Introduction
Nucleoside/nucleotide analogues (NAs) are widely
used for treating chronic hepatitis B virus (HBV) infection as the
first-line antiviral drugs. NAs are prescribed to effectively
suppress HBV DNA to achieve low or undetectable levels, prevent the
progression of the disease to liver cirrhosis or hepatocellular
carcinoma, and improve the quality of life and survival of affected
patients (1). However, a major
limitation of NAs is the development of drug resistance. Successful
treatment of chronic HBV infection necessitates long-term
suppression of the virus, which must be coupled with the prevention
of the selection of drug-resistant mutants (2). Poor compliance and economic
disadvantage directly contribute to a suboptimal response and may
engender resistance to multiple NAs. Numerous patients do not
respond to anti-virus medications even if treated with adefovir
(ADV)-based combination therapies, including ADV plus lamivudine
(LAM), ADV plus telbivudine or ADV plus entecavir (ETV). Thus, the
development of an alternative treatment for patients with chronic
hepatitis B with a suboptimal response to ADV-based combination
therapy is crucial.
Tenofovir disoproxil fumarate (TDF) is an oral
pro-drug of tenofovir, a nucleotide analogue that is one of the
most potent HBV inhibitors (1) and
is characterized by a high genetic barrier to resistance (2–4). It not
only exhibited high efficacy in NA-naïve chronic hepatitis B
patients but also produced a viral suppression response in patients
with a history NA treatment (5–7).
However, in these previous studies, the majority of patients that
were switched to TDF had received previous monotherapy with LAM,
ADV or ETV, or sequential therapy. In clinical practice, due to
poor patient compliance and unsuitable initial drug selection,
numerous patients require treatment with ADV-based combination
therapy, which frequently produces suboptimal responses (8). The currently available data on the
efficacy of the switch of chronic hepatitis B patients with a
suboptimal response to ADV-based combination therapy to TDF therapy
are limited. This paucity of clinically relevant information
necessitates the further analysis of the clinical records of
patients with chronic hepatitis B whose treatment involved a switch
to TDF. Therefore, the major objective of the present study was to
retrospectively evaluate the efficacy and safety of TDF switch
therapy in chronic hepatitis B patients after a suboptimal response
to ADV-based combination therapy.
Patients and methods
Study population
The present retrospective study enrolled patients
with chronic hepatitis B who received TDF therapy after a
suboptimal response to ADV-based combination therapy. The subjects
were selected from patients treated at the Department of Infectious
Diseases, The Third Affiliated Hospital, Sun Yat-sen University
(Guangzhou, China); the samples were obtained between June 2012 and
December 2015. The suboptimal response to ADV-based combination
therapy was defined as either a nonresponse (decreased serum HBV
DNA <2 log10IU/ml after 6 months of treatment) or an
incomplete response (a decrease in HBV DNA of >1
log10IU/ml but detectable HBV DNA after at least 6
months of therapy in compliant patients). The inclusion criterion
was the presence of serum HBV DNA at levels of ≥103
IU/ml at the time of initiation of the TDF switch therapy. Patients
with either human immunodeficiency virus or other hepatitis virus
infections, or evidence of liver decompensation, as well as
pregnant and breast-feeding women were excluded from the study. A
virologic breakthrough was defined as an increase in HBV DNA of
>1 log10IU/ml in comparison with the baseline at any
time during treatment.
Clinical indexes and measurement
methods
Subjects received TDF monotherapy (300 mg/day) or of
TDF (300 mg/day) combined with ETV (0.5 mg/day). A 2-ml blood
sample was collected at the baseline and every 12 weeks thereafter
and stored at −80°C for future assessment. The assays included
hematological analysis, biochemical indices in liver parameters,
HBV DNA, serological analysis, hepatic synthetic function, creatine
kinase (CK), blood urea nitrogen and creatinine levels. The
measurements were performed using automated techniques. Blood was
centrifuged for 5 min at 3,000 × g and 25°C to obtain the serum.
The serum HBV DNA levels were measured by the HBV nucleic acid
quantitative detection kit (cat. no. LANBORUI0001; DAAN Gene Co.,
Ltd., Guangzhou, China), with a minimum detection limit of 100
IU/ml. Hepatitis B s antigen (HBsAg; cat. no. 11820532122), HBeAg
(cat. no. 11820583122) and the respective antibodies anti-HBs (cat.
no. 11820524122) and anti-HBe (cat. no. 11820613122) antibodies
were determined using commercially available chemiluminescence
assay kits (Roche Diagnostic Systems, Basel, Switzerland). An
ultrasound examination of the liver was also performed. The
patients were thoroughly examined at each follow-up visit every 12
weeks over 144 weeks and requested to report any incidence of
adverse events.
End-points
The primary end-point was the cumulative probability
of patients achieving VR (undetectable HBV DNA, i.e. <100 IU/ml)
during TDF treatment. The secondary end-points were the rate of
HBeAg seroconversion in HBeAg-positive patients, alanine
aminotransferase (ALT) normalization and the percentage of cases
with elevated creatinine and CK.
Statistical analysis
Data were analyzed using the SPSS software package
version 13.0 (SPSS Inc., Chicago, IL, USA). Quantitative data are
expressed as the mean ± standard deviation. The categorical data
are presented as counts and percentages. HBV DNA levels are
presented in the log-transformed format. Student's t-test was used
to evaluate the statistical significance of quantitative data with
a normal distribution, including the liver and kidney indexes. The
cumulative probability of achieving undetectable HBV DNA was
assessed using the Kaplan-Meier method. The difference between the
cumulative curves was estimated using the log-rank test. A
two-tailed P<0.05 was considered to indicate a statistically
significant difference.
Results
Baseline characteristics
The baseline characteristics of the study subjects
are presented in Table I. In the
cohort of 50 patients, 41 (82%) were treated with TDF alone and 9
(18%) were treated with TDF plus ETV. The median age was 35 years
(range, 23–51 years), and 43 patients (86%) were males. A total of
48 patients were HBeAg-positive (96%), 3 (6%) suffered from
cirrhosis and 1 (2%) had liver cancer diagnosed as small
hepatocellular carcinoma by magnetic resonance imaging and computed
tomography examination. In this patient, the ADV-based combination
therapy was immediately discontinued and was replaced by TDF
combined with ETV, while small hepatectomy was performed to treat
the liver cancer. Additionally, in this patient, no recurrence of
hepatocellular carcinoma was identified at the follow-up at the
week 144 and the mean serum HBV DNA level was 4.8±1.6
log10IU/ml. The number of patients previously treated
with LAM plus ADV, telbivudine (LdT) plus ADV and ETV plus ADV was
17 (34%), 14 (28%) and 19 (38%), respectively. The median follow-up
duration during TDF treatment with or without ETV was 102 weeks
(range, 24–192 weeks).
 | Table I.Characteristics of patients at
baseline (n=50). |
Table I.
Characteristics of patients at
baseline (n=50).
