Introduction
The acetabulum is an important component of the
human hip joint, as well as the largest movable joint and
weight-bearing joint in the human body, which can be easily
damaged. The acetabulum is characterized by well-developed
surrounding muscles and deep joint position, and it is surrounded
by complex nerves and blood vessels. The acetabular fracture is
mostly caused by central dislocation of hip joint, hip fracture or
pubic fracture involving the acetabulum and so on (1). The acetabular fracture is the
intra-articular fracture caused by high-energy injury, accounting
for approximately 3% of systemic fractures, which can cause damage
to articular surface in severe cases (2). There are complex and diverse acetabular
fractures. At present, major therapeutic methods in the western
medicine for acetabular fracture include conservative treatment and
operative treatment. However, acetabular fracture is often
accompanied with obvious displacement of more than 3 mm, so it is
hard for conservative treatment to reduce the femoral head and
acetabulum, and it can also lead to femoral head necrosis,
ankylosis and other hip dysfunctions (3). Since Judet et al (4) adopted operation in the treatment of
acetabular fracture for the first time, operative treatment for
acetabular fracture has been gradually matured and become a
mainstream therapeutic method in the Orthopedics Department in The
Second Affiliated Hospital of Luohe Medical College (Luohe, China).
Compared with conservative treatment, operative treatment is
characterized by a short treatment cycle, early weight-bearing time
and decreased incidence rate of complications (5). However, due to the high difficulty of
anatomy of acetabulum joint, difficulty in intraoperative exposure,
small operative and visual space and other adverse factors, how to
avoid the damage to the nerves, blood vessels and organs during
operation has become the key to successful operation. The treatment
of acetabular fracture aims to restore the biomechanical property
of pelvis and acetabulum through reconstructing the articular
surface and restoring the anatomical structure (6). However, there are certain limitations
in the conventional X-ray and computed tomography (CT) scan in the
operative plan, often leading to certain defects in the operative
plan. Improper operative plan may result in large exposure area,
long operation time, large amount of bleeding, ectopic ossification
and other complications (7).
Therefore, the precise, individualized and optimized preoperative
design is necessary for the operation.
In recent years, with the in-depth application of
computer-aided technology and three-dimensional (3D) printing
technique in the field of orthopedics, it has been gradually
transformed from virtual simulation to realistic simulation.
Clinicians, through the 3D printing model, can perform
minimally-invasive reduction of surgical site, optimize the
surgical approach and realize the precise design and simulation
operation, thereby reducing the operative complications and
ensuring a successful operation. In this study, therefore, the
clinical feasibility and application value of computer virtual
reduction combined with 3D printing technique in the patients with
complex acetabular fracture were investigated with conventional
operation as the control.
Patients and methods
General data
A total of 96 patients diagnosed with complex
acetabular fracture via complete pelvic CT scan in the Orthopedics
Department in The Second Affiliated Hospital of Luohe Medical
College from January 2016 to June 2017 were selected and randomly
divided into the routine operation group (n=48) and the 3D model
group (n=48) according to the admission number of the patients.
This study was approved by the Ethics Committee of The Second
Affiliated Hospital of Luohe Medical College, and all patients
voluntarily signed the informed consent.
Inclusion criteria
i) Patients diagnosed with complex hip fracture and
fracture of acetabular posterior wall via CT scan, including the
T-shaped type, anterior + transverse type, both-column type,
posterior wall type, posterior column + posterior wall type and
transverse + posterior wall type, ii) patients aged 18–64 years,
iii) patients with duration from injury to operation of less than 2
weeks, and iv) patients who voluntarily signed the informed
consent.
Exclusion criteria
i) Patients diagnosed with a single fracture via CT
scan, including posterior wall fracture, posterior column fracture,
anterior wall fracture, anterior column fracture and transverse
fracture, ii) patients with delayed acetabular fracture, iii)
patients aged <18 years, iv) patients complicated with vascular
injury, v) patients with poor mental status or confusion of
consciousness, vi) patients with severe cardiovascular or
cerebrovascular diseases or hepatorenal syndrome, or vii) patients
with immune system diseases.
Methods
Preoperative treatment
After admission, routine examinations, such as
biochemical and cardiopulmonary function examinations, were
performed for patients. Patients accompanied with posterior
dislocation of hip joint were treated with manual reduction of
acetabular dislocation and skeletal traction of 6–8 kg on the
femoral condyle on the affected side. The pelvic orthotopic,
obturator oblique and Iliac oblique X-ray films of patients were
examined, and CT plain scan and 3D reconstruction were performed.
