Introduction
Peripheral artery disease (PAD) is caused by the
formation of atherosclerotic plaques in the lower extremities,
resulting in arterial stenosis and occlusion to finally lead to
chronic ischemia of the extremities. Epidemiological surveys have
indicated that PAD is positively correlated with age, and
hypertension, hyperlipidemia, smoking and a family history of PAD
are all risk factors for PAD (1,2). In
China, the incidence of patients with PAD and arteriosclerosis
obliterans of the lower extremities is increasing annually, and
this is attributed o an aging population due to improved medical
care and overall living standards (3). Minimally invasive endovascular
therapies, including stent placement (4) and percutaneous transluminal angioplasty
(PTA) (5), provide a safer and more
reliable treatment for PAD. However, these therapies may cause
damage to the vascular intima, leading to post-operative vascular
restenosis (6). Furthermore,
interventional procedures severely affect post-operative recovery
and the quality of life of elderly PAD patients (7). Therefore, early prediction and
treatment of post-operative vascular restenosis in PAD patients may
greatly improve their prognosis (8).
P-selectin (Ps) (9) and endothelin-1
(ET-1) (10) are important proteins
that reflect the damage, activation and synthesis of vascular
endothelial cells (VECs). In the present study, the serum levels of
Ps and ET-1 were monitored in PAD patients after endovascular
therapy and their correlation with post-operative vascular
restenosis was assessed in order to determine their early
predictive value regarding this adverse event.
Patients and methods
Patients
A total of 20 PAD cases with restenosis and another
20 PAD cases or without restenosis after endovascular therapy were
enrolled in the present study between March 2015 and December 2015
from Taizhou Hospital Affiliated to Nanjing University of Chinese
Medicine. The restenosis and non-restenosis groups were comparable
in age, sex, incidence of concurrent hypertension or
hyperlipidemia, location of the lesion, Rutherford classification
and family history of PAD (P>0.05). The demographic and
clinicopathological characteristics of the subjects at baseline are
presented in Table I. All patients
provided written informed consent. All of the experiments were
approved by the Ethics Committee of Nanjing University of Chinese
Medicine (Nanjing, China).
 | Table I.Comparison of the demographic and
clinicopathological characteristics of the patients in the
restenosis vs. non-restenosis group (n=20 per group). |
Table I.
Comparison of the demographic and
clinicopathological characteristics of the patients in the
restenosis vs. non-restenosis group (n=20 per group).
| Characteristics | Restenosis group | Non-restenosis
group | t/χ2 | P-value |
|---|
| Average age,
years | 63.20±6.39 | 62.70±6.18 | 0.252 | 0.803 |
| Male, n (%) | 12 (60) | 11 (55) | 0.102 | 0.794 |
| Comorbidities |
|
|
|
|
|
Hypertension, n (%) | 18 (90) | 19 (95) | 0.360 | 0.548 |
|
Hyperlipidemia, n (%) | 16 (80) | 13 (65) | 1.129 | 0.288 |
| Family history of
PAD, n (%) | 15 (75) | 13 (65) | 0.476 | 0.490 |
| Smoking, n (%) | 12 (60) | 8 (40) | 1.600 | 0.206 |
| Rutherford stage, n
(%) |
|
| 0.702 | 0.873 |
| III | 3 (15) | 5 (25) |
|
|
| IV | 9 (45) | 8 (40) |
|
|
| V | 4 (20) | 4 (20) |
|
|
| VI | 4 (20) | 3 (15) |
|
|
| Lesion site, n
(%) |
|
| 0.567 | 0.904 |
|
Unilateral iliac artery | 6 (30) | 5 (25) |
|
|
| Simple
superficial femoral artery | 5 (25) | 7 (35) |
|
|
|
Ipsilateral iliac and femoral
artery | 5 (25) | 5 (25) |
|
|
| Femoral
popliteal artery | 4 (20) | 3 (15) |
|
|
Diagnostic methods and
comparisons
Restenosis was diagnosed by post-operative
examination using computed tomography angiography (CTA). Cases with
and without restenosis were compared regarding age, sex, incidence
of concurrent hypertension or hyperlipidemia, location of the
lesion, Rutherford classification, family history of diseases and
smoking status. The serum levels of Ps and ET-1 prior to the
operation and at 1 h, 1, 2 and 3 weeks after the operation were
compared within and between groups.
