Introduction
In numerous clinical situations, including cardiac,
pulmonary and thoracic surgeries, one-lung ventilation (OLV) is
required to facilitate visibility in surgical procedures; the
management of OLV remains a challenge in the practice of thoracic
anesthesia. Double-lumen tube (DLT) is the most commonly used
device by the majority of anesthesiologists for OLV in thoracic
surgeries (1,2); however, DLTs may be difficult to place
in patients with restricted airways due to their larger diameter
and distal curvature, and are more rigid than single-lumen tubes
(SLTs) (3). Bronchial blockers (BBs)
are an alternative to DLTs (4);
however, BBs have numerous disadvantages, including increased
duration of application (5) and
collapse of the non-ventilated lung due to smaller lumen size
(6).
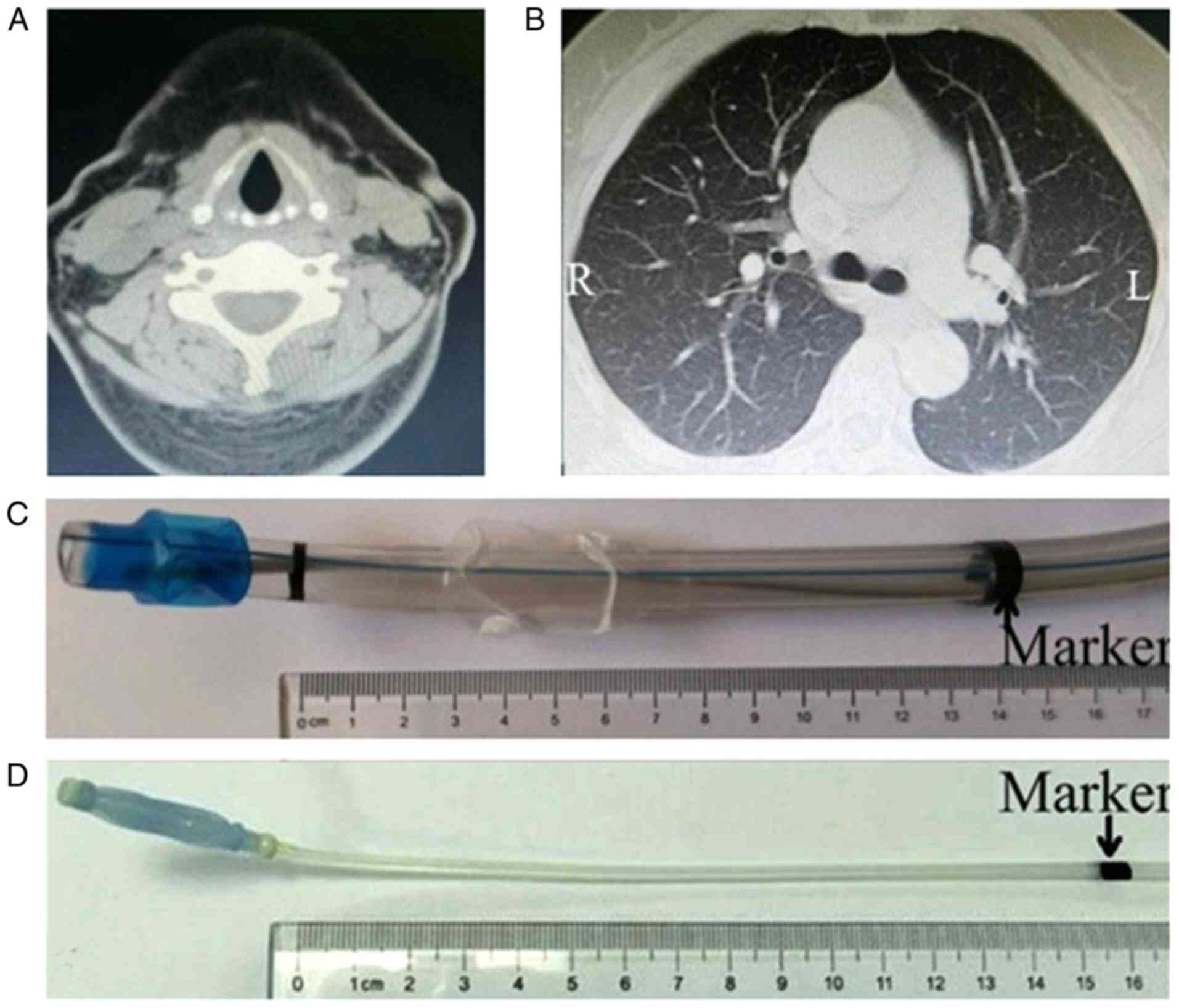
A previous study by our group reported that chest CT
images may be used to accurately predict the optimal insertion
depth of left-sided DLT (LDLT) (7).