Patients complicated with severe craniocerebral and chest and
abdominal injury should be treated first, followed by operative
treatment after the patient's condition became stable. Certain
anti-coagulant and anti-infection treatments were given before the
operation.
On the basis of the above examination, the patients
in the 3D model group were required to perform a 1.0 mm CT scan
(Aquilion 64; Toshiba, Tokyo, Japan) on the thin pelvic layer, and
the data were kept in the DICOM format. The editing function of
Mimisc14.0 (Materialise, Belgium) was used to separate the pelvis
from the femur bone and remove the femur image. The acetabular and
fracture blocks were used to increase the function of the area, and
the acetabular body and the fracture blocks with clinical
significance were completely divided. In the 3D modeling window,
the displacement and rotation function was used to restore each
fracture block. The data before and after reduction were saved as
STL format and sent to MakerBot Replicator 2 printer, and the 3D
physical fracture model was printed as 1:1. According to the 3D
physical fracture model before the reduction, the fracture
classification, fracture displacement degree, the deformation
direction, rotation direction and angle of each fracture block were
further defined. The whole process of the operation was simulated,
including the selection of the incision, the sequence of reduction,
the placement of the reduction clamp, the rotation direction, the
specific placement of the steel plate and screw, the angle, the
length, and the degree of pre-bending, so as to make it as
reasonable as possible to achieve effective strong fixation. The
effect of reduction was evaluated according to the 3D physical
fracture model after reduction.
Surgical approach
According to the acetabular fracture of patients in
the 3D physical model, the supine position or lateral floating
position was selected. Kocher-Langenbeck approach was selected for
the posterior column fracture accompanied with posterior wall
fracture and transverse fracture accompanied with posterior wall
fracture, ilioinguinal approach was selected for the anterior
fracture accompanied with transverse fracture, and
anterior-posterior combined approach was selected for the
both-column fracture. The approach for T-shaped fracture was
designed based on the patient's fracture morphology.
Operation methods
In the 3D model group, after tracheal intubation and
general anesthesia, the hip on the affected side of patients was
underlaid for 45 degrees in a hemi-lateral position, and the
internal surface and anterior column of the pelvis were exposed via
the ilioinguinal approach. The hip on the affected side was pushed
forward until 90 degrees in a lateral position, and the internal
surface, anterior and posterior columns and posterior wall of the
pelvis were exposed via the Kocher-Langenbeck approach. Then the
pre-bent steel plate was inserted into the fracture site and fixed
with the pre-designed screws. The operation was completed after the
intraoperative X-ray fluoroscopy displayed good reduction and
fixation of the fracture. In the control group, the conventional
reduction and fixation of acetabular fracture were performed after
X-ray fluoroscopy and CT scan.
Postoperative treatment
The broad-spectrum antibiotics were applied for 24 h
after operation, and the low-molecular-weight heparin was
subcutaneously injected for 2 weeks. The muscle contraction
function on the affected side was exercised 1 day after operation.
The knees and hip joints on the affected side were exercised 3 days
after operation, and they could be moved actively at 2 weeks.
Patients could exercise out of bed protectively at 4 weeks.
Weight-bearing activity was strictly forbidden within 3 months.
After 3 months, patients could gradually take full weight-bearing
activity according to their recovery status.
Evaluation indexes
Operation time (min): The time from skin incision to
suture in both groups was recorded.
Amount of intraoperative bleeding (ml) (8): Amount of intraoperative bleeding =
(intraoperative amount of liquid absorbed by the gauze + amount of
liquid sucked by the autologous blood transfusion equipment +
amount of liquid sucked on the wound surface) - amount of washing
liquid.
Times of intraoperative fluoroscopy (times):
Fluoroscopy was performed during operation to effectively observe
the reduction of fracture or internal fixation status of
patients.
Incidence rate of postoperative complications (%)
(9): After operation, the incidence
rate of such complications as inflammatory response, iatrogenic
neurological symptoms, loss of reduction, ectopic ossification and
traumatic arthritis were recorded in both groups.
Score of reduction quality of acetabular fracture
(points): X-ray examination was performed for review 3 days after
operation, and the reduction of fracture was evaluated according to
the Matta imaging scoring criteria (10). Evaluation criteria: Excellent,
residual displacement of fracture <1 mm; good, residual
displacement of fracture = 2–3 mm; and poor, residual displacement
of fracture >3 mm.