| Characteristic | Value |
|---|
| Male gender | 43 (86) |
| Age (years) | 35 (23–51) |
| Body mass index
(kg/m2) | 23.1±3.23 |
| Family history of
HBV infection | 25 (50) |
| Presence of
cirrhosis | 3 (6) |
| Presence of
hepatocellular carcinoma | 1 (2) |
| ALT (U/l) | 43.5
(13.0–893.0) |
| HBV DNA
(log10IU/ml) | 4.8±1.6 |
| HBeAg
positivity | 48 (96) |
| History of
treatment with ADV plus other NAs |
|
|
LAM+ADV | 17 (34) |
|
LdT+ADV | 14 (28) |
|
ETV+ADV | 19 (38) |
| Treatment
regimen |
|
|
TDF | 41 (82) |
|
TDF+ETV | 9 (18) |
| Duration of
follow-up (weeks) | 102 (24–192) |
| Poor curative
effect | 5 |
| Virological
breakthrough | 6 |
Antiviral efficacy of TDF
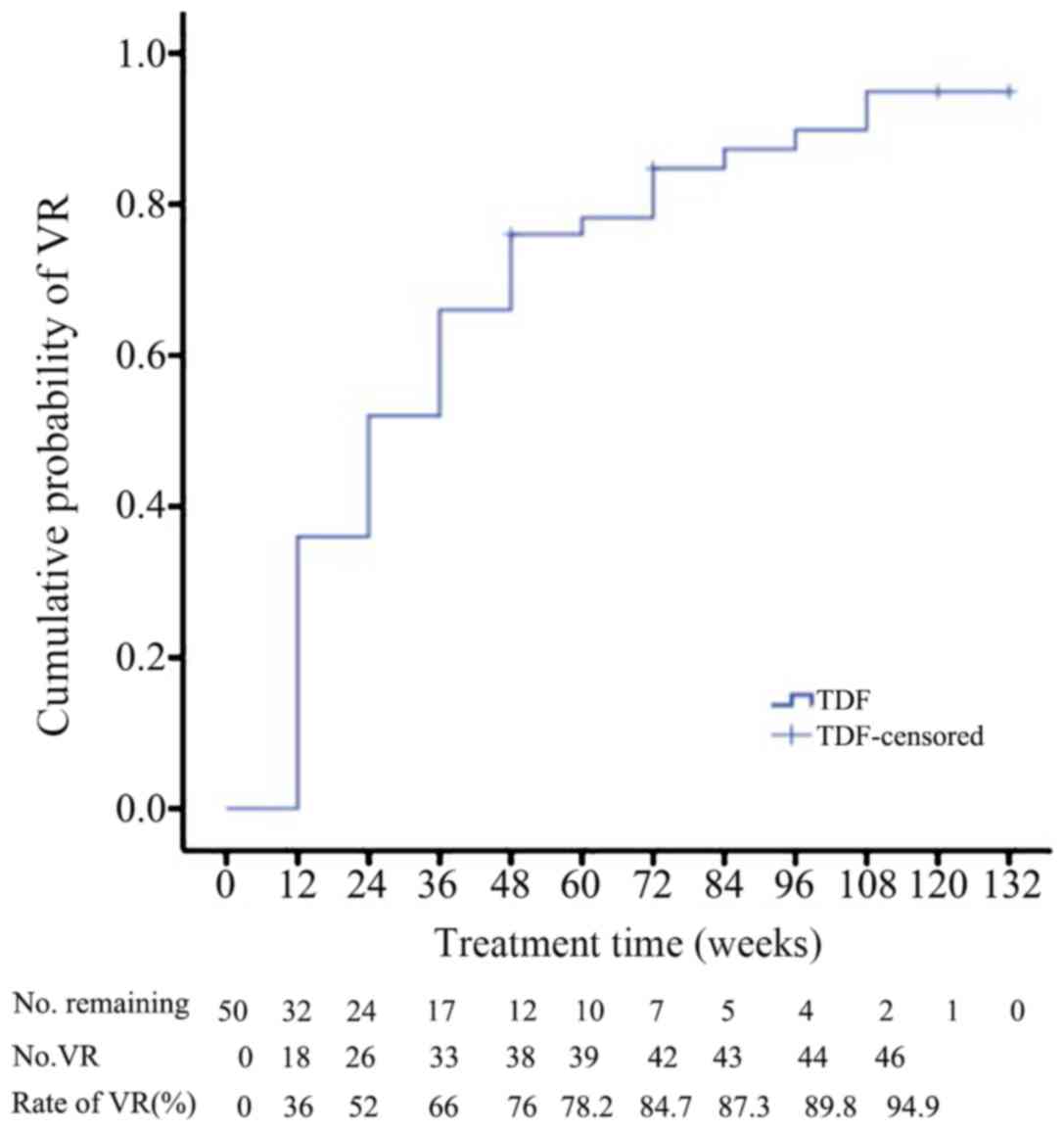
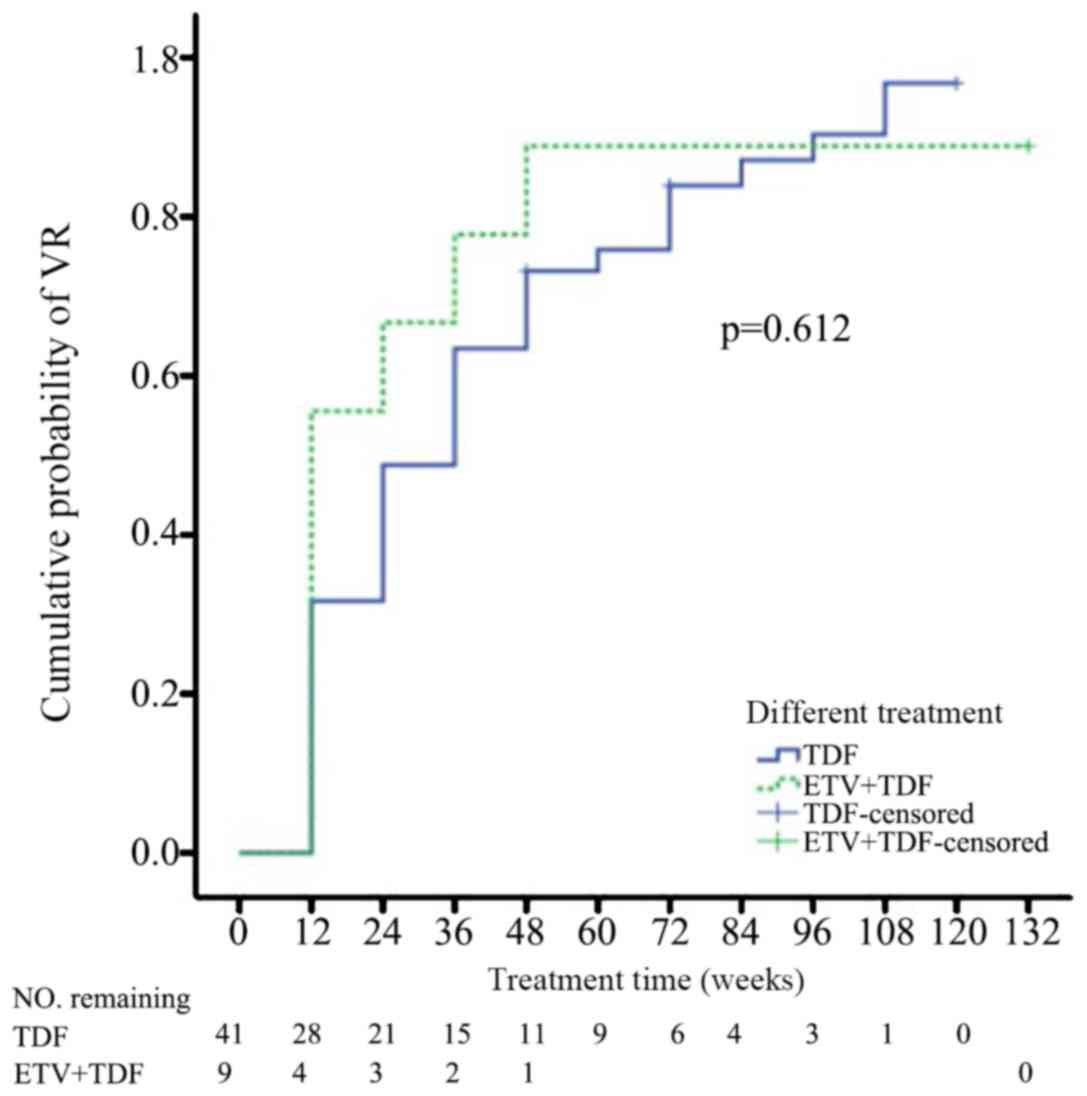
The cumulative probability of achieving a VR at 12,
24, 48, 60, 72, 84, 96 and 108 weeks was 36.0, 52.0, 66, 76.0,
78.2, 89.8 and 94.9%, respectively (Fig.
