Introduction
Bone fracture, particularly in the hip and
vertebrae, is a major cause of morbidity and mortality among
patients with diabetes mellitus (DM) (1). It is evident that diabetic patients
have a higher fracture risk when compared with non-diabetic
patients (2–4). In contrast to type 1 DM (T1DM), T2DM is
associated with an increased body mass index (BMI) and higher bone
mineral density (BMD), which is paradoxical to the increased
fracture risk (5). This indicates
that the BMD may not reflect bone fragility in patients with T2DM.
Insulin deficiency and dysfunction, obesity and hyperinsulinemia,
altered level of estrogen, leptin and adiponectin, as well as
diabetes-associated complications, particularly peripheral
neuropathy, orthostatic hypotension or reduced vision due to
retinopathy may all be associated with an impairment of bone
metabolism and increased risk of fracture (5). In addition, medications used for
diabetes management may have an important role in bone metabolism
and fracture risk.
The association between insulin use and fracture
risk in T2DM is being increasingly recognized. Insulin induces
anabolic effects on the bone, which includes the regulation of bone
cell proliferation and apoptosis, and the synthesis of collagen
(6). Most of the studies published
to date have indicated that insulin-treated diabetes is associated
with an increased risk of bone fracture (1,2,4,7–9); However, the conclusions of certain
studies appear to be inconsistent (10,11).
Kennedy et al (12) confirmed
that patients taking insulin had an increased risk of accidents,
which was most likely associated with the increased tendency of
insulin-treated patients to fall during a hypoglycemic episode. To
test the hypothesis that insulin use is associated with fracture
risk among patients with T2DM and to determine confounding factors
that may account for any association, the present meta-analysis was
performed.
Materials and methods
Search strategy
PubMed, Embase and Cochrane Library databases were
searched for studies published prior to and including April 2018
without any restrictions regarding country, publication type or
language. Combinations of the following key words were used:
[insulin (Title/Abstract)] AND [fracture (Title/Abstract)] AND
[diabetes (Title/Abstract)]. As the search terms and strategy did
not retrieve all relevant articles, the references listed in
eligible papers were also screened to supplement the results.
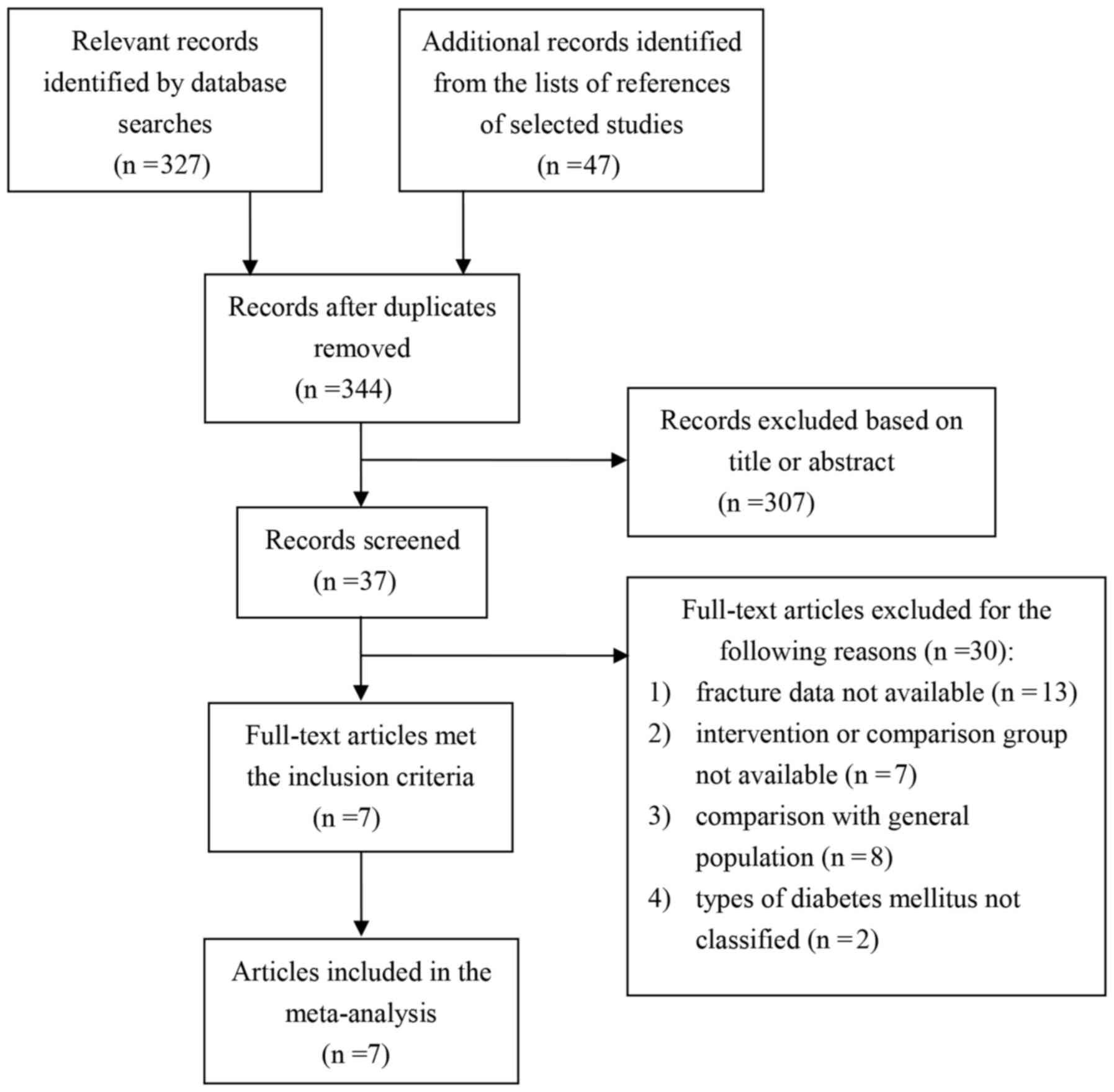
Details of the search strategy implemented in the current study are
illustrated in Fig. 1.