Processing and detection of blood
samples
From each subject, 5 ml blood was drawn on the
morning prior to the operation and at 1 h, 1, 2 and 3 weeks after
the operation. The blood samples were collected in tubes containing
Na2EDTA anti-coagulant and centrifuged at 1,500 × g for
10 min. The supernatant was collected and preserved at −80°C or
directly used for the detection of Ps and ET-1. Serum Ps was
detected using a human Ps detection kit (cat. no. P1038; Shanghai
Airui Biotechnology Co., Ltd., Shanghai, China) and serum ET-1 was
detected using a human ET-1 detection kit (cat. no. E2567; Shanghai
Yu Bo Biotech Co., Ltd., Shanghai, China), which were performed in
triplicate.
Statistical analysis
Data were analyzed using SPSS 19.0 software (IBM
Corp., Armonk, NY, USA). The patient age and serum levels of Ps and
ET-1 were expressed as the mean ± standard deviation. An
independent-samples t-test was performed to determine the
significance of differences between the two groups. Count data were
expressed as n (%) and compared between the two groups using the
Chi-squared test. The predictive value of Ps and ET-1 for
restenosis was determined by generating receiver operating
characteristics (ROC) curves and determining the area under the ROC
curve (AUC), as well as the sensitivity and specificity at optimal
cut-off values. P<0.05 was considered to indicate a
statistically significant difference.
Results
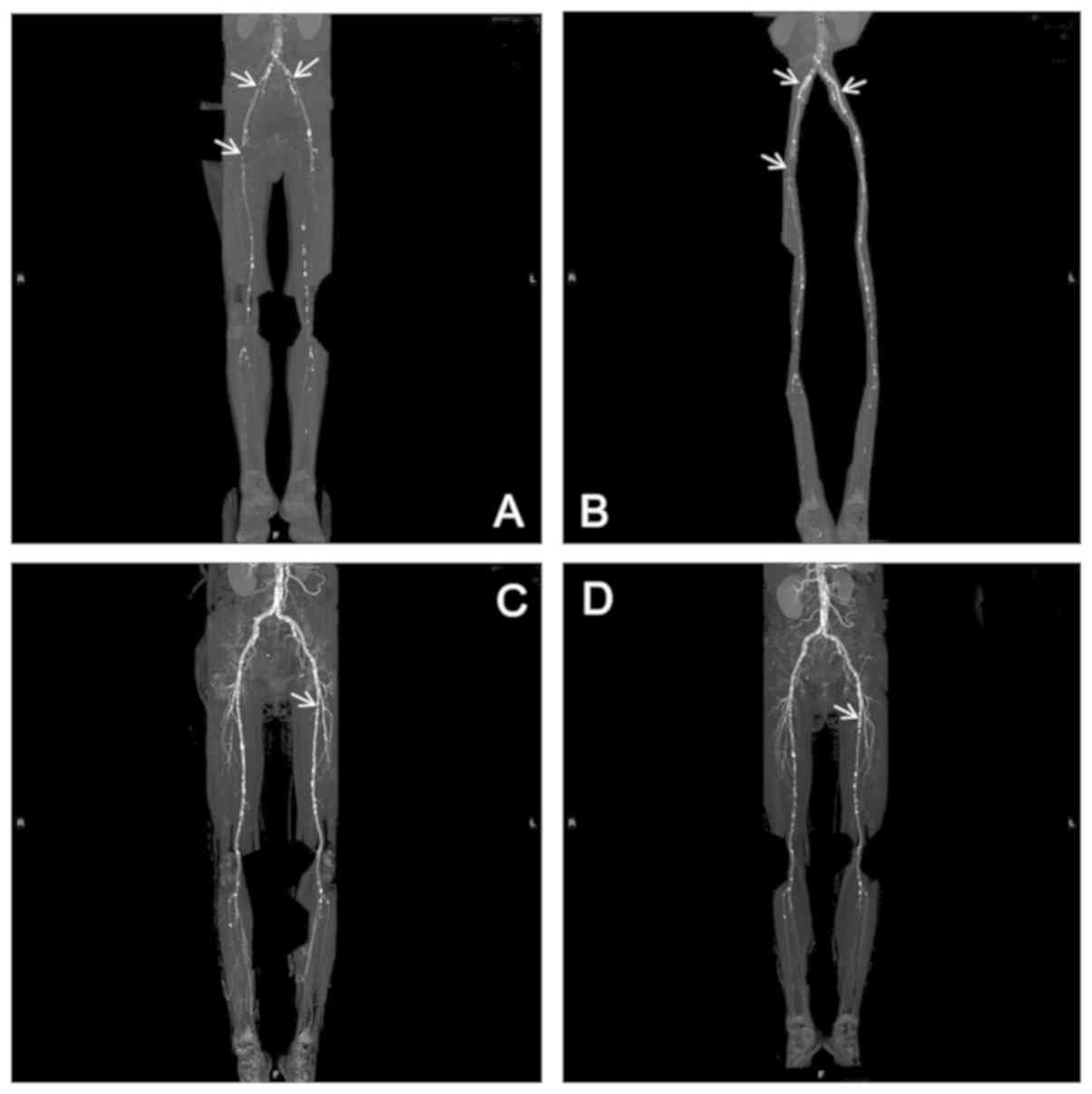
Comparison of pre- and post-operative
CTA observations between the two groups
The position of the lesions was confirmed by CTA.
The two representative cases in Fig. 1A
and B had stenosis of the iliac artery and received PTA
combined with stent placement. They were followed up for 1 year
post-operatively. The first representative case had post-operative
restenosis (Fig. 1C), while the
second one had no restenosis (Fig.
1D).
Comparison of serum Ps levels at
different time-points
Compared with the pre-operative level, the level of