Therefore, the present study aimed to compare the efficacy and
adverse effects of extraluminal application of the Uniblocker
(8) and LDLT under the guidance of
chest CT for OLV.
Materials and methods
Patients
The present study was approved by the Ethics
Committee of The First Hospital of Qinhuangdao (Qinhuangdao, China;
ClinicalTrials.gov registration no. NCT03392922). A total of 60
adult patients undergoing elective left-side thoracic surgery
requiring the Uniblocker or LDLT for OLV were included in the
present study. The inclusion criteria were as follows: Age of 18-70
years, American Society of Anesthesiologists (ASA) classifications
I-III and body mass index (BMI) ≤35 kg/m2. The exclusion
criteria were as follows: Pre-operative systolic blood pressure
>140 mmHg and/or diastolic blood pressure >90 mmHg, neck
deformity, ankylosing spondylitis, chronic bronchitis, bronchial
asthma, history of airway hyperresponsiveness, thoracic surgery
within the last month prior to enrolment, systemic infection or
suspected tuberculosis, pre-operative hoarseness or combined
visceral diseases of the heart, brain, liver or kidney. The
patients were randomly allocated to the Uniblocker group (U group;
n=30) or LDLT group (D group; n=30). Randomization (1:1) was based
on codes generated by a computer and these codes were kept in
sequentially numbered opaque envelopes until the end of the
study.
Methods of anesthesia
A senior anesthesiologist trained by a senior
radiologist pre-operatively screened all of the patients and
performed the measurements of the distance from the vocal cord to
the carina via the Picture Archiving and Communication System of
the hospital. The measured distance was calculated based on the
number of CT sections (5 mm) from the vocal cord to the carina
where the left and right bronchus were able to be distinctly
observed as a singular structure (Fig.
1A and B).
In the operating theatre, the patients were
monitored via electrocardiogram; invasive arterial blood pressure,
heart rate and peripheral oxygen saturation were also monitored
after placing patients in the supine position. For the induction of
anesthesia, the patients in the two groups were administered
midazolam 0.05 mg/kg, 2-4 µg/kg fentanyl, 0.6 mg/kg rocuronium and
0.3 mg/kg etomidate. All patients were intubated by an experienced
anesthesiologist 2 min following the administration of rocuronium
using one of the two devices.
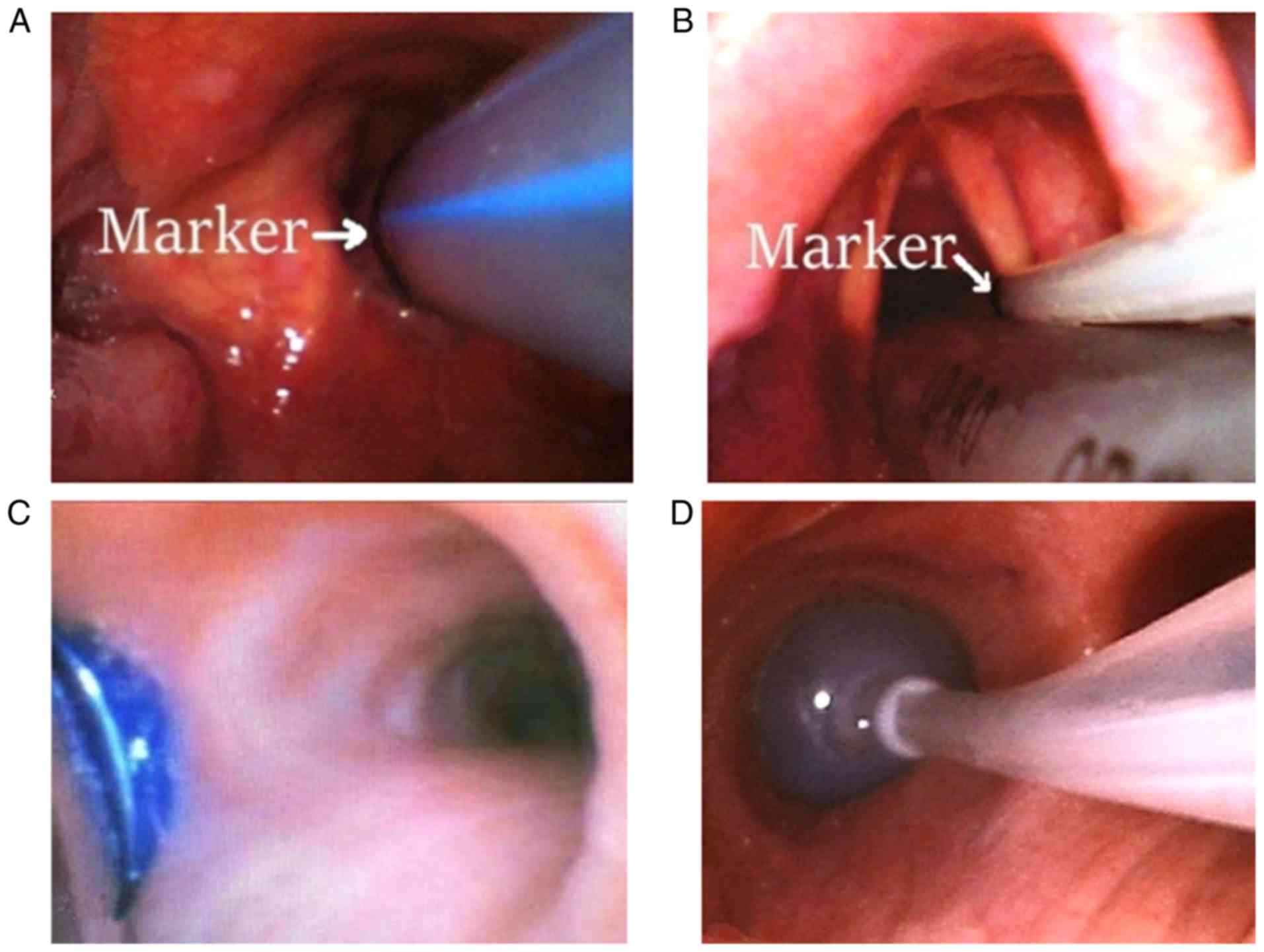
In the D group, an LDLT (Tuoren Medical Technology)
of adequate size (35 Fr for female and 37 Fr for male) was used for
intubation, which was performed as follows: The operator measured
the aforementioned distance, between the vocal cords and carina
according to the CT images of the patient's chest (Fig. 1C), on the LDLT from the black line on
the endobronchial side of the tube to the side nearest to the
mouth; a mark was made on the LDLT. Once the cuff of the
endobronchial side of the tube had passed the vocal cords, the
stylet was removed; the LDLT was rotated 90˚ toward the left
main-stem bronchus and gently inserted further. The operator then
