Introduction
Lumbar intervertebral disc protrusion (LIDP) is
usually caused by degenerative changes of contents of
intervertebral disc (IVD), such as nucleus pulposus (NP) and
annulus fibrosus, it often occurs in the posterolateral region and
is the main cause of low back pain. It shows high incidence rate
and causes high medical expenses, thus increasing social and family
burdens (1,2). Lumbar discectomy is still one of the
best choices for patients who failed in conservative treatment, and
advantages of surgical treatment include its quick effects on the
improvement of symptoms and its good long-term efficacy (3,4).
However, the incidence rate of reherniation of IVD in patients
undergoing surgery is still 3–18%, which is the most important
reason for most patients to receive lumbar discectomy again, and
patients are 10 times more likely to have future spinal surgery
than standard care patients (5,6).
Therefore, choices of surgical methods are of great significance in
clinical practice.
Traditional fenestration discectomy involves a large
number of normal bones, muscle tissues, and small joints, which
causes great damage to the stability of spinal structure of
patients. Lumbar segmental instability is one of the causes of
failure of lumbar surgery (7,8). With
the continuous development of minimally invasive amplification
technology and the renewal of minimally invasive concepts,
minimally invasive surgery has been applied to various surgical
treatments and has achieved good effects (9). The application of endoscopic discectomy
in the clinical treatment of lumbar intervertebral disc protrusion
(LIDP) is increasing, which significantly reduces the damage to
patients and maximizes the stability of the spinal structure
(10,11). However, its efficacy has not been
widely recognized clinically.
Therefore, this study analyzed effects of endoscopic
removal of NP of IVD on LIDP again, as well as its influences on
inflammatory factors and immune function, so as to provide
references for clinical treatment of LIDP.
Patients and methods
Objects of study
A total of 145 patients with LIDP aged between 30
and 60 years were admitted to The First Affiliated Hospital of
Bengbu Medical College (Bengbu, China) from June 2017 to December
2018 were selected and were electively treated. Patients were
divided into two groups according to different treatment methods.
There were 87 patients treated with fenestration discectomy
(fenestration group) and 58 patients treated with endoscopic
removal of NP of IVD (minimally invasive group). The inclusion
criteria were as follows: Patients diagnosed as LIDP by X-ray
imaging and met the diagnostic criteria of LIDP (12); patients failed in conservative
treatment, with no spondylolisthesis and spinal stenosis. The
exclusion criteria were as follows: Patients experienced recurrence
of LIDP, or with previous history of surgery and multi-segmental
protrusion of IVD; patients with LIDP combined with diabetes,
hypertension, congenital spinal deformity, greater bone
compression, bone metabolic disease, tumor, severe infection,
hemophilia or other coagulation diseases.
This study was approved by the Medical Ethics
Committee of The First Affiliated Hospital of Bengbu Medical
College. Signed informed consents were obtained from the patients
or the guardians.
Surgical methods
Patients in the fenestration group underwent general
anesthesia in lateral posture. The location of lesion was localized
by X-ray after successful anesthesia. The skin was incised on the
fourth to the first spinous process. Surrounding tissues were
bluntly separated to show ligamentum flavum, and en bloc excision
of ligamentum flavum was performed. Nerve roots and dura mater were
separated by epidural detacher; longitudinal ligament and annulus
fibrosus were cut after exposing IVD; herniated NP was pulled out
by nerve root retractor; diseased tissues were removed and the
blood was stopped from flowing. Local anesthesia was adopted in the
minimally invasive group. The needle was inserted into vertebral
posterior or the center of the pedicle of vertebral arch under the
guidance of X-ray, and the needle was inserted through the
intervertebral foramen to the intervertebral space [2 ml suspension
of omnipaque and methylthioniniumchloride (6:1)]; and then
radiography was performed, guidewire was inserted, puncture needles
were out and catheter was put in; devices such as intervertebral
foramen were connected, the working channel of intervertebral
foramen was 8 mm; flocculent substances and fat were cleaned; loose
NP was removed and the blood was stopped from flowing after no
leakage.
Observation indicators
The efficacy of patients in the two groups within 6
months after surgery was evaluated by the modified MacNab score.
Differences in surgical related indexes (length of incision,
intraoperative blood loss, time of operation, time in bed, hospital
stays) of patients were compared between the two groups. The
Oswestry dysfunction score (pain in back and loin, leg pain,
ability of daily life, lifting, walking, sitting, standing) and VAS
pain score of patients were evaluated before surgery and 1, 3 and 6
months after surgery. The incidence rate of complications of
patients was counted in the two groups. Changes of inflammatory
factors (TNF-α, IL-4, IL-6) and immune function (CD3+,
CD4+ and CD8+ cells) of patients between the
two groups were compared before surgery, 24 and 48 h after
surgery.
