Introduction
Under normal circumstances, pain is a protective
reaction in the body. Pain response can lead to a series of
reflexes to avoid damage (1).
However, in neuropathic pain, due to damage or disturbance in a
certain part of the reflex, such as the sensory system and central
nervous system, the pain threshold is reduced, resulting in
over-sensitive pain sensation caused by various stimuli, and even
without any external stimulus, spontaneous pain would also be
produced. This continuous intense pain causes great pressure on
patients and also brings a series of stress changes to the body
(2). The expression levels of the
inflammatory cytokines TNFα and IL-1β are significantly elevated in
chronic constriction injury (CCI) models, whereas TNFα is
neurotoxic in the central nervous system (3). Neuropathic pain can be caused by a
variety of factors, such as infection and spinal cord injury.
Incidence of neuropathic pain is as high as 7%, but the specific
pathogenesis is not yet clear, and there is currently no effective
treatment (4).
Histone deacetylase 2 (Hdac2) is widely present in
eukaryotic organisms and plays an important role in the
proliferation and differentiation of cells and in the homeostasis
of the body. Acetylation plays an irreplaceable role in
inflammation and sensitization of chronic pain (5). Acetylation can open the chromatin
structure, activate transcription sites, increase gene expression,
and Hdac2 deacetylation can cause the polycondensation of
chromatin, inhibit transcription of related genes, and promote the
occurrence of neuropathic pain (6).
Inpp5f (Sac2), namely inositol 4-phosphatase, has inositol
tetra-phosphate (PI4P) as its substrate. Phosphoinositides (PIs)
are metabolites produced by the phosphorylation of
phosphatidylinositol at the inositol 3,4,5 positions. PIs are key
regulatory phospholipids located in cell membranes, which can
regulate cell signal transduction, membrane transport, cytoskeleton
and lipid balance. Phosphorylation of PI4P affects the function of
synaptic binding proteins which use PI4P as a substrate, thereby
affecting the transport of synaptic vesicles to the synaptic active
area and inhibiting the transmission of pain signals in neuropathic
pain (7,8).
Pregabalin can agonize γ-aminobutyric acid (GABA)
receptors, thereby interrupting voltage-dependent calcium channels
and inhibiting neurotransmitter release in synaptic vesicles.
Pregabalin therefore does not exert anti-inflammatory effects and
does not affect physiological pain (9). Clinically, pregabalin is often used for
the treatment of pathological pain in peripheral nerves and for the
adjuvant treatment of locali-zed epilepsy (10). This study explored the effect of
pregabalin on neuropathic pain in CCI rats by measuring the
expression levels of Hdac2 and Inpp5f, so as to explore its
pathogenesis and provide possible targets for related drugs.
Materials and methods
Materials
A total of 90 healthy, specific pathogen-free clean
grade male Sprague-Dawley rats aged 2 months and weighing 200±20 g
were provided by Shanghai Sleek Laboratory Animal Co., Ltd.,
Shanghai, China [SCXK (Shanghai) 2012-0002]. The rats were kept in
cages with free access to food and water and temperature was
maintained at 23°C. There was a 12/12 h light/dark cycle and
humidity was 60±10%. A tactile pain measuring instrument was
provided from Friends Honesty life Sciences Company Limited
(Beijing, China). A tail-flick foot tester was purchased from
Shanghai Yuyan Instruments Co., Ltd. (Shanghai, China). Pregabalin
was provided by Shanghai Shifeng Biological Technology Co., Ltd.
(Shanghai, China). A UV spectrophotometer MD1000 was purchased from
Beijing Thmorgan Biotecnology Co., Ltd. (Beijing, China). TRIzol
reagent was purchased from (Shanghai Mingjing Biotechnology Co.,
Ltd. (Shanghai, China). Reverse transcription kit was purchased
from Thermo Fisher Scientific (China) Co., Ltd. (Shanghai, China).
PCR kit was purchased from Beijing ComWin Biotech Co., Ltd.
(Beijing, China). ELISA kit was provided by Wuhan Moshake Biotech
Co., Ltd. (Wuhan, China) and Primer sequences were purchased from
Sangon Biotech (Shanghai) Co., Ltd. (Shanghai, China).
The study was approved by the Ethics Committee of
The Fifth Hospital of Wuhan (Wuhan, China).
Model establishment and grouping
SD rats were randomly divided into 3 groups: the
treatment group, the model control group and the normal control
group (30 in each group). The normal control group was treated with
sham operation. The treatment and model control groups were
subjected to CCI modeling based on Bennett method (11). Each rat was weighed and given an
intraperitoneal injection of 10% chloral hydrate at a dose of 200
mg/kg for anesthesia. The surgical area was disinfected with 75%
ethanol, and the skin parallel to the upper side of the femur was
incised. The muscles and sciatic nerves were bluntly separated. The
fork of the sciatic nerve was found and was ligated with 4-0 silk
thread at 5 cm above the site (the normal control group was not
ligated after separating nerves). Four ligations with an interval
of 1 cm were made. Ganglion subsidence but unblocked outer membrane
blood flow was the standard. Incision was closed layer by layer and
the muscles and skin were sutured. Injection of penicillin at a
dose of 80,000 IU was performed. Mechanical withdrawal threshold
(MWT) and thermal withdrawal latency (TWL) were measured 1 week
after operation. MWT decline of >40% was regarded as a
successful modeling. Modeling was successful in 28 out of 30 rats
(93.33%) in the treatment group and in 27 out of 30 rats (90.00%)
in the model control group. Rats in the treatment group were
weighed on the 8th day after operation and pregabalin was given by
gavage at a dose of 3 mg/kg. Rats in the model control group
received the same volume of normal saline. MWT and TWL of the rats
in the three groups were detected before and at approximately 10 am
at 7, 10, 14, and 21 days after modeling. Behavioral test was
completed and all rats were sacrificed by decapitation at 21 days
after operation. Lumbar enlargement tissue was isolated from the
lumbar spinal cord.
