Introduction
The invention of a wireless capsule endoscope by
Israeli scientists in 2000 not only ended the long history of
visual inaccessibility of the small intestine, but also brought
about a new era of painless minimally invasive gastrointestinal
endoscopy. Shortly thereafter, capsule esophagoscopy and capsule
colonoscopy were developed (1–4).
First-generation capsules are propelled by gastrointestinal
peristaltic movement, which makes them ill-suited for use in
thorough examination of the wider area of the stomach.
In 2010, the same Israeli scientists reported the
first use of a magnet-controlled capsule endoscope in the stomach
of a young male volunteer. Under synchronous observation of
traditional upper gastrointestinal endoscopy (UGIE), the capsule
was demonstrated to move precisely and rapidly to a designated
location in response to the movement of a handheld external magnet
around the torso of the volunteer (5). Subsequent studies attempting to
replicate the success of that first trial have been unable to
recreate the flexibility of manipulation described, regardless of
whether the magnetic capsule was manipulated with a handheld magnet
or a robot-assisted magnetic manipulation system. Furthermore,
operators have had difficulty achieving complete exploration of the
stomach (i.e., without any blind areas), especially of the gastric
fundus and cardia (6–11). In China, a magnet-controlled capsule
specialized for the stomach has been approved for clinical use, but
has also failed to solve the aforementioned problems (12,13).
Analysis of the differences between the first trial
and subsequent reports revealed methodological differences, which
may be responsible for the inconsistent findings. The first trial
was conducted with the volunteer lying on his left side, whereas
the majority of the subsequent studies were conducted with subjects
lying in a supine position. Additionally, in the first trial,
gastric distention was maintained by continuous gas injection in
association with concomitant UGIE, whereas in subsequent studies,
gastric distention was achieved by pre-examination drinking of
water and gas producing agents. Thus, the different findings
between the first and subsequent studies may be due to difference
in the subjects' body positioning, the extent of gastric
distention, and potentially the distance between the internal
capsule and the external magnet.
Rahman et al (8) used computed tomography (CT) modeling of
the abdomen to determine the optimal placement of a magnetic
capsule endoscope in the stomach, with respect to enabling complete
mucosal visualization, and to determine the optimal placement of
the handheld magnet for traversing the pylorus. Maximal
visualization (85%) was achieved with a combination of two stations
at opposite ends of the stomach, one at the fundus and one at the
