Introduction
The high rate of caesarean section has been a
medical and social problem in China for many years. Since 1985, the
international medical community has always considered the ‘ideal’
rate of cesarean section to be between 10 and 15% (1); the rate of caesarean section in China
is far higher than this level, and in some areas, it is up to 90%
(2). After cesarean section, pain
stimulation can cause a series of pathophysiological changes, which
not only brings great pain to the puerperae but also affects the
functions of the respiratory, digestive, circulatory, endocrine and
immune systems of the puerperae, and produces postoperative
complications (3).
Dexmedetomidine is a highly selective α2 adrenergic
receptor (α2-AR) agonist that is clinically used in sedation
(4). A previous study also found
that postoperative intravenous infusion of dexmedetomidine
hydrochloride can improve the relief of postoperative acute pain
and reduce opioid dosage (5). Recent
studies have shown that dexmedetomidine use, combined with opioid
use, in analgesia after cesarean section can not only reduce the
consumption of analgesic drugs but can also reduce the pressing
times for patient-controlled analgesia, reduce the incidence of
postoperative complications and improve patient satisfaction with
postoperative analgesia (6).
However, previous research has found that the opioid analgesic
effect is influenced by genetic factors (7), and that there is substantial variation
in the effect of drug application between individuals. Therefore,
the study of genetic factors has important clinical significance
for the effect of dexmedetomidine on anesthesia and analgesia in
cesarean section. The α2-AR is a receptor for dexmedetomidine, and
whether its genetic polymorphisms affect the efficacy of
dexmedetomidine is still unclear.
The adrenoceptor alpha 2A gene (ADRA2A)-coded α2-AR
protein is a member of the G protein coupling receptor subfamily
and consists of three highly homologous subtypes, αA, αB and α2C,
which regulate neurotransmitters released by the sympathetic and
adrenergic neurons. These subtypes play an important role in the
regulation of the central nervous system (8). The SNPs were analyzed to determine
their influence on the anesthestic and analgesic effects of
dexmedetomidine in Chinese Han women. From National Center for
Biotechnology Information (NCBI; https://www.ncbi.nlm.nih.gov/snp/) single nucleotide
polymorphism database, it was found that the C/G mutation at
rs1800035 leads to the mutation of Asn amino acid into Lys amino
acid (9), the C/T mutation at
rs201376588 (https://www.ncbi.nlm.nih.gov/snp/rs201376588#variant_details)
leads to the mutation of Arg amino acid into Cys, and the C/T
mutation at rs775887911 (https://www.ncbi.nlm.nih.gov/snp/rs775887911) leads to
the mutation of Pro amino acid into Leu. It is not clear whether
these three types of mutations lead to the alteration of amino acid
sequence and the structural and functional changes of α2-ARs.
The present study aimed to investigate the effect of
ADRA2A rs1800035, rs201376588 and rs775887911 SNPs on
dexmedetomidine, which provides a theoretical basis for improving
the administration of dexmedetomidine.
Materials and methods
General information
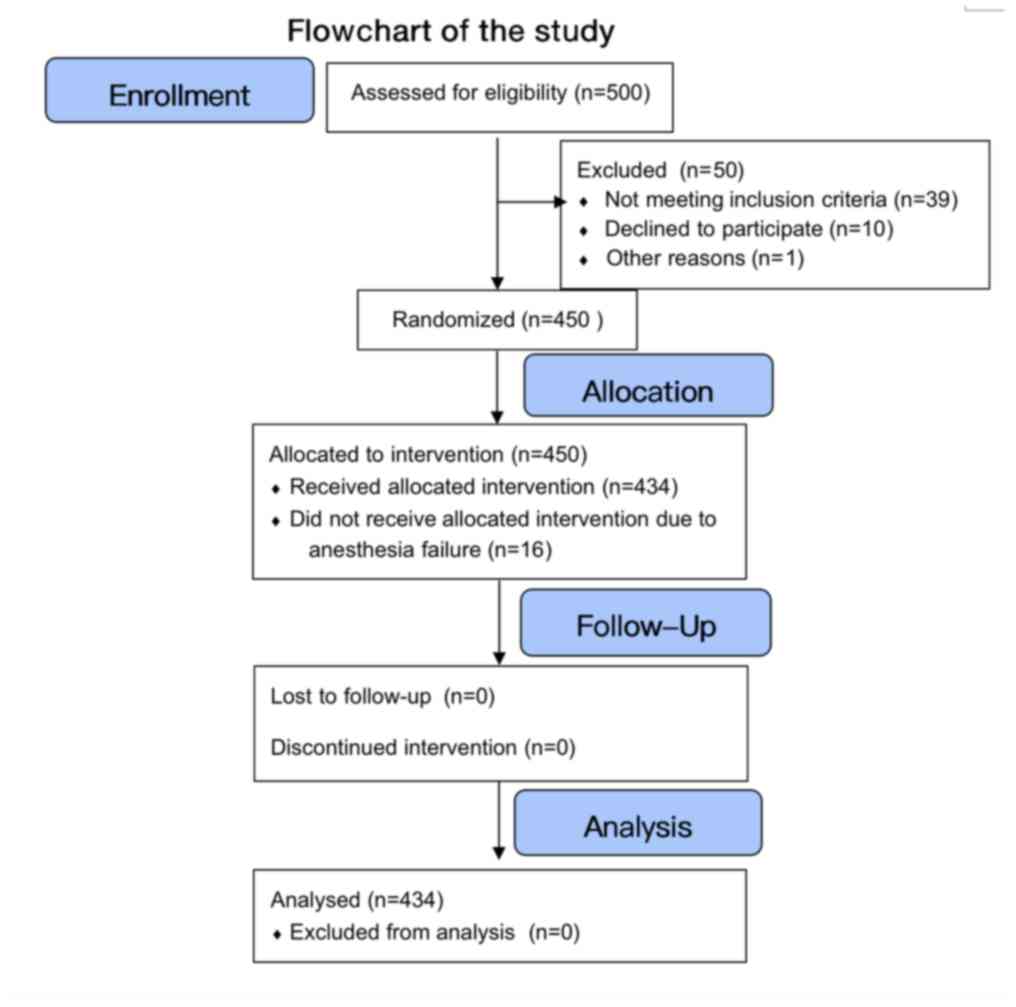
From May 2013 to October 2017, 434 Chinese Han women
who underwent caesarean section under combined spinal epidural
anesthesia in the Tongde Hospital of Zhejiang Province (Zhejiang
province) were selected (Fig. 1),
who were in line with the American Society of Anesthesiologists
grading I-II; mean age, 29.5±3.9 years, range, 20-36 years; body
weight, 58-82 kg; body mass index (BMI) 27.2±3.5 kg/m2
(average BMI, 27.2+3.5 kg/m2); and gestational age,
38-40 weeks. Exclusion criteria were as follows: Congenital heart
and lung disease, spinal canal anesthesia contraindication,
hypertension or gestational hypertension, hyperthyroidism or
hypothyroidism, diabetes or gestational diabetes mellitus. The
present study was approved by the medical ethics committee of the
Tongde Hospital of Zhejiang Province, (Zhejiang, China) and all
subjects provided informed consent.
Methods
The anesthesia used within the present study
consisted of an intrathecal injection of 10 mg bupivacaine and 4 mg
dexmedetomidine. The epidural analgesia was performed at the L2-3
interspace by an 18-gauge Tuohy needle using the method of loss of
resistance to air in the left lateral position. After the epidural
puncture was successful, the epidural puncture needle was used as a
guide. A 25G lumbar puncture needle was inserted, and the arachnoid
was pierced through the epidural puncture needle. The needle core
was withdrawn and the cerebrospinal fluid was discharged from the
needle. A volume of 2-3 ml of 0.5% ropivacaine and 0.5 µg/ml
dexmedetomidine was injected via the spine, and a lumbar puncture
needle was inserted into the epidural catheter via an epidural
needle. The epidural needle was withdrawn, the puncture point was
covered with a sterile gauze, and the catheter was fixed.