serum Ps 1 h after the operation was significantly increased in the
PAD cases (P<0.05), and then declined over time until
stabilizing 2 weeks post-operatively. The serum Ps levels at 1 h,
1, 2 and 3 weeks after the operation in the restenosis group were
significantly higher than those in the non-restenosis group
(P<0.05). Within the restenosis group, the post-operative Ps
levels were also significantly higher than the pre-operative ones
(P<0.05). However, for the non-restenosis group, the serum Ps
levels at 1, 2 and 3 weeks post-operatively were not significantly
different from the pre-operative levels (P>0.05; Table II).
 | Table II.Comparison of serum P-selectin levels
at different time-points (ng/ml). |
Table II.
Comparison of serum P-selectin levels
at different time-points (ng/ml).
| Groups/time | Restenosis group
(n=20) | Non-restenosis group
(n=20) | t | P-value |
|---|
| Pre-operative | 20.54±2.40 | 20.97±2.13 |
0.594 |
0.556 |
| Post-operative |
|
|
|
|
| 1 h |
41.67±3.89a |
34.82±3.16a |
6.123 | <0.001 |
| 1
week |
34.19±3.76a | 22.63±3.69 |
9.817 | <0.001 |
| 2
weeks |
32.15±2.56a | 19.95±2.05 | 16.616 | <0.001 |
| 3
weeks |
32.00±2.77a | 19.88±1.76 | 16.504 | <0.001 |
Comparison of serum ET-1 levels at
different time-points
As compared with the pre-operative level, the serum
ET-1 level at 1 h after the operation was significantly increased
in all PAD cases (P<0.05), and it declined afterwards until
stabilizing at 2 weeks post-operatively. The serum ET-1 levels at 1
h, 1, 2 and 3 weeks post-operatively in the restenosis group, were
significantly higher than those in the non-restenosis group
(P<0.05). Within the restenosis group, they were also
significantly higher than the pre-operative levels (P<0.05).
However, in the non-restenosis group, the serum ET-1 levels at 1, 2
and 3 weeks post-operatively were not significantly different from
the pre-operative levels (P>0.05; Table III).
 | Table III.Comparison of serum endothelin-1
levels (pg/ml) at different time-points. |
Table III.
