Introduction
Thrombosis is a common complication of autologous
arteriovenous fistulas (AVF) for hemodialysis access in patients
with end-stage renal disease (1).
AVF thrombosis accounts for 65–85% of permanent access loss
(2). Following the creation of AVFs,
early-onset thrombosis is due to inadequate blood inflow and
late-onset thrombosis is associated with stenotic lesions (1,3,4). AVF thrombosis is also a major cause of
permanent access loss (3), resulting
in missed hemodialysis, hospitalization and increased medical costs
(1). Taking into consideration that
vascular injury, platelet abnormalities and hypercoagulability may
contribute to fistula thrombosis, fish oil, anti-platelet agents
and oral anti-coagulants have been tested in clinical trials for
preventing thrombosed access. However, to the best of our
knowledge, there is currently no pharmacological therapy with a
proven ability to prevent AVF thrombosis (5).
Only a limited number of methods have been developed
to treat access thrombosis, including pharmacological thrombolytic
therapy, surgical thrombectomy and percutaneous declotting
procedures (3). Urokinase has been
successfully used as a thrombolytic agent for resolving thrombosed
vascular access (6,7). Previously, urokinase was administered
through a 22-gauge angiographic catheter introduced into the
fistula prior to percutaneous interventions, also known as the
‘lyse and wait’ technique (2,8).
Pulse-spray-aided pharmacomechanical thrombolysis employs the
administration of tissue plasminogen activator and mechanical
declotting techniques (9). According
to the Clinical Practice Guidelines for Vascular Access published
by the Vascular Access 2006 Work Group, thrombosed fistulas may be
declotted purely by using a mechanical method or a thrombolytic
agent (10). Intravenous (IV)
infusion of urokinase is a feasible strategy that does not require
introduction of a catheter. Urokinase has been used in thrombolytic
treatment for venous thrombosis through the systemic and
locoregional routes (11). In a
thrombosed AVF, urokinase infused via peripheral veins reaches the
access thrombus from the radial artery end through the systemic
blood flow, whereas urokinase infused into the fistulous vein may
come in direct contact with the access thrombus. However, the
optimal route for IV infusion of urokinase for the treatment of
access thrombosis remains elusive.
In the present study, it was hypothesized that local
venous infusion of urokinase is superior to peripheral
administration for the treatment of patients with AVF thrombosis.
Retrospective data analysis was performed, and comparisons of
thrombolytic success rates and adverse events were performed
between patients receiving local and peripheral venous infusion of
urokinase for the treatment of access thrombosis. The factors
affecting the success rate of local venous thrombolytic therapy
were also examined.
Materials and methods
Study population
A total of 106 patients (56 males; median age, 47
years; age range, 27–66 years) who received hemodialysis at a
single high-care hemodialysis unit at the First Affiliated Hospital
of Chongqing Medical University (Chongqing, China) between January
2011 and December 2014 were included in the present study. All
patients presented with acute thrombosis in their radio-cephalic
AVFs. The thrombus age was determined as the time period from the
moment the patients experienced disappearance of thrill, as
reported by the patient, to the initiation of thrombolytic therapy.
The diagnosis of a thrombosed fistula was based on the absence of
thrill on physical examination and evidence of thrombosis on
vascular ultrasound scanning. The exclusion criteria were as
follows: i) Active bleeding or bleeding tendency; ii) active liver
disease; iii) severe hypertension (systolic blood pressure >160
mmHg and/or diastolic blood pressure >90 mmHg). Informed consent
to participate in the current study was obtained from all patients.
The Institutional Review Board of the First Affiliated Hospital of
Chongqing Medical University (Chongqing, China) reviewed and
approved the study protocol.