Methods of analgesia
Ropivacaine hydrochloride (0.1%) and 0.5 µg/kg
dexmedetomidine hydrochloride were diluted in 0.9% normal saline to
100 ml, and epidural continuous auto-control analgesia was
provided. When the mean arterial pressure of the puerpera was
<60 mmHg, 10 mg ephedrine was injected intravenously, and 0.2 mg
atropine sulfate was injected intravenously at a heart rate (HR)
<50 bpm. Epidural 10 ml of 1% lidocaine was administrated to
rescue if visual analogue score (VAS) was >3 after 30 min of
epidural injection.
Indicators for observation and
evaluation
Maternal basic information including maternal age,
gestational age, height, weight and operation time, was assessed.
When each patient entered the operating room, vital signs were
continuously monitored by an Agilent V24C monitor (Agilent
Technologies, Inc.) before anesthesia and 5, 10 and 30 min after
anesthesia. Mean arterial pressure (MAP), HR and blood oxygen
saturation (SpO2) were monitored in the puerperae after
surgery. A pain threshold (PTh) detector (EP601C PTh detector;
Teaching Equipment Factory of Shanghai East China Normal
University) was used to monitor the PTh and the pain tolerance
threshold (PTTh) of the women before and after anesthesia.
Measurements were taken before administration of the anesthetic and
1 h after administration. The PTh and PTTh were measured by a pain
threshold detector using a microwave current stimulation method,
and the two electrodes were fixed on the deltoid muscle of the left
upper arm 1.5 cm apart. The detector produced a 50 Hz electrical
stimulation with a pulse width of 0.5 msec. The current intensity
gradually increased from 0 to 5 mA. When the pain was first felt,
the measured value was the PTh, and when the pain became
unbearable, the measured value was the PTTh. The degree of pain
caused by cesarean section at 6, 12, 24 and 48 h after the
operation was assessed by the VAS (10,11). The
VAS ranges between 0 and 10; 0 points indicates no pain; a score of
1-3 indicates mild pain; a score of 4-6 indicates moderate pain;
and a score of 7-10 indicates severe pain. The sedation score at 6,
12, 24 and 48 h after the operation was evaluated by the Ramsay
sedation score system (12). Level 1
indicates anxiety or irritability; level 2 indicates that the
patient is cooperative, quiet, and well directed; level 3 means
drowsiness, but responds to instructions; level 4 indicates a quick
response to tapping the brow or strong sound stimulation; level 5
indicates the patient is unresponsive to tapping the brow or strong
sound stimulation; and level 6 indicates that the patient has no
reaction to tapping the brow or strong sound stimulation. A sample
of 4 ml fasting venous blood was taken before the operation and at
6, 12, 24 and 48 h after the operation. After standing for 20 min,
the serum was separated and stored at -20˚C. The stress response of
the patient before anesthesia and 6, 12, 24 and 48 h after surgery
was detected by cortisol (Cor; cat. no. SKGE008B; R&D Systems,
Inc.) and blood glucose (Glu) detection kits (cat. no. ml076792;
Shanghai Enzyme-linked Biotechnology Co., Ltd.). A satisfaction
questionnaire of the analgesic effect was used to investigate the
satisfaction of the puerperae with the analgesic effect, including
‘very satisfied’ (comfort), ‘satisfaction’ (no obvious discomfort),
‘general’ (mild discomfort, but not obvious) and ‘not satisfied’
(with obvious discomfort). The following formula was used:
Satisfaction rate=(very satisfied + satisfaction)/total number of
participants x100%. The side effects of using narcotic analgesics
are well documented (13). The
primary outcome indicators in this study were the PTh, PTTh, VAS
and Ramsay scores. Secondary outcome indicators were Cor and Glu
levels, and maternal satisfaction with cesarean delivery.
SNP locus selection
The drug target predicted by the Kyoto Encyclopedia
of Genes and Genomes (KEGG) Pathway database showed that the target
of dexmedetomidine was the ADRA2A. Based on the prediction of the
influence of ADRA2A single-nucleotide polymorphism (SNP) site
mutations on the protein structure and function in the Ensembl
database (http://asia.ensembl.org/index.html), three loci were
selected (rs1800035, rs20137658 and rs775887911) that had a great
influence on protein structure and function.
Genotyping
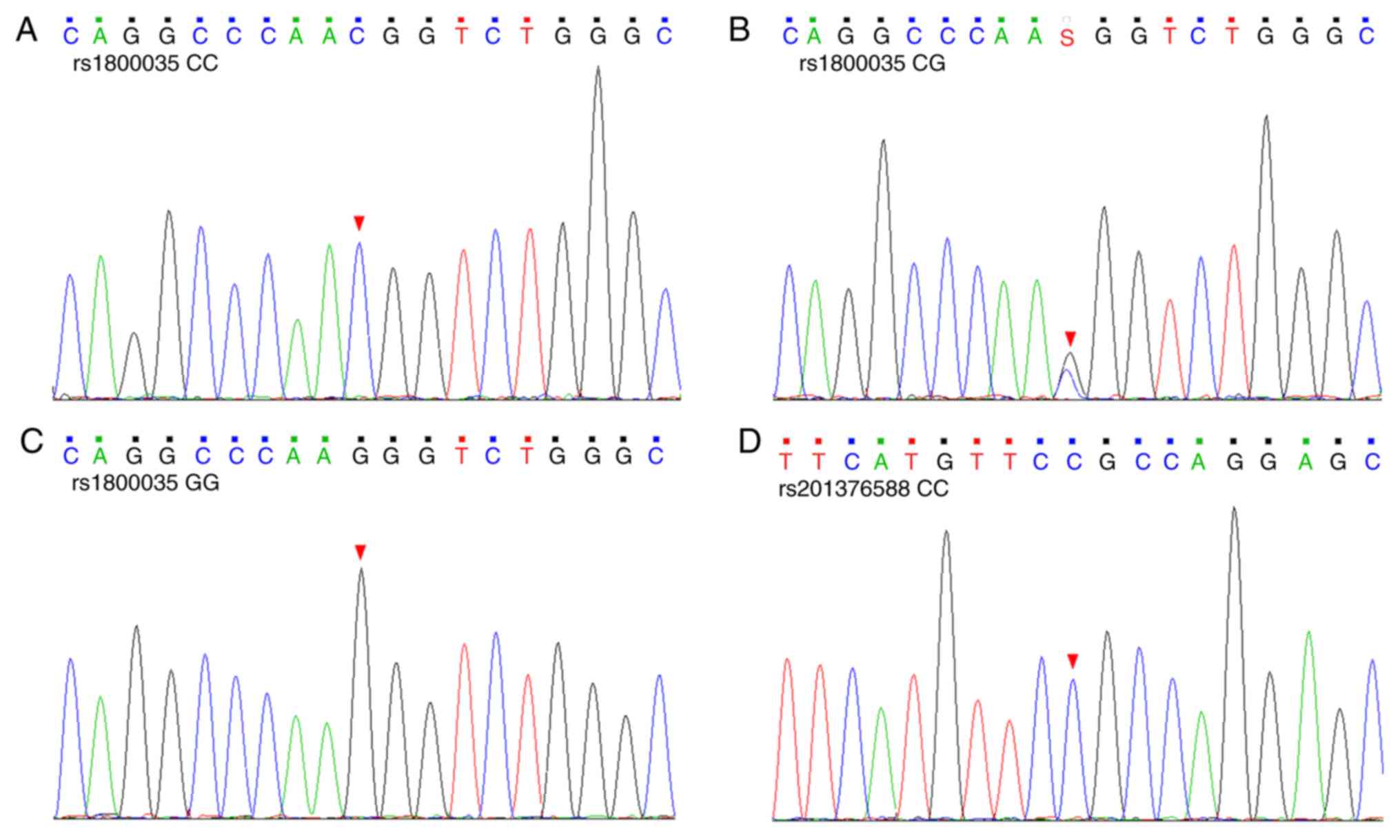
Genomic DNA was extracted from 2 ml of venous blood
from each participant using a QIAamp DSP DNA Blood Mini kit (cat.
no. 51104; Qiagen GmbH). The genotypes of the rs1800035,
rs201376588 and rs775887911 loci were analyzed by PCR/Sanger
sequencing. PCR products were purified after PCR amplification and
then analyzed for each locus genotype by Sanger sequencing
(Fig. 2). The primer sequences for
PCR amplification at the rs1800035 site were as follows: Forward
primer, CCTGGCTTAATTTTCCAGGCT and reverse primer,
GAGTCCTGCCATCGCCTTTA (primer melting temperature (Tm), 59˚C). The
primer sequences for PCR amplification at the rs201376588 site were
as follows: Forward primer, CTGGCAGCAGGCCCAG and reverse primer,
CATGGGCGCAAAGCTGC (Tm, 60˚C). The primer sequences for PCR
amplification at the rs775887911 site were as follows: Forward
primer, CGTTCATGTTCCGCCAGGAG and reverse primer, CCGTTCCAGCTCGCGTT
(Tm, 60˚C).