identified the mark on the LDLT just above the vocal cords and
further insertion was terminated (Fig.
2A). The correct position of the LDLT was determined by
fiberoptic bronchoscope (FOB) (Fig.
2C). In addition, the insertion depth at the upper incisors was
recorded and indicated on the LDLT with tape. The LDLT was firmly
fixed at the patient's mouth with cloth tape.
In the U group, the Uniblocker (Changhua Medical
Technology) was inserted by the same anesthesiologist. The
intubation steps were as follows: The operator measured the
distance, plus 10 mm, from the vocal cords to the carina according
to the chest CT images (Fig. 1A and
B) at the upper edge of the cuff to
the side of the mouth and a mark was made on the Uniblocker
(Fig. 1D). Once the tip of the
Uniblocker had passed the glottis, it was inserted further toward
the left main-stem bronchus. Insertion was stopped once the
operator viewed the marker on the Uniblocker just above the vocal
cords (Fig. 2B). The laryngoscope
and Uniblocker were simultaneously held in the right hand of the
operator; an SLT of appropriate size (7.0 mm for females and 7.5 mm
for males) was inserted via a video laryngoscope to the appropriate
depth (Fig. 2B). The correct
position of the Uniblocker was then determined by FOB (Fig. 2D); the insertion depth at the upper
incisors was recorded and a mark was made on the Uniblocker, which
was then separately fixed with the SLT at the patient's mouth with
cloth tape.
The duration required for the initial insertion of
the Uniblocker or LDLT, the number of optimal positions of the
Uniblocker or LDLT upon blind insertion, the number of attempts to
adjust the Uniblocker or LDLT to an optimal position, the incidence
of tube displacement, the injuries of bronchi and carina assessed
via FOB, the duration of lung collapse, the number of failed
intubations, post-operative atelectasis or pneumonia diagnosis via
X-ray, and the occurrence of hoarseness and sore throat within 24 h
post-surgery were recorded.
The duration for initial intubation was defined as
the time from when the operator inserted the video laryngoscope
between the patient's teeth until the Uniblocker or LDLT was at the
optimal position. The optimal position of the Uniblocker was
achieved when the upper edge of the Uniblocker cuff was located
5-20 mm below the carina in the left main-stem bronchus; the
optimal position of the LDLT was achieved when the upper edge of
the cuff was located below the carina in the left main-stem
bronchus. The patients were placed in the lateral decubitus
position and the placement of the Uniblocker or LDLT was determined
via FOB; failure of intubation was defined as the inability to
insert the Uniblocker or LDLT into the left main bronchus after
three attempts.
Following completion of the intubation procedure,
the indicators of bronchi and carina injury were assessed by
another independent anesthesiologist using FOB. Injuries to the
bronchi and carina were graded as follows: 1, clear; 2, few
petechiae; 3, coalesced petechiae, hemorrhage or ecchymosis; and 4,
erosion (8).
