Introduction
The ovaries are a pair of structures that are ~15 g
and are attached by ligaments to the lateral pelvic wall and the
uterus. Ovarian vein thrombosis (OVT), which is a rare puerperal
complication, is a type of deep vein thrombosis that can be life
threatening. The right ovarian vein is associated with the site of
thrombosis due to the right ovarian veins being larger than the
left, and due to retrograde flow in the left ovarian veins. The
right ovarian vein joins the inferior vena cava (IVC) below the
right renal vein, and the left ovarian vein drains into the left
renal vein. The right ovarian vein enters the IVC at an acute
angle, which makes it more susceptible to compression. Pregnancy is
a risk factor for OVT with the sudden stagnation of blood within
the dilated ovarian vein combined with contractions during natural
delivery or cesarean sections (CS) (1). CS is a risk factor of OVT (2). OVT occurs in 0.05-0.18% of pregnancies
worldwide, with the incidence rising to 1-2% following caesarean
section (3). In a prospective study,
the incidence of ovarian venous thrombosis was demonstrated to be
0.1% for CS (4).
OVT may result in propagation of the thrombosis into
the IVC. IVC is a central manifestation of deep venous thrombosis
and a major cause of fatal pulmonary embolism (PE) (5). Therefore, ovarian vein and inferior
vena cava thrombosis is the leading cause of maternal mortality
worldwide (6). The diagnosis of
ovarian vein and inferior vena cava thrombosis can be performed
using CT. Blood FDP and D-Dimer and fibrinogen levels can be used
as an indicator of the rapid progression of blood coagulation and
fibrinolysis (7). It has recently
been indicated that early diagnosis and appropriate treatment can
aid in the prevention of these potentially life threatening
complications (8). The current study
reports a case of ovarian vein and inferior vena cava thrombosis
that was effectively treated with no further requirement for
interventional procedures.
Case presentation
A 30-year old pregnant woman presented at the
Maternity and Child Health Hospital of Zhenjiang (Jiangsu, China),
and without complication, gave birth to a second child, a female
weighing 3,200 g, with an Apgar score of 9/10(9). On the second day following a cesarean
section, the patient complained of abdominal soreness in the right
lower abdominal and waist. Physical examination revealed soreness
in the right lower quadrant region. The patients temperature was
36˚C, blood pressure was 112/78 mmHg, respiratory rate was 18
breaths/min and pulse was 82 beats/min. A pelvic examination failed
to identify any abnormalities. The patient's medical and family
history revealed no previous history of any thrombotic events. The
estimated blood loss during the cesarean section was 200 ml.
Laboratory tests performed were as follows: Leukocyte count,
8.3x109/l (reference-range,
4.00-10.00x109/l); hemoglobin, 118 g/l (reference range,
115-175 g/l); platelets 226x109/l (reference range,
100-350x109/l); increased plasma FDP, 11.60-15.40 µg/ml
(reference range, 0.0-5.0 µg/ml); D-Dimer 632-1164 ng/ml (reference
range, 0-255 ng/ml) and fibrinogen, 6.04-7.96 g.l-1
(reference range, 2.38-4.98 g.l-1). Full laboratory test
results are presented in Table I.
Other coagulation parameters such as thrombin time (s) (reference
range, 15.8-24.9), prothrombin time percent activity (reference
range, 80-120), prothrombin time ratio and prothrombin time
international normalized ratio (reference range, 0.82-2.00) were
within normal ranges. Biochemical results for lipid of cholesterol
total and triglyceride and low density lipoprotein were also
remarkably increased (Table
II).
 | Table ILaboratory tests for coagulation
parameters. |
Table I
Laboratory tests for coagulation
parameters.
| Main parameters | Admission | 3 days pre-op | CS | OVT at diagnosis | day of filter op | 1 day filter
post-op | 2 day filter post
op | Follow-up (1
month) | Normal range |
|---|
| Thrombin time
(sec) | 10.40 | 10.80 | 10.80 | 11.00 | 11.80 | 11.80 | 11.60 | 11.10 | 15.8-24.9 |
| Fibrinogen
(g.l-1) | 6.04 | 6.95 | 6.92 | 7.21 | 7.96 | 4.59 | 2.80 | 2.89 | 2.38-4.98 |
| FDP (µg/ml) | 3.80 | 11.60 | 9.70 | 13.60 | 15.40 | 9.70 | 3.50 | 2.50 | 0.0-5.0 |
| PTR ratio | 0.91 | 0.95 | 0.95 | 0.96 | 1.02 | 1.03 | 1.14 | 1.15 | 0.82-2.00 |
| PT-INR | 0.91 | 0.95 | 0.95 | 0.97 | 1.02 | 1.03 | 1.14 | 1.02 | 0.82-2.00 |
| PT percent
activity | 107 | 100 | 89 | 97 | 96 | 120 | 100 | 73 | 80-120 |
| D-dimer | 632 | 1,047 | 1,193 | 1,191 | 1,164 | 998 | 432 | 207 | 0-255 |
 | Table IILaboratory parameters for maternal
lipids. |
Table II
Laboratory parameters for maternal
lipids.