Haploid analysis and SNP-SNP
interaction analysis
Haploid analysis of the ADRA2A gene at rs1800035,
rs201376588 and rs775887911 was performed using the Haploview 4.2
software (14,15). The degree of linkage is defined by
the R2 value, presented as 0 ≤ R2 ≤ 1; the larger R2, the higher
the linkage degree, the smaller R2, the lower the linkage degree.
SNP-SNP interaction analysis was performed using multi-factor
dimensionality reduction (MDR) (16). In the Fruchterman Rheingold diagram,
‘n %’ between different SNP sites was used to correlate interaction
intensity of between the two factors; the larger the value, the
stronger the interaction between these two SNP sites. The smaller
the distance within the tree diagram, the stronger the interaction
between SNP sites. In contrast, the larger the distance, the weaker
the interaction between the SNPs.
Statistical analysis
Statistical analysis was performed using SPSS 20.0
(IBM Corp.). The categorical data are expressed as (n (%)),
Pearson's χ2 test was used for statistical analysis of
categorical variables. Continuous data are presented as mean ±
standard deviation. The Kruskal-Wallis test was used for
statistical analysis unless otherwise stated. One-way ANOVA was
performed to evaluate the difference between the three genotypes
group followed by Tukey's post hoc tests. Kruskal-Wallis test was
used to analyze the comparison of three discontinuous categorical
variables. P<0.05 was considered to indicate a statistically
significant difference.
Results
Demographic characteristics
A total of 434 Chinese Han women with 434 cases were
eventually included in the study (Fig.
1), aged 20-36 years, with a mean age 29.5±3.9 years, including
the following: 315 cases with a wild type (CC) ADRA2A rs1800035
locus, accounting for 72.6%, and 119 cases of mutants (CG+GG) of
the ADRA2A rs1800035 locus, accounting for 27.4%; 304 cases of a
wild type (CC) ADRA2A rs201376588 locus, accounting for 70.0%, and
130 cases of mutants (CT+TT) of the ADRA2A gene rs201376588 locus,
accounting for 30.0%; 310 cases of a wild type (CC) ADRA2A gene
rs775887911 locus, accounting for 71.4%, and 124 cases of mutants
(CT+TT) of the ADRA2A gene rs775887911 locus, accounting for 28.6%.
The demographic characteristics of the subjects are shown in
Table I. The three SNP loci of the
ADRA2A showed no significant difference in age, BMI, gestational
age or cesarean section operation time (P>0.05).
 | Table IDemographic characteristic parameters
of the subjects. |
Table I
Demographic characteristic parameters
of the subjects.
| SNPs | Age, years | BMI,
kg/m2 | Gestational age,
weeks | Operation time,
min |
|---|
| rs1800035 | | | | |
|
CC
(n=315) | 29.7±3.2 | 27.1±3.4 | 38.5±1.9 | 39.3±7.2 |
|
CG
(n=85) | 29.6±3.7 | 27.1±3.6 | 38.7±1.8 | 39.5±6.7 |
|
GG
(n=34) | 30.2±4.1 | 27.4±3.7 | 39.1±1.1 | 40.2±7.6 |
|
P-value | 0.69 | 0.94 | 0.95 | 0.71 |
| rs201376588 | | | | |
|
CC
(n=304) | 29.5±3.5 | 27.5±3.6 | 38.6±1.8 | 39.5±6.8 |
|
CT
(n=87) | 29.8±3.8 | 27.3±3.4 | 38.9±1.7 | 39.8±7.4 |
|
TT
(n=43) | 30.1±3.9 | 27.6±3.2 | 39.2±1.0 | 40.3±7.8 |
|
P-value | 0.85 | 0.93 | 0.77 | 0.90 |
| rs775887911 | | | | |
|
CC
(n=310) | 28.9±3.5 | 27.4±3.4 | 38.6±1.9 | 39.6±6.5 |
|
CT
(n=88) | 29.7±3.8 | 27.6±3.4 | 38.8±1.0 | 39.4±7.4 |
|
TT
(n=36) | 30.3±4.3 | 27.4±3.8 | 39.1±1.2 | 39.9±8.1 |
|
P-value | 0.66 | 0.76 | 0.80 | 0.75 |
Association between SNPs, PTh and
PTTh
Results of the PTh and PTTh of subjects with
different genotypes of the ADRA2A at rs1800035, rs201376588 and
rs775887911 loci, at different administration times, are shown in
Table II. There was no significant
difference between PTh and PTTh for each SNP locus before
anesthesia (P>0.05). After anesthesia, one-way ANOVA results
showed that the PTh and PTTh of all SNP site wild type caesarean
section puerperae were higher than those of the mutant cesarean
section puerperae. This was found to be statistically significant
(P<0.05).
 | Table IIComparison of pain threshold and pain
tolerance threshold at different time points. |
Table II
Comparison of pain threshold and pain
tolerance threshold at different time points.