antrum. The optimal magnet position for traversing the pylorus
posteriorly was found to be between vertebrae T5 and L2. However,
the inability to achieve 100% visualization of the fundus and
cardia with any station combination remains a major challenge.
The aim of the present study was to examine the
influence of body positioning and magnet-capsule distance on
intragastric navigation of the capsule, an area of research that
has received limited attention (7,8).
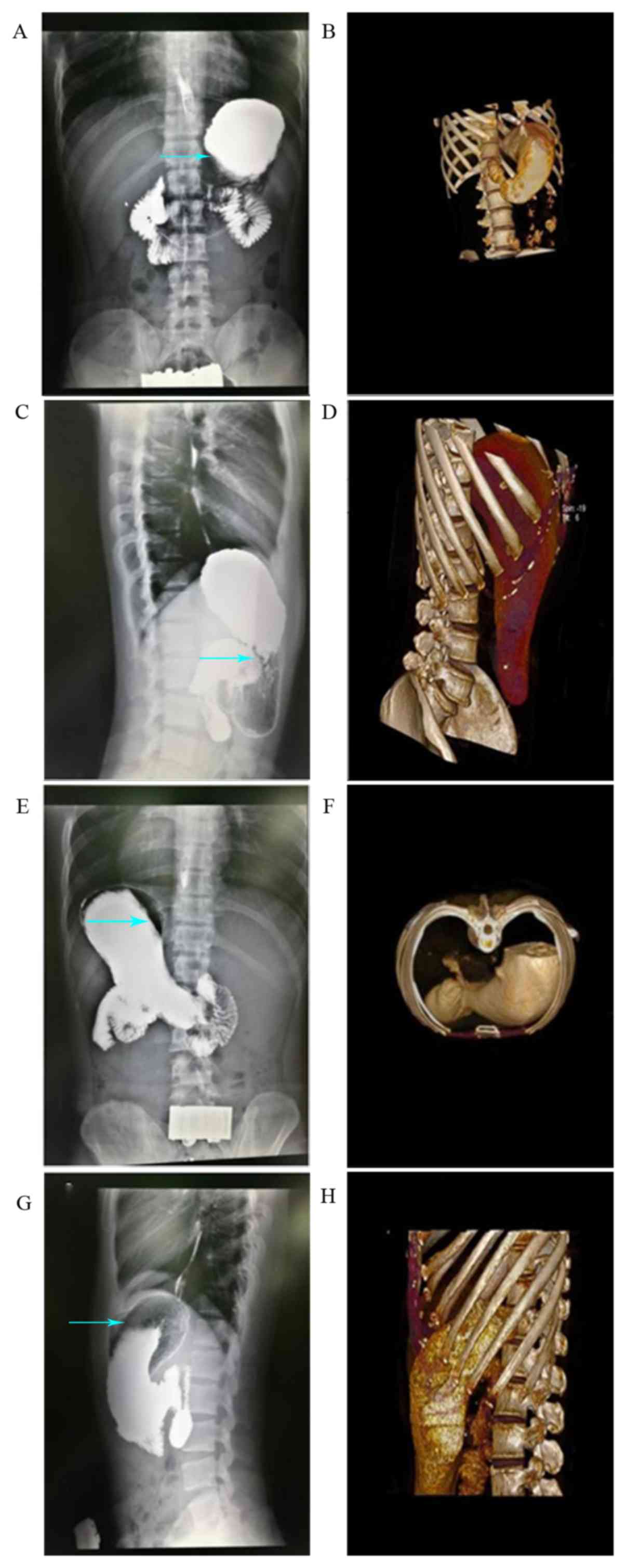
Radiology and UGIE images were examined to compare gastric
morphology between subjects in different body positions with the
aim of determining optimal subject body position and external
control magnet placement in order to enable magnet-controlled
capsule endoscopy with a thorough exploration of the stomach.
Materials and methods
Subjects
In total, 10 healthy adult volunteers [age, 30–49
years; body mass index (BMI), 20.7–24.6] were enrolled between 1st
March and 1st April 2018 at Nanshan Hospital, Guangdong Medical
University (Guangdong. China) including 5 subjects (2 men and 3
women) who received double-contrast barium upper gastrointestinal
X-ray radiography (UGI–XR), 4 subjects (2 men and 2 women) who
received virtual anatomical stomach modeling by spiral CT with a
volume rendering technique (VRT), and 1 male subject who received
traditional UGIE. The inclusion criteria were as follows: i) Age
range, 20–60 years; ii) no pregnancy planed within six months; and
iii) signed written informed consent. The exclusion criteria were
as follows: i) Overweight (BMI>25) or underweight (BMI<19);
ii) liver and kidney dysfunction; iii) afflicted with other
gastrointestinal diseases, including gastrointestinal bleeding or
intestinal obstruction; and iv) exhibited allergy to contrast
agent.
The study protocol was approved by the Independent
Ethics Committee of Nanshan Hospital, Guangdong Medical University.
Written informed consent was obtained from every volunteer.
UGI–XR
UGI–XR was conducted according to routine clinical
protocol. The subjects were instructed to fast overnight to ensure
at least 8 h of fasting before the examination. At 10 min post-oral
administration of a spasmolytic agent (10 mg anisodamine, Minsheng
Pharmaceutical Co., Ltd.), 3 g gas-producing agent powder (citric
acid, sodium bicarbonate 1:1, Bosen Pharmacy Co., Ltd.) was
administered orally, followed by rapid drinking of 200 ml barium
(220% weight/volume). For each subject, eight X-ray images of the
stomach were captured with a DR Definium 6000 (GE Healthcare) as
follows: Supine decubitus (1 image), prone decubitus (1 image),
right lateral decubitus (1 image), left lateral decubitus (1 image)
and standing upright (4 images). The standing upright images
included a ventral-facing image, a dorsal-facing image, a
left-facing image and a right-facing image.