Comparison of serum endothelin-1
levels (pg/ml) at different time-points.
| Groups/time | Restenosis group
(n=20) | Non-restenosis group
(n=20) | t | P-value |
|---|
| Pre-operative | 75.29±3.62 | 75.16±3.56 | 0.110 | 0.913 |
| Post-operative |
|
|
|
|
| 1 h |
114.21±4.60a |
101.97±5.18a | 7.901 | <0.001 |
| 1 week |
98.58±5.16a | 80.66±5.46 | 10.664 | <0.001 |
| 2 weeks |
97.95±5.88a | 77.39±4.79 | 12.114 | <0.001 |
| 3 weeks |
97.71±5.34a | 77.04±3.34 | 14.680 | <0.001 |
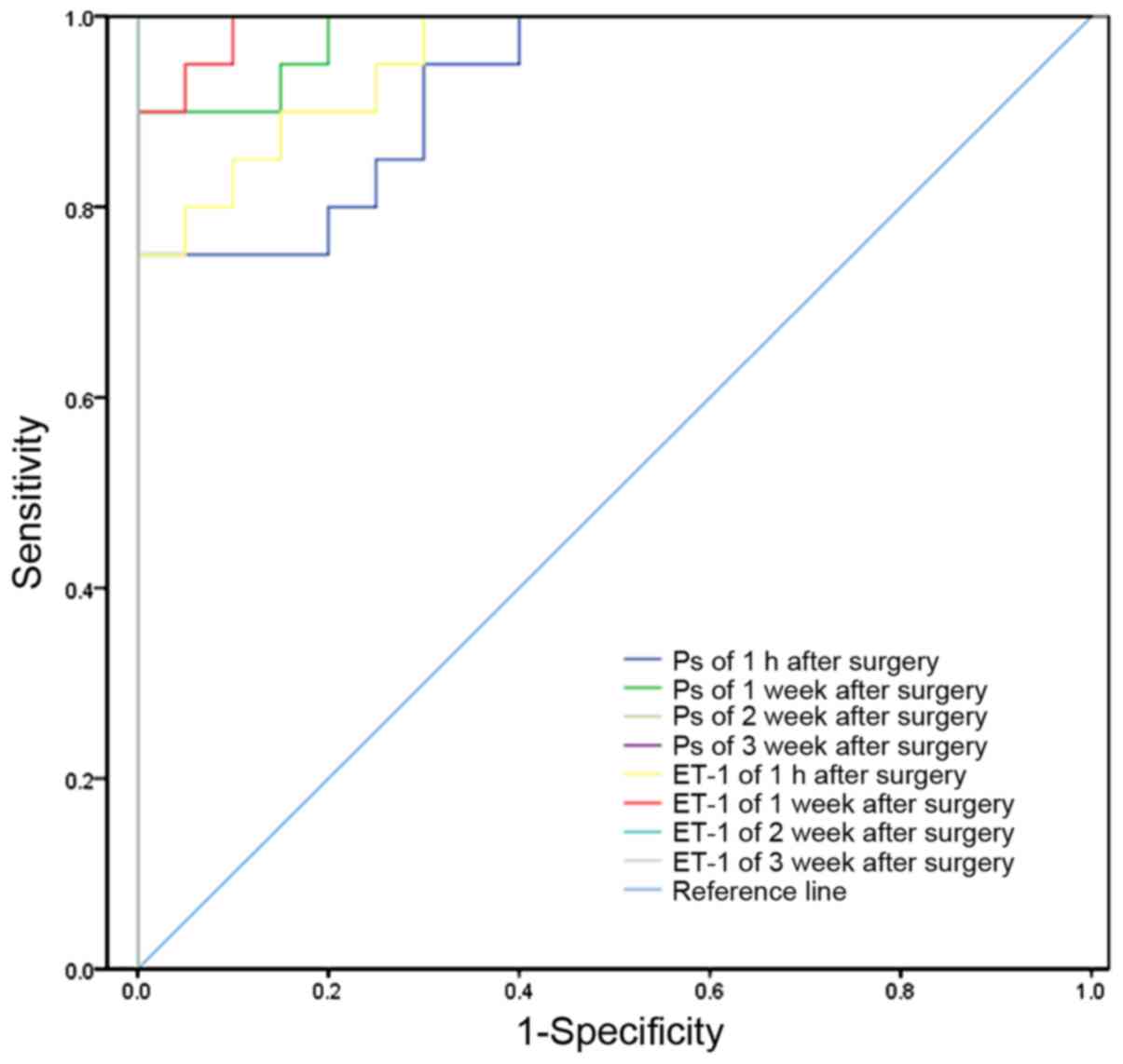
Predictive value of Ps and ET-1 levels
for post-operative restenosis
ROC curves comparing the sensitivity vs. specificity
of the serum levels of Ps or ET-1 for predicting post-operative
restenosis were plotted using SPSS 19.0 software (Fig. 2). For the serum levels of Ps as well
as ET-1, the AUC was >0.5 at each time-point post-operatively.