Detection methods
The fasting peripheral blood of patients was
collected in the early morning. After heparin anticoagulation,
serum was centrifuged at 100 × g at 4°C for 10 min to detect
inflammatory factors of patients. Levels of TNF-α, IL-4 and IL-6
were all detected by ELISA. The detection kits were purchased from
Abcam, with cat. nos. ab181421, ab46022 and ab46027, respectively.
Altogether 20 µl samples or standard products were added into
96-well plates and negative controls were set. Each sample was
provided with three parallel wells, water bath was carried out at
37°C for 30 min after sealing the membrane, excess liquid was
poured out, washing buffer was used 3 times, each time for 30 sec,
and enzyme-labeled antibody was added. Then, the above steps were
repeated for incubation and washing, 50 µl of developer A and B
were successively added, they were developed at 37°C in the dark
for 15 min, 50 µl of stopping solution was added to terminate the
reaction, absorbance of the samples was measured within 15 min with
450 nm measuring wavelength. The microplate reader was purchased
from Beijing Putian Xinqiao Technology Co., Ltd. CD3+,
CD4+ and CD8+ cells were detected by Attune
NxT flow cytometer and purchased from Thermo Fisher Scientific,
Inc., and relevant reagents and instruments were supplied by Thermo
Fisher Scientific, Inc.
Statistical analysis
SPSS 19.0 (SPSS, Inc., Chicago, IL, USA) was
adopted. The measurement data were expressed as [n (%)], and
comparison of ratios between the two groups was tested by
χ2 test. The enumeration data were expressed as mean ±
standard deviation (mean ± SD), and the comparison between the two
groups was performed by independent-samples t-test. The comparison
of different time points in the group was performed by repeated
measures analysis of variance, and the post hoc test was performed
by LSD test. P<0.05 was considered to indicate a statistically
significant difference.
Results
General data
There were 87 patients in the fenestration group,
including 48 males (55.17%) and 39 females (44.83%), aged
36.75±5.48 years. There were 58 patients in the minimally invasive
group, including 34 males (58.62%) and 24 females (41.38%), aged
38.16±5.93 years. There were no statistical differences in ratios
of sex and age between the two groups (P>0.05), neither any
significant difference in other data such as body mass index (BMI),
course of disease, and pathological segments between them
(P>0.05) (Table I).
 | Table I.General data. |
Table I.
General data.
| Variables | Fenestration group
(n=87) | Minimally invasive
group (n=58) | χ2/t | P-value |
|---|
| Sex [n (%)] |
|
| 0.168 | 0.682 |
| Male | 48 (55.17) | 34 (58.62) |
|
|
|
Female | 39 (44.83) | 24 (41.38) |
|
|
| Age (years) | 36.75±5.48 | 38.16±5.93 | 1.469 | 0.144 |
| BMI
(kg/m2) | 23.75±3.14 | 23.48±3.86 | 0.462 | 0.645 |
| Course of disease
(years) | 1.04±0.12 | 1.06±0.14 | 0.919 | 0.360 |
| Pathologic segments
[n (%)] |
|
| 1.394 | 0.498 |
|
L3-L4 | 10 (11.49) | 6
(10.34) |
|
|
|
L4-L5 | 45 (51.72) | 25 (43.10) |
|
|
|
L5-S1 | 32 (36.78) | 27 (46.55) |
|
|
| Prominent types [n
(%)] |
|
| 0.065 | 0.799 |
| Central
type | 18 (20.69) | 11 (18.97) |
|
|
|
Peripheral type | 69 (79.31) | 47 (81.03) |
|
|
| Straight leg
raising test [n (%)] |
|
| 0.115 | 0.734 |
|
Positive | 44 (50.57) | 31 (53.45) |
|
|
|
Negative | 43 (49.43) | 27 (46.55) |
|
|
| Combined with
paresthesia [n (%)] |
|
| 0.105 | 0.746 |
|
Yes | 19 (21.84) | 14 (24.14) |
|
|
| No | 68 (78.16) | 44 (75.86) |
|
|
| Combined with
abnormal movements [n (%)] |
|
| 0.070 | 0.791 |
|
Yes | 15 (17.24) | 11 (18.97) |
|
|
| No | 72 (82.76) | 47 (81.03) |
|
|
Clinical efficacy
There were no significant differences in rates of
excellent, good, acceptable, and poor efficacy of patients between
the two groups (P>0.05) (Table
II).
 | Table II.Analysis of clinical efficacy of
patients in the two groups [n (%)]. |
Table II.