Pulmonary collapse (1 min following pleural opening)
was ranked by the same independent thoracic surgeons as follows: 1,
excellent (complete collapse of lung); 2, fair (total collapse of
lung, but a certain amount of residual air remains) and 3, poor (no
collapse or partial collapse of lung) (6,9). The
incidence and subjective intensity of sore throat and hoarseness
within 24 h post-surgery were recorded by an independent
anesthesiologist in a blinded manner.
Statistical analysis
Continuous data were expressed as the mean ±
standard deviation. A Student's t-test was used for comparisons
between groups. The categorical data were presented as percentages;
Fisher's exact test or a χ2 test was used for
comparisons between groups. Injuries to the bronchi and carina were
analyzed by a Mann-Whitney U test. Statistical analysis was
performed using SPSS 21 statistical software (IBM Corp.). P<0.05
was considered to indicate a statistically significant
difference.
Results
Patient characteristics
There were no significant differences between the
two groups in patient demographics, including age, sex, body
weight, body height, BMI, ASA grade, surgery time, OLV time and the
type of thoracic surgery (P>0.05; Table I).
 | Table IDemographic characteristics of
patients, one-lung ventilation time, surgery time and types of
surgery in the two groups. |
Table I
Demographic characteristics of
patients, one-lung ventilation time, surgery time and types of
surgery in the two groups.
| Patient
characteristic | U group (n=30) | D group (n=30) | P-value |
|---|
| Age (years) | 56.5±14.5 | 55.5±11.3 | 0.79 |
| Sex (M/F) | 14/16 | 17/13 | 0.44 |
| ASA grade
(I/II/III) | 13/13/4 | 12/15/3 | 0.77 |
| Body weight (kg) | 61.6±11.8 | 66.4±11.5 | 0.13 |
| Body height (cm) | 167.6±8.9 | 167.9±7.1 | 0.85 |
| BMI
(kg/m2) | 21.8±2.9 | 23.6±4.2 | 0.14 |
| Surgery time
(min) | 118.8±54.5 | 141.7 ±60.3 | 0.15 |
| OLV time (min) | 93.4±49.0 | 106.9 ±60.6 | 0.38 |
| Type of surgery | 30 | 30 | |
|
Lung
surgery | 24 | 21 | 0.37 |
|
Esophageal
surgery | 3 | 4 | 1.00 |
|
Mediastinal
mass surgery | 3 | 5 | 0.70 |
Position of tube and intubation
time
There were no significant differences in the number
of optimal positions of the tube upon initial blind insertion
(26/30 for LDLT vs. 24/30 for Uniblocker), the duration of reaching
successful tube placement (83.9±19.4 vs. 84.3±17.1 sec for LDLT and
Uniblocker, respectively) and the number of repositioning attempts
and tube dislodgements following repositioning between the two
groups (P>0.05).
Lung collapse
The degree of lung collapse 1 min following opening
of the pleura was better in the D group than in the U group
(P<0.01), while the time required for complete collapse of the
lung was shorter in the D group (3.3±0.5 min) than that in the U
group (8.4±1.2 min; P<0.01; Table
II).
 | Table IIThe number of optimal positions of
the tube upon initial blind insertion, the number of repositioning
attempts, times for intubation and lung collapse, dislodgement and
the degree of lung collapse. |
Table II
The number of optimal positions of
the tube upon initial blind insertion, the number of repositioning
attempts, times for intubation and lung collapse, dislodgement and
the degree of lung collapse.
| Factor | U group (n=30) | D group (n=30) | P-value |
|---|
| Optimal positions
upon initial blind insertion | 24(80) | 26(87) | 0.73 |
| Repositioning
attempts | | | 0.42 |
|
1 | 5(17) | 2(7) | |
|
2 | 1(3) | 2(7) | |
|
3 | 0 (0) | 0 (0) | |
| Time for intubation
(sec) | 84.3±17.1 | 83.9±19.4 | 0.95 |
| Time to lung
collapse (sec) | 8.4±1.2 | 3.3±0.5 | <0.01 |
| Degree of lung
collapse | | | <0.01 |
|
Excellent | 0 (0) | 7(23) | |
|
Fair | 12(40) | 18(60) | |
|
Poor | 18(60) | 5(17) | |
| Dislodgement | 1(3) | 3(10) | 0.60 |
Incidence of complications
The incidence of injury to the carina and bronchi
was significantly lower in the U group (2/30 cases) compared with
that in the D group (10/30 cases; P<0.05); the incidence of sore
throat was also lower in the U group (2/30 cases) than that in the
D group (9/30 cases; P<0.05). The hoarseness of patients and the
incidence of pneumonia or post-operative atelectasis were not
significantly different between the two groups (P>0.05; Table III).