Procedures and observations
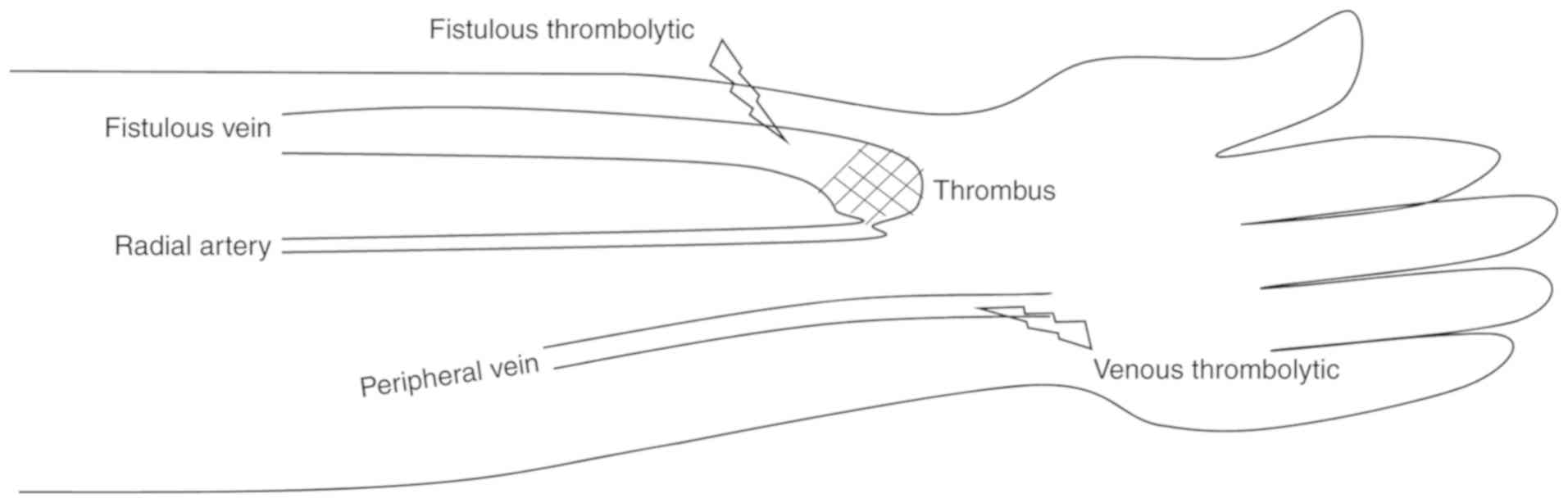
Patients received urokinase infusion through either
the fistulous vein (local venous thrombolysis) or the peripheral
vein (peripheral venous thrombolysis). As illustrated in Fig. 1, for local thrombolysis, an IV needle
was inserted into the fistulous vein with the needle tip directed
towards the thrombus. For peripheral venous thrombolysis, the IV
needle was inserted into the dorsal venous network of the hand. For
each thrombolytic therapy, 300,000 U urokinase in 20 ml saline was
infused within 1 h. The effect of the thrombolytic therapy was
observed through physical examination every 20 min by detecting
palpable thrill and bruit with auscultation. The urokinase
thrombolytic therapy was performed three times in total with an
interval period of 30 min until the thrombus was dissolved. The
total amount of urokinase used in the thrombolytic therapy was
recorded. Adverse effects, including ecchymosis, epistaxis,
gingival bleeding, bleeding at punctures sites and systemic
bleeding complications (i.e., gastrointestinal bleeding) were
recorded as well. The criteria for considering a thrombolysis
successful included the following: Recurrence of thrill and bruit
on physical examination; dissolution of thrombi and restoration of
blood flow in the AVF, verified by vascular ultrasound; and >1
completed hemodialysis session with a blood flow of >180 ml/min.
This value was adapted from a previous study (12). In addition, a blood flow of <180
ml/min was considered to indicate access failure (13). Subsequent to thrombolysis therapy,
the patients were administered the following for the next 7 days:
Low-molecular-weight heparin (1 mg/kg, subcutaneously) twice daily
and aspirin (100 mg/day, orally) daily.
Statistical analysis
Values are expressed as the mean ± standard
deviation for continuous variables and as n (%) for categorical
variables. Statistical analysis was performed using SSPS version
21.0 software (IBM Corp., Armonk, NY, USA). For comparison of
continuous variables between two groups, the Student's t-test was
performed. Categorical variables were analyzed using the
χ2 test. Factors that potentially affect the success of
thrombolysis were analyzed by using binary logistic regression, and
the odds ratio (OR) and confidence interval (CI) were calculated.
P<0.05 was considered to indicate statistical significance.