Inclusion and exclusion criteria
Two authors (XKM and YYL) independently performed
literature searches, preliminary screening study titles and
abstracts. The full-text articles were subsequently evaluated
according to the inclusion and exclusion criteria; a third author
(YHD) extracted valuable data from the eligible studies to be
included in the analysis. Any discrepancies were resolved through
discussion. The inclusion criteria were as follows: i) The
participants were diagnosed with T2DM; ii) each study used oral
anti-diabetic drugs as the control arm; iii) the duration of the
study was at least one year; and iv) complete fracture data for the
insulin and non-insulin groups were available. Studies were
excluded if: i) They compared their dataset to the general
population; and ii) only reported on T1DM or did not classify the
DM type.
Data synthesis and analysis
Considering the heterogeneity of the included
studies, the random-effects model was used to calculate the pooled
risk ratio (RR), with a 95% confidence interval (CI). Heterogeneity
was evaluated using I2 statistics, with values of >25, >50
and >75% representing low, moderate and high heterogeneity,
respectively. A sensitivity analysis was performed to verify the
robustness of the results by removing one study at a time. If there
was a significant change in heterogeneity after removing a study,
then this study was removed. To assess sources of heterogeneity,
subgroup analyses were performed based on sex, fracture sites,
region and study design. The results were regarded as statistically
significant if a two-sided P<0.05 was obtained. Statistical
analyses were performed using Comprehensive Meta-Analysis version 2
(www.Meta-Analysis.com) and Stata
(version 12; www.Stata.com).
Results
Study selection
A total of 344 records were selected by searching
the databases and the literature references of the articles
retrieved. After 337 exclusions, 7 articles (1,3,8,13–16) were
determined to be eligible for the present meta-analysis (Fig. 1). Overall, 138,690 patients were
enrolled in the studies selected (3,879 insulin users and 134,811
non-insulin users); among them, 5,798 cases of fracture were
reported. The publication dates for the studies ranged from 2001 to
2018 and the follow-up time ranged from 2.3 to 22.0 years. The
study population mostly included middle-aged and elderly
participants. Among the eligible studies, two studies exclusively
included women. Fracture sites included the vertebrae, hip and
other non-vertebral locations. The study locations included Asia,
Europe and North America. The study design included prospective and
retrospective studies. The characteristics of the seven trials are
provided in Table I.
 | Table I.Characteristics of the eligible
studies of fracture risk in patients with type 2 diabetes. |
Table I.
Characteristics of the eligible
studies of fracture risk in patients with type 2 diabetes.
| Author, year | Study design | Population
size | Region | Sex | Follow-up time,
years | Fracture site | (Refs.) |
|---|
| Pscherer et
al, 2016 | Retrospective
database analysis | 105,960 | Germany | Mixed | 2.3 | All three | (13) |
| Janghorbani et
al, 2006 | Prospective
study | 8,348 | North America | Women | 22.0 | Hip | (1) |
| Schwartz et
al, 2001 | Prospective
study | 657 | North America | Women | 9.4 | Hip, vertebra,
non-vertebra | (3) |
| Ahmed et al,
2006 | Population-based
cohort study | 455 | Norway | Men, women | 6.0 | Hip,
non-vertebra | (8) |
| Hung et al,
2017 | Nationwide
population-based cohort study | 7,761 | International | Mixed | 3.9 Y | Hip | (15) |
| Kanazawa et
al, 2010 | Retrospective
study | 838 | Japan | Men, women | NA | Vertebra | (14) |
| Josse et al,
2017 | Randomized
double-blinded study | 14,671 | Europe | Mixed | NA | All three | (16) |
Association between insulin intake and
risk of fracture in patients with T2DM
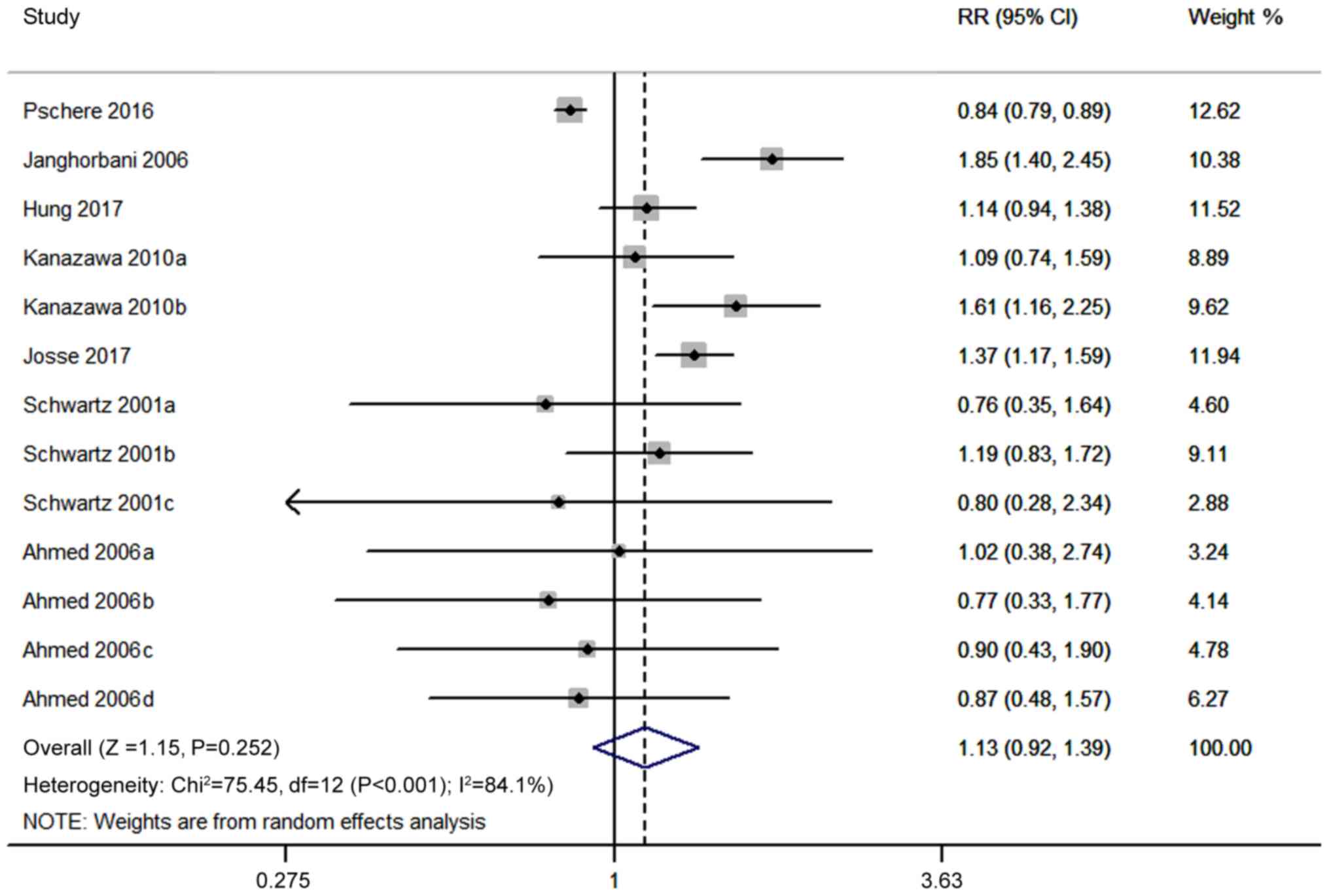
Overall, the pooled data from the seven trials
evaluating the risk of fractures associated with insulin used in
diabetic patients indicated that insulin did not significantly
increase the risk of fracture compared to oral anti-diabetic drugs
(RR=1.13, 95% CI, 0.92–1.39; P=0.252; Fig. 2). However, the I2 values indicated a
significant heterogeneity among the trials included (I2=84.1%).
