Introduction
White spot lesions (WSLs) are among the most common
side effects of orthodontic treatment, and the labial surfaces
around braces and gingival margins are the most common sites for
WSLs (1). The incidence of new WSLs
during orthodontic treatment has been reported to be 32.0–72.9%,
and the activity of cavitated lesions has been observed to increase
over the orthodontic treatment period (2,3). The
insertion of fixed appliances may considerably alter the oral
microenvironment, since it provides bacterial colonization and
accumulation areas for dental biofilm and fungi (4). It has been demonstrated that
Streptococcus (S.) mutans and
Lactobacillus are the major constituents of the pathogenic
bacterial flora in WSLs and dental caries (1).
Saliva is regarded as a microbial repository and
transport medium, which is affected by oral health status, as well
as the quantity and types of bacteria. Saliva is also considered to
contain innate immune factors and various salivary defense
proteins. Since secretory immunoglobulin A (sIgA) is a key antibody
in the salivary defense system (5),
it may respond to changes in the oral microenvironment during
orthodontic treatment. Furthermore, myeloperoxidase (MPO) and
lactate dehydrogenase (LDH) act as salivary markers of
periodontitis that are involved in periodontal metabolism, and the
activity of MPO and LDH is promoted in the initial period of
orthodontic treatment (6–8). However, the immune response during
long-term treatment has yet to be fully elucidated.
Various clinical studies have indicated that changes
in S. mutans or Lactobacillus are complex and
unpredictable during the first 2–6 months of orthodontic treatment
(4,9,10).
However, follow-up times have not previously been extended beyond 6
months, despite a typical orthodontic treatment lasting 18–36
months. The association between bacterial levels and innate immune
factors during long-term orthodontic therapy remains poorly
understood. The aim of the present prospective cohort study was to
observe the major pathogens and immune-associated proteins relevant
to long-term orthodontic treatment, and the association between
them. The present study illustrates that characteristics of the
oral microbial environment are affected by long-term orthodontic
treatment, and may provide information for the development of
potential management strategies for the side effects of orthodontic
treatment.
Materials and methods
Subjects and clinical procedures
The present study included 15 subjects who were
scheduled for fixed orthodontic therapy at the Department of
Orthodontics of West China Hospital of Stomatology (Sichuan
University, Chengdu, China). They had first presented at the
department between July 2013 and March 2014. In a preliminary
study, the mean bacterial DNA levels and standard deviations were
defined. The hypothesized mean value and standard deviations were
calculated with the assumption that the statistical significance
level was 0.05, and an adequate statistical power was typically
regarded as 0.9. Subsequently, the sample size required was
estimated to be 6 per group, and 15 cases were therefore included
in the present study to achieve an adequate sample size. All
experimental procedures were in accordance with the Declaration of
Helsinki. The study was entered in the Chinese Clinical Trial
Registry (no. ChiCTR-RCH-13003295). Prior to enrolment, informed
consent forms were signed by the patients, or by their guardians if
they were <18 years old.
The inclusion criteria were as follows: i) Patients
with >24 permanent teeth; ii) patient age between 14 and 20
years; and iii) a treatment period of >18 months. The exclusion
criteria were as follows: i) Any systemic or infectious diseases;
ii) any active carious lesions; iii) a history of smoking; and iv)
any antibiotic or hormone therapy within 1 month prior to or during
orthodontic treatment.
Patients were treated with fixed orthodontic
appliances (straight wire technique) and divided into two groups.
Treatment with either of two types of fixed orthodontic appliances
was performed by the orthodontist according to each patient's
situation and individual preference. The groups received two
different types of braces: Conventional braces (CB; HX, Shinye
Inc., Hangzhou, China; n=6) and self-ligating braces (SLB; Tomy,
Inc., Japan or Damon Q, Ormco, Orange, CA, USA; n=9). The
orthodontic procedure started with the implementation of NiTi wire
for the alignment and initial leveling stages, followed by
stainless steel wires for the subsequent stages. All subjects were
required to use fluoride-containing toothpaste according to oral
hygiene instructions.
Sample collection
For each patient, a self-contrast approach was
designed to assess changes in oral microbiota and salivary proteins
during the treatment period. A volume of 4 ml unstimulated whole
saliva was collected at four time-points: Prior to bonding (T1), 3
months after bonding (T2), 6 months after bonding (T3) and 18
months after bonding (T4), according to a previous study (4). The saliva was collected between 1:00
and 4:00 p.m. Participants were suggested to have lunch prior to
clinical visiting, and tooth brushing was required following
eating. For sample collection, participants were asked to refrain
from eating and drinking for ≥1 h prior to sample collection, and
they were required to rinse their mouths and sit quietly prior to
collection. Saliva was collected in sterile centrifugal tubes
within 15 min, and divided into 2 tubes: 1 ml for quantitative
polymerase chain reaction (qPCR) analysis and 3 ml for ELISA. The
saliva was then centrifuged at 22,673 × g for 10 min at 4°C, and
then stored at −80°C for subsequent detection.
DNA isolation and qPCR
The sediment of centrifuged saliva samples (1 ml)
was collected. Bacterial chromosomal DNA was extracted using a DNA
kit (cat. no. 56304; Qiagen GmbH, Hilden, Germany), according to
the manufacturer's protocol. A Nanodrop 2000 (Thermo Fisher
Scientific, Inc., Waltham, MA, USA) was used to assess the quality
and purity of the extracted DNA. DNA extracted from S.
mutans UA159 and Lactobacillus (L.)
acidophilus 4356 provided by the State Key Laboratory of
Oral Disease, Sichuan University (Chengdu, China) were used as
standards with 16S ribosomal RNA as a reference. The standard
curves were generated using a series of 10-fold dilutions from
10–106 copies (Fig.
1).
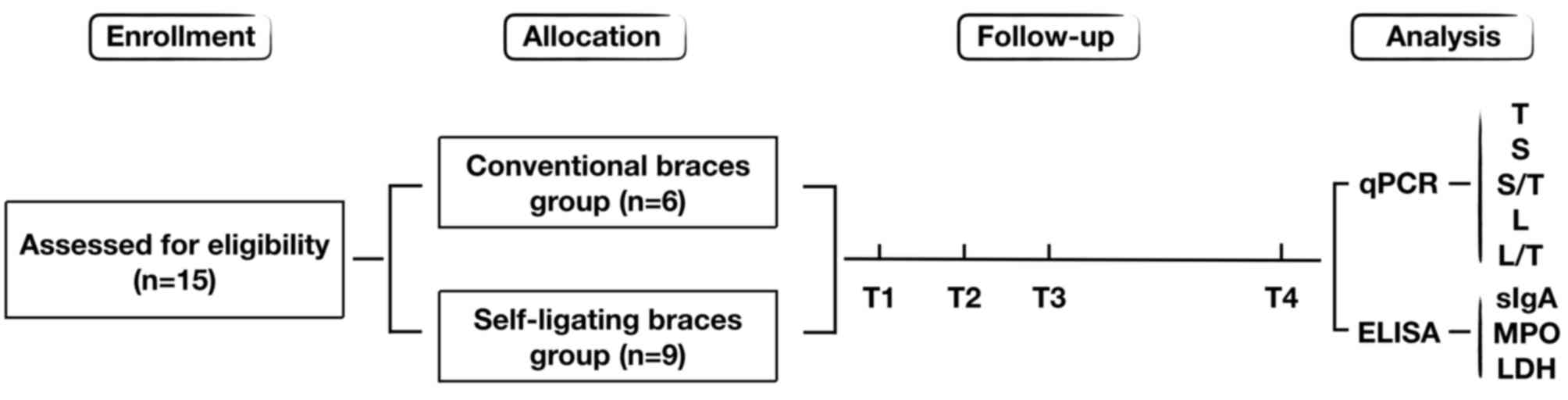
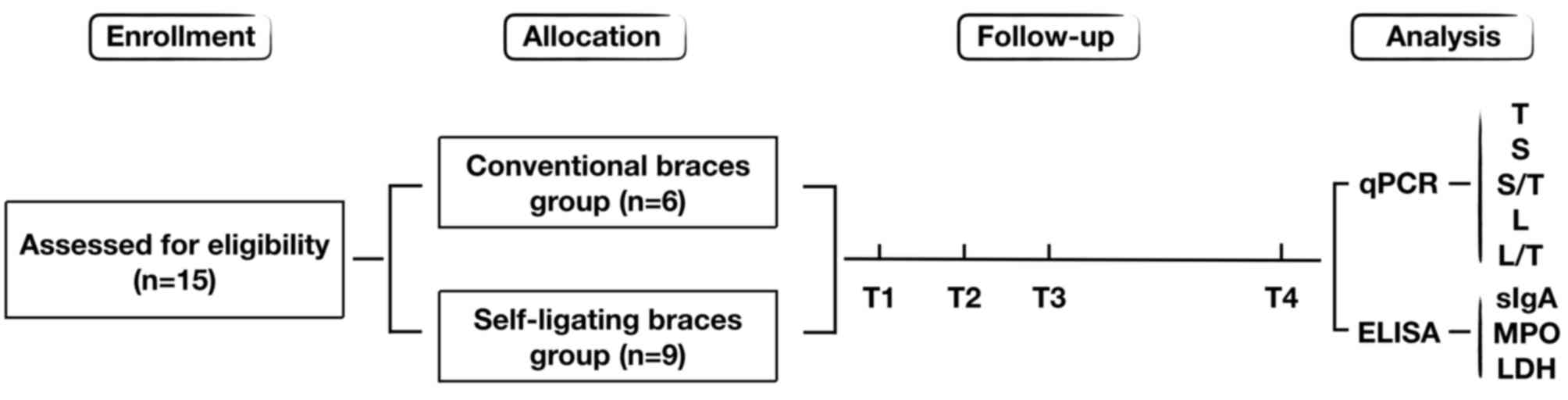 | Figure 1.Study flow diagram for bacterial
quantification. Flow diagram for the enrollment and progression of
the patients in the present study. Time-points: T1, Prior to
bonding; T2, 3 months after bonding; T3, 6 months after bonding;
and T4, 18 months after bonding. T, total bacteria DNA; S,
Streptococcus mutans DNA; L, Lactobacillus DNA; sIgA,
secretory immunoglobulin A; MPO, myeloperoxidase; LDH, lactate
dehydrogenase. |
A total of 20 ng DNA was used for each qPCR
analysis. qPCR was performed using the ABI 7300 system (Applied
Biosystems; Thermo Fisher Scientific, Inc.), and 16S ribosomal RNA
was used to quantify total bacteria (11). The specific primer for S.
mutans was designed according to the glucosyltransferase-I gene
(12). The Lacto-forward and
Lacto-reverse primers were used as the primary Lactobacillus
primers to represent all lactobacilli, as previously described
(13) (Table I). Reaction mixtures were subjected
to a standard qPCR program (n=3), according to the following
thermocycling conditions: 95°C for 5 min, then 40 cycles of 95°C
for 10 sec and 60°C for 30 sec, followed by 72°C for 10 min.
 | Table I.Primers for polymerase chain
reaction. |
Table I.
Primers for polymerase chain
reaction.
| Type | Name/direction | Sequence
(5′-3′) |
|---|
| Total bacteria | 16S-F |
GGTTAAGTCCCGCAACGAGC |
|
| 16S-R |
AGGGGCATGATGATTTGACG |
| Streptococcus
mutans | gtfB-F |
CTACACTTTCGGGTGGCTTG |
|
| gtfB-R |
GAAGCTTTTCACCATTAGAAGCTG |
|
Lactobacilli | Lacto-F |
TGGAAACAGRTGCTAATACCG |
|
| Lacto-R |
GTCCATTGTGGAAGATTCCC |
ELISA
For salivary sIgA, MPO and LDH determination, the
supernatant was collected from the centrifuged saliva sample (3
ml). Standard curves were generated and sample preparations were
performed according to the protocols of the Human Secretory
Immunoglobulin A/Myeloperoxidase/Lactate Dehydrogenase ELISA kits
(cat. nos. KB10115, KB11580 and KB12774, respectively; Shanghai
Jiang Lai Biotechnology, Inc. Shanghai, China). The absolute sample
densities were determined using linear regression equations with
multiplication of the results by the dilution factor.
Statistical analysis
Prior to bonding, a Student's t-test was used to
compare the amount of total bacteria (T), the ratio of S.
mutans (S) to total bacteria (S/T) and that of
Lactobacillus (L) to total bacteria (L/T) between males and
females, and between the two types of braces, in order to evaluate
the baseline characteristics. A repeated-measures analysis of
variance (ANOVA) was used to determine the time-dependent
differences in T, S, S/T, L and L/T with regard to sex or type of
braces. Independent comparisons of the T, S, S/T, L and L/T, as
well as salivary sIgA, MPO and LDH between different time-points
were performed using one-way ANOVA and least significant difference
analysis. Statistical analysis was performed using SPSS 13.0
software (SPSS, Inc., Chicago, IL, USA). Pearson's correlation
coefficient was determined to evaluate correlations between sIgA
and T, S/T or L/T. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
A total of 15 patients who met the inclusion
criteria and were enrolled in the present study. The mean age of
the patients was 16.64±2.03 years (17.00±1.91 years for the CB
group and 16.44±1.83 years for the SLB group). The male-to-female
ratio in the CB group and the SLB group was 1:2. At baseline, there
were no significant differences in T, S/T and L/T within the groups
between males and females.
qPCR analysis of salivary
bacteria
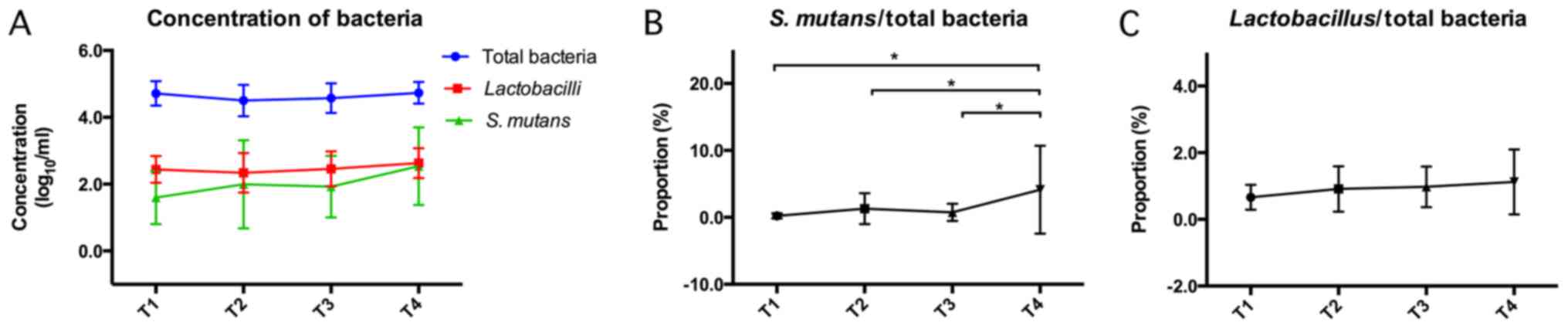
S. mutans and Lactobacillus levels in
saliva samples were evaluated using qPCR. The absolute levels of T,
S/T and L/T were evaluated from T1 to T4 (Fig. 2 and Table
II). The results demonstrated that there were no significant
differences in the amount of total bacteria over the 18-month
orthodontic treatment (Fig. 2A).
However, a slight but insignificant increase was observed in the
proportion of Lactobacillus from T1 to T4 (Fig. 2C). A significant increase in the
proportion of S. mutans was observed from month 6 to month
18 (P<0.05; Fig. 2B).
 | Table II.Bacterial levels at T1-T4. |
Table II.
Bacterial levels at T1-T4.
| Parameter | T1 | T2 | T3 | T4 |
|---|
| T
(Log10/ml) | 4.72±0.37 | 4.50±0.47 | 4.57±0.44 | 4.73±0.33 |
| S
(Log10/ml) | 1.55±0.74 | 1.95±1.80 | 1.89±0.89 | 2.52±1.17 |
| L
(Log10/ml) | 2.44±0.40 | 2.34±0.59 | 2.45±0.52 | 2.62±0.45 |
| S/T (%) |
0.21±0.38a |
1.29±2.30a |
0.75±1.28a | 4.14±6.56 |
| S/T-CB (%) |
0.45±0.52a |
2.84±2.95a |
1.50±1.75a | 8.64±8.14 |
| S/T-SLB (%) | 0.04±0.04 | 0.15±0.26 | 0.18±0.22 | 0.77±1.55 |
| L/T (%) | 0.66±0.37 | 0.91±0.68 | 0.97±0.61 | 1.12±0.97 |
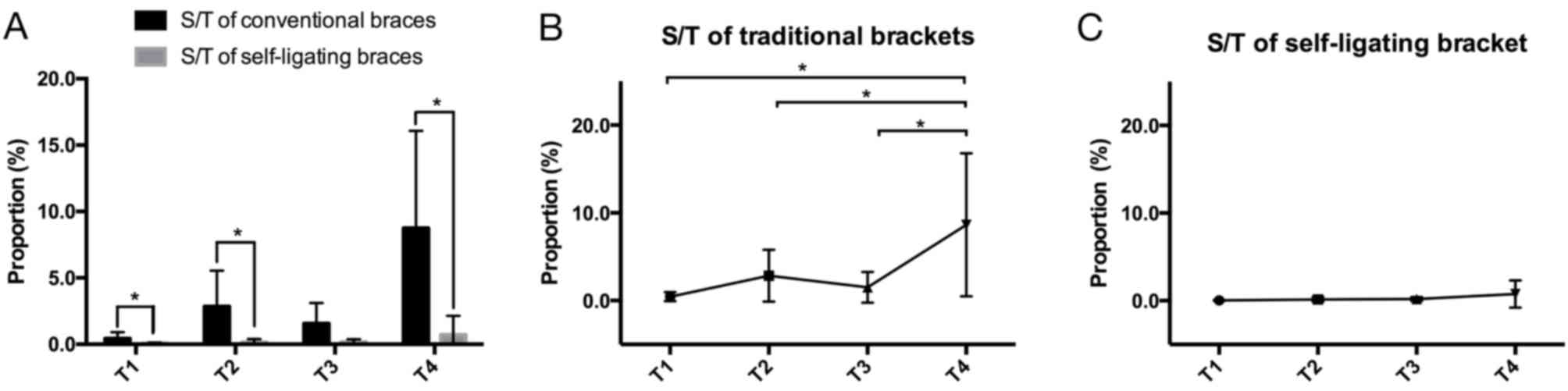
At T1, T2 and T4, there was a significant difference
in the proportion of S. mutans between the CB and SLB groups
(P<0.05; Fig. 3). The proportion
of S. mutans in patients with self-ligating braces was lower
compared with that in patients with conventional braces (Table II).
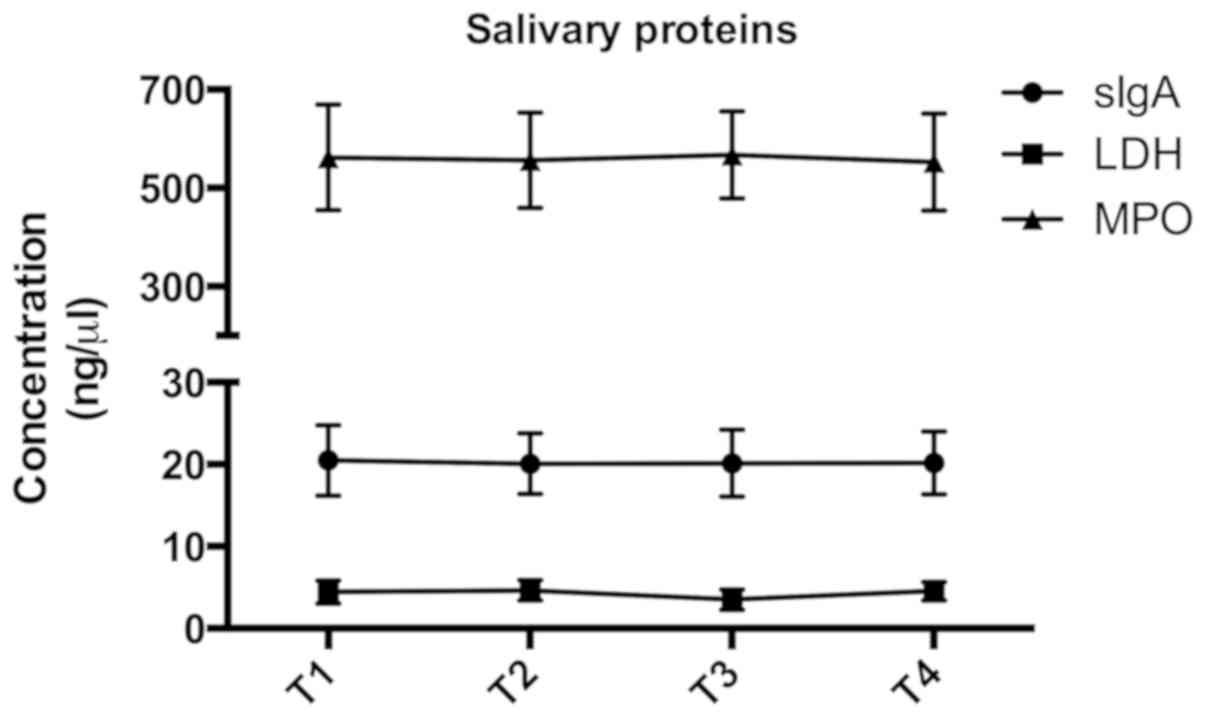
Analysis of salivary proteins
Standard curves and linear regression coefficients
of salivary sIgA, MPO and LDH were generated based on standard
densities and optical density values obtained by ELISA. All of
these parameters remained constant over the orthodontic treatment
period (P>0.05). The average concentration of salivary sIgA, MPO
and LDH was 20.22±3.97, 561.86±97.49 and 4.20±1.28 µg/ml,
respectively (Fig. 4). Furthermore,
Pearson's correlation analysis indicated no correlation between
sIgA and T, S/T or L/T (data not shown).
Discussion
In the present study, the levels of salivary total
bacteria, S. mutans and Lactobacillus of patients who
received fixed orthodontic treatment for ≥18 months were evaluated.
Salivary samples were harvested at four observation time-points, at
which salivary parameters, including sIgA, LDH and MPO, were
assessed. To the best of our knowledge, the present study was the
first to investigate the association between bacteria and
immune-associated proteins in patients undergoing long-term fixed
orthodontic treatment.
Orthodontic appliances include braces, wires and
attachments, which retain more food particles and provide retentive
sites for dental plaque. This makes it more difficult to maintain
oral hygiene, increasing the likelihood for WSLs and dental caries
to develop. Since S. mutans and Lactobacillus are
critical pathogenic bacteria in WSLs and dental caries,
demineralization was observed at 1 month after bonding (14). S. mutans and
Lactobacillus have been previously demonstrated to markedly
increase from month 3 to month 6 of orthodontic treatment (4,15). Other
studies have demonstrated no significant difference in the levels
of S. mutans and total bacteria within the first 3 months
(9,10). The observation times of these
previous investigations were restricted to the early stages of
orthodontic treatment. However, the majority of observations of WSL
or dental caries have been recorded following ~2 years of
orthodontic treatment, so that bacterial alterations may have been
missed in studies with a shorter duration. The present study was
designed as a long-term observation. The detection of S.
mutans and Lactobacillus in samples was performed by
qPCR, which is more rapid and sensitive for detecting specific
bacteria than the bacilli culture methods used in previous studies,
and they allow for the calculation of absolute numbers of bacteria
(11).
The number of total bacteria was predominately
stable over the 18-month period, suggesting that total bacterial
homeostasis was maintained during the orthodontic treatment. The
increase in S. mutans at 3 months was in line with a number
of previous studies (4,9,10,15).
However, the present study demonstrated that S. mutans
increased significantly over an 18-month treatment period in the CB
group, even when total bacteria did not increase. The accumulation
of S. mutans may cause WSLs and caries, and the present
results indicate that it is difficult to maintain oral hygiene over
a long treatment duration; WSLs occurred in some patients at this
time-point. S. mutans binds to the tooth surface by
producing water-insoluble glucans; its glucosyltransferases may
serve critical roles in the development of virulent dental plaque,
and enable S. mutans to thrive in the acidic environment and
escape the buffer function of saliva (16). In addition, surface roughness of
dental materials and S. mutans biofilm adhesion increase
with extended periods of treatment (17). As a result, the incidence of caries
increases with a longer treatment time, possibly due to the
sustained action and constant adhesion of S. mutans. This
indicates that long-term treatment is a critical risk factor for
the development of caries. Although it is difficult to define the
precise time range for the occurrence of dental caries, this result
suggests that particular attention should be paid to oral hygiene,
since the factors described above, including the acidogenic
ability, adhesion frequency and time of S. mutans,
contribute to the occurrence of caries when dental plaque
accumulates above a certain threshold.
Repeated measurement analyses demonstrated
significant differences between conventional and self-ligating
braces. Arch wires were placed in conventional braces using
ligature wires or elastomeric rings. Self-ligating braces restrict
wires into slots using self-ligating components that markedly
reduce friction and provide less space for plaque accumulation
around braces. It is easier to clear bacteria from self-ligating
braces, and differences in wire or accessory roughness may affect
biofilm adhesion, leading to a lower incidence of dental caries in
patients with self-ligating braces. In the present study, the
proportion of S. mutans in the CB and SLB groups exhibited a
slight but insignificant increase over the first 1–3 months, which
was consistent with previous studies (18,19). Of
note, the results of the present study demonstrated a significant
increase in the proportion of S. mutans only in patients
with conventional braces over the 18-month treatment period, while
the proportion of S. mutans in the SLB group remained at a
much lower level without any significant increasing. Similarly,
previous studies have demonstrated that the prevalence of patients
who develop WSLs after orthodontic treatment with self-ligating
braces was lower compared with that of patients with conventional
braces, and lower amounts of total bacteria, particularly oral
streptococci, were identified in the plaque of teeth bonded with
self-ligating braces (3,20). The present study provided evidence
from a long-term investigation that the self-ligating orthodontic
system is likely to have advantages over conventional braces in
terms of reduced biofilm adhesion and plaque accumulation, and
allows for better maintenance of oral hygiene through improving the
convenience of cleaning.
In dental caries, >7 dominant species of
Lactobacillus were identified as pathogenic bacteria
(21). In the present study,
Lactobacillus levels also displayed a slight increase from
T1 to T4, which was consistent with the results of previous
short-term studies (22,23). In previous research, the association
between Lactobacillus and dental caries was established, and
caries appears to be important for the sustained colonization of
Lactobacillus (24). In
advanced dental caries, 18 different phylotypes of
Lactobacillus were detected, and L. gasseri and L.
ultunensis were of highest loads (13). Despite pathogenic
Lactobacillus, certain probiotic Lactobacillus may
also be extracted from the digestive system, and food containing
probiotic Lactobacillus may increase the resistance to
caries. Although the amount of total Lactobacillus remained
stable throughout the treatment period in the present study,
specific Lactobacillus types should be evaluated when active
caries or possible dentinal caries occur, and the roles and levels
of probiotic and pathogenic Lactobacillus during the
orthodontic treatment should be confirmed in future studies.
Salivary sIgA is considered to be a critical
antibody in the mucosal immune response. However, the association
between sIgA levels and dental caries remain controversial:
Conflicting studies have identified sIgA to be decreased in
pediatric patients with active caries (25), increased in pediatric patients with
active caries (26), or to have no
association with dental caries or S. mutans (27). In adult patients receiving
orthodontic therapy, the association between sIgA and the level of
oral pain was evaluated, and the results indicated no significant
change in the initial arch phase (28). In the present study, no statistically
significant correlation was identified between sIgA and S.
mutans throughout the orthodontic treatment, and sIgA levels
remained stable.
In addition, two key enzymes, LDH and MPO, were
evaluated in the present study. LDH is released during cell death
and is associated with gingival inflammation (6). Salivary LDH activity is also an
indicator of oral mucosa pathologies and the periodontal status
(29). Previous studies have
indicated that LDH levels were higher in the initial 7 days to 10
weeks after tooth movement. Similarly, the activity of MPO enzyme
serves as a biochemical marker of oral inflammation. MPO was
demonstrated to be elevated from 2 h to 7 days after bonding in the
saliva and gingival crevicular fluid, and returned to the baseline
at day 14 (7,8). In addition to the initial changes
described above, the present study aimed to identify changes of LDH
and MPO during long-term orthodontic treatment. The results
indicated a stable level of salivary LDH and MPO from T1 to T4. The
maintained level in the later stages may be attributed to the oral
secretion balance and environmental adaptation over a longer
follow-up period compared with that in the aforementioned studies.
Collectively, the expression of the salivary proteins indicated a
relatively stable microenvironment with respect to the oral
salivary immune response and inflammatory processes during the
18-month orthodontic treatment period.
A limitation of the present study was that the
evaluation period was from 3 to 18 months. A longer period with
more observation time-points may be required to better detect any
fluctuations in S. mutans levels. Furthermore, the sample
size was relatively small, and the data may only marginally reflect
the variation trend of these microenvironmental indexes and not be
representative of the average concentrations in larger cohorts.
Another limitation was that WSLs were not systematically recorded.
A further study assessing the correlation between WSLs and S.
mutans in a larger sample of orthodontic patients is under
consideration.
In conclusion, the present study demonstrated an
increase of the pathogen S. mutans as an alteration in the
oral bacterial flora in patients with long-term fixed orthodontic
treatment, especially when using conventional braces. S.
mutans may become a potential therapeutic target to maintain a
healthy oral environment in further research. Oral hygiene should
be emphasized during the entire treatment period, and self-ligating
braces should be preferred over conventional braces.
Acknowledgements
Not applicable.
Funding
This work was supported by grants from National
Natural Science Foundation of China (grant nos. 81771048 and
81800964).
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author, on reasonable
request.
Authors' contributions
All authors have read and approved the manuscript.
Study design: DJ and ZZ. Study conduction: JD, JH, YS, GT and YY.
Data collection: JD, SY and TG. Data analysis: DJ, YS, GT and JH.
Data interpretation: DJ, SY, TG and JH. Drafting of manuscript: DJ,
LL and ZZ. Revision of manuscript content: LL and ZZ. Approval of
final version of manuscript: DJ, JH, YS, GT, LL and ZZ.
Ethical approval and consent to
participate
All experimental procedures were in accordance with
the Declaration of Helsinki. The study was approved by the Ethics
Committee of West China Hospital of Stomatology (Chengdu, China;
approval no. WCHSIRB-D-2013-070). Prior written informed consent
was obtained from all patients, or by the guardians of the patients
if they were <18 years old. The study was added to the Chinese
Clinical Trial Registry (registration no. ChiCTR-RCH-13003295).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tanner AC, Sonis AL, Lif Holgerson P,
Starr JR, Nunez Y, Kressirer CA, Paster BJ and Johansson I:
White-spot lesions and gingivitis microbiotas in orthodontic
patients. J Dent Res. 91:853–858. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Richter AE, Arruda AO, Peters MC and Sohn
W: Incidence of caries lesions among patients treated with
comprehensive orthodontics. Am J Orthod Dentofacial Orthop.
139:657–664. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Akin M, Tezcan M, Ileri Z and Ayhan F:
Incidence of white spot lesions among patients treated with self-
and conventional ligation systems. Clin Oral Investig.
19:1501–1506. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Topaloglu-Ak A, Ertugrul F, Eden E, Ates M
and Bulut H: Effect of orthodontic appliances on oral microbiota-6
month follow-up. J Clin Pediatr Dent. 35:433–436. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Smith DJ and Taubman MA: Cariogenic
microflora and the immune response. Inter Oral Health Sci. 394–399.
2010.
|
|
6
|
Alfaqeeh SA and Anil S: Lactate
dehydrogenase activity in gingival crevicular fluid as a marker in
orthodontic tooth movement. Open Dent J. 5:105–109. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Marcaccini AM, Amato PA, Leão FV, Gerlach
RF and Ferreira JT: Myeloperoxidase activity is increased in
gingival crevicular fluid and whole saliva after fixed orthodontic
appliance activation. Am J Orthod Dentofacial Orthop. 138:613–616.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Navarro-Palacios A, García-López E,
Meza-Rios A, Armendariz-Borunda J and Sandoval-Rodríguez A:
Myeloperoxidase enzymatic activity is increased in patients with
different levels of dental crowding after initial orthodontic
activation. Am J Orthod Dentofacial Orthop. 146:92–97. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kupietzky A, Majumdar AK, Shey Z, Binder R
and Matheson PB: Colony forming unit levels of salivary
LactobacilliStreptococcus mutans in orthodontic patients. J
Clin Pediatr Dent. 30:51–53. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jurela A, Repic D, Pejda S, Juric H,
Vidakovic R, Matic I and Bosnjak A: The effect of two different
bracket types on the salivary levels of S mutansS sobrinus
in the early phase of orthodontic treatment. Angle Orthod.
83:140–145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Klein MI, Scott-Anne KM, Gregoire S,
Rosalen PL and Koo H: Molecular approaches for viable bacterial
population and transcriptional analyses in a rodent model of dental
caries. Mol Oral Microbiol. 27:350–361. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jung WS, Kim H, Park SY, Cho EJ and Ahn
SJ: Quantitative analysis of changes in salivary mutans
streptococci after orthodontic treatment. Am J Orthod Dentofacial
Orthop. 145:603–609. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Byun R, Nadkarni MA, Chhour KL, Martin FE,
Jacques NA and Hunter N: Quantitative analysis of diverse
Lactobacillus species present in advanced dental caries. J
Clin Microbiol. 42:3128–3136. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
O'Reilly MM and Featherstone JD:
Demineralization and remineralization around orthodontic
appliances: An in vivo study. Am J Orthod Dentofacial Orthop.
92:33–40. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chang HS, Walsh LJ and Freer TJ: The
effect of orthodontic treatment on salivary flow, pH, buffer
capacity, and levels of mutans streptococci and lactobacilli. Aust
Orthod. 15:229–234. 1999.
|
|
16
|
Bowen WH and Koo H: Biology of
Streptococcus mutans-derived glucosyltransferases: Role in
extracellular matrix formation of cariogenic biofilms. Caries Res.
45:69–86. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Taha M, El-Fallal A and Degla H: In vitro
and in vivo biofilm adhesion to esthetic coated arch wires and its
correlation with surface roughness. Angle Orthod. 86:285–291. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
do Nascimento LE, Pithon MM, dos Santos
RL, Freitas AO, Alviano DS, Nojima LI, Nojima MC and Ruellas AC:
Colonization of Streptococcus mutans on esthetic brackets:
Self-ligating vs conventional. Am J Orthod Dentofacial Orthop. 143
Suppl 4:S72–S77. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Uzuner FD, Kaygisiz E and Cankaya ZT:
Effect of the bracket types on microbial colonization and
periodontal status. Angle Orthod. 84:1062–1067. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pellegrini P, Sauerwein R, Finlayson T,
McLeod J, Covell DA Jr, Maier T and Machida CA: Plaque retention by
self-ligating vs elastomeric orthodontic brackets: Quantitative
comparison of oral bacteria and detection with adenosine
triphosphate-driven bioluminescence. Am J Orthod Dentofacial
Orthop. 135:426–427.e1-e9. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Caufield PW, Schön CN, Saraithong P, Li Y
and Argimón S: Oral Lactobacilli and Dental Caries. J Dent Res. 94
Suppl 9:S110–S118. 2015. View Article : Google Scholar
|
|
22
|
Peros K, Mestrovic S, Anic-Milosevic S and
Slaj M: Salivary microbial and nonmicrobial parameters in children
with fixed orthodontic appliances. Angle Orthod. 81:901–906. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lara-Carrillo E, Montiel-Bastida NM,
Sánchez-Pérez L and Alanís-Tavira J: Effect of orthodontic
treatment on saliva, plaque and the levels of Streptococcus
mutansLactobacillus. Med Oral Patol Oral Cir Bucal.
15:e924–e929. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xu X, He J, Xue J, Wang Y, Li K, Zhang K,
Guo Q, Liu X, Zhou Y, Cheng L, et al: Oral cavity contains distinct
niches with dynamic microbial communities. Environ Microbiol.
17:699–710. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chawda JG, Chaduvula N, Patel HR, Jain SS
and Lala AK: Salivary SIgA and dental caries activity. Indian
Pediatr. 48:719–721. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shifa S, Muthu MS, Amarlal D and Rathna
Prabhu V: Quantitative assessment of IgA levels in the unstimulated
whole saliva of caries-free and caries-active children. J Indian
Soc Pedod Prev Dent. 26:158–161. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Koga-Ito CY, Martins CA, Balducci I and
Jorge AO: Correlation among mutans streptococci counts, dental
caries, and IgA to Streptococcus mutans in saliva. Braz Oral
Res. 18:350–355. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
da Silva Campos MJ, Souza Alves CC,
Barbosa Raposo NR, Ferreira AP and Farinazzo Vitral RW: Influence
of salivary secretory immunoglobulin A level on the pain
experienced by orthodontic patients. Med Sci Monit. 16:CR405–CR409.
2010.PubMed/NCBI
|
|
29
|
De La Peña VA, Diz Dios P and Tojo Sierra
R: Relationship between lactate dehydrogenase activity in saliva
and oral health status. Arch Oral Biol. 52:911–915. 2007.
View Article : Google Scholar : PubMed/NCBI
|