Hip joint function score (points): The hip joint
function was evaluated based on the Harris score (11) at 6 months after operation. Evaluation
criteria: A total of 100 points (excellent, >90 points; good,
80–89 points; fine, 70–79 points; and poor, <70 points).
Statistical analysis
Statistical Product and Service Solutions (SPSS)
17.0 (SPSS, Inc., Chicago, IL, USA) was used for statistical
analysis. Measurement data were expressed as mean ± standard
deviation (mean ± SD), and t-test was used. Enumeration data were
expressed as percentage, and Chi-square test was adopted. P<0.05
suggested that the difference was statistically significant.
Results
Comparisons of general data and
acetabular fractures of patients in two groups
There was no statistically significant difference
between the two groups in sex, average age, average injury time and
acetabular fracture classification (P>0.05) (Tables I and II).
 | Table I.Comparison of general data of patients
in two groups. |
Table I.
Comparison of general data of patients
in two groups.
|
| Sex | Age (years) | Time from injury to
operation (days) |
|---|
|
|
|
|
|
|---|
| Groups | Male | Female | Mean | Range | Mean | Range |
|---|
| 3D model group | 34 | 14 | 43.44±4.53 | 20–61 | 10.12±1.41 | 4–14 |
| Routine operation
group | 32 | 16 | 41.88±4.97 | 19–62 | 10.41±1.06 | 5–14 |
|
χ2/t-test | 0.19 | 1.61 |
| 1.29 |
|
| P-value | 0.65 | 0.11 |
| 0.19 |
|
 | Table II.Comparison of acetabular fractures of
patients in two groups. |
Table II.
Comparison of acetabular fractures of
patients in two groups.
| Characteristics | 3D model group | Routine operation
group | χ2
test | P-value |
|---|
| Acetabular fracture
classification |
| T-shaped
fracture | 7 | 8 | 0.07 | 0.77 |
| Posterior column
fracture accompanied with posterior wall fracture | 12 | 11 | 0.06 | 0.81 |
| Both-column
fracture | 8 | 9 | 0.07 | 0.79 |
| Transverse fracture
accompanied with posterior wall fracture | 11 | 12 | 0.06 | 0.81 |
| Anterior fracture
accompanied with transverse fracture | 7 | 6 | 0.08 | 0.76 |
| Acetabular marginal
fracture | 2 | 1 | 0.34 | 0.55 |
| Compression fracture
of articular surface of acetabulum | 2 | 1 | 0.34 | 0.55 |
| Associated
injury |
| Limb fracture | 26 | 25 | 0.04 | 0.83 |
| Chest and abdominal
injury | 13 | 14 | 0.05 | 0.82 |
| Craniocerebral
injury | 8 | 9 | 0.07 | 0.78 |
Comparison of operation time, amount
of intraoperative bleeding and times of intraoperative fluoroscopy
between the two groups
There were statistically significant differences in
the comparison of operation time and times of intraoperative
fluoroscopy between the two groups of patients (P<0.05). The
amount of intraoperative bleeding in the 3D model group was
significantly less than that in the routine operation group,
showing a statistically significant difference (P<0.05). The
number of intraoperative fluoroscopy was compared between the two
groups, and the difference was statistically significant
(P<0.05) (Table III).
 | Table III.Comparison of operation time, amount
of intraoperative bleeding and times of intraoperative fluoroscopy
between the two groups (mean ± SD). |
Table III.
Comparison of operation time, amount
of intraoperative bleeding and times of intraoperative fluoroscopy
between the two groups (mean ± SD).
| Groups | n | Operation time
(min) | Amount of
intraoperative bleeding (ml) | Times of
intraoperative fluoroscopy |
|---|
| 3D model group | 48 | 210.8±54.5 | 1,147.2±235.4 |
6.8±1.6 |
| Routine operation
group | 48 | 296.4±66.2 | 1,832.5±268.1 | 12.4±2.1 |
| t-test |
| 6.92 | 13.31 | 14.7 |
| P-value |
| <0.001 | <0.001 | <0.001 |
Comparison of incidence rate of
postoperative complications between the two groups
There were 1 case of inflammatory response, 1 case
of iatrogenic neuropathy, 1 case of heterotopic ossification and 2
cases of traumatic arthritis in the 3D model group. In the routine
operation group, there were 6 cases of inflammatory reaction, 5
cases of iatrogenic nerve symptoms, 3 cases of heterotopic
ossification and 4 cases of traumatic arthritis. The number of
postoperative complications was compared between the two groups,
and the difference was statistically significant (P<0.05)
(Table IV).
 | Table IV.Comparison of the number of patients
with postoperative complications between the two groups. |
Table IV.