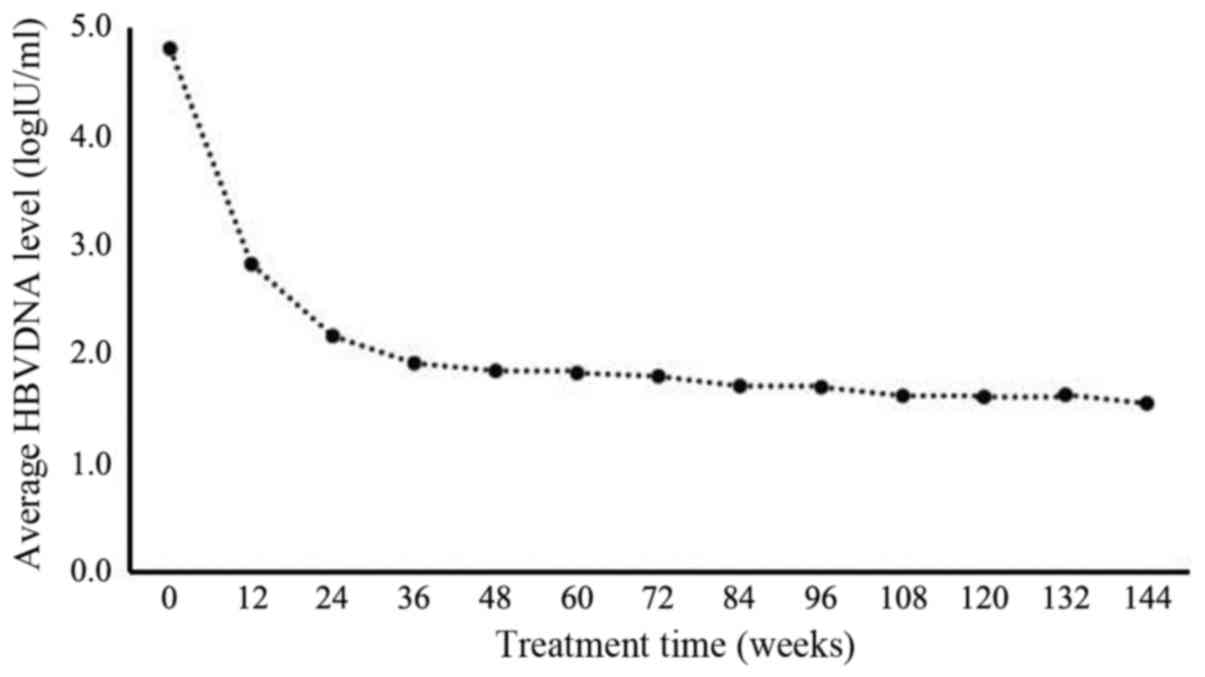
1). The highest decrease in the levels of HBV DNA was detected
at week 12 and the reduction continued with time to reach stable
levels at 48 weeks (Fig. 2).
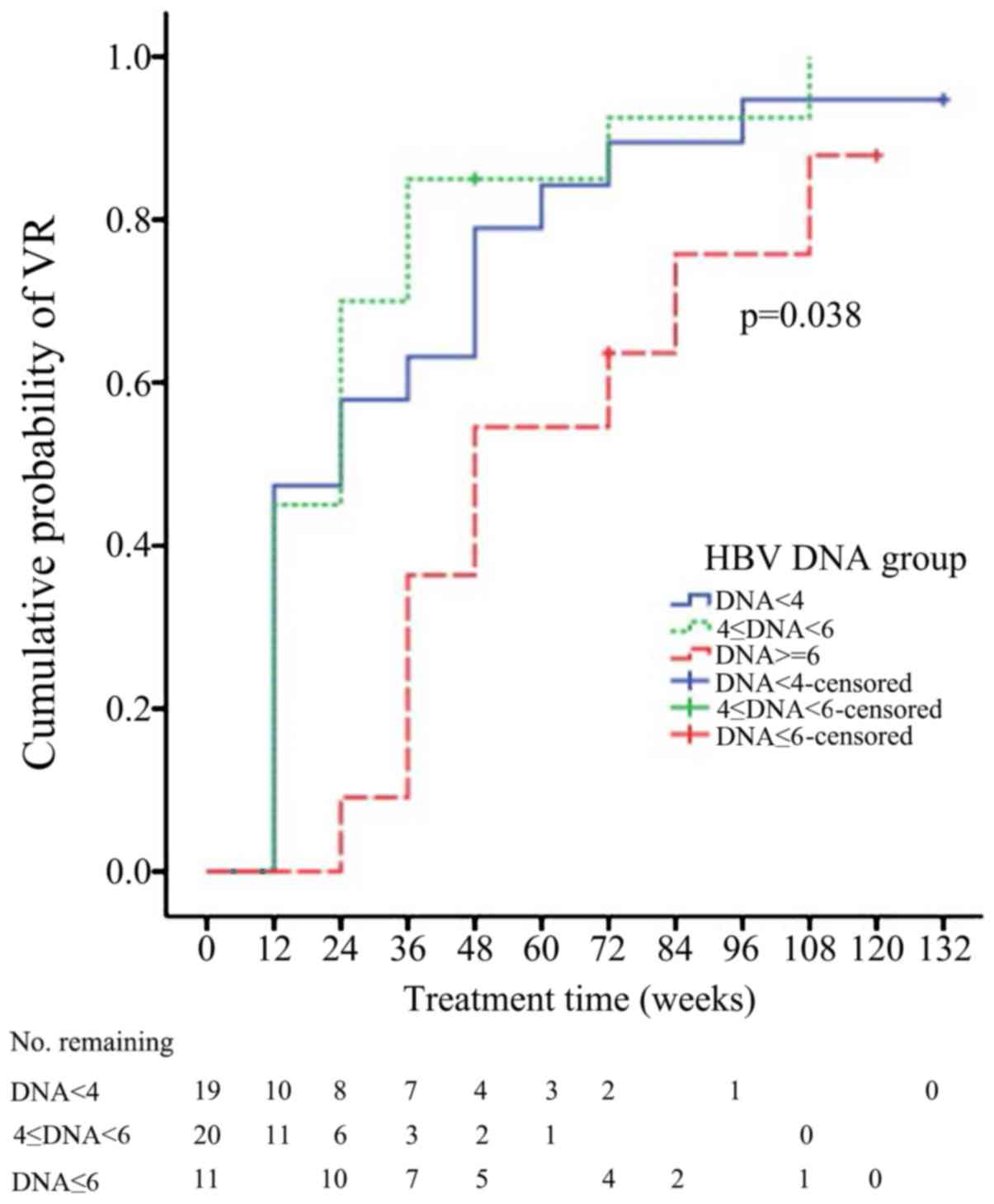
According to three distinct levels of HBV DNA at the baseline
(<4, 4–6 and ≥6 log10IU/ml), the patients were
assigned to three groups. A HBV DNA level of ≥6
log10IU/ml at the baseline was significantly associated
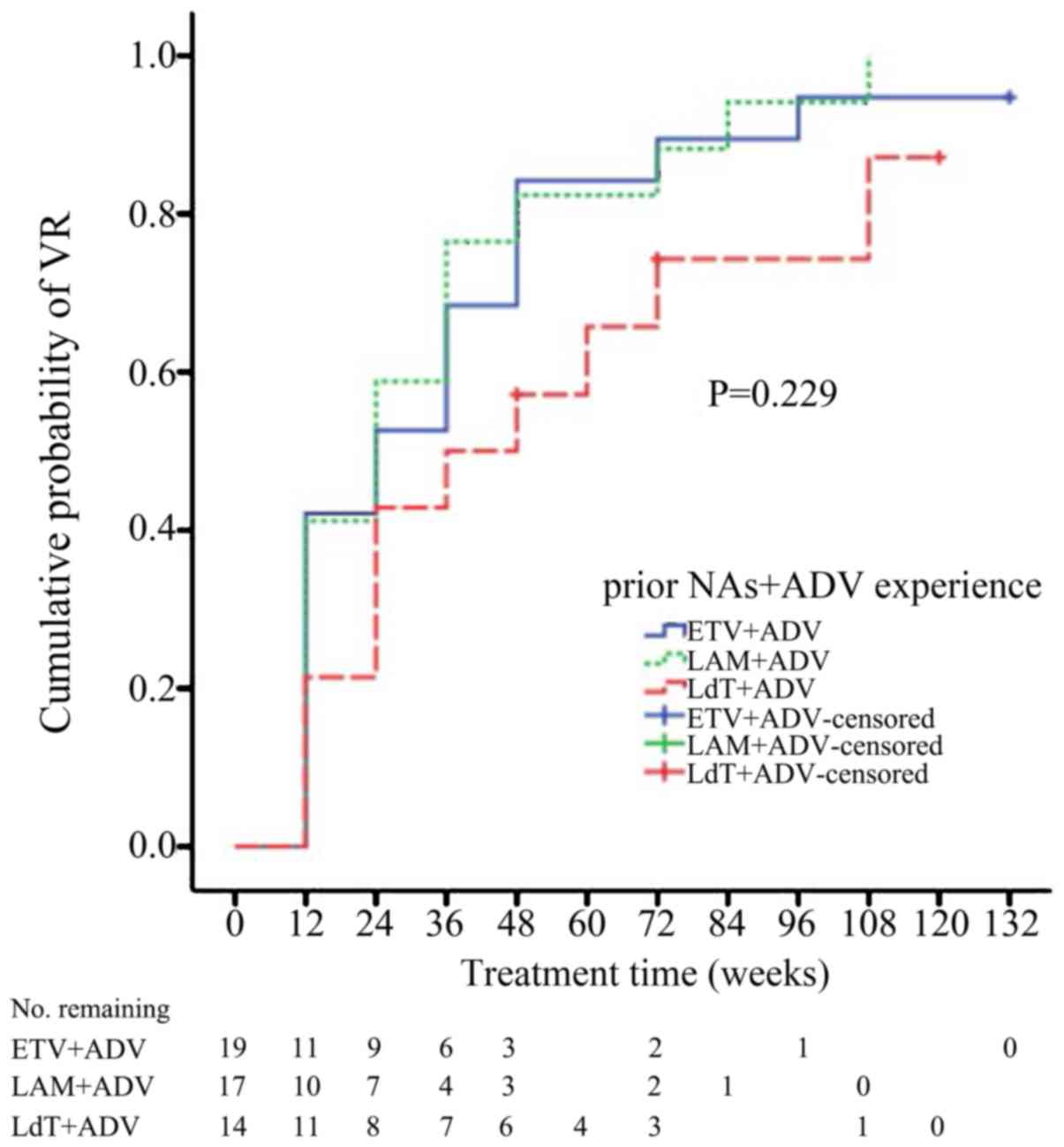
with an increased VR rate among the patients (P=0.038; Fig. 3). According to the history of
treatment, the patients were divided into three groups: LAM plus
ADV, LdT plus ADV and ETV plus ADV. The cumulative VR rates of
patients previously treated with LAM plus ADV were 41.2, 58.8,70.6,
82.4, 88.2 and 94.1% at weeks 12, 24, 36, 48, 72 and 84,
respectively, while those of patients previously treated with LdT
plus ADV were 21.4, 42.9, 50.0, 57.1 and 78.6% at weeks 12, 24, 36,
48 and 72, respectively. In addition, in the group with a history
of ETV plus ADV treatment, the response rates were 42.1, 52.6,
68.4, 84.2, 89.5 and 94.7% at weeks 12, 24, 36, 48, 72 and 96,
respectively. However, the cumulative probability of VR among the
