Introduction
Scar carcinoma is also known as Marjolin's ulcer,
named after the French surgeon Marjolin who first described a tumor
arising from burn scars in 1928 (1).
Initially, the term ‘Marjolin's ulcer’ specifically referred to
squamous cell carcinoma that developed after the malignant
transformation of ulcers after a burn. However, as a result of
in-depth study of the malignant transformation of other cellular
components in scars after burns and case reports on the malignant
transformation of scars caused by non-burn wounds, the current
concept of Marjolin's ulcer encompasses all malignant tumors that
primarily occur in body surface ulcers (1,2). In
terms of histopathological classification, Marjolin's ulcers now
are classified into squamous cell carcinoma, basal cell carcinoma,
melanoma, sarcoma and other rare cell types (2,3). The
majority of Marjolin's ulcers are squamous cell carcinomas,
followed by basal cell carcinoma and melanoma (1). The malignant transformation rate was
reported as 1–2% (4).
In general, Marjolin's ulcer remains the most common
type of malignancy occurring in deep partial-thickness or
full-thickness burn wounds that do not receive any surgical
treatment. Other causes include pressure sores, venous ulcers,
chronic osteomyelitis, unhealed wounds resulting from various
causes and scars that have undergone repeated ulceration (5). The disease course of Marjolin's ulcer
is long and is usually accompanied by ulcer formation. The typical
Marjolin's ulcer is easy to diagnose based on a history of unhealed
scar ulcers and characteristic local clinical presentations
(6,7). However, atypical cases are easily
ignored initially or misdiagnosed as general scar ulcers. At
present, the most effective treatment method for Marjolin's ulcer
is surgery. Radiotherapy is recommended for patients who cannot
undergo surgery or is used for consolidation treatment after
surgery. Chemotherapy is not generally considered an effective
therapeutic method for Marjolin's ulcer. In addition, the exact
pathogenesis of Marjolin's ulcer remains to be fully elucidated.
The inflammatory irritation hypothesis and immune deficiency
hypothesis are the generally accepted theories at present (8). However, a recent study has indicated
that Marjolin's ulcer mainly exhibit infiltrating growth along the
direction of tension. Therefore, tension stimulation is considered
a potential factor in the development and progression of Marjolin's
ulcer (9).
Marjolin's ulcers have been described by numerous
previous studies. However, due to the lack of large-scale studies,
the reported aetiology and clinical characteristics, as well as
treatment methods and effects vary considerably (5,10,11). For
instance, the recurrence times of Marjolin's ulcers vary between
studies; certain studies have reported the mean recurrence time of
4.66±2.07 months, while others have reported recurrence times of
3–10 months with a mean of 5.4 months, and still others have
reported recurrence in 6–11 months with a mean of 8.8 months
(3,12–14). To
further elucidate the features of this pathology, the present study
retrospectively analyzed the aetiology, clinical characteristics
and therapeutic efficiency in patients with Marjolin's ulcer who
were admitted to and treated at the Institute of Burn Research of
Southwest Hospital (third Military Medical University, Chongqing,
China) between January 2013 and December 2017. The present study
aimed to provide information that may aid in the establishment of
clinical practice guidelines for the diagnosis and treatment of
Marjolin's ulcer.
Materials and methods
Data collection
The clinical data of 140 Marjolin's ulcer patients
who were admitted to and treated at the Institute of Burn Research,
Southwest Hospital, the Third Military Medical University
(Chongqing, China) between January 2013 and December 2017 were
collected. All of the cases were confirmed by pathological
examination (for patients who were hospitalized several times due
to recurrence, only data from the first hospitalization were
collected). Among these patients, only 65 patients were followed
up, and data regarding their recurrent conditions were
statistically analyzed. The following factors of all patients were
considered in the statistical analysis: i) Demographic data,
including gender, age at initial injury or primary disease onset,
and age at the onset of Marjolin's ulcer; ii) clinical
characteristics, including initial injury or primary disease,
latency period, lesion location, lesion type, lesion area and
pathological type; iii) presence of bone invasion and lymph node
metastasis of tumor cells; and iv) treatment methods and prognosis,
mainly including the number of surgeries, surgical methods.
Statistical analyses
Values are expressed as the mean ± standard
deviation. The analyses were performed using SPSS 18.0 statistical
software (SPSS, Inc., Chicago, IL, USA). The correlation between
age at onset of initial injury or disease and the length of the
latency period were examined using Spearman correlation analyses.
The presence of bone invasion for different primary lesion
locations were examined using chi-square tests or Fisher's exact
test. The age at onset between male and female was analyzed using
t-test. The time to recurrence of Marjolin's ulcer for different
lesion locations was analyzed using the Kaplan-Meier method.
P<0.05 was considered to indicate statistical significance.
