Introduction
Pityriasis rubra pilaris (PRP) was first described
in 1828 by Tarral and was named by Besnier in 1889. It is a chronic
papulosquamous disorder of unknown etiology, characterized by
reddish orange scaly plaques, islands of sparing, palmoplantar
keratoderma, and keratotic follicular papules (1). The disease can be acquired or inherited
(2). Griffiths divided PRP into 5
categories: classic adult type, atypical adult type, classic
juvenile type, circumscribed juvenile type, and atypical juvenile
type (3). More recently, an
HIV-associated type has been added to this classification (4–7). Other
reported associations include various infections, autoimmunity,
drugs, and malignancies, although their true significance remains
unclear (1). Cases of PRP associated
with malignancy are unusual. Only a few cases of PRP associated
with an underlying malignancy have been documented (8).
Case report
A 58-year-old man presented an onset of the current
disease for four months, with a prior diagnosis of exfoliative
dermatitis affecting the extremities, neck, face, scalp, palms and
soles. He reported pain, itching, and swelling of the affected
areas. The rash appeared to be worst on the hands and feet, and the
associated itch made daily activities difficult. His treatment
regimen upon admission included systemic and local corticotherapy
without significant improvement. The dermatological examination
revealed erythematous papillary follicular hyperkeratosis,
orange-red and salmon-colored scaly patches and plaques with sharp
borders, clearly delimited, sometimes covered by fine, white scales
localized on the trunk and neck, confluent in an erythematosquamous
plaque on the face and ears. Similar lesions were present on the
arms, forearms, knees and thighs. Areas of uninvolved skin,
referred to as islands of sparing, were also present (Fig. 1 and 2). The palms and soles had severe confluent
orange colored keratoderma. Several painful fissures were present