Spiral CT with VRT
To limit radiation exposure, each volunteer was
scanned only once in one of the following designated positions:
Supine (49-year-old female; BMI, 23.9), left lateral (46-year-old
male; BMI, 24.6), prone (43-year-old female; BMI, 23.2) and right
lateral (40-year-old male; BMI, 22.9). After overnight fasting,
each subject drank 500 ml contrast agent (50 ml iodide dissolved in
water, diluted to 300 mg/ml. Taizhou Tianrui Pharmaceutical Co.,
Ltd.) 5 min before the examination. Images were obtained with a
Somatom Sensation 64 CT scanner (Siemens AG). A CT scan was
performed at 7-mm intervals from the mid-esophagus to the symphysis
pubis. Reformats were viewed on a dedicated diagnostic IDS7 PACS
workstation (Sectra Medical Systems GmbH) with multiplanar
reformatting. A VRT was applied to produce three-dimensional (3D)
stomach images.
UGIE
Only 1 healthy male (59 years old; BMI, 21)
undergoing a routine UGIE for early gastric cancer screening was
included in the present study. The UGIE examination was performed
in the standard left lateral decubitus position.
Data processing
To determine the optimal body position for
magnet-controlled capsule endoscopy, gastric angles were used as
judgment indexes. As a gastric wall scan-derived 3D model was
unavailable, gastric angles were estimated qualitatively based on
the available UGI–XR and 3D VRT-derived images. Two-dimensional
plain air-barium contrast UGI–XR films showed the complete shape of
the stomach and the locations of intragastric barium and air, which
were dependent upon gravity. 3D VRT showed a stereo model of the
intragastric fluid and air-fluid interface. The cross-angle between
the longitudinal axis of the fundus and the longitudinal axis of
the gastric body (FB angle), and the cross-angle between the
longitudinal axis of the gastric body and the longitudinal axis of
the antrum (BA angle), were examined. Each angle was categorized as
acute (≤90°) or obtuse (>90°) based on a combination of UGI–XR
and 3D VRT analysis across dynamic position changes. As a greater
angle reduces the level of resistance to capsule movement, the body
position with the greatest gastric angle was considered optimal for
magnetic capsule endoscopy. To better understand the hindrance of
FB and BA angles to intragastric capsule movement, special
attention was paid to recording variation in these angles in the
subject who underwent UGIE.
To assess external magnet placement during capsule
endoscopy, the vertical distances from the surface of the body to
distal points of the gastric fundus and antrum were measured in
UGI–XR and spiral CT images. These distances represent the maximal
distance that the capsule would likely be from the surface of the
body. As magnetic strength is inversely related to distance, the
surface of the torso with the shortest vertical distance to the
distal points of the fundus and antrum was chosen for external
magnet placement.
Statistical analysis
Descriptions of observations were applied to
non-numerical indexes. Each individual subject's numerical data are
reported directly; group data are presented as the mean and
standard deviation. Vertical distances from the body surface to the
distal gastric fundus/antrum of four directions in the same
position were compared with one-way ANOVA followed by the
Student-Newman-Keuls post hoc test. Two-tailed P-values of <0.05
were considered significant. All analyses were performed in SPSS
version 4.0 (SPSS, Inc.).
Results
Position of the stomach in different
positions
All 10 volunteers completed their examinations
without any adverse reactions. Plain film images and 3D models of
the stomach in the various decubitus positions are shown in
Fig. 1. When the subject was in a
supine position, the stomach was horizontal and located in the left
hypochondrium (fundus, body), with the antrum extending into the
epigastric region. When the subject was lying on either side, the
stomach had a tilted orientation, with the fundus being the lowest
point near the spine and the antrum being the highest point near
the ventral wall.