Considering the obvious heterogeneity, a sensitivity analysis and
subgroup analysis were performed to explore the sources of
heterogeneity.
Sensitivity and subgroup analyses
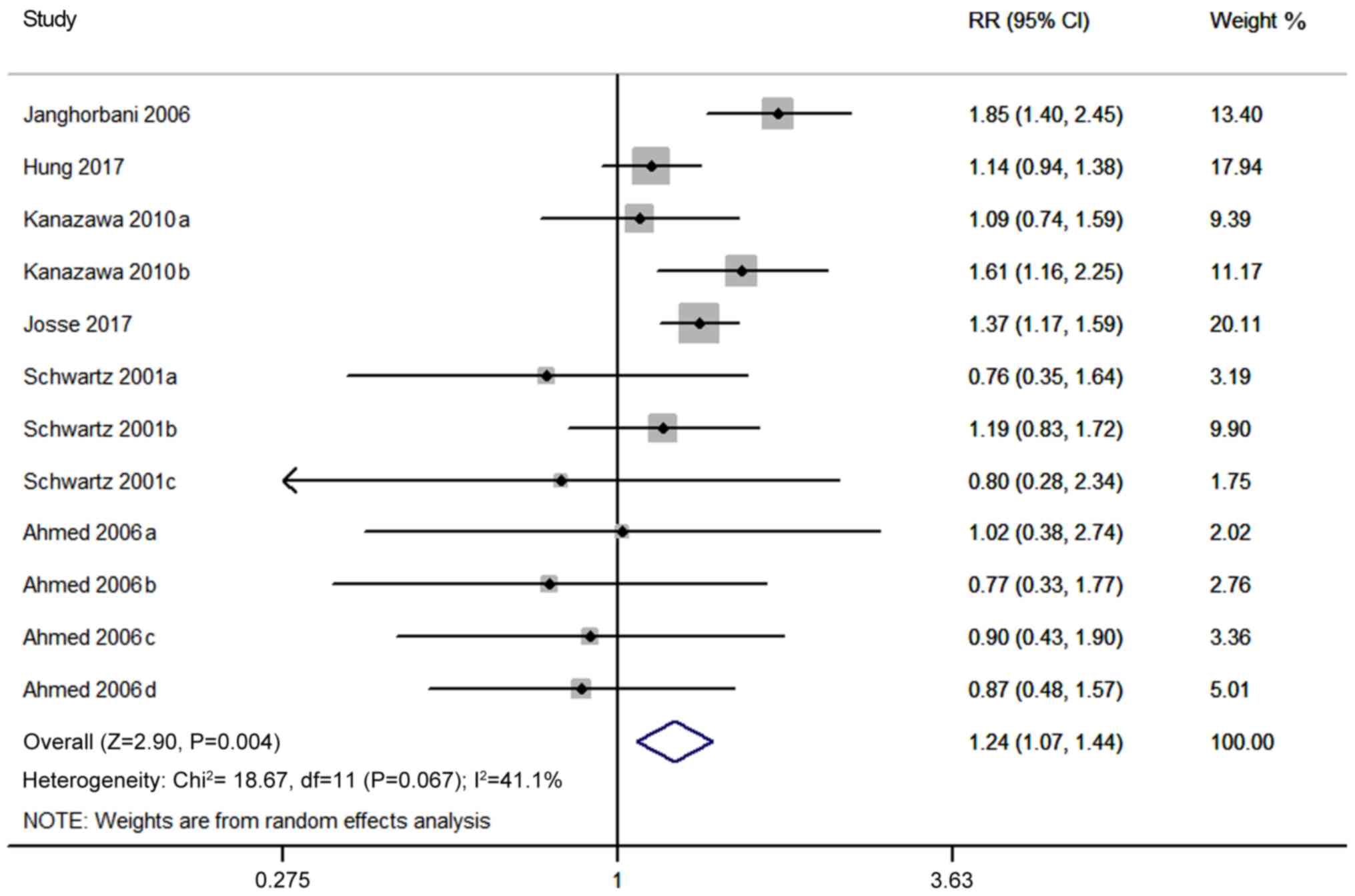
A sensitivity analysis was performed to verify the
robustness of the results by removing one study at a time. The
analysis revealed that the results changed following the exclusion
of the study conducted by Pscherer et al (13) (RR=1.24, 95% CI, 1.07–1.44; P=0.004;
Fig. 3), with the heterogeneity
markedly decreased (I2=41.1%).
