Introduction
Early extubation or fast track techniques are used
in areas as diverse as routine cardioanesthesia and post-surgical
anesthesia, and they are also used during neuroanesthesia (1,2). An even
greater effect occurs in anesthesiology, mainly as the assessment
of a patient's neurological condition in a conscious individual is
the best and least expensive neuromonitoring method available
(3). Early extubation should be
performed jointly with neurosurgery so that execution of the
technique does not negatively alter the result of surgical
procedure. In the present study, the role of early extubation in
neuroanesthesia was evaluated, considering the physiopathological
repercussions and the benefits and drawbacks of early and late
awakening, providing a basis for the establishment of a possible
rapid transitional anesthetic plan. Early awakening and extubation
in neuroanesthesia are desirable and possible in numerous
cases.
It is estimated that ~200,000 patients per year
require mechanical ventilation due to neurological damage in the
USA (1). The neurosurgical patient
poses a series of challenges to the clinician with regard to airway
management, mechanical ventilation and determination of the ideal
time-point for extubation. Prior neurological damage may, directly
or indirectly, influence control of breathing or the airways. For
this reason, extubation criteria should be reviewed for each
patient.
The rate of mortality of neurosurgical patients who
require airway control and ventilatory assistance ranges between 20
and 50%. The cost associated with the care of these patients has
been estimated at >25 billion dollars per year in the USA.
Therefore, decreasing the time on mechanical ventilation has a
great medical and economic significance (2). Extubation of the neurosurgical patient
requires particular consideration of respiratory mechanics and
airway resistance, as well as specific factors relevant to the
neurosurgical patient in terms of endotracheal tube withdrawal and
avoidance of the use of mechanical ventilation as much as possible
(3).
Fast track is an alternative in neurosurgical
patients that avoids, as much as possible, the use of mechanical
ventilation in the intensive care unit (ICU) and the associated
complications. It is based on the premise that assessment of the
neurological condition in a conscious patient is the best and least
costly neuromonitoring method available (4). A patient who wakes up from anesthesia
in the operating room and is then transferred to the recovery room
and then to the ward has a lower risk of acquiring a nosocomial
infection, atelectasis, pneumonia, ventilator complications and
other risks inherent in the ICU. Reducing or avoiding stays in the
ICU allows for an increase in survival and reduces the risk of
illness for the patient in addition to reducing costs for both the
patient and the institution.
Early recognition of central nervous system
dysfunction reduces complications. In the neurosurgical patient,
complete recovery of consciousness is the most important issue for
the surgical team. Intracranial surgery is rarely performed on a
normal brain; therefore, post-surgical assessment may pose a
certain degree of difficulty. Invasion of the airways should be
discontinued as soon as practically possible. Extubation is a
critical procedure and constitutes a determinant of the immediate
future of the surgical patient in terms of satisfactory recovery or
life-threatening complications (5).
Since the beginning of the 21st century, attempts have been made to
create early extubation protocols in neuroanesthesia. However,
there is no consensus as to when and in what patients early
extubation should be attempted (6).
An adequate anesthetic technique that allows for rapid awakening of
a neurosurgical patient is not exempt from possible complications.
Certain systemic and neurological situations must always be
considered, since mismanagement of these aspects may complicate a
rapid extubation technique (7,8).
At present, evaluation of the neurological condition
in a conscious patient is the best and least expensive
neuromonitoring method; therefore, early awakening of these
patients represents a trend that is on the rise. For this reason,
the objective of the present study was to determine whether less
ventilator-associated post-surgical complications occur when
patients are extubated early after surgery comprising drainage of
an intracranial hematoma. The present study also assessed whether
early extubation was associated with a reduced ICU stay.
Materials and methods
Patients
The present study was a controlled, experimental,
cross-sectional, prospective, comparative, non-blinded clinical
trial in post-surgery intracranial hematoma evacuation patients to
assess fast track (early extubation) vs. conventional extubation in
the period from January 2014 to August 2015 at the Hospital
Universitario ‘Dr Jose Eleuterio Gonzalez’ (Monterrey, Mexico). The
17 patients included were randomly divided into two groups: In
Group 1, patients were extubated at the end of the surgical
procedure and in Group 2, the patients were extubated in a
conventional manner (8 h after the surgery was completed). In the
randomization process, sealed envelopes with randomized computer
results were used to assign each patient to one of the two groups.