Results
Demographic characteristics
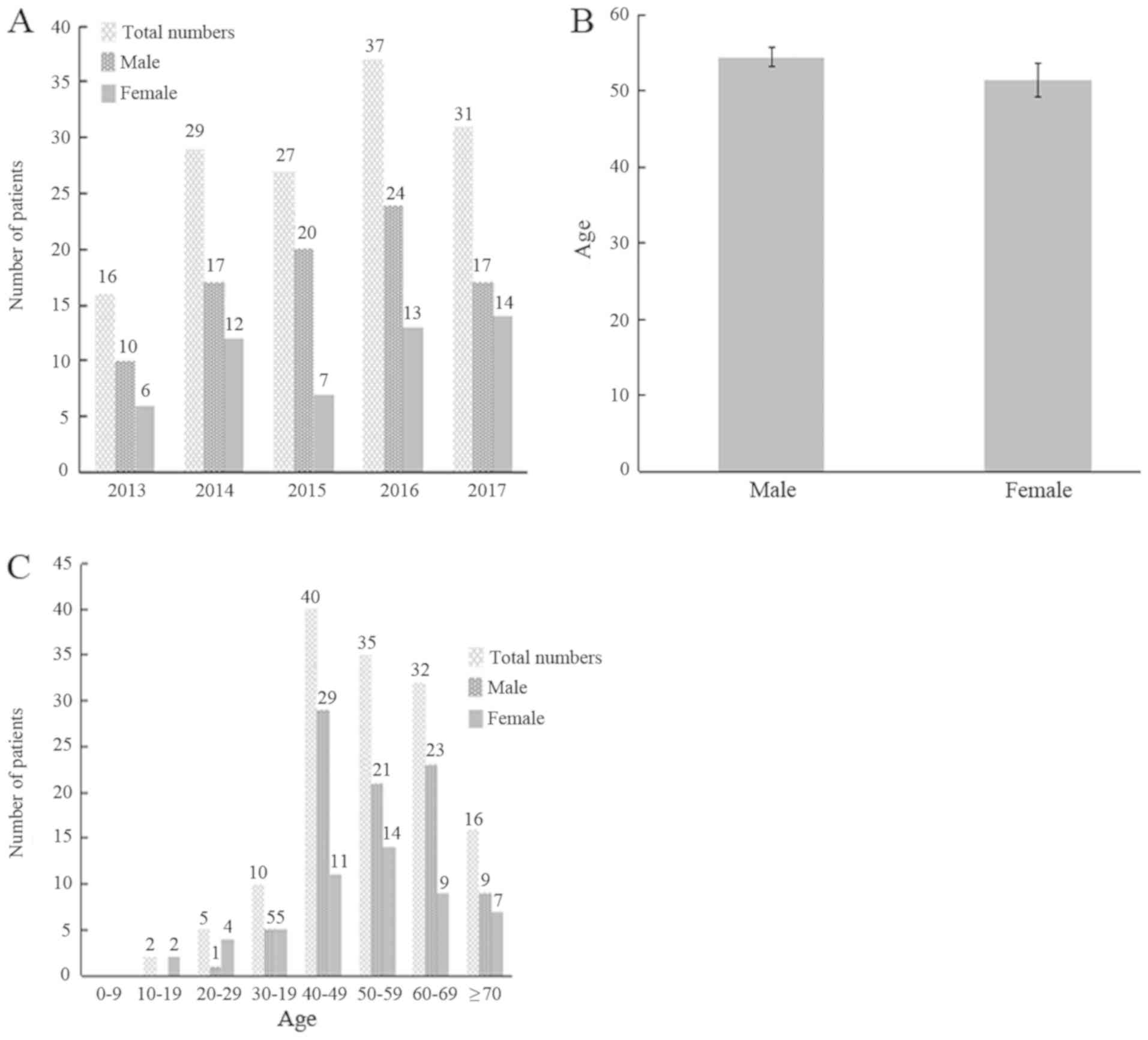
The cohort of 140 Marjolin's ulcer patients
comprised 88 males (62.9%) and 52 females (37.1%), and the
male-to-female ratio was ~1.7:1.0. The number of patients and the
male-to-female ratio exhibited large variations in different years
(Fig. 1A). The majority of the
patients resided in the local province (n=81, 57.9%) and ~40% of
the patients (n=56) came from adjacent provinces, including Guizhou
(22.2%), Sichuan (15.7%) and Hubei (2.1%), while only few patients
(n=3, 2.1%) came from more distant provinces. The age at onset of
Marjolin's ulcer ranged from 15–85 years, and the mean age at onset
was 53.3±1.2 years. The age at the onset of Marjolin's ulcer was
54.4±1.3 years in males and 51.4±2.3 in females, and the difference
was not statistically significant (P>0.05; Fig. 1B). In the present study, none of the
Marjolin's ulcer patients were aged <10 years. Within the
patient population, the subgroup with the age range of 40–49 years
was largest, followed by the group aged 50–59 years, while the
group aged 10–19 years was the smallest. For males, the age range
with the largest population was still 40–49 years, while the
smallest population was that with the age range of 20–29 years. For
females, the group with the age range of 50–59 years was the
largest, while the 10–19-year group was the smallest (Fig. 1C).