on the soles (Fig. 3). No nail, eye
or mucous membrane changes were found. There was moderate pruritus
as well. According to the patient, there was no fever, abdominal
pain, arthralgia or other relevant subjective symptoms. His medical
history was unremarkable. The clinical general examination of
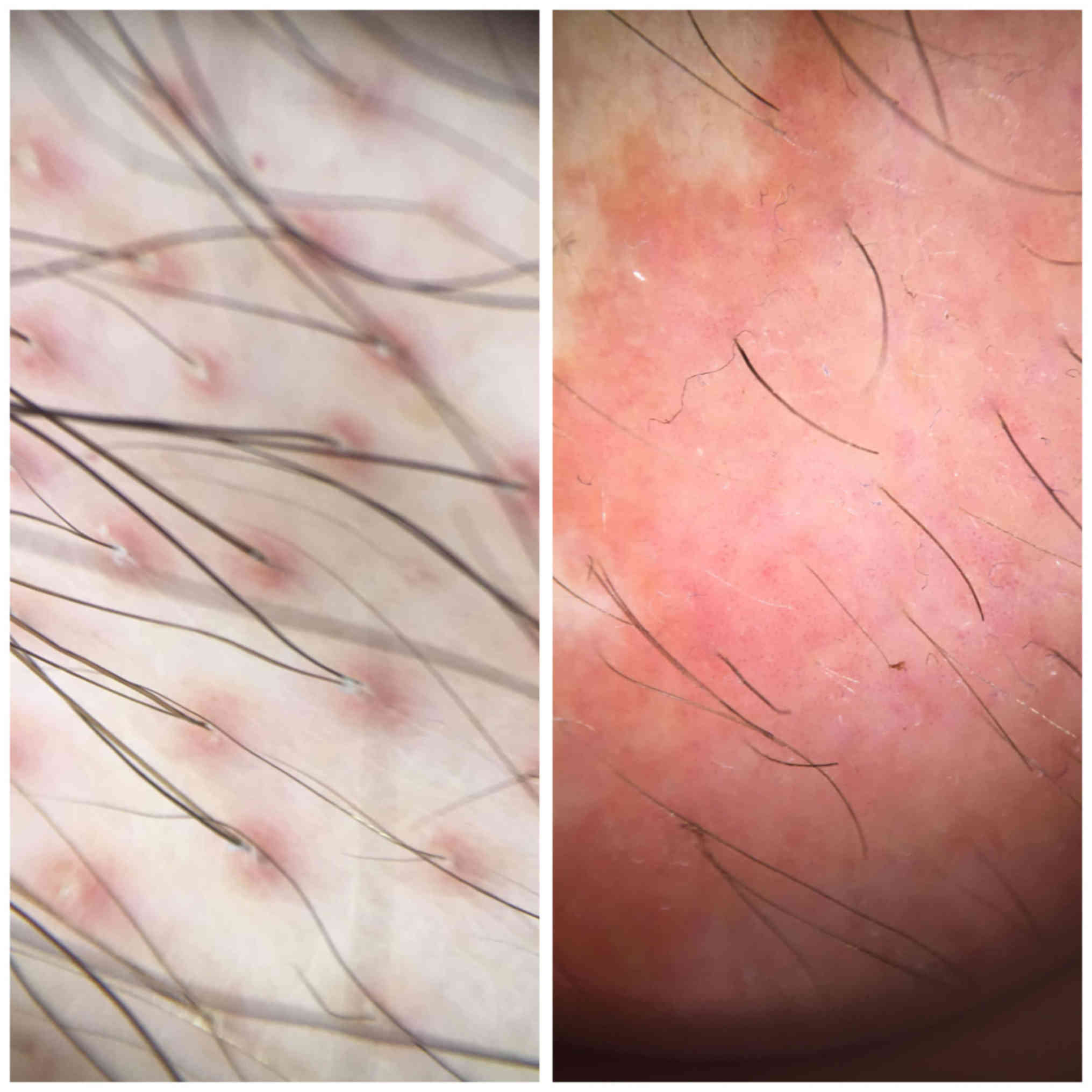
systems and organs revealed no relevant findings. The dermoscopic
evaluation revealed follicular keratotic plugs and point size
vessels with glomerular appearance (Fig.
4). Based on the typical clinical findings, our presumptive
clinical diagnosis was PRP. Other diseases, such as psoriasis,
keratodermias, acquired ichthyosis or lymphomas were considered as
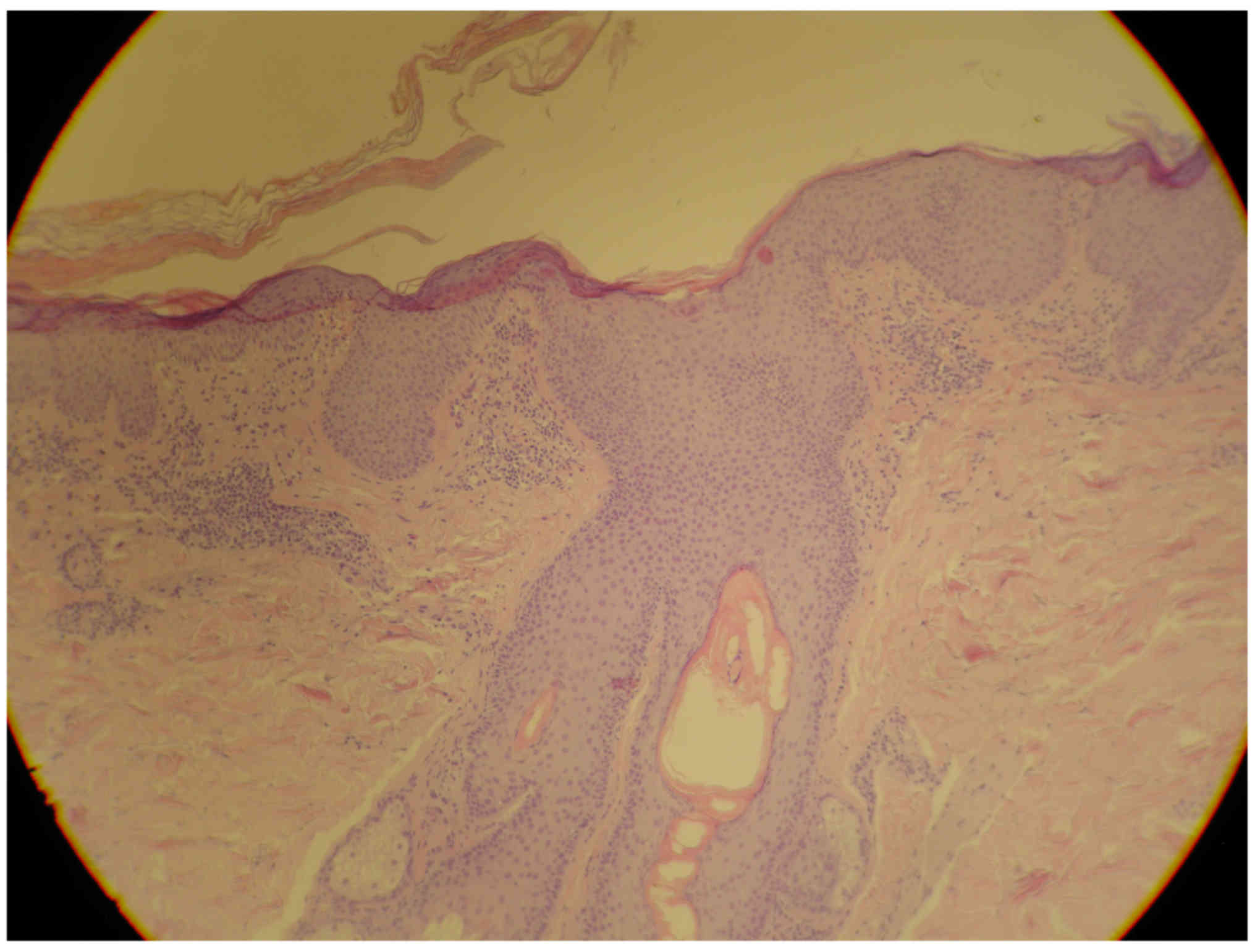
differential diagnosis. A biopsy was performed. The histopathology
revealed lamellar hyperkeratosis with alternating orthokeratosis
and parakeratosis forming a checkerboard pattern in the stratum
corneum, focal hypergranulosis, typical follicular plugging
with perifollicular parakeratosis; the presence of a superficial
dermal lymphocytic perivascular infiltration confirmed the PRP
diagnosis (Fig. 5). Routine
laboratory results, including biochemistry and hematology panel,
were within normal range, except the number of eosinophils, which
was elevated and the number of lymphocytes, which was lower, at a
normal range of white blood cell count. The authors found 21.23%
(normal: 0–4%) eosinophilia and 19.65% (normal: 25–45%)
lymphopenia, with an absolute eosinophil count of 1.69
×103/µl (normal: 0.05–0.35×103/µl). After a
thorough hematologic examination, the cause of hypereosinophilia
remained unclear. The renal function was unimpaired, and the
results of urinalysis were within normal range. No other clinical
signs or symptoms and laboratory findings possibly related to an
infection or to inflammatory diseases were noted. An imagistic
examination was performed in order to exclude underlying diseases.
