Introduction
Clavicular fracture is quite common accounting for
approximately 5% of all fractures in adults. More than 80% of these
fractures are located in the middle third of the clavicle and are
displaced (1,2). Several clinical trials have shown
better functional outcomes after open reduction and internal
fixation for displaced midshaft clavicular fractures (DMCF), and
have confirmed the superiority of operative treatment in clinical
practice (3,4). Additionally, the nonunion rate seems to
be lower after operative treatment (0–3%) than conservative
treatment (21%) (4,5). Recent studies have shown that construct
failure rates range from 1.2 to 12.6%, including breaking or
bending of the plate and screw loosening (6–9).
Plates can be subdivided into reconstruction plates
and locking compression plates. Reconstruction plates have a lower
profile with a concentrated mass around the screw holes which
reduces the plate stiffness, resulting in a higher failure rate
than the locking compression plate when used for the fixation of
displaced clavicular fractures (6).
Locking compression plates, available in a straight and
anatomically pre-shaped design, are stronger and therefore much
more difficult to bend (6). The
failure rate of locking compression plate is low, and there is
little literature discussing the associated risk factors.
Additionally, there are few studies reporting whether second
surgery or nonoperative treatment was required in the occurrence of
plate breakage with fracture nonunion.
The primary aim of this study was to identify