Histological types and lesion
characteristics
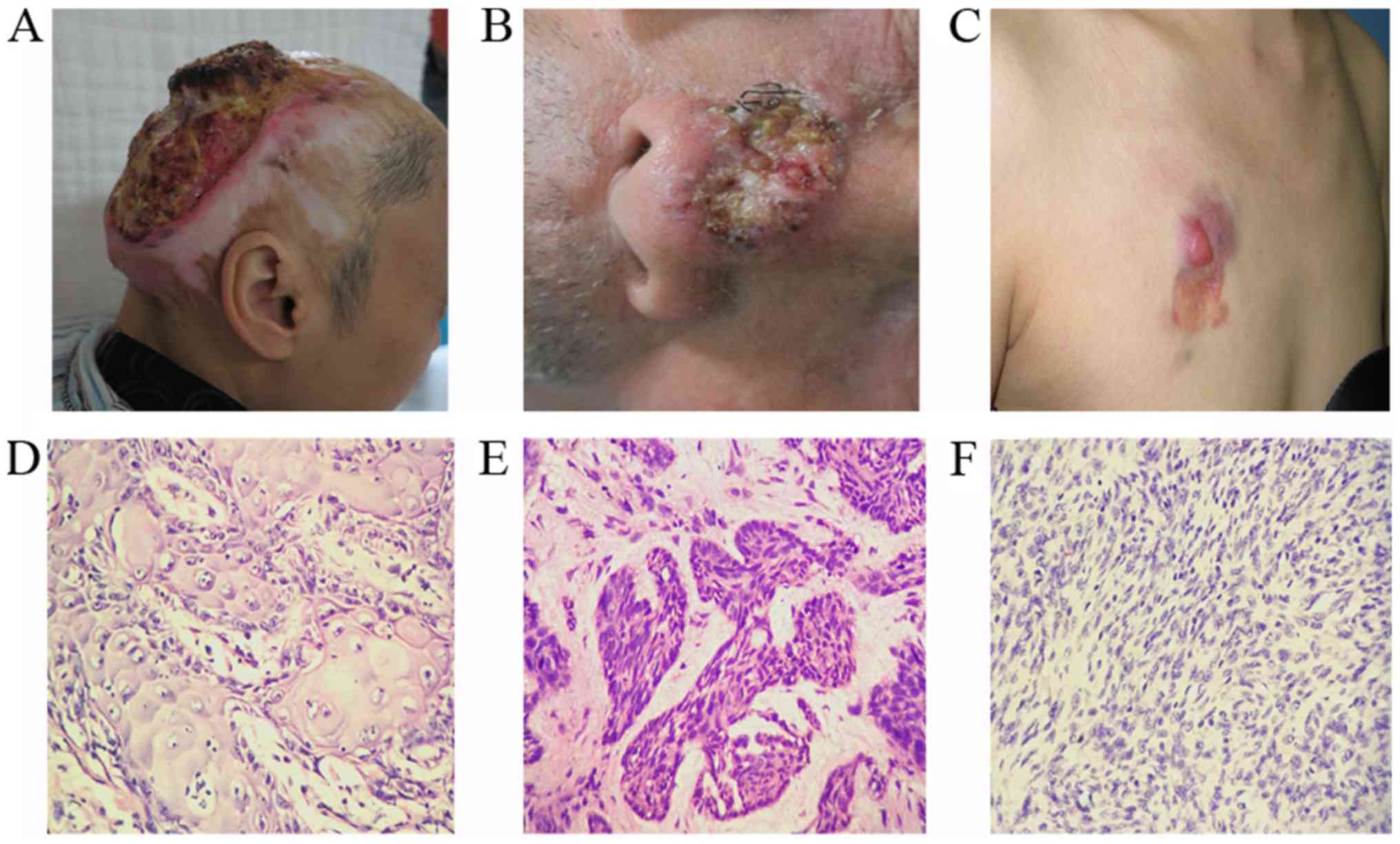
The majority of the 140 Marjolin's ulcer patients
had squamous cell carcinomas (n=123, 87.9%), followed by basal cell
carcinomas (n=10, 7.1%), dermatofibrosarcoma protuberans (n=6,
4.3%) and adenocarcinoma (n=1, 0.7%). Representative images of
lesions are provided in Fig. 2. In
three cases of squamous cell carcinoma, the patients had two
locations of invasion on the body; in one case of squamous cell
carcinoma, the patient had 3 locations of invasion, while all
others had one location of invasion. Overall, Marjolin's ulcer
mainly occurred on the lower limbs (42.1%), followed by the head
and neck (34.5%), whereas the perineum had the lowest incidence
(2.1%). The lesion types in the 6 cases of dermatofibrosarcoma
protuberans were all painless masses. The lesion types of other
Marjolin's ulcers were infiltrative ulcers (n=66, 49.3%) or
cauliflower-like masses (n=68, 50.7%); the difference in the
incidence between these two types was not large. The lesion areas
ranged from l-625 cm2 and the mean area was 71.3±7.7
cm2. In the majority of cases, the lesion area was
>10 cm2 and ≤50 cm2 (35.7%), followed by
the ≤10 cm2 (22.9%) group and the >50 cm2
and ≤100 cm2 group (20.0%). Only 5% of the cases had
lesion sizes of >200 cm2 (Table I).
 | Table I.Distribution of histological types,
lesion areas and lesion locations of Marjolin's ulcer. |
Table I.
Distribution of histological types,
lesion areas and lesion locations of Marjolin's ulcer.