Results
Patient characteristics
In total, 106 patients receiving hemodialysis were
included. The patient characteristics in the two groups (local or
peripheral venous thrombolysis) are presented in Table I. Age, sex, period of dialysis, time
of AVF placement, systolic and diastolic blood pressure, and
thrombus age were similar between patients who underwent local and
peripheral venous thrombolytic therapy (Table I). All thrombi were located at
juxta-anastomotic sites, as illustrated in Fig. 1. The total amount of urokinase used
in the local and peripheral thrombolysis group was 31.4±16.6 and
34.2±14.8×104 U, respectively (Table I). Biochemical test results in the
two groups prior to and after thrombolytic therapy are presented in
Supplementary Table SI. Serum
alanine aminotransferase levels were significantly increased (but
the levels remained within the normal range) following thrombolytic
therapy in the peripheral venous group (P<0.05), but the levels
did not increase in the local venous group (Table SI). Serum creatinine levels were
slightly and significantly increased (within the normal range)
following thrombolysis in the peripheral and local venous groups
(both P<0.01). Prothrombin time was significantly increased
while fibrinogen levels were significantly decreased following
thrombolytic therapy in the peripheral and local venous groups (all
P<0.01).
 | Table I.Demographic and clinical
characteristics of the patients. |
Table I.
Demographic and clinical
characteristics of the patients.
| Parameter | Local venous
thrombolysis (n=49) | Peripheral venous
thrombolysis (n=57) | P-value |
|---|
| Age (years) | 46.4±7.3 | 47.0±9.1 | 0.74 |
| Males | 26 (53.1) | 30 (52.6) | 0.96 |
| Dialysis period
(months) | 54.0±15.2 | 58.1±17.9 | 0.22 |
| Fistula age
(months) | 45.1±23.5 | 46.5±16.5 | 0.71 |
| SBP (mmHg) | 142.7±18.8 | 143.0±20.3 | 0.94 |
| DBP (mmHg) | 84.1±17.3 | 81.7±16.1 | 0.46 |
| Thrombus age (h) | 25.6±12.6 | 27.3±13.6 | 0.52 |
| Urokinase dose
(×104 U) | 31.4±16.6 | 34.2±14.8 | 0.36 |
Success rates of thrombolytic
therapy
As presented in Table
II, the cumulative success rates of thrombolytic therapy with
urokinase were 44.9 vs. 29.8% (P=0.11) following one, 65.3 vs.
49.1% (P=0.09) following two and 85.7 vs. 68.4% (P=0.04) following
three sessions. In the local thrombolysis group, the thrombolysis
success rate was >85% following three sessions of thrombolytic
therapy, which was significantly higher compared with that in the
peripheral thrombolysis group (P<0.05; Table II).
 | Table II.Rates of successful thrombolysis. |
Table II.
Rates of successful thrombolysis.
| Item | Local venous
thrombolysis (n=49) | Peripheral venous
thrombolysis (n=57) | P-value |
|---|
| First thrombolytic
therapy | 22 (44.9) | 17 (29.8) | 0.11 |
| Second thrombolytic
therapy | 10 (37.0) | 11 (27.5) | 0.43 |
| Third thrombolytic
therapy | 10 (58.8) | 11 (37.9) | 0.23 |
| Cumulative success
after second thrombolytic therapy | 32 (65.3) | 28 (49.1) | 0.09 |
| Cumulative success
after third thrombolytic therapy | 42 (85.7) | 39 (68.4) | 0.04 |
Adverse effects of thrombolytic
therapy
Mild superficial hemorrhages, including ecchymosis,
epistaxis and gingival bleeding, occurring in patients of the local
thrombolysis and peripheral venous thrombolysis groups were
recorded (Table III). However, no
massive hemorrhagic events were observed. Patients in the local
thrombolysis group tended to have less ecchymosis (4.1 vs. 14.0%;
P=0.07) and epistaxis (2.0 vs. 10.5%; P=0.08) events compared with
those in the peripheral venous thrombolysis group. In particular,
the rate of gingival bleeding was significantly lower in the local
thrombolysis group compared with that in the peripheral venous
thrombolysis group (4.1 vs. 19.3%; P=0.02; Table III). No infectious or
thrombo-embolic complications were observed following the
procedure.
 | Table III.Adverse effects in patients who
underwent thrombolytic therapy. |
Table III.