Comparison of the number of patients
with postoperative complications between the two groups.
| Groups | n | Inflammatory
response | Iatrogenic
neurological symptoms | Ectopic
ossification | Traumatic
arthritis |
|---|
| 3D model group | 48 | 1 | 1 | 1 | 2 |
| Routine operation
group | 48 | 6 | 5 | 3 | 4 |
| χ2
test |
|
| 9.66 |
|
|
| P-value |
|
| 0.002 |
|
|
Comparison of excellent-good rates of
reduction quality of acetabular fracture and hip joint function
after operation between the two groups
There were no statistically significant differences
in the comparison of excellent-good rates of reduction quality of
acetabular fracture at 3 days after operation and hip joint
function at 6 months after operation between the two groups of
patients (P>0.05) (Table V).
 | Table V.Comparison of excellent-good rates of
reduction quality of acetabular fracture and hip joint function
after operation between the two groups (%). |
Table V.
Comparison of excellent-good rates of
reduction quality of acetabular fracture and hip joint function
after operation between the two groups (%).
| Groups | n | Reduction quality of
acetabular fracture | Hip joint
function |
|---|
| Routine operation
group | 48 | 77.08 (17/20) | 83.33
(19/21) |
| 3D model group | 48 | 81.25 (20/19) | 87.5 (24/18) |
| t-test |
| 0.25 | 0.33 |
| P-value |
| 0.61 | 0.56 |
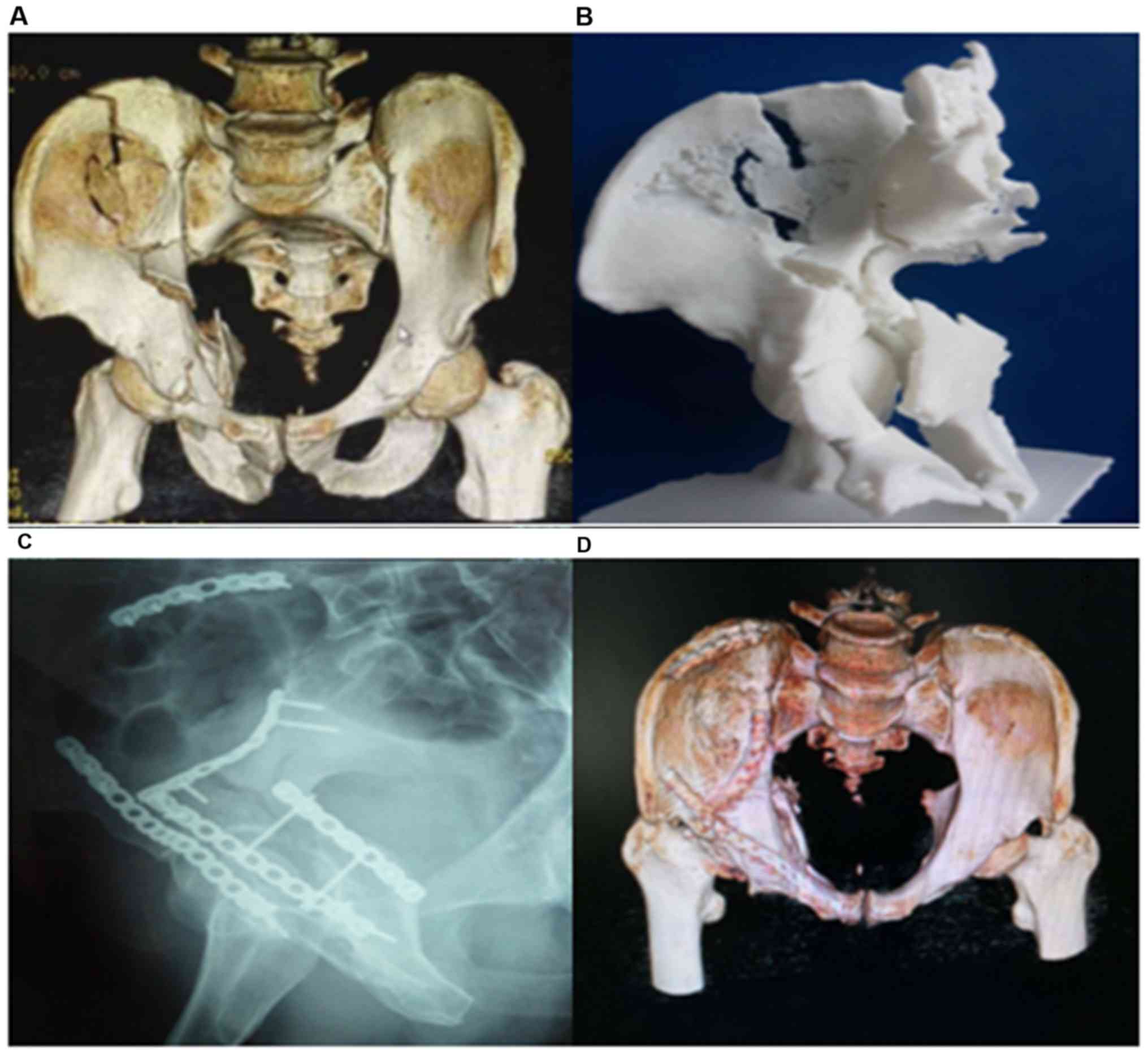
Acetabular fracture morphology before
and after operation
The acetabular fracture morphology before and after
operation is shown in Fig. 1. The
patient suffered from severe right acetabular fracture (Fig. 1A). The 3D physical model could
clearly display the acetabular fracture morphology in patients
(Fig. 1B), thus helping observe the
fracture type and design the operative plan. The reduction of
acetabular fracture in patients was good at 3 days after operation
(Fig. 1C). CT scan at 6 months after
operation showed that the acetabular morphology was well restored
(Fig. 1D).
Discussion
The acetabulum is in a deep concave hemispherical
shape with a radius of ~1.8 cm, which is composed of anterior
column and posterior column intersecting and overarching 60
degrees. There are abundant muscles, nerve networks, blood vessels
and anastomotic branches around the acetabulum, the physiological
structure is complex, and more bleeding and porosis will be easily