| Characteristic | N (%) |
|---|
| Histological
type |
|
| Squamous
cell carcinoma | 123 (87.9) |
| Basal
cell carcinoma | 10
(7.1) |
|
Dermatofibrosarcoma
protuberans | 6
(4.3) |
|
Adenocarcinoma | 1
(0.7) |
| Lesion area
(cm2) |
| ≤10 | 32
(22.9) |
| >10
and ≤50 | 50
(35.7) |
| >50
and ≤100 | 28
(20.0) |
| >100
and ≤200 | 23
(16.4) |
|
>200 | 7
(5.0) |
| Lesion location |
| Head,
face and neck | 50
(35.7) |
| Upper
limb | 13
(9.3) |
| Lower
limb | 61
(43.6) |
|
Trunk | 10
(7.1) |
|
Perineum | 3
(2.1) |
| Hip | 8
(5.7) |
Primary aetiology, age and latency
period
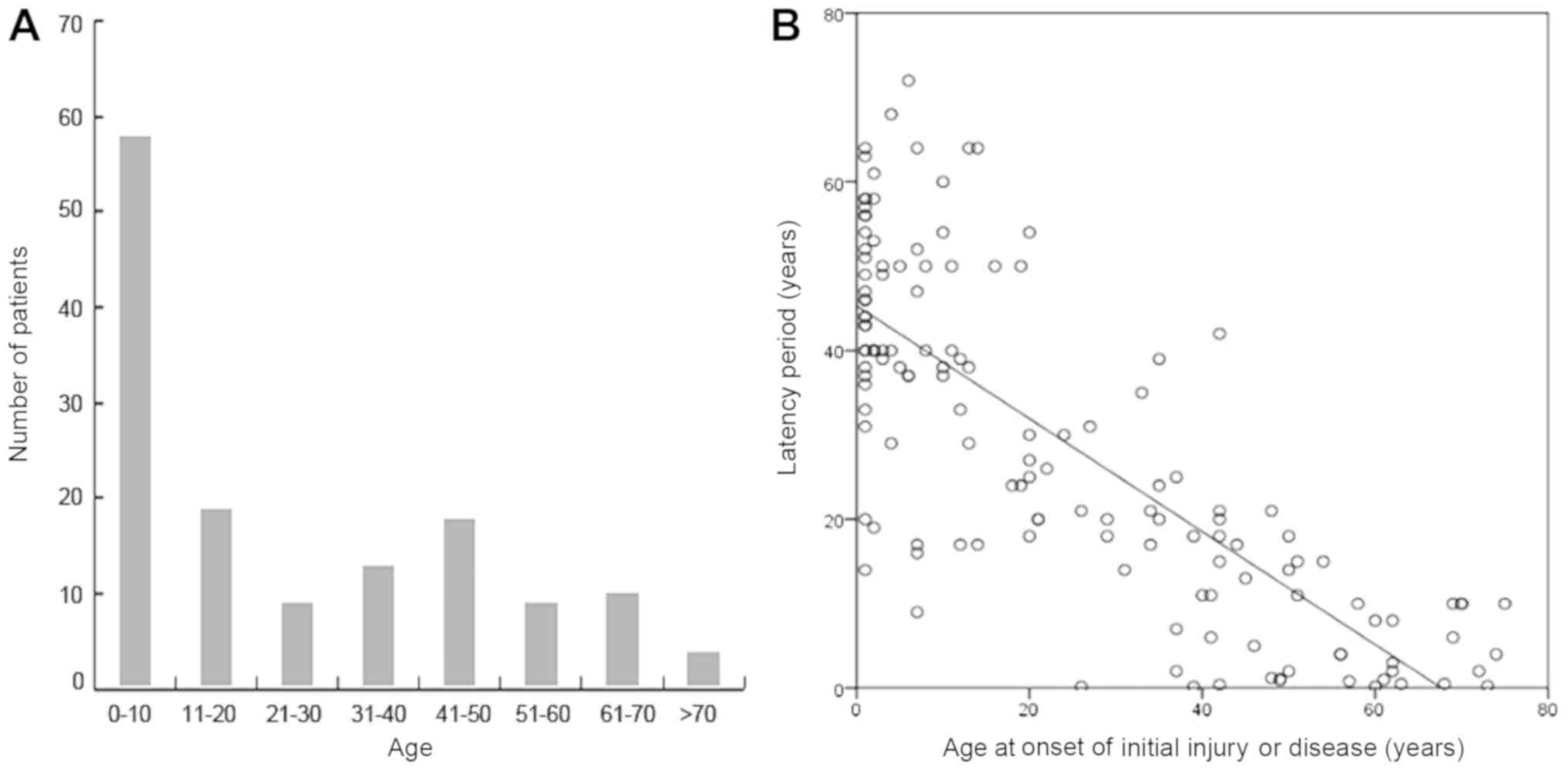
Among the patients of the present study, the most
common type of initial injury was flame burns, followed by skin
masses (defined as original masses located in the epidermis, dermis
or hypodermis, with or without pain and accompanying symptoms),
trauma, skin ulcerations caused by repeated scratching/friction and
scalding (Table II). Among the 140
patients, the age at initial injury or primary disease onset ranged
from 1–75 years, and the mean was 24.6±1.9 years. Most of the
initial injuries or diseases occurred at an age of ≤10 years
(41.4%), followed by 11–20 years (13.6%) and 41–50 years (12.9%;
Fig. 3A). Most of the patients had a
history of local ulcers after scar formation. The longest latency
period was 72 years and the shortest was 2 months, and the mean
period was 28.8±1.7 years. The majority of the patients had a
latency period of >1 year (92.1%) and only 11 patients (7.9%)
had a disease onset within 1 year (Table II). The patients' age at onset of
initial injury or disease exhibited a significant negative
correlation with the length of the latency period (r=−0.780,
P<0.01; Fig. 3B).
 | Table II.Distribution of the causes of initial
injury or disease and latency periods of Marjolin's ulcer. |
Table II.
Distribution of the causes of initial
injury or disease and latency periods of Marjolin's ulcer.
| Characteristic | N (%) |
|---|
| Initial injury or
disease |
|
| Flame
burn | 63 (45.0) |
| Skin
mass | 22 (15.7) |
|
Trauma | 20 (14.3) |
| Skin
scratch/friction ulceration | 14 (10.0) |
|
Scald | 12 (8.6) |
| Skin
infection | 3
(2.1) |
| Pigment
plaque | 2
(1.4) |
| Electric
burn | 2
(1.4) |
| Pressure
sore | 2
(1.4) |
| Latency period
(years) |
| ≤1 | 11
(7.9) |
|
>1 | 129 (92.1) |
Bone invasion of tumors and lymph node
metastasis
Among the 140 patients, 46 (32.9%) presented with
bone invasion by tumor cells; among them, 38 (27.1%) only had 1
bone invasion in only 1 location and 8 (5.7%) had 2 bone invasions.
Among the 50 cases of Marjolin's ulcer arising from head and neck
wounds, 28 had bone invasion, including 25 cases of skull invasion.