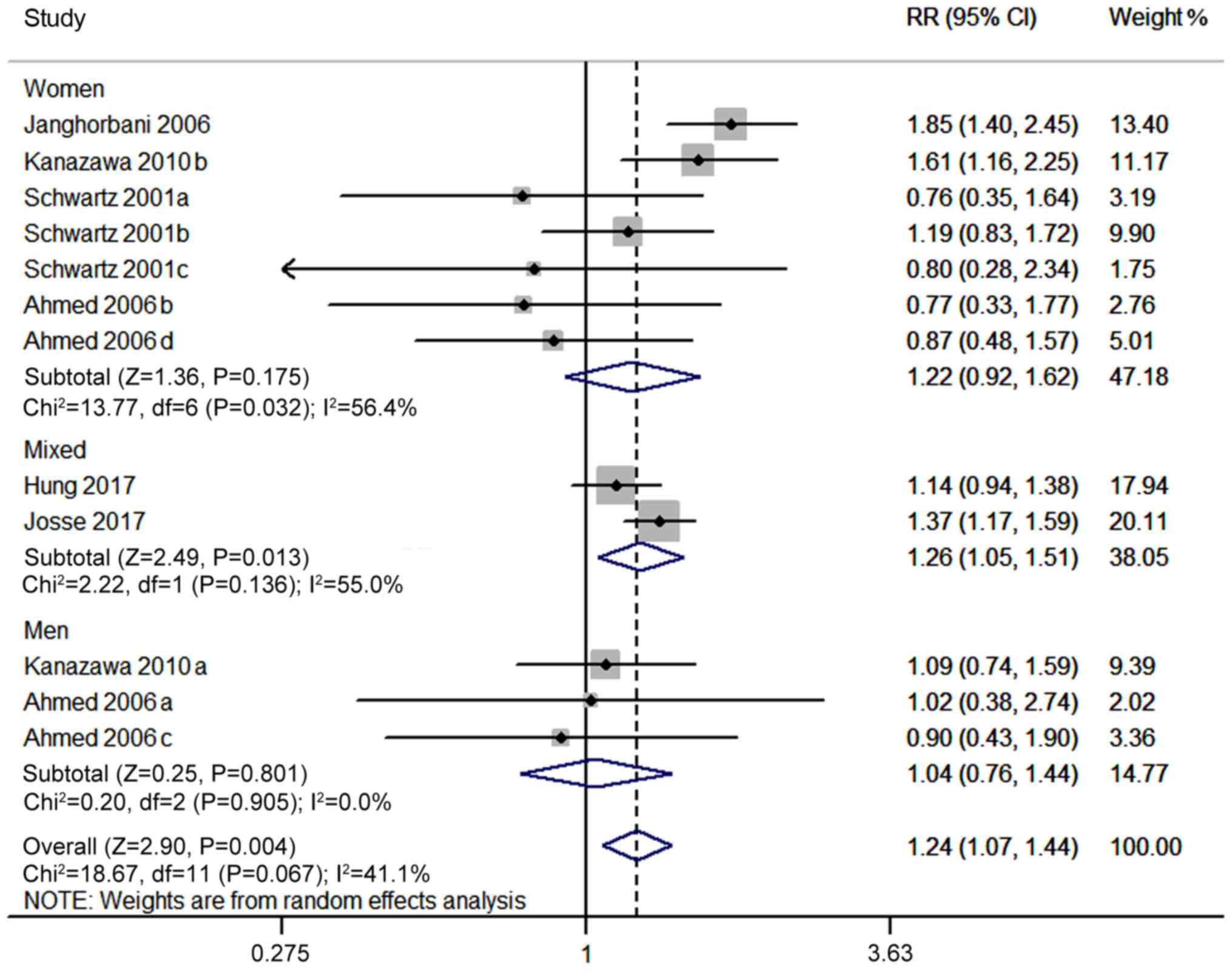
Subsequently, subgroup analyses by sex, fracture
site, study design and geographical region were performed to
identify the sources of heterogeneity. In the subgroup analysis by
sex, the corresponding RR for males was 1.04 (95% CI, 0.76–1.44,
P=0.801) and that for females was 1.22 (95% CI, 0.92–1.62,
P=0.175), while that for females and males combined was 1.26 (95%
CI, 1.05–1.51, P=0.013; Fig. 4). No
heterogeneity was identified in the subgroup of males
(I2=0.0%), whereas the female and mixed sex subgroups
demonstrated moderate heterogeneity (I2=56.4 and 55.0%,
respectively).
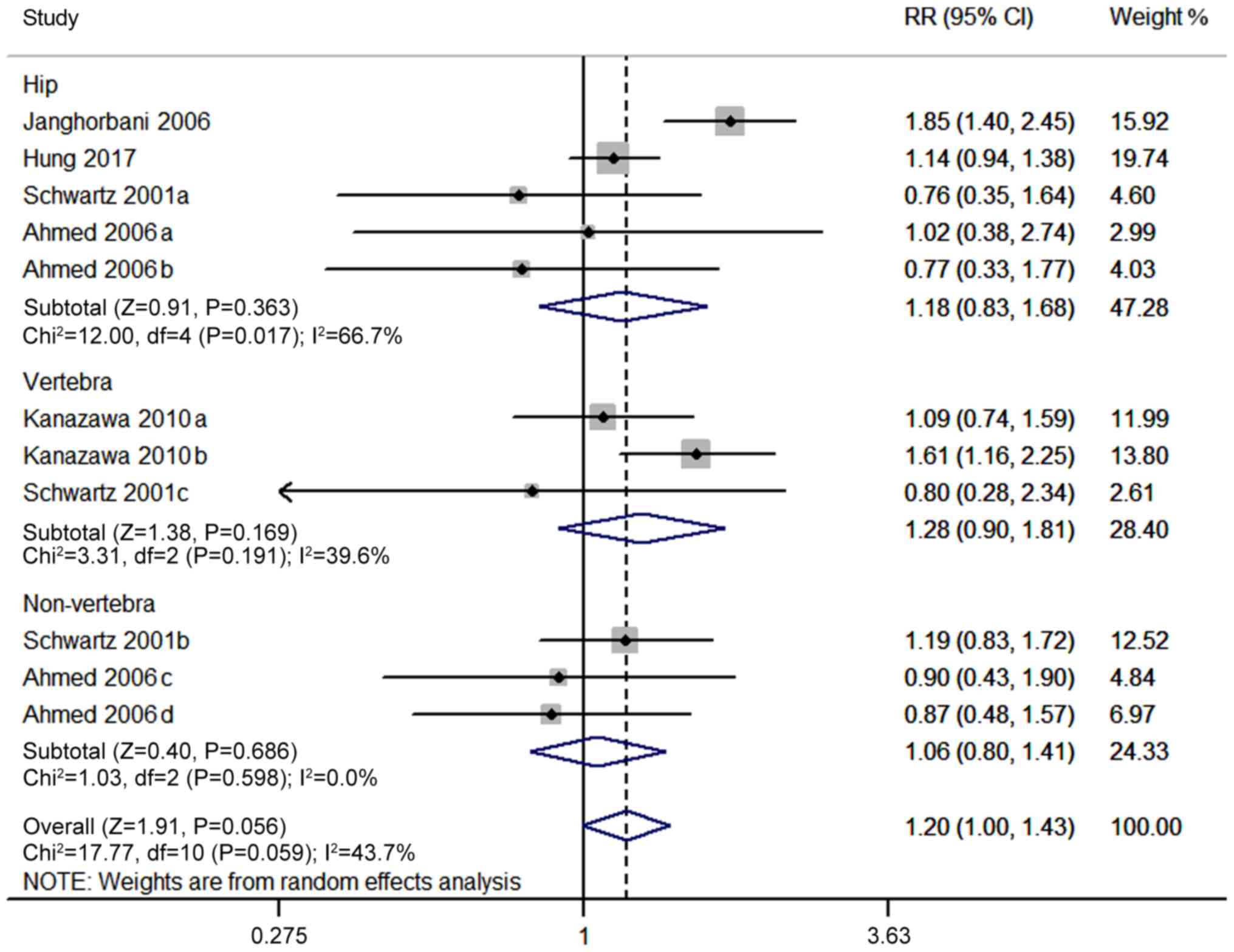
In the subgroup analysis by fracture site, the
corresponding RR for hip was 1.18 (95% CI, 0.83–1.68, P=0.363), for
non-vertebral sites (including hip) was 1.06 (95% CI, 0.80–1.41,
P=0.686) and for vertebral was 1.28 (95% CI, 0.90–1.81, P=0.169)
(Fig. 5). The heterogeneity in the
non-vertebral (including hip), vertebral and hip subgroups were
0.0, 39.6 and 66.7%, respectively.
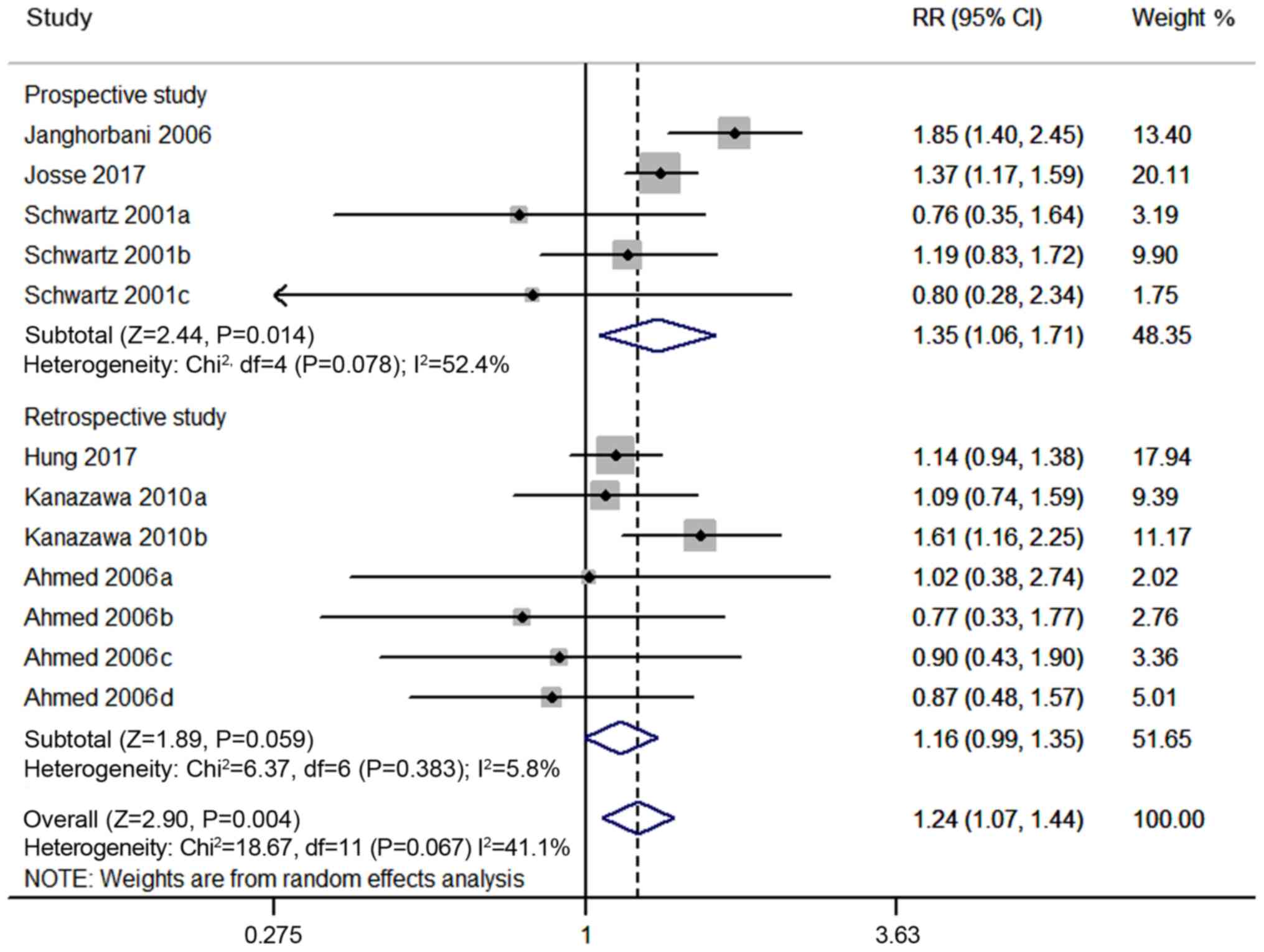
In the subgroup analysis by study design, the
corresponding RR for prospective and retrospective study subgroups
was 1.35 (95% CI, 1.06–1.71, P=0.014) and 1.16 (95% CI, 0.99–1.35,
P=0.059), respectively (Fig. 6). The
heterogeneity was low in the retrospective study subgroup
(I2=5.8%) and moderate in the prospective study subgroup
(I2=52.4%).
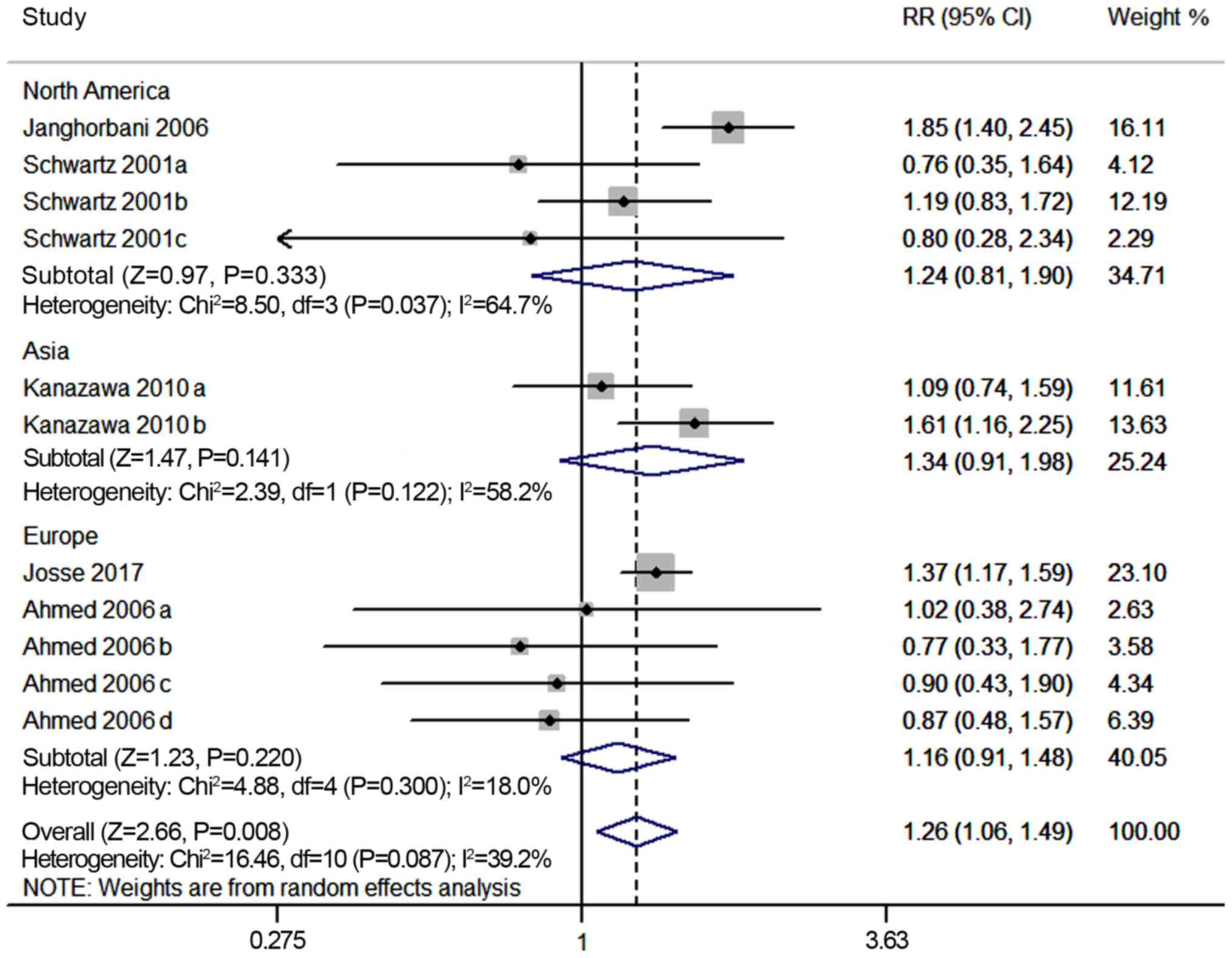
In the subgroup analysis stratified by geographical
region, the corresponding RR for North America was 1.24 (95% CI,
0.81–1.90, P=0.333), that for Asia was 1.34 (95% CI, 0.91–1.98,
P=0.141) and that for Europe was 1.16 (95% CI, 0.91–1.48, P=0.220;
Fig. 7). The heterogeneity was low
in the Europe subgroup (I2=18.0%), but moderate in the
North America and Asia subgroups (I2=64.7 and 58.2%,
respectively).
Discussion
Insulin has been used as one of several therapeutic
options for diabetic patients for numerous years. However, the
association between insulin use and fracture risk of diabetes
patients remains controversial. It is important to clarify this
issue, as bone fractures, particularly those of the hip and
vertebrae, are a major cause of disability and mortality among
elderly patients with T2DM. Therefore, a meta-analysis was
performed to determine the potential association between insulin
use and fractures in patients with T2DM.
After exclusion of the study by Pscherer et
al (13), the corrected
meta-analysis indicated that the use of insulin significantly
increased the risk of fractures among patients with T2DM compared
with oral antidiabetic drugs, which was consistent with the results
from previously published studies (1,2,7–9,15). Subgroup analyses based on sex, study
design, fracture sites and geographical region were employed to
detect subgroup differences. The subgroup analysis by sex indicated
that insulin significantly enhanced the risk of fracture from
females and males combined, while there was so significant
difference between males and females and no significant association
was identified for either sex separately. When the cohort was
stratified according to study design, the prospective study
subgroups exhibited significantly higher fracture risk associated
with insulin treatment, whereas no such association was observed in
the retrospective subgroups. In addition, this association was not
observed in the subgroups that were stratified according to
fracture site and the region.
The source of heterogeneity in a meta-analysis
should be comprehensively investigated to avoid any possible
adverse influences. Considerable heterogeneity was present in the
initial meta-analysis, and the possible source was determined by
removing one study each time and re-performing the meta-analysis.
Using this strategy, the study by Pscherer et al (13) was identified as the major source of
heterogeneity. This may be due to the mean follow-up time being too
short in the insulin and control groups when compared with the
follow-up times in the other studies. Furthermore, the mean
follow-up time was unbalanced in the insulin group (2.0 years) and
the control group (2.5 years), which may have led to bias regarding
in the incidence of fracture. This indicated that the inconsistent
follow-up periods may account for the heterogeneity observed. In
addition, the heterogeneity also changed after subgroup analysis.
Some subgroups had very low heterogeneity while some subgroups
still remained at moderate levels of heterogeneity. Therefore, it
may be postulated that sex, fracture site, study design and region
may have contributed to the heterogeneity in the present
meta-analysis.
Insulin, as an anabolic agent in the bone,
stimulates the regulation of osteoblast function, increasing the
proliferation and differentiation from mesenchymal stem cells
(17). In a study using a mouse
model, insulin receptor substrates caused osteopenia with decreased
bone formation and increased bone resorption (18). According to a clinical study,
osteopenia and osteoporosis are frequent complications in adult and
pediatric patients with T1DM (6). In
a 7-year follow-up study in young patients (age range, 20–36 years)
with T1DM, intensive insulin therapy stabilized the BMD and
decreased bone resorption markers (19). In T2DM, insulin resistance reduces
the efficiency of insulin in promoting glucose uptake and
utilization, leading to relative insulin deficiency. The body
produces compensatory amounts of insulin to maintain stable blood
glucose levels, resulting in hyperinsulinemia. Furthermore, it is
well-known that once insulin therapy is established, adequate
levels of portal insulin are obtained at the expense of peripheral
hyperinsulinemia, which may have an impact on various organs and
tissues. Certain studies have indicated that insulin resistance,
particularly hyperinsulinemia, may negatively affect bone strength
relative to load (20,21).
The mechanisms responsible for the increased
fracture risk in insulin users remain to be fully elucidated. There
are several potential mechanisms. First, most studies have reported
that endogenous insulin is an anabolic agent in bone (22–24),
whereas the effect of exogenous insulin remains ambiguous (25–31).
Barrett-Connor and Kritz-Silverstein (32) reported that exogenous insulin therapy
removes the impact of endogenous insulin as an anabolic agent on
bone. Second, diabetic insulin users are usually more likely to
have chronic hyperglycemia, which may impair bone quality (20). Third, patients requiring insulin
administration usually have a long history of diabetes and diabetic
complications, which may affect the occurrence of bone fractures.
Several studies have indicated that advanced disease increases the
risk of fracture (17,33). Fourth, insulin treatment is
associated with an increased tendency to fall during a hypoglycemic
episode. Kennedy et al (12)
observed that insulin-treated subjects were more likely to fall and
sustain bone fracture due to a fall during a hypoglycemic episode
when compared to non-insulin-treated patients. Finally, insulin
users are more likely to have diabetic retinopathy and peripheral
neuropathy, which increases the prevalence of chronic gait/balance
impairments and impaired vision (4,9).
Of note, the present study had certain limitations.
First, a certain degree of heterogeneity was present in the current
meta-analysis, even after removing one study. Bias analysis was
also not performed due to the relatively small number of studies
included in this analysis. Second, several confounding factors,
including BMD, BMI, calcium/vitamin D levels, glycosylated
hemoglobin, duration of diabetes, dose of insulin, level of glucose
and any other treatments affecting the fracture risk, were not
considered, as most of studies did not include this data and
therefore the pooled adjusted RR was not calculated. Further
studies are necessary to analyze the correlation of different
statuses of insulin and fracture risk. Third, the present study did
not include patients with T1DM, as only few studies reported on it;
certain studies have indicated that different types of DM affect
bone to varying degrees and through various mechanisms (34,35).
Fourth, the study population mostly included elderly participants
and post-menopausal women who appeared to have higher insulin
intake, and this may have biased the outcomes. A further
meta-analysis should be performed to examine age and menopausal
status of women with T1DM. The geographical distribution was
another possible limitation of the present results, with only one
out of seven studies were conducted in Asia. Therefore, further
meta-analysis is required and should include are more studies from
Asia.
Despite these limitations, the present meta-analysis
indicated that insulin treatment is associated with an increased
fracture risk among patients with T2DM, when compared to oral
anti-diabetic drugs. Subgroup analysis indicated that the
association was influenced by sex, fracture site, study design and
geographical region. These results suggest that the risk of
fracture associated with insulin use should be considered in the
process of deciding on a treatment approach. However, further
randomized, controlled studies are required to confirm these
results.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YZ and QC contributed to the conception and design
of the study, the analysis and interpretation of data and the
revision of the manuscript. YL, LZ, YD and XM participated in
literature screening and data extraction. BZ provided guidance and
generated the figures. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing
interests.
References
|
1
|
Janghorbani M, Feskanich D, Willett WC and
Hu F: Prospective study of diabetes and risk of hip fracture: The
Nurses' Health Study. Diabetes Care. 29:1573–1578. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lipscombe LL, Jamal SA, Booth GL and
Hawker GA: The risk of hip fractures in older individuals with
diabetes: A population-based study. Diabetes Care. 30:835–841.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schwartz AV, Sellmeyer DE, Ensrud KE,
Cauley JA, Tabor HK, Schreiner PJ, Jamal SA, Black DM and Cummings
SR; Study of Osteoporotic Features Research Group, : Older women
with diabetes have an increased risk of fracture: A prospective
study. J Clin Endocrinol Metab. 86:32–38. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ivers RQ, Cumming RG, Mitchell P and
Peduto AJ; Blue Mountains Eye Study, : Diabetes and risk of
fracture: The blue mountains eye study. Diabetes Care.
24:1198–1203. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Russo GT, Giandalia A, Romeo EL, Nunziata
M, Muscianisi M, Ruffo MC, Catalano A and Cucinotta D: Fracture
risk in type 2 diabetes: Current perspectives and gender
differences. Int J Endocrinol. 2016:16157352016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Thrailkill KM, Lumpkin CK Jr, Bunn RC,
Kemp SF and Fowlkes JL: Is insulin an anabolic agent in bone?
Dissecting the diabetic bone for clues. Am J Physiol Endocrinol
Metab. 289:E735–E745. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Melton LJ III, Leibson CL, Achenbach SJ,
Therneau TM and Khosla S: Fracture risk in type 2 diabetes: Update
of a population-based study. J Bone Miner Res. 23:1334–1342. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ahmed LA, Joakimsen RM, Berntsen GK,
Fønnebø V and Schirmer H: Diabetes mellitus and the risk of
non-vertebral fractures: The Tromsø study. Osteoporos Int.
17:495–500. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Napoli N, Strotmeyer ES, Ensrud KE,
Sellmeyer DE, Bauer DC, Hoffman AR, Dam TT, Barrett-Connor E,
Palermo L, Orwoll ES, et al: Fracture risk in diabetic elderly men:
The MrOS study. Diabetologia. 57:2057–2065. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vestergaard P, Rejnmark L and Mosekilde L:
Relative fracture risk in patients with diabetes mellitus, and the
impact of insulin and oral antidiabetic medication on relative
fracture risk. Diabetologia. 48:1292–1299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Monami M, Cresci B, Colombini A, Pala L,
Balzi D, Gori F, Chiasserini V, Marchionni N, Rotella CM and
Mannucci E: Bone fractures and hypoglycemic treatment in type 2
diabetic patients: A case-control study. Diabetes Care. 31:199–203.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kennedy RL, Henry J, Chapman AJ, Nayar R,
Grant P and Morris AD: Accidents in patients with insulin-treated
diabetes: Increased risk of low-impact falls but not motor vehicle
crashes-a prospective register-based study. J Trauma. 52:660–666.
2002.PubMed/NCBI
|
|
13
|
Pscherer S, Kostev K, Dippel FW and
Rathmann W: Fracture risk in patients with type 2 diabetes under
different antidiabetic treatment regimens: A retrospective database
analysis in primary care. Diabetes Metab Syndr Obes. 9:17–23.
2016.PubMed/NCBI
|
|
14
|
Kanazawa I, Yamaguchi T, Yamamoto M and
Sugimoto T: Relationship between treatments with insulin and oral
hypoglycemic agents versus the presence of vertebral fractures in
type 2 diabetes mellitus. J Bone Miner Metab. 28:554–560. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hung YC, Lin CC, Chen HJ, Chang MP, Huang
KC, Chen YH and Chen CC: Severe hypoglycemia and hip fracture in
patients with type 2 diabetes: A nationwide population-based cohort
study. Osteoporos Int. 28:2053–2060. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Josse RG, Majumdar SR, Zheng Y, Adler A,
Bethel MA, Buse JB, Green JB, Kaufman KD, Rodbard HW, Tankova T, et
al: Sitagliptin and risk of fractures in type 2 diabetes: Results
from the TECOS trial. Diabetes Obes Metab. 19:78–86. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hamann C, Kirschner S, Gunther KP and
Hofbauer LC: Bone, sweet bone-osteoporotic fractures in diabetes
mellitus. Nat Rev Endocrinol. 8:297–305. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Akune T, Ogata N, Hoshi K, Kubota N,
Terauchi Y, Tobe K, Takagi H, Azuma Y, Kadowaki T, Nakamura K and
Kawaguchi H: Insulin receptor substrate-2 maintains predominance of
anabolic function over catabolic function of osteoblasts. J Cell
Biol. 159:147–156. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Campos Pastor MM, López-Ibarra PJ,
Escobar-Jiménez F, Serrano Pardo MD and García-Cervigón AG:
Intensive insulin therapy and bone mineral density in type 1
diabetes mellitus: A prospective study. Osteoporos Int. 11:455–459.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang S, Kaw M, Harris MT, Ebraheim N,
McInerney MF, Najjar SM and Lecka-Czernik B: Decreased
osteoclastogenesis and high bone mass in mice with impaired insulin
clearance due to liver-specific inactivation to CEACAM1. Bone.
46:1138–1145. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Srikanthan P, Crandall CJ, Miller-Martinez
D, Seeman TE, Greendale GA, Binkley N and Karlamangla AS: Insulin
resistance and bone strength: Findings from the study of midlife in
the United States. J Bone Miner Res. 29:796–803. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shah CS, Shah VN, Likhar N, Mothe RK,
Kanukula R and Dang A: Association between bone mineral density and
type 1 diabetes mellitus: A meta-analysis of observational studies.
Value in Health. 18:A582015. View Article : Google Scholar
|
|
23
|
Klein GL: Insulin and bone: Recent
developments. World J Diabetes. 5:14–16. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vestergaard P: Discrepancies in bone
mineral density and fracture risk in patients with type 1 and type
2 diabetes-a meta-analysis. Osteoporos Int. 18:427–444. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wallander M, Axelsson KF, Nilsson AG,
Lundh D and Lorentzon M: Type 2 diabetes and risk of hip fractures
and non-skeletal fall injuries in the elderly: A study from the
fractures and fall injuries in the elderly cohort (FRAILCO). J Bone
Miner Res. 32:449–460. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ghodsi M, Larijani B, Keshtkar AA,
Nasli-Esfahani E, Alatab S and Mohajeri-Tehrani MR: Mechanisms
involved in altered bone metabolism in diabetes: A narrative
review. Diabetes Metab Disord. 15:522016. View Article : Google Scholar
|
|
27
|
Adami S: Bone health in diabetes:
Considerations for clinical management. Curr Med Res Opin.
25:1057–1072. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
de Waard EAC, Koster A, Melai T, van Geel
TA, Henry RMA, Schram MT, Dagnelie PC, van der Kallen CJ, Sep SJS,
Stehouwer CDA, et al: The association between glucose metabolism
status, diabetes severity and a history of fractures and recent
falls in participants of 50 years and older-the Maastricht study.
Osteoporos Int. 27:3207–3216. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Starup-Linde J, Gregersen S, Frost M and
Vestergaard P: Use of glucose-lowering drugs and risk of fracture
in patients with type 2 diabetes. Bone. 95:136–142. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Dutta MK, Pakhetra R and Garg MK:
Evaluation of bone mineral density in type 2 diabetes mellitus
patients before and after treatment. Med J Armed Forces India.
68:48–52. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yan W and Li X: Impact of diabetes and its
treatments on skeletal diseases. Front Med. 7:81–90. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Barrett-Connor E and Kritz-Silverstein D:
Does hyperinsulinemia preserve bone? Diabetes Care. 19:1388–1392.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Napoli N, Chandran M, Pierroz DD,
Abrahamsen B, Schwartz AV and Ferrari SL; IOF Bone and Diabetes
Working Group, : Mechanisms of diabetes mellitus-induced bone
fragility. Nat Rev Endocrinol. 13:208–219. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Oei L, Rivadeneira F, Zillikens MC and Oei
EH: Diabetes, diabetic complications, and fracture risk. Curr
Osteoporos Rep. 13:106–115. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Khan TS and Fraser LA: Type 1 diabetes and
osteoporosis: From molecular pathways to bone phenotype. J
Osteoporos. 2015:1741862015. View Article : Google Scholar : PubMed/NCBI
|