MWT assay
MWT of the rats in the three groups was detected
before and at approximately 10 am at 7, 10, 14, and 21 days after
modeling. Rats were placed on test bench for 30 min and a pressure
sensor was used to prick the middle of the forefoot of rats
vertically. The stimulation was performed slowly and uniformly to
avoid disturbing rats. Paw withdrawal reactions and tail flick
reactions were positive reaction, and the number of grams on the
electronic display screen at this time-point was MWT. The left and
right paws of rats were tested alternately and measurement was
performed once every 5 min and was repeated three times. The
average value was calculated.
TWL determination
TWL of the rats in three groups were detected before
and at approximately 10 am at 7, 10, 14, and 21 days after
modeling. The rats were placed in a plexiglass box for 15 min
before the test. A halogen spotlight was used to vertically
illuminate the hind paw of the rat. Leg withdrawing and reaction
evading were positive reactions and the timing at this time-point
was TWL. The left and right paws of the rats were tested
alternately and measurement was performed once every 5 min and was
repeated three times. The average value was calculated.
Detection of inflammatory factors by
ELISA
Enlarged lumbar spinal cord tissues in each group
were extracted to grind and homogenize and diluted 30-fold, and the
content of inflammatory factors was detected by ELISA according to
the manufacturer's instructions of TNFα and IL-1β ELISA.
Determination of Hdac2 and Inpp5f mRNA
by RT-qPCR
Enlarged lumbar spinal cord tissues were subjected
to total RNA extraction using TRIzol reagent according to the
manufacturer's instructions. A micro-ultraviolet spectrophotometer
was used to measure the concentration and purity of SYBR-Green
(Thermo Fisher Scientific, Inc., Waltham, MA, USA) and A260/A280
ratio should be between 1.8 and 2.0. Reverse transcription was
performed using a 20 µl reaction system in strict accordance with
the manufacturer's instructions. Reaction conditions were: 37°C for
45 min and 95°C for 5 min. The synthesized cDNA was performed using
a 20 µl amplification system in accordance with the instructions of
RT-qPCR kit. Reaction conditions were: 95°C for 10 min, followed by
40 cycles of 95°C for 10 sec, 60°C for 20 sec and 72°C for 10 sec,
and then 72°C for another 5 min. Primers used in PCR reactions
were: 5′-GTGGGGCGCCCCAGGCACCA-3′ (forward) and
5′-CTCCTTAATGTCACGCACGATTTC-3′ (reverse) for β-actin;
5′-TGACATTGTGCTTGCTGTCC-3′ (forward) and 5′-CCCTCAAGTCTCCTGTTCCA-3′
(reverse) for Hdac2; 5′-GGAGGCCACTTGTGTAGAT-3′ (forward) and
5′-GGAGGCCACTTGTGTAGAT-3′ (reverse) for Inpp5f. Data were processed
using 2−∆∆Cq method (12).
Statistical analysis
Data were processed using SPSS 19.0 (Asia Analytics
Formerly SPSS China) software package. MWT and TWL values, and the
content or expression of related substances were expressed as mean
± standard deviation. According to data distribution
characteristics, comparisons among three or more groups were
compared by analysis of variance followed by Dunnetts test as a
post hoc test. Intragroup comparisons were performed by repeated
measurement analysis of variance. The significance level was
α=0.05.
Results
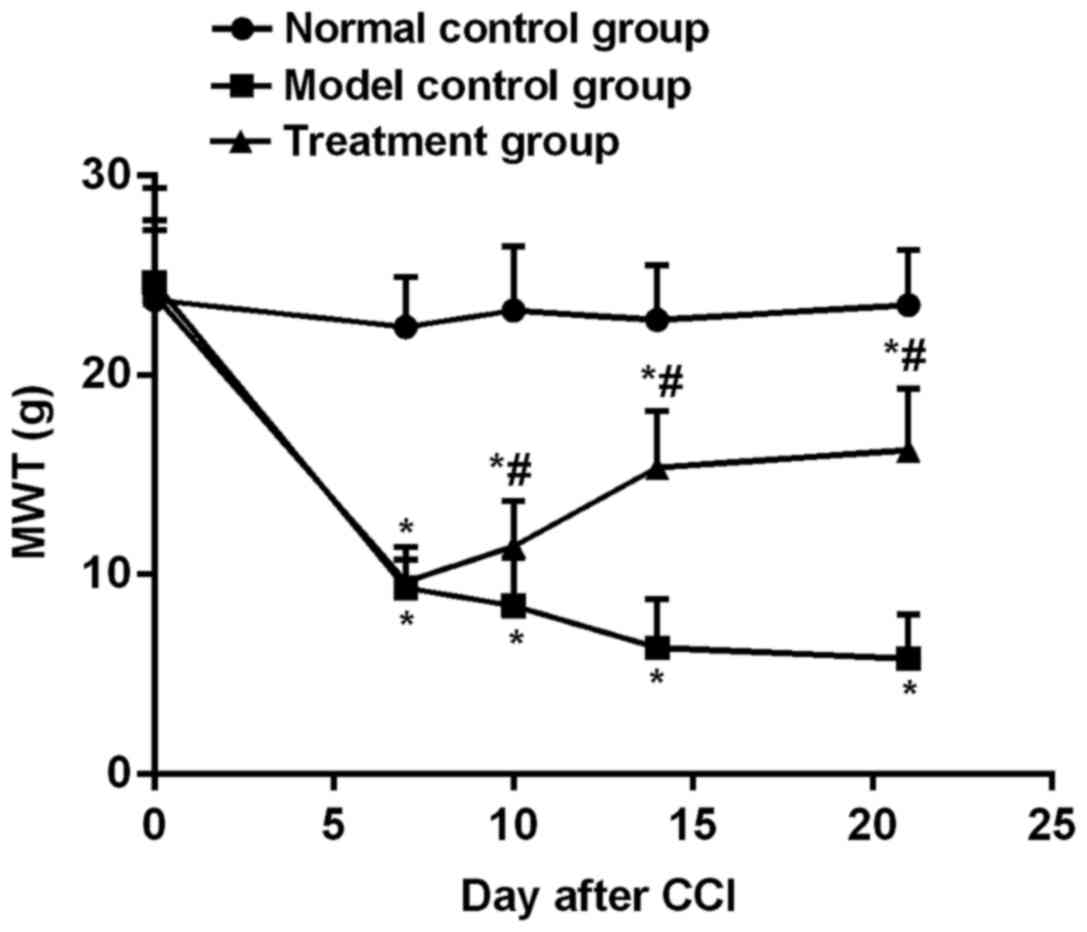
Changes in MWT of rats in each
group
Before modeling, MWT values of the normal control,
model control and treatment groups were 23.76±3.51, 24.65±4.73, and
24.01±3.76 g, respectively, and no significant differences were
found among the three groups (P>0.05). At 7 days after modeling,
MWT values of the normal control, model control and treatment
groups were 22.41±2.51, 9.34±1.42, and 9.63±1.76 g, respectively.