Among the 13 cases of Marjolin's ulcer arising from upper limb
wounds, 2 had bone invasion, and of the 61 cases with lesions from
lower limb wounds, 14 had bone invasion. Among the 10 cases with a
primary lesion location on the trunk, 1 had bone invasion. Among
the 8 cases of Marjolin's ulcer arising from hip wounds, 1 had bone
invasion. The percentage of bone invasion in patients with head and
neck Marjolin's ulcers was significantly higher than that in
patients with other wound locations (χ2=20.802,
P<0.01; Table III). Among the
25 patients with skull invasion, 9 had dura invasion, including 4
cases with brain tissue invasion. A total of 33 patients in this
group had regional lymph node enlargement diagnosed on palpation,
which accounted for 23.6% of the total cases. Furthermore, 7
patients had lymph node enlargement in 2 locations: The popliteal
fossa and the inguen (Table IV). Of
the 25 cases with obvious enlargement, those with suspected
metastasis based on physical examination underwent lymph node
dissection. Only 5 patients (3.6%) had lymph node metastasis of
tumor cells and the positive rate of dissection was only 20%. Among
the 11 patients who had positive positron emission
tomography-computed tomography (PET-CT) examination results,
pathological examination of lymph nodes revealed tumor cell
metastasis in only 2 subjects, and the positive rate was 18.2%. The
other patients were all negative (Table
V).
 | Table III.Distribution of Marjolin's ulcer
patients with bone invasion in different locations |
Table III.
Distribution of Marjolin's ulcer
patients with bone invasion in different locations
| Tumour
locationa | Bone invasion | No invasion | Total |
|---|
| Head, face and
neck | 28b | 22 | 50 |
| Upper limb | 2 | 11 | 13 |
| Lower limb | 14 | 47 | 61 |
| Trunk | 2 | 8 | 10 |
| Perineum | 0 | 3 | 3 |
| Hip | 1 | 7 | 8 |
| Total | 47 | 98 | 145 |
 | Table IV.Distribution of patients with lymph
node metastasis. |
Table IV.
Distribution of patients with lymph
node metastasis.
| Location | Number of cases
with lymph node enlargement (n=33) (%) | Number of cases
with tumour cell metastasis (n=5) (%) |
|---|
| Neck | 3
(9.1) | 2 (40) |
| Mandible | 1
(3.0) | 0 |
| Axilla | 5
(15.2) | 0 |
| Inguen | 23 (69.7) | 3 (60) |
| Popliteal
fossa | 8
(24.2) | 0 |
| Inguen and
popliteal fossa | 7
(21.2) | 0 |
 | Table V.Accuracy rates of diagnosis of lymph
node metastasis using different methods. |
Table V.
Accuracy rates of diagnosis of lymph
node metastasis using different methods.
| Detection
method | Suspected
positive | Pathologically
confirmed positive | Positive rate
(%) |
|---|
| Clinical
diagnosis | 25 | 5 | 20 |
| PET-CT | 11 | 2 | 18.2 |
Treatment methods
Among the patients included in the present study,
116 received surgical treatment. The remaining 24 did not receive
surgery; of these, 14 refused surgery and 10 did not receive
surgical treatment due to considerable surgical difficulties and
high risks. Among the 116 patients who underwent surgery, 7
received palliative surgery and the other 109 cases received
surgery with extended lesion resection. The majority of the
patients required only 1 surgery and only few patients required 2
or more surgeries. Depending on the condition of the lesion after
resection, 76 patients received skin grafts, 23 received local skin
flap repair, 12 underwent amputation and 5 patients underwent
island skin flap repair (Table
VI).
 | Table VI.Distribution of the number of
surgeries, surgery types and methods for Marjolin's ulcer
patients. |
Table VI.
Distribution of the number of
surgeries, surgery types and methods for Marjolin's ulcer
patients.
| Characteristic | N (%) |
|---|
| Number of
surgeries |
|
| 0 | 24
(17.2) |
| 1 | 100 (71.4) |
| 2 | 13
(9.3) |
| 3 | 2
(1.4) |
| 4 | 1
(0.7) |
| Surgical type |
|
|
Palliative surgery | 7
(6.0) |
|
Extended resection | 109 (94.0) |
| Surgical
method |
|
| Skin
grafting | 76
(65.5) |
|
Autologous skin grafting | 75
(64.6) |
|
Allogeneic skin grafting | 1
(0.9) |
| Skin flap | 28
(24.1) |
| Local
skin flap | 23
(19.8) |
| Island
skin flap | 5
(4.3) |