The chest x-ray was negative. An abdominal ultrasound examination
revealed only a prostate hypertrophy. The prostate-specific antigen
(PSA) level was examined; the result was 4.0 ng/ml. According to
the urologic examiner, the PSA level and the ultrasound examination
were to be repeated within one month. A treatment with Acitretin
0.5 mg/kg body weight/day combined with emollients, photoprotection
and keratolytics on the palms and soles was started. One month
after initiating the treatment, the patient's state presented
improvements (Fig. 6). The repeated
complete blood cell count with differential showed a decrease of
eosinophils to a level of 7.2%. In addition, the PSA level was
measured, finding an increased level of 19.2 ng/ml. The urologic
consultation based on clinical, imagistic and microscopic features
diagnosed an early stage prostate carcinoma. The final diagnosis
was a paraneoplastic PRP in association with prostate carcinoma.
Written informed consent of the patient was obtained. The Ethics
approval was obtained from the Ethics Committee for Research of the
University of Medicine and Pharmacy (Târgu Mureş, Romania)
(approval nos. 24/2016).
Discussion
A paraneoplastic syndrome is a syndrome that
represents the consequence of a malignancy in the human body.
Paraneoplastic syndromes are typical among middle-aged to older
patients, when different types of cancers usually occur. Sometimes,
the symptoms of paraneoplastic syndromes occur before the diagnosis
of a malignancy, but they can be present at the same time as the
malignancy or they appear late in the evolution of the cancer. A
thorough review of literature was performed using international
database search. Available case reports and current review articles
were investigated to provide up-to-date information on PRP as
paraneoplastic syndrome. According to a search in the
PubMed/MEDLINE, Google Scholar and Web of Science databases, twelve
published cases on the association of PRP with malignancies were
found (2,8–18).