 | Table IIIDegree of bronchial and carina
injuries, and postoperative adverse events in the two groups. |
Table III
Degree of bronchial and carina
injuries, and postoperative adverse events in the two groups.
| Factor | U group (n=30) | D group (n=30) | P-value |
|---|
| Injury to bronchi
and carina | 2(7) | 10(33) | 0.02 |
|
1 | 1(3) | 5(17) | 0.20 |
|
2 | 1(3) | 3(10) | 0.61 |
|
3 | 0 (0) | 2(7) | 0.47 |
|
4 | 0 (0) | 0 (0) | |
| Sore throat | 2(7) | 9(30) | 0.04 |
| Hoarseness | 0 (0) | 3(10) | 0.24 |
| Post-operative
pneumonia or atelectasis | 7(23) | 4(13) | 0.51 |
Vital signs at different
time-points
The mean arterial pressure (MAP) immediately
following intubation was lower in the U group (122.0±13.4 mmHg)
than that in the D group (129.2±12.1 mmHg; P<0.05) and there
were no significant differences between the two groups at before
anesthesia, before intubation, 3 min after intubation.(P>0.05).
The heart rate and oxygen saturation were not significantly
different between the two groups at any of the time-points
(P>0.05; Table IV).
 | Table IVHemodynamic alterations in patients
during intubation. |
Table IV
Hemodynamic alterations in patients
during intubation.
| Factor | U group (n=30) | D group (n=30) | P-value |
|---|
| MAP (mmHg) |
|
T0 | 96.4±8.6 | 100.0±9.1 | 0.14 |
|
T1 | 73.9±8.1 | 76.2±9.1 | 0.10 |
|
T2 | 122.0±13.4 | 129.2±12.1 | 0.04 |
|
T3 | 109.2±16.8 | 112.2±14.4 | 0.50 |
| HR (bpm) |
|
T0 | 74.8±9.4 | 76.2±9.1 | 0.60 |
|
T1 | 72.0±10.4 | 76.2±12.5 | 0.19 |
|
T2 | 90.9±9.9 | 93.7±13.3 | 0.39 |
|
T3 | 83.6±11.8 | 86.9±14.1 | 0.37 |
| SpO2
(%) |
|
T0 | 98.9±1.2 | 98.6±1.6 | 0.89 |
|
T1 | 99.7±0.5 | 99.6±0.7 | 0.51 |
|
T2 | 99.8±0.4 | 99.7±0.5 | 0.76 |
|
T3 | 99.0±1.4 | 99.7±0.6 | 0.31 |
Discussion
The results of the present study demonstrated that
LDLT had a shorter duration to lung collapse (3.3 vs. 8.4 min) and
better lung collapse at 1 min following opening of the pleura,
while the Uniblocker was associated with a reduced incidence of
carinal and bronchial injuries and sore throat, and a lower MAP
immediately following intubation. The duration of intubation did
not significantly differ between the two devices.
OLV is fundamental in thoracic anesthesia as the
majority of thoracic surgeries require lung isolation to facilitate
visibility in surgical procedures and protect the healthy lung from
cross-contamination. DLT is the preferred device for OLV; however,
DLT is associated with numerous disadvantages, including difficulty
in intubation in patients with restricted airways (10) and increased incidence of airway
injury due to its large diameter (11,12).
Furthermore, in patients requiring post-operative ventilation
support, the DLT may be replaced with an SLT. The first application
of the BB was reported by Magill (13) in 1936. The first modern BB, known as
the 'Univent tube', was presented by Inoue et al (14) in 1982. To date, the use of BBs,
including the Univent blocker, Uniblocker, Cohen blocker (15), Coopdech blocker (16), Arndt blocker (17) and the EZ blocker (18) has increased in OLV. It has been
reported that BBs are more advantageous than DLTs due to easier
insertion, particularly in patients with restricted airways
(19). In addition, the tube does
not have to be replaced when post-operative mechanical ventilation
is required; however, it was reported that the placement of BBs was
more time-consuming and additional intra-operative attempts in
repositioning may be required compared with the LDLT (5). DLTs and BBs have been used for more
than seven decades; however, which device is the most effective and
has fewer adverse effects in patients has remained controversial
(20-22).
In a previous study by our group, chest CT images
were used to accurately predict the optimal insertion depth of an
LDLT (7), and the extraluminal use
of the Uniblocker was determined to be faster and more accurate
than the conventional intraluminal use of the Uniblocker for
left-side thoracic surgery (8).