| Amputation | 12
(10.4) |
Prognosis and recurrence
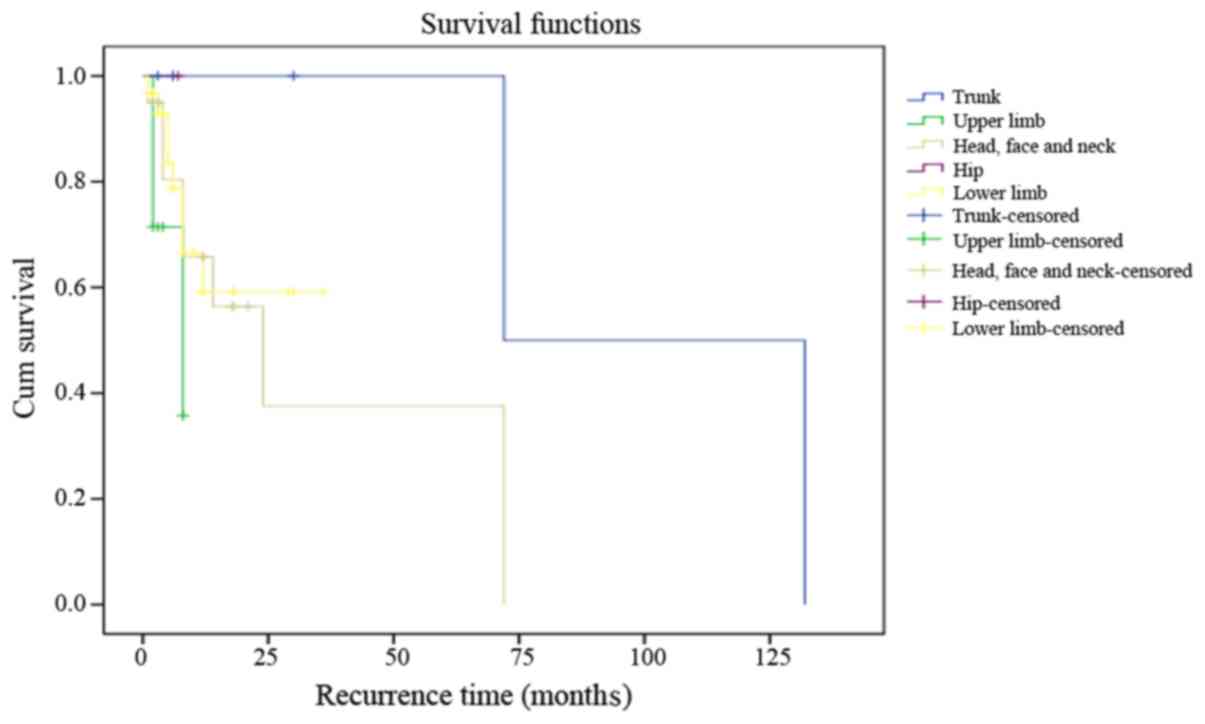
Among the 65 Marjolin's ulcer patients who received
follow-up, 22 had recurrence, including 9 cases with recurrence on
the head and neck, 3 cases on the upper limbs, 8 cases on the lower
limbs and 2 cases on the trunk (data not shown). No significant
differences in the recurrence rates of Marjolin's ulcer on
different body parts were identified according to the Kaplan-Meier
survival analysis (P>0.05; Fig.
4). The shortest recurrence time for Marjolin's ulcer was 1
month and the longest was 11 years; the mean period was 21.7±7.2
months. A total of 5 cases (22.7%) experienced recurrence after ≤3
months, another 5 had a recurrence time of >3 months and ≤6
months, another 5 cases had a recurrence time of >6 months and
≤12 months, 3 cases (13.6%) had a recurrence time of >1 year and
≤3 years and 4 cases (18.2%) had a recurrence time of >3 years
(Table VII).
 | Table VII.Distribution of the time to
recurrence of Marjolin's ulcer (n=22). |
Table VII.
Distribution of the time to
recurrence of Marjolin's ulcer (n=22).
| Recurrence time
(months) | N (%) |
|---|
| ≤3 | 5 (22.7) |
| >3 and ≤6 | 5 (22.7) |
| >6 and ≤12 | 5 (22.7) |
| >12 and ≤36 | 3 (13.6) |
| >36 | 4 (18.2) |
Discussion
The present study reported on 140 cases of
Marjolin's ulcer admitted and treated over 5 years, resembling a
significantly larger cohort than that reported by other studies
(4,10,15–17). The
following factors may explain for this high patient number: First,
our institution is located in southwest China, a region with a
relative low education level of the population where patients do
not sufficiently understand the severity of Marjolin's ulcer and
consequently do not seek timely treatment after scar ulceration.
Second, our institution is the largest burn and scar lesion
treatment center in southwest China, where a large number of
patients from various provinces seek treatment every year. Among
these 140 cases, squamous cell carcinoma was the major type of
Marjolin's ulcer, followed by basal cell carcinoma and
dermatofibrosarcoma protuberans, which was identical to the
distribution reported in similar studies (1,2,5,9).
However, a typical pathological type, malignant melanoma, which is
common in Western countries (1,6), was not
observed in the present study. A possible reason may be differences
in ethnicity and a lack of long-term sunlight exposure among the
population of southwest China. In addition, the male-to-female
ratio, age at initial injury and age at the first onset observed in
the present study were similar to those in certain previous studies
(2,18). Although the initial onset age did not
significantly differ between genders, the predilection age of male
patients was significantly lower than that of female patients.
Furthermore, the present study indicated that the mean latency
period for Marjolin's ulcer was 28.8±1.7 years with a median of
26.5 years, which were shorter than those reported in another study
(15). These results indicated that
the present study included more patients with shorter latency
periods than the previous one. In the present cohort, 11 patients
had a latency period of <1 year and 3 patients had a latency
period of 2 months. Marjolin's ulcer may occur on any part of the
body's surface, but they are commonly observed at specific sites. A
previous study reported that the lower limbs are the most common
site, followed by the head and neck, upper limbs, trunk, hips and
perineum (14). The predilection
sites of Marjolin's ulcer in the present study were similar to
those in other studies. However, Marjolin's ulcers in different
locations tended to have different histological types. The
histological type of Marjolin's ulcers on the lower limbs and the
head and neck was mainly squamous cell carcinoma, while those
occurring on the face were mainly basal cell carcinoma and those on
the trunk were mostly dermatofibrosarcoma protuberans.
In general, Marjolin's ulcer does not easily
metastasize for a considerable amount of time after their onset.