| Main parameters
(mmol/l) | Admission | 3 days pre-op | CS | OVT at diagnosis | day-filter-op | 1 day filter
post-op | Follow-up (1
month) | Normal range |
|---|
| Cholesterol
total | 10.88 | 8.01 | 8.98 | 6.26 | 5.89 | 5.39 | 5.26 | 3.10-5.20 |
| Triglyceride | 4.82 | 4.88 | 5.08 | 5.11 | 5.17 | 5.10 | 3.28 | 0.40-1.70 |
| Low density
lipoprotein | 6.52 | 5.22 | 5.29 | 4.88 | 5.39 | 5.11 | 4.22 | 0.00-3.37 |
| High density
lipoprotein | 2.73 | 1.91 | 1.78 | 1.71 | 1.78 | 1.58 | 1.58 | 1.15-2.00 |
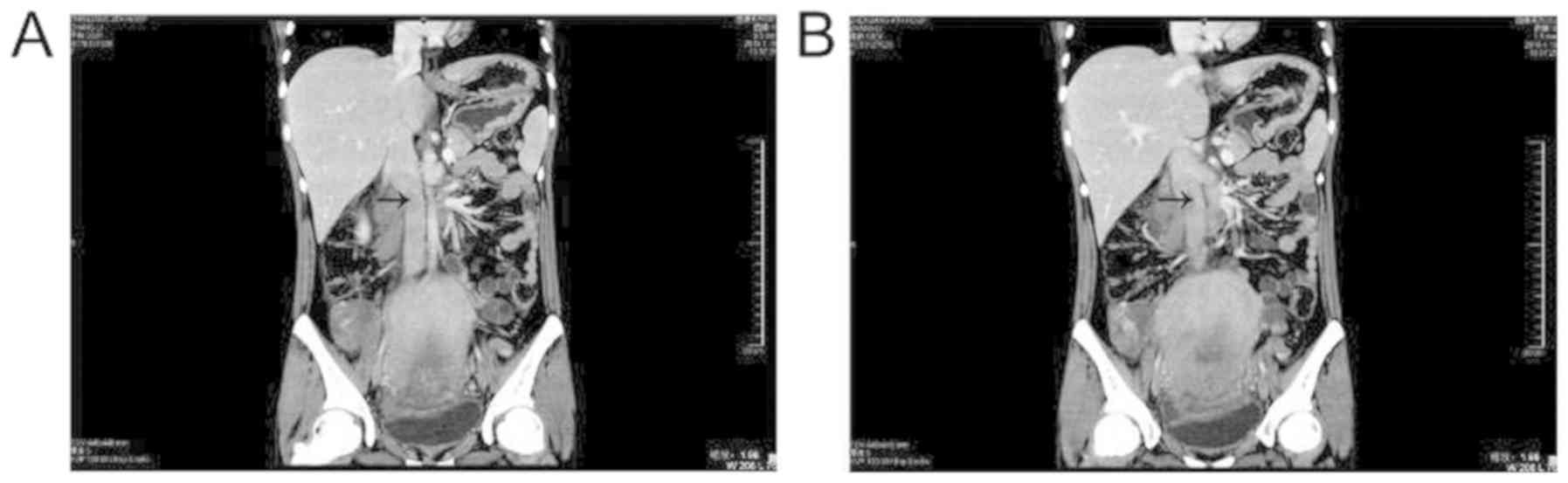
Ultrasonographic examination revealed 5.2x6.5x5.1 cm
hypoechoic areas that were causing filling defects within the right
ovarian vein. CT with contrast enhancement demonstrated a thrombus
in the right ovarian vein and inferior vena cava (Fig. 1), and a diagnosis of OVT and IVC
thrombosis was made.
The treatment of ovarian and inferior vena cava
thrombosis is determined using the clinical scenario and patient
symptoms (10). An anticoagulant
therapy was started with a subcutaneous injection of low molecular
weight heparin calcium (0.4 ml, every 12 h for 7 days), urokinase
as a thrombolytic agent intravenous drip (25 UI/ day for 3 days).