caused after injury (12). With the
rapid social development, increasingly more patients suffer from
comminuted and irregular acetabular fractures due to high-energy
impact (traffic accidents, falling objects and heavy impact). At
the same time, fractures in other sites or organ injuries in the
thoracic cavity, abdominal cavity and pelvic cavity are concurrent,
seriously affecting the quality of life of patients and increasing
the social burden. Currently, the acetabular fracture is divided
into simple fracture and complex fracture according to the
principle of Letournel E. The simple fracture includes fractures in
the anterior wall, anterior column, posterior wall, posterior
column and transverse site, while the complex fracture includes
posterior column fracture accompanied with posterior wall fracture,
transverse fracture accompanied with posterior wall fracture,
anterior column or anterior wall fracture accompanied with
posterior column or transverse fracture, T-shaped fracture and
both-column fracture. Operative treatment is a preferred choice for
clinicians, which, in particular, can better realize the anatomical
reduction and fixation, and recover the function early for complex
fracture with dislocation. However, operative treatment of
acetabular fracture is also faced with many difficulties, such as
the complex anatomical structure, selection of surgical approach,
complex reduction and severe postoperative complications. How to
improve the quality of operation, shorten the treatment time,
reduce the incidence rate of postoperative complications and
restore the physiological function of patients is the key to the
treatment of patients with acetabular fracture.
With the development of X-ray, CT technique and so
on, clinicians can conduct the simple 2D image analysis for the
complex and comminuted fractures, but the fracture morphology
cannot be reflected intuitively. According to Schreiner et
al (13), clinicians are limited
by factors such as the angle of the fracture site or overlapping
fracture patches and occlusion, which often leads to long operation
time, excessive blood loss and uneven joint surface, resulting in
high incidence of postoperative complications. Therefore, the
simple 2D X-ray examination and CT scan fail to meet the clinical
needs of orthopedics.