Regarding the documented malignancies associated
with PRP the following locations were found: cutaneous in three
cases, respiratory tract in three cases, abdominal involved in
three cases, two cases with hematological starting and one case
with renal involvement. The association of prostate carcinoma with
PRP, as in the presented case, has not previously been reported
(2,8–18). In
cutaneous tumors, there are reported cases of spinocellular,
basocellular and Merkel cell carcinomas. Regarding the respiratory
tract, in two of the cases it was lung carcinoma and in one case -
a laryngeal tumor. In abdominal locations, there were one case of
cholangiocarcinoma, one hepatic tumor and one case of liver
metastasis with unknown location of the primary tumor. The other
remaining cases presented an association of leukemia, Sézary
syndrome, and renal carcinoma with PRP. In only two cases (basal
cell and spinocellular carcinoma) PRP appeared during the evolution
of the cancers. For the rest, PRP was the first clinical sign of a
malignancy. The diagnosis of the primary tumors was possible due to
the routine clinical, laboratory and imagistic examinations in all
of the cases.
The diagnosis of PRP was made based on the clinical
and histological findings, as in the present case. The performed
dermoscopic examination in this case revealed follicular keratotic
plugs and point size vessels with glomerular appearance usually
present in PRP (19). No dermoscopic
examination was performed by the authors. The increased number of
eosinophils found in this case, which decreased under treatment,
was not found in the other cases. It is mentioned in literature
that eosinophilia can be present in PRP (20). The most likely explanation for the
eosinophilia was a reactive process secondary to the extreme
inflammatory state. In two cases, PRP had a recalcitrant evolution
to retinoid systemic treatment (8,9). In the
rest of the cases, the disease reacted to treatment, including in
our case. The treatment in all cases was retinoid therapy, except
for one case in which locally used steroids were efficient
(12). In all cases, the different
curative treatments of the malignancies led to healing or marked
improvement of the PRP, concluding that PRP can be considered a
paraneoplastic syndrome (21–24).
PRP is a rare disease; the incidence may vary from 1
in 5,000 in Britain to 1 in 50,000 in India, affecting both sexes
equally (3). Most of the cases are
acquired, like the present case. The association with malignancies
is unusual. This case represented a rare coexistence of PRP with
malignancy, particularly with prostate carcinoma, and indicates
that PRP can occur as paraneoplastic dermatosis, heralding a
malignancy. This is the first case to present PRP associated with
prostate carcinoma. The limited number of cases found in literature
precludes any meaningful interpretation of data about PRP as
paraneoplastic syndrome. Nevertheless, the authors suggest that PRP
can be considered a paraneoplastic syndrome; therefore, tumor
screening is mandatory in cases presenting this disease.
Acknowledgements
Professional editing, linguistic and technical
assistance performed by Individual Service Provider Irina Radu,
certified translator in Medicine and Pharmacy.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
GLF was responsible for the clinical management of
the patient, the data evaluation and analysis, and the writing of
the manuscript. DB contributed to the microscopic examination, the
analysis of the data, the corrections and the preparation of the
manuscript. CC contributed to the database research and the writing
of the manuscript. LF performed the biopsy and contributed to the
data analysis, the corrections, the preparation of the manuscript
and the database research. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The Ethics approval was obtained from the Ethics
Committee for Research of the University of Medicine and Pharmacy
(Târgu Mureş, Romania) (approval nos. 24/2016). Written informed
consent of the patient was obtained.
Consent for publication
Written informed consent of the patient has been
obtained.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
GLF: Associate Professor of Dermatology, Dermatology
Department, University of Medicine and Pharmacy, Dermatology
Clinic, Târgu Mureş, Romania.
References
|
1
|
Wang D, Chong VC, Chong WS and Oon HH: A
review on pityriasis rubra pilaris. Am J Clin Dermatol. 19:377–390.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Batinac T, Kujundzić M, Peternel S,
Cabrijan L, Troselj-Vukić B and Petranović D: Pityriasis rubra
pilaris in association with laryngeal carcinoma. Clin Exp Dermatol.
34:e917–e919. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Griffiths WA: Pityriasis rubra pilaris.
Clin Exp Dermatol. 5:105–112. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Auffret N, Quint L, Domart P, Dubertret L,
Lecam JY and Binet O: Pityriasis rubra pilaris in a patient with
human immunodeficiency virus infection. J Am Acad Dermatol.
27:260–261. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Blauvelt A, Nahass GT, Pardo RJ and Kerdel
FA: Pityriasis rubra pilaris and HIV infection. J Am Acad Dermatol.
