Introduction
Recent changes in society and lifestyle have caused
a variety of cervical spine diseases to become more prevalent
(1). A previous study demonstrated
that neck pain accounts for 14.6% of all musculoskeletal diseases
(2). Cervical diseases are common in
individuals that have long-term immobilization of the neck or
excessive neck activity, with most patients exhibiting flexor head
injuries (3). A variety of cervical
diseases lead to a decrease in cervical spine range of motion ROM
(1,4). Cervical ROM is an indicator of cervical
pain and a variety of cervical spine diseases (2). ROM can be used as an evaluation
parameter to monitor the effect of cervical disease treatment,
including when assessing clinical results after anterior
decompression and cervical spine fusion (2,5,6). With ROM measurements, clinicians can
adjust treatment plans according to cervical vertebral mobility
changes (5). Accurate cervical ROM
measurements are important. However, due to the complex anatomy of
the cervical spine and the coupled movement of the cervical and
thoracic spine, it is currently challenging to obtain accurate
cervical ROM measurements (6,7). Several
methods are currently used to measure cervical vertebrae activity,
including eye measurements (8,9), general
protractor use (10), and cervical
ROM (CROM) device (3,11,12),
cervical laser (13), radiographic
(14), computed tomographic
(15) and tap measurements (10,16,17).
Currently, no absolute method has yet been established for
measuring cervical vertebral activity.
A CROM device consists of a plastic frame and three
independent inclinometers. During use, the plastic frame is placed
on the head of the patient to stabilize the device. Three
independent inclinometers are attached to the frame in the
sagittal, frontal and horizontal planes to indicate the position of
the head during flexion and extension, lateral bending and cervical
spine rotation (3,11). Previous studies have reported a high
validity and repeatability when using a CROM device (2,18,19).
Although this device has numerous advantages, it includes trunk
motion and therefore does not measure pure cervical ROM.
The optical motion capture system (OMCS) is commonly
used in biomechanical studies to measure human kinematics at high
accuracy (20). The aim of the
present study was to evaluate the test-retest reliability and
validity of using OMCS and CROM, by comparing neck ROMs during
flexion, extension, left lateral bending, right lateral bending,
left rotation and right rotation.
Materials and methods
Participants
From February 2018 to April 2018, a total of 20
healthy postgraduates (13 men; 7 women; mean age, 26.8±1.32 years)
from the Chinese Academy of Chinese Medical Sciences (Beijing,
China) were included in the current study. The inclusion criteria
were as follows: No cervical disease, no history of neck pain or
limitation of cervical spine mobility, no bone, muscle or nervous
system diseases and no history of neck surgery. The exclusion
criterion was a history of neck disease or neck surgery. Prior to
enrollment, each participant was screened for neck movement by a
high-grade physician to determine if cervical vertebral activity
was normal. The current study was approved by the Ethics Committee
of Wangjing Hospital of Chinese Academy of Chinese Medical Sciences
(Beijing, China) and each participant provided verbal and written
informed consent prior to enrollment in the current study.
Instruments
Cervical spine ROM was measured using a CROM and
OMCS device (V120:Trio; NaturalPoint, Inc.). Each measurement was
recorded twice for each participant, with a 1-h interval.
CROM device measurement
The CROM device (Fig.
1) was placed on the participant's head while they were seated
and looking directly forwards. The lower front edge of the device
was placed on the upper edge of the eyebrow arch, with the lower
back edge of the CROM device at the same level. The physician
assisted in keeping the body (excluding the neck) fixed in position
when movement was assessed by placing their hands on the
participants shoulders. The difference between the pointer value
and the value after movement was recorded as the motion angle of
the cervical vertebrae. When measuring axis activity, the other two
axis active pointers remained unchanged to avoid coupling motions
in multiple directions. Two physicians viewed the degree of change
exhibited by the CROM device to reduce subjective error. i) To test
for neck flexion and extension, the chin and head was moved up and
down. Each movement was stopped when the maximum angle was reached.
The difference between the values of flexion limit, extension
movement angle and the initial pointer value was used as the angle
of activity. ii) To test for left and right neck flexion,
participants flexed the neck to the left and right sides. When the
maximum angle was reached, the movement was stopped and the change
in the forehead protractor pointer was recorded. iii) To test for
left and right neck rotation, participants rotated the neck to the
left and right sides. When the maximum angle was reached, the
movement was stopped and changes in the head pointer was
recorded.