The acetabular fracture is mostly an articular
surface fracture, and the local bone shape is irregular, so
multi-angle and all-round observation is needed before the
operative plan is developed. Computer virtual technique overcomes
the shortcomings of 2D images, such as the lack of stereoscopic
effect and overlapping among tissues. Computer simulation reduction
technique can reconstruct the stereoscopic and intuitional 3D model
of the acetabular fracture through X-ray examination and CT scan,
and observe from any angle through such functions as translation
and rotation (14), which can help
clinicians, especially those with inadequate clinical experience,
understand the disease more comprehensively and develop therapeutic
regimen. Computer virtual technique provides the virtual
therapeutic environment for clinicians and simulates the clinical
operation steps, and site and angle of internal fixation, which,
compared with conventional operation, is characterized by
intuition, no damage, visualization and repeatability (15). Moreover, computer virtual technique
can develop an individualized therapeutic regimen based on the
condition of patients, and improve the clinical effect and
postoperative life of patients, which has great value of social
generalization.
As one of the important reforms in the medical
field, 3D printing technique is a bridge between computer virtual
technique and realistic clinical operation. The 3D physical model
displaying the acetabular fracture of patients perfectly can
clearly identify the fracture line, broken bone fragment and its
positional relation. In particular, the steel plate and screw can
be selected for the quadrilateral and acetabular reduction and
fixation according to the 3D physical model of acetabular fracture,
followed by pre-bending treatment before operation, thus
effectively reducing the operation time, improving the safety and
optimizing the operative plan (16).
Results of this study revealed that the operation
time, amount of intraoperative bleeding and times of intraoperative
fluoroscopy in 3D model group were significantly reduced, and
differences were statistically significant compared with routine
operation group (P<0.05). The incidence rate of postoperative
complications in the 3D model group had a statistically significant
difference compared with that in the routine operation group
(P<0.05). Besides, no statistically significant differences were
found in the Matta imaging score at 3 days after operation and
Harris score at 6 months after operation between the two groups
(P>0.05). The above results indicate that computer virtual
reduction combined with the 3D printing technique can obviously
reduce the operation time, amount of intraoperative bleeding and
incidence rate of postoperative complications of patients without
adverse effects on the postoperative acetabular healing and
function of patients. It can reduce the error and the surgical
injury during the operation. There was no adverse effect on
postoperative recovery of joint function. The main reason is that
computer virtual reduction combined with the 3D printing technique
can accurately restore the operative plan designed before operation
and improve the accuracy and safety of operation, and the operation
is simple and less time-consuming, making up for defects of the
existing method of screw implantation. However, there are also some
shortcomings in computer virtual reduction combined with the 3D
printing technique. Firstly, high-quality CT images are required
for the operation to improve the accuracy of model and avoid the
operative error. Lou et al (17) considered that 3D objects can improve
the clinical practice ability to a certain extent, but this
technology cannot reflect the soft tissue, blood vessels, nerves
and other conditions of the bone injury site. In the process of
operation, the guidance of experienced clinicians is needed.
Secondly, it is the skeletal structure that is scanned and printed
in the operation, excluding the soft tissues, blood vessels and
nerves, around the bone. Therefore, the operative plan design
differs from the actual plan implemented during operation, and
experienced clinicians are needed for guidance. Thirdly, the 3D
printing of pelvis takes a long time, so it is not applicable for
emergency patients. Therefore, clinician cannot rely completely on
the operative plan designed in advance during operation, but should
provide the corresponding treatment based on the actual condition
of patients. There are some limitations in this study. Due to the
short study time, the number of cases included in this study is not
that large. It can prove the advantage of the computer virtual
restoration in combination with the 3D printing to a certain
degree, but its application effect remains to be tested by time and
patients, which will be the focus of our future research. We will
continue to add clinical cases and long-term follow-ups to provide
guidance for the development of computer virtual reset combined
with the 3D printing technology in clinic.