possible risk factors for construct failure after the locking
compression plate fixation of DMCF. The secondary aim of this study
was to discuss the treatment strategies after the diagnosis of
plate breakage and fracture nonunion.
Materials and methods
This is a retrospective study, based on medical
records from the archives of the Shanghai Fengxian District Central
Hospital, from 2015 to 2017. This clinical study was approved by
the Shanghai Fengxian District Central Hospital Medical Ethics
Committee, and informed consent was obtained from the patients for
surgical procedures and inclusion of data in the study.
Six patients diagnosed with fracture nonunion and
plate breakage were included in this study. Preoperative
demographic and clinical variables are documented, including age of
the patient at the time of injury, gender, laterality, hand
dominance, mechanism of injury, treatment of the fracture preceding
the nonunion, and treatment of the nonunion after the diagnosis of
plate breakage. More specific nonunion risk factors were also
investigated, including prior clavicle fractures, previous clavicle
surgery, smoking history, and diabetes.
Plain X-ray film or computerized tomography (CT)
scans were carried out immediately after the injury, 2 days after
the surgery, and at every follow-up.
Results
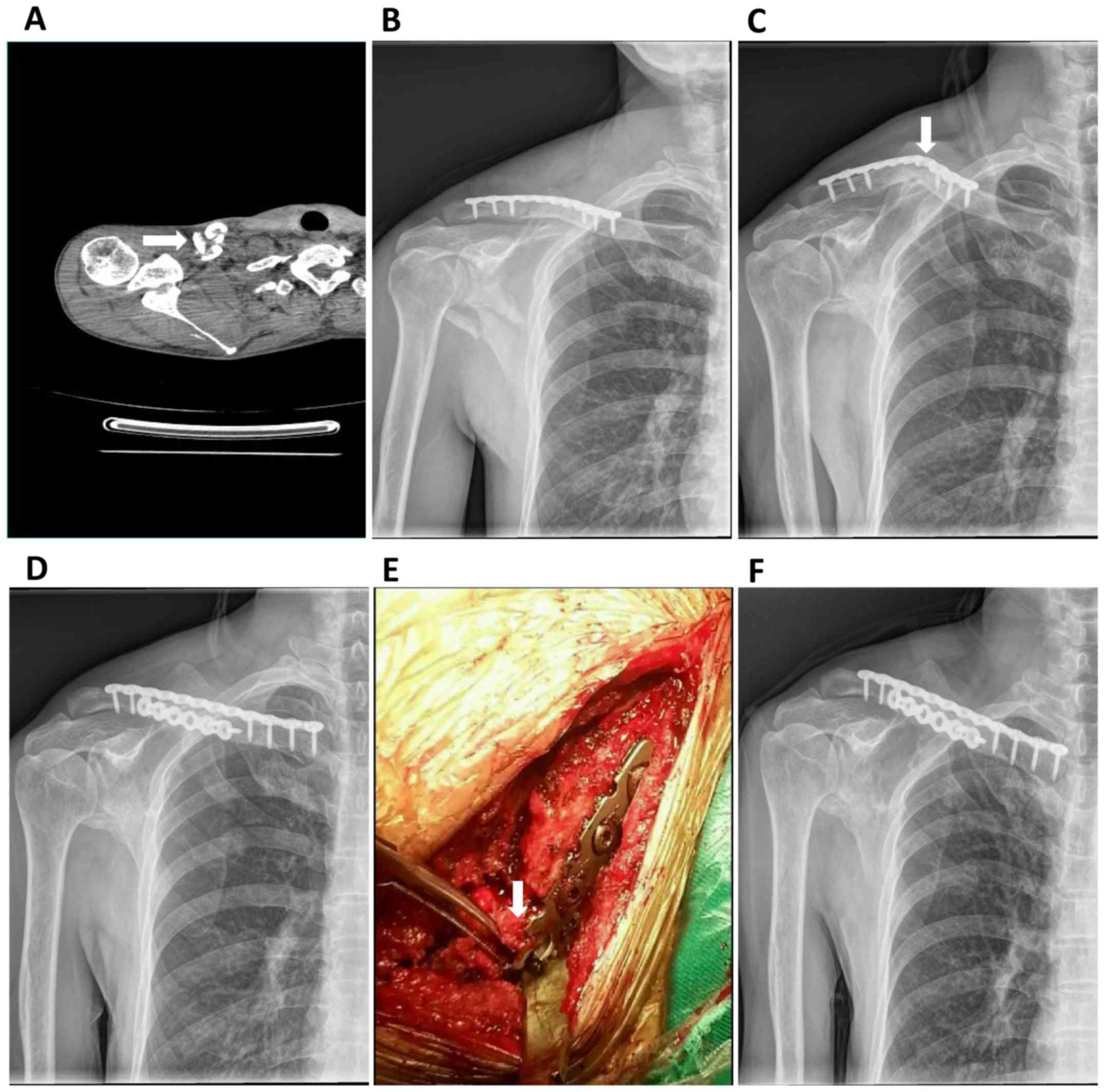
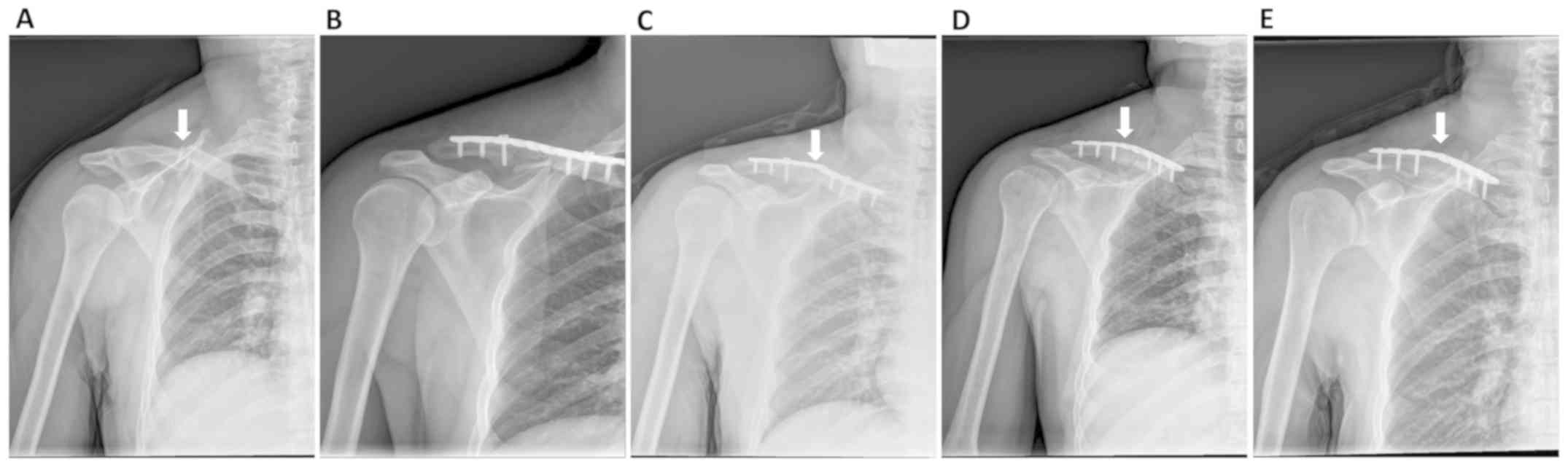
Six patients were included in the study. The
demographic data of the patients are documented in Table I. The fracture nonunion and plate
breakage occurred between 3 and 6 months after the first surgery.