Analysis of clinical efficacy of
patients in the two groups [n (%)].
| Variables | Fenestration group
(n=87) | Minimally invasive
group (n=58) | χ2 | P-value |
|---|
| Excellent | 46 (52.87) | 36 (62.07) | 1.198 | 0.274 |
| Good | 28 (32.18) | 17 (29.31) | 0.134 | 0.714 |
| Acceptable | 9
(10.34) | 4
(6.90) | 0.507 | 0.476 |
| Poor | 4
(4.60) | 1
(1.72) | 0.863 | 0.353 |
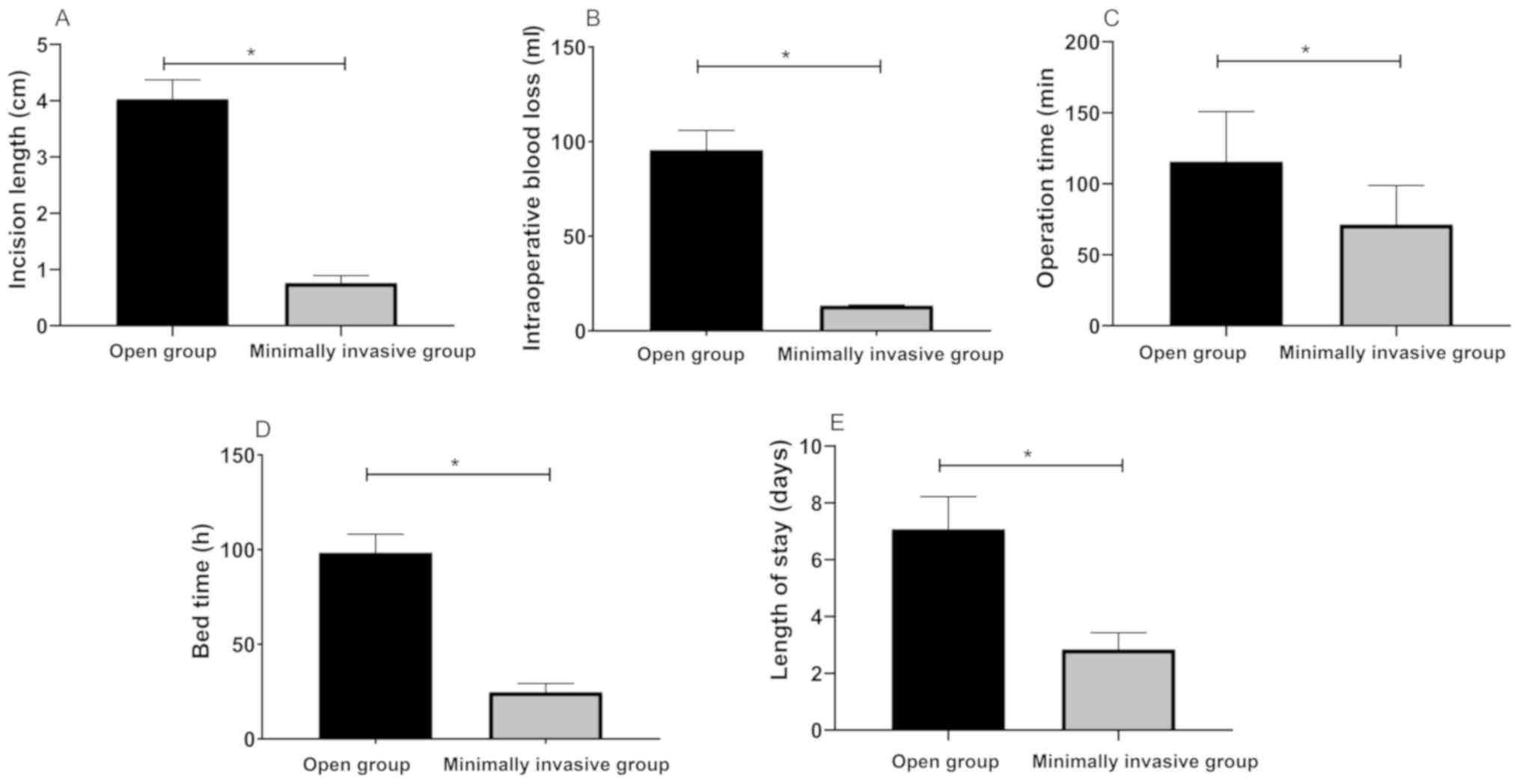
Analysis of surgical related
indicators
Length of surgical incision, intraoperative blood
loss, time of operation, time in bed, and hospital stays of
patients in minimally invasive group were lower than those in
fenestration group (P<0.05) (Fig.
1).