In conclusion, computer virtual technique can
provide the individualized operative plan for patients, and 3D
printing technique creates a bridge between virtual technique and
realistic operation. Their combination can remarkably improve the
safety and accuracy of clinical operation, which has a higher
clinical application value and great social significance.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LW and XZ were involved in the conception and design
of the study. KL and PC drafted the manuscript. LW, XZ and SZ
recorded and analyzed the basic data of patients. KL, PC and JL
were responsible for CT scan analysis. LW and GW were in charge of
surgical approach and statistical analysis. The final version was
read and approved by all the authors.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Second Affiliated Hospital of Luohe Medical College (Luohe,
China). Signed informed consents were obtained from the patients
and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Keil H, Beisemann N, Schnetzke M, Vetter
SY, Swartman B, Grützner PA and Franke J: Intraoperative assessment
of reduction and implant placement in acetabular
fractures-limitations of 3D-imaging compared to computed
tomography. J Orthop Surg Res. 13:782018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ma L, Zhou Y, Zhu Y, Lin Z, Chen L, Zhang
Y, Xia H and Mao C: 3D printed personalized titanium plates improve
clinical outcome in microwave ablation of bone tumors around the
knee. Sci Rep. 7:76262017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Liu X, Zeng CJ, Lu JS, Lin XC, Huang HJ,
Tan XY, Cai DZ and Orthopedics DO: Application of 3D printing and
computer-assisted surgical simulation in preoperative planning for
acetabular fracture. Nan Fang Yi Ke Da Xue Xue Bao. 37:378–382.
2017.(In Chinese). PubMed/NCBI
|
|
4
|
Judet R, Judet J and Letournel E:
Fractures of the acetabulum: classification and surgical approaches
for open reduction. Preliminary report. J Bone Joint Surg Am.
46:1615–1646. 1964. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Uei H, Tokuhashi Y, Maseda M, Nakahashi M,
Sawada H, Matsumoto K and Miyakata H: Exploratory analysis of
predictors of revision surgery for proximal junctional kyphosis or
additional postoperative vertebral fracture following adult spinal
deformity surgery in elderly patients: A retrospective cohort
study. J Orthop Surg Res. 13:2522018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Deng C, Ni WD, Guo SQ, Luo G, Shui W and
Qiao B: Operative treatment of delayed acetabular fractures through
combined anterior and Kocher-Langenbeck approaches. Zhonghua Wai Ke
Za Zhi. 56:196–200. 2018.(In Chinese). PubMed/NCBI
|
|
7
|
Clough TM, Alvi F and Majeed H: Total
ankle arthroplasty: What are the risks? Bone Joint J 100-B.
1352–1358. 2018. View Article : Google Scholar
|
|
8
|
Cao D, Zhang S, Yang F, Shen K and Tan Z:
Hidden blood loss and its influencing factors after percutaneous
kyphoplasty surgery: A retrospective study. Medicine (Baltimore).
97:e04352018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
de Vries LM, Neve WC and Steens J:
Prosthesis retention after an infected hip prosthesis: Hip
fractures versus primary total hip prosthesis, data from 1998–2015.
J Bone Jt Infect. 3:118–122. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bücking TM, Hill ER, Robertson JL, Maneas
E, Plumb AA and Nikitichev DI: From medical imaging data to 3D
printed anatomical models. PLoS One. 12:e01785402017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ho D, Squelch A and Sun Z: Modelling of
aortic aneurysm and aortic dissection through 3D printing. J Med
Radiat Sci. 64:10–17. 2017. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Porter SE, Russell GV, Dews RC, Qin Z,
Woodall J Jr and Graves ML: Complications of acetabular fracture
surgery in morbidly obese patients. J Orthop Trauma. 22:589–594.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schreiner AJ, Schmidutz F, Ateschrang A,
Ihle C, Stöckle U, Ochs BG and Gonser C: Periprosthetic tibial
fractures in total knee arthroplasty - an outcome analysis of a
challenging and underreported surgical issue. BMC Musculoskelet
Disord. 19:3232018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Maini L, Verma T, Sharma A, Sharma A,
Mishra A and Jha S: Evaluation of accuracy of virtual surgical
planning for patient-specific pre-contoured plate in acetabular
fracture fixation. Arch Orthop Trauma Surg. 138:495–504. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang YC, Ma Y, Yu WZ, Li YF and Liu YH:
Application of the computer-assisted virtual reduction combined
with 3D printing technique in acetabular fractures. Zhongguo Gu
Shang. 30:627–632. 2017.(In Chinese). PubMed/NCBI
|
|
16
|
Arabnejad S, Johnston B, Tanzer M and
Pasini D: Fully porous 3D printed titanium femoral stem to reduce
stress-shielding following total hip arthroplasty. J Orthop Res.
35:1774–1783. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lou Y, Cai L, Wang C, Tang Q, Pan T, Guo X
and Wang J: Comparison of traditional surgery and surgery assisted
by three dimensional printing technology in the treatment of tibial
plateau fractures. Int Orthop. 41:1875–1880. 2017. View Article : Google Scholar : PubMed/NCBI
|