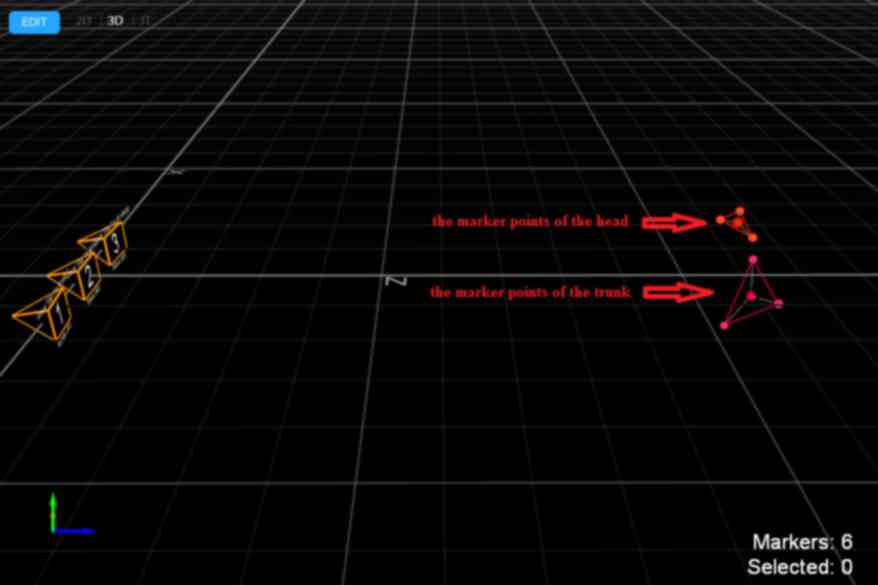
OMCS measurement
An OptiTrack-V120: Trio device (NaturalPoint, Inc.)
was used to measure OMCS (Fig. 2).
Optitrack Motive and Visual3D V5 software (NaturalPoint, Inc.) was
used to visualize results. The OptiTrack-V120: Trio device was
fixed in place with a 3-foot frame to ensure the cameras were in a
horizontal position. This was located 2 m from the participant and
at a height that was the same as that of the participants neck. All
participants wore a motion capture suit (NaturalPoint, Inc.), which
enabled the device to record measurements more accurately. Three
marker points were placed at each of four positions: The forehead,
the two bilateral temporal sites and at the top of the head. These
were used to determine the position of the head when the body was
rigid. No marker points were blocked or lost during the measurement
process. Three additional marker points were located on both sides
of the shoulder and the middle of the sternum. These were used to
determine the chest position when the body was rigid. At least six
marker points were located on the torso. The OptiTrack-V120 device
was connected to the power supply and to the computer with the
Optitrack Motive software via a USB connection line. The Optitrack
Motive software was opened.
Participants were seated close to the back of the
chair and looked straight ahead. Six movements of the cervical
vertebrae were measured, including flexion-return,
extension-return, left lateral bending-return, right lateral
bending-return, left rotation-return and right rotation-return.
During the measurements, the position of the head marker point was
adjusted as required to avoid the marker points becoming blocked.
The movement should be slow and smooth. The outer limit position of
each action should remain for 1–2 sec to facilitate the
determination of each position in the analysis process. Optitrack
Motive software tracked marker point movement as presented in
Fig. 3. Dynamic images of cervical
spine mobility measurements in all directions are shown in Videos S1–6.
Tracked movement recorded by the software was saved
as a C3D file and imported into Visual3D software. Angles were then
calculated as presented in Fig.
4.
The measurement process of this experiment is that
two instruments measure cervical range of motion at the same time,
and the physician assisted in keeping the body (excluding the neck)
in a fixed position, as presented in Fig. 5.
Statistics
Data were analyzed using SPSS version 22 software
(IBM Corp.) and presented as the mean ± standard deviation (SD).
Test-retest repeatability was evaluated using the mean of the first
and second measurements and the inter-class correlation coefficient
(ICC), which describes one-rater (intra-rater) reliability of the
two trials. The absolute reliability of the measurement was
evaluated using the SEM and the minimum detectable change (MDC).
The SEM was calculated using the following formula (21): SEM=SDx1-ICC. The 95% confidence interval
(CI) of the MDC was subsequently calculated based on the SEM value
(22). MDC was calculated using the
following formula: MDC=SEMx2xσ95, where the σ95 score was the
95% CI of 1.96. ICC values for intra-rater agreement were
interpreted as: 0–0.2 (poor), 0.2–0.4 (fair), 0.4–0.6 (moderate),
0.6–0.8 (substantial) and 0.8–1.0 (almost perfect) (23). ICC ≥0.6 was considered to represent
substantial reliability (24).