| | PTh, mA | PTTh, mA |
|---|
| SNPs | Pre-anesthesia |
Post-anesthesia | Pre-anesthesia |
Post-anesthesia |
|---|
| rs1800035 | | | | |
|
CC
(n=315) | 1.5±0.4 | 1.7±0.5 | 2.3±0.5 | 2.7±0.5 |
|
CG
(n=85) | 1.5±0.5 | 1.6±0.4 | 2.4±0.4 | 2.5±0.6 |
|
GG
(n=34) | 1.5±0.4 | 1.4±0.6 | 2.3±0.6 | 2.4±0.4 |
|
P-valuea | 0.82 | <0.01 | 0.78 | 0.02 |
| rs201376588 | | | | |
|
CC
(n=304) | 1.5±0.5 | 1.7±0.6 | 2.3±0.5 | 2.7±0.4 |
|
CT
(n=87) | 1.5±0.4 | 1.5±0.4 | 2.4±0.4 | 2.5±0.3 |
|
TT
(n=43) | 1.5±0.6 | 1.5±0.5 | 2.4±0.5 | 2.4±0.4 |
|
P-valuea | 0.87 | 0.02 | 0.75 | 0.02 |
| rs775887911 | | | | |
|
CC
(n=310) | 1.5±0.5 | 1.7±0.5 | 2.4±0.4 | 2.7±0.3 |
|
CT
(n=88) | 1.5±0.6 | 1.6±0.5 | 2.4±0.3 | 2.5±0.4 |
|
TT
(n=36) | 1.5±0.4 | 1.4±0.6 | 2.3±0.4 | 2.4±0.5 |
|
P-valuea | 0.90 | 0.01 | 0.54 | 0.01 |
Hemodynamic changes in women during
anesthesia for cesarean section
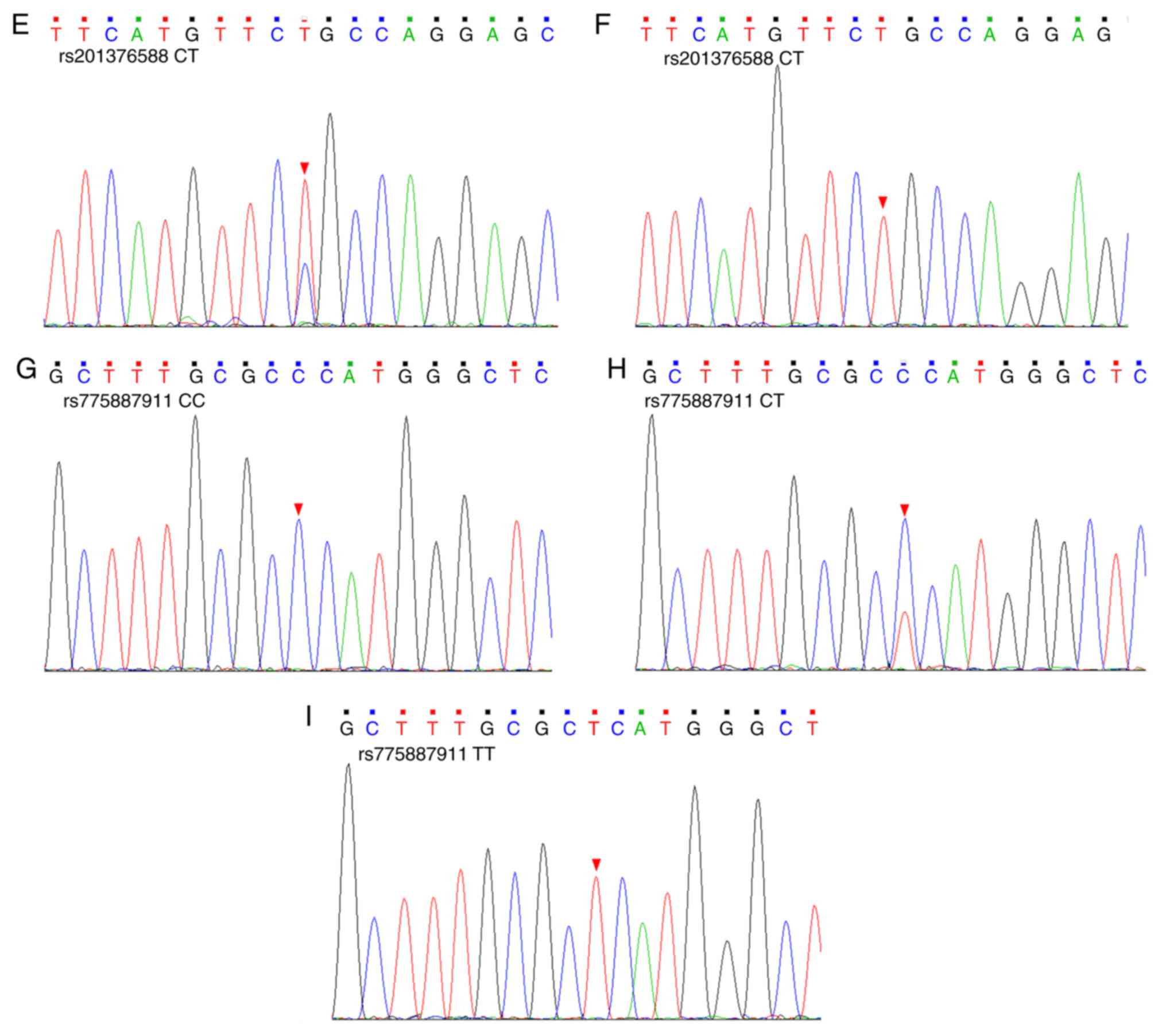
Changes in the hemodynamic indexes of the women
during the anesthesia are shown in Fig.
3. After anesthesia, the MAP of the women showed a downward
trend, and the HR showed an upward trend. The MAP and HR levels at
different time points were statistically significant, as analyzed
by one-way ANOVA (P<0.05). The changes in SpO2 level
before and after anesthesia were not significant (P>0.05). There
was no significant difference in MAP, HR or SpO2 between
different genotypes at the same time point after anesthesia
(P>0.05).
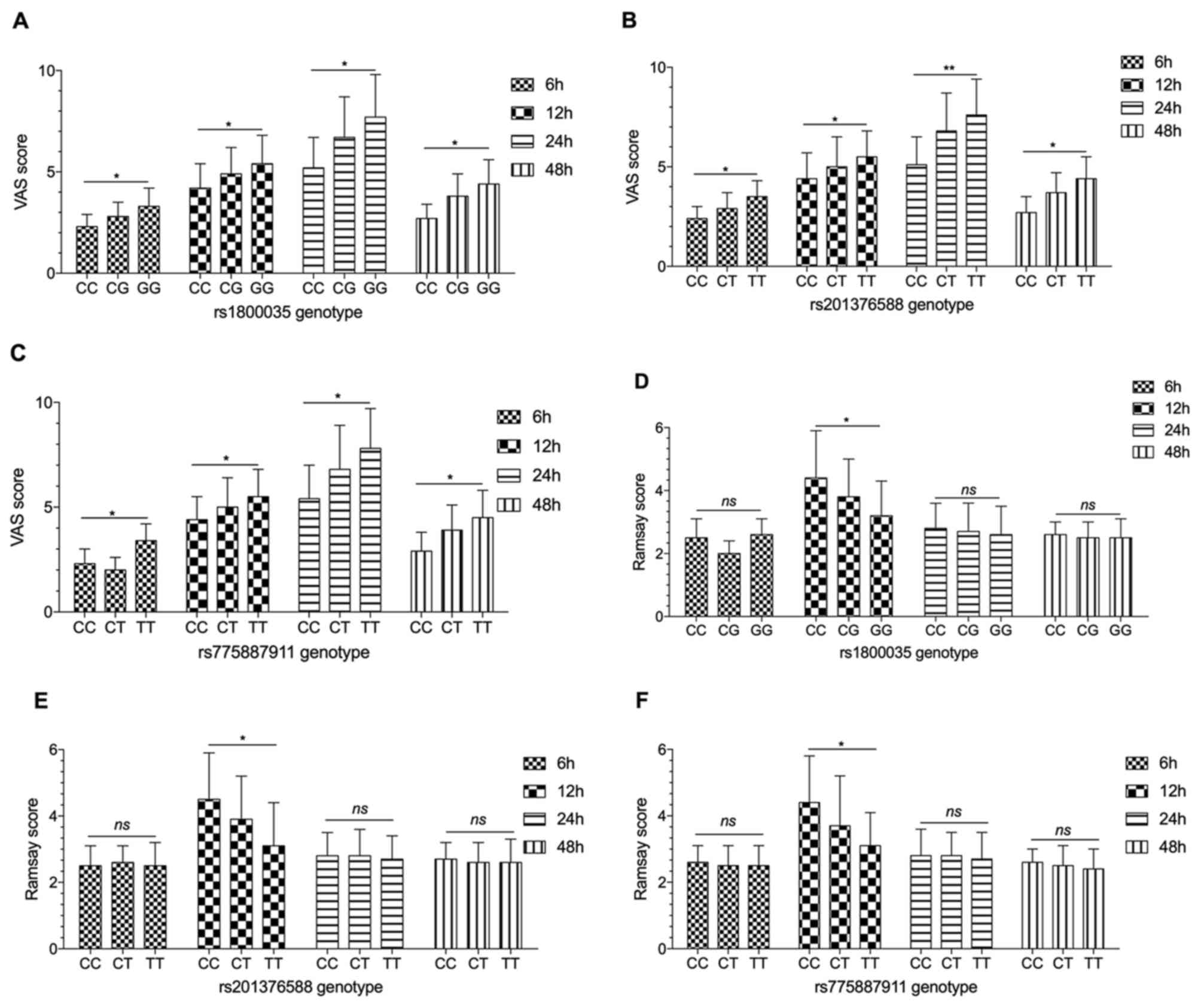
VAS and Ramsay scores
Results of VAS and Ramsay scores at 6, 12, 24 and 48
h after the operation are shown in Fig.