Patients about to receive open cranial surgery due to an
intracranial hematoma with an anesthesia risk of I-III according to
the American Society of Anesthesiologists (ASA) (9), an age of at least 18 years, no
intubation prior to entering the operating room and a Glasgow score
of ≥8 were included (10).
Patients aged <18 years, those with
catecholamine-secreting tumors, coagulation disorders, or
decompensated heart or lung disease were excluded. Patients with a
scheduled surgery in another area of the body and with hypovolemic
shock were also excluded. Furthermore, patients whose surgeries
lasted for >480 min or were accompanied by massive or
uncontrollable bleeding (loss of 50% of blood volume for 3 h (~1
l/h) or >150 ml/kg of body weight or >1.5 ml/kg/min for
>20 min) were eliminated.
Post-surgical procedures
The patients from the two groups were assessed on
admission to the operating room according to established standards,
and once the selection criteria were met, general anesthesia was
induced with propofol (2 mg/kg) and fentanyl (2 µg/kg). Propofol
administration was maintained as a continuous intravenous infusion.
A dose of fentanyl of 1 µg/kg/h was used for maintenance. The
propofol infusion and fentanyl doses were adjusted based on
hemodynamic parameters (blood pressure and heart rate). The main
aim of the procedure was to reduce the time of extubation.
Hemodynamic stability was also assessed post-operatively (number of
anesthetic adjustments required to maintain hemodynamic parameters
within 20% of pre-induction values).
The patient was extubated when the following
criteria were fulfilled (11):
Regular breathing, without intercostal retraction and with a
respiratory rate of >8 breaths per minute, a telespiratory
CO2 pressure of <45 mmHg, an oxygen saturation
(SatO2) of >95% with an inspired oxygen fraction of
100%, presence of a swallowing reflex, body temperature between 36
and 37˚C, hemodynamic stability (a change in baseline blood
pressure of ≤15 mmHg), and a cooperative and oriented patient able
to respond to verbal orders.
Attempted fast-track extubation was performed after
post-operative neurological assessment by the same responsible
surgeon. The difference between the two groups was in extubation
time criteria; extubation was 8 h after surgery in the conventional
group, but extubation was immediately post-surgical in the
fast-track group. If a patient did not meet the criteria, they were
considered to have failed extubation and were transferred to the
ICU to receive mechanical ventilation. Subsequently, they were
declared as ‘fast-track group patients with failed extubation’; no
patients had that declaration.
Statistical analysis
Demographic variables are presented as n or mean ±
standard deviation and described in Table I. Differences in the distribution of
patients depending on their ASA score were analyzed using the
chi-square test. For parameters described by continuous variables,
a Kolmogorov-Smirnov test of normality was performed and
differences between groups were determined using Student's t-test
or a Mann-Whitney U-test as appropriate. SPSS version 21 software
(IBM Corp.) was used for statistical analysis.
 | Table IDemographic data and ASA score in the
two groups. |
Table I
Demographic data and ASA score in the
two groups.
| Parameters | Group 1: Early
extubation (fast track) (n=10) | Group 2: Conventional
extubation (n=7) | P-value |
|---|
| Sex | | | 0.99 |
|
Male
(n) | 8 | 7 | |
|
Female
(n) | 2 | 0 | |
| Age (years) | 50.50±21.15 | 48.28±19.42 | 0.87 |
| Weight (kg) | 66.60±7.24 | 72.57±5.98 | 0.82 |
| Height (cm) | 164.6±11.39 | 168.57±12.04 | 0.91 |
| ASA score | | | 0.34 |
|
I | 4 | 1 | |
|
II | 5 | 4 | |
|
III | 1 | 2 | |
|
IV | 0 | 0 | |
|
V | 0 | 0 | |
For comparison of parameters throughout the
post-operative period, including blood pressure, heart rate,
respiratory rate, SatO2 or Glasgow coma scale score, a
general linear model was used to determine the differences between
repeated measurements. Comparisons with a p-value of ≤0.05 were
significant; all the hypothesis tests were two-tailed.
Results
Patient characteristics
The data from the 17 patients were analyzed; 7
patients were subjected to conventional extubation and 10 to
fast-track extubation after surgery. There was no statistically
significant difference in age, weight, height and ASA scores
between groups (Table I).