Adverse effects in patients who
underwent thrombolytic therapy.
| Adverse event | Local venous
thrombolysis (n=49) | Peripheral venous
thrombolysis (n=57) | P-value |
|---|
| Ecchymosis | 2 (4.1) | 8 (14.0) | 0.07 |
| Epistaxis | 1 (2.0) | 6 (10.5) | 0.08 |
| Gingival
bleeding | 2 (4.1) | 11 (19.3) | 0.02 |
| Total events | 5 (10.2) | 25 (43.9) | <0.01 |
Factors affecting the success of
thrombolysis
A comparison of the demographic and clinical
characteristics between patients who had a successful and an
unsuccessful thrombolysis in the local thrombolysis group was
performed. The results indicated that age, sex, period of dialysis,
time of AVF placement and the total amount of infused urokinase
were similar between patients with successful and unsuccessful
thrombolysis (Table IV). In the
local venous thrombolysis group, systolic and diastolic blood
pressure levels were higher (P<0.01), but the age of the thrombi
(P<0.05) was lower in patients with successful thrombolysis
compared with that in patients with unsuccessful thrombolysis
(Table IV). Univariate logistic
regression analysis demonstrated that systolic (OR=1.10; 95% CI,
1.03–1.17; P<0.01) and diastolic (OR=1.08; 95% CI, 1.02–1.14;
P<0.05) blood pressure were protective factors, whereas thrombus
age (OR=0.91; 95% CI, 0.84–0.99; P<0.05) was a risk factor for
thrombolysis success among patients who underwent local
thrombolytic therapy (Table V).
However, a multivariate logistic regression analysis only
identified systolic blood pressure as a protective factor for
thrombolysis success in local thrombolytic therapy (OR=1.11; 95%
CI, 1.02–1.21; P<0.05; Table V).
In the peripheral venous thrombolysis group, only the thrombus age
was higher in patients with failed thrombolysis compared with
patients with successful thrombolysis (P<0.01; Table IV). Univariate logistic regression
analysis demonstrated that the thrombus age was a risk factor for
thrombolysis success in patients who underwent peripheral
thrombolytic therapy (OR=0.94; 95% CI, 0.90–0.99; P<0.05).
 | Table IV.Characteristics of patients with
successful or failed thrombolytic therapy. |
Table IV.
Characteristics of patients with
successful or failed thrombolytic therapy.
|
| Local venous
thrombolysis | Peripheral venous
thrombolysis |
|---|
|
|
|
|
|---|
| Parameter | Successful
(n=42) | Failed (n=7) | Successful
(n=39) | Failed (n=18) |
|---|
| Age (years) | 45.5±8.7 | 46.7±9.2 | 47.6±9.5 | 45.7±8.4 |
| Males | 22 (52.4) | 4 (57.1) | 20 (51.3) | 10 (55.6) |
| Dialysis age
(months) |
55.2±17.4 |
57.7±18.2 |
60.5±18.6 |
52.7±15.4 |
| Fistula age,
months |
44.6±25.2 |
45.7±16.4 |
47.2±17.3 |
45.1±15.0 |
| SBP (mmHg) | 146.8±16.2 |
118.3±14.9a | 142.5±20.4 | 143.9±20.6 |
| DBP (mmHg) |
87.0±16.9 |
66.9±6.8a |
80.8±16.1 |
83.6±16.3 |
| Thrombus age
(h) |
23.9±11.6 |
35.9±14.3b |
24.3±11.8 |
33.7±15.4b |
 | Table V.Factors contributing to successful
local venous thrombolytic therapy. |
Table V.