three groups was not statistically different (P=0.229; Fig. 4). In the LdT plus ADV group, the
probability of VR was lower compared with the other groups, however
the size of the group (n=14; 28%) may be too small to be
statistically significant. The efficacy of TDF monotherapy did not
significantly differ from that of combined therapy with TDF and ETV
(P=0.612; Fig. 5). During the
follow-up, 6 patients suffered from a virologic breakthrough. Five
of these cases received treatment with TDF and 1 was treated with
TDF plus ETV. Among them, 3 patients (2 treated with TDF and 1 with
TDF plus ETV) failed to achieve a VR.
Response regarding biochemical and
serological parameters
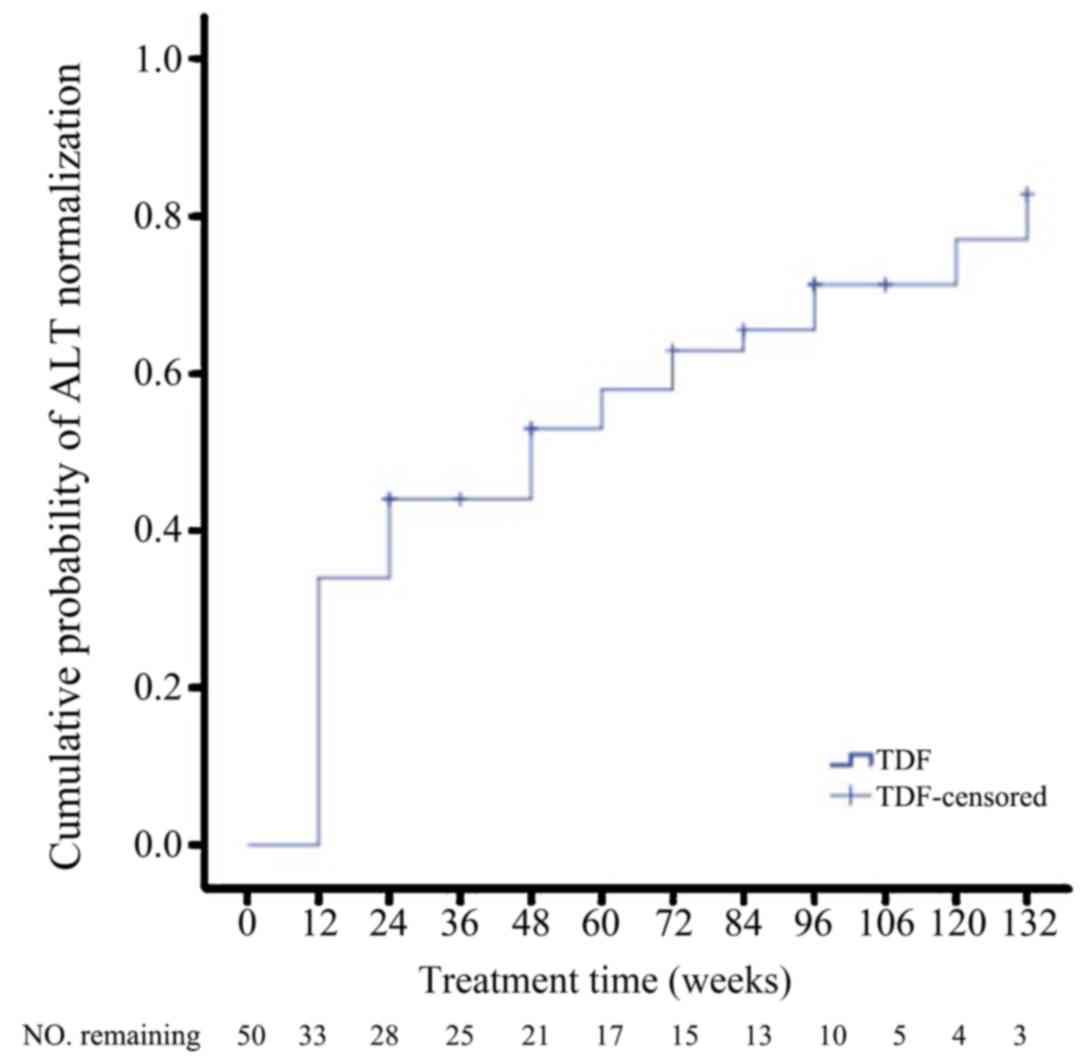
The cumulative probability of ALT normalization at
12, 24, 36, 48, 60, 72, 84, 96, 108, 120 and 132 weeks was 34.0,
44.0, 50.0, 58.0, 66.0, 70.0, 74.0, 80.0, 90.0, 92.0 and 94.0%,
respectively (Fig. 6). Among the 48
patients that were HBeAg-positive at baseline, 5 (10.4%) achieved
HBeAg seroconversion at 72, 84, 96 and 108 weeks respectively. The
cumulative probability of HBeAg seroconversion at 72, 84, 96 and
108 weeks was 2.5, 7.9, 11.2 and 15.2%, respectively (Table II).
 | Table II.HBeAg seroconversion rate among the
patients who were HBeAg-positive at baseline (n=48). |
Table II.