To check data validity, a linear regression analysis
was performed for the CROM measurements recorded by the CROM and
OMCS devices. Mean differences in the measured data from the two
methods were calculated and scatter plots, regression lines, the
determination coefficient (R2) and Pearson's correlation
coefficient were used to support method validity. Bland-Altman
plots were also used to display the differences between the
outcomes of the two methods (25).
Results
Repeatability study
The test-retest reliability of the cervical vertebra
activity data was analyzed using ICC, SEM and MDC (Table I). The data revealed that the CROM
and OMCS methods had a good repeatability. All ICCs were at the
substantial or almost perfect level [CROM device, ICC (1,2)
=0.768–0.948; OMCS, ICC (1,2) =0.802–0.981; Table I]. CROM and OMCS methods had the
highest reliability when the cervical spine was in extension. The
lowest reliability was obtained when the right lateral bending of
the cervical vertebrae was measured. Changes in the SEM and MDC
values of CROM and OMCS methods were small for all neck ROM
directions. SEM values range from 1.04° (right lateral bending) to
2.45° (extension) using the CROM device and from 0.98° (right
lateral bending) to 1.38° (flexion) using the OMCS method. The MDC
values were between 2.89° (right lateral bending) and 6.78°
(extension) for the CROM device and between 2.72° (right lateral
bending) and 3.81°(flexion) for the OMCS (Table I). The OMCS measured all cervical
ROMs at a higher ICC value compared with the CROM device. The SEM
and MDC ranges were also lower in the OMCS devise, indicating that
both exhibit good repeatability. However, the results demonstrated
that the repeatability of OMCS was more reliable compared with the
CROM device.
 | Table I.Test-retest reliability of the OMCS
and CROM measurements of cervical ROM. |
Table I.
Test-retest reliability of the OMCS
and CROM measurements of cervical ROM.
|
| OMCS (x±s) |
|
|
| CROM (x±s) |
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|---|
| Movement | First
measurement | Second
measurement | ICC (95% CI) | SEM | MDC | First
measurement | Second
measurement | ICC (95%CI) | SEM | MDC |
|---|
| Flexion | 63.22±7.68 | 63.4±7.16 | 0.965
(0.913–0.986) | 1.38 | 3.81 | 60.1±8.5 | 60.2±8.73 | 0.931
(0.834–0.972) | 2.22 | 6.16 |
| Extension | 62.01±9.93 | 62.28±9.87 | 0.981
(0.952–0.992) | 1.36 | 3.76 | 64.45±11.39 | 65.05±10.33 | 0.948
(0.876–0.979) | 2.45 | 6.78 |
| Left lateral
bending | 52.84±3.13 | 52.9±3.24 | 0.822
(0.601–0.926) | 1.28 | 3.54 | 53.85±4.56 | 54.95±5 | 0.805
(0.57–0.918) | 2.01 | 5.58 |
| Right lateral
bending | 48.96±2.48 | 48.38±2.16 | 0.802
(0.571–0.916) | 0.98 | 2.72 | 50±2.48 | 49.95±2.19 | 0.768
(0.498–0.902) | 1.04 | 2.89 |