Factors contributing to successful
local venous thrombolytic therapy.
| A, Univariate
logistic regression analysis |
|---|
|
|---|
| Parameter | β | SE | P-value | OR | 95%CI |
|---|
| SBP (mmHg) | 0.10 | 0.03 | <0.01 | 1.10 | 1.03–1.17 |
| DBP (mmHg) | 0.08 | 0.03 | <0.05 | 1.08 | 1.02–1.14 |
| Thrombus age
(h) | −0.09 | 0.04 | <0.05 | 0.91 | 0.84–0.99 |
|
| B, Multivariate
logistic regression analysis |
|
| SBP
(mmHg) | 0.10 | 0.04 |
<0.05 | 1.11 |
1.02–1.21 |
|
| DBP (mmHg) | 0.09 | 0.05 | 0.06 | 1.10 | 1.00–1.21 |
| Thrombus age
(h) | −0.05 | 0.05 | 0.39 | 0.95 | 0.86–1.06 |
Discussion
The major result of the present study was that
thrombolytic therapy with urokinase infusion into the local
fistulous vein was superior to peripheral venous infusion in terms
of thrombolytic and adverse effects. In addition, a relatively
higher blood pressure was associated with higher thrombolysis
success, while thrombus age was associated with thrombolysis
failure with local infusion of urokinase.
Thrombosis is a common complication of AVF and
arteriovenous grafts. Compared with thrombosed grafts, AVF
thrombosis has a higher risk and requires treatment within 48 h;
otherwise, thrombi may adhere to the vessel wall, making it
difficult to remove then (3,14). In the present study, only thrombosed
AVFs were included. Surgical thrombectomy and endovascular
interventions have been developed to salvage thrombosed AVF
accesses (3). It was reported that
the initial success rate of surgical thrombectomy was 84% for
thrombosed AVFs (15). Surgical
thrombectomy was reported to produce an immediate success rate of
93.8% in thrombosed AVF and a success rate of 78% in thrombosed
arteriovenous grafts (16,17). Endovascular interventions involve
pharmacological thrombolysis and mechanical thromboaspiration.
Previous studies have reported that endovascular intervention has a
success rate of >78% in thrombosed fistulas (15,18,19). An
advantage of endovascular intervention is that underlying stenosis
may be treated at the same time as the declotting treatment. In the
present study, pharmacological thrombolysis with urokinase
monotherapy achieved a success rate of >85% in acutely
thrombosed fistulas, which was comparable to the success rates of
surgical and percutaneous approaches. Of note, the cost of
urokinase monotherapy is lower compared with that of surgical and
percutaneous procedures. Therefore, urokinase infusion-based
thrombolytic therapy should be considered as an alternative option
for the salvage of acutely thrombosed fistulas. A head-to-head
study comparing the thrombolytic effects of urokinase monotherapy
and mechanical declotting procedures should be performed in the
future to provide further evidence.
In terms of adverse events, only superficial
hemorrhages were observed in the present study during and following
urokinase infusion, which were minor and acceptable. It remains
elusive whether the increased epistaxis was associated with higher
blood pressure. It was reported that 4% (4/107) of patients who
underwent surgical thrombectomy suffered a post-operative infection
and required a repeated procedure and antibiotic therapy (20). Endovascular interventions are
associated with embolization (21–23), in
particular arterial emboli, which occur in >6% of patients
receiving percutaneous declotting (24,25). To
avoid severe adverse effects, a methodical approach to patient
selection is important and patients with contraindications for each
procedure should be excluded (2,24).
Taking the efficacy and safety into account, the optimal available
declotting procedure should be selected for each given patient with
a thrombosed fistula.
The present study demonstrated that local infusion
of urokinase was superior to venous administration. The advantage
of the local infusion is that urokinase is able to concentrate in
the fistula vein and is in direct contact with the thrombus, which
may decrease systemic adverse effects and improve the success rate
of thrombolysis. A previous study used a tourniquet to restrict
urokinase within the fistula (26).
The disadvantage of the local infusion is that urokinase is infused
in a retrograde direction, in addition to being downstream from the
thrombus. Once the fistula blood flow is partially restored, the
urokinase infused into the local vein is flushed away along the
blood stream without coming into immediate contact with the
thrombus, therefore leading to a decreased thrombolytic effect and
an increased risk of hemorrhage. Urokinase infused into the
peripheral vein reaches the thrombus via the systemic circulation,
while the advantage of this is that urokinase will be transported
to the thrombus by the arterial blood flow in an antegrade
direction. In general, intra-fistula infusion of thrombolytic
agents provides a pharmacological thrombolytic therapy that avoids
the use of a catheter. An early study attempted thrombolysis using
a bolus of urokinase; however, a subsequent angioplasty was
performed to restore the blood flow of thrombosed fistula (27). Furthermore, the half-life of
urokinase is 10–20 min in the plasma; therefore, continuous IV
administration is essential to warrant thrombolytic efficacy of
urokinase. A previous study reported a 94% technical success rate
of thrombolysis by using a small dose of urokinase in combination
with balloon angioplasty in 15 patients (7).