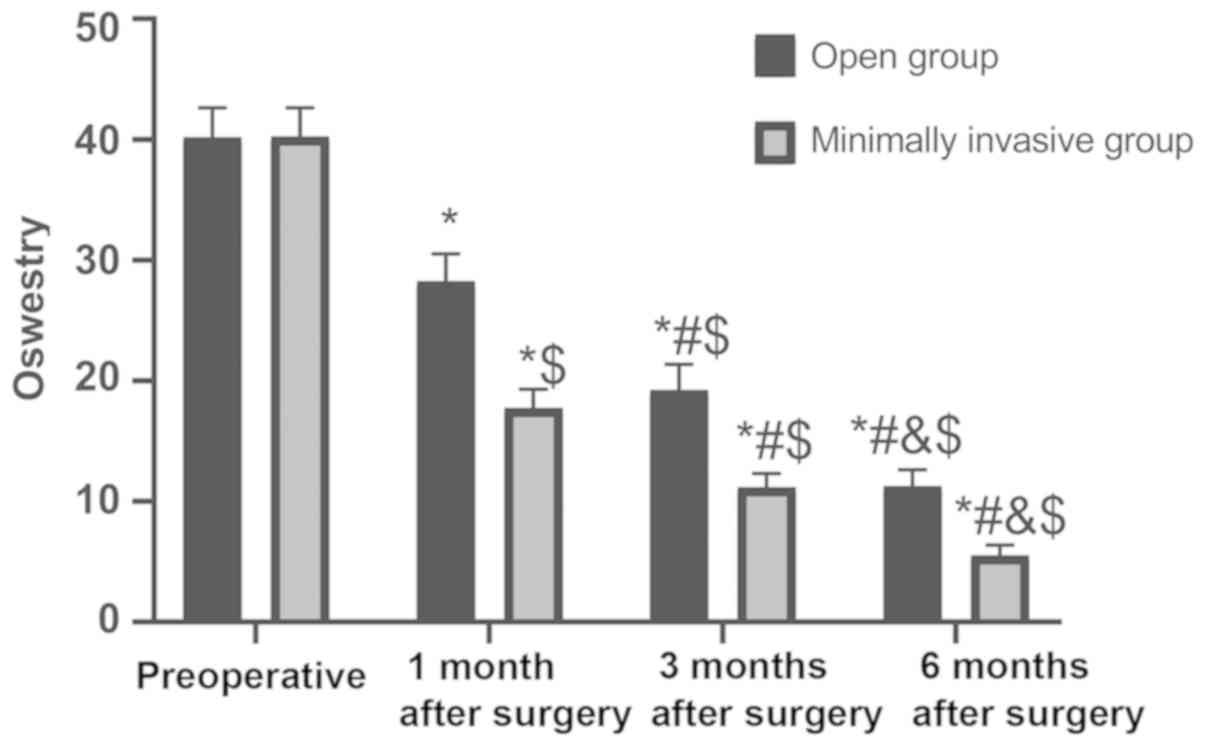
Analysis of Oswestry dysfunction
There were no statistical differences in the
Oswestry score of patients between the two groups before surgery
(P>0.05). The Oswestry score of patients in the two groups
continuously decreased 1, 3 and 6 months after surgery (P<0.05),
and the Oswestry score of patients in minimally invasive group was
lower than those in fenestration group 1, 3 and 6 months after
surgery (P<0.05) (Fig. 2).
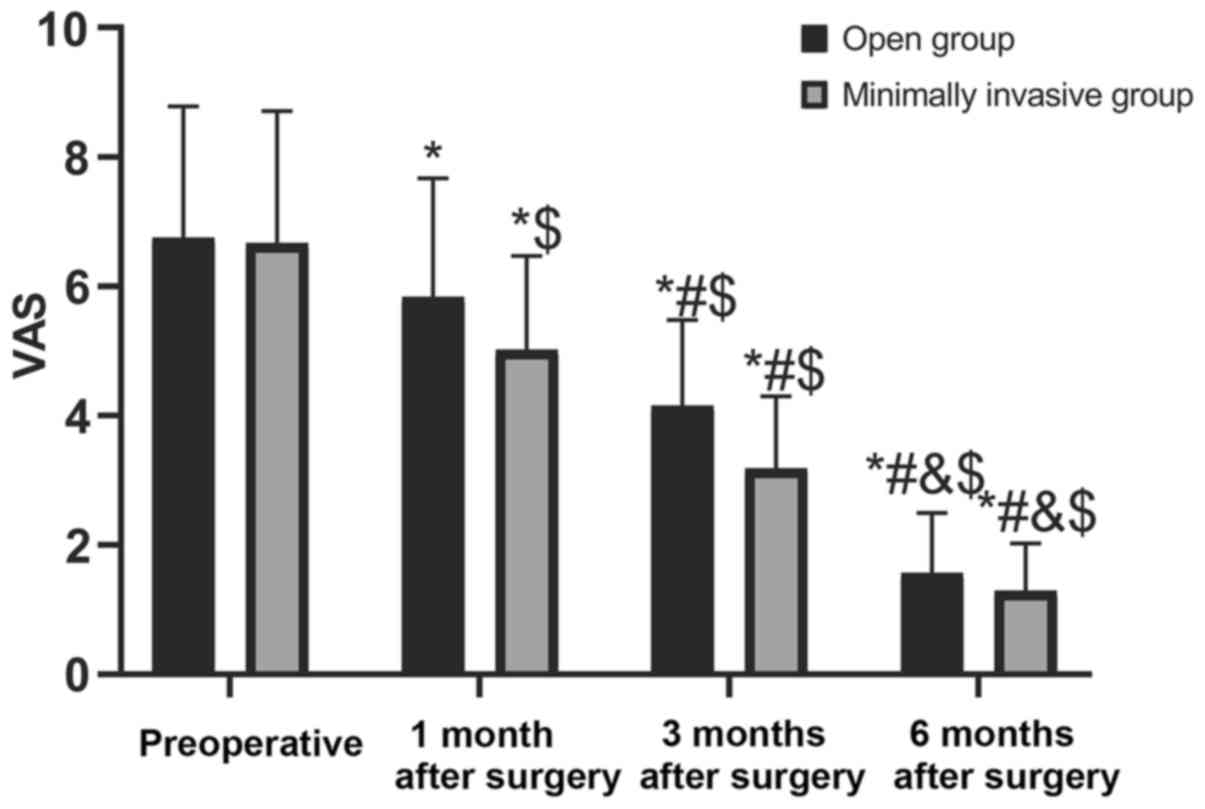
Results of VAS score
There were no significant differences in the VAS
score of patients between the two groups before surgery
(P>0.05). The VAS score of patients in the two groups
continuously decreased 1, 3 and 6 months after surgery (P<0.05),
and the VAS score of patients in the minimally invasive group was
lower than those in the fenestration group 1, 3 and 6 months after
surgery (P<0.05) (Fig. 3).