4. The VAS scores of the puerperae tended to increase at first
and then decrease, with the highest level observed at 24 h after
the operation, followed by a decrease at 48 h. The Ramsay score of
the puerperae also showed a trend of first increasing and
decreasing, reaching a peak at 12 h and decreasing for the
remainder of the observation period. The results of comparative
analysis of the genotypes of SNPs showed that the VAS score of
wild-type puerperae was lower than that of puerperae with mutations
at the same time (P<0.05). However, there was a significant
difference in Ramsay score among all genotypes of the puerperae 12
h after the operation, and the Ramsay score of the wild-type
(rs1800035 genotype: CC; rs201376588 genotype: CC; rs775887911
genotype: CC) puerperae was significantly higher compared with that
of the mutant genotypes (rs1800035 genotype: CG/GG; rs201376588
genotype: CC/TT; rs775887911 genotype: CT/TT; P<0.05).
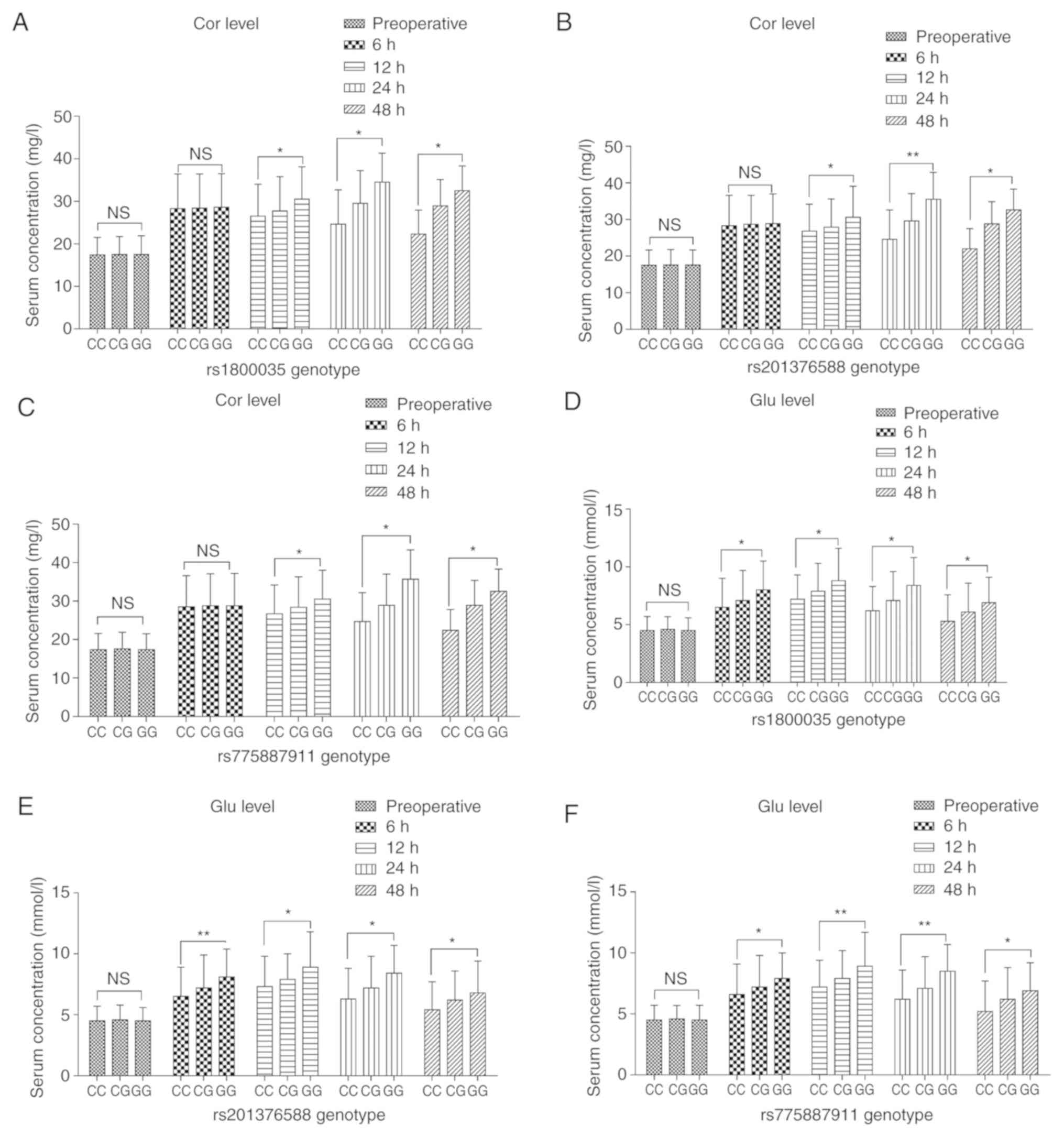
Comparison of stress response
index
Puerperae postoperative Cor and Glu levels at 6, 12,
24, and 48 h are shown in Fig. 5.
The postoperative levels of Cor and Glu were higher than that
before the operation, and the difference was statistically
significant (P<0.05). At 12, 24 and 48 h after the operation,
there was a significant difference between the Cor and Glu levels
for different genotypes of the rs1800035, rs201376588 and
rs775887911 ADRA2A loci. Mothers with mutations had higher levels
of Cor and Glu than wild-type mothers (P<0.05).
Investigation of surgical
satisfaction
Results of the investigation into the satisfaction
of puerperae with cesarean section are shown in Table III. The satisfaction degree of
puerperae after cesarean section was 88.9% (386/434), of which 204
puerperae were very satisfied (47%), 182 were satisfied (41.9%),
and 4 were not satisfied (0.9%). The comparison of the genotypic
puerperae showed that the satisfaction of the wild type puerperae
was higher than the mutant puerperae (P<0.05).
 | Table IIIComparison of the satisfaction of
puerperae with cesarean section by genotype. |
Table III
Comparison of the satisfaction of
puerperae with cesarean section by genotype.
| SNPs | Very satisfied, n
(%) | Satisfied, n
(%) | Normal, n (%) | Not satisfied, n
(%) | Satisfaction rate,
% |
|---|
| rs1800035 | | | | | |
|
CC
(n=315) | 172 (54.6) | 126 (40.0) | 16 (5.1) | 1 (0.3) | 94.6% |
|
CG
(n=85) | 26 (30.6) | 42 (49.4) | 16 (18.8) | 1 (1.2) | 80.0% |
|
GG
(n=34) | 6 (17.6) | 14 (41.2) | 12 (35.3) | 2 (5.9) | 58.8% |
|
P-valuea | | | | | <0.01 |
| rs201376588 | | | | | |
|
CC
(n=304) | 157 (51.6) | 121 (39.8) | 24 (7.9) | 2 (0.7) | 91.5% |
|
CT
(n=87) | 40 (46.0) | 32 (36.8) | 14 (16.1) | 1 (1.1) | 82.8% |
|
TT
(n=43) | 7 (16.3) | 29 (67.4) | 6 (14.0) | 1 (2.3) | 83.7% |
|
P-valuea | | | | | 0.04 |
| rs775887911 | | | | | |
|
CC
(n=310) | 169 (54.5) | 118 (38.1) | 21 (6.8) | 2 (0.6) | 92.6% |
|
CT
(n=88) | 25 (28.4) | 44 (50.0) | 18 (20.5) | 1 (1.1) | 78.4% |
|
TT
(n=36) | 10 (27.8) | 20 (55.6) | 5 (13.9) | 1 (2.8) | 83.3% |
|
P-valuea | | | | | <0.01 |
Postoperative adverse reaction
Adverse reactions after cesarean section in this
study included nausea (30 cases), vomiting (22 cases), chills (31
cases) and pruritus (12 cases), as shown in Table IV. Kruskal-Wallis test showed that
there was no significant difference in postoperative adverse
reactions between the different genotypes (P>0.05).
 | Table IVComparison of postoperative adverse
effects of various genotypic puerperae. |
Table IV
Comparison of postoperative adverse
effects of various genotypic puerperae.