In the present study, it was indicated that higher
blood pressure levels were associated with increased thrombolysis
success rates in the local venous thrombolytic therapy. This
phenomenon, to the best of our knowledge, has not been reported in
previous studies. The underlying mechanism remains elusive;
however, it is clear that hypotension and reduced blood flow
increase the risk for thrombosis (3,28,29). It
was also indicated that thrombus age was associated with a reduced
thrombolysis success rate. In other words, it was more difficult to
resolve older thrombi by thrombolytic therapy. Although
thrombectomy of a fistula that has been thrombosed for several days
may still be successful (10), the
prognosis is better if treatment is performed early (9).
Of note, the present study has certain limitations.
The size of the thrombi was not measured and the study did not
focus on underlying stenosis, while these two parameters may
constitute as confounding factors (20). Another limitation of the study was
the lack of long-term follow-up. The long-term efficacy and safety
of thrombolytic therapy with urokinase require further
evaluation.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
ZW and BT designed the study. ZW, RX, HW, QZ and BT
analyzed and interpreted the data. ZW and BT drafted and revised
the manuscript. All authors read and approved the final
manuscript.
Ethical approval and consent to
participate
Informed consent was obtained from all patients. The
Institutional Review Board of the First Affiliated Hospital of
Chongqing Medical University (Chongqing, China) reviewed and
approved the study protocol.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Smits JH, van der Linden J, Blankestijn PJ
and Rabelink TJ: Coagulation and haemodialysis access thrombosis.
Nephrol Dial Transplant. 15:1755–1760. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Quencer KB and Friedman T: Declotting the
thrombosed access. Tech Vasc Interv Radiol. 20:38–47. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
MacRae JM, Dipchand C, Oliver M, Moist L,
Lok C, Clark E, Hiremath S, Kappel J, Kiaii M, Luscombe R, et al:
Arteriovenous access failure, stenosis, and thrombosis. Can J
Kidney Health Dis. 3:20543581166691262016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
May RE, Himmelfarb J, Yenicesu M, Knights
S, Ikizler TA, Schulman G, Hernanz-Schulman M, Shyr Y and Hakim RM:
Predictive measures of vascular access thrombosis: A prospective
study. Kidney Int. 52:1656–1662. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Irish AB, Viecelli AK, Hawley CM, Hooi LS,
Pascoe EM, Paul-Brent PA, Badve SV, Mori TA, Cass A, Kerr PG, et
al: Effect of Fish Oil Supplementation and Aspirin Use on
arteriovenous fistula failure in patients requiring hemodialysis: A
randomized clinical trial. JAMA Intern Med. 177:184–193. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mangiarotti G, Canavese C, Thea A,
Segoloni GP, Stratta P, Salomone M and Vercellone A: Urokinase
treatment for arteriovenous fistulae declotting in dialyzed
patients. Nephron. 36:60–64. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schon D and Mishler R: Salvage of occluded
autologous arteriovenous fistulae. Am J Kidney Dis. 36:804–810.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vogel PM, Bansal V and Marshall MW:
Thrombosed hemodialysis grafts: Lyse and wait with tissue
plasminogen activator or urokinase compared to mechanical
thrombolysis with the arrow-trerotola percutaneous thrombolytic
device. J Vasc Interv Radiol. 12:1157–1165. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Quencer KB and Oklu R: Hemodialysis access
thrombosis. Cardiovasc Diagn Ther. 7 Suppl 3:S299–S308. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vascular A ccess Work Group, . Clinical
practice guidelines for vascular access. Am J Kidney Dis. 48 Suppl
1:S176–S247. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schweizer J, Kirch W, Koch R, Elix H,
Hellner G, Forkmann L and Graf A: Short- and long-term results
after thrombolytic treatment of deep venous thrombosis. J Am Coll
Cardiol. 36:1336–1343. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang X, Su F, Ding J, Zhu H, Zhu X and
Xing C: Salvage of an occluded radiocephalic fistula using
urokinase and a tourniquet for patients undergoing hemodialysis.