| Left rotation | 81.01±3.27 | 81.39±3.13 | 0.815
(0.595–0.922) | 1.31 | 3.64 | 81.5±2.12 | 82.7±2.54 | 0.78
(0.142–0.931) | 1.06 | 2.94 |
| Right rotation | 79.18±4.02 | 79.54±3.64 | 0.927
(0.828–0.906) | 1.02 | 2.82 | 82.65±4.56 | 82.85±4.4 | 0.791
(0.543–0.912) | 1.93 | 5.36 |
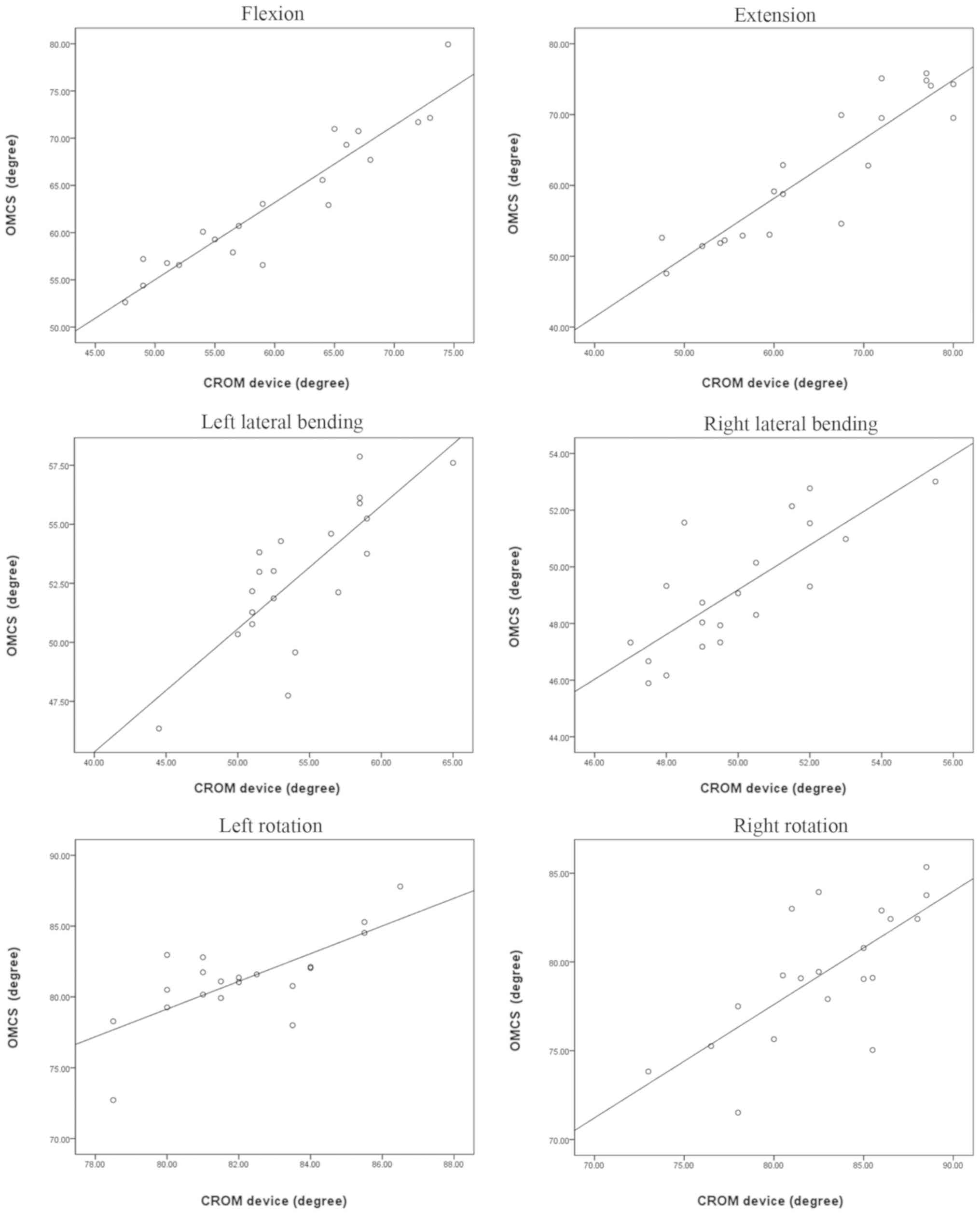
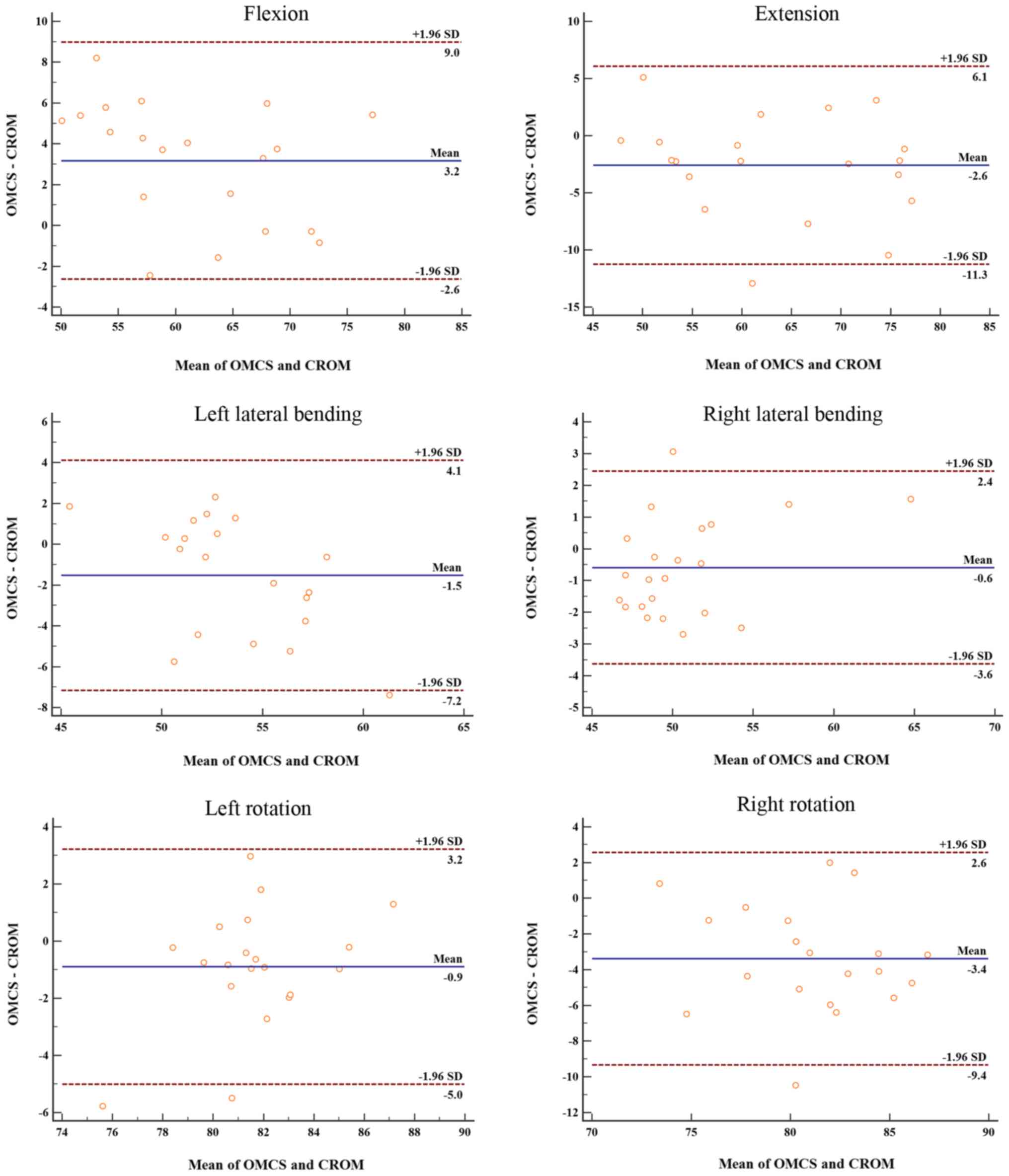
Validity study
As presented in Table
II, comparisons of the cervical ROM measurements were recorded
using the OMCS and CROM devices. The results revealed that the mean
difference varied little between them (0.81±1.47, right lateral
bending; 3.39±3.04, right rotation). Pearson's correlation
coefficient for the cervical movements was between 0.753 and 0.939
(Table II), indicating a
significant correlation. The results of the regression analysis for
all movements revealed a high R2 (0.568–0.882). Fig. 6 presents the regression lines and
scatter plots for each movement. Bland-Altman plots of all
movements reveal that differences were scattered close to zero,
with the majority of data points located within the 95% CI
(Fig. 7). All determined correlation
coefficients, demonstrate that OMCS and CROM measurements are in
good agreement, indicating that OMCS is an effective technique for
ROM measurement of the cervical vertebrae.
 | Table II.Validity of the two methods used to
measure cervical ROM. |
Table II.