Therefore, in the present study, the efficacy and adverse effects
of the Uniblocker and LDLT for OLV were investigated under the
guidance of chest CT images. The results revealed that the number
of optimal positions of the tube upon initial blind insertion and
repositioning attempts were similar in the two groups. The duration
of successful LDLT placement was 83.9 sec and that for the
Uniblocker was 84.3 sec; the time was recorded from when the
laryngoscope was inserted between the teeth of patients until the
optimal position was obtained as determined via FOB. Campos and
Kernstine (6) reported that the
duration for successful LDLT placement was 128 sec and that for the
Univent BB was 158 sec (as recorded from when the tube passed the
vocal cords until satisfactory placement of the tube was achieved).
Ruetzler et al (23) reported
that the time recorded for initial LDLT placement was 85 sec, while
that for the EZ blocker was 192 sec (the duration from the tube
passing the vocal cords to satisfactory placement). In a study by
Narayanaswamy et al (5), the
intubation time (from the beginning of laryngoscopy to lung
isolation) for the LDLT was 93 sec and that for the Uniblocker was
203 sec. The present study reported a comparatively shorter time
for LDLT placement (83.9 sec), while that for the Uniblocker was
84.3 sec. The shorter placement time of the LDLT compared with that
in previous studies (5,6,23) may be
associated with the use of chest CT images, which is more accurate
and effective. A reduced placement time of the Uniblocker may due
to the extraluminal insertion of the SLT, in which the operator is
able to rotate the Uniblocker an additional 20˚ counterclockwise to
the left main-stem bronchus for posterior access to the trachea
branches (24). In addition, the
extraluminal use of Uniblocker allowed the tube to be inserted with
ease. Furthermore, the operator was able to accurately measure the
insertion depth based on the chest CT images. The operator viewed
the marker on the Uniblocker just above the vocal cords during
intubation to identify the optimal depth in the left main-stem
bronchus. Therefore, the extraluminal use of the Uniblocker under
the guidance of chest CT images may allow for rapid and easy
insertion compared with the conventional intubation method.
Displacement of BBs or DLTs is a common event during
intubation, particularly when the patient is moved from a supine to
a lateral position, or from surgical manipulation of the operated
lung, which may result in insufficient lung collapse and increases
the risk of hypoxia during OLV (5).
Narayanaswamy et al (5)
revealed that repositioning of the DLT was required for 2/26
patients, while repositioning of the Uniblocker was performed in
11/26 patients. In the present study, displacement was recorded for
3/30 patients for the LDLT and 1/30 patients for Uniblocker
intubation. The reasons for this may be as follows: The present
study only selected patients undergoing left-side thoracic surgery
and the left main-stem bronchus is longer than the right one. In
addition, the insertion depth of the Uniblocker was 10 mm below the
carina (the distance between the vocal cords and carina plus 10 mm)
and the Uniblocker was inserted extraluminally to the trachea;
thus, there was a greater space for the Uniblocker to move.
Furthermore, whilst moving patients into the lateral decubitus
position, the LDLT or Uniblocker was securely held near the
incisors and the patient's head was kept in a neutral position.
Therefore, displacement of the BB or LDLT was reduced in the
present study.
The degree of lung collapse may affect visibility in
surgical procedures. In the present study, the results revealed
that the LDLT had a shorter time for lung collapse (3.3 vs. 8.4
min) and better lung collapse 1 min following pleura opening
compared with the Uniblocker. This may be due to the larger lumen
of the LDLT than the Uniblocker catheter (internal diameter, 1.6
mm), which may be associated with increased gas flow (25). On the contrary, deflating the cuff of
the Uniblocker prior to pleura opening may induce a period of apnea
(30 sec); however, with adequate suctioning via SLT, it is possible
to insert a suction catheter into the SLT for the extraluminal
application of the Uniblocker. Thus, the non-ventilated lung may
also collapse well (26). Upon
complete deflation, no differences between the two devices were
observed (6).
Hoarseness and sore throat are common post-operative
symptoms following tracheal intubation. Christensen et al
(27) reported that the incidence of
hoarseness following tracheal intubation was ~50%. In a study by
Zhong et al (28), the
incidence of sore throat from Coopdech was 13%, that from Arndt was
20% and that from Univent was 30%. Knoll et al (9) observed the notable frequency of
post-operative hoarseness in the DLT group (44%) compared with that
in the BB group (17%). In the present study, sore throat was
reported in 2/30 cases in the U group and in 9/30 cases in the D
group; hoarseness occurred in 1/30 cases in the U group and in 4/30
cases in the D group. An explanation for this may be that the LDLT
with a larger diameter and distal curvature is more rigid than the
SLT (3). Furthermore, during
intubation, the LDLT must be rotated 90˚ toward the left main-stem
bronchus after the cuff of the tube passes the vocal cords; this
process may cause injury to the glottis. Thus, the incidence of
post-operative hoarseness was higher in the LDLT group than in the
Uniblocker group. The results demonstrated that the size of the
tracheal tube is a common risk factor associated with higher
incidences of hoarseness and sore throat.