Int J Clin Exp Med. 11:812–817. 2018.
|
|
13
|
Gamal WM and Wagdy WM: Short-term
follow-up of the effect of preoperative radial arterial diameter on
early failure of arteriovenous fistula for hemodialysis. Ital J
Vasc Endovasc. 23:144–147. 2016.
|
|
14
|
Sadaghianloo N, Jean-Baptiste E, Gaid H,
Islam MS, Robino C, Declemy S, Dardik A and Hassen-Khodja R: Early
surgical thrombectomy improves salvage of thrombosed vascular
accesses. J Vasc Surg. 59:1377–1384 e1-2. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lipari G, Tessitore N, Poli A, Bedogna V,
Impedovo A, Lupo A and Baggio E: Outcomes of surgical revision of
stenosed and thrombosed forearm arteriovenous fistulae for
haemodialysis. Nephrol Dial Transplant. 22:2605–2612. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ponikvar R: Surgical salvage of thrombosed
native arteriovenous fistulas for hemodialysis by interventional
nephrologists. Ther Apher Dial. 13:340–344. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ponikvar R, Premru V and Kersnic B:
Surgical thrombectomy of thrombosed arteriovenous grafts by
interventional nephrologists. Ther Apher Dial. 15:306–310. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Turmel-Rodrigues L, Pengloan J, Baudin S,
Testou D, Abaza M, Dahdah G, Mouton A and Blanchard D: Treatment of
stenosis and thrombosis in haemodialysis fistulas and grafts by
interventional radiology. Nephrol Dial Transplant. 15:2029–2036.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schon D and Mishler R: Pharmacomechanical
thrombolysis of natural vein fistulas: Reduced dose of TPA and
long-term follow-up. Semin Dial. 16:272–275. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Koraen-Smith L, Krasun M, Bottai M, Hedin
U, Wahlgren CM and Gillgren P: Haemodialysis access thrombosis:
Outcomes after surgical thrombectomy versus catheter-directed
thrombolytic infusion. J Vasc Access. 19:535–541. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sadjadi SA and Sharif-Hassanabadi M: Fatal
pulmonary embolism after hemodialysis vascular access declotting.
Am J Case Rep. 15:172–175. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu S, Ahmad I, Qayyum S, Wicky S and Kalva
SP: Paradoxical embolism after declotting of hemodialysis
fistulae/grafts in patients with patent foramen ovale. Clin J Am
Soc Nephrol. 6:1333–1336. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pinard EA, Fazal S and Schussler JM:
Catastrophic paradoxical embolus after hemodialysis access
thrombectomy in a patient with a patent foramen ovale. Int Urol
Nephrol. 45:1215–1217. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Weng FL and Berns JS: Complications of
percutaneous treatment of thrombosed hemodialysis access grafts.
Semin Dial. 16:257–262. 2003.PubMed/NCBI
|
|
25
|
Kim DH, Goo DE, Yang SB, Moon C and Choi
DL: Endovascular management of immediate procedure-related
complications of failed hemodialysis access recanalization. Korean
J Radiol. 6:185–195. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kim HK, Kwon TW, Cho YP and Moon KM:
Outcomes of salvage procedures for occluded autogenous
radiocephalic arteriovenous fistula. Ther Apher Dial. 15:448–453.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zaleski GX, Funaki B, Kenney S, Lorenz JM
and Garofalo R: Angioplasty and bolus urokinase infusion for the
restoration of function in thrombosed Brescia-Cimino dialysis
fistulas. J Vasc Interv Radiol. 10:129–136. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chang TI, Paik J, Greene T, Desai M, Bech
F, Cheung AK and Chertow GM: Intradialytic hypotension and vascular
access thrombosis. J Am Soc Nephrol. 22:1526–1533. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Neyra NR, Ikizler TA, May RE, Himmelfarb
J, Schulman G, Shyr Y and Hakim RM: Change in access blood flow
over time predicts vascular access thrombosis. Kidney Int.
54:1714–1719. 1998. View Article : Google Scholar : PubMed/NCBI
|