All patients reported no history of injury before the plate
breakage but did have a history of daily heavy lifting. The
breakage site was near the free hole area around the fracture zone.
After the diagnosis of clavicle nonunion and plate breakage, four
patients received revision surgery of plate renewal and bone
grafting, and two patients received nonoperative treatment of
figure-of-eight splint and sling immobilization. All of the four
patients with revision surgery realized fracture union 3–9 months
after the second surgery (Figs. 1
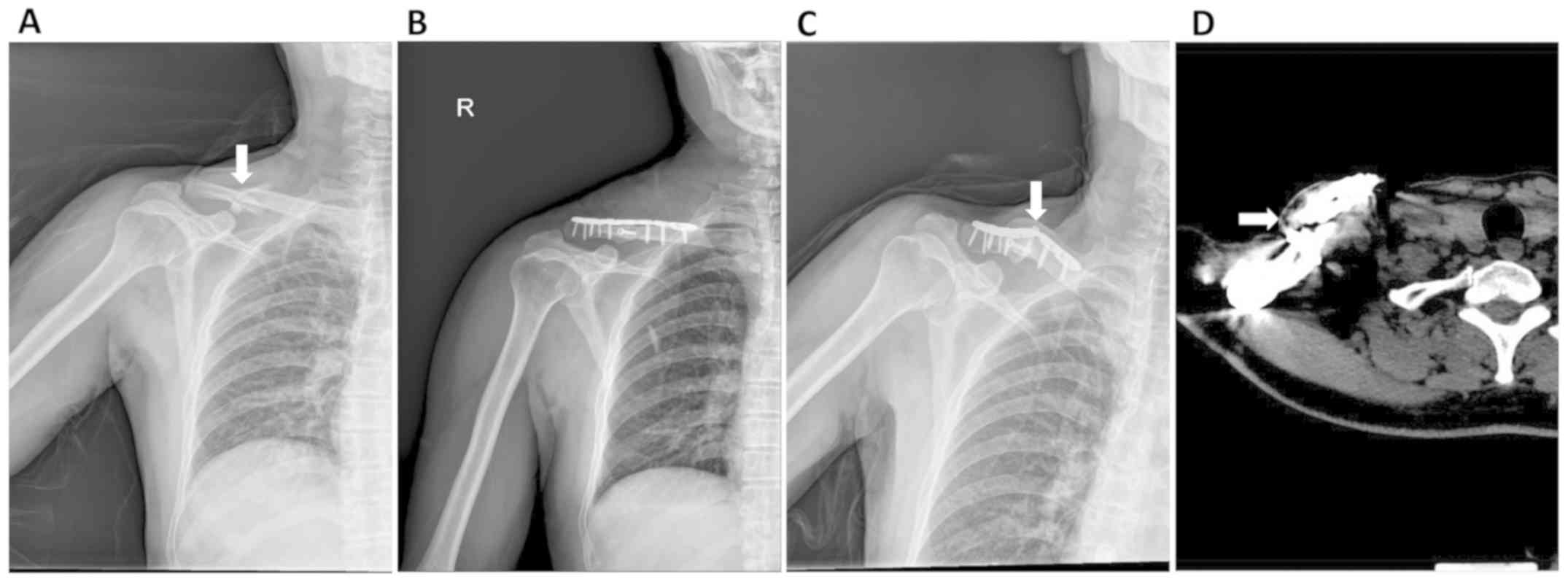
and 2). One patient with
nonoperative treatment still could not realize fracture union and
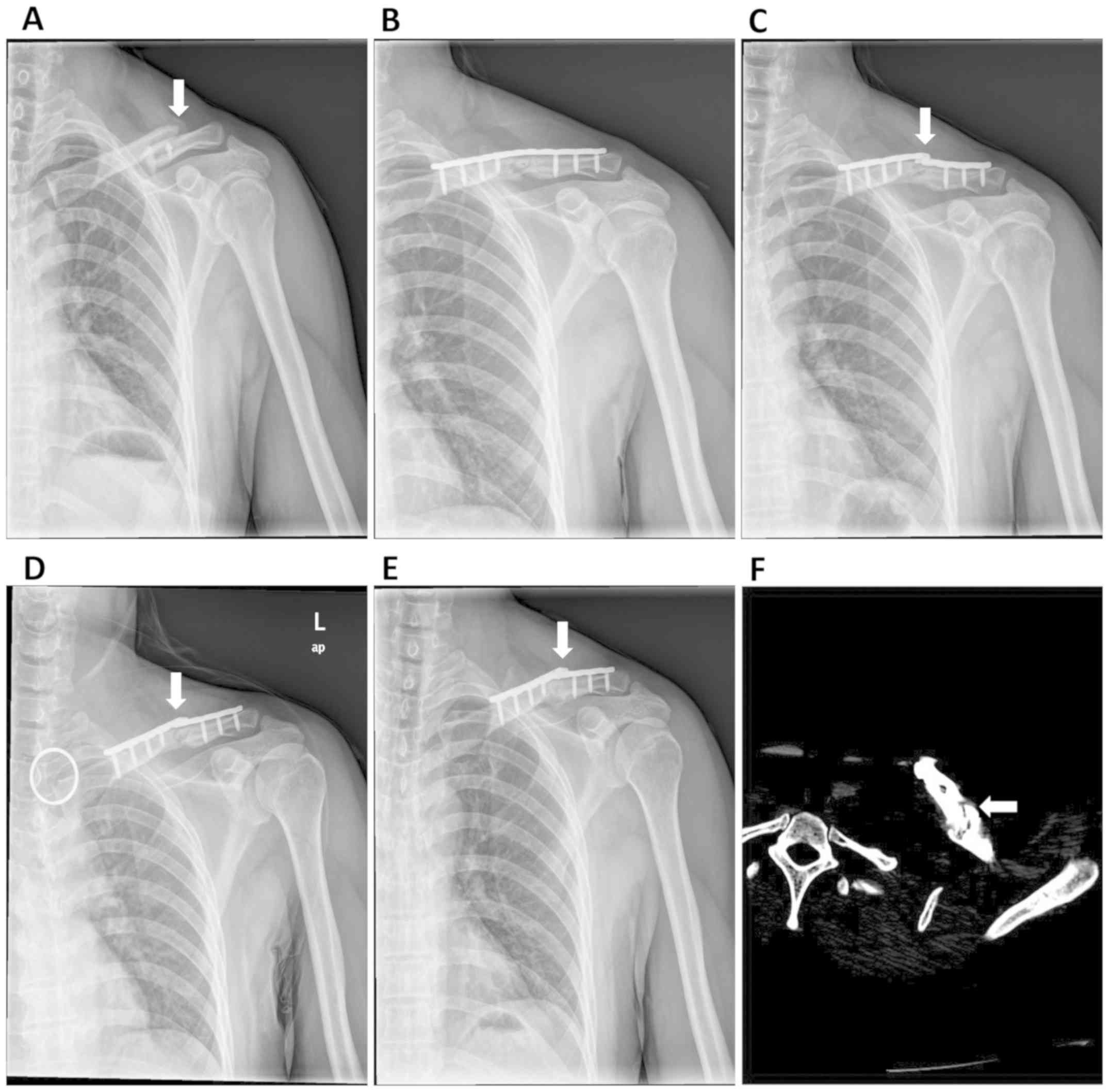
possibly needed revision surgery in the near fracture (Fig. 3). The other patient with nonoperative
treatment realized partial fracture union 6 months after the
diagnosis of plate breakage (Fig.
4).
 | Table I.Demographics and technical data of the
patients in the present study (n=6). |
Table I.
Demographics and technical data of the
patients in the present study (n=6).
| Demographic and
technical data | No. of patients |
|---|
| Sex |
|
| Male | 6 |
|
Female | 0 |
| Age, mean (range) in
years | 46.7 (35–68) |
| Mechanism of
injury |
|
| Fall from
height | 4 |
| Road
traffic accident | 2 |
| Laterality |
|
| Left | 1 |
|
Right | 5 |
| Hand dominance |
|
| Left | 0 |
|
Right | 6 |
| Prior clavicle
fractures |
|
| Yes | 0 |
| No | 6 |
| Prior clavicle
surgery |
|
| Yes | 0 |
| No | 6 |
| Smoking history |
|
| Yes | 3 |
| No | 3 |
| Diabetes history |
|
| Yes | 0 |
| No | 6 |
| AO
classification |
|
|
Completely displaced midshaft
fracture | 4 |
| Partially
displaced midshaft fracture | 2 |
| Length of first stay
(days) | 7±1 |
| Length between
initial surgery and plate breakage (months) | 3–6 |
| History of injury
before plate breakage |
|
| Yes | 0 |
| No | 6 |
Discussion
The clavicle is the major supporting structure for
the shoulder, and is mainly positioned under two frequent loading
modes: bending and compressive loads (10). Clavicle fractures are the most
frequent cited fractures of the shoulder with most of them are
located in the midshaft; this is related to the morphological and
mechanical features of the bone where the two inverse curves enable
the bone to absorb stress (11).
Open reduction and plate fixation are the common routine methods
for the treatment of clavicle fractures.
Reconstruction plates have a lower profile with a
concentrated mass around the screw holes which reduces the plate
stiffness. Locking compression plates, available in a straight and
anatomically pre-shaped design, and precisely pre-contoured to
reduce the need for additional intraoperative contouring, are
stronger and much more difficult to bend. Gilde et al
(12) discouraged the use of
reconstruction plates because of the higher rate of plate failure
in comparison to the stiffer dynamic compression plate. Currently,
locking compression plates are the mainstream internal implant for
clavicle fracture. Yet, locking compression plates still display a
certain rate of fixation failure.
When discussing implant failure, mechanical and
biological factors should be taken into account (10). The biological factor is usually
related to poor bone quality; when the failure point is located at
the bone-screw interface, the biological factor may play a more
important role. The mechanical factor usually concerns bending
stress on the bone that is transmitted to the implant and generates
a failure located at the screw-plate junction. We suspected that
our case was mainly due to a complex type of mechanical factors
because the patients are all middle-aged and have a low rate of
osteoporosis.
The traditional AO principles regarding bridge
plating (6,13) recommend to leave at least two or
three plate holes without screws in the fracture zone to avoid
stress concentration and plate failure. But in this case, we found
that plate breakage usually occurred between 3 and 6 months after
the first surgery, and the breakage point was right in the free
holes area around the fracture zone. Because of the fracture
pattern, it was not possible for a screw insertion in the
intermediary bone fragment without the risk for further damage.
Therefore, the unobstructed holes in this bridging technique
created a zone of minimal resistance in the area free of screws,
which induced plate breakage. It may be hypothesized that an
appropriate plate should not have unobstructed holes at all, and
monocortical screws or obturators placed in the free holes may
enhance mechanical plate integrity and prevent its failure.
Previous studies have shown that surgical techniques
of clavicular nonunion and plate breakage seem to be acceptable
with a good clinical outcome (6,10). In
the majority of cases, the authors performed a corrective osteotomy
followed by plate fixation and/or bone grafting. This seems to be
the preferred technique in the literature, as the primary goal of
surgical intervention should be the restoration of clavicle anatomy
(especially length, rotation and alignment) while creating an
environment that is conducive to bony union (14). In our case, the patients treated with
plate renewal and bone grafting realized fracture union in the next
3–9 months. One patient treated with nonoperative management still
did not realize fracture union and there was a high probability for
this patient to receive surgical treatment in the near future. The
other patient treated with nonoperative management realized partial
fracture union after 7 months of diagnosis of the plate breakage.
Thus, we believe that surgical treatment is necessary after the
diagnosis of fracture nonunion and plate breakage. A rigid fixation
by means of a plate to prevent rotation and allow early
mobilization combined with bone grafting to create a conducive
osteoblastic environment seems to be the best option for most
patients with clavicle malunions.
There are still several limitations to the present
study. Firstly, because of the small sample size, we could not
perform biomechanics analysis to further support our hypothesis.
Secondly, the retrospective design of the study also impaired its
validity. Thirdly, we also did not use monocortical screws in the
cases. Thus, this study is a case report. In the future, a higher
number of cases must be collected and detailed biomechanic analyses
must be performed to confirm our hypothesis.
In conclusion, it was demonstrated that the increase
in stress in the free holes area around the fracture zone is a risk
factor for fracture nonunion and plate breakage, and monocortical
screws or simple obturators for the holes around the fracture zone
should be used to protect the comminuted fragment for further
damage and enhance plate strength. After the diagnosis of fracture
nonunion and plate breakage, a second surgery for plate renewal and
bone grafting could provide high union rates, and should be a
necessary remedy.
Acknowledgements
Not applicable.
Funding
The present work was supported by the Natural
Science Foundation of Fengxian District, Shanghai (grant no.
20181703) and by the Foundation of Shanghai Municipal Commission of
Health and Family Planning (grant no. 201840135).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XH and HX researched and collected the data for the
study. FX and HX designed and directed the research study. XH wrote
the manuscript. All authors read and approved the manuscript and
agree to be accountable for all aspects of the research in ensuring
that the accuracy or integrity of any part of the work are
appropriately investigated and resolved.
Ethics approval and consent to
participate
The present study was approved by the Shanghai
Fengxian District Central Hospital Medical Ethics Committee and
written informed consent was obtained from all patients.
Patient consent for publication
All patients agreed with the publication of this
article.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nordqvist A and Petersson C: The incidence
of fractures of the clavicle. Clin Orthop Relat Res. 127–132.
1994.PubMed/NCBI
|
|
2
|
Postacchini F, Gumina S, De Santis P and
Albo F: Epidemiology of clavicle fractures. J Shoulder Elbow Surg.
11:452–456. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bernstein J: Nonoperative treatment
compared with plate fixation of displaced midshaft clavicular
fractures. J Bone Joint Surg Am. 89:1866–1867. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Robinson CM, Goudie EB, Murray IR, Jenkins
PJ, Ahktar MA, Read EO, Foster CJ, Clark K, Brooksbank AJ, Arthur
A, et al: Open reduction and plate fixation versus nonoperative
treatment for displaced midshaft clavicular fractures: A
multicenter, randomized, controlled trial. J Bone Joint Surg Am.
95:1576–1584. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Robinson CM, Court-Brown CM, McQueen MM
and Wakefield AE: Estimating the risk of nonunion following
nonoperative treatment of a clavicular fracture. J Bone Joint Surg
Am. 86:1359–1365. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Meeuwis MA, Pull Ter Gunne AF, Verhofstad
MH and van der Heijden FH: Construct failure after open reduction
and plate fixation of displaced midshaft clavicular fractures.
Injury. 48:715–719. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fridberg M, Ban I, Issa Z, Krasheninnikoff
M and Troelsen A: Locking plate osteosynthesis of clavicle
fractures: Complication and reoperation rates in one hundred and
five consecutive cases. Int Orthop. 37:689–692. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Andrade-Silva FB, Kojima KE, Joeris A,
Santos Silva J and Mattar R Jr: Single, superiorly placed
reconstruction plate compared with flexible intramedullary nailing
for midshaft clavicular fractures: A prospective, randomized
controlled trial. J Bone Joint Surg Am. 97:620–626. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Woltz S, Duijff JW, Hoogendoorn JM,
Rhemrev SJ, Breederveld RS, Schipper IB and Beeres FJ:
Reconstruction plates for midshaft clavicular fractures: A
retrospective cohort study. Orthop Traumatol Surg Res. 102:25–29.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Marinescu R, Antoniac VI, Stoia DI and
Lăptoiu DC: Clavicle anatomical osteosynthesis plate
breakage-failure analysis report based on patient morphological
parameters. Rom J Morphol Embryol. 58:593–598. 2017.PubMed/NCBI
|
|
11
|
Bachoura A, Deane AS, Wise JN and Kamineni
S: Clavicle morphometry revisited: A 3-dimensional study with
relevance to operative fixation. J Shoulder Elbow Surg. 22:e15–e21.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gilde AK, Jones CB, Sietsema DL and
Hoffmann MF: Does plate type influence the clinical outcomes and
implant removal in midclavicular fractures fixed with 2.7-mm
anteroinferior plates? A retrospective cohort study. J Orthop Surg
Res. 9:552014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wagner M: General principles for the
clinical use of the LCP. Injury. 34 (Suppl 2):B31–B42. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Martetschläger F, Gaskill TR and Millett
PJ: Management of clavicle nonunion and malunion. J Shoulder Elbow
Surg. 22:862–868. 2013. View Article : Google Scholar : PubMed/NCBI
|