Introduction
Varicose veins are common; in Western countries, an
estimated 23% of adults have varicose veins and 6% have more
advanced chronic venous disease, including skin changes and healed
or active venous ulcers (1). These
have a significant impact on healthcare resources. It has been
estimated that 1–3% of total healthcare expenditures are linked to
venous disorders (2).
Open surgical treatment with ligation and stripping
of the saphenous vein, combined with excision of large
varicosities, has been the standard of care for numerous years.
Endovenous thermal radiofrequency ablation (RFA) and endovenous
laser ablation are safe and effective alternatives, with high
long-term target vein closure rates. Although the two techniques
have gained broad acceptance in numerous countries, a major
disadvantage is the requirement for tumescent anesthesia to avoid
thermal injury to surrounding structures (3).
Cyanoacrylate closure (CAC) using the VenaSeal™
Closure System (Medtronic) for varicose veins has recently been
introduced for the treatment of incompetent saphenous veins
(4–6). Although preliminary studies have been
limited to moderate-sized great saphenous veins (GSVs), larger
diameters of up to 20 mm have been included in certain studies
(7). The purpose of the present
study was to investigate the correlation of the saphenous vein
diameter or reflux time (RT) with the stump length after CAC.
Materials and methods
Data collection
A retrospective review was performed of
prospectively collected data of patients with varicose vein who
underwent CAC at Kyung Hee University Hospital at Gangdong (Seoul,
Korea) from November 2016 to February 2017. A detailed review of
the medical history and physical examination were performed at the
initial visit to the outpatient department.
Measurement of vein diameter and
reflux time
Colorized duplex scanning was performed prior to the
procedure. The maximum diameter of the GSV and the small saphenous
vein (SSV) were measured in the standing position using a tilt
table. With gray-scale imaging, the inner anechoic diameter of the
GSV was measured from the saphenofemoral junction (SFJ) to 5 cm
distal to the junction. The SSV diameter was measured in the same
manner from the saphenopopliteal junction (SPJ) to 5 cm distal to
the junction. If a cranial extension of the SSV was present, the
diameter was measured at 5 cm distal to the connection with the
deep venous system. If no definite connections with the deep venous
system were present, the diameter was measured at the site where
the SSV was in contact with the fascia. The largest diameter was
selected to analyze the correlation between diameter and stump
length. After measurement of the diameter, the RT at the SFJ, SPJ
and truncal vein in response to a Valsalva maneuver and/or manual
distal compression followed by release in standing position were
evaluated. Saphenous reflux was defined as RT of >500 msec.
Surgical procedure
Indications for CAC were clinical grade C2-C6
(8) and symptoms or cosmetic
concerns. The CAC procedure was performed under local anesthesia
with or without sedation in the operating room. An 18-G angio
catheter was inserted into the saphenous vein under ultrasound
guidance. Access sites were selected around the knee joint for the
GSV and the lower calf for the SSV. A 0.035-inch guidewire was
inserted into the deep vein through the SFJ or SPJ. This was
followed by positioning of an introducer sheath up to the junction.
Subsequently, the dilator and guidewire were removed. After
flushing the sheath, it was gently pulled back 5 cm from the
junction under ultrasound guidance. A prepared catheter loaded with
cyanoacrylate glue was introduced through the sheath. The sheath
and catheter were then connected. The tip of the catheter was
positioned 5 cm from the junction. With the catheter in place and
secured at this level, an ultrasound probe was positioned 2 cm
proximal to the tip of the catheter. Subsequently, 0.1 ml of glue
was injected by pressing the trigger. The catheter was pulled back
1 cm distally and another 0.1 ml of glue was injected. The catheter
was then pulled back 3 cm distally. The injected segment was
compressed for 3 min with the right hand. After successful closure
of this segment, the catheter tip was checked with an ultrasound
probe. Subsequently, 0.1 ml of glue was injected and the catheter
was pulled back 3 cm distally. The injected segment was again
compressed for 30 sec in the same manner as above. This process was
repeated until approaching the skin surface to 5 cm below and the
catheter was then removed. After completion of the procedure,
ultrasound examination was performed for evaluation of complete
closure of the saphenous vein and the presence of glue extension
into the common femoral vein or popliteal vein. The pain score was
evaluated immediately after the procedure by using the visual
analog scale (VAS) (7).