The lymphatic system is the primary pathway of metastasis. At
present, it remains controversial whether preventive lymph node
dissection should be performed for Marjolin's ulcer patients
(19). It is generally considered
that preventive lymph node dissection does not have any obvious
influence on tumor recurrence and should not be performed for this
purpose (13). However, according to
certain studies, the metastatic rate of lymph nodes in the lower
limb region is relatively high, and for cases of Marjolin's ulcer
without lymph node metastasis in the lower limb region, preventive
lymph node dissection should be considered (20). It has also been proposed that the
level of tissue differentiation may be used as a basis for
determining whether preventive local lymph node dissection should
be performed (21). Studies from
other countries have reported a rate of metastasis of Marjolin's
ulcer in local lymph nodes of 22% (2). However, a recent study from China
indicated that among 187 patients with lymph node enlargement, 64
underwent local lymph node dissection and only 18 developed tumor
cell metastasis to the lymph nodes (9). During the treatment of the 140 patients
in the present study, only 5 patients developed lymph node
metastasis (3.6%), yielding a low metastatic rate. In addition,
after the surgical dissection of 11 cases of lymph node metastasis
diagnosed by PET-CT, only two cases were discovered to be positive,
and the positive rate of PET-CT was only 18.1%. Therefore, it
appears reasonable that the decision to perform regional lymph node
dissection should be based on a comprehensive evaluation, including
the patient's systemic condition, tumor differentiation level,
lesion location, wound size, invasion depth and lymph node imaging
results.
At present, the most effective treatment method for
Marjolin's ulcer is surgery. Radiotherapy is often used for
inoperable patients or as a consolidating treatment after surgery.
In the present study, all of the post-operative patients with
completely healed wounds were advised to undergo local
radiotherapy; however, only a small proportion of the patients
chose to do so. In addition, patients who did not undergo surgery
were not advised to undergo radiotherapy due to the presence of
wounds. Extended lesion resection and amputation were the major
surgical methods applied. Extended resection usually includes the
areas >2 cm away from the ulcer tissues. In certain cases,
extension to 5 cm from the wound edge is recommended (22). The resection depth is determined by
the invasion level of the tumor cells, which may reach the
superficial layer of the deep fascia, the deep sarcolemma, the
muscle tissue or even the periosteum. Deep tissue invasion and/or
bone and joint invasion makes the radical resection of the lesion
difficult to complete. Radical resection may cause severe
impairment of limb function, and wounds cannot be covered after the
extensive resection of tumors; the requirement for such extensive
resection in Marjolin's ulcer patients is an indicator for
amputation (23). However, it is at
times difficult to determine whether bone destruction and
periosteal reaction detected on imaging result from inflammatory
infection or tumor cell invasion. Therefore, bone tissues with
suspected involvement may be excised to prevent recurrence caused
by residual tumors. The bone invasion locations of Marjolin's ulcer
have not been sufficiently evaluated by previous studies. Among the
46 patients with bone invasion in the present study, 25 had skull
bone invasion, suggesting that the skull is the bone that is most
susceptible to invasion of Marjolin's ulcer. Scalp Marjolin's
ulcers that invade the skull are difficult to completely excise and
have a high recurrence rate. In addition, as the surgical risk of
skull tissue invasion is high, the percentage of patients with
skull invasion who refuse surgery is also higher. Among the 25
Marjolin's ulcer patients with skull invasion in the present study,
9 refused surgery and 5 received palliative surgery. Together,
these groups represented 56% of the patients with skull invasion,
which is similar to the percentage reported in a previous study
(24). After the excision of
Marjolin's ulcer, wound repair and functional reconstruction are
key to improving life quality. It is generally considered that skin
graft repair should be used as much as possible. If bones and
tendons are exposed, skin flap repair should be performed. Local
skin flap repair should be used if possible, while island skin flap
graft repair is the second most desirable alternative. Free skin
flap repair should not be the common method of choice. Among the
116 patients who received surgery in the present study, 76 received
skin grafts, 28 received local skin flap or island skin flap
repair, and none underwent the complex free flap repair. In total,
71.4% of the patients only required one surgery. These results
indicate that skin grafting and simple skin flap repair are still
the preferred methods for wound repair after extended resection of
Marjolin's ulcer and provide the most satisfactory outcomes.
In the present study, the recurrence rates of
Marjolin's ulcers in different locations did not exhibit any
significant differences. This may be due to the limited sample size
and the number of cases that were lost to follow-up. However, among
the 22 cases of recurrence, 17 (77.3%) were on the head, neck and
lower limbs. Furthermore, the trend in recurrence time is another
characteristic of Marjolin's ulcer. Various studies have reported
that Marjolin's ulcer has a short recurrence time (12–14).
However, the present study indicated that the mean recurrence time
for Marjolin's ulcers was 21.7±7.2 months, and the recurrence time
was significantly longer than that reported in previous studies.
One possible reason for this discrepancy is that in the present
study, 4 cases had recurrence at >3 years after surgery (1 case
after 11 years and 3 cases after 6 years). Among the cases with
recurrence, the majority (68.1%) relapsed within 1 year after
surgery, suggesting that 1 year after surgery is the peak period of
recurrence and patients should be closely followed up and observed.
Furthermore, the recurrence rates in different body parts had no
significant differences in the present study.
In conclusion, the present retrospective study
indicated that Marjolin's ulcer mainly occurred in males and was
mainly scar carcinoma after a flame burn. The pathological type was
mainly squamous cell carcinoma. Autologous skin grafting and local
skin flap repair were the major repair methods used. The skull bone
was the site most susceptible to invasion.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural
Science Foundation of China (grant no. 81571898) and the New
Clinical Technology Plan for Military Medicine and War Trauma
Treatment of Southwest Hospital (grant no. SWH2016BZGFKJ-38).