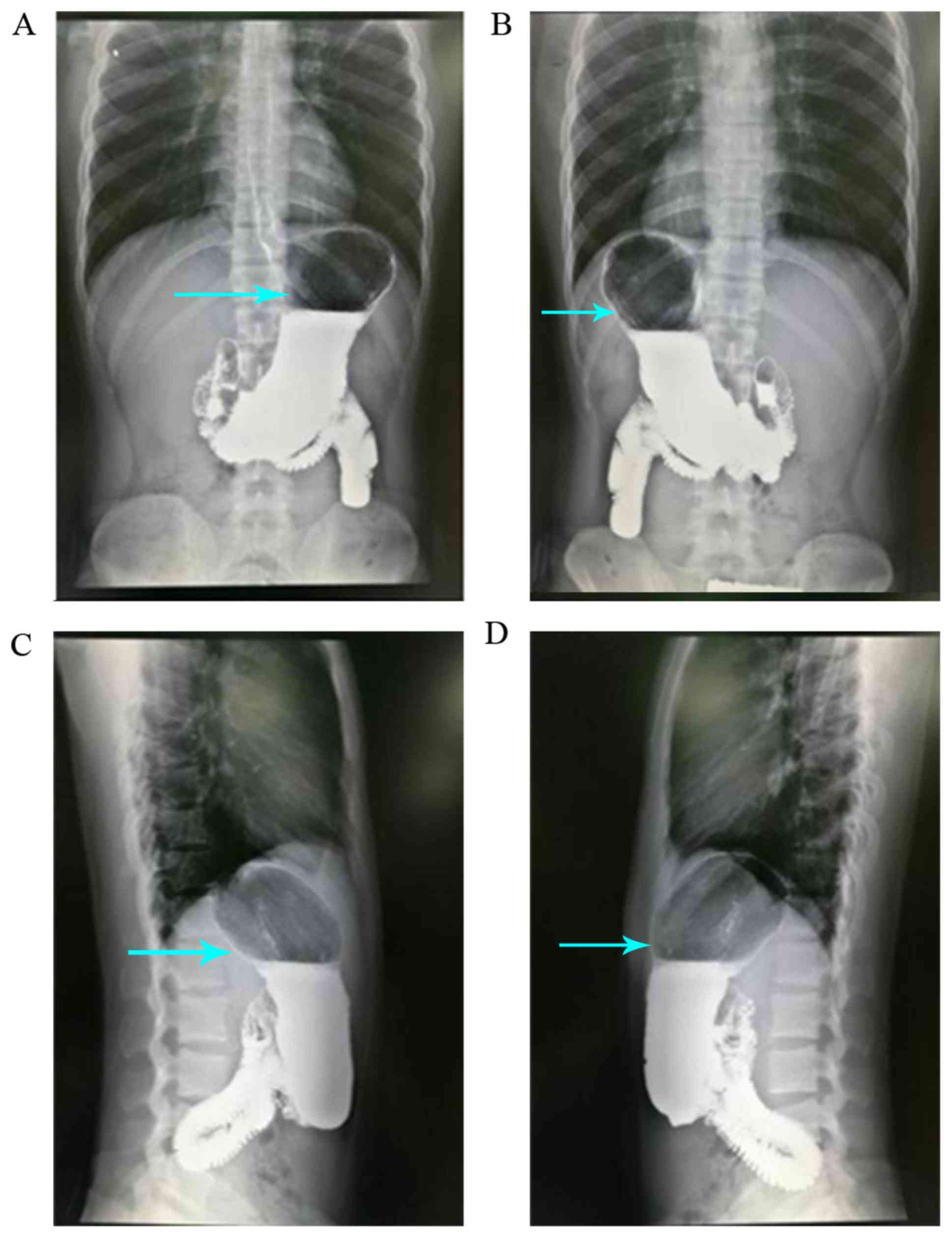
Plain film images of the stomach from the ventral,
dorsal, right side, left side and upright positions are shown in
Fig. 2. Compared with the supine
position, the stomach in standing subjects had shifted from a
largely horizontal position to a vertical position, descending to
near the ilium, and in one case even into the pelvis. When subjects
moved from lying supine to standing, the shape and location of the
stomach shifted, with the light gas ascending gradually and the
heavy contrast agent descending. The magnitude of gas/contrast
separation differed across the position as follows (from least to
most difference): Supine, left lateral, prone, right lateral and
standing (The arrows showed the magnitude of gas/contrast
separation in Figs. 1 and 2).
Gastric angles and optimal body
position
The FB angle was sharply acute in the supine
position, slightly wider, though still acute, in the left lateral
position, and slightly obtuse in the prone position and the right
lateral position. The FB angle flattened instantly to almost 180°
when the subject reached a standing position, wherein the
longitudinal axis of the fundus was nearly overlapping with the
longitudinal body axis. The BA angle was acute in all four
decubitus positions and obtuse in only the standing position. Given
the expectation that tighter FB and BA angles would be associated
with more resistance to capsule movement, the supine position and
left lateral position, which are used in traditional gastroscopy,
were ruled out as potentially suitable positions. Among the three
remaining candidate positions the prone position was least
suitable, due to its relatively small FB angle and its
inconvenience and discomfort for the person being examined. The
optimal position for magnetic capsule endoscopy was therefore
determined to be standing, and the second most optimal was
determined to be the right lateral decubitus position.
