adult
patients. Blood Coagul Fibrinolysis. 27:645–647. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Al-Omran AS and Sadat-Ali M: Arthroscopic
joint lavage in osteoarthritis of the knee. Is it effective? Saudi
Med J. 30:809–812. 2009.PubMed/NCBI
|
|
24
|
Yoon KH, Bae DK, Kim HS and Song SJ:
Arthroscopic synovectomy in haemophilic arthropathy of the knee.
Int Orthop. 29:296–300. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nuss R, Kilcoyne RF, Geraghty S, Wiedel J
and Manco-Johnson M: Utility of magnetic resonance imaging for
management of hemophilic arthropathy in children. J Pediatr.
123:388–392. 1993. View Article : Google Scholar : PubMed/NCBI
|