MWT of the treatment and model control groups was lower than that
of the normal control group (P<0.05). There was no difference in
the MWT between the treatment and model control groups (P>0.05).
Intragastric administration of drug was performed at 8 days after
operation. On the 10th, 14th and 21st days after modeling, MWT of
the treatment group was higher than that of the model control
group, but lower than that of the normal control group (P<0.05).
MWT was at a relatively stable level in the normal control group at
7–21 days after operation (Fig.
1).
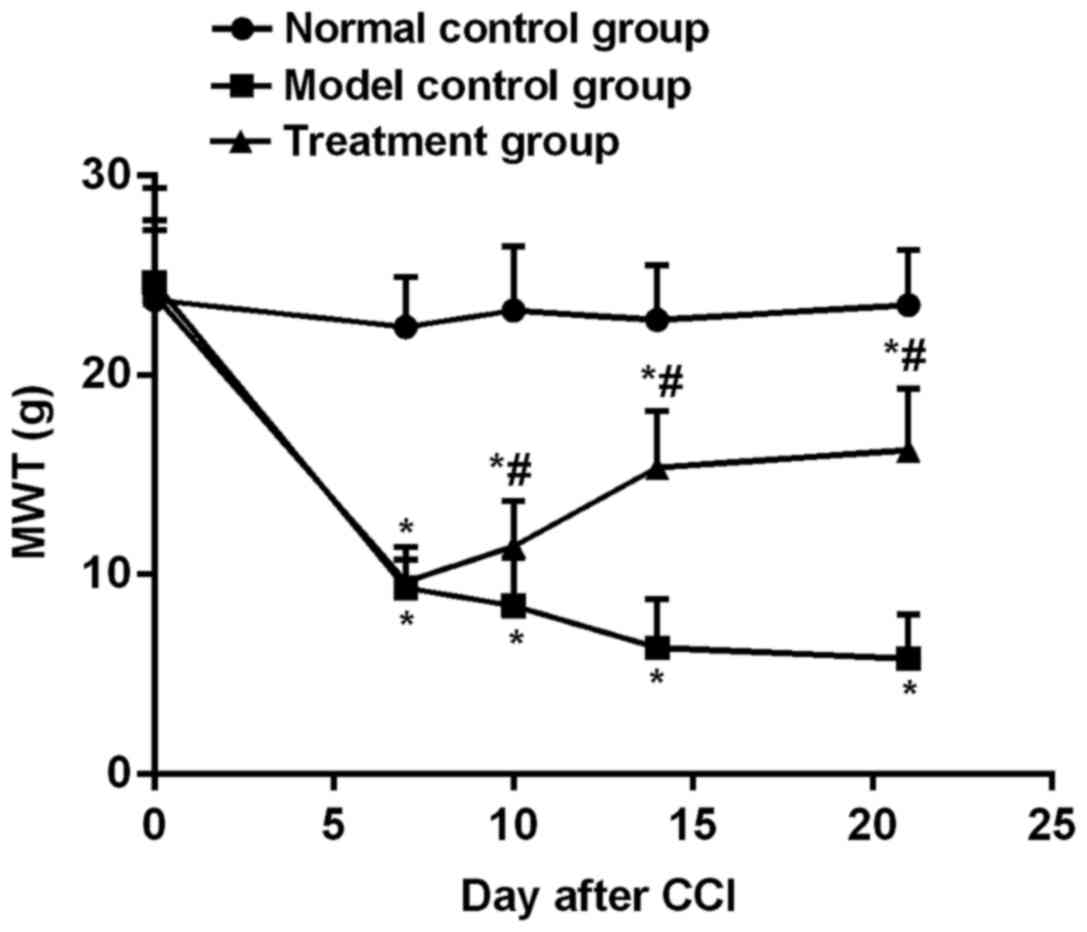 | Figure 1.MWT changes in each group. Before the
modeling, there was no significant difference in MWT among the
normal control, model control and treatment groups (P>0.05).