Vertical distances and external magnet
placement
The vertical distances from the body surface to
distal points of the fundus and antrum are shown in Tables I and II. The left lower lateral chest surface
and ventral wall had the shortest possible distance to the fundus
and antrum of any superficial body site in the same position. This
difference was statistically significant. Given the expectation
that a shorter distance would be associated with greater magnetic
strength, suitable placement positions for the external magnet
included the left lower lateral chest and the presently used
ventral wall.
 | Table I.Vertical distances from the surface of
the torso to the distal gastric fundus. |
Table I.
Vertical distances from the surface of
the torso to the distal gastric fundus.
| A, Mean vertical
distance to torso surface determined by UGI–XR, cm |
|---|
|
|---|
|
| Body position |
|---|
|
|
|
|---|
| Torso surface | Supine | Left side | Prone | Right side | Standing upright |
|---|
| Ventral | NDb | 16.3±3.0 | ND | 14.0±3.0 | 15.5±2.6 |
| Dorsal | ND | 15.3±4.6 | ND | 19.3±1.8 | 16.9±1.4 |
| Left lateral | 13.0±1.4a | ND | 12.5±1.4a | ND | 12.0±1.5a |
| Right lateral | 28.2±2.8 | ND | 26.6±4.0 | ND | 26.3±2.3 |
|
| B, Vertical
distance to torso surface determined by CT, cm |
|
|
| Body
position |
|
|
|
| Torso
surface | Supine | Left side | Prone | Right
side | Standing
upright |
|
| Ventral | 15.16 | 15.67 | ND | 13.42 | ND |
| Dorsal | 13.05 | 14.93 | ND | 16.11 | ND |
| Left lateral | 10.17 | 12.51 | ND | 9.13 | ND |
| Right lateral | 24.60 | 23.81 | ND | 23.52 | ND |
 | Table II.Vertical distances from the surface of
the torso to the distal gastric antrum. |
Table II.
Vertical distances from the surface of
the torso to the distal gastric antrum.
| A, Mean vertical
distance to torso surface determined by UGI–XR, cm |
|---|
|
|---|
|
| Body position |
|---|
|
|
|
|---|
| Torso surface | Supine | Left side | Prone | Right side | Standing upright |