Post-surgical condition and
extubation
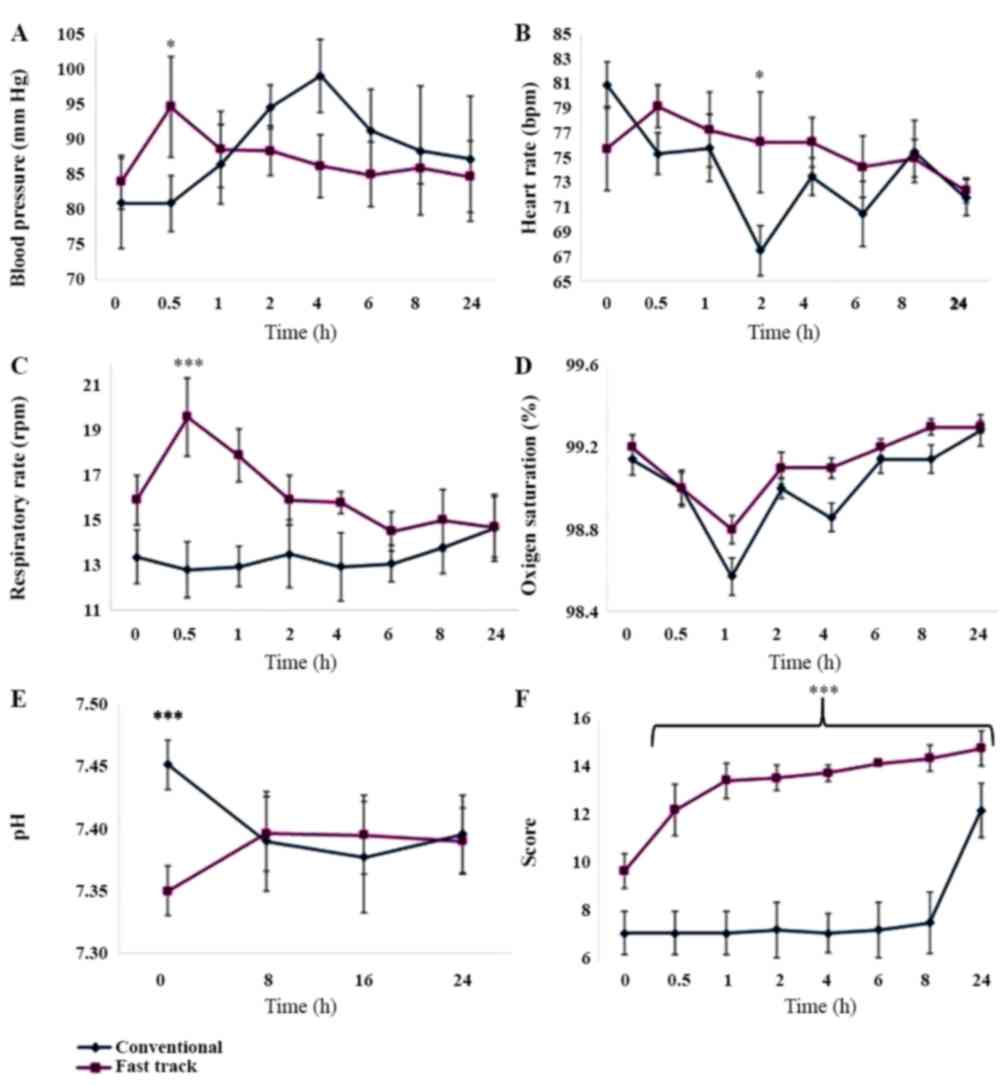
The respiratory rate was regular throughout the
patient follow-up. Only one patient in the fast-track group had an
irregular respiratory rhythm at the beginning of the study, due to
the use of accessory muscles. During the post-operative
observation, no significant differences in post-operative blood
pressure changes were observed between the two groups; a peak in
blood pressure was observed at 30 min post-extubation for the
fast-track group and at 4 h for the conventional treatment group.