After 7 days, the treatment and model control groups showed a
significantly lower MWT compared with the normal control group
(P<0.05), and there was no difference in MWT between the
treatment and model control groups (P>0.05). Intragastric
administration of drug was performed at 8 days after operation. On
the 10th, 14th and 21st days after modeling, MWT of the treatment
group was higher than that of the model control group, but lower
than that of the normal control group (P<0.05). MWT is at a
relatively stable level in the normal control group at 7–21 days
after operation, but MWT increased in the treatment group and
decreased in the model control group. *P<0.05, compared with the
normal control group; #P<0.05, compared with the
model control group. |
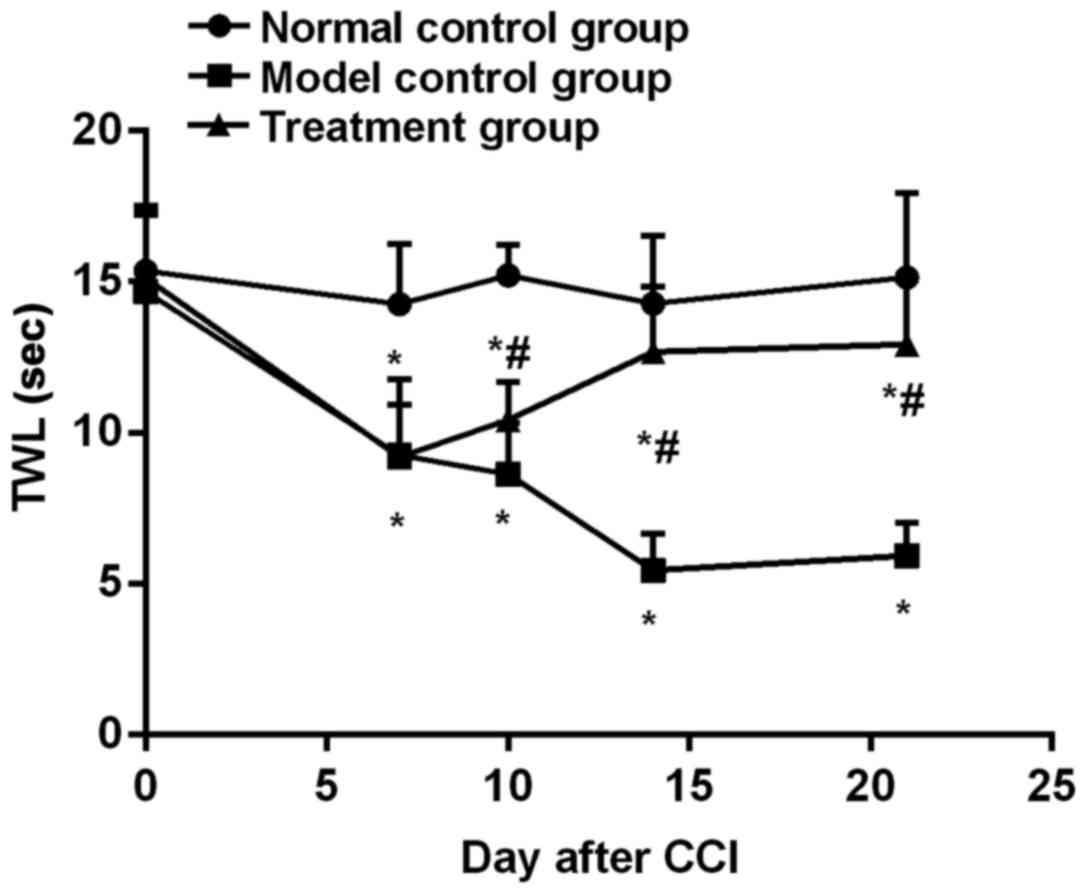
Changes in TWL of rats in each
group
Before modeling, TWL values of the normal control,
model control and treatment groups were 15.35±2.15, 14.68±2.52, and
15.12±2.21 g, respectively, and there was no statistical difference
in TWL among the three groups (P>0.05). At 7 days after
operation, values of MWT in the normal control, model control and
treatment groups were 14.25±2.01, 9.25±2.51, and 9.19±1.76 g,
respectively. After operation, TWL gradually decreased in the model
control group and increased gradually in the treatment group until
the 21st day. Compared with the level to that at 7 days, TWL
increased significantly at 21 days (P<0.01). TWL was always
shorter in the treatment group than in the normal control group
(Fig. 2).
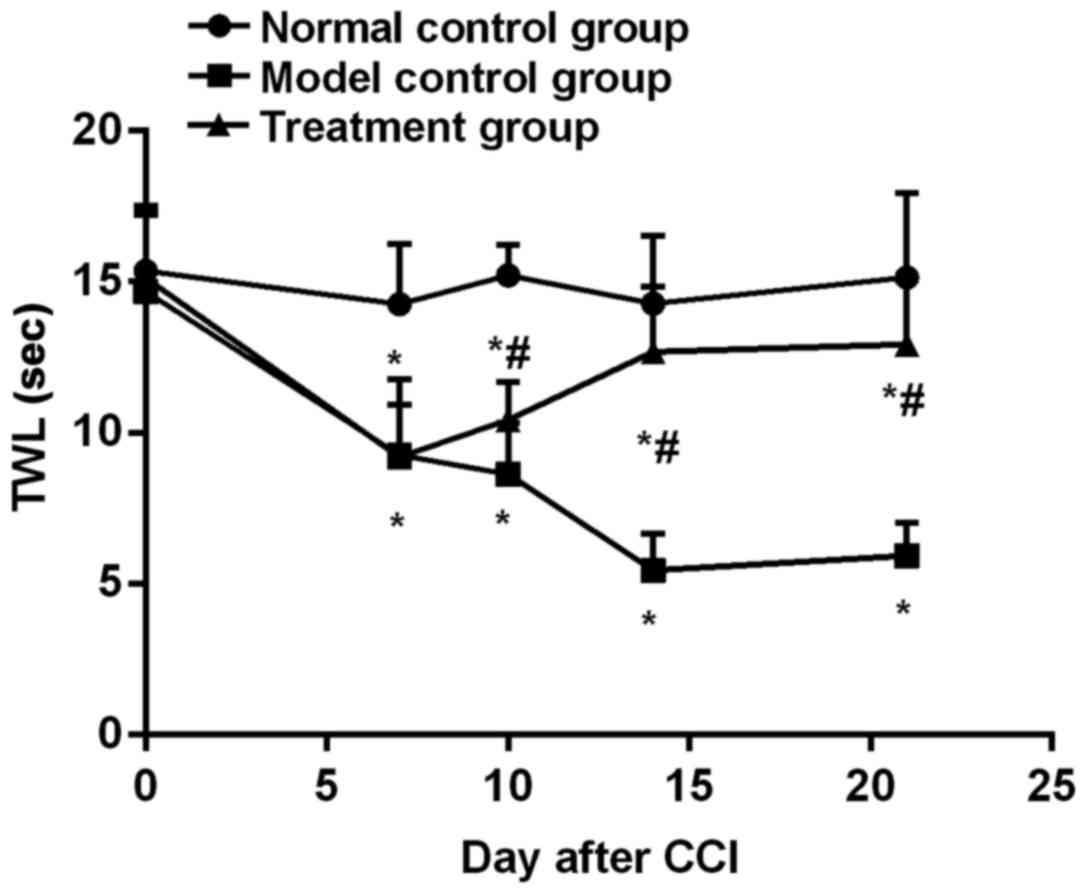 | Figure 2.Changes of TWL in the rats of each