Validity of the two methods used to
measure cervical ROM.
|
| Cervical ROM SD
(x±s) |
|
|
|
|---|
| Movement |
|
|
|
|
|---|
|
| OMCS | CROM | Mean difference
(x±s) | Pearson's
correlation coefficients | Determination
coefficient |
|---|
| Flexion | 63.31±7.35 | 60.15±8.46 | −3.16±2.96 | 0.94 | 0.88 |
| Extension | 62.15±9.85 | 64.75±10.73 | 2.6±4.43 | 0.91 | 0.83 |
| Left lateral
bending | 52.87±3.03 | 54.4±4.56 | 1.53±2.88 | 0.79 | 0.62 |
| Right lateral
bending | 49.17±2.21 | 49.98±2.17 | 0.81±1.47 | 0.79 | 0.63 |
| Left rotation | 81.2±3.05 | 82.1±2.26 | 0.9±2.10 | 0.77 | 0.59 |
| Right rotation | 79.36±3.77 | 82.65±4.19 | 3.39±3.04 | 0.75 | 0.57 |
Discussion
A variety of neck diseases, such as cervical
spondylosis, directly cause limited cervical vertebrae mobility
(6). The degree of cervical
vertebral ROM reduction is associated with the severity of neck
disease (26). The American College
of Physicians use cervical ROM as a standard for determining the
level of cervical vertebral damage (27). The accurate measurement of cervical
vertebral ROM is therefore important in clinical practice. A
variety of methods are used to measure cervical spine mobility. A
visual measurement is often used as it has the advantage of being
simple and repeatable, although the error range is large (9). A tape measure can be used to measure
changes in anatomical landmarks on the body surface during cervical
spine activity and indirectly reflecting the ROM of the cervical
vertebra (10). Whitcroft et
al (17) demonstrated that tape
measurements were not completely accurate when compared with
measurements obtained using a CROM device. Therefore, the authors
determined that tape measurements are inaccurate and should not be
used in clinical practice. However, more evidence-based medical
studies are required to clarify the reliability and validity of
tape measurements for cervical spine ROM. Physicians often use
either a visual survey (8) or a CROM
device (3) to determine neck ROM
clinically and in formal studies. The torso however inevitably
moves in conjunction with neck movement, so cervical ROM results
include the combined movement of the trunk and neck (28). Additionally, when measuring the
mobility of the neck in one direction, it should be considered that
neck motions involve more than one plane (29). Within observations of cervical
flexion, the cervical vertebrae exhibit lateral flexion and
rotational direction motion.
According to the results of the current study, the
OMCS obtains values of higher accuracy when measuring cervical ROM.
OMCS measures three-dimensional motions dynamically and accurately
and its technology eliminates the influence of trunk activity via
software calculations of cervical vertebral activity. Therefore,
OMCS only calculates the angle of cervical ROM. Using visual 3D
software, the three-dimensional angle change in cervical vertebral
activity can be accurately calculated, without the use of the plane
angle.
In the present study, OMCS was used to detect
cervical vertebral activity. The results were: Cervical flexion
(63.31±7.35°), extension (62.15±9.85°), left lateral bending
(52.87±3.03°), right lateral bending (49.17±2.21°), left rotation
(81.2±3.05°) and right rotation (79.36±3.77°). With the exception
of flexion, which may be due to this being the first action, these
ROM values were lower than those obtained with the CROM device. The
participant torso was close to the back of the chair to reduce
involuntary torso movements when the actions were performed.
However, the CROM device measured the coupled angle of the neck and
trunk to account for this. The current study demonstrated that OMCS
measurements of cervical vertebra had a high ICC and low SEM and
MDC values when compared with those obtained using the CROM device.
These results are consistent with the results obtained by Inokuchi
et al (28). This consistency
may be due to the increased accuracy of OMCS as it is capable of
capturing fast moving objects with a global shutter imager and 120
FPS capture speed. Using advanced image processing to maximize
resolution from three 640×480 VGA sensors, the OMCS can also track
markers down to sub-millimeter movements with repeatable accuracy
(Available from: www.optitrack.com/products/v120-trio/specs.html).
There may be subjective bias when using CROM. The CROM device was
selected for the present study due to it being previously tested,
revealing it to exhibit high validity and repeatability for the
measurement of cervical ROM (2,18,19).
CROM has also been used in other studies (13,30).
Neck muscle strength is associated with cervical vertebrae activity
(31), therefore the decrease of
muscle strength may cause the decrease of cervical ROM. Healthy
individuals were selected as participants in order decrease
variability between participants and reduce bias.
The results of the present study indicated that CROM
and OMCS techniques exhibit advantages and disadvantages. OMCS
exhibits high accuracy and repeatability when measuring cervical
vertebral ROM. However, this technology requires high quality
equipment, as well as physicians that are familiar with the
equipment and software operations. OMCS disadvantages include the
complicated operation and long data processing times. OMCS may
therefore be suitable for scientific research that requires
accurate calculations and measurements of neck ROM. In contrast,
the CROM device offers a convenient operation, low price and
immediate results. However, the measurement of error is slightly
larger, which is acceptable for measuring cervical vertebral ROM in
patients with cervical diseases, clinically (2).