These observations may correspond to the time sequence of
extubation attempts (Fig. 1A). In
regards to the heart rate (HR), no significant difference was
observed between the two groups at all time points (P=0.58);
however, those patients with conventional management had a tendency
of low heart rates during most of the follow-up; the conventional
group had a decrease in HR, but it was reestablished at next
measurement (4 h post extubation). This may be due to the
persistent use of sedation and longer times under mechanical
ventilation (Fig. 1B). For the
respiratory rate, the statistical difference between the two groups
was observed to be not significant except for 0.5 h after the
procedure (P=0.021) (Fig. 1C). The
patients in the fast-track group had a higher respiratory rate, and
the fast-track treatment appears to be the cause of this difference
(Fig. 1C). Also, no significant
differences in SatO2% measurements were identified
between the groups (P=0.63; Fig.
1D). Blood pH values were not significantly different between
the two groups (Fig. 1E). The
Glasgow Come Scale score was significantly different fast-track
against conventional extubation (P=0.001; Fig. 1F). Only three of the 17 patients
evaluated were extubated after the first 8 h.
Complications
Among the patients who were extubated in a
conventional manner (≥8 h after the end of surgery), one presented
with a seizure and was re-intubated and transferred to the ICU; one
presented with signs of aspiration and was not able to remain
extubated for a long time. None of the patients who had the fast
track procedure presented with complications and all were
neurologically assessed at the end of the surgery. However, certain
clinical complications were observed in the conventional extubation
group when compared with the fast track group, including a torpid
outcome in four of the seven patients evaluated, seizure in one
patient and failed extubation in three cases with development of
pulmonary atelectasis (n=2) and aspiration (n=1). A total of four
patients were classified as cases of failed extubation due to
pulmonary complications. Compared with the fast track group,
significant differences in clinical complications events were
observed in the conventional extubation group (57%; P=0.015; data
not shown).
There was no significant difference in the procedure
depending on age (P=0.87), sex (P=0.99) or surgical risk ASA score
(P=0.35) among patients with complications or those with a
favorable outcome (Table II). The
relative risk of the fast track procedure compared with