group. Before modeling, TWL values of the normal control, model
control, and treatment groups were 14.25±2.01, 9.25±2.51, and
9.19±1.76 g, respectively, and there was no statistical difference
in TWL among the three groups (P>0.05). At 7 days after
operation, TWL gradually decreased in the model control group and
increased gradually in the treatment group until the 21st day.
Compared with the level to that at 7 days, TWL increased
significantly at 21 days (P<0.01). TWL is always shorter in the
treatment group than in the normal control group (P<0.05).
*P<0.05, compared with the normal control group;
#P<0.05, compared with the model control group. |
ELISA detection of TNFα and IL-1β
At 21 days after operation, TNFα and IL-1β contents
in enlarged lumbar spinal cord tissues from each group were
measured. The levels of TNFα and IL-1β in the model control and
treatment groups were higher than those in the normal control
group. The levels of TNFα and IL-1β in the treatment group were
lower than those in the model control group (P<0.05) (Table I).
 | Table I.The content of TNFα and IL-1β in
enlarged lumbar spinal cord tissues at 21 days after operation. |
Table I.
The content of TNFα and IL-1β in
enlarged lumbar spinal cord tissues at 21 days after operation.
| Groups | TNFα (pg/mg) | IL-1β (pg/mg) |
|---|
| Normal control | 27.42±4.75 | 55.12±9.13 |
| Model control |
54.24±7.86a |
110.86±16.31a |
| Treatment |
39.42±6.32a,b |
78.82±12.42a,b |
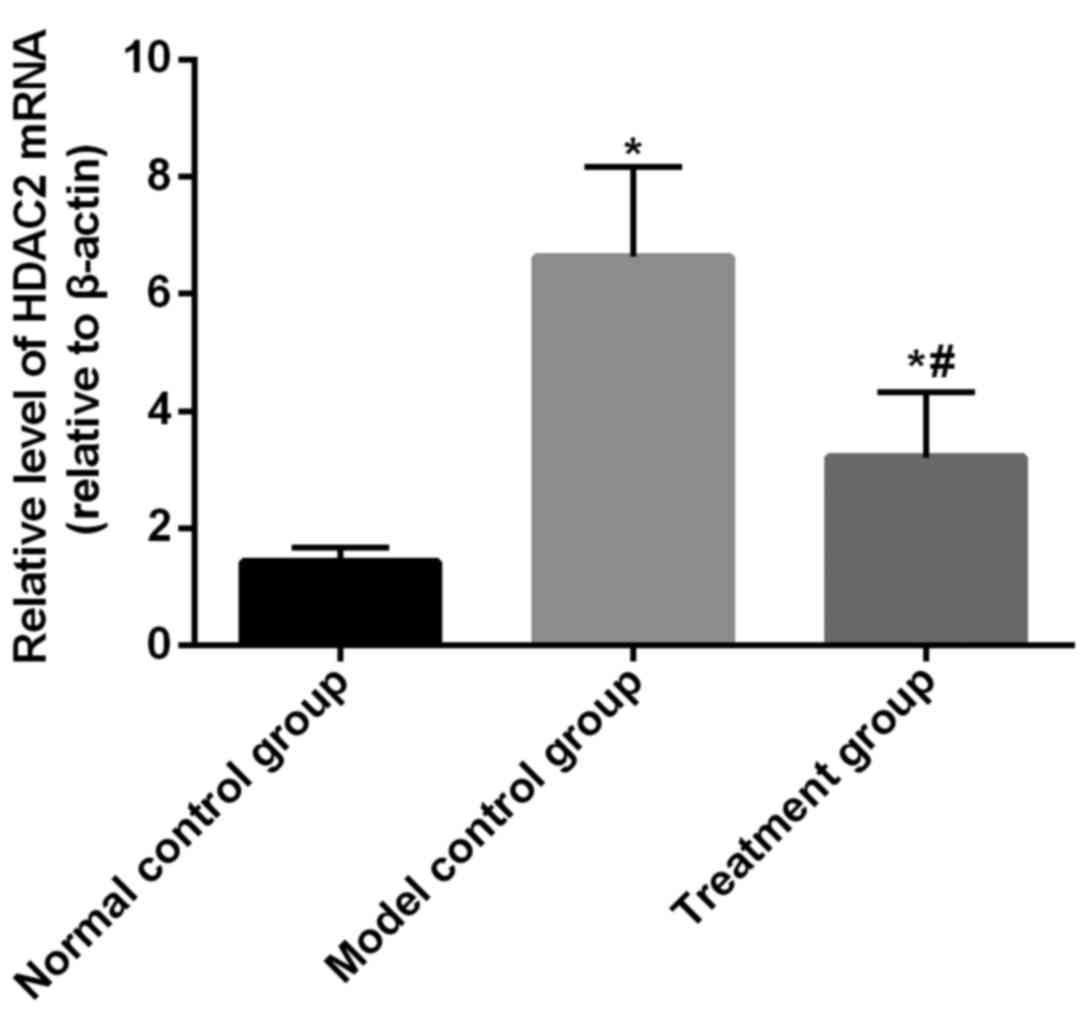
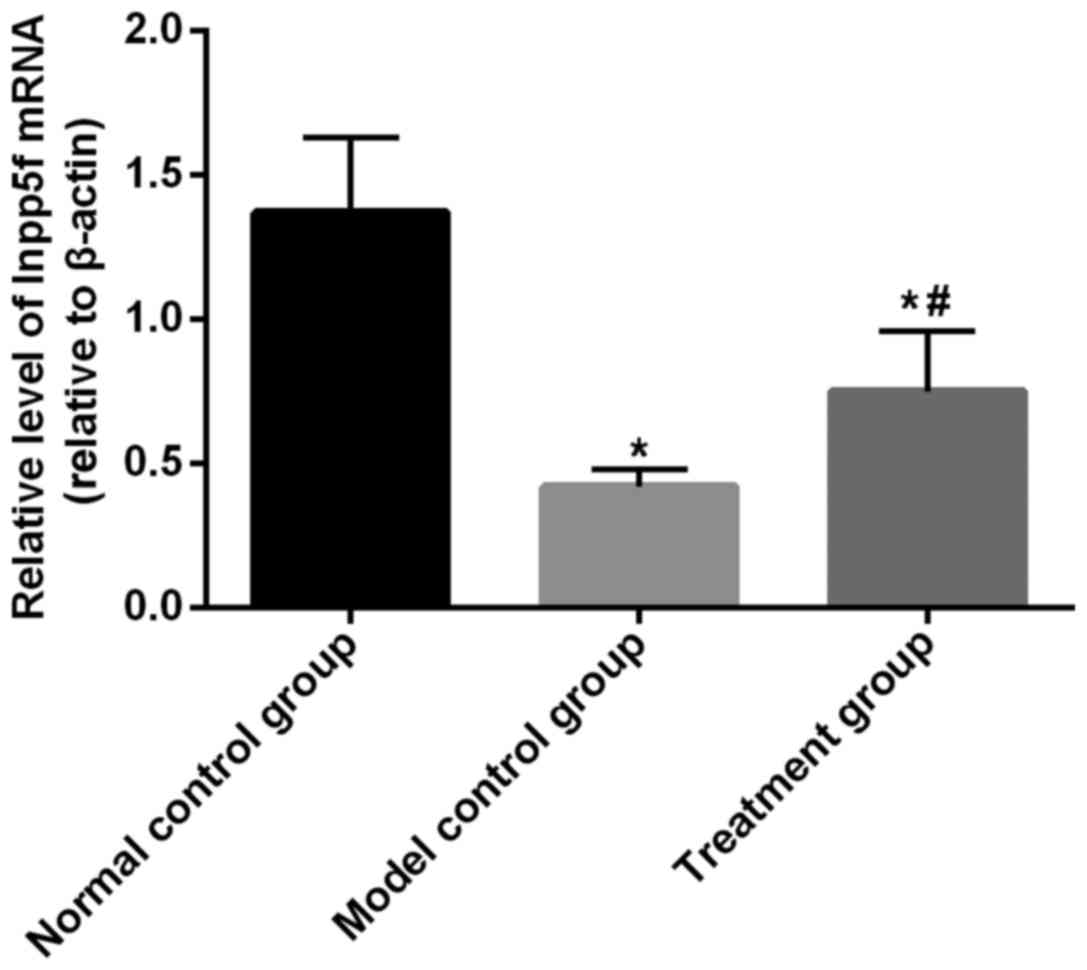
Determination of Hdac2 and Inpp5f mRNA
by RT-qPCR
The expression of Hdac2 and Inpp5f mRNA was detected