HBeAg seroconversion rate among the
patients who were HBeAg-positive at baseline (n=48).
| Weeks |
log10(COI of HbeAg
expression)a | HBeAg
seroconversion | The cumulative
probability of HBeAg seroconversion (%) |
|---|
| 72 | 2.00 (0.33,
3.13) | 10.4% (5/48) | 2.5 |
| 84 | 1.76 (−0.25,
3.17) | 10.4% (5/48) | 7.9 |
| 96 | 1.69 (−0.33,
3.25) | 10.4% (5/48) | 11.2 |
| 108 | 1.56 (−0.44,
3.22) | 10.4% (5/48) | 15.2 |
Detection of viral drug
resistance-associated gene mutations
Viral genes associated with drug resistance were
detected in serum samples obtained from 6 patients who had
experienced a virologic breakthrough during TDF treatment and from
5 patients who had a poor response to TDF within 24 weeks (Table I). In 3 of the 6 patients who had a
virologic breakthrough, the TDF treatment was temporarily
discontinued; upon resumption of the therapy, a VR was still
obtained. In addition, 3 patients developed a virologic
breakthrough during the course of TDF treatment. The genes were
sequenced from the serum of 2 patients with poor efficacy and 3
patients with VR (Table II). The
drug resistance mutation points were (204V) and (204I) in the
patients with poor efficacy, and (181V, 236T), (181V, 204V) and
(181V, 204I, 236T) in the 3 patients with VR (whose HBV genotype
was B; Table III). A 204V mutation
(HBV genotype, B) and 204I mutation (HBV genotype, C) were detected
separately in 2 out of 5 patients who had a poor response to TDF
within 24 weeks.
 | Table III.Results of gene sequencing analysis
of resistance-associated viral mutations in 2 patients with
suboptimal response, one of which had a virological breakthrough
and 3 patients with virologic breakthrough during TDF salvage
treatment. |
Table III.
Results of gene sequencing analysis
of resistance-associated viral mutations in 2 patients with
suboptimal response, one of which had a virological breakthrough
and 3 patients with virologic breakthrough during TDF salvage
treatment.
|
|
|
| Drug resistance
mutation points determined at different events |
|---|
|
|
|
|
|
|---|
| Case no. | Treatment
history | Genotype | Baseline of rescue
therapy | Suboptimal response
at 24 weeks | Virologic
breakthrough |
|---|
| 9 |
LdT→ADV→ADV+LdT→TDF | B | 181V, 236T | – | 181V, 236T |
| 10 |
ADV→ADV+LAM→TDF | C | 181V, 204V | – | 181V, 204V |
| 18 |
ADV→ADV+LAM→TDF | B | 204V | 204V | – |
| 33 |
LAM→ADV→ETV→ADV+ETV→TDF | B | 181V, 204I,
236T | – | 181V, 204I,
236T |
| 37 |
LAM→ADV→ADV+ETV→TDF | C | 204I | 204I | – |
Safety
No severe adverse events were reported during the
study. The baseline levels of CK were recorded for 50 patients, out
of which 5 had values slightly higher than the normal reference
range (24–194 IU/l) at week 132. Consistent with previous results
(7), however, the activity of this
enzyme returned to normal levels after these patients reduced their
physical exercise. The remaining patients did not display any
elevated CK concentration after 132 weeks of the follow-up. Normal
ranges were as follows: CK, 24–294 U/l (9); CR, 44–133 µmol/l (10); Ca, 2.25–2.75 mmol/l (11); P, 0.97–1.61 mmol/l; AST, 8–40 U/l)
(12); ALT, 5–40 U/l (13); ALB, 40–55 G/l; TB, 1.71~17.1 µmol/l
(14).
To assess the renal safety, the creatinine levels
were analyzed in a subset of 50 patients, for which the baseline
values were available. Only 1 patient, treated with TDF plus ETV,
exhibited slightly elevated creatinine. This female patient was 38
years old and free of any renal disease. The serum creatinine was
130 µmol/l at baseline, fluctuated between 128 and 146 µmol/l
during the treatment and was 130 µmol/l at 132 weeks, i.e., the
last follow-up. The blood phosphorus and calcium concentrations
were also measured in all patients. The blood phosphorus content
remained within the 0.95–1.79 µmol/l range, and the blood calcium
content was within the range of 2.03–2.67 µmol/l. Only four
patients had calcium concentrations below the normal range.
Compared with TDF alone, the number of patients whose serum levels
of CK, CR, P, Ca, ALT, AST, ALB and TB tended to be normal after
TDF + EVT treatment was markedly improved (Table IV). No significant difference was
identified in the mean CK, CR, P, Ca, AST, ALT, ALB and TB
concentrations in the different treatment groups at the follow-up
time-points (Table V).
 | Table IV.Liver and kidney function of patients
with chronic hepatitis B treated with TDF alone (n=41) or with TDF
plus ETV (n=9). |
Table IV.
Liver and kidney function of patients
with chronic hepatitis B treated with TDF alone (n=41) or with TDF
plus ETV (n=9).
|
| CK (>194
U/l) | CR (>133
µmol/l) | Ca (<2.25
mmol/l) | P (<0.97
mmol/l) | P (>1.61
mmol/l) | AST (>40
U/l) | ALT (>40
U/l) | ALB (>55
G/l) | TB (>17.1
µmol/l) |
|---|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Index; Time
(weeks) | THF | THF+ETV | THF | THF+ETV | THF | THF+ETV | THF | THF+ETV | THF | THF+ETV | THF | THF+ETV | THF | THF+ETV | THF | THF+ETV | THF | THF+ETV |
|---|
| 0 | 7 | 0 | 1 | 1 | 4 | 0 | 2 | 0 | 1 | 0 | 14 | 3 | 21 | 5 | 1 | 0 | 3 | 3 |
| 12 | 5 | 3 | 0 | 0 | 4 | 0 | 3 | 0 | 0 | 0 | 10 | 1 | 21 | 3 | 0 | 0 | 4 | 0 |
| 24 | 9 | 3 | 0 | 0 | 0 | 1 | 4 | 0 | 0 | 0 | 7 | 4 | 16 | 6 | 0 | 0 | 5 | 2 |
| 36 | 7 | 3 | 0 | 1 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 2 | 13 | 4 | 0 | 0 | 4 | 3 |
| 48 | 11 | 3 | 0 | 1 | 1 | 0 | 2 | 0 | 0 | 1 | 2 | 1 | 12 | 4 | 0 | 0 | 5 | 3 |
| 60 | 6 | 3 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 | 0 | 8 | 3 | 0 | 0 | 2 | 3 |
| 72 | 7 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 3 | 0 | 11 | 4 | 0 | 0 | 2 | 2 |
| 84 | 6 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 4 | 1 | 8 | 2 | 0 | 0 | 3 | 4 |
| 96 | 5 | 0 | 0 | 1 | 1 | 0 | 3 | 0 | 0 | 0 | 6 | 1 | 8 | 2 | 0 | 0 | 2 | 2 |
| 108 | 4 | 3 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 3 | 0 | 4 | 1 | 0 | 0 | 2 | 2 |
| 120 | 5 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 3 | 0 | 4 | 1 | 0 | 0 | 1 | 1 |
| 132 | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 3 | 1 | 0 | 0 | 0 | 1 |
| 144 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
 | Table V.Level of liver and kidney function
(n=50). |
Table V.