Analysis of the incidence rate of
complications in the two groups
The incidence rate of spinal instability of patients
in minimally invasive group was significantly lower than that in
fenestration group (P<0.05). There were no statistical
differences in the incidence rate of incision infection and
transient nerve paralysis (P>0.05). The incidence rate of
complications of patients was also higher than that in minimally
invasive group (P<0.05) (Table
III).
 | Table III.Analysis of incidence rate of
complications of patients in the two groups [n (%)]. |
Table III.
Analysis of incidence rate of
complications of patients in the two groups [n (%)].
| Variables | Fenestration group
(n=87) | Minimally invasive
group (n=58) | χ2 | P-value |
|---|
| Incision
infection | 7
(8.05) | 3 (5.17) | 0.448 | 0.504 |
| Transient nerve
paralysis | 10 (11.49) | 2 (3.45) | 2.003 | 0.157 |
| Spinal
instability | 7
(8.05) | 0 (0.00) | Fisher | 0.042 |
| Total
complications | 24 (27.59) | 5 (8.62) | 7.823 | 0.005 |
Analysis of levels of inflammatory
factors after surgery of patients in the two groups
Levels of TNF-α, IL-4 and IL-6 of patients in the
two groups were not significantly different before surgery
(P>0.05). Levels of TNF-α and IL-6 of patients in the two groups
continuously decreased 24 and 48 h after surgery (P<0.05).
Levels of IL-4 continued to rise (P<0.05); however, levels of
TNF-α and IL-6 of patients in minimally invasive group after
surgery were lower than those in fenestration group (P<0.05) and
levels of IL-4 were higher (P<0.05) (Table IV).
 | Table IV.Analysis of levels of inflammatory
factors after surgery of patients in the two groups (pg/ml). |
Table IV.
Analysis of levels of inflammatory
factors after surgery of patients in the two groups (pg/ml).
| Variables | Fenestration group
(n=87) | Minimally invasive
group (n=58) | t | P-value |
|---|
| TNF-α |
| Before
surgery |
90.24±9.64 |
91.19±9.14 |
0.593 |
0.554 |
| 24 h
after surgery |
68.42±5.25a |
50.13±4.86a | 21.164 | <0.001 |
| 48 h
after surgery |
51.24±3.43a,b |
20.02±2.73a,b | 58.106 | <0.001 |
| IL-4 |
| Before
surgery |
24.28±3.12 |
23.83±2.87 |
0.878 |
0.381 |
| 24 h
after surgery |
35.22±3.02a |
46.48±1.85a | 25.381 | <0.001 |
| 48 h
after surgery |
40.24±1.88a,b |
49.22±1.83a,b | 28.477 | <0.001 |
| IL-6 |
| Before
surgery | 234.58±28.64 | 233.76±27.15 |
0.172 |
0.863 |
| 24 h
after surgery |
164.73±20.42a |
131.68±17.15a | 10.163 | <0.001 |
| 48 h
after surgery |
92.19±14.32a,b |
60.47±12.36a,b | 13.787 | <0.001 |
Changes in postoperative immune
function of patients in the two groups
There were no statistical differences in cellular
levels of CD3+, CD4+, and CD8+ of
patients between the two groups before surgery (P>0.05).
Cellular levels of CD3+, CD4+, and
CD8+ in the two groups 24 h after surgery were lower
than those before surgery (P<0.05). CD3+ and
CD4+ cells in the two groups 48 h after surgery
recovered to preoperative similar level (P>0.05), which were
higher than those at 24 h after surgery (P<0.05). But cellular
levels of CD8+ continued to decrease (P<0.05).