| SNPs | Nausea | Vomiting | Chills | Pruritus |
|---|
| rs1800035 | | | | |
|
CC
(n=315) | 23 | 12 | 22 | 10 |
|
CG
(n=85) | 5 | 8 | 6 | 2 |
|
GG
(n=34) | 2 | 2 | 3 | 0 |
|
P-valuea | 0.88 | 0.11 | 0.92 | 0.55 |
| rs201376588 | | | | |
|
CC
(n=304) | 22 | 14 | 23 | 9 |
|
CT
(n=87) | 5 | 6 | 5 | 3 |
|
TT
(n=43) | 3 | 2 | 3 | 0 |
|
P-valuea | 0.89 | 0.69 | 0.84 | 0.45 |
| rs775887911 | | | | |
|
CC
(n=310) | 23 | 13 | 21 | 9 |
|
CT
(n=88) | 6 | 6 | 6 | 2 |
|
TT
(n=36) | 1 | 4 | 4 | 1 |
|
P-valuea | 0.45 | 0.29 | 0.85 | 0.92 |
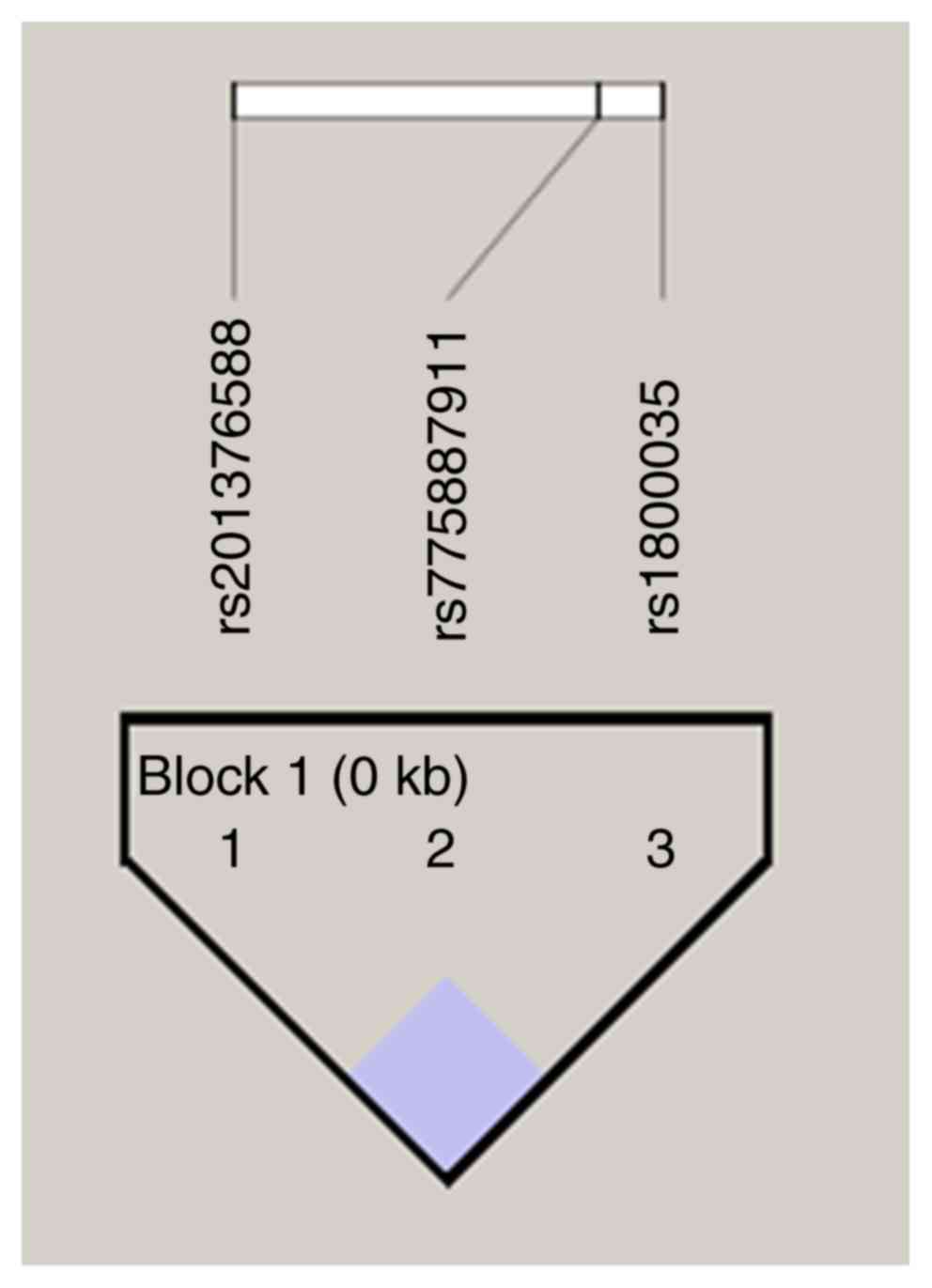
Linkage disequilibrium analysis of
rs1800035, rs201376588 and rs775887911 loci of the ADRA2A
Linkage disequilibrium of the rs1800035, rs201376588
and rs775887911 loci of the ADRA2A was analyzed by Haploview 4.2,
and the results showed that r2=0.2 (Fig. 6). In addition, multifactorial
dimensionality reduction (MDR) was used to analyze the interaction
of rs1800035, rs201376588 and rs775887911 loci of the ADRA2A. The
results showed that there was a strong interaction between
rs1800035 and rs775887911 loci (Fig.
7).
Discussion
The present study analyzed the effects of ADRA2A
rs1800035, rs201376588 and rs775887911 SNPs on dexmedetomidine
anesthesia and analgesia in Chinese Han women. The results showed
that the mutations of rs1800035, rs201376588 and rs775887911 in the
ADRA2A reduced the anesthetic and analgesic effect of
dexmedetomidine after cesarean section in women of the Chinese Han
dynasty. The postoperative analgesia of mutant maternal women may
require more doses of analgesic drugs, but the mutation did not
affect the safety of the medication.
The pain after cesarean section is most severe at 48
h post-surgery, and is mainly somatic pain caused by the abdominal
surgery incision and uterine contraction pain. The two pain
pathways in the spinal cord and above are different (17); the pain caused by uterine contraction
is visceral pain, mainly transmitted by the sympathetic afferent
fibers into the cervix and lower abdomen through the plexus into
the lumbar sympathetic chain and then into the spinal dorsal horn
via the T10, 11, 12 and L1 segments (18); the pain in the abdominal incision is
located at the incision and passes into the spinal dorsal horn
through the spinal nerve of the T10-L1 segment (19). Pain after cesarean section will lead
to maternal sympathetic excitement and increased secretion of
catecholamines and metabolic hormones, thereby affecting the
maternal digestive system function and physical recovery; this is a
main reason for the negative emotions exhibited by new mothers,
affecting their lactation (20,21).
Morphine is a classical epidural analgesic that enters the
cerebrospinal fluid and binds to opiate receptors in the glia of
the dorsal horn of the spinal cord, producing a potent,
long-lasting analgesic effect (22).
However, studies have shown that morphine can excite µ receptors,
resulting in nausea, vomiting, pruritus and other adverse reactions
(23).
In this study, dexmedetomidine hydrochloride
combined with ropivacaine was used for continuous epidural
auto-control analgesia after cesarean section surgery.
Dexmedetomidine hydrochloride is a new type of highly selective
α2-AR agonist. Its main mechanism is that it acts on presynaptic
α2-ARs of spinal cord C class or Aδ nerve fibers, reducing the
release of nerve fiber neurotransmitters, and thus nociceptive
signals cannot be transmitted between neurons, thereby achieving
the effect of analgesia (24). At
the same time, dexmedetomidine can also act on the postsynaptic
membrane α2-ARs in the posterior horn neurons of the spinal cord,
causing hyperpolarization of the neurons in the posterior horn of
the spinal cord. The nociceptive signals thus cannot be transmitted
in the nerve fibers, resulting in antinociceptive effects (25). In addition, dexmedetomidine also has
high liposolubility and can be absorbed from the bloodstream
through the blood-brain barrier into the human central nervous
system locus coeruleus to produce a calming effect, to eliminate
anxiety, tension and fear caused by pain (25). Some studies have shown that
dexmedetomidine has a synergistic effect with other local
anesthetic drugs, which can enhance the analgesic effect and reduce
the use of local anesthetic drugs, while dexmedetomidine can also
be effective in inhibiting postoperative chills and reducing
nausea, vomiting, pruritus and other adverse reactions (26). However, there are often some
differences in the effect of the same dose of the drug in clinical
application (27). The existence of
variability in drug response between individuals has long been
known (28). In drug therapy,
susceptibility to toxic or inadequately treated individuals is
important. Genetic polymorphisms of genes responsible for drug
reactions are expected to be used to track differences between
individuals (29). The influence of
genetic factors is not clear. After searching the KEGG database,
the target of dexmedetomidine was determined to be the ADRA2A, and
the effect of SNPs of this gene on the analgesic effect of
dexmedetomidine was analyzed. Due to technical limitations, only
three potential SNP loci that affected the structure and function
of the α2-AR protein were screened, namely, rs1800035, rs201376588
and rs775887911.