Level of liver and kidney function
(n=50).
|
| THF | THF+ETV |
|---|
|
|
|
|
|---|
| Treatment group;
Time-point (weeks) | CK | CR | Ca | P | ALB | AST | ALT | TB | CK | CR | Ca | P | ALB | AST | ALT | TB |
|---|
| 0 | 173.60± | 95.70± | 2.37± | 1.22± | 46.55± | 58.94± | 99.53± | 12.19± | 148.00± | 87.49± | 2.46± | 1.15± | 43.82± | 37.89± | 50.89± | 13.72± |
|
| 164.00 | 97.75 | 0.12 | 0.18 | 0.69 | 12.91 | 29.04 | 0.65 | 26.82 | 25.08 | 0.17 | 0.20 | 1.10 | 5.50 | 10.12 | 2.26 |
| 12 | 158.30± | 78.04± | 2.38± | 1.14± | 46.49± | 36.92± | 52.15± | 12.73± | 174.00± | 85.04± | 2.44± | 1.19± | 43.71± | 35.13± | 49.13± | 13.35± |
|
| 70.32 | 19.69 | 0.13 | 0.15 | 0.34 | 3.82 | 5.10 | 0.70 | 66.91 | 26.16 | 0.12 | 0.14 | 1.98 | 4.29 | 6.23 | 1.28 |
| 24 | 162.80± | 82.68± | 2.42± | 1.13± | 46.38± | 31.08± | 41.84± | 12.36± | 181.20± | 83.24± | 2.41± | 1.24± | 43.46± | 39.11± | 69.44± | 13.7± |
|
| 81.36 | 12.58 | 0.10 | 0.13 | 0.39 | 1.56 | 3.08 | 0.66 | 63.02 | 25.56 | 0.12 | 0.14 | 1.33 | 5.87 | 22.33 | 1.25 |
| 36 | 161.70± | 83.43± | 2.39± | 1.16± | 46.57± | 29.83± | 39.04± | 16.54± | 266.30± | 87.13± | 2.45± | 1.14± | 45.25± | 35.00± | 40.88± | 17.36± |
|
| 76.23 | 12.95 | 0.11 | 0.17 | 0.41 | 1.28 | 3.14 | 4.26 | 245.70 | 27.62 | 0.07 | 0.16 | 1.85 | 5.88 | 4.35 | 0.95 |
| 48 | 169.20± | 80.95± | 2.40± | 1.14± | 45.98± | 28.22± | 35.39± | 12.80± | 222.00± | 83.41± | 2.47± | 1.28± | 44.37± | 32.29± | 41.88± | 15.70± |
|
| 79.65 | 15.01 | 0.09 | 0.16 | 0.5 | 1.43 | 2.39 | 0.73 | 149.70 | 27.32 | 0.14 | 0.19 | 1.85 | 4.48 | 5.15 | 1.13 |
| 60 | 156.80± | 81.16± | 2.43± | 1.18± | 45.19± | 28.26± | 35.22± | 11.23± | 189.60± | 83.79± | 2.40± | 1.12± | 43.7± | 28.71± | 40± | 16.44± |
|
| 78.12 | 18.99 | 0.10 | 0.16 | 0.42 | 1.4 | 2.46 | 0.72 | 59.87 | 29.09 | 0.14 | 0.09 | 1.48 | 1.38 | 7.68 | 2.50 |
| 72 | 199.00± | 84.55± | 2.44± | 1.20± | 46.56± | 28.14± | 36.90± | 12.96± | 165.00± | 85.03± | 2.46± | 1.23± | 44.50± | 28.14± | 41.00± | 15.55± |
|
| 176.80 | 14.75 | 0.13 | 0.18 | 0.42 | 1.59 | 2.49 | 0.92 | 92.69 | 27.89 | 0.20 | 0.18 | 1.60 | 1.93 | 6.51 | 2.92 |
| 84 | 158.60± | 80.48± | 2.49± | 1.14± | 45.78± | 30.20± | 34.04± | 12.05± | 151.30± | 87.30± | 2.36± | 1.09± | 44.25± | 33.67± | 38.50± | 18.90± |
|
| 76.18 | 12.95 | 0.15 | 0.13 | 0.37 | 2.37 | 2.83 | 0.64 | 58.44 | 29.49 | 0.13 | 0.16 | 1.86 | 7.98 | 7.43 | 2.15 |
| 96 | 161.70± | 80.00± | 2.41± | 1.11± | 44.08± | 30.27± | 34.41± | 12.22± | 138.00± | 85.24± | 2.48± | 1.12± | 43.14± | 27.86± | 37.57± | 15.60± |
|
| 96.62 | 16.26 | 0.13 | 0.14 | 1.63 | 2.56 | 3.67 | 1.15 | 37.20 | 32.53 | 0.01 | 0.21 | 1.03 | 3.77 | 6.29 | 2.29 |
| 108 | 163.60± | 81.69± | 2.44± | 1.19± | 45.23± | 33.27± | 34.42± | 12.39± | 193.80± | 99.60± | 2.28± | 1.09± | 43.98± | 28.40± | 33.29± | 16.90± |
|
| 63.73 | 13.34 | 0.10 | 0.15 | 0.93 | 5.04 | 4.28 | 1.09 | 45.98 | 32.99 | 0.08 | 0.16 | 1.37 | 1.86 | 3.35 | 2.31 |
| 120 | 217.20± | 94.13± | 2.46± | 1.17± | 45.58± | 32.67± | 38.45± | 13.76± | 174.40± | 91.14± | 2.40± | 1.02± | 43.32± | 29.00± | 35.60± | 15.66± |
|
| 146.90 | 12.59 | 0.09 | 0.18 | 0.81 | 4.27 | 4.08 | 1.44 | 37.59 | 25.07 | 0.05 | 0.23 | 1.19 | 2.61 | 2.58 | 1.27 |
| 132 | 165.10± | 84.40± | 2.48± | 1.19± | 42.03± | 29.89± | 40.22± | 11.87± | 186.00± | 92.98± | 2.36 | 0.85 | 45.58± | 28.75± | 41.25± | 13.33± |
|
| 54.85 | 16.04 | 0.09 | 0.18 | 3.68 | 5.27 | 8.20 | 0.84 | 68.57 | 27.36 |
|
| 0.63 | 2.06 | 2.66 | 2.20 |
| 144 | 145.80± | 84.43± | 2.42± | 1.07± | 45.23± | 27.67± | 25.50± | 11.67± | 125.70± | 72.33± |
|
| 45.17± | 24.33± | 32.67± | 19.2± |
|
| 35.41 | 16.75 | 0.04 | 0.15 | 0.96 | 1.99 | 3.79 | 1.16 | 38.59 | 12.50 |
|
| 0.64 | 3.84 | 2.40 | 2.27 |
Discussion
The results of the present study demonstrate that
long-term treatment with TDF, applied in the cases chronic
hepatitis B with a suboptimal response to ADV-based combination
treatment, provides a robust viral response and a high rate of ALT
normalization. A gradual increase of the cumulative VR rate was
observed with prolonged administration of TDF. The efficacy of the
TDF therapy was associated with the baseline level of HBV: Patients
with HBV DNA <6 log10IU/ml at baseline displayed a
significantly higher VR rate than those with HBV DNA ≥6
log10IU/ml.
Previous studies have documented that TDF has a
favorable tolerability profile and induces a rapid and sustained
suppression of HBV DNA in patients with chronic hepatitis B,
regardless of their previous treatment with NAs (15–18). A
prospective study from Germany has indicated that after 36 months
of treatment with TDF, the HBV DNA became undetectable in 91% of
previously TDF-naïve patients and in 96% of patients with prior NA
treatment (6). In a trial involving
252 chronic hepatitis B patients, the TDF switch therapy yielded a
stable VR in 84.9% of subjects with previous NA treatment after 22
months (19). In another study on 29
patients with a suboptimal response to previous LAM monotherapy or
sequential therapy with LAM and ETV, undetectable HBV DNA was
achieved in >80% of cases after 18 months of TDF monotherapy
(7). The effectiveness of tenofovir
switch therapy in patients with prior NA treatment of chronic
hepatitis B patients was further proven by a study which determined
that introduction of tenofovir in subjects resistant to LAM, ADV or
ETV achieved cumulative VR rates of 82.8, 81.4 and 84.1%,
respectively (20).