conventional extubation was determined as 0.2727 (95% CI,
0.0126-5.9166), which was not significant (P=0.4079). Differences
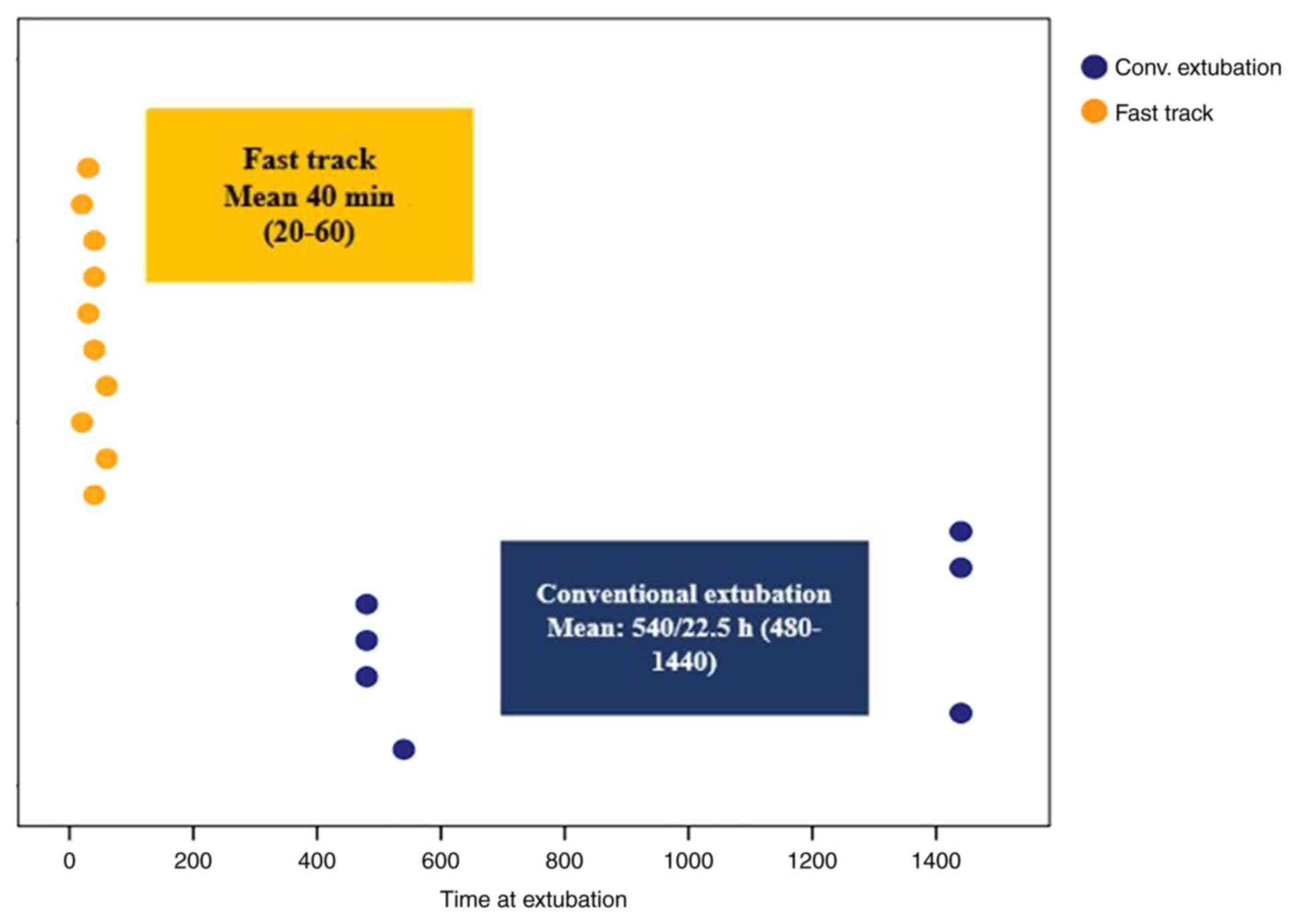
in extubation time between the two groups were 40±20 min for the
fast-track group, whilst for conventional patients they were
940±480 min (Fig. 2).
 | Table IIVital signs 0.5 h after extubation
procedure. |
Table II
Vital signs 0.5 h after extubation
procedure.
| Parameter | Group 1: Early
extubation (fast track) (n=10) | Group 2: Conventional
extubation (n=7) | P-value |
|---|
| MAP (mean) mmHg | 94.500±17.190 | 80.850±11.890 | 0.033 |
| SatO2
(%) | 99.000±0.940 | 99.000±0.580 | 0.500 |
| Body temperature
(˚C) | 36.800±0.010 | 36.590±0.230 | 0.099 |
| Heart rate
(beats/min) | 79.100±15.750 | 75.290±10.950 | 0.277 |
| Respiratory rate
(breaths/min) | 19.000±4.180 | 12.430±1.610 | 0.003 |
Discussion
The results of the present study indicate that
patients who remain intubated and undergo mechanical ventilation at
the ICU present with more complications than those who are
extubated early if they meet the necessary criteria. Cai et
al (12) assessed the causes of
delayed extubation of neurosurgical patients. That study included
800 patients subjected to craniotomy for resection of intracerebral
tumors, of which 398 (49.8%) received delayed extubation. Bruder
and Ravussin (8) provided
information regarding the factors associated with this delay were
dysfunction of the cranial nerves, hydrocephalus, tumor location,
duration of surgery of >6 h and blood loss of >1,000 ml. In a
previous clinical study conducted by Bruder and Ravussin (8), patients exhibited greater severity of
pneumonia, a prolonged stay at the ICU and at the hospital with
higher hospitalization costs compared with the early extubation
group in the present study.
Cai et al (12) determined predictive factors of
extubation failure in 2,118 patients who underwent craniotomy; in
this cohort, the extubation attempt failed in 94 patients (4.4%). A
number of major factors were identified to be predictors of
extubation failure: Previous craniotomy, cranial nerve dysfunction,
tumor size, tumor site and extreme changes in blood pressure during
surgery. Failed extubation was also associated with pneumonia, ICU
mortality, unfavorable Glasgow scale score, longer ICU and hospital
stay, and higher hospital costs compared to patients who were
successfully extubated (12). In the
present study, patients who were extubated later than those who
were extubated early also had complications including seizures,
failed extubation, atelectasis and aspiration.