Post-operative management
After completion of the procedure, concomitant
phlebectomy was performed. All wounds were closed with skin
adhesive. The treated legs were dressed using a 10 cm wide,
short-stretch cohesive elastic bandage (Karl Otto Braun GmbH &
Co) if required. The elastic bandage was replaced with thigh-length
compression stockings after 24 h. This was then worn for up to 7
days. Patients were discharged at a minimum of 6 h post-operatively
after full recovery and confirmation of no procedure-associated
side effects. The patients were prescribed analgesics only when
required and returned to work when they were comfortable.
Follow-up
Patients were followed up at 1 week and at 3 months
after the CAC procedure. At all subsequent visits, the patients
were clinically examined and subjected to duplex ultrasound
scanning. At 1 week, duplex scanning was performed to confirm
saphenous vein closure and to detect any complications, including
deep vein thrombosis, endovenous glue-induced thrombosis (EGIT), or
any complications associated with the procedure. The pain score was
again measured by using the VAS.
Measurement of stump length
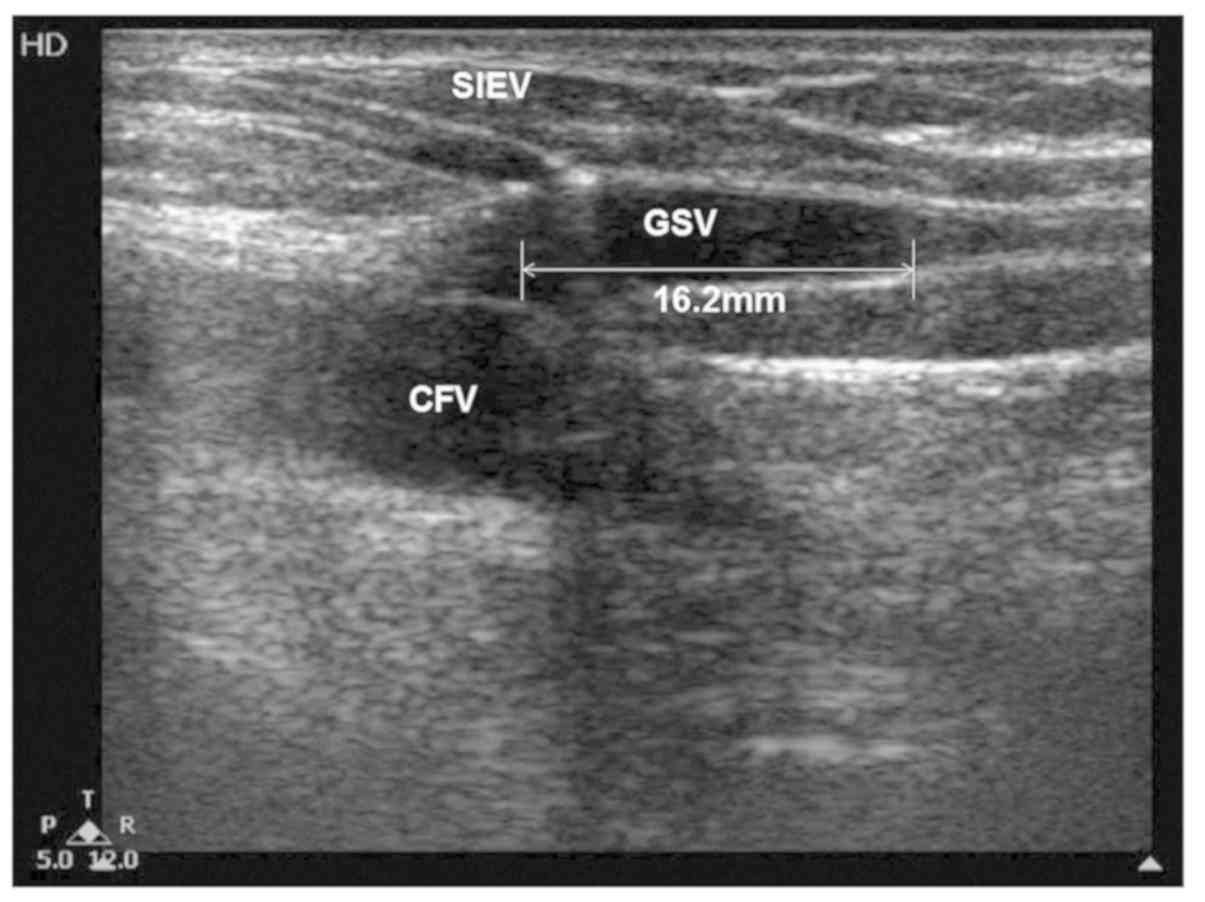
On Doppler ultrasound, the stump length was measured
from the SFJ or SPJ to the leading point of closure at the end of