In the present study, the efficiency of TDF switch
therapy in chronic hepatitis B patients with a suboptimal response
to ADV-based combination therapy was noteworthy. The cumulative
probability rate of a VR reached 52.0, 76.0, 89.8 and 94.9% at week
24, 48, 96 and 108, respectively. Other studies indicated a similar
kinetics of HBV DNA decline in patients exhibiting a suboptimal
response to ADV or ADV resistance. Baran et al (21) reported that the rate of complete VR
in patients with chronic hepatitis B with a suboptimal response or
resistance to ADV-based combination therapy, respectively, was 75
and 58% at 12 months, 87 and 79% at 24 months and 94 and 79% at 36
months after switching to TDF. Similar rates of wild-type and
rtN236T-mutant HBV DNA decline were noted following 4 weeks of
treatment with TDF (22), despite
the proportion of rtN236T mutant HBV DNA remaining unaltered during
the therapeutic intervention. It has been demonstrated in
vitro that HBV mutations selected by ADV confer a multi-drug
resistance that also affects the efficacy of TDF (23). However, van Bömmel et al
(24) observed that although ADV
resistance mutations (rtN236T and/or rtA181V/T) remained detectable
after TDF switch therapy, the level of HBV DNA in most of the
patients decreased at 12 months, and 2 patients achieved a complete
viral response after 72 weeks. This result demonstrates that
ADV-resistant HBV variants may be further selected during TDF
treatment; however, they only cause a mild decrease in the
sensitivity to TDF. Of note, the switch to TDF rescue treatment due
to a suboptimal response to ETV plus ADV combination therapy had a
potent effect: The cumulative VR rate reached 52.6, 84.2 and 94.7%
at week 24, 48 and 96, respectively (18). Simultaneously, the cumulative
response rates among ADV plus LAM/LdT/ETV groups were not
significantly different (P=0.229), suggesting that TDF may be
employed as an efficient agent irrespective of the type of prior
ADV-based combination therapy.
The present study revealed that the VR rates after
switching to TDF treatment were associated with the baseline levels
of HBV DNA. In this regard, Lo et al (19) evaluated the response of HBV to TDF
switch therapy by Kaplan-Meier analysis. The patients were
stratified into groups based on their HBV DNA levels during the
switch to TDF (<200 IU/ml, 200–19,999 and ≥20,000 IU/ml). The
results indicated that, in a manner similar to that observed in the
present study, a low HBV DNA level at the time of switching to TDF
was an independent predictor of the treatment efficacy in
NAs-experienced chronic hepatitis B patients. Another study also
assessed the effect of TDF in 151 NAs-naïve subjects and revealed
that the HBV DNA levels at baseline were significantly associated
with a greater VR (3). Comparable
conclusions were reached by Park et al (25), who determined that when patients are
stratified according to their HBV DNA levels at baseline (2–3, 3–4,
4–5 and ≥6 log10IU/ml), the increase in VR is highest
for the group with the lowest viral DNA burden. Together, these
findings support the notion that the HBV DNA level at the time of
switching to TDF is the most crucial factor affecting the VR.
In the present study, the cumulative rate of the VR
to TDF monotherapy was comparable to that of TDF plus ETV
(P=0.612). At the beginning of the treatment, the cumulative rate
of response to the combination of TDF plus ETV was higher than that
to TDF monotherapy (24 weeks, 66.7 vs. 48.8%; 48 weeks, 88.9 vs.
73.2%). However, with prolonged treatment, the cumulative rate of
VR was similar between the two groups. Similar results were
reported by other studies. For instance, Lim et al (26) demonstrated that TDF monotherapy
achieved a response comparable to that of TDF plus ETV combination
therapy, and its application for up to 96 weeks was safe in
patients with ADV-resistant HBV and multiple-drug failure. Lu et
al (27) compared the effects of
TDF monotherapy or TDF plus ETV combination therapy for hepatitis B
patients with a partial VR to ETV. In their study, the complete
viral suppression rate after 6 and 12 months was similar for the
TDF monotherapy and TDF plus ETV combination therapy groups.
Furthermore, the VR to TDF monotherapy was
comparable to that of combination therapies employing TDF plus
other NS analogs. Park et al (28) compared the efficiency of TDF
monotherapy and TDF plus LAM in 81 patients. These patients were
ADV-resistant and exhibited only a partial response to the
combination therapy with LAM plus ADV. However, the rates of VR at
6 and 12 months were not significantly different between the groups
treated with TDF monotherapy and TDF plus LAM combination therapy.
In addition, the treatment efficacy of TDF alone or TDF plus LAM
did not significantly depend on the presence of pre-existing ADV-
or LAM-resistant strains. A meta-analysis performed to compare the
efficacy of TDF and TDF-based combination therapy against
LAM-resistant HBV in patients with chronic hepatitis B confirmed
that TDF monotherapy is as efficient as TDF-based combination
therapy in maintaining viral suppression in these subjects
(29).
Despite the small number of patients included,
certain conclusions regarding the mutations responsible for TDF
resistance may be reached on the basis of analyses performed using
the sera of 6 patients had virologic breakthroughs whilst being
treated with TDF and 5 patients with poor curative effect after 24
weeks of TDF treatment. In 3 cases of virologic breakthrough, a
drug resistance gene was detected. One patient experienced
virologic breakthrough at 60 weeks of TDF treatment and they were
identified to be resistant to ADV (specific resistance loci: 181V,
236T). After 120 weeks of TDF treatment, the level of HBV DNA was
decreased, but the 181V and 236T ADV resistance loci were still
present and no new resistance loci were detected. Another patient
was treated with TDF for 48 weeks and the 181V, 204I and 236T
mutations responsible for drug resistance were detected. After TDF
treatment for 132 weeks, the level of HBV DNA was below the lower
limit of detection. There was a viral breakthrough in the third
patient switched to TDF after 120 weeks of treatment with LdT plus
TDF; the specific resistance loci 181V and 204V were identified. VR
was obtained by continuing TDF treatment for 156 weeks. Of two
patients with poor drug efficacy, one was treated with TDF alone
for 24 weeks; the 204V locus mutation responsible for the
resistance was detected. After 108 weeks of TDF monotherapy, the
HBV DNA was significantly reduced, but still detectable. In the
other patient, the drug resistance mutation 204I was detected and
TDF monotherapy was continued for 96 weeks, at which the VR was
achieved. 204T/V is a common resistance mutation site for
nucleoside analogues and, based on the above analysis, it may
represent the mutation site associated with TDF resistance.
In conclusion, the present study demonstrated that
TDF rescue treatment was efficient and safe for chronic hepatitis B
patients with a suboptimal response to ADV-based combination
therapy.
Acknowledgements
Not applicable.
Funding
The study was supported by the 12th five-year
National Science and Technology Major Project (grant no.
2012ZX10004-902).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XL, JL, YZ and XS conceived of and designed the
study, performed the literature search, acquired and analyzed the
data, and prepared the manuscript. CZ, YW, ZL and YJ assisted in
acquiring and analyzing the data, and performing the statistical
analysis. YZ, GL and XL performed the literature search, acquired
the data, and edited the manuscript. All authors have read and
approved the content of the manuscript.
Ethical approval and consent to
participate
The study protocol conformed to the ethical
guidelines of the Declaration of Helsinki and was approved by the
Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen
University (Guangzhou, China). Informed consent from the patients
regarding the use of their anonymized data was not required due to
the retrospective nature of the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ADV
|
adefovir
|
|
ALT
|
alanine aminotransferase
|
|
CK
|
creatine kinase
|
|
ETV
|
entecavir
|
|
LAM
|
lamivudine
|
|
LdT
|
telbivudine
|
|
NAs
|
nucleotide/nucleoside analogues
|
|
TDF
|
tenofovir disoproxil fumarate
|
References
|
1
|
Liaw YF, Kao JH, Piratvisuth T, Chan HL,
Chien RN, Liu CJ, Gane E, Locarnini S, Lim SG, Han KH, et al:
Asian-Pacific consensus statement on the management of chronic
hepatitis B: A 2012 update. Hepatol Int. 6:531–561. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Marcellin P, Zoulim F, Hezode C, Causse X,
Roche B, Truchi R, Pauwels A, Ouzan D, Dumortier J, Pageaux GP, et
al: Effectiveness and safety of tenofovir disoproxil fumarate in
chronic hepatitis B: A 3-year, prospective, real-world study in
france. Dig Dis Sci. 61:3072–3083. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen HL, Lee CN, Chang CH, Ni YH, Shyu MK,
Chen SM, Hu JJ, Lin HH, Zhao LL, Mu SC, et al: Efficacy of maternal
tenofovir disoproxil fumarate in interrupting mother-to-infant
transmission of hepatitis B virus. Hepatology. 62:375–386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kitrinos KM, Corsa A, Liu Y, Flaherty J,
Snow-Lampart A, Marcellin P, Borroto-Esoda K and Miller MD: No
detectable resistance to tenofovir disoproxil fumarate after 6
years of therapy in patients with chronic hepatitis B. Hepatology.