in lumbar enlargement tissues of each group at 21 days after
operation. The expression level of Hdac2 in the normal control
group (1.43±0.24) and treatment group (3.21±1.11) was significantly
lower than that in the model control group (6.64±1.54). The
expression level of Hdac2 in the treatment group was significantly
higher than that in the normal control group (P<0.05, Fig. 3). The expression level of Inpp5f mRNA
in the treatment group (0.75±0.21) and normal control group
(1.37±0.26) was significantly higher than that in the model control
group (0.42±0.06, P<0.05), but the expression level of Inpp5f
mRNA was lower in the treatment group than in the normal control
group (P<0.05, Fig. 4).
Discussion
Neuropathic pain is the pain sensitization resulting
from nervous system injury caused by a variety of complex factors
and spontaneous pain is produced, which brings great harm to both
individuals and society (13). This
disease involves a wide variety of complex neural pathways and
transmitters, therefore, up to now, its pathogenesis remains
unclear and there is no effective therapeutic regimen (14). Hdac2 is mainly expressed in
post-mitotic or differentiated neurons. In addition to the actions
on histones, Hdac2 can also act on non-histone proteins, such as
glutamic acid decarboxylase 65, thereby inhibiting GABA function
and improving neuropathic pain (15). The protein encoded by Inpp5f has a
SAC phosphatase domain, so Inpp5f can exert SAC phosphatase
activity, inhibit the conversion of PIP2 to PIP3, promote the
conversion of PIP2 to PIP, and inhibit PI3K/AKT signaling pathway
(16).