the procedure and on post-operative day 7, as showcased in Fig. 1. The correlation between the
pre-operative saphenous vein diameter or RT and stump length was
assessed.
Statistical analysis
For statistical evaluation, a Student's t-test and
Pearson correlation analysis were performed using SPSS statistics
version 22.0 (IBM Corp). P<0.05 was considered to indicate
statistical significance.
Results
Demographics
During the study period, 21 consecutive patients (28
limbs) were subjected to the CAC procedure. Patient demographics
are provided in Table I. The mean
age was 56.9±12.6 years (range, 31–73 years), and the cohort
included 15 females and 6 males. The most common symptom indication
for this procedure was discomfort, followed by heaviness, night
cramping, pain and swelling. Saphenous veins with pathologic reflux
were treated simultaneously. CAC was performed on 1 truncal vein in
12 patients (57.1%), 2 truncal veins in 8 patients (38.1%) and 4
truncal veins in 1 patient (4.8%).
 | Table I.Demographics and clinicopathological
characteristics of the patients of the present study (n=21). |
Table I.
Demographics and clinicopathological
characteristics of the patients of the present study (n=21).
| Parameter | Value |
|---|
| Age (years) | 56.9±12.6
(31–73) |
| Sex |
|
| Male | 6
(28.6%) |
|
Female | 15 (71.4%) |
| Indication for
treatment |
|
|
Discomfort | 19 (90.5) |
|
Heaviness | 18 (85.7) |
| Night
cramping | 17 (81.0) |
|
Itching | 3
(14.3) |
| Pain | 2 (9.5) |
|
Swelling | 1 (4.8) |
| Limbs |
|
|
Total | 28 |
|
Right | 5 (23.8) |
| Left | 9 (42.9) |
|
Bilateral | 7 (33.3) |
| Treated truncal veins
with one session |
|
|
Total | 32 |
| 1 | 12 (57.1) |
| 2 | 8
(38.1) |
| 3 | 0 (0.0) |
| 4 | 1 (4.8) |
| Diameter of saphenous
vein (mm) | 7.0±2.2
(1.7–12.3) |
| Stump length
(mm) |
|
|
Immediately after
procedure | 26.1±10.2
(11.5–43.2) |
| At 7 days
post-surgery | 28.1±13.6
(6.4–56.2) |
Outcomes
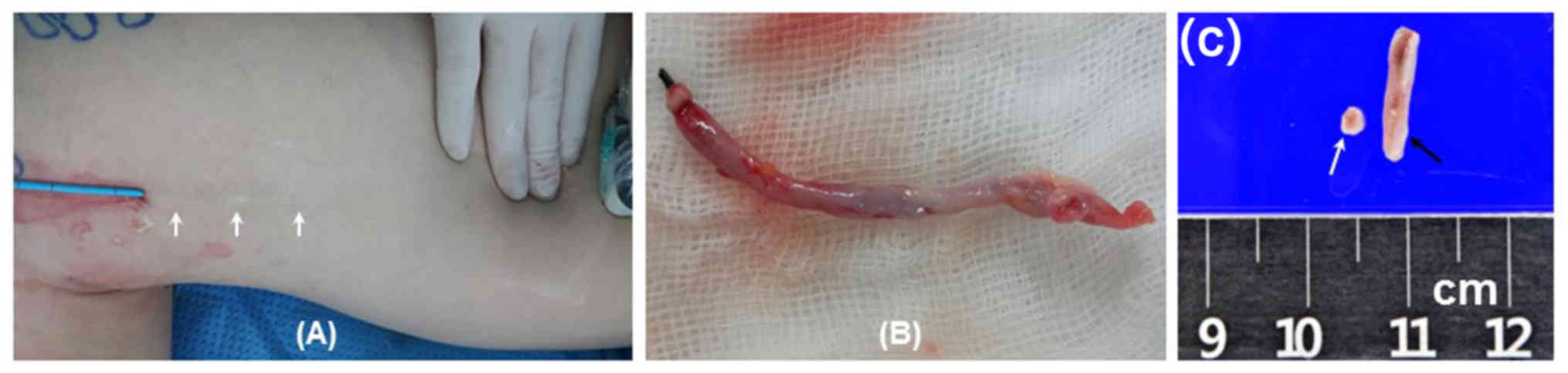
Complete closure, defined as Doppler ultrasound
examination indicating closure along the entire treated target vein
segment, with no discrete segments of patency located <5 cm away
from the junction, was achieved in all patients. In 1 patient, a
specimen of the treated saphenous vein was obtained. After
treatment, the superficially-located GSV in the knee area was
revealed. Therefore, the GSV was removed. Complete closure was
confirmed as presented in Fig. 2.
The VAS pain scores were 2.59 and 0.32 immediately after the
procedure and on post-operative day 7, respectively (P<0.0001).
There was no EGIT. Phlebitis occurred in 1 patient on day 10 after
the procedure, and was resolved with the use of analgesics and
ibuprofen.
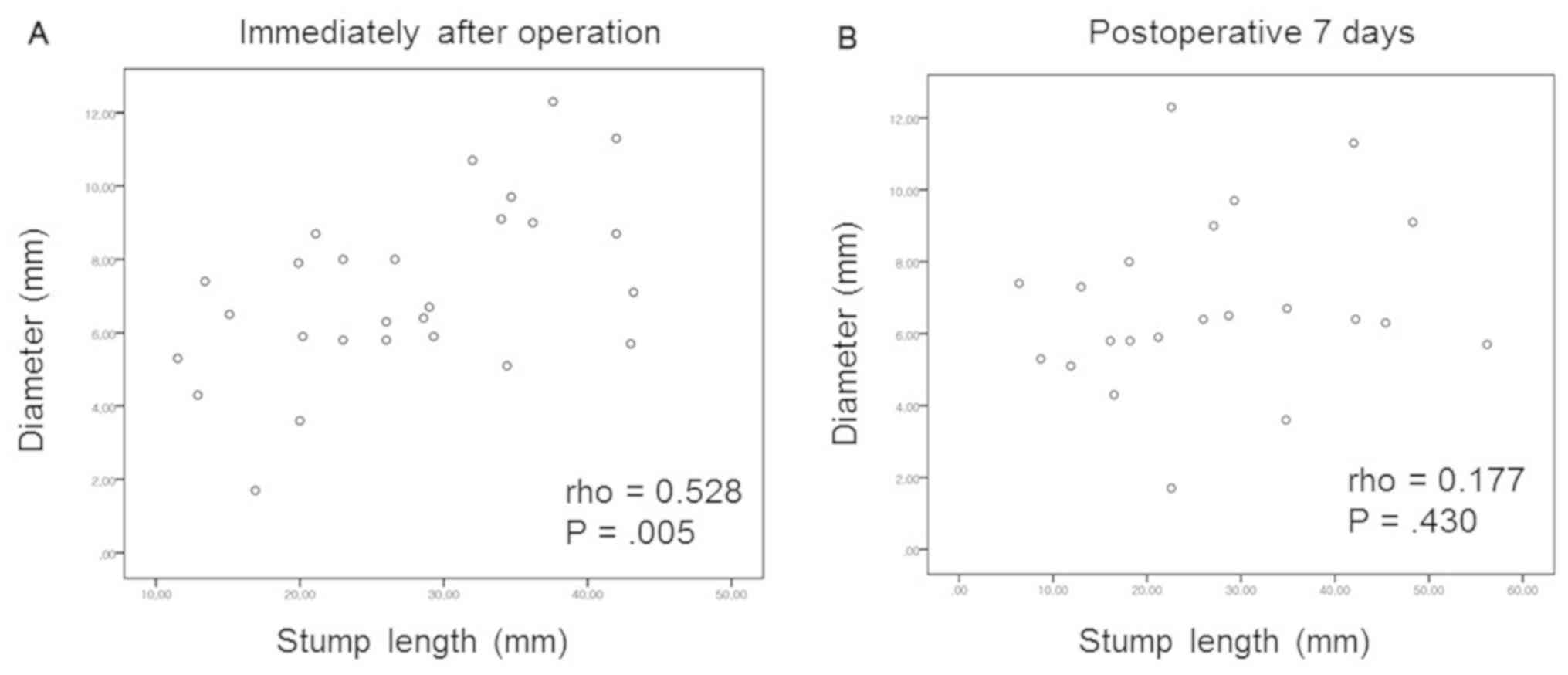
Correlation analysis
There was a positive correlation between saphenous
vein diameter and stump length immediately after the procedure
(Pearson's coefficient, 0.528; P=0.005), as presented in Fig. 3. However, there was no correlation on
post-operative day 7 (Pearson's coefficient, 0.177; P=0.430).
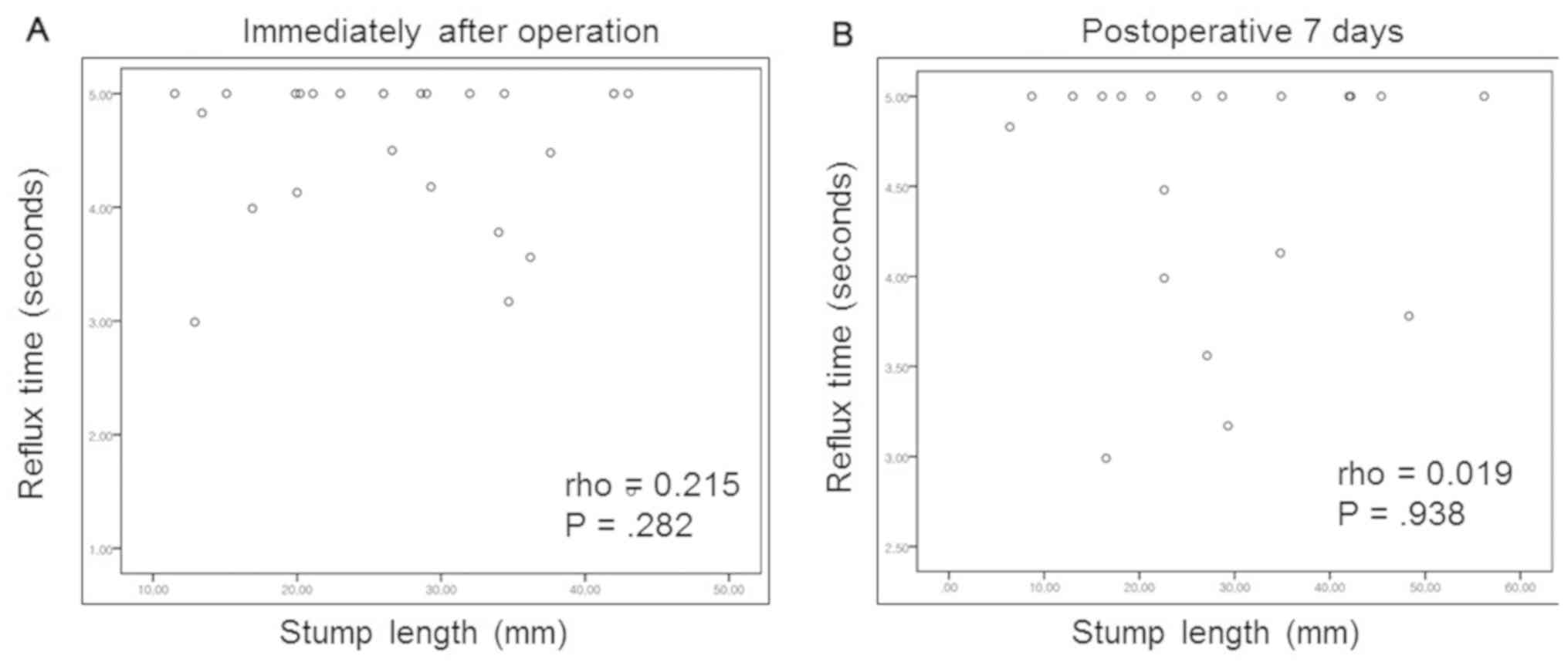
Furthermore, there was no correlation between the saphenous vein RT
and stump length immediately after the procedure (Pearson's
coefficient, 0.215; P=0.282) and on post-operative day 7 (Pearson's
coefficient, 0.019; P=0.938), as presented in Fig. 4.
Discussion
The present study demonstrates that CAC is effective
and safe for the treatment of saphenous vein insufficiency.
Complete occlusion of the treated segments was achieved in all
patients. There were no obvious side effects, except for phlebitis
in 1 patient. The results of the present study were in
correspondence with those of previous ones. A European multicenter
cohort study reported a cumulative 12-month free from
recanalization rate of 92.9% (9).
The first randomized trial comparing CAC and RFA for incompetent
GSVs determined a 3-month closure rate of 99% for the CAC group
(4).
Certain studies on the saphenous vein stump after
endovenous treatment suggest that its presence may contribute to
the formation of late inguinal varicose vein recurrence. Geier
et al (10) reported that a
long residual saphenofemoral stump was present in approximately
two-thirds of patients with symptomatic groin recurrences.
Therefore, the stump length should be kept as short as possible.
Several factors may affect the stump length after CAC, including
the initial position of the delivery catheter tip, as well as the
saphenous vein diameter, RT and peak RT. The saphenous vein
diameter and RT may be the major factor affecting the stump length.
In the present study, a positive correlation between saphenous vein
diameter and stump length was identified immediately after the
procedure (Pearson's coefficient, 0.528; P=0.005). The stump length
increased with the diameter of the saphenous vein. No correlation
was identified between the saphenous vein RT and stump length
immediately after the procedure (Pearson's coefficient, 0.215;
P=0.282) and on post-operative day 7 (Pearson's coefficient, 0.019;
P=0.938). The initial position of the catheter tip was 5 cm distal
to the junction in all patients.
In the cohort of the present study, none of the
patients developed deep vein thrombosis after the procedure. Glue
extension into a deep vein is a possible complication. EGIT is
similar to endovenous heat-induced thrombosis after RFA or laser
ablation (11–13). In the WAVES study, 1 out of 50
patients had thrombus extension that protruded 2 mm into the SFJ on
post-operative day 7 as identified on duplex evaluation (7). Chan et al (14) reported minimal extension into the
deep veins in 2 of 108 legs (1.9%). The risk factors for EGIT
remain elusive. Theoretically, the glue may extend closer to the
junction in smaller-diameter of saphenous veins. Therefore, secure
compression of the proximal segment with the ultrasound probe is
required if the patient has a smaller-diameter of saphenous
vein.
Phlebitis was reported to be the most common
complication of this procedure (4),
and this occurred somewhat more commonly than in RFA-treated
subjects (20 vs. 14%; P=0.36). Almeida et al (15) reported a lower rate of phlebitis of
15.8%. Sensitization to cyanoacrylate after dermal wound repair or
occupational contact has been described (16). Eosinophilic inflammation was reported
in a small proportion after embolization of intracranial
arteriovenous malformations (17). A
lower incidence of phlebitis was reported by Tekin et al
(18) (3.2%), but this may have been
due to a shorter follow-up period. Koramaz et al (19) reported the lowest rate of phlebitis
(2.1%). The authors suggested that the lower incidence of phlebitis
compared with that in other studies was due to continuous injection
and lower viscosity of cyanoacrylate. In the present study,
phlebitis occurred in 1 patient (4.7%) after CAC was performed for
bilateral GSV reflux. An access was made below the knee GSV segment
in both legs. In all other patients, however, venous access was
made above the knee joint. Mechanical stress due to knee joint
movement may have been a cause of phlebitis.
The primary advantage of CAC is that it does not
require the injection of perivenous tumescent solution. Thermal RFA
and laser technology necessitate the placement of perivenous
tumescent fluid to dissipate the heat. This is time-consuming to
administer and requires several painful percutaneous injections.
Another advantage is less bruising than with thermal technologies
(4).
The present study has several limitations, including
the single-center study design, the retrospective nature of the
database analysis and the relatively small number of patients.
Further and bigger-sized studies are required to confirm the
results of the present study.
In conclusion, CAC is effective for the treatment of
saphenous vein insufficiency. The stump length increased with the
diameter of the saphenous veins. However, the RT was not correlated
with the stump length after CAC.
Acknowledgements
Not applicable.
Funding
No was funding received.
Availability of data and materials
The datasets used and/or analyzed are available from
the corresponding author on reasonable request.
Authors' contributions
JK collected the data, wrote the manuscript and
performed statistical analysis. JJ conceived and designed the
current study, analyzed and interpreted the data, and takes
responsibility for the manuscript. HP acquired the data and revised
the manuscript.
Ethics approval and consent to
participate
Not required due to retrospective nature of the
study.
Patient consent for publication
The respective patient provided written informed
consent regarding the publication of their images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kaplan RM, Criqui MH, Denenberg JO, Bergan
J and Fronek A: Quality of life in patients with chronic venous
disease: San Diego population study. J Vasc Surg. 37:1047–1053.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lafuma A, Fagnani F, Peltier-Pujol F and
Rauss A: Venous disease in France: An unrecognized public health
problem. J Mal Vasc. 19:185–189. 1994.PubMed/NCBI
|
|
3
|
van den Bos R, Arends L, Kockaert M,
Neumann M and Nijsten T: Endovenous therapies of lower extremity
varicosities: A meta-analysis. J Vasc Surg. 49:230–239. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Morrison N, Gibson K, McEnroe S, Goldman
M, King T, Weiss R, Cher D and Jones A: Randomized trial comparing
cyanoacrylate embolization and radiofrequency ablation for
incompetent great saphenous veins (VeClose). J Vasc Surg.
61:985–994. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kolluri R, Gibson K, Cher D, Madsen M,
Weiss R and Morrison N: Roll-in phase analysis of clinical study of
cyanoacrylate closure for incompetent great saphenous veins. J Vasc
Surg Venous Lymphat Disor. 4:407–415. 2016. View Article : Google Scholar
|
|
6
|
Chan YC, Law Y, Cheung GC, Ting AC and
Cheng SW: Cyanoacrylate glue used to treat great saphenous reflux:
Measures of outcome. Phlebology. 32:99–106. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gibson K and Ferris B: Cyanoacrylate
closure of incompetent great, small and accessory saphenous veins
without the use of post-procedure compression: Initial outcomes of
a post-market evaluation of the VenaSeal System (the WAVES Study).
Vascular. 25:149–156. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gloviczki P, Comerota AJ, Dalsing MC,
Eklof BG, Gillespie DL, Gloviczki ML, Lohr JM, McLafferty RB,
Meissner MH, Murad MH, et al: The care of patients with varicose
veins and associated chronic venous diseases: Clinical practice
guidelines of the Society for Vascular Surgery and the American
Venous Forum. J Vasc Surg 53 (5 Suppl). 2S–48S. 2011. View Article : Google Scholar
|
|
9
|
Proebstle TM, Alm J, Dimitri S, Rasmussen
L, Whiteley M, Lawson J, Cher D and Davies A: The European
multicenter cohort study on cyanoacrylate embolization of refluxing
great saphenous veins. J Vasc Surg Venous Lymphat Disord. 3:2–7.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Geier B, Stucker M, Hummel T, Burger P,
Frings N, Hartmann M, Stenger D, Schwahn-Schreiber C, Schonath M
and Mumme A: Residual stumps associated with inguinal varicose vein
recurrences: A multicenter study. Eur J Vasc Endovasc Surg.
36:207–210. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim J, Cho S, Joh JH, Ahn HJ and Park HC:
Effect of diameter of saphenous vein on stump length after
radiofrequency ablation for varicose vein. Vasc Specialist Int.
31:125–129. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Joh JH, Kim WS, Jung IM, Park KH, Lee T
and Kang JM; Consensus Working Group, : Consensus for the treatment
of varicose vein with radiofrequency ablation. Vasc Specialist Int.
30:105–112. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Harlander-Locke M, Jimenez JC, Lawrence
PF, Derubertis BG, Rigberg DA, Gelabert HA and Farley SM:
Management of endovenous heat-induced thrombus using a
classification system and treatment algorithm following segmental
thermal ablation of the small saphenous vein. J Vasc Surg.
58:427–431. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chan YC, Law Y, Cheung GC and Cheng SW:
Predictors of recanalization for incompetent great saphenous veins
treated with cyanoacrylate glue. J Vasc Interv Radiol. 28:665–671.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Almeida JI, Javier JJ, Mackay E, Bautista
C and Proebstle TM: First human use of cyanoacrylate adhesive for
treatment of saphenous vein incompetence. J Vasc Surg Venous
Lymphat Disord. 1:174–180. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aalto-Korte K, Alanko K, Kuuliala O and
Jolanki R: Occupational methacrylate and acrylate allergy from
glues. Contact Dermatitis. 58:340–346. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Quinn JC, Mittal N, Baisre A, Cho ES,
Sharer LR, Gandhi C and Prestigiacomo CJ: Vascular inflammation
with eosinophils after the use of n-butyl cyanoacrylate liquid
embolic system. J Neurointerv Surg. 3:21–24. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tekin Aİ, Tuncer ON, Memetoğlu ME, Arslan
Ü, Öztekin A, Yağmur B, Biçer M and Özmen R: Nonthermal,
nontumescent endovenous treatment of varicose veins. Ann Vasc Surg.
36:231–235. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Koramaz I, El Kılıç H, Gökalp F, Bitargil
M, Bektaş N, Engin E, Egici MT and Bozkurt AK: Ablation of the
great saphenous vein with nontumescent n-butyl cyanoacrylate versus
endovenous laser therapy. J Vasc Surg Venous Lymphat Disord.
5:210–215. 2017. View Article : Google Scholar : PubMed/NCBI
|