24:703–705. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Martin AG, Weaver CC, Cockerell CJ and
Berger TG: Pityriasis rubra pilaris in the setting of HIV
infection: Clinical behaviour and association with explosive cystic
acne. Br J Dermatol. 126:617–620. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miralles ES, Núñez M, De Las Heras ME,
Pérez B, Moreno R and Ledo A: Pityriasis rubra pilaris and human
immunodeficiency virus infection. Br J Dermatol. 133:990–993. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bar-Ilan E, Gat A, Sprecher E and Zeeli T:
Paraneoplastic pityriasis rubra pilaris: Case report and literature
review. Clin Exp Dermatol. 42:54–57. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Remedios IM, Jensen JD, Beckum K, McKay K
and Kissel R: Paraneoplastic pityriasis rubra pilaris as the
presenting manifestation of metastatic squamous cell carcinoma. J
Drugs Dermatol. 13:610–612. 2014.PubMed/NCBI
|
|
10
|
Kurzydlo AM and Gillespie R:
Paraneoplastic pityriasis rubra pilaris in association with
bronchogenic carcinoma. Australas J Dermatol. 45:130–132. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Garretson CB, Machan ML, Krejci-Manwaring
J, Aires D and Tonkovic-Capin V: Letter: Adenocarcinoma of the lung
associated with pityriasis rubra pilaris. Dermatol Online J.
17:14–17. 2011.PubMed/NCBI
|
|
12
|
Sánchez-Regaña M, López-Gil F, Salleras M
and Umbert P: Pityriasis rubra pilaris as the initial manifestation
of internal neoplasia. Clin Exp Dermatol. 20:436–438. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Batchelor RJ, Yung A, Merchant W and
Goodfield MJ: Pityriasis rubra pilaris as the initial presentation
of renal cell carcinoma? Clin Exp Dermatol. 30:442–443. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sharma S, Weiss GR and Paulger B:
Pityriasis rubra pilaris as an initial presentation of
hepatocellular carcinoma. Dermatology. 194:166–167. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Reinhardt LA and Rosen T: Pityriasis rubra
pilaris as the initial manifestation of leukemia. Cutis.
31:100–102. 1983.PubMed/NCBI
|
|
16
|
Roger J, Burg G, Miller K and Lanz U:
Pityriasis rubra pilaris-artiges Vorstadium eines Sezary-Syndroms.
Syndroms (Pityriasis rubra pilaris the precursor of a Sezaryís
syndrome). Z Hautkr. 66:1046–1050. 1991.(In German).
|
|
17
|
Tannenbaum CB, Billick RC and Srolovitz H:
Multiple cutaneous malignancies in a patient with pityriasis rubra
pilaris and focal acantholytic dyskeratosis. J Am Acad Dermatol.
35:781–782. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Huynh NT, Hunt MJ, Cachia AR and Veness
MJ: Merkel cell carcinoma and multiple cutaneous squamous cell
carcinomas in a patient with pityriasis rubra pilaris. Australas J
Dermatol. 43:48–51. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Abdel-Azim NE, Ismail SA and Fathy E:
Differentiation of pityriasis rubra pilaris from plaque psoriasis
by dermoscopy. Arch Dermatol Res. 309:311–314. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Price L and Lesesky E: Pityriasis rubra
pilaris and severe hypereosinophilia. Cutis. 100:E6–E7.
2017.PubMed/NCBI
|
|
21
|
Fekete GL, Cotoi OS and Fekete JE:
Multiple nodular cutaneous metastases as the first clinical sign of
signet ring cell gastric carcinoma: Case report. Acta
Dermatovenerol Croat. 20:34–37. 2012.PubMed/NCBI
|
|
22
|
Neagu M, Caruntu C, Constantin C, Boda D,
Zurac S, Spandidos DA and Tsatsakis AM: Chemically induced skin
carcinogenesis: Updates in experimental models (Review). Oncol Rep.
35:2516–2528. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Boda D: Cellomics as integrative omics for
cancer. Curr Proteomics. 10:237–245. 2013. View Article : Google Scholar
|
|
24
|
Neagu M, Constantin C, Tanase C and Boda
D: Patented biomarker panels in early detection of cancer. Recent
Pat Biomark. 1:10–24. 2011. View Article : Google Scholar
|