Nakatsu et al (17) found that the Sac domain of
synaptojanin has Inpp5f activity, which may be related to the
release of synaptic proteins that regulate neurotransmitters and
their involvement in the early development of neurons. Zou et
al (18) found that neurons
lacking Inpp5f were able to regenerate axons more efficiently than
wild-type neurons. Zhang et al (19) found that silencing of Inpp5f (Sac2)
resulted in regeneration of axons and increased growth cones.
Pregabalin reduces intracellular calcium concentration by
inhibiting voltage-dependent calcium channels. Pregabalin can
prevent excitatory neurotransmitters from acting on the
postsynaptic membrane, block the production of neuropathic pain,
and can effectively treat allergy of nervous system to pain as well
as hypersensitivity symptoms (10).
Damaged nerve can induce TNFα and IL-1β to express in ganglion,
TNFα and IL-1β can further promote the occurrence of inflammation,
and can also induce the release of excitatory neurotransmitters,
resulting in sensitized nerve (20).
No significant differences in MWT were found among
the 3 groups before modeling. At 7 days after modeling, the
treatment and model control groups showed a significantly lower MWT
(a reduction range of >40%) compared with the normal control
group, indicating that the modeling was successful. At 7–21 days,
MWT in the normal control group was at a relatively stable level,
but MWT increased in the treatment group and decreased in the model
control group; but the lowest level was always observed in the
normal control group, followed by the treatment group and then the
model control group. The increase amplitude of MWT at 14–21 days in
the treatment group decreased, indicating that pregabalin can
inhibit the decrease of MWT in CCI rats, but cannot completely
reverse the changes and this effect has a certain timeliness. No
significant differences in TWL were found among the 3 groups before
modeling. After 7 days, TWL of the model control group gradually
decreased, and TWL of the treatment group gradually increased until
14 days. TWL in the treatment group was always smaller than that of
the normal control group, indicating that pregabalin has an
inhibitory effect on the decrease of TWL in CCI rats. At 21 days
after operation, the levels of TNFα and IL-1β in lumbar enlargement
tissue of the model control and treatment groups were higher than
those in the normal control group, and levels of TNFα and IL-1β in
the treatment group were lower than those in the model control
group. It indicated that the contents of TNFα and IL-1β in rat
spinal cord increased after CCI modeling, and TNFα and IL-1β may be
involved in the pathogenesis of CCI. Khan et al (21) also reached the same conclusion.
Although pregabalin does not exert anti-inflammatory effects, its
effect on repairing nervous system damage in rats may inhibit the
rise in TNFα and IL-1β levels. At 21 days, the expression of Hdac2
and Inpp5f mRNA in lumbar enlargement tissues of each group was
detected. The expression level of Hdac2 in the normal control and
treatment groups was lower than that in the model control group.
The expression level of Hdac2 was higher in the treatment group
than in the normal control group. Yuan et al (22) also found that expression level of
Hdac2 increased after nerve damage. This may be because Hdac2 can
inhibit GABA-mediated inhibition of the endogenous pain pathways.
After modeling, the expression of Hdac2 in the model control and
treatment groups increased, and the inhibition of the endogenous
pain pathway was weakened, and MWT and TWL values of the rats
decreased. Pubbarenin can inhibit the activity of GABA receptors to
counteract the inhibitory effect of Hdac2 on GABA, and the decrease
of Hdac2 expression in the treatment group also reduces the
decrease amplitude of MWT and TWL. The expression level of Inpp5f
mRNA in the treatment and normal control groups was significantly
higher than that in the model control group (P<0.05), but the
expression level of Inpp5f mRNA in the treatment group was lower
than that in the normal control group (P<0.05). Therefore, it is
suggested that the expression of Inpp5f may be involved in the
pathogenesis of neuropathic pain. Zou et al (18) found that Inpp5f can inhibit the
repair of spinal cord injury, but its effect on neuropathic pain is
unknown. PIP2 can upregulate TRPM8 receptors in dorsal root
ganglion, so as to promote pain sensitization and participate in
neuropathic pain. Inpp5f dephosphorylates PIP2 into PIP, so as to
inhibit the formation of hyperalgesia, and thus alleviates the
decline in MWT and TWL values in the treatment group (18). Trivedi et al (23) found that HDAC2 acts as a
transcriptional repressor and can inhibit the activity of
phosphatases such as PI3K and Inpp5f.
CCI rat model used in this experiment does not fully
represent the actual occurrence of neuropathic pain, and in
particular, it does not represent the hyperalgesia caused by
genetic mutations. Mutations of Hdac2 and Inpp5f gene caused by
viral infection or other autologous diseases also result in
neuropathic pain (24). In our
study, altered expression of Hdac2 and Inpp5f and values of MWT and
TWL were observed in CCI rats, while the mechanism of the role of
Hdac2 and Inpp5f in neuropathic pain remains unclear, or this may
be because the decrease of MWT and TWL values leads to change of
Hdac2/Inpp5f expression. Moreover, Pregabalin treatment may relieve
neuropathic pain through Hdac2/Inpp5f or other pathways. Therefore,
more studies are still needed to answer these questions.
In summary, Hdac2/Inpp5f may modulate neuropathic
pain in rats. Pregabalin may effectively relieve neuropathic pain
in CCI rats, and its action may be related to Hdac2/Inpp5f.
Therefore, our study may provide references for the clinical
treatment of neuropathic pain.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LY and TL helped with model establishment and
grouping. YW and YL helped with MWT assay. XZ performed ELISA. LY,
TL and CL were responsible for RT-qPCR. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Fifth Hospital of Wuhan (Wuhan, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bouhassira D and Attal N: Translational
neuropathic pain research: A clinical perspective. Neuroscience.