Cellular levels of CD3+, CD4+, and
CD8+ of patients in minimally invasive group were higher
than those in fenestration group 24 and 48 h after surgery
(P<0.05) (Table V).
 | Table V.Changes in postoperative immune
function of patients in the two groups (%). |
Table V.
Changes in postoperative immune
function of patients in the two groups (%).
| Variables | Fenestration group
(n=87) | Minimally invasive
group (n=58) | t | P-value |
|---|
| CD3 |
| Before
surgery | 58.67±14.75 | 59.43±13.43 | 0.315 | 0.753 |
| 24 h
after surgery |
51.36±10.57a |
55.83±11.39a | 2.398 | 0.018 |
| 48 h
after surgery |
55.85±10.42b |
59.86±10.27b | 2.283 | 0.024 |
| CD4 |
| Before
surgery | 31.47±7.66 | 30.75±8.15 | 0.540 | 0.590 |
| 24 h
after surgery |
24.13±9.07a |
28.48±8.39a | 2.914 | 0.004 |
| 48 h
after surgery |
29.17±9.83b |
32.82±11.28b | 2.064 | 0.041 |
| CD8 |
| Before
surgery | 25.12±9.17 | 25.85±9.22 | 0.524 | 0.601 |
| 24 h
after surgery |
16.04±7.25a |
20.79±8.64a | 3.928 | <0.001 |
| 48 h
after surgery |
12.87±5.69a,b |
17.13±6.11a,b | 4.759 | <0.001 |
Discussion
LIDP is an increasingly serious public health
problem characterized by increased fibrosis, decreased content of
proteins and polysaccharides, reduced ability of tissue binding and
water retention, and impaired mechanical properties of the motor
segment. Its recurrence rate ranges from 5 to 25% (13,14).
Safe and effective surgical treatment of LIDP is of great
importance to surgeons. Minimally invasive surgery has always been
an important research direction for surgical treatment. This study
analyzed the therapeutic value of endoscopic discectomy in patients
with LIDP.
The results of this study showed that there were no
differences in clinical effects of the two surgical methods, but
the incidence rate of postoperative complications after minimally
invasive surgery was significantly lower than that after
fenestration surgery, especially the incidence rate of spinal
instability. Spinal instability is the main complication after
surgery of fenestration discectomy. Fenestration discectomy
requires extensive resection of bone tissues and ligaments, so
patients after it often require fixation of additional surgical
instruments to reduce postoperative spinal instability (15), which can be avoided with endoscopic
discectomy. The spinal canal can fully enter the midline of the
spinal canal without extensive resection of the small joint or
adjacent pedicle. In the present study of Li et al (16), IVD total endoscopic surgery of L5/S1
through lamina was a safe, reasonable and effective minimally
invasive spinal surgery technique with good short-term clinical
efficacy. Similar results were reported in another study (17). There were no significant changes in
the height of IVD of patients under percutaneous endoscopic lumbar
discectomy, and the height of IVD was significantly reduced from
23.7±3.3 to 19.1±3.7 in patients with fenestration discectomy. The
study also showed that the minimally invasive group experienced
significantly shorter time of surgery, hospitalization and
returning to work, which was similar to our results. Our results
also showed that the length of incision, amount of intraoperative
blood loss, time of operation, time in bed, and hospital stays in
minimally invasive group were lower than those in fenestration
group. Similar conclusions were found in the study of Garg et
al (18): The amount of bleeding
and hospital stays were significantly shorter in patients
undergoing microendoscopic discectomy. These indicators are related
to surgical safety. Chen et al (19) indicated that percutaneous endoscopic
discectomy had better safety and was associated with less blood
loss, shorter hospital stays, and short incision, and was the best
choice for patients with LIDP. Pan et al (20) also compared endoscopic lumbar
discectomy with traditional lumbar discectomy in patients with
LIDP. In their results, patients in the endoscope group were
significantly more satisfied with the treatment than those in the
traditional treatment group, and the bleeding volume, hospital
stays, and wound size in the endoscope group were also smaller than
those in the traditional treatment group. In addition, they also
found that the improvement of inflammatory cytokines IL-6 and CPR
in the endoscope group at 24 and 48 h after surgery was
significantly better than that in the traditional treatment group,
which was similar to our results. However, they did not find any
difference in the incidence rate of complications between the two
groups. Only one case of numb nerve occurred in the endoscope group
and recovered after 2 weeks, while no complications occurred in the
traditional treatment group. The incidence rate of complications
after discectomy reportedly ranges from 13.2 to 19.3% (21), which requires further analysis of
more factors, such as the proficiency of surgical operators,
surgical approach, postoperative nursing and so on.