There were no significant differences for age,
gestational age, BMI, operation time and all of the genotypes of
SNPs of the subjects enrolled in this study, which precluded the
interference of these factors. Nie et al (30) showed that intravenous injections with
dexmedetomidine at an initial stage after delivery can increase
maternal PTh and PTTh in cesarean section patients, consistent with
the results of the present study. The present study compared the
PTh and PTTh values of ADRA2A rs1800035, rs201376588 and
rs775887911 genotypes at different times after administration of
analgesia.
Inflammatory reactions induced by traumatic
stimulation after cesarean section can lead to inflammatory
mediator release. Without direct analgesia, this can also cause
maternal vasodilatation, tissue edema, an increase in the
sensitivities of the effector and a decrease in pain threshold,
which leads to hyperalgesia (31).
From the results of the present study, it can be seen that women
who are wild-type at the rs1800035, rs201376588 and rs775887911
loci of the ADRA2A have a higher pain threshold than mutant
puerperae. Since obviously mutant puerperae are more sensitive to
pain, these types of patients may need higher or additional doses
of drugs for anesthesia and analgesia. In addition, the hemodynamic
parameters of post-anesthesia puerperae had a downward MAP trend,
and their HR showed an upward trend, which may be due to
hypotension caused by sympathetic nerve blocks during anesthesia,
or possibly due to a slightly higher dose of drug. There was no
significant change in the level of SpO2, suggesting that
respiratory inhibition was not produced under the dosage of the
drug in this study. Similarly, the analysis results of the
hemodynamic level between different locus genotypes showed no
significant difference in the level of MAP, HR or SpO2
at the same time point after anesthesia, indicating that there was
no significant association between the rs1800035, rs201376588, and
rs775887911 loci SNPs of the ADRA2A and the level of hemodynamics
of the puerperae during the anesthesia. We speculate that the
differences between the different genotypes of puerperae may have
been reduced by compensatory, rehydration and vasoconstrictor
drugs, but this needs to be confirmed.
Dexmedetomidine has a strong postoperative analgesic
effect. It can be seen from the results of this study that the VAS
score of puerperae first increased and then decreased during the
observed timeframe after the operation, with the highest level at
24 h post-surgery. Our analysis suggests that dexmedetomidine
inhibits the transmission of pain information by entering spinal
α2-ARs through spinal pinholes and diffusion. The Ramsay score of
puerperae during the observed timeframe after surgery also showed a
trend of first rising and then decreasing, with the highest level
at 12 h after the operation, followed by a decline up to the last
observation at 48 h. It is hypothesized that dexmedetomidine exerts
a sedative effect by the direct action of cerebrospinal fluid on
locus coeruleus α2-ARs. A previous study (32) found that the ADRA2A C1291C, C1291G
and G1291G sites carrying variant genotypes had higher bispectral
index scores and Ramsay sedation scores, indicating a longer time
to falling asleep. It has been reported that that the ADRA2A-1291
C-> G polymorphism is associated with abnormal cortisol response
to dexamethasone, elevated glucose levels and increased diastolic
blood pressure. Pathophysiology may involve a change in the density
of α2A-ARs, which makes the
sympathetic-hypothalamic-pituitary-adrenal system unstable in those
with genetic susceptibility in the ADRA2A promoter (33). Another study found that the
ADRA2A-1291C/G SNP is associated with the efficacy of
methylphenidate (MPH) in the treatment of attention
deficit/hyperactivity disorder in children and adolescents in
Taiwan. Reactive subjects carrying the homozygous-1291G allele are
more likely to respond better to MPH therapy, indicating that the
-1191C/G SNP is very sensitive to MPH (34). In addition, as seen from the results
of the present study, the VAS score of wild-type puerperae was
lower than the mutant puerperae at the same time after surgery,
while the Ramsay scores of wild-type puerperae 12 h after surgery
were significantly higher than the mutant puerperae, indicating
that wild-type puerperae are more sensitive to dexmedetomidine than
mutant puerperae, probably because genetic mutations alter the
structure and/or function of the protein to weaken the interaction
between dexmedetomidine and α2-ARs. It is also possible that this
SNP site mutation affects protein expression levels. However, there
are limited studies on the effects of this SNP site mutation on the
structure and function of α2-ARs, and further research is needed.
However, according to the results of sequence analysis, the C>G
mutation at rs1800035 will cause the Asn amino acid to be mutated
into a Lys amino acid, from a neutral amino acid to a basic amino
acid. The C>T mutation at rs201376588 leads to the mutation of
Arg amino acid to Cys, from basic amino acid to neutral amino acid,
and the C>T mutation at rs775887911 leads to the mutation of Pro
amino acid to Leu, both of which are neutral amino acids. These
types of mutations have changed the amino acid sequence. It is
unclear whether it causes changes in protein structure. However,
from the results of the present study, it may be speculated that
the changes in these amino acid sequences affect the structure and
function of α2-ARs. The postoperative maternal Cor and Glu levels
were higher than the preoperative levels, which is also due to the
normal physiological trauma caused by surgery. In addition, this
study found that the levels of Cor and Glu of the mutant puerperae
were higher than that of the wild-type puerperae at the same time
after the operation, indicating that the stress response of mutant
puerperae is stronger than that of wild-type mothers, and puerperae
with a mutation in the locus are more sensitive to the stress
reaction caused by surgical trauma. The specific mechanism needs
further study. Furthermore, the satisfaction degree of wild-type
puerperae with postoperative analgesia was higher than that of
mutant puerperae, which also confirms that the mutant puerperae are
less sensitive to the dexmedetomidine than the wild type.
Fortunately, based on the results of this study, the mutations did
not affect the adverse reactions produced by dexmedetomidine.
There are limitations with this study. Due to
technical limitations, the concentration and receptor density of
dexmedetomidine was not detected in this study. In future studies,
we plan to analyze the concentration of dexmedetomidine by means of
mass spectrometry. An in vitro study model to study the
density of its receptors will be designed to analyze the
relationship between ADRA2A polymorphisms on concentrations of
dexmedetomidine and receptor densities. In addition, the
association between anesthetic analgesic effects and SNPs at
different dexmedetomidine doses was not explored, which is also one
of the focuses of further research.
It can be concluded from the results of this study
that the mutation of the ADRA2A at the rs1800035, rs201376588 and
rs775887911 loci can reduce the anesthetic and analgesic effect on
Chinese Han cesarean section puerperae; for postoperative
analgesia, they may require more anesthetics, but the gene
mutations at those SNPs do not affect drug safety.
Acknowledgements
Not applicable.
Funding
The present study was supported by grants from
Medical Health Science and Technology Program of Zhejiang Province
(grant no. 2018KY323).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZMF and DDW designed the study. ZMF, BWH, TTM and
QDW performed the data collection. ZMF, BWH and TTM analyzed and
interpreted the data. ZMF drafted the manuscript and DDW revised
the manuscript.
Ethics approval and consent to
participate
This study was approved by the medical ethics
committee of Tongde Hospital of Zhejiang Province hospital
(Zhejiang, China), and all women provided informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Betran AP, Torloni MR, Zhang JJ and
Gülmezoglu AM: WHO Working Group on Caesarean Section: WHO
statement on caesarean section rates. BJOG. 123:667–670.