|---|
| Ventral | NDb | 8.1±1.4a | ND | 8.6±0.4a | 6.8±1.2a |
| Dorsal | ND | 18.1±3.6 | ND | 16.3±3.2 | 19.5±2.4 |
| Left lateral | 17.2±3.8 | ND | 15.6±2.3 | ND | 14.5±4.3 |
| Right lateral | 14.8±1.2 | ND | 14.6±0.6 | ND | 13.0±1.5 |
|
| B, Vertical
distance to torso surface determined by CT, cm |
|
|
| Body
position |
|
|
|
| Torso
surface | Supine | Left side | Prone | Right
side | Standing
upright |
|
| Ventral | 7.06 | 5.53 | ND | 7.65 | ND |
| Dorsal | 15.57 | 17.86 | ND | 17.17 | ND |
| Left lateral | 19.13 | 12.89 | ND | 16.19 | ND |
| Right lateral | 9.94 | 9.47 | ND | 8.33 | ND |
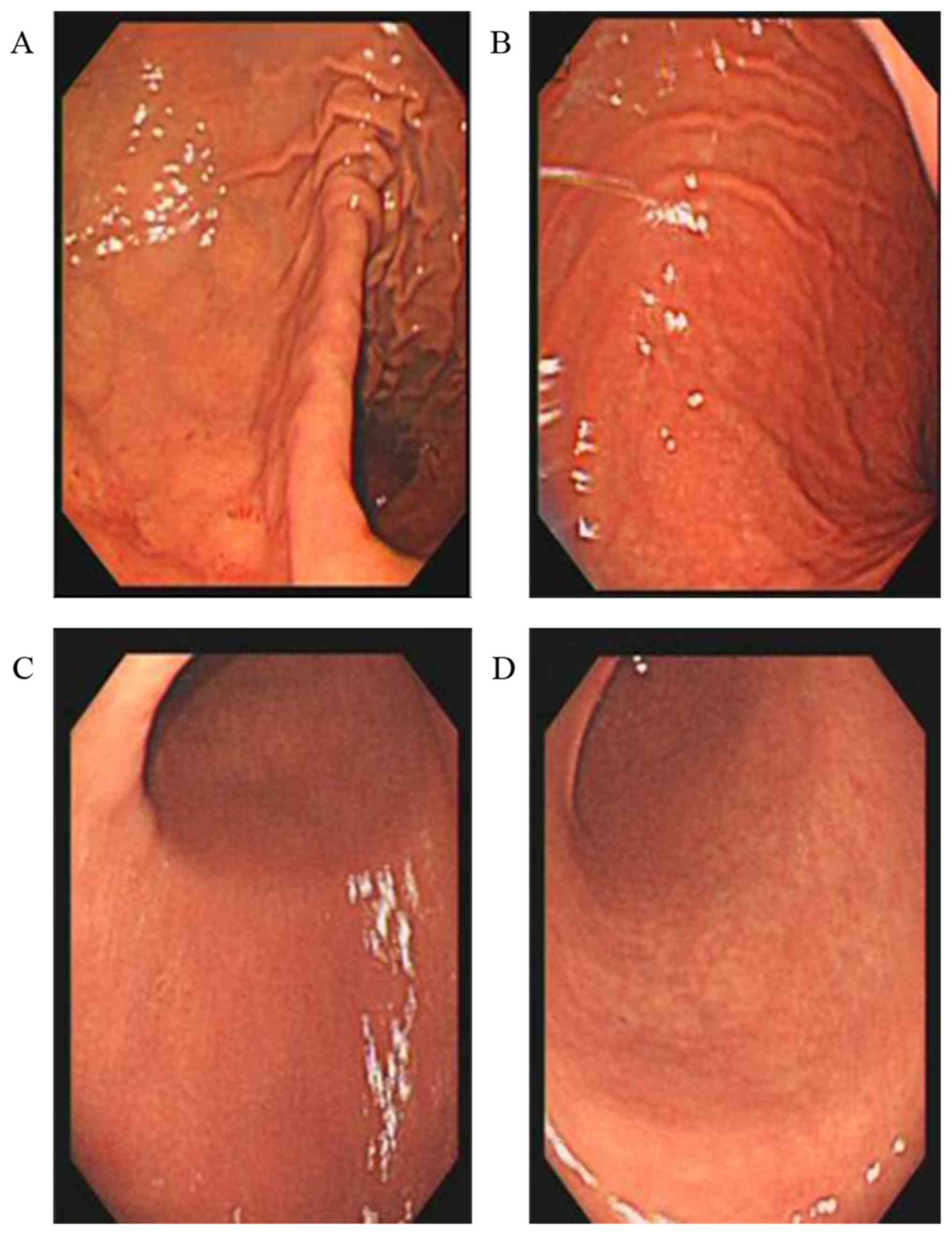
UGIE
UGIE performed on a 56-year-old healthy volunteer in
a routine left lateral position, with special attention being paid
to the FB angle and BA angle, revealed a ridged fundus-body
junction, with an acute FB angle when the endoscope passed through
the cardia (Fig. 3). As air
continued to be injected, inflating the stomach cavity, the FB
angle widened gradually from sharply acute to obtuse. When the
endoscope reached the distal body, the steep slope-like body-antrum
junction had an acute BA angle; the junction flattened as
additional air was injected, underscoring the importance of
inflating the gastric cavity fully to facilitate capsule movement
under the control of an external magnet.
Discussion
The analysis of the data obtained by UGI–XR, spiral
CT with VRT and UGIE in the present study showed that, of the
positions examined, the best position for a patient to be in during
magnet-controlled capsule endoscopy was standing, followed by the
right lateral decubitus position. The commonly used supine position
was found to be relatively disadvantageous. Additionally, the
analysis indicated that it would be beneficial to place the
external controlling magnet on the left lateral lower chest in
addition to the common placement position of the abdominal
wall.