The AUC increased over time, indicating a better diagnostic value
of the later time-points for post-operative restenosis. However, in
the clinic, earlier discovery and treatment of post-operative
restenosis for PAD cases results in better the outcomes.
The optimal diagnostic threshold at 1 h
post-operatively was 38.83 ng/ml for serum Ps levels, as calculated
from the ROC curve. The corresponding sensitivity and specificity
for predicting restenosis were 75 and 90%, respectively. The
optimal diagnostic threshold at 1 h post-operatively was 0.1089
ng/ml for serum ET-1 levels, as calculated from the ROC curve. The
corresponding sensitivity and specificity for predicting restenosis
were 85 and 85%, respectively.
Discussion
VECs provide a barrier between the vascular system
and underlying tissues. The nitric oxide, endothelin, angiotensin
and growth factors secreted by VECs mediate vascular relaxation and
contraction. Arteriosclerosis may induce the secretion of
heparin-like substances, smooth muscle relaxant factors and smooth
muscle constricting factors by VECs, thus inhibiting the
proliferation and migration of VECs (9,10).
Abnormal proliferation and migration of the VECs are considered as
the major reasons for post-operative restenosis for PAD patients,
as they result in intimal hyperplasia and remodeling of elasticity
of vascular walls (11).
Interventional therapies for PAD patients may cause damage to the
vascular endothelium, leading to decreased secretion of factors
that inhibit the proliferation and migration of smooth muscle cells
(SMCs); this in turn may cause restenosis to occur (6). In addition, damage of VECs may further
promote thrombosis and vasoconstriction, leading to restenosis.
Therefore, evaluating the damage of VECs in PAD patients after
endovascular therapy is of high importance for predicting
post-operative restenosis.
Ps is an important member of the selectin family of
cell adhesion molecules (12). Under
normal physiological conditions, Ps rests on the granule membrane
of platelets. Once activated by VEC damage, the platelets release
the platelet α granules and Ps is released along with them.
Therefore, Ps is considered as an indicator of the activated state
of the platelets. For PAD patients who have received interventional
therapy, the activated state of the platelets may be used to assess
the degree of VEC damage. Therefore, Ps is an indirect indicator of
VEC damage. In the present study, the serum Ps levels were
significantly increased in PAD patients at 1 h after the operation
as compared with the pre-operative levels (P<0.05). Thomas et
al (13) reported a significant
correlation between Ps levels and the post-operative onset of
cardiovascular events in acute coronary syndrome. According to
Myers Jr et al (14), oral Ps
inhibitor PSI-697 reduced thrombosis in rats with venous stenosis.
This means that Ps levels in the blood are not only an indicator of
VEC damage, but also associated with thrombosis and restenosis.
Inhibiting blood Ps may help reduce restenosis in PAD cases.
In the present study, the serum Ps levels at 1 h, 1,
2 and 3 weeks post-operatively in the restenosis group were
significantly higher than those in the non-restenosis group
(P<0.05); they were also considerably increased as compared with
the pre-operative level within the restenosis group (P<0.05).
However, for the non-restenosis group, there was no significant
difference in the serum Ps levels at 1 h, 1, 2 and 3 weeks
post-operatively as compared with the pre-operative level
(P>0.05). For the serum Ps levels, the sensitivity and
specificity for predicting restenosis in PAD patients were 75 and
90%, respectively, with a cut-off at 38.85 ng/ml. Ps on the
platelet α granule membrane not only promotes the expression and
secretion of tissue factors by the leukocytes, thus triggering
coagulation, but also recruit neutrophil granulocytes, thus
aggravating VEC damage. This further promotes thrombosis and
increases the risk of restenosis (15). Ps is a member of the selectin family
of cell adhesion molecules. It is expressed on stimulated
endothelial cells and activated platelets, and mediates leukocyte
rolling on stimulated endothelial cells, as well as heterotypic
aggregation of activated platelets onto leukocytes (16). The importance of Ps-mediated cell
adhesive interactions in the pathogeneses of inflammation and
thrombosis has been demonstrated in Ps-knockout mice (17). Therefore, the post-operative serum Ps
levels in PAD cases may provide information on VEC damage and serve
in the prediction of restenosis.