338:27–35. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Finnerup NB, Haroutounian S, Kamerman P,
Baron R, Bennett DL, Bouhassira D, Cruccu G, Freeman R, Hansson P,
Nurmikko T, et al: Neuropathic pain: An updated grading system for
research and clinical practice. Pain. 157:1599–1606. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu FX, Bian JJ, Miao XR, Huang SD, Xu XW,
Gong DJ, Sun YM, Lu ZJ and Yu WF: Intrathecal siRNA against
Toll-like receptor 4 reduces nociception in a rat model of
neuropathic pain. Int J Med Sci. 7:251–259. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lefaucheur JP: Cortical neurostimulation
for neuropathic pain: State of the art and perspectives. Pain. 157
Suppl 1:S81–S89. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen D, Weng Y, Ouyang B, Guo M and Guo Q:
Effect of intrathecal ropivacaine on spinal HDAC1 and HDAC2
expression in rats with neuropathic pain. Chin J Anaesth.
35:1093–1095. 2015.(In Chinese).
|
|
6
|
Maiarù M, Morgan OB, Tochiki KK, Hobbiger
EJ, Rajani K, Overington DW and Géranton SM: Complex regulation of
the regulator of synaptic plasticity histone deacetylase 2 in the
rodent dorsal horn after peripheral injury. J Neurochem.
138:222–232. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bai D, Zhang Y, Shen M, Sun Y, Xia Q,
Zhang Y, Liu X, Wang H and Yuan L: Hyperglycemia and hyperlipidemia
blunts the Insulin-Inpp5f negative feedback loop in the diabetic
heart. Sci Rep. 6:220682016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Palermo G, Maisel D, Barrett M, Smith H,
Duchateau-Nguyen G, Nguyen T, Yeh RF, Dufour A, Robak T, Dornan D,
et al: REACH investigators: Gene expression of INPP5F as an
independent prognostic marker in fludarabine-based therapy of
chronic lymphocytic leukemia. Blood Cancer J. 5:e3532015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Toth C: Pregabalin: Latest safety evidence
and clinical implications for the management of neuropathic pain.
Ther Adv Drug Saf. 5:38–56. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Verma V, Singh N and Singh Jaggi A:
Pregabalin in neuropathic pain: Evidences and possible mechanisms.
Curr Neuropharmacol. 12:44–56. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bennett GJ and Xie YK: A peripheral
mononeuropathy in rat that produces disorders of pain sensation
like those seen in man. Pain. 33:87–107. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jiang BC, Cao DL, Zhang X, Zhang ZJ, He
LN, Li CH, Zhang WW, Wu XB, Berta T, Ji RR, et al: CXCL13 drives
spinal astrocyte activation and neuropathic pain via CXCR5. J Clin
Invest. 126:745–761. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim J, Ryu SB, Lee SE, Shin J, Jung HH,
Kim SJ, Kim KH and Chang JW: Motor cortex stimulation and
neuropathic pain: How does motor cortex stimulation affect
pain-signaling pathways? J Neurosurg. 124:866–876. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang SE, Ko SY, Jo S, Choi M, Lee SH, Jo
HR, Seo JY, Lee SH, Kim YS, Jung SJ, et al: TRPV1 regulates stress
responses through HDAC2. Cell Rep. 19:401–412. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim HS, Li A, Ahn S, Song H and Zhang W:
Inositol Polyphosphate-5-Phosphatase F (INPP5F) inhibits STAT3
activity and suppresses gliomas tumorigenicity. Sci Rep.
4:73302014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nakatsu F, Messa M, Nández R, Czapla H,
Zou Y, Strittmatter SM and De Camilli P: Sac2/INPP5F is an inositol
4-phosphatase that functions in the endocytic pathway. J Cell Biol.
209:85–95. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zou Y, Stagi M, Wang X, Yigitkanli K,
Siegel CS, Nakatsu F, Cafferty WB and Strittmatter SM:
Gene-silencing screen for mammalian axon regeneration identifies
Inpp5f (Sac2) as an endogenous suppressor of repair after spinal
cord injury. J Neurosci. 35:10429–10439. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang S, Sarmiere PD, Doolen S, Kluge B,
Huang F, White JT and Holmberg E: Scar ablation combined with cell
transplantation promotes tissue repair and axon regeneration in
chronic contusion injury of rat spinal cord. 25th Annual
National-Neurotrauma-Society Symposium. 24:12562007.
|
|
20
|
Lu Y, Jiang BC, Cao DL, Zhang ZJ, Zhang X,
Ji RR and Gao YJ: TRAF6 upregulation in spinal astrocytes maintains
neuropathic pain by integrating TNF-α and IL-1β signaling. Pain.
155:2618–2629. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Khan J, Noboru N, Young A and Thomas D:
Pro- and anti-inflammatory cytokine levels (TNF-α, IL-1β, IL-6 and
IL-10) in rat model of neuroma. Pathophysiology. 24:155–159. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yuan Y, Peng W, Liu Y and Xu Z: Palmatine
attenuates isoproterenol-induced pathological hypertrophy via
selectively inhibiting HDAC2 in rats. Int J Immunopathol Pharmacol.
30:406–412. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Trivedi CM, Luo Y, Yin Z, Zhang M, Zhu W,
Wang T, Floss T, Goettlicher M, Noppinger PR, Wurst W, et al: Hdac2
regulates the cardiac hypertrophic response by modulating Gsk3 beta
activity. Nat Med. 13:324–331. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ma H, Marti-Gutierrez N, Park SW, Wu J,
Lee Y, Suzuki K, Koski A, Ji D, Hayama T, Ahmed R, et al:
Correction of a pathogenic gene mutation in human embryos. Nature.
548:413–419. 2017. View Article : Google Scholar : PubMed/NCBI
|