Another interesting finding of this study was that
patients in minimally invasive group had lower levels of
postoperative inflammatory response and faster immune function
recovery. Chang et al (22)
drew similar conclusions in their study. The levels of inflammatory
factors TNF-α and CRP in patients undergoing percutaneous
endoscopic lumbar discectomy were also significantly lower than
those in patients undergoing open discectomy. We speculated that
this was related to postoperative pain in patients. Pain of the
patients with IVD protrusion after the NP removal was reduced, the
compression nerve and the local inflammation caused by it were also
reduced. Therefore, the degree of inflammation is an indirect
indicator for judging effects of surgery (23). In some studies, it has been reported
that increased inflammatory response caused by surgical stress is
an important cause of postoperative pain in patients because
inflammatory factors are also important mediators of pain (24). In a basic study, pain behavior was
increased after injection of TNF-α in IVD puncture model of mice
(25). The Oswestry score can assess
functions of pain in back and loin, leg pain, ability of daily
life, lifting, walking, sitting, and standing (26). In our results, the Oswestry score in
the minimally invasive group was significantly better than those in
fenestration group at 1, 3 and 6 months after surgery. Results of
further analysis of pain also showed that the degree of
postoperative pain of patients in minimally invasive group was
significantly lower than that in fenestration group. In the study
of Liu and Wang (27), it was also
found that percutaneous endoscopic discectomy could effectively
treat LIDP, which was beneficial to reduce pain and inflammation.
However, there are few reports on effects of these two surgical
methods on postoperative immune function. Postoperative pain could
cause immunosuppression and lead to decreased immune function in
patients (28). The minimally
invasive group experienced lower postoperative pain, so the degree
of inhibition of immune function was lower. This result was also
confirmed by our studies. Although cellular levels of
CD3+, CD4+, and CD8+ in the two
groups were decreased 24 h after surgery, the minimally invasive
group had significantly higher levels than the fenestration
group.
The deficiency of this study was that a prospective
analysis was adopted. Although we set strict inclusion criteria,
there still may be some bias in the inclusion process of patients.
This study only analyzed the short-term efficacy of patients in the
two groups, and the long-term efficacy results still need further
tracking.
In conclusion, endoscopic removal of NP of IVD has
good therapeutic effects in patients with LIDP, and can reduce
inflammation and suppression of immune function with higher safety,
which is worthy of clinical use.
Acknowledgements
Not applicable.
Funding
This study was supported by the Study on
Degenerative Intervertebral Disc of Pulposus and Mesenchymal Stem
Cells Transfected with Injectable Hydrogels Carrying Lentiviruses
of General Program of Natural Science Foundation of Anhui Province
in 2019 (project no. 1908085MC90).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
GX observed the indicators and wrote the manuscript.
XL interpreted and analyzed the patient data. CZ and KZ designed
the study and performed the experiments. ZB and PZ were responsible
for the analysis and discussion of the data. All the authors read
and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Medical Ethics
Committee of The First Affiliated Hospital of Bengbu Medical
College (Bengbu, China). Signed informed consents were obtained
from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sun D, Liu P, Cheng J, Ma Z, Liu J and Qin
T: Correlation between intervertebral disc degeneration, paraspinal
muscle atrophy, and lumbar facet joints degeneration in patients
with lumbar disc herniation. BMC Musculoskelet Disord. 18:1672017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Messner A, Stelzeneder D and Trattnig S,
Welsch GH, Schinhan M, Apprich S, Brix M, Windhager R and Trattnig
S: Does T2 mapping of the posterior annulus fibrosus indicate the
presence of lumbar intervertebral disc herniation? A 3.0 Tesla
magnetic resonance study. Eur Spine J. 26:877–883. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lurie JD, Tosteson TD, Tosteson AN, Zhao
W, Morgan TS, Abdu WA, Herkowitz H and Weinstein JN: Surgical
versus nonoperative treatment for lumbar disc herniation:
Eight-year results for the spine patient outcomes research trial.
Spine. 39:3–16. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Atlas SJ, Keller RB, Wu YA, Deyo RA and
Singer DE: Long-term outcomes of surgical and nonsurgical
management of sciatica secondary to a lumbar disc herniation: 10
year results from the Maine lumbar spine study. Spine. 30:927–935.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Leven D, Passias PG, Errico TJ, Lafage V,
Bianco K, Lee A, Lurie JD, Tosteson TD, Zhao W, Spratt KF, et al:
Risk factors for reoperation in patients treated surgically for
intervertebral disc herniation: A subanalysis of eight-year SPORT
data. J Bone Joint Surg Am. 97:1316–1325. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Huang W, Han Z, Liu J, Yu L and Yu X: Risk
factors for recurrent lumbar disc herniation: A systematic review
and meta-analysis. Medicine (Baltimore). 95:e23782016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Majeed SA, Vikraman CS, Mathew V and S AT:
Comparison of outcomes between conventional lumbar fenestration
discectomy and minimally invasive lumbar discectomy: An
observational study with a minimum 2-year follow-up. J Orthop Surg
Res. 8:342013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mascarenhas AA, Thomas I, Sharma G and
Cherian JJ: Clinical and radiological instability following
standard fenestration discectomy. Indian J Orthop. 43:347–351.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Norton MJ and Ischy ND: Apparatus and
method for minimally invasive surgery. US Patent 9,820,771(P).