There are three sets of movements involved in UGIE,
each with particular purposes, as follows: i) Maintenance of
moderate gastric inflation by air injection and deflation; ii)
keeping the visual field clean with suctioning and washing; and
iii) reaching a target site through scope advancement, retreat, and
rotation (14). Correspondingly,
magnet-controlled capsule endoscopy requires minimal obstacles to
capsule movement, clear visual imaging and sufficient magnetic
force to move the capsule (5).
Magnetic force is determined directly by magnetic
flux density and affected inversely by distance (8). The intensity of the external magnet
should be maximized to ensure that there is sufficient magnetic
power for capsule control. Magnetic power at a given magnetic
induction intensity is maximized by minimizing the distance between
the capsule target region and the controlling magnet. The gastric
antrum and body are near the abdominal wall, whereas the gastric
fundus is near the left lateral lower chest. Therefore, the
anterior abdominal wall is a good location for external magnet
placement, especially when the goal of the examination is to
explore the gastric antrum and body. However, this placement is not
well suited for exploring the fundus and cardia; the left lateral
lower chest is a better magnet placement site for optimal control
of the capsule in the fundus and cardia. Indeed, several reports
have attributed fundus/cardia exploration failures to a weak
magnetic force (6,7).
Currently, impedance of intragastric capsule
mobility by gastric angles is dealt with by inflating the stomach
with water and gas-generating reagents (12,13).
However, patient tolerance of inflation is limited (13). Belching and gastric emptying also
lead to continual loss of inflation (13,15). In
the present study, gastric angles were found to differ in relation
to body position owing to gravity effects. Notably, the supine
position, which is in common use, emerged as the worst position of
the five studied positions due to its association with sharp acute
BF and BA angles. Conversely, in the standing position, the FB and
BA angles are extended, placing the fundus, body and antrum in a
nearly linear relationship, which is highly amenable to capsule
movement. Among the four decubitus positions examined, the right
lateral position was found to be the preferred choice owing to its
associated relatively wide FA angle.
Regarding visualization clarity, the currently used
standard methods of patient fasting with ingestion of deforming
agents are far from satisfactory. The challenge of optimizing
visualization clarity, however, was beyond the scope of the present
modeling study.
The findings of the present analysis and UGIE case
observation suggest several possible reasons for the flexibility
reported in the first human trial of magnet-controlled capsule
endoscopy not being replicated thereafter. In the first trial,
capsule endoscopy was performed concomitantly with traditional UGIE
with the subject lying on the left side. There was ongoing air
injection to maintain gastric inflation, which tends to diminish
the FB angle, thereby facilitating capsule movement (5). Conversely, inflation of the stomach in
the subsequent studies relied on the subject drinking water with
gas-producing agents, which is less effective than active air
injection. Hence, capsule movement may have been hindered by a
non-extended FB angle in the subsequent studies.
There were several limitations to the present study.
First, 3D VRT was not conducted in the standing position due to the
technical limitations of CT. 3D sonography in the standing position
was attempted as an alternative, but it was not possible to
complete volume reconstruction, as the intragastric fluid volume
was too great for single-point scanning. The lack of these data may
lead to a bias in the model analysis. Additionally, gastric angles
were estimated qualitatively, rather than measured precisely.
Importantly, this limitation, while not ideal, had no effect on the
conclusions of the model analysis. The study cohort was also small.
In this regard, however, it is important to note that the gastric
shape changes associated with the various positions compared in
this study are common knowledge among radiologists.
In summary, the UGI–XR, spiral CT, and UGIE results
of the present study suggest that magnet-controlled capsule
endoscopy should be performed with the subject standing upright if
possible, or lying in the right lateral position if the patient is
unable to stand for the examination. Additionally, the results of
the present study indicate that suitable positions for placement of
the external control magnet include the left lower chest in
addition to the commonly employed ventral wall placement,
particularly for navigation of the gastric fundus and cardia. It
should be pointed out that this was a model analysis study and
further validation studies with both animals and humans are
warranted.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HDZ conceived and designed the study. TJS and CSC
were responsible for the collection and analysis of patient data.