The age range and sample size of the participants in
the current study is a limiting factor; the present study is a
preliminary investigation into the validity of using the OMCS and
CROM methods. A total of 20 healthy young participants were
enrolled in the current study. Individual differences in the neck
may exist. Future studies should therefore focus on the inclusion a
greater number of patients of a variety of ages with neck
disorders. Finally, due to all participants wearing the same cat
suit with fixed marker points, the slack that developed in the cat
suit over time caused the marker points to change position,
resulting in measurement errors in addition to those due to
individual fat- and lean-tissue differences.
The results of the current study confirmed the high
repeatability and validity of neck ROM measurements acquired using
OMCS. This device can therefore be recommended for measuring
cervical ROM for research purposes. Future studies that include
patient groups with cervical diseases should be conducted to
further substantiate the results of the current study.
Supplementary Material
Supporting Data
Supporting Data
Supporting Data
Supporting Data
Supporting Data
Supporting Data
Supporting Data
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
LZ contributed to the conception and design of the
current study. LL, MF, WS and GL designed and performed the
experiments. TH, XY and XW recorded and analyzed the
operation-related data. LL and MF wrote and revised the manuscript.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of Wangjing Hospital of Chinese Academy of Chinese
Medical Sciences (Beijing, China; institutional review board
reference no. WJEC-KT-2017-020-P001). Signed informed consents were
obtained from the individuals who participated in the current
study.
Patient consent for publication
Signed informed consents were obtained from the
individuals who participated in the current study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cohen SP and Hooten WM: Advances in the
diagnosis and management of neck pain. BMJ. 358:j32212017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Côté P, Cassidy JD, Carroll LJ and
Kristman V: The annual incidence and course of neck pain in the
general population: A population-based cohort study. Pain.
112:267–273. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Audette I, Dumas JP, Cote JN and De Serres
SJ: Validity and between-day reliability of the cervical range of
motion (CROM) device. J Orthop Sports Phy Ther. 40:318–323. 2010.
View Article : Google Scholar
|
|
4
|
Aranha MF, Muller CE and Gaviao MB: Pain
intensity and cervical range of motion in women with myofascial
pain treated with acupuncture and electroacupuncture: A
double-blinded, randomized clinical trial. Braz J Phy Ther.
19:34–43. 2015. View Article : Google Scholar
|
|
5
|
Silva ACO, Biasotto-Gonzalez DA, Oliveira
FHM, Andrade AO, Gomes CAFP, Lanza FC, Amorim CF and Politti F:
Effect of osteopathic visceral manipulation on pain, cervical range
of motion, and upper trapezius muscle activity in patients with
chronic nonspecific neck pain and functional dyspepsia: A
randomized, double-blind, placebo-controlled pilot study. Evid
Based Complement Alternat Med. 2018:49292712018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gao Z, Song H, Ren F, Li Y, Wang D and He
X: Reliability and validity of CODA motion analysis system for
measuring cervical range of motion in patients with cervical
spondylosis and anterior cervical fusion. Exp Ther Med.
14:5371–5378. 2017.PubMed/NCBI
|
|
7
|
Bogduk N and Mercer S: Biomechanics of the
cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon).
15:633–648. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kubas C, Chen YW, Echeverri S, McCann SL,
Denhoed MJ, Walker CJ, Kennedy CN and Reid WD: Reliability and
validity of cervical range of motion and muscle strength testing. J
Strength Cond Res. 31:1087–1096. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hirsch BP, Webb ML, Bohl DD, Fu M, Buerba
RA, Gruskay JA and Grauer JN: Improving visual estimates of
cervical spine range of motion. Am J Orthop (Belle Mead NJ).
43:E261–E265. 2014.PubMed/NCBI
|
|
10
|
Asha SE and Pryor R: Validation of a
method to assess range of motion of the cervical spine using a tape
measure. J Manipulative Physiol Ther. 36:538–545. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dunleavy K, Neil J, Tallon A and Adamo DE:
Reliability and validity of cervical position measurements in
individuals with and without chronic neck pain. J Man Manip Ther.