If the patient is suitable for early extubation,
this should be attempted to avoid the use of mechanical ventilation
at the ICU, since this is a pre-disposing factor for respiratory
complications, hospital infections, neuroinfection and death. In a
study by Vora et al (13) on
1,150 patients who were intubated prior to admission to the ICU,
the survival rate was 57.75%, with ventilator-associated pneumonia
being the most common complication (53.33%), followed by decubitus
ulcers (40%) and deep venous thrombosis (8.89%). The cost of
ventilator-associated complications is high; therefore, patient
intubation for an extended period should be avoided as much as
possible (13).
Another study indicated that ventilator-associated
pneumonia (S. aureus or P. aeruginosa) contributed to
patients remaining intubated for 37.9 days (S. aureus) or
55.4 days (P. aeruginosa) on average, while non-intubated
patients had decreased average duration of hospitalization of 7.2
days; in addition, the ICU stay for those intubated patients was
longer (6.9 or 14.8 vs. 1.1 days), mechanical ventilation use was
increased (62.6 or 62.3 vs. 7.4%), the mortality rate was higher
(16 or 20.2 vs. 3.1%) and the mean cost of hospitalization was
higher (US$ 146,978 or 213,104 vs. 33,851) (13). The study also indicated that
pneumonia survivors had an increased risk of re-hospitalization at
30 days (27.2 or 31.1 vs. 15.3%) and it was concluded that the
cost, staffing levels and material resources used in health care
were higher in ICU patients with ventilator-associated pneumonia
(S. aureus or P. aeruginosa). By reducing the
incidence of hospitalizations in those ICU of patients who may be
extubated in the operating room, the rate of ventilator-associated
pneumonia, hospital morbidity and mortality, as well as
hospitalization cost are accordingly reduced (14).
Early self-awakening of a neurosurgical patient is,
in most cases, a surgeon's request, since obeying orders and
responding to verbal commands indicate, to a certain point,
neurological stability. Namen et al (15) reported a marked increase in
successful extubation in neurosurgical patients with a Glasgow coma
score >8. They identified extubation failure in 61% of patients
with a Glasgow coma score of ≤8(15). The present study was based on these
results and extubation was attempted only in patients who entered
the operating room without intubation and with a Glasgow score of
≥8.
The intention of the present study was to reduce, as
much as possible, the ICU stay of patients and the time on
mechanical ventilation, and the present results confirm what
previous studies reported (11,12,15). In
the present study, it was possible to create a similar setting in
the two groups of patients regarding hemodynamics, respiratory
rate, temperature, SatO2, expired CO2
stability and acid-base balance throughout the surgical event and
up to 24 h later. Therefore, the statistical analysis does not
indicate any significant difference between the groups. This
stability allows for comparison of patients subjected to extubation
at an early stage and those intubated for >8 h after the
surgical procedure. The present study provides a clear indication
that the use of mechanical ventilation may be a factor that
complicates the respiratory status of these patients, leading to
even more serious conditions, including hypostatic pneumonia or
contamination of mechanical ventilators; in addition, due to the
presence of antibiotic-resistant bacteria at the ICU, those
patients are at risk of neuroinfection, a condition with severe
adverse outcomes. This indicates that complications associated with
ventilator use in intensive care may be reduced if the patient
meets the criteria necessary for extubation, in both conventional
and fast track procedures.
For the surgeon, flexibility is required regarding
the previously made decisions that are intended to benefit the
patient. However, a neurosurgeon under pressure should be cautious
not to make any hasty decisions. Hypothermia, pre-existing
neurological damage or damage generated during surgery remain key
points to consider when selecting the time-point of awakening and
extubation for a patient. Finally, it should be remembered that the
protocol for early extubation is not rigid and the fast-track
strategy may be discarded immediately if the patient's condition is
not ideal. With the purpose of standardizing the technique of early
extubation in the management of the neurosurgical patient, rigorous
controlled trials should be performed in the future to further
evaluate techniques.
Fast track should be regarded as a routine technique
in patients who meet the required criteria, so that they may be
discharged faster and with fewer complications that may potentially
endanger their lives or prolong their hospital stay. Deliberate
delay or failed extubation increases the incidence of
post-operative pneumonia, mortality and longer stays in the ICU and
hospital. Another important issue, after considering the patient's
life and safety first, is the economic factor. If the patient is
discharged without admission to the ICU, the economic burden for
the patient, the hospital or the medical insurance company is
significantly reduced.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
GGC designed the experiments, performed experiments,
analyzed data and co-wrote the paper. YNES and BIGC performed the
experiments. DPR designed the experiments and co-wrote the paper.