HDZ revised the manuscript critically for important intellectual
content. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Independent Ethics
Committee of Nanshan Hospital, Guangdong Medical University.
Patients provided written informed consent.
Patient consent for publication
Written informed consent for publication was
obtained from every volunteer.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Iddan G, Meron G, Glukhovsky A and Swain
P: Wireless capsule endoscopy. Nature. 405:4172000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Iddan GJ and Swain CP: History and
development of capsule endoscopy. Gastrointest Endosc Clin N Am.
14:1–9. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Iddan GJ: A short history of the
gastrointetinal capsuleAtlas of Video Capsule Endoscopy. Keuchel M,
Hagenmüller F and Tajiri D: Springer; Berlin, Heidelberg: pp. 2–3.
2006, View Article : Google Scholar
|
|
4
|
Gong F, Swain P and Mills T: Wireless
endoscopy. Gastrointest Endosc. 51:725–729. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Swain P, Toor A, Volke F, Keller J, Gerber
J, Rabinovitz E and Rothstein RI: Remote magnetic manipulation of a
wireless capsule endoscope in the esophagus and stomach of humans
(with videos). Gastrointest Endosc. 71:1290–1293. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Keller J, Fibbe C, Volke F, Gerber J,
Mosse A, Reimann-Zawadzk M, Rabinovitz E, Layer P, Schmitt D,
Andresen V, et al: Inspection of the human stomach using
remote-controlled capsule endoscopy: A feasibility study in healthy
volunteers (with videos). Gastrointest Endosc. 73:22–28. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rahman I, Pioche M, Shim CS, Lee SP, Sung
IK, Saurin JC and Patel P: Magnet-assisted capsule endoscopy in the
upper GI tract by using a novel navigation system (with video).
Gastrointest Endosc. 83:889–895.e1. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rahman I, Kay M, Bryant T, Pelitari S,
Salter S, Dimitrov B and Patel P: Optimizing the performance of
magnetic-assisted capsule endoscopy of the upper GI tract using
multiplanar CT modelling. Eur J Gastroenterol Hepatol. 27:460–466.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rey JF, Ogata H, Hosoe N, Ohtsuka K, Ogata
N, Ikeda K, Aihara H, Pangtay I, Hibi T, Kudo S and Tajiri H:
Feasibility of stomach exploration with a guided capsule endoscope.
Endoscopy. 42:541–545. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rey JF, Ogata H, Hosoe N, Ohtsuka K, Ogata
N, Ikeda K, Aihara H, Pangtay I, Hibi T, Kudo SE and Tajiri H:
Blinded nonrandomized comparative study of gastric examination with
a magnetically guided capsule endoscope and standard
videoendoscope. Gastrointest Endosc. 75:373–381. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Denzer U, Röch T, Hoytat B, Abdel-Hamid M,
Hebuterne X, Vanbiervielt G, Filippi J, Ogata H, Hosoe N, Ohtsuka
K, et al: Magnetically guided capsule versus conventional
gastroscopy for upper abdominal complaints: A prospective blinded
study. J Clin Gastroenterol. 49:101–107. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liao Z, Duan XD, Xin L, Bo LM, Wang XH,
Xiao GH, Hu LH, Zhuang SL and Li ZS: Feasibility and safety of
magnetic controlled capsule endoscopy system in examination of
human stomach: A pilot study in healthy volunteers. J Interv
Gastroenterol. 2:155–160. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liao Z, Hou X, Lin-Hu EQ, Sheng JQ, Ge ZZ,
Jiang B, Hou XH, Liu JY, Li Z, Huang QY, et al: Accuracy of
magnetically controlled capsule endoscopy, compared with
conventional gastroscopy in detection of gastric diseases. Clin
Gastroenterol Hepatol. 14:1266–1273.e1. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Martin T, Schwab K and Singh S: Principles
of gastrointestinal endoscopy. Surgery. 32:139–144. 2014.
|
|
15
|
Zou WB, Hou XH, Xin L, Liu J, Bo LM, YU
GY, Liao Z and Li ZS: Magnetic-controlled capsule endoscopy vs.
gastroscopy for gastric diseases: A two center self-controlled
comparative trial. Endoscopy. 47:525–528. 2015. View Article : Google Scholar : PubMed/NCBI
|