ET-1 is a vasoconstrictor secreted mainly by
endothelial cells. It activates the Ca2+ channel of
vascular SMCs by binding to receptors and then induces contraction
of vascular SMCs. In the present study, a significant increase in
the serum ET-1 levels was identified in PAD patients at 1 h
post-operatively (P<0.05). Furthermore, the ET-1 levels at 1 h,
1, 2 and 3 weeks post-operatively in the restenosis group were
significantly higher than those in the non-restenosis group
(P<0.05); they were also higher than the pre-operative levels
within the restenosis group (P<0.05). However, for the
non-restenosis group, the serum ET-1 levels at 1 h, 1, 2 and 3
weeks post-operatively were not significantly different from the
pre-operative level (P>0.05).
The reasons for the increased ET-1 secretion after
endovascular therapy remain to be fully elucidated. Upregulation of
ET-1 promotes the proliferation and migration of SMCs, thus leading
to intimal hyperplasia and post-operative restenosis (18). According to Biasin et al
(19) and Jiang et al
(20) upregulation of ET-1 resulted
in the proliferation of pulmonary artery SMCs. Under normal
conditions, a dynamic balance between vasoconstrictive factors
(e.g., ET-1) and vasodilatory factors (e.g., nitric oxide)
prevails. However, upregulation of ET-1 following endovascular
therapy disturbs this balance, leading to enhanced platelet
adhesion, thrombosis, and abnormal proliferation and migration of
SMCs (21,22). This finally results in restenosis.
Therefore, the ET-1 levels after endovascular therapy may serve as
a predictive marker for restenosis. Based on the present results,
the sensitivity and specificity of serum ET-1 with a cut-off at
0.1089 pg/ml at 1 h after the operation for predicting restenosis
were 85 and 85%, respectively.
In conclusion, the levels of serum Ps and ET-1 in
PAD patients after endovascular surgery are of great clinical value
for predicting post-operative vascular restenosis.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed in the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NC and TL contributed to the concept and design of
the study. NC and TL analyzed and interpreted the patient data. LC,
SJ and ZW analyzed the data. NC, LC and TL prepared the manuscript.
All authors read and approved the final manuscript.
Ethical approval and consent to
participate
All of the experiments were approved by the Ethics
Committee of Nanjing University of Chinese Medicine (Nanjing,
China). All patients provided written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Alahdab F, Wang AT, Elraiyah TA, Malgor
RD, Rizvi AZ, Lane MA, Prokop LJ, Montori VM, Conte MS and Murad
MH: A systematic review for the screening for peripheral arterial
disease in asymptomatic patients. J Vasc Surg. 61 Suppl 3:S42–S53.
2015. View Article : Google Scholar
|
|
2
|
Criqui MH and Aboyans V: Epidemiology of
peripheral artery disease. Circ Res. 116:1509–1526. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lin TY, Yang FC, Lin CL, Kao CH, Lo HY and
Yang TY: Herpes zoster infection increases the risk of peripheral
arterial disease: A nationwide cohort study. Medicine (Baltimore).
95:e44802016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Baerlocher MO, Kennedy SA, Rajebi MR,
Baerlocher FJ, Misra S, Liu D and Nikolic B: Meta-analysis of
drug-eluting balloon angioplasty and drug-eluting stent placement
for infrainguinal peripheral arterial disease. J Vasc Interv
Radiol. 26:459–473. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kumada Y, Aoyama T, Ishii H, Tanaka M,
Kawamura Y, Takahashi H, Toriyama T, Aoyama T, Yuzawa Y, Maruyama
S, et al: Long-term outcome of percutaneous transluminal
angioplasty in chronic haemodialysis patients with peripheral
arterial disease. Nephrol Dial Transplant. 23:3996–4001. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Koskinas KC, Chatzizisis YS, Antoniadis AP
and Giannoglou GD: Role of endothelial shear stress in stent
restenosis and thrombosis: Pathophysiologic mechanisms and
implications for clinical translation. J Am Coll Cardiol.