IPRS, designed part of trial and co-wrote the manuscript. ARMPDL
analyzed data and co-wrote the paper.
Ethical approval and consent to
participate
The present study was authorized by the ethics
committee of Hospital Universitario ‘Dr Jose Eleuterio Gonzalez’
(Monterrey, Mexico) and the research sub-directorate with the
number AN14-003. Patients provided informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Myles PS, Daly DJ, Djaiani G, Lee A and
Cheng DC: A systematic review of the safety and effectiveness of
fast-track cardiac anesthesia. Anesthesiology. 99:982–987.
2003.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Henao FA, Restrepo CE, Botero LF, Arango
MF and Jaramillo AF: Extubación temprana (fast-track) en
neuroanestesia: Una alternativa segura? Rev Col Anest. 32:179–184.
2004.
|
|
3
|
González-Villavelázquez ML,
Castelazo-Arredondo JA and Osorio-Santiago MA: Extubación temprana
en neurocirugía. Revista Mexicana de Anestesiología.
Neuroanestesiología. 28 (Suppl 1):S120–S112. 2005.
|
|
4
|
Souter MJ and Manno EM: Ventilatory
management and extubation. Criteria of the
Neurological/Neurosurgical patient. Neurohospitalist. 3:39–45.
2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mayer SA, Copeland D, Bernardini GL,
Boden-Albala B, Lennihan L, Kossoff S and Sacco RL: Cost and
outcome of mechanical ventilation for life threatening stroke.
Stroke. 31:2346–2353. 2000.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gujjar AR, Deibert E, Manno EM, Duff S and
Diringer MN: Mechanical ventilation for ischemic stroke and
intracerebral hemorrhage: Indications, timing, and outcome.
Neurology. 51:447–451. 1998.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cooper RN: Desintubación segura. In:
Clínicas anestesiológicas de Norte América, Editorial Ciudad de
Mexico, Interamericana Mc Graw Hill, pp680-706, 1995.
|
|
8
|
Bruder N and Ravussin P: Recovery from
anesthesia and postoperative extubation of neurosurgical patients:
A review. J Neurosurg Anesthesiol. 11:282–293. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Borstnar CR and Cardellach F: Farreras
Rozman. Medicina Interna. Elsevier Health Sciences, 2016. American
Society of Anesthesiologist. New Classification of Physical Status.
Anesthesiology. 24(111)1963.
|
|
10
|
Spahn DR and Rossaint R: Coagulopathy and
blood components transfusion in trauma. Br J Anaesthes. 95:130–139.
2005. View Article : Google Scholar
|
|
11
|
Cai YH, Zeng HY, Shi ZH, Shen J, Lei YN,
Chen BY and Zhou JX: Factors influencing delayed extubation after
infratentorial craniotomy for tumour resection: A prospective
cohort study of 800 patients in a Chinese neurosurgical centre. J
Int Med Res. 41:208–217. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Cai YH, Wang HT and Zhou JX: Perioperative
predictors of extubation failure and the effect on clinical outcome
after infratentorial craniotomy. Med Sci Monit. 22:2431–2438.
2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Vora CS, Karnik ND, Gupta V, Nadkar MY and
Shetye JV: Clinical profile of patients requiring prolonged
mechanical ventilation and their outcome in a tertiary care medical
ICU. J Assoc Physicians India. 63:14–19. 2015.PubMed/NCBI
|
|
14
|
Kyaw MH, Kern DM, Zhou S, Tunceli O, Jafri
HS and Falloon J: Healthcare utilization and costs associated with
S. aureus and P. aeruginosa pneumonia in the
intensive care unit: A retrospective observational cohort study in
a US claims database. BMC Health Serv Res. 15(241)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Namen AM, Ely EW, Tatter SB, Case LD,
Lucia MA, Smith A, Landry S, Wilson JA, Glazier SS, Branch CL, et
al: Predictors of successful extubation in neurosurgical patients.
Am J Respir Crit Care Med. 163:658–664. 2001.PubMed/NCBI View Article : Google Scholar
|