59:434–442. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Batirel A, Guclu E, Arslan F, Kocak F,
Karabay O, Ozer S, Turanli M and Mert A: Comparable efficacy of
tenofovir versus entecavir and predictors of response in
treatment-naive patients with chronic hepatitis B: A multicenter
real-life study. Int J Infect Dis. 28:153–159. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Petersen J, Heyne R, Mauss S, Schlaak J,
Schiffelholz W, Eisenbach C, Hartmann H, Wiese M, Boeker K, Loehr
HF, et al: Effectiveness and safety of tenofovir disoproxil
fumarate in chronic hepatitis B: A 3-year prospective field
practice study in germany. Dig Dis Sci. 61:3061–3071. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kozielewicz D, Halota W and
Wietlicka-Piszcz M: Tenofovir rescue therapy in chronic hepatitis B
patients who failed previous nucleoside analogue treatment. Hepatol
Int. 10:302–309. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jia H, Ding F, Chen J, Zhang Y, Xiang D,
Lian J, Zeng L, Yu L, Hu J, Li Y, et al: LAM add-on ADV combination
therapy or ETV monotherapy for CHB patients with suboptimal
response to ADV. Ann Hepatol. 14:175–180. 2015.PubMed/NCBI
|
|
9
|
Wang M, Da Y, Cai H, Lu Y, Wu L and Jia J:
Telbivudine myopathy in a patient with chronic hepatitis B. Int J
Clin Pharm. 34:422–425. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hannon H, Bagnis CI, Benhamou Y, Beaufils
H, Sullivan M, Brosgart C, Izzedine H, Poynard T and Deray G: The
renal tolerance of low-dose adefovir dipivoxil by
lamivudine-resistant individuals co-infected with hepatitis B and
HIV. Nephrol Dial Transplant. 19:386–390. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang J, Wei F, Wang LH, Hai-Bo YU, Zhi LU,
Wang Z, et al: Effects of different serum calcium levels on
vascular calcification and cardiovascular death in patients with
end-stage renal disease. J Tianjin Med University. 2017.(In
Chinese).
|
|
12
|
Sharma A, Thompson JA, Repaka A and
Mehnert JM: Ipilimumab administration in patients with advanced
melanoma and hepatitis B and C. J Clin Oncol. 31:e370–e372. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Song WJ and Lu YP: Characteristics of
liver histology and the correlated index in patients with chronic
hepatitis B and normal ALT levels. Chin Foreign Med Res. 2013.(In
Chinese).
|
|
14
|
Thapa BR and Walia A: Liver function tests
and their interpretation. Indian J Pediatr. 74:663–671. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim JH, Jung SW, Byun SS, Shin JW, Park
BR, Kim MH, Kim CJ and Park NH: Efficacy and safety of tenofovir in
nucleos(t)ide-naive patients with genotype C chronic hepatitis B in
real-life practice. Int J Clin Pharm. 37:1228–1234. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ayaz C, Celen MK, Dal T, Deveci O, Bayan
K, Mert D, Oruç E, Özcan N, Kandemir I and Dal MS: Tenofovir
disoproxil fumarate treatment in HbeAg-positive patients. Infez
Med. 23:31–35. 2015.PubMed/NCBI
|
|
17
|
Idilman R, Gunsar F, Koruk M, Keskin O,
Meral CE, Gulsen M, Elhan AH, Akarca US and Yurdaydin C: Long-term
entecavir or tenofovir disoproxil fumarate therapy in
treatment-naive chronic hepatitis B patients in the real-world
setting. J Viral Hepat. 22:504–510. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim BG, Jung SW, Kim EH, Kim JH, Park JH,
Sung SJ, Park BR, Kim MH, Kim CJ, Lee BU, et al: Tenofovir-based
rescue therapy for chronic hepatitis B patients who had failed
treatment with lamivudine, adefovir, and entecavir. J Gastroenterol
Hepatol. 30:1514–1521. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lo AO, Wong VW, Wong GL, Tse YK, Chan HY
and Chan HL: Efficacy of tenofovir switch therapy for
nucleos(t)ide-experienced patients with chronic hepatitis B.
Aliment Pharmacol Ther. 41:1190–1199. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lee S, Park JY, Kim DY, Kim BK, Kim SU,
Song K, Ku HJ, Han KH and Ahn SH: Prediction of virologic response
to tenofovir mono-rescue therapy for multidrug resistant chronic
hepatitis B. J Med Virol. 88:1027–1034. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Baran B, Soyer OM, Ormeci AC, Gokturk S,
Evirgen S, Akyuz F, Karaca C, Demir K, Besisik F, Onel D, et al:
Tenofovir disoproxil fumarate has a substantial efficacy against
multidrug-resistant strains of hepatitis B virus. Liver Int.
35:2265–2274. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Svarovskaia ES, Curtis M, Zhu Y,
Borroto-Esoda K, Miller MD, Berg T, Lavocat F, Zoulim F and
Kitrinos KM: Hepatitis B virus wild-type and rtN236T populations
show similar early HBV DNA decline in adefovir refractory patients
on a tenofovir-based regimen. J Viral Hepat. 20:131–140. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
van B, ömmel F, de Man RA, Wedemeyer H,
Deterding K, Petersen J, Buggisch P, Erhardt A, Hüppe D, Stein K,
Trojan J, et al: Long-term efficacy of tenofovir monotherapy for
hepatitis B virus-monoinfected patients after failure of
nucleoside/nucleotide analogues. Hepatology. 51:73–80. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
van B, ömmel F, Trojan J, Deterding K,
Wedemeyer H, Wasmuth HE, Huppe D, Möller B, Bock FJ, Feucht HH and
Berg T: Evolution of adefovir-resistant HBV polymerase gene
variants after switching to tenofovir disoproxil fumarate
monotherapy. Antivir Ther. 17:1049–1058. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Park HS, Lee DH, Heo J, Kim GH, Kang DH,
Song GA and Cho M: Correlation of HBV DNA level and viral
breakthrough during lamivudine therapy for chronic hepatitis B.
Korean J Hepatol. 12:173–183. 2006.(In Korean). PubMed/NCBI
|
|
26
|
Lim YS, Yoo BC, Byun KS, Kwon SY, Kim YJ,
An J, Lee HC and Lee YS: Switching tenofovir disoproxil fumarate
(TDF) plus entecavir combination therapy to TDF monotherapy is safe
and efficacious in patients with multiple drug-resistant chronic
hepatitis B: Randomized trial. J Hepatol. 64:S606–S. 2016.
View Article : Google Scholar
|
|
27
|
Lu L, Yip B, Trinh H, Pan CQ, Han SH, Wong
CC, Li J, Chan S, Krishnan G, Wong CC and Nguyen MH:
Tenofovir-based alternate therapies for chronic hepatitis B
patients with partial virological response to entecavir. J Viral
Hepat. 22:675–681. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Park JH, Jung SW, Park NH, Park BR, Kim
MH, Kim CJ, Lee BU, Jeong ID, Kim BG, Bang SJ and Shin JW: Efficacy
of tenofovir-based rescue therapy in lamivudine-resistant chronic
hepatitis B patients with failure of lamivudine and adefovir
combination. Clin Ther. 37:1433–1442. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang HL, Lu X, Yang X and Ning Q: Efficacy
of tenofovir-based rescue therapy in patients with
lamivudine-resistant hepatitis B virus: A systematic review and
meta-analysis. Clin Res Hepatol Gastroenterol. 40:447–456. 2016.
View Article : Google Scholar : PubMed/NCBI
|