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All the authors contributed extensively to the work
presented in this study. FX and YSH conceived and designed the
study. FX wrote the manuscript. Data analysis and interpretation,
revision and final approval of the study were performed by FX, HPS
and YSH.
Ethics approval and consent to
participate
This study was approved by the Institutional Review
Board of the Southwest Hospital, Third Military Medical University
(Chongqing, China).
Patient consent for publication
The patients whose images are shown in Fig. 2 provided informed consent for the
publication of these images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Onesti MG, Fino P, Fioramonti P, Amorosi V
and Scuderi N: Ten years of experience in chronic ulcers and
malignant transformation. Int Wound J. 12:447–450. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Das KK, Chakaraborty A, Rahman A and
Khandkar S: Incidences of malignancy in chronic burn scar ulcers:
Experience from Bangladesh. Burns. 41:1315–1321. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hahn SB, Kim DJ and Jeon CH: Clinical
study of Marjolin's ulcer. Yonsei Med J. 31:234–241. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chalya PL, Mabula JB, Rambau P, Mchembe
MD, Kahima KJ, Chandika AB, Giiti G, Masalu N, Ssentongo R and
Gilyoma JM: Marjolin's ulcers at a university teaching hospital in
Northwestern Tanzania: A retrospective review of 56 cases. World J
Surg Oncol. 10:382012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pekarek B, Buck S and Osher L: A
comprehensive review on Marjolin's ulcers. Diagnosis and treatment.
J Am Col Certif Wound Spec. 3:60–64. 2011.PubMed/NCBI
|
|
6
|
Bazaliński D, Przybekmita J, Barańska B
and Więch P: Marjolin's ulcer in chronic wounds-review of available
literature. Contemp Oncol. 21:197–202. 2017.
|
|
7
|
Kheiri B, Osman M and Al Hadidi S: From a
burn scar to malignancy! Marjolin's ulcer, a disease of wound
neglect. Oxf Med Case Reports. 2018:omy0442018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nthumba PM: Marjolin's ulcers: Theories,
prognostic factors and their peculiarities in spina bifida
patients. World J Surg Oncol. 8:1–5. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu Z, Zhou Y, Zhang P, Zhang M, Ren L,
Zeng J, Zhou J, Liang P and Huang X: Analysis of clinical
characteristics of 187 patients with Marjolin's ulcers. Zhonghua
Shao Shang Za Zhi. 32:293–298. 2016.(In Chinese). PubMed/NCBI
|
|
10
|
Sisti A, Pica Alfieri E, Cuomo R, Grimaldi
L, Brandi C and Nisi G: Marjolin's ulcer arising in a burn scar. J
Burn Care Res. 39:636–639. 2018.PubMed/NCBI
|
|
11
|
Fishman JR and Parker MG: Malignancy and
chronic wounds: Marjolin's ulcer. J Burn Care Rehabil. 12:218–23.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Altunay I, Cerman AA, Sakiz D and Ates B:
Marjolin's ulcer presenting with in-transit metastases: A case
report and literature review. Ann Dermatol. 27:442–445. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Choi JY, Bae YC, Nam SB and Bae SH: Impact
of disturbed wound healing after surgery on the prognosis of
Marjolin's ulcer. Arc Plast Surg. 40:198–202. 2013. View Article : Google Scholar
|
|
14
|
Aydogdu E, Yildirim S and AkSz T: Is
surgery an effective and adequate treatment in advanced Marjolin's
ulcer? Burns. 31:421–431. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jellouli-Elloumi A, Kochbati L, Dhraief S,
Ben Romdhane K and Maalej M: Cancers arising from burn scars: 62
cases. Ann Dermatol Venereol. 130:413–416. 2003.PubMed/NCBI
|
|
16
|
Fazeli MS, Lebaschi AH, Hajirostam M and
Keramati MR: Marjolin's ulcer: Clinical and pathologic features of
83 cases and review of literature. Med J Islam Repub Iran.
27:215–224. 2013.PubMed/NCBI
|
|
17
|
Shen R, Zhang J, Zhang F, DU Y, Liang W,
Xu L, DU X, Chen P and Chen X: Clinical characteristics and
therapeutic analysis of 51 patients with Marjolin's ulcers. Exp
Ther Med. 10:1364–1374. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yu N, Long X, Lujan-Hernandez JR, Hassan
KZ, Bai M, Wang Y, Wang X and Zhao R: Marjolin's ulcer: A
preventable malignancy arising from scars. World J Surg Oncol.
11:3132013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fernandes MG, Brandão M and Dias EM:
Marjolin's ulcer with axillary lymph node metastasis. Acta Med
Port. 31:5152018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dupree MT, Boyer JD and Cobb MW:
Marjolin's ulcer arising in a burn scar. Cutis. 62:49–51.
1998.PubMed/NCBI
|
|
21
|
Ozek C, Celik N, Bilkay U, Akalin T, Erdem
O and Cagdas A: Marjolin's ulcer of the scalp: Report of 5 cases
and review of the literature. J Burn Care Rehabil. 22:65–69. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bozkurt M, Kapi E, Kuvat SV and Ozekinci
S: Current concepts in the management of Marjolin's ulcers:
Outcomes from a standardized treatment protocol in 16 cases. J Burn
Care Res. 31:776–780. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Opara KO and Otene IC: Marjolin's ulcers:
A review. TNHJ. 11:107–111. 2011.
|
|
24
|
Onah II, Okwor B and Onuigbo WI:
Penetrating scalp Marjolin's ulcer involving bone and dura mater in
a Nigerian hospital: Case report and literature review. Burns.
36:e39–e43. 2010. View Article : Google Scholar : PubMed/NCBI
|