Injuries to the bronchi and carina were reported in
2/30 patients in the U group and 10/30 patients in the D group.
This may have resulted from the larger outer diameter of the LDLT
compared with the SLT, and as the endobronchial tube has a distal
curvature, the endobronchial tube was required to be rotated 90˚
during intubation to pass the vocal cords, trachea and carina and
enter the left main-stem bronchus. Therefore, this process may
cause injury to the tracheal mucosa; however, the Uniblocker and
SLT are thinner than the LDLT. Thus, the injuries to the bronchi
and carina were more severe in the D group than in the U group. The
MAP following intubation was higher in the D group than in the U
group. This may be associated with the size of the DLT applied in
the D group, which may induce injuries, particularly when passing
the carina.
In numerous clinical situations, including the
intubation of patients with restricted airways or tracheostomy,
intubation with DLT tends to be difficult and at times impossible
(29,30). In other situations, including
empyema, hemothorax or blood and secretion in the trachea, the
healthy lung may be exposed to cross-contamination with the use of
the Uniblocker. Under these conditions, an alternative device for
guaranteeing patient safety must be selected (31), and regardless of whether DLTs or BBs
are employed, it is important that the operator is familiar with
the devices (32).
There are also numerous limitations to the present
study. The patient cohort was small and those patients with an
undetectable glottis during intubation were excluded from the
analysis. In addition, pre-operative chest CT scans must contain
slices of vocal cord and carina, from which the distance between
vocal cord and carina may be determined. Furthermore, there may be
a bias in the procedure performed, as it was not performed in a
blinded manner.
In conclusion, the duration until lung collapse was
longer with Uniblocker intubation compared with the LDLT; providing
a period of apnea is induced (30 sec) and adequate suctioning is
performed via an SLT, the non-ventilated lung may also collapse
well. Therefore, the extraluminal use of the Uniblocker under the
guidance of chest CT images may be an easy and efficient method for
OLV in left-side thoracic surgery with few adverse effects.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed generated during
the study are available from the corresponding author on reasonable
request.
Authors' contributions
ZL contributed to the conception and design. LZ, YZ
and QQJ collected the data. XCY, LB and SJL performed the analysis
of data and interpretation of results. LZ and YZ wrote the
manuscript and were involved in its critical revision. All authors
reviewed and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of The First Hospital of Qinhuangdao (Qinhuangdao, China)
and informed written consent was obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Shelley B, Macfie A and Kinsella J:
Anesthesia for thoracic surgery: A survey of UK practice. J
Cardiothorac Vasc Anesth. 25:1014–1017. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Della Rocca G, Langiano N, Baroselli A,
Granzotti S and Pravisani C: Survey of thoracic anesthetic practice
in Italy. J Cardiothorac Vasc Anesth. 27:1321–1329. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Angie Ho CY, Chen CY, Yang MW and Liu HP:
CY AH: Use of the Arndt wire-guided endobronchial blocker via nasal
for one-lung ventilation in patient with anticipated restricted
mouth opening for esophagectomy. Eur J Cardiothorac Surg.
28:174–175. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Campos JH: An update on bronchial blockers
during lung separation techniques in adults. Anesth Analg.
97:1266–1274. 2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Narayanaswamy M, McRae K, Slinger P, Dugas
G, Kanellakos GW, Roscoe A and Lacroix M: Choosing a lung isolation
device for thoracic surgery: A randomized trial of three bronchial
blockers versus double-lumen tubes. Anesth Analg. 108:1097–1101.
2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Campos JH and Kernstine KH: A comparison
of a left-sided Broncho-Cath with the torque control blocker
univent and the wire-guided blocker. Anesth Analg. 96:283–289.
2003.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Liu Z, Zhao L, Jia Q, Yang X, Liang SJ and
He W: Chest computed tomography image for accurately predicting the
optimal insertion depth of left-sided double-lumen tube. J
Cardiothorac Vasc Anesth. 32:855–859. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Liu Z, He W, Jia Q, Yang X, Liang S and
Wang X: A comparison of extraluminal and intraluminal use of the
Uniblocker in left thoracic surgery: A CONSORT-compliant article.
Medicine (Baltimore). 96(e6966)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Knoll H, Ziegeler S, Schreiber JU,
Buchinger H, Bialas P, Semyonov K, Graeter T and Mencke T: Airway
injuries after one-lung ventilation: A comparison between
double-lumen tube and endobronchial blocker: a randomized,
prospective, controlled trial. Anesthesiology. 105:471–477.
2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Benumof JL: Difficult tubes and difficult
airways. J Cardiothorac Vasc Anesth. 12:131–132. 1998.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu H, Jahr JS, Sullivan E and Waters PF:
Tracheobronchial rupture after double-lumen endotracheal
intubation. J Cardiothorac Vasc Anesth. 18:228–233. 2004.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yüceyar L, Kaynak K, Cantürk E and Aykaç
B: Bronchial rupture with a left-sided polyvinylchloride
double-lumen tube. Acta Anaesthesiol Scand. 47:622–625.