59:1337–1349. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wilson WR, Fitridge RA, Weekes AJ, Morgan
C, Tavella R and Beltrame JF: Quality of life of patients with
peripheral arterial disease and chronic stable angina. Angiology.
63:223–228. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kumakura H, Kanai H, Araki Y, Hojo Y,
Iwasaki T and Ichikawa S: 15-year patency and life expectancy after
primary stenting guided by intravascular ultrasound for iliac
artery lesions in peripheral arterial disease. JACC Cardiovasc
Interv. 8:1893–1901. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kutlar A, Ataga KI, McMahon L, Howard J,
Galacteros F, Hagar W, Vichinsky E, Cheung AT, Matsui N and Embury
SH: A potent oral P-selectin blocking agent improves
microcirculatory blood flow and a marker of endothelial cell injury
in patients with sickle cell disease. Am J Hematol. 87:536–539.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abraham D and Distler O: How does
endothelial cell injury start? The role of endothelin in systemic
sclerosis. Arthritis Res Ther. 9 Suppl 2:S22007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Michel JB, Li Z and Lacolley P: Smooth
muscle cells and vascular diseases. Cardiovasc Res. 95:135–137.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gu P, Theiss A, Han J and Feagins LA:
Increased cell adhesion molecules, PECAM-1, ICAM-3, or VCAM-1,
predict increased risk for flare in patients with quiescent
inflammatory bowel disease. J Clin Gastroenterol. 51:522–527. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Thomas MR, Wijeyeratne YD, May JA, Johnson
A, Heptinstall S and Fox SC: A platelet P-selectin test predicts
adverse cardiovascular events in patients with acute coronary
syndromes treated with aspirin and clopidogrel. Platelets.
25:612–618. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Myers DD Jr, Henke PK, Bedard PW,
Wrobleski SK, Kaila N, Shaw G, Meier TR, Hawley AE, Schaub RG and
Wakefield TW: Treatment with an oral small molecule inhibitor of P
selectin (PSI-697) decreases vein wall injury in a rat stenosis
model of venous thrombosis. J Vasc Surg. 44:625–632. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pabinger I and Ay C: Biomarkers and venous
thromboembolism. Arterioscler Thromb Vasc Biol. 29:332–336. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Geng JG, Chen M and Chou KC: P-selectin
cell adhesion molecule in inflammation, thrombosis, cancer growth
and metastasis. Curr Med Chem. 11:2153–2160. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Panicker SR, Mehta-D'souza P, Zhang N,
Klopocki AG, Shao B and Mcever RP: Circulating soluble P-selectin
must dimerize to promote inflammation and coagulation in mice.
Blood. 130:181–191. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Pabinger I and Ay C: Biomarkers and venous
thromboembolism. Arterioscler Thromb Vasc Biol. 29:332–336. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Biasin V, Chwalek K, Wilhelm J, Best J,
Marsh LM, Ghanim B, Klepetko W, Fink L, Schermuly RT, Weissmann N,
et al: Endothelin-1 driven proliferation of pulmonary arterial
smooth muscle cells is c-fos dependent. Int J Biochem Cell Biol.
54:137–148. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jiang HN, Zeng B, Chen GL, Lai B, Lu SH
and Qu JM: Lipopolysaccharide potentiates endothelin-1-induced
proliferation of pulmonary arterial smooth muscle cells by
upregulating TRPC channels. Biomed Pharmacother. 82:20–27. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Meoli DF and White RJ: Endothelin-1
induces pulmonary but not aortic smooth muscle cell migration by
activating ERK1/2 MAP kinase. Can J Physiol Pharmacol. 88:830–839.
2010. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Romano F, Gambara G, De Cesaris P, Ziparo
E, Palombi F and Filippini A: Endothelin induces functional
hypertrophy of peritubular smooth muscle cells. J Cell Physiol.
212:264–273. 2007. View Article : Google Scholar : PubMed/NCBI
|