2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Liu Xiao Jing JG and Yan Y: Analysis of
cesarean section rate and indication of cesarean section in 10
years. Maternal Child Health Care China. 30:551–553. 2015.
|
|
3
|
Snijder CA, Cornette JM, Hop WC, Kruip MJ
and Duvekot JJ: Thrombophylaxis and bleeding complications after
cesarean section. Acta Obstet Gynecol Scand. 91:560–565.
2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Blaudszun G, Lysakowski C, Elia N and
Tramèr MR: Effect of perioperative systemic α2 agonists on
postoperative morphine consumption and pain intensity: Systematic
review and meta-analysis of randomized controlled trials.
Anesthesiology. 116:1312–1322. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Unlugenc H, Gunduz M, Guler T, Yagmur O
and Isik G: The effect of pre-anaesthetic administration of
intravenous dexmedetomidine on postoperative pain in patients
receiving patient-controlled morphine. Eur J Anaesthesiol.
22:386–391. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Qi X, Chen D, Li G, Huang X and Li Y, Wang
X and Li Y: Comparison of intrathecal dexmedetomidine with morphine
as adjuvants in cesarean sections. Biol Pharm Bull. 39:1455–1460.
2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pettersson FD, Grönbladh A, Nyberg F,
Sundström-Poromaa I and Åkerud H: The A118G single-nucleotide
polymorphism of human µ-opioid receptor gene and use of labor
analgesia. Reprod Sci. 19:962–967. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tian WN, Duzic E, Lanier SM and Deth RC:
Determinants of alpha 2-adrenergic receptor activation of G
proteins: Evidence for a precoupled receptor/G protein state. Mol
Pharmacol. 45:524–531. 1994.PubMed/NCBI
|
|
9
|
Kohli U, Muszkat M, Sofowora GG, Harris
PA, Friedman EA, Dupont WD, Scheinin M, Wood AJ, Stein CM and
Kurnik D: Effects of variation in the human alpha2A- and
alpha2C-adrenoceptor genes on cognitive tasks and pain perception.
Eur J Pain. 14:154–159. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Farshchi A and Ghiasi G: Comparison the
analgesic effects of single dose administration of tramadol or
piroxicam on postoperative pain after cesarean delivery. Acta Med
Iran. 48:148–153. 2010.PubMed/NCBI
|
|
11
|
Kelly AM: The minimum clinically
significant difference in visual analogue scale pain score does not
differ with severity of pain. Emerg Med J. 18:205–207.
2001.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Rasheed AM, Amirah MF, Abdallah M, P J P,
Issa M and Alharthy A: Ramsay sedation scale and richmond agitation
sedation scale: A Cross-sectional study. Dimens Crit Care Nurs.
38:90–95. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Camilleri M, Lembo A and Katzka DA:
Opioids in gastroenterology: Treating adverse effects and creating
therapeutic benefits. Clin Gastroenterol Hepatol. 15:1338–1349.
2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chon J, Hong JH, Kim J, Han YJ, Lee BW,
Kim SC, Kim DH, Yoo SD, Kim HS and Yun DH: Association between BH3
interacting domain death agonist (BID) gene polymorphism and
ossification of the posterior longitudinal ligament in Korean
population. Mol Biol Rep. 41:895–899. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lv Y, Jia C, Jiang A, Zhang H, Wang Y, Liu
F, Yang L, Sun Y, Lv R and Song X: Analysis of association between
MGMT and p53 gene single nucleotide polymorphisms and laryngeal
cancer. Anticancer Res. 37:4399–4403. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yang CH, Chuang LY and Lin YD:
Multiobjective differential evolution-based multifactor
dimensionality reduction for detecting gene-gene interactions. Sci
Rep. 7(12869)2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lavand'homme P: Postcesarean analgesia:
Effective strategies and association with chronic pain. Curr Opin
Anaesthesiol. 19:244–248. 2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zwissler B: Regional anesthesia and
analgesia for labor and delivery. N Engl J Med. 348:1818–1820.
2003.PubMed/NCBI
|
|
19
|
McDonnell JG, O'Donnell BD, Farrell T,
Gough N, Tuite D, Power C and Laffey JG: Transversus abdominis
plane block: A cadaveric and radiological evaluation. Reg Anesth
Pain Med. 32:399–404. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Niklasson B, Georgsson Öhman S, Segerdahl
M and Blanck A: Risk factors for persistent pain and its influence
on maternal wellbeing after cesarean section. Acta Obstet Gynecol
Scand. 94:622–628. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Borges NC, Pereira LV, de Moura LA, Silva
TC and Pedroso CF: Predictors for moderate to severe acute
postoperative pain after cesarean section. Pain Res Manag.
2016(5783817)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Stavropoulou E, Balkamou XA, Giannaka F,
Papadopoulos G, Papadopoulos K and Stamatopoulos G: 303:
Opiod-induced adverse reactions of intravenous patient controlled
analgesia: Comparison of morphine and fentanyl for acute
postoperative analgesia. Regional Anesthesia Pain Med. 33 (Suppl
1)(e166)2008. View Article : Google Scholar
|
|
23
|
Chan K, Brodsky M, Davis T, Franklin S,
Inturrisi CE and Yoburn BC: The effect of the irreversible
mu-opioid receptor antagonist clocinnamox on morphine potency,
receptor binding and receptor mRNA. Eur J Pharmacol. 287:135–143.
1995.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Dawson C, Ma D, Chow A and Maze M:
Dexmedetomidine enhances analgesic action of nitrous oxide:
Mechanisms of action. Anesthesiology. 100:894–904. 2004.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Afonso J and Reis F: Dexmedetomidine:
Current role in anesthesia and intensive care. Rev Bras Anestesiol.
62:118–133. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ren C, Chi M, Zhang Y, Zhang Z, Qi F and
Liu Z: Dexmedetomidine in postoperative analgesia in patients
undergoing hysterectomy: A CONSORT-prospective, randomized,
controlled trial. Medicine (Baltimore). 94(e1348)2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Marto N, Morello J, Monteiro EC and
Pereira SA: Implications of sulfotransferase activity in
interindividual variability in drug response: Clinical perspective
on current knowledge. Drug Metab Rev. 49:357–371. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lim MH, Kim JW, Song EY, Kim TH, Park TW,
Lee HJ, Paik KC and Kim HW: COMT gene polymorphism association and
drug response in Tourette syndrome. Psychiatr Genet.
19(158)2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zastrozhin MS, Brodyansky VM, Skryabin VY,
Grishina EA, Ivashchenko DV, Ryzhikova KA, Savchenko LM, Kibitov
AO, Bryun EA and Sychev DA: Pharmacodynamic genetic polymorphisms
affect adverse drug reactions of haloperidol in patients with
alcohol-use disorder. Pharmgenomics Pers Med. 10:209–215.
2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Nie Y, Liu Y, Luo Q and Huang S: Effect of
dexmedetomidine combined with sufentanil for post-caesarean section
intravenous analgesia: A randomised, placebo-controlled study. Eur
J Anaesthesiol. 31:197–203. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Solca M: Acute pain management: Unmet
needs and new advances in pain management. Eur J Anaesthesiol
Suppl. 25:3–10. 2002.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yagar S, Yavaş S and Karahalil B: The role
of the ADRA2A C1291G genetic polymorphism in response to
dexmedetomidine on patients undergoing coronary artery surgery. Mol
Biol Rep. 38:3383–3391. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Rosmond R, Bouchard C and Björntorp P: A
C-1291G polymorphism in the alpha2A-adrenergic receptor gene
(ADRA2A) promoter is associated with cortisol escape from
dexamethasone and elevated glucose levels. J Intern Med.
251:252–257. 2002.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Huang HC, Wu LS, Yu SC, Wu BJ, Lua AC, Lee
SM and Liu CZ: The alpha-2A adrenergic receptor gene-1291C/G single
nucleotide polymorphism is associated with the efficacy of
methylphenidate in treating Taiwanese children and adolescents with
attention-deficit hyperactivity disorder. Psychiatry Investig.
15:306–312. 2018.PubMed/NCBI View Article : Google Scholar
|