2003.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Magill IW: Anesthesia in thoracic surgery,
with special reference to lobectomy: (Section of Anesthetics). Proc
R Soc Med. 13:643–653. 1936.PubMed/NCBI
|
|
14
|
Inoue H, Shohtsu A, Ogawa J, Kawada S and
Koide S: New device for one-lung anesthesia: Endotracheal tube with
movable blocker. J Thorac Cardiovasc Surg. 83:940–941.
1982.PubMed/NCBI
|
|
15
|
Cohen E: The Cohen flexitip endobronchial
blocker: An alternative to a double lumen tube. Anesth Analg.
101:1877–1879. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Garcia-Guasch R, Flo A and de Castro PL:
Coopdech bronchial blocker is useful in abnormalities of the
tracheobronchial tree. J Cardiothorac Vasc Anesth. 24:735–736.
2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Arndt GA, Kranner PW, Rusy DA and Love R:
Single-lung ventilation in a critically ill patient using a
fiberoptically directed wire-guided endobronchial blocker.
Anesthesiology. 90:1484–1486. 1999.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mungroop HE, Wai PT, Morei MN, Loef BG and
Epema AH: Lung isolation with a new Y-shaped endobronchial blocking
device, the EZ-Blocker. Br J Anaesth. 104:119–120. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
García-Aguado R, Mateo EM, Onrubia VJ and
Bolinches R: Use of the Univent System tube for difficult
intubation and for achieving one-lung anaesthesia. Acta
Anaesthesiol Scand. 40:765–767. 1996.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Slinger P: Con: The new bronchial blockers
are not preferable to double-lumen tubes for lung isolation. J
Cardiothorac Vasc Anesth. 22:925–929. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cohen E: Pro: The new bronchial blockers
are preferable to double-lumen tubes for lung isolation. J
Cardiothorac Vasc Anesth. 22:920–924. 2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Campos JH: Which device should be
considered the best for lung isolation: Double-lumen endotracheal
tube versus bronchial blockers. Curr Opin Anaesthesiol. 20:27–31.
2007.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ruetzler K, Grubhofer G, Schmid W, Papp D,
Nabecker S, Hutschala D, Lang G and Hager H: Randomized clinical
trial comparing double-lumen tube and EZ-Blocker for single-lung
ventilation. Br J Anaesth. 106:896–902. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Patel RV, Van Noord BA, Patel D, Hong EJ,
Bourne E, Patel RR, Chandrasoma J, Chan L, Szenohradszki J and Lumb
PD: Determination of the true inclination angle of the main bronchi
relative to the median sagittal plane for placement of a left-sided
double-lumen tube. J Cardiothorac Vasc Anesth. 31:434–440.
2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Brodsky JB: Con: A bronchial blocker is
not a substitute for a double-lumen endobronchial tube. J
Cardiothorac Vasc Anesth. 29:237–239. 2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Bussières JS, Somma J, Del Castillo JL,
Lemieux J, Conti M, Ugalde PA, Gagné N and Lacasse Y: Bronchial
blocker versus left double-lumen endotracheal tube in
video-assisted thoracoscopic surgery: A randomized-controlled trial
examining time and quality of lung deflation. Can J Anaesth.
63:818–827. 2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Christensen AM, Willemoes-Larsen H, Lundby
L and Jakobsen KB: Postoperative throat complaints after tracheal
intubation. Br J Anaesth. 73:786–787. 1994.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhong T, Wang W, Chen J, Ran L and Story
DA: Sore throat or hoarse voice with bronchial blockers or
double-lumen tubes for lung isolation: A randomised, prospective
trial. Anaesth Intensive Care. 37:441–446. 2009.PubMed/NCBI
|
|
29
|
Kawamoto M, Iwanami Y, Igarashi K, Yamada
N, Matsuno K and Iwasaki H: Anesthetic management of patients with
tracheal bronchus. Masui. 57:152–157. 2008.PubMed/NCBI
|
|
30
|
Schmidt MH, Riley RH and Hee GY: Difficult
double-lumen tube placement due to laryngeal web. Anaesth Intensive
Care. 38:194–196. 2010.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Campos JH: Lung isolation techniques for
patients with difficult airway. Curr Opin Anaesthesiol. 23:12–17.
2010.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Campos JH, Hallam EA, Van Natta T and
Kernstine KH: Devices for lung isolation used by anesthesiologists
with limited thoracic experience: Comparison of double-lumen
endotracheal tube, Univent torque control blocker, and Arndt
wire-guided endobronchial blocker. Anesthesiology. 104:261–266.
2006.PubMed/NCBI View Article : Google Scholar
|