23:188–196. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
De-la-Puente-Ranea L, Garcia-Calvo B, La
Touche R, Fernandez-Carnero J and Gil-Martinez A: Influence of the
actions observed on cervical motion in patients with chronic neck
pain: A pilot study. J Exerc Rehabil. 12:346–354. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wibault J, Vaillant J, Vuillerme N,
Dedering A and Peolsson A: Using the cervical range of motion
(CROM) device to assess head repositioning accuracy in individuals
with cervical radiculopathy in comparison to neck- healthy
individuals. Man Ther. 18:403–409. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tousignant M, de Bellefeuille L,
O'Donoughue S and Grahovac S: Criterion validity of the cervical
range of motion (CROM) goniometer for cervical flexion and
extension. Spine (Phila Pa 1976). 25:324–330. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ito K, Yukawa Y, Machino M, Kobayakawa A
and Kato F: Range of motion determined by multidetector-row
computed tomography in patients with cervical ossification of the
posterior longitudinal ligament. Nagoya J Med Sci. 77:221–228.
2015.PubMed/NCBI
|
|
16
|
Maksymowych WP, Mallon C, Richardson R,
Conner-Spady B, Jauregui E, Chung C, Zappala L, Pile K and Russell
AS: Development and validation of a simple tape-based measurement
tool for recording cervical rotation in patients with ankylosing
spondylitis: Comparison with a goniometer-based approach. J
Rheumatol. 33:2242–2249. 2006.PubMed/NCBI
|
|
17
|
Whitcroft KL, Massouh L, Amirfeyz R and
Bannister G: Comparison of methods of measuring active cervical
range of motion. Spine (Phila Pa 1976). 35:E976–E980. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tousignant M, Smeesters C, Breton AM,
Breton E and Corriveau H: Criterion validity study of the cervical
range of motion (CROM) device for rotational range of motion on
healthy adults. J Orthop Sports Phys Ther. 36:242–248. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tousignant M, Duclos E, Lafleche S, Mayer
A, Tousignant-Laflamme Y, Brosseau L and O'Sullivan JP: Validity
study for the cervical range of motion device used for lateral
flexion in patients with neck pain. Spine (Phila Pa 1976).
27:812–817. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Aurand AM, Dufour JS and Marras WS:
Accuracy map of an optical motion capture system with 42 or 21
cameras in a large measurement volume. J Biomech. 58:237–240. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Stratford PW and Goldsmith CH: Use of the
standard error as a reliability index of interest: An applied
example using elbow flexor strength data. Phys Ther. 77:745–750.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Beaton DE, Bombardier C, Katz JN and
Wright JG: A taxonomy for responsiveness. J Clin Epidemiol.
54:1204–1217. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Landis JR and Koch GG: The measurement of
observer agreement for categorical data. Biometrics. 33:159–174.
1977. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mehta S, Bastero-Caballero RF, Sun Y, Zhu
R, Murphy DK, Hardas B and Koch G: Performance of intraclass
correlation coefficient (ICC) as a reliability index under various
distributions in scale reliability studies. Stat Med. 37:2734–2752.
2018. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bland JM and Altman DG: Agreed statistics:
Measurement method comparison. Anesthesiology. 116:182–185. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Langenfeld A, Bastiaenen C, Sieben J and
Swanenburg J: Development and validation of a self-administered
neck mobility assessment tool (S-ROM-Neck) in chronic neck pain
patients. Musculoskel Sci Pract. 37:75–79. 2018. View Article : Google Scholar
|
|
27
|
Dvir Z, Gal-Eshel N, Shamir B, Prushansky
T, Pevzner E and Peretz C: Cervical motion in patients with chronic
disorders of the cervical spine: A reproducibility study. Spine
(Phila Pa 1976). 31:E394–E399. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Inokuchi H, Tojima M, Mano H, Ishikawa Y,
Ogata N and Haga N: Neck range of motion measurements using a new
three-dimensional motion analysis system: Validity and
repeatability. Eur Spine J. 24:2807–2815. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Song H, Li HP, Gao ZY, Gao ZC and He XJ:
The research status and progress of cervical range motion
measurement. Orthopaedic Biomechanics Materials and Clinical Study.
14:63–69. 2017.(In Chinese).
|
|
30
|
Williams MA, Williamson E, Gates S and
Cooke MW: Reproducibility of the cervical range of motion (CROM)
device for individuals with sub-acute whiplash associated
disorders. Eur Spine J. 21:872–878. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lee H, Nicholson LL and Adams RD: Cervical
range of motion associations with subclinical neck pain. Spine.
29:33–40. 2004. View Article : Google Scholar : PubMed/NCBI
|