Filed on March 3, 2006; issued November 21, 2017.
|
|
10
|
Kim JS, Jung B and Lee SH: Instrumented
minimally invasive spinal-transforaminal lumbar interbody fusion
(MIS-TLIF). Clin Spine Surg. 31:E302–E309. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Phan K and Mobbs RJ: Minimally invasive
versus open laminectomy for lumbar stenosis: A systematic review
and meta-analysis. Spine. 41:E91–E100. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kreiner DS, Hwang SW, Easa JE, Resnick DK,
Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P II, Fernand R,
et al North American Spine Society, : An evidence-based clinical
guideline for the diagnosis and treatment of lumbar disc herniation
with radiculopathy. Spine J. 14:180–191. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gorth DJ, Shapiro IM and Risbud MV:
Transgenic mice overexpressing human TNF-α experience early onset
spontaneous intervertebral disc herniation in the absence of overt
degeneration. Cell Death Dis. 10:72018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vinas-Rios JM, Sanchez-Aguilar M, Medina
Govea FA, Von Beeg-Moreno V and Meyer F; DWG Registry-group, :
Incidence of early postoperative complications requiring surgical
revision for recurrent lumbar disc herniation after spinal surgery:
A retrospective observational study of 9,310 patients from the
German Spine Register. Patient Saf Surg. 12:92018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Regev GJ, Salame K, Behrbalk E, Keynan O
and Lidar Z: Minimally invasive transforaminal, thoracic
microscopic discectomy: Technical report and preliminary results
and complications. Spine J. 12:570–576. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li ZZ, Hou SX, Shang WL, Song KR and Zhao
HL: The strategy and early clinical outcome of full-endoscopic
L5/S1 discectomy through interlaminar approach. Clin Neurol
Neurosurg. 133:40–45. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Choi KC, Kim JS and Park CK: Percutaneous
endoscopic lumbar discectomy as an alternative to open lumbar
microdiscectomy for large lumbar disc herniation. Pain Physician.
19:E291–E300. 2016.PubMed/NCBI
|
|
18
|
Garg B, Nagraja UB and Jayaswal A:
Microendoscopic versus open discectomy for lumbar disc herniation:
A prospective randomised study. J Orthop Surg (Hong Kong).
19:30–34. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen P, Hu Y and Li Z: Percutaneous
endoscopic transforaminal discectomy precedes interlaminar
discectomy in the efficacy and safety for lumbar disc herniation.
Biosci Rep. 39:BSR201818662019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pan L, Zhang P and Yin Q: Comparison of
tissue damages caused by endoscopic lumbar discectomy and
traditional lumbar discectomy: A randomised controlled trial. Int J
Surg. 12:534–537. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Epstein NE: A review of complication rates
for anterior cervical diskectomy and fusion (ACDF). Surg Neurol
Int. 10:102019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chang F, Zhang T, Gao G, Yu C, Liu P, Zuo
G and Huang X: Therapeutic effect of percutaneous endoscopic lumbar
discectomy on lumbar disc herniation and its effect on oxidative
stress in patients with lumbar disc herniation. Exp Ther Med.
15:295–299. 2018.PubMed/NCBI
|
|
23
|
Suri P, Pearson AM, Zhao W, Lurie JD,
Scherer EA, Morgan TS and Weinstein JN: Pain recurrence after
discectomy for symptomatic lumbar disc herniation. Spine.
42:755–763. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Reddi D: Preventing chronic postoperative
pain. Anaesthesia. 71 (Suppl 1):64–71. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lai A, Moon A, Purmessur D, Skovrlj B,
Laudier DM, Winkelstein BA, Cho SK, Hecht AC and Iatridis JC:
Annular puncture with tumor necrosis factor-alpha injection
enhances painful behavior with disc degeneration in vivo. Spine J.
16:420–431. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Brodke DS, Goz V, Lawrence BD, Spiker WR,
Neese A and Hung M: Oswestry Disability Index: A psychometric
analysis with 1,610 patients. Spine J. 17:321–327. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liu SW and Wang XY: Comparison of pain
media and inflammatory factors after percutaneous transforaminal
endoscopic discectomy and traditional fenestration operation
treatment of protrusion of lumbar intervertebral disc. Hainan
Yixueyuan Xuebao. 23:108–111. 2017.(In Chinese).
|
|
28
|
Beilin B, Shavit Y, Trabekin E, Mordashev
B, Mayburd E, Zeidel A and Bessler H: The effects of postoperative
pain management on immune response to surgery. Anesth Analg.
97:822–827. 2003. View Article : Google Scholar : PubMed/NCBI
|