Introduction
Cancer-induced bone pain (CIBP) is a common symptom
in advanced cancer patients (1).
Numerous types of cancer (e.g., breast cancer, prostate cancer)
have a high preference to metastasize to bone, which disrupts the
process of bone remodeling and leads to significant pain (2). Currently, there are several animal
models of CIBP, which promote understanding of the mechanisms of
CIBP (3–5). One of the animal models that used most
commonly is intratibial injection of Walker 256 cells induced CIBP
(6–8). Although marked advances have been made
in recent years, the mechanism underlying CIBP remains largely
unclear. Therefore, it is important to find novel therapeutic
strategies for the management of CIBP.
Ginsenosides are the principle active constituents
in ginseng, which has been used for thousands of years in
traditional medicine (9). There are
a number of ingredients isolated from ginseng including Rb1, Rg3,
Rg1, and Rh1 (10). These
ingredients have unique functions based on differences in the
chemical structures (11). As a
major ingredient of ginseng, Ginsenoside Rb1 (GRb1) exhibits a wide
range of functions including anti-inflammatory, antioxidant, and
neuroprotective effects (12,13). It
was reported that GRb1 attenuated damage to cerebral cortex neurons
by downregulating nitric oxide, superoxide, and tumor necrosis
factor (TNF)-α expression in hypoxia-activated microglia (14). A recent study provided evidence that
GRb1 attenuated inflammatory pain induced by intraplantar injection
of formalin by inhibiting neuronal phosphorylation of extracellular
signal-regulated kinase (ERK) via regulating the nuclear factor
erythroid 2-related factor 2 (Nrf2) and nuclear factor (NF)-κB
pathways (15). Furthermore, other
ingredients of Ginsenoside have also been reported to have
antinociceptive effects (16–19).
However, whether GRb1 can alleviate CIBP remains unknown.
Therefore, the present study investigated the analgesic effect of
GRb1 on a well-established rat model of CIBP established by
intratibial injection of Walker 256 cells.
Several lines of evidence suggest that
neuroinflammation in the central nervous system serves a vital role
in the development and maintenance of CIBP (20,21).
Neuroinflammation under CIBP condition is characterized by
activation of glial cells (e.g., microglia and astrocyte) in the
spinal cord and brain, which subsequently release proinflammatory
cytokines (e.g., interleukin (IL)-1β, IL-6 and TNF-α). It is
well-established that iba1, which is the maker of microglia, is
significantly unregulated during CIBP (22,23).
Additionally, inhibition of microglia activation or proinflammatory
cytokines release by glial cells significantly attenuated CIBP
(24). It was repeatedly reported
that GRb1 demonstrated an anti-neuroinflammation effect in animal
models including Alzheimer's disease and post-operative cognitive
dysfunction (25,26). Therefore, the present study
investigated whether GRb1 could suppress the activation of
microglia and the production of proinflammatory cytokines in
CIBP.
Materials and methods
Animals
The present study used adult female Sprague-Dawley
rats (180–200 g; Xi'an Jiaotong University, Xi'an, China). Rats
were housed in a controlled lighting environment (12-h light/dark
cycle) with ad libitum access to food and water. All the
experimental protocols were approved by the Animal Care and Use
Committee of Baoji Central Hospital.
Establishment of CIBP rat model
The CIBP rat model was established as previously
described (27). Briefly, the rats
were anesthetized by pentobarbital sodium [50 mg/kg,
intraperitoneal (i.p.)]. The right leg of the rats was shaved, and
the skin was disinfected with 75% (v/v) ethanol. Then, 10 µl volume
of Walker 256 mammary gland carcinoma cells (4×105
cells) was injected into the right tibia of the rats. Sham rats
were injected with of 10 µl volume of PBS into the right tibia. The
injection site was sealed with medical glue to prevent leakage.
Finally, the wound was disinfected with 75% (v/v) ethanol and
sutured with 3-0 silk thread.
Behavioral tests
Mechanical allodynia was measured as previously
described (28). Briefly, single
rats were placed in a customized chamber and allowed to acclimate
for 30 min prior to testing. Then, von Frey filaments (Stoelting
Co., Wood Dale, IL, USA) were applied to the mid-plantar surface of
hind paw in ascending order (0.4, 0.6, 1.4, 2, 4, 6, 8, 10 and 15
g). Each Von Frey hair was held for 6 to 8 sec with a 5 min
interval between applications. Brisk withdrawal or paw flinching
upon stimulus was considered as positive response. The lowest force
of the filament required to elicit a positive response was
considered to be the paw withdrawal threshold (PWT). Thermal
hyperalgesia was measured as previously described (29). Briefly, single rats were placed in a
customized chamber and allowed to acclimate for 30 min prior to
testing. Then, the radiant heat source was delivered by a Plantar
Analgesia meter (ITC Life Science Inc., Victory Blvd Woodland
Hills, CA, USA) and focused onto the mid-plantar surface of hind
paw. The heat source was turned off when the rat lifted the foot.
The time from onset of radiant heat application to withdrawal of
the rat's hind paw was defined as the paw withdrawal latency (PWL).
A 25 sec cutoff was used to prevent tissue damage. The right hind
paw was tested three times at an interval of 5 min. The behavioral
tests were performed by an investigator blinded to the tested
groups.
Drug administration
GRb1 was purchased from Sigma-Aldrich; Merck KGaA
(Darmstadt, Germany) and dissolved in normal saline. The
appropriate dosage of GRb1 was determined by preliminary
experiments and previous studies (30,31). To
determine the analgesic effect of GRb1 on established CIBP, GRb1
(1, 5, and 10 mg/kg, i.p.) was treated at day 14 following surgery.
Pain behaviors were measured at 15, 30, 45, 60, 75, 90 min
following intraperitoneal injection of GRb1. To determine the
analgesic effect of multiple administration of GRb1 on established
CIBP, GRb1 (10 mg/kg, i.p.) was treated from day 12 for three
consecutive days. To determine the effect of GRb1 on the activation
of microglia and expression of proinflammatory cytokines, GRb1 (10
mg/kg, i.p.) was treated from day 12 for three consecutive days.
The rats were sacrificed 30 min following the last injection of
GRb1.
Western blot analysis
Briefly, the rats were deeply anesthetized by
pentobarbital sodium (120 mg/kg, i.p.). Then, the L4-L6 spinal cord
was removed and stored at −80°C until use. The tissue samples were
homogenized in lysis buffer containing PMSF and 0.02% protease
inhibitor cocktail. The homogenates were centrifuged at 12,000 × g
for 10 min at 4° to obtain the supernatants. Protein concentrations
were determined by the Bradford method. Equivalent amounts of
protein (50 µg) were separated by 10% SDS-PAGE and transferred onto
polyvinylidene difluoride membranes. Then, the membranes were
blocked with 5% non-fat milk for 2 h at room temperature (RT) and
incubated overnight at 4°C with primary antibodies for iba1
(1:1,000; Abcam, Cambridge, UK), IL-1β (1:1,000; Abcam), IL-6
(1:500; Sigma-Aldrich; Merck KGaA), TNF-α (1:2,000; EMD Millipore,
Billerica, MA, USA) and GAPDH (1:5,000; Cell Signaling Technology,
Inc., Danvers, MA, USA). The membranes were washed in tris buffered
saline with tween 20 and then incubated with appropriate
horseradish peroxidase-conjugated secondary antibody (1:5,000;
Sigma-Aldrich; Merck KGaA). Bands were revealed using an ECL kit
(EMD Millipore). The intensity of proteins was measured by image
lab software and normalized to GAPDH. The protein intensity of
control groups was set as 1.
Immunohistochemistry
Briefly, the rats were deeply anesthetized by
pentobarbital sodium (120 mg/kg, i.p.) and perfused with 0.1 M PBS
followed by 4% paraformaldehyde (PFA). The L4-L6 spinal cord
segments were removed and post-fixed in 4% PFA for 4 h at 4°C, then
placed in a 30% sucrose solution at 4°C for three days. The
embedded samples were sectioned 30-µm thick in a cryostat and
stored in PBS until use. The sections were blocked with 5% donkey
serum and 0.3% Triton X-100 for 2 h at RT, then incubated overnight
at 4°C with the primary antibody against iba1 (1:200; Abcam). After
washed in PBS for three times, the sections were incubated with
Alexa Fluor 594-labeled donkey anti-goat secondary antibody (1:400,
Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA).
Following immunostaining procedures, the sections were examined
using a fluorescence microscope (Leica Microsystems GmbH, Wetzlar,
Germany) at the same exposure time.
Statistical analysis
Statistical analysis was performed using GraphPad
Prism 5 (GraphPad Software, Inc., La Jolla, CA, USA). All data were
presented as means ± standard error of the mean. Western blotting
data was analyzed using one-way analysis of variance (ANOVA) with
repeated measures followed by the Bonferroni post hoc test.
Behavioral tests data was analyzed using two-way ANOVA with
repeated measures followed by Bonferroni post hoc test. P<0.05
was considered to indicate a statistically significant
difference.
Results
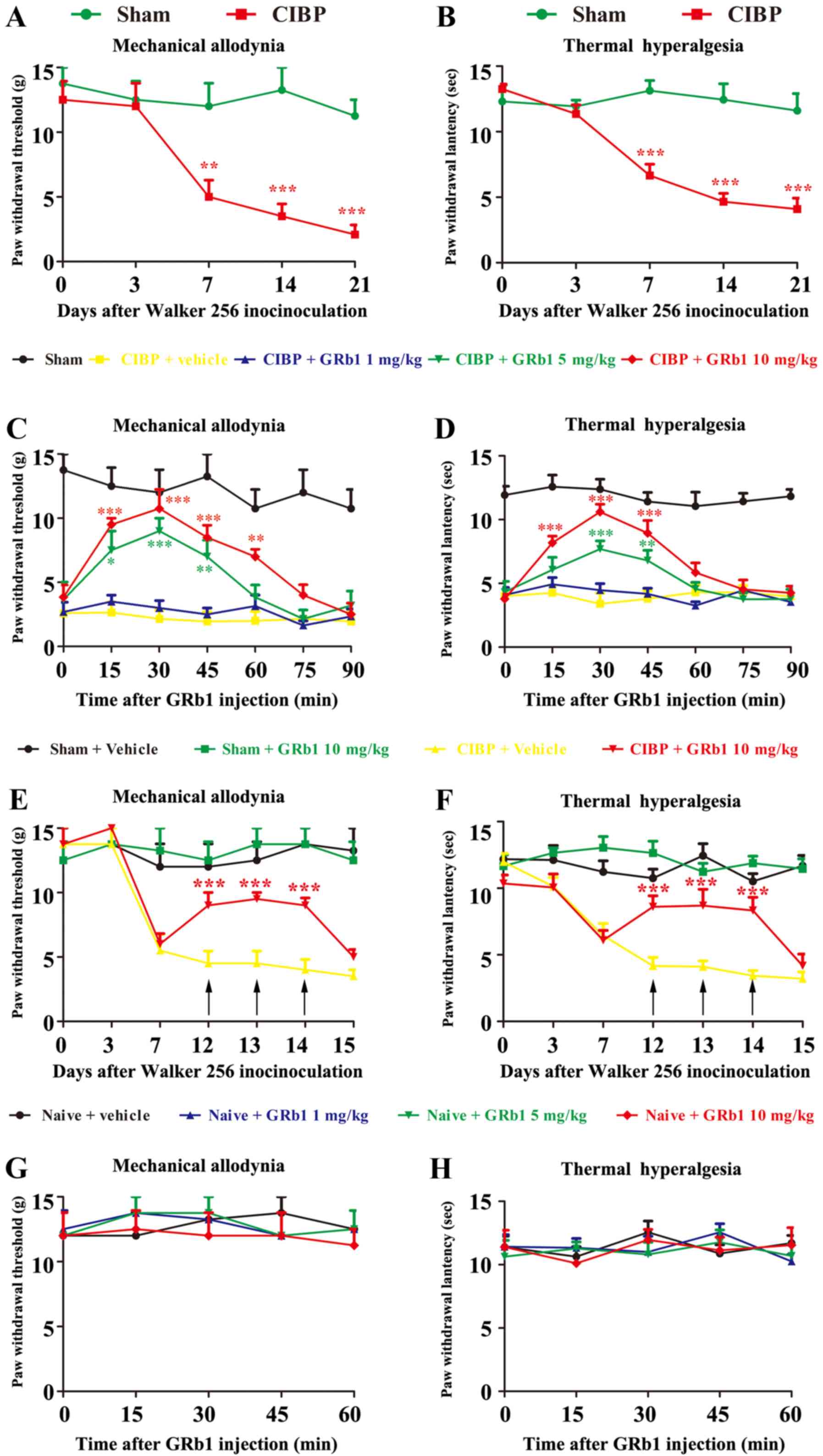
Time course of mechanical allodynia
and thermal hyperalgesia induced by intratibial inoculation of
Walker 256 cells
The PWT and PWL were at a similar baseline in all
rats. Compared with the sham rats, the CIBP rats began to exhibit a
decrease in PWT and PWL in the ipsilateral hind paw at 7 days
following surgery, which indicates the development of mechanical
allodynia and thermal hyperalgesia, respectively. Furthermore, the
PWT and PWL progressively decreased from day 7 to day 21 (Fig. 1A and B). These results indicated that
the model of CIBP was established successfully.
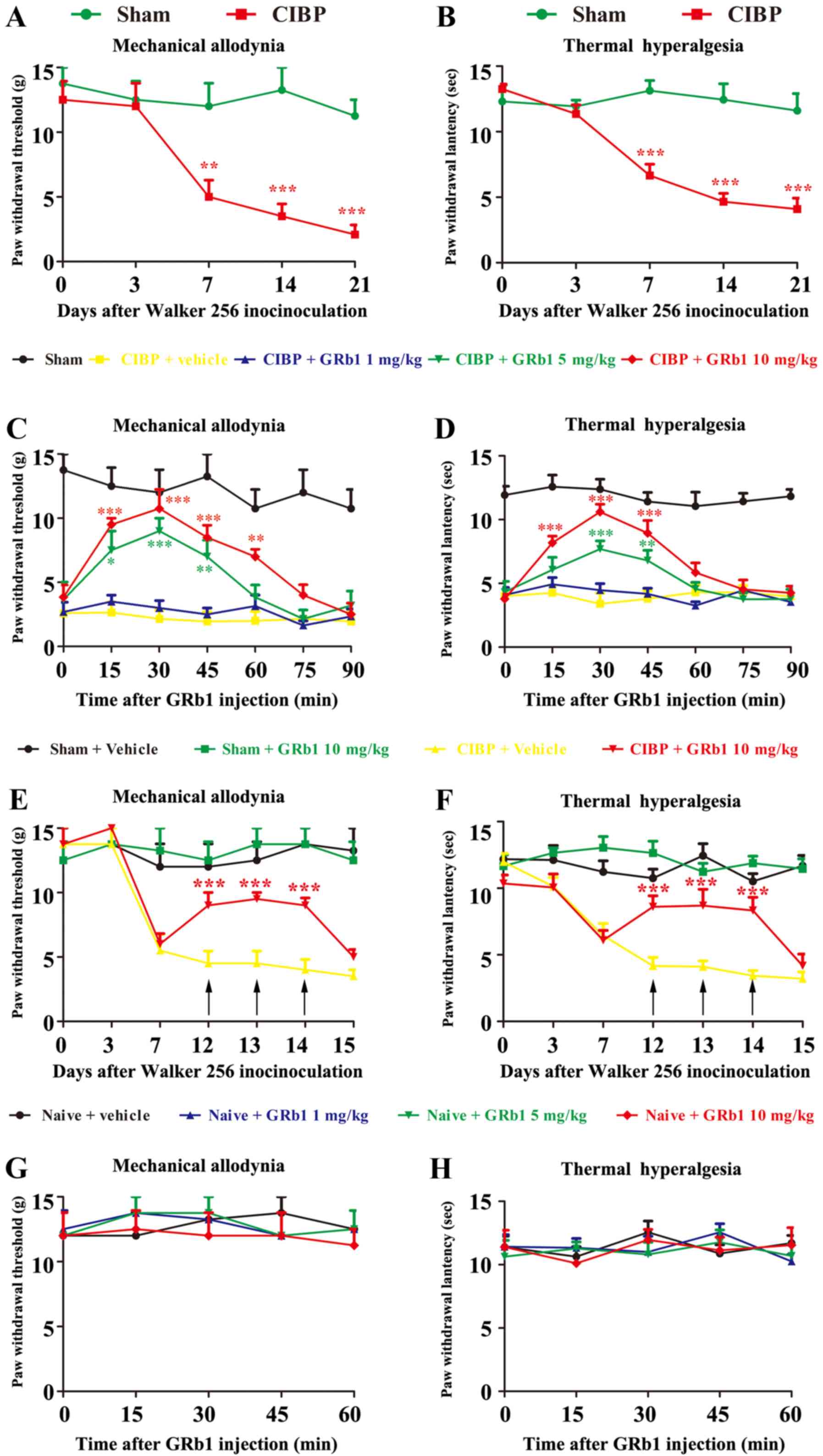 | Figure 1.GRb1 attenuated established CIBP. A
significant decrease of (A) PWT and (B) PWL was observed in CIBP
rats compared with sham rats from day 7 to 21. **P<0.01,
***P<0.001 vs. the sham group. Data were presented as the mean ±
SEM. n=6 rats in each group. At 14 days following surgery when the
pain behavior is established, i.p. injection of GRb1 (5 and 10
mg/kg, but not 1 mg/kg) partially and transiently reversed the
mechanical allodynia (C) and thermal hyperalgesia (D) in CIBP rats.
*P<0.05, **P<0.01 and ***P<0.001 vs. the CIBP rats treated
with the vehicle. Pain behaviors were measured at 15, 30, 45, 60,
75 and 90 min following i.p. injection of GRb1. Data were presented
as the mean ± standard error of the mean. n=6 rats in each group.
I.p. injection of GRb1 (1, 5 and 10 mg/kg) has no significant
effects on PWT (E) and PWL (F) in naïve rats. Data were presented
as the mean ± SEM. n=6 rats in each group. Repeated administration
of GRb1 persistently elevated PWT (G) and PWL (H) in CIBP rats.
***P<0.001 vs. the CIBP rats treated with vehicle. GRb1 (10
mg/kg, i.p.) was treated from day 12 for three consecutive days.
Pain behaviors were measured at 30 min following i.p. injection of
GRb1. Data were presented as the mean ± SEM. n=6 rats in each
group. PWT, paw withdrawal threshold; CIBP, cancer-induced bone
pain; i.p., intraperitoneal; SEM, standard error of the mean; PWL,
paw withdrawal lantency; GRb1, Ginsenoside Rb1. |
Analgesic effects of GRb1 on
established CIBP
To determine the analgesic effect of GRb1 on
established CIBP, GRb1 (1, 5, and 10 mg/kg; i.p.) was administered
at day 14 following surgery. Pain behaviors were measured at 15,
30, 45, 60, 75 and 90 min following intraperitoneal injection of
GRb1. At 14 days following surgery when the pain behavior is
established, intraperitoneal injection of GRb1 (5 and 10 mg/kg, but
not 1 mg/kg) partially and transiently reversed the mechanical
allodynia and thermal hyperalgesia in CIBP rats (Fig. 1C and D). The analgesic effect of GRb1
started at 15 min following injection and lasted for ~1 h. However,
CIBP rats treated with a vehicle exhibited no significant
alterations regarding PWT and PWL.
To determine the analgesic effect of multiple
administrations of GRb1 on established CIBP, GRb1 (10 mg/kg, i.p.)
was given from day 12 for three consecutive days. Pain behaviors
were measured at 30 min following i.p. injection of GRb1. It was
demonstrated that repeated administration of GRb1 exhibited
persistent analgesic effects as indicated by a significant
upregulation of PWT and PWL (Fig. 1E and
F).
Effects of GRb1 on pain threshold of
naive rats
To determine whether treatment with GRb1 could
affect the pain threshold of naive rats, naive rats were injected
intraperitonally with GRb1 (1, 5, and 10 mg/kg). The behavioral
tests demonstrated that none of the doses chosen effected the PWT
and PWL in naive rats (Fig. 1G and
H), suggesting that GRb1 did not affect the pain behavior in
naive rats.
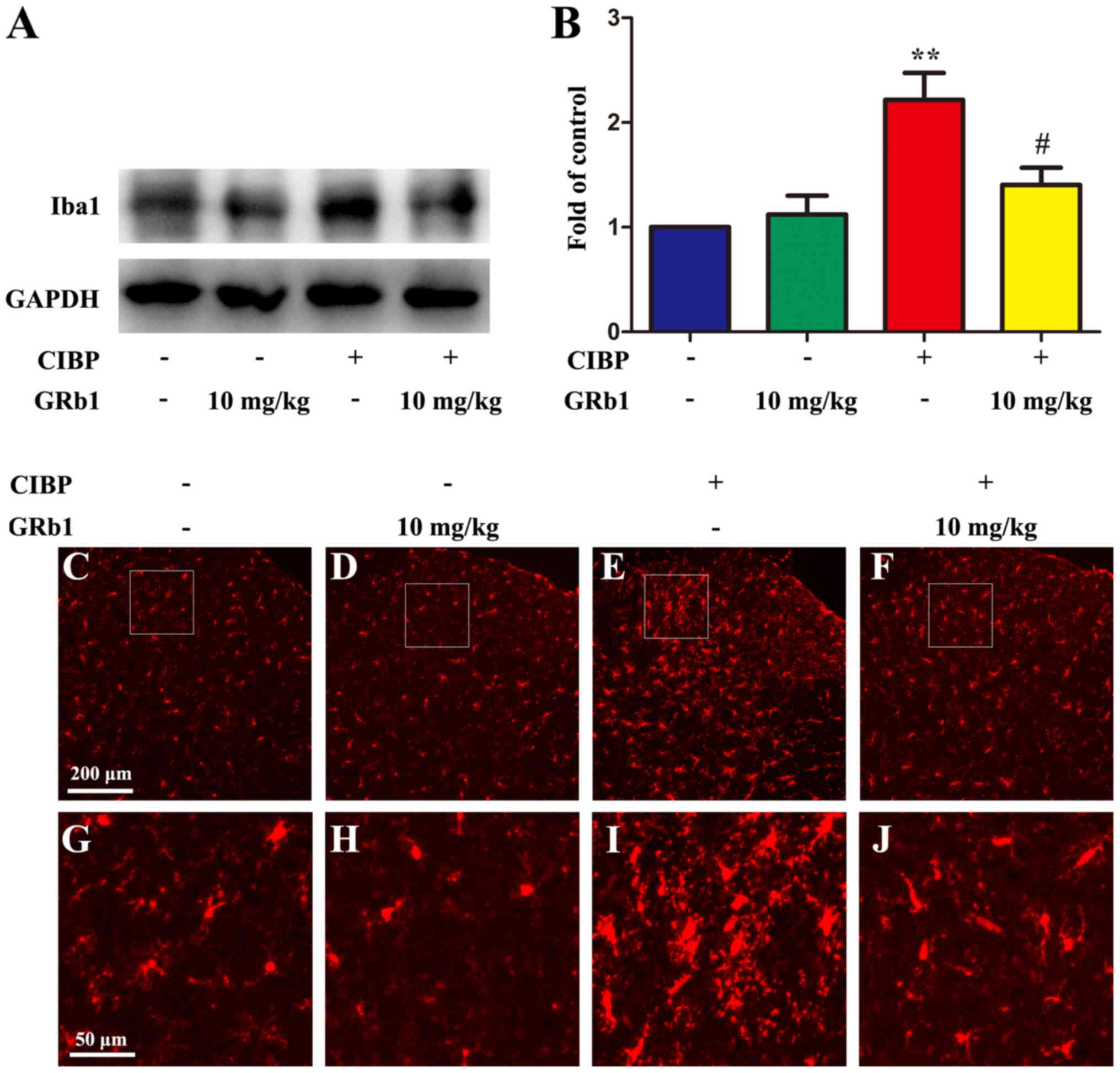
Effects of GRb1 on the activation of
microglia in the spinal cord
It was reported that the activation of microglia in
the spinal cord serves an important role in the development of CIBP
and microglia inhibitor could alleviate CIBP (32). Therefore, whether treatment with GRb1
could affect the activation of microglia was investigated. GRb1 was
intraperitoneally injected (10 mg/kg) from day 12 for three
consecutive days. The rats were sacrificed 30 min following the
last injection of GRb1. The protein expression of iba1, which is
the maker of microglia, was significantly suppressed by the
treatment with GRb1 in the spinal cord of CIBP rats (Fig. 2A and B). Furthermore, the
immunohistochemistry results also confirmed that the
immunoreactivity of iba1 was significantly decreased in the spinal
cord of CIBP rats intraperitoneally injected with GRb1 (10 mg/kg)
from day 12 for three consecutive days (Fig. 2C-J). Additionally, i.p. injection of
GRb1 did not alter the protein expression and immunoreactivity of
iba1 in the spinal cord of sham rats.
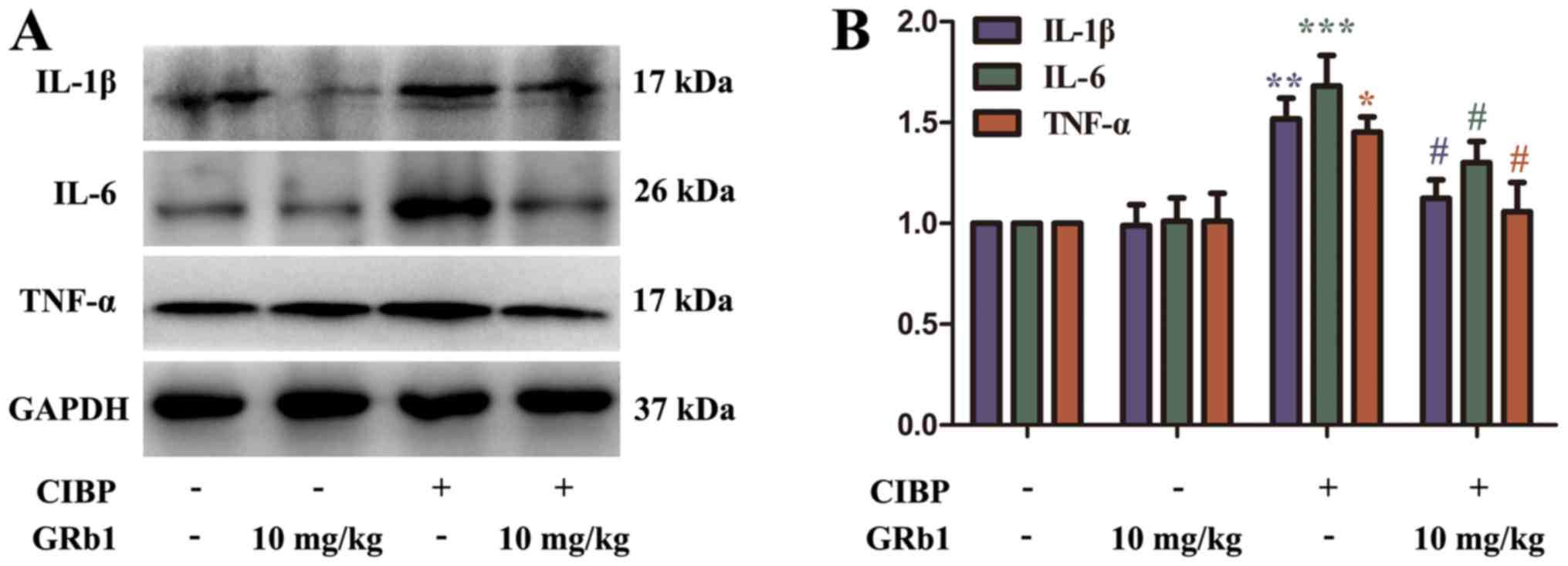
Effects of GRb1 on the expression of
proinflammatory cytokines in the spinal cord
It is well established that upregulation of
proinflammatory cytokines contributes to the development of CIBP
(33). Consistent with previous
studies, the results of the present study demonstrate that CIBP
rats exhibited upregulated protein expression levels of IL-1β,
IL-6, and TNF-α. GRb1 was intraperitoneally injected (10 mg/kg)
from day 12 for three consecutive days. The rats were sacrificed 30
min following the last injection of GRb1. The protein expression of
IL-1β, IL-6 and TNF-α was significantly suppressed by the treatment
with GRb1 in CIBP rats compared with CIBP rats treated with a
vehicle (Fig. 3).
Discussion
The present study provided evidence that intratibial
injection of Walker 256 cells could induce mechanical allodynia and
thermal hyperalgesia from day 7–21. Furthermore, i.p. injection of
GRb1 (5 and 10 mg/kg, but not 1 mg/kg), which belongs to the family
of triterpene glycosides, partially and transiently reversed the
mechanical allodynia and thermal hyperalgesia in CIBP rats.
Additionally, intraperitoneal injection of GRb1 did not affect the
pain threshold in naive rats. Notably, i.p. injection of GRb1 (10
mg/kg) suppressed the activation of microglia and glial-derived
proinflammatory cytokines including IL-1β, IL-6 and TNF-α.
Together, these results suggested that GRb1 may alleviate CIBP via
suppression neuroinflammation in the spinal cord.
Breast cancer has a high prevalence of metastasizing
to the bone, which causes osteolytic lesions, hypercalcaemia, bone
fractures, and significant pain (34,35).
Currently, the available therapeutic strategies for CIBP includes
localized radiation therapy, non-steroidal anti-inflammatory drugs,
and opioids. However, at least half of these patients did not
obtain adequate pain relief (36).
More importantly, increasing doses of analgesic drugs due to
analgesics tolerance leads to unsatisfied side effects including
nausea and vomiting as well as addiction (37). Therefore, it is important to discover
novel therapeutic strategy for the management of CIBP.
GRb1 is one of main active constituents isolated
from a traditionally used herb named ginseng (38). Previous studies have demonstrated
that GRb1 has multiple functions. For example, GRb1 serves a
protective role in animal models of cerebral and intestinal as well
as spinal cord ischemia/reperfusion injury (31,39–41). In
addition, in vitro and in vivo studies have
demonstrated that GRb1 has anti-inflammatory and anti-apoptosis
effect (42–46). Additionally, treatment with GRb1
attenuates oxidative stress, suggesting an antioxidant effect of
GRb1 (47–49). A recent study provided evidence that
GRb1 attenuates inflammatory pain induced by intraplantar injection
of formalin by inhibiting neuronal phosphorylation of ERK via
regulating the Nrf2 and NF-κB pathways (15). Other ingredients of Ginsenoside have
also been reported to have antinociceptive effects (16–19). The
present study investigated the analgesic effect of GRb1 on a
well-established rat model of CIBP established by intratibial
injection of Walker 256 cells. Consistent with previous study, the
present study's behavioral results demonstrated that CIBP rats
exhibited a significant decrease in PWT and PWL in the ipsilateral
hind paw from day 7 to day 21. Furthermore, it was demonstrated
that i.p. injection of GRb1 (5 and 10 mg/kg, but not 1 mg/kg)
partially and transiently reversed the mechanical allodynia and
thermal hyperalgesia in CIBP rats at 14 days following surgery when
the pain behavior was established. In addition, repeated
administration of GRb1 showed persistent analgesic effect. However,
treatment with GRb1 did not affect the pain threshold of naive
rats. These results suggested that GRb1 may be an effective drug
for the management of CIBP.
To determine the underlying mechanisms of the
analgesic effect of GRb1 against CIBP the effect of GRb1 on
neuroinflammation in the spinal cord was investigated. Emerging
evidence has indicated that glial-derived neuroinflammation serves
a fundamental role in the initiation and maintenance of CIBP
(8,50–52).
Pharmacological inhibition of the activation of microglia and
glial-derived proinflammatory cytokines inhibited the pain
behaviors in CIBP rats (53–56). In a rat model of Alzheimer's disease,
Wang et al (26) demonstrated
that GRb1 treatment improved learning and memory deficit via its
anti-neuroinflammatory effect. In another study, Miao et al
(25) demonstrated that i.p.
injection of GRb1 mitigated isoflurane/surgery-induced cognitive
impairment by downregulating the expression level of reactive
oxygen species, TNF-α and IL-6 in the mice hippocampus. The results
of the present study consistently demonstrated that the proteins
expression and immunoreactivity of iba1, was upregulated in CIBP
rats compared with the sham rats. Furthermore, i.p. injection of
GRb1 (10 mg/kg) from day 12 for three consecutive days
significantly suppressed the activation of microglia. Finally, the
protein express levels of IL-1β, IL-6, and TNF-α in the spinal cord
of CIBP rats was measured. The western blotting results of the
present study demonstrated upregulated expression level of IL-1β,
IL-6 and TNF-α in the spinal cord, which were significantly
inhibited by the treatment of GRb1 (i.p., 10 mg/kg) from day 12 for
three consecutive days. Together, these results indicated that GRb1
may attenuate CIBP via inhibiting the activation of microglia and
glial-derived proinflammatory cytokines.
In conclusion, this study provided evidence that
i.p. injection of GRb1 alleviated mechanical allodynia and thermal
hyperalgesia in a rat model of CIBP. Mounting evidence showed that
microglia inhibitors attenuated CIBP by suppressing the activation
of microglia (6,57). Considering that GRb1 showed
anti-neuroinflammation effect in animal models such as Alzheimer
disease (26) and post-operative
cognitive dysfunction (25), we
explored whether GRb1 could suppressed the activation of microglia
under CIBP condition. GRb1 was intraperitoneal injected (10 mg/kg)
from day 12 after surgery for three consecutive days. The rats were
sacrificed 30 min after the last injection of GRb1. Our results
showed that repeated administration of GRb1 inhibited the
activation of microglia. Consistently, repeated administration of
GRb1 showed persistent analgesic effect. It is well-established
that activated microglia in the spinal cord increase in number,
change their morphology, and release proinflammarory cytokines such
as IL-1β, IL-6 and TNF-α. Previous studies have demonstrated that
microglia inhibitors could suppressed the expression of these
proinflammarory cytokines under CIBP condition (33,58).
Since we found repeated treatment with GRb1 suppressed the
activation of microglia, we subsequently explored whether GRb1
could inhibited the expression of proinflammarory cytokines. It
turns out that GRb1 did downregulated the expression of
proinflammarory cytokines in CIBP rats. Therefore, we conclude that
inhibiting the activation of microglia and glial-derived
proinflammatory cytokines may be involved in the analgesic effect
of GRb1 under CIBP condition. However, it must be acknowledged that
there may be other mechanisms regarding the antinociceptive effect
of GRb1 on CIBP. Further studies are warranted to investigate more
detailed mechanisms underlying the analgesic effect of GRb1.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets generated and/or analyzed during the
present study are available from the corresponding author on
reasonable request.
Authors' contributions
FDY and JQY designed the experiments, conducted the
experiments, analyzed the data, created the figures and wrote the
manuscript. YCH conducted the experiments and analyzed the data.
MPL, WJY and BZ performed the analysis with constructive
discussions. XJL designed the experiments and contributed
significantly to the revision of manuscript.
Ethics approval and consent to
participate
All the experimental protocols were approved by the
Animal Care and Use Committee of Baoji Central Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Schwei MJ, Honore P, Rogers SD,
Salak-Johnson JL, Finke MP, Ramnaraine ML, Clohisy DR and Mantyh
PW: Neurochemical and cellular reorganization of the spinal cord in
a murine model of bone cancer pain. J Neurosci. 19:10886–10897.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Honoré P, Schwei J, Rogers SD,
Salak-Johnson JL, Finke MP, Ramnaraine ML, Clohisy DR and Mantyh
PW: Cellular and neurochemical remodeling of the spinal cord in
bone cancer pain. Prog Brain Res. 129:389–397. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Muralidharan A, Wyse BD and Smith MT:
Optimization and characterization of a rat model of prostate
cancer-induced bone pain using behavioral, pharmacological,
radiological, histological and immunohistochemical methods.
Pharmacol Biochem Behav. 106:33–46. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Menéndez L, Lastra A, Fresno MF, Llames S,
Meana A, Hidalgo A and Baamonde A: Initial thermal heat hypoalgesia
and delayed hyperalgesia in a murine model of bone cancer pain.
Brain Res. 969:102–109. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Medhurst SJ, Walker K, Bowes M, Kidd BL,
Glatt M, Muller M, Hattenberger M, Vaxelaire J, O'Reilly T,
Wotherspoon G, et al: A rat model of bone cancer pain. Pain.
96:129–140. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yang Y, Li H, Li TT, Luo H, Gu XY, Lü N,
Ji RR and Zhang YQ: Delayed activation of spinal microglia
contributes to the maintenance of bone cancer pain in female Wistar
rats via P2X7 receptor and IL-18. J Neurosci. 35:7950–7963. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu Y, Liang Y, Hou B, Liu M, Yang X, Liu
C, Zhang J, Zhang W, Ma Z and Gu X: The inhibitor of
calcium/calmodulin-dependent protein kinase II KN93 attenuates bone
cancer pain via inhibition of KIF17/NR2B trafficking in mice.
Pharmacol Biochem Behav. 124:19–26. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mao-Ying QL, Wang XW, Yang CJ, Li X, Mi
WL, Wu GC and Wang YQ: Robust spinal neuroinflammation mediates
mechanical allodynia in Walker 256 induced bone cancer rats. Mol
Brain. 5:162012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gum SI, Rahman MK, Won JS and Cho MK: A
distinctive pattern of beauveria bassiana-biotransformed
ginsenoside products triggers mitochondria/FasL-mediated apoptosis
in colon cancer cells. Phytother Res. 30:136–143. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lu C, Shi Z, Dong L, Lv J, Xu P, Li Y, Qu
L and Liu X: Exploring the effect of ginsenoside Rh1 in a sleep
deprivation-induced mouse memory impairment model. Phytother Res.
31:763–770. 2017. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kezhu W, Pan X, Cong L, Liming D, Beiyue
Z, Jingwei L, Yanyan Y and Xinmin L: Effects of ginsenoside Rg1 on
learning and memory in a reward-directed instrumental conditioning
task in chronic restraint stressed rats. Phytother Res. 31:81–89.
2017. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Siddiqi MH, Siddiqi MZ, Kang S, Noh HY,
Ahn S, Simu SY, Aziz MA, Sathishkumar N, Jiménez Pérez ZE and Yang
DC: Inhibition of osteoclast differentiation by ginsenoside Rg3 in
RAW264.7 cells via RANKL, JNK and p38 MAPK pathways through a
modulation of cathepsin K: An in silico and in vitro study.
Phytother Res. 29:1286–1294. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen W, Guo Y, Yang W, Zheng P, Zeng J and
Tong W: Protective effect of ginsenoside Rb1 on integrity of
blood-brain barrier following cerebral ischemia. Exp Brain Res.
233:2823–2831. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ke L, Guo W, Xu J, Zhang G, Wang W and
Huang W: Ginsenoside Rb1 attenuates activated microglia-induced
neuronal damage. Neural Regen Res. 9:252–259. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jang M, Lee MJ, Choi JH, Kim EJ, Nah SY,
Kim HJ, Lee S, Lee SW, Kim YO and Cho IH: Ginsenoside Rb1
attenuates acute inflammatory nociception by inhibition of neuronal
ERK phosphorylation by regulation of the Nrf2 and NF-κB pathways. J
Pain. 17:282–297. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim IJ, Park CH, Lee SH and Yoon MH: The
role of spinal adrenergic receptors on the antinociception of
ginsenosides in a rat postoperative pain model. Korean J
Anesthesiol. 65:55–60. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ahn EJ, Choi GJ, Kang H, Baek CW, Jung YH,
Woo YC and Bang SR: Antinociceptive effects of ginsenoside Rg3 in a
rat model of incisional pain. Eur Surg Res. 57:211–223. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yoon MH, Huang LJ, Choi JI, Lee HG, Kim WM
and Kim CM: Antinociceptive effect of intrathecal ginsenosides
through alpha-2 adrenoceptors in the formalin test of rats. Br J
Anaesth. 106:371–379. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yoon MH, Kim WM, Lee HG, Choi JI, Kim YO
and Song JA: Analgesic effect of intrathecal ginsenosides in a
murine bone cancer pain. Korean J Pain. 23:230–235. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hu S, Mao-Ying QL, Wang J, Wang ZF, Mi WL,
Wang XW, Jiang JW, Huang YL, Wu GC and Wang YQ: Lipoxins and
aspirin-triggered lipoxin alleviate bone cancer pain in association
with suppressing expression of spinal proinflammatory cytokines. J
Neuroinflammation. 9:2782012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Song H, Han Y, Pan C, Deng X, Dai W, Hu L,
Jiang C, Yang Y, Cheng Z, Li F, et al: Activation of adenosine
monophosphate-activated protein kinase suppresses neuroinflammation
and ameliorates bone cancer pain: Involvement of inhibition on
mitogen-activated protein kinase. Anesthesiology. 123:1170–1185.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hu XF, He XT, Zhou KX, Zhang C, Zhao WJ,
Zhang T, Li JL, Deng JP and Dong YL: The analgesic effects of
triptolide in the bone cancer pain rats via inhibiting the
upregulation of HDACs in spinal glial cells. J Neuroinflammation.
14:2132017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pevida M, González-Rodríguez S, Lastra A,
García-Suárez O, Hidalgo A, Menéndez L and Baamonde A: Involvement
of spinal chemokine CCL2 in the hyperalgesia evoked by bone cancer
in mice: A role for astroglia and microglia. Cell Mol Neurobiol.
34:143–156. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bu H, Shu B, Gao F, Liu C, Guan X, Ke C,
Cao F, Hinton AO Jr, Xiang H, Yang H, et al: Spinal IFN-γ-induced
protein-10 (CXCL10) mediates metastatic breast cancer-induced bone
pain by activation of microglia in rat models. Breast Cancer Res
Treat. 143:255–263. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Miao HH, Zhang Y, Ding GN, Hong FX, Dong P
and Tian M: Ginsenoside Rb1 attenuates isoflurane/surgery-induced
cognitive dysfunction via inhibiting neuroinflammation and
oxidative stress. Biomed Environ Sci. 30:363–372. 2017.PubMed/NCBI
|
|
26
|
Wang Y, Liu J, Zhang Z, Bi P, Qi Z and
Zhang C: Anti-neuroinflammation effect of ginsenoside Rbl in a rat
model of Alzheimer disease. Neurosci Lett. 487:70–72. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hang LH, Yang JP, Shao DH, Chen Z and Wang
H: Involvement of spinal PKA/CREB signaling pathway in the
development of bone cancer pain. Pharmacol Rep. 65:710–716. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yin Q, Cheng W, Cheng MY, Fan SZ and Shen
W: Intrathecal injection of anti-CX3CR1 neutralizing antibody
delayed and attenuated pain facilitation in rat tibial bone cancer
pain model. Behav Pharmacol. 21:595–601. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shen W, Hu XM, Liu YN, Han Y, Chen LP,
Wang CC and Song C: CXCL12 in astrocytes contributes to bone cancer
pain through CXCR4-mediated neuronal sensitization and glial
activation in rat spinal cord. J Neuroinflammation. 11:752014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hou YL, Tsai YH, Lin YH and Chao JC:
Ginseng extract and ginsenoside Rb1 attenuate carbon
tetrachloride-induced liver fibrosis in rats. BMC Complement Altern
Med. 14:4152014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huang F, Li YN, Yin F, Wu YT, Zhao DX, Li
Y, Zhang YF and Zhu QS: Ginsenoside Rb1 inhibits neuronal apoptosis
and damage, enhances spinal aquaporin 4 expression and improves
neurological deficits in rats with spinal cord ischemia-reperfusion
injury. Mol Med Rep. 11:3565–3572. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Song ZP, Xiong BR, Guan XH, Cao F,
Manyande A, Zhou YQ, Zheng H and Tian YK: Minocycline attenuates
bone cancer pain in rats by inhibiting NF-κB in spinal astrocytes.
Acta Pharmacol Sin. 37:753–762. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lu C, Liu Y, Sun B, Sun Y, Hou B, Zhang Y,
Ma Z and Gu X: Intrathecal injection of JWH-015 attenuates bone
cancer pain via time-dependent modification of pro-inflammatory
cytokines expression and astrocytes activity in spinal cord.
Inflammation. 38:1880–1890. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bloom AP, Jimenez-Andrade JM, Taylor RN,
Castañeda-Corral G, Kaczmarska MJ, Freeman KT, Coughlin KA,
Ghilardi JR, Kuskowski MA and Mantyh PW: Breast cancer-induced bone
remodeling, skeletal pain, and sprouting of sensory nerve fibers. J
Pain. 12:698–711. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Domchek SM, Younger J, Finkelstein DM and
Seiden MV: Predictors of skeletal complications in patients with
metastatic breast carcinoma. Cancer. 89:363–368. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Paice JA and Ferrell B: The management of
cancer pain. CA Cancer J Clin. 61:157–182. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Mantyh P: Bone cancer pain: Causes,
consequences, and therapeutic opportunities. Pain. 154 Suppl
1:S54–S62. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ahmed T, Raza SH, Maryam A, Setzer WN,
Braidy N, Nabavi SF, de Oliveira MR and Nabavi SM: Ginsenoside Rb1
as a neuroprotective agent: A review. Brain Res Bull. 125:30–43.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Jiang Y, Zhou Z, Meng QT, Sun Q, Su W, Lei
S, Xia Z and Xia ZY: Ginsenoside Rb1 treatment attenuates pulmonary
inflammatory cytokine release and tissue injury following
intestinal ischemia reperfusion injury in mice. Oxid Med Cell
Longev. 2015:8437212015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wang J, Qiao L, Li S and Yang G:
Protective effect of ginsenoside Rb1 against lung injury induced by
intestinal ischemia-reperfusion in rats. Molecules. 18:1214–1226.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Sun Q, Meng QT, Jiang Y, Liu HM, Lei SQ,
Su WT, Duan WN, Wu Y and Xia ZY and Xia ZY: Protective effect of
ginsenoside Rb1 against intestinal ischemia-reperfusion induced
acute renal injury in mice. PLoS One. 8:e808592013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Wu Y, Yu Y, Szabo A, Han M and Huang XF:
Central inflammation and leptin resistance are attenuated by
ginsenoside Rb1 treatment in obese mice fed a high-fat diet. PLoS
One. 9:e926182014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Cheng W, Wu D, Zuo Q, Wang Z and Fan W:
Ginsenoside Rb1 prevents interleukin-1 beta induced inflammation
and apoptosis in human articular chondrocytes. Int Orthop.
37:2065–2070. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Chen WZ, Liu S, Chen FF, Zhou CJ, Yu J,
Zhuang CL, Shen X, Chen BC and Yu Z: Prevention of postoperative
fatigue syndrome in rat model by ginsenoside Rb1 via
down-regulation of inflammation along the NMDA receptor pathway in
the hippocampus. Biol Pharm Bull. 38:239–247. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Lee JS, Song JH, Sohn NW and Shin JW:
Inhibitory effects of ginsenoside Rb1 on neuroinflammation
following systemic lipopolysaccharide treatment in mice. Phytother
Res. 27:1270–1276. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Na JY, Kim S, Song K, Lim KH, Shin GW, Kim
JH, Kim B, Kwon YB and Kwon J: Anti-apoptotic activity of
ginsenoside Rb1 in hydrogen peroxide-treated chondrocytes:
Stabilization of mitochondria and the inhibition of caspase-3. J
Ginseng Res. 36:242–247. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ni N, Liu Q, Ren H, Wu D, Luo C, Li P, Wan
JB and Su H: Ginsenoside Rb1 protects rat neural progenitor cells
against oxidative injury. Molecules. 19:3012–3024. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zhuang CL, Mao XY, Liu S, Chen WZ, Huang
DD, Zhang CJ, Chen BC, Shen X and Yu Z: Ginsenoside Rb1 improves
postoperative fatigue syndrome by reducing skeletal muscle
oxidative stress through activation of the PI3K/Akt/Nrf2 pathway in
aged rats. Eur J Pharmacol. 740:480–487. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Lu JM, Weakley SM, Yang Z, Hu M, Yao Q and
Chen C: Ginsenoside Rb1 directly scavenges hydroxyl radical and
hypochlorous acid. Curr Pharm Des. 18:6339–6347. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Xu J, Zhu MD, Zhang X, Tian H, Zhang JH,
Wu XB and Gao YJ: NFκB-mediated CXCL1 production in spinal cord
astrocytes contributes to the maintenance of bone cancer pain in
mice. J Neuroinflammation. 11:382014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Grenald SA, Doyle TM, Zhang H, Slosky LM,
Chen Z, Largent-Milnes TM, Spiegel S, Vanderah TW and Salvemini D:
Targeting the S1P/S1PR1 axis mitigates cancer-induced bone pain and
neuroinflammation. Pain. 158:1733–1742. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zhou YQ, Liu Z, Liu ZH, Chen SP, Li M,
Shahveranov A, Ye DW and Tian YK: Interleukin-6: An emerging
regulator of pathological pain. J Neuroinflammation. 13:1412016.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Zhu S, Wang C, Han Y, Song C, Hu X and Liu
Y: Sigma-1 receptor antagonist BD1047 reduces mechanical allodynia
in a rat model of bone cancer pain through the inhibition of spinal
NR1 phosphorylation and microglia activation. Mediators Inflamm.
2015:2650562015. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Zhang MY, Liu YP, Zhang LY, Yue DM, Qi DY,
Liu GJ and Liu S: Levo-tetrahydropalmatine attenuates bone cancer
pain by inhibiting microglial cells activation. Mediators Inflamm.
2015:7525122015. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Cong Y, Sun K, He X, Li J, Dong Y, Zheng
B, Tan X and Song XJ: A traditional chinese medicine xiao-ai-tong
suppresses pain through modulation of cytokines and prevents
adverse reactions of morphine treatment in bone cancer pain
patients. Mediators Inflamm. 2015:9616352015. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Li Q and Zhang X:
Epigallocatechin-3-gallate attenuates bone cancer pain involving
decreasing spinal tumor necrosis factor-α expression in a mouse
model. Int Immunopharmacol. 29:818–823. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Zhou YQ, Liu Z, Liu HQ, Liu DQ, Chen SP,
Ye DW and Tian YK: Targeting glia for bone cancer pain. Expert Opin
Ther Targets. 20:1365–1374. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Gu X, Zheng Y, Ren B, Zhang R, Mei F,
Zhang J and Ma Z: Intraperitoneal injection of thalidomide
attenuates bone cancer pain and decreases spinal tumor necrosis
factor-α expression in a mouse model. Mol Pain. 6:642010.
View Article : Google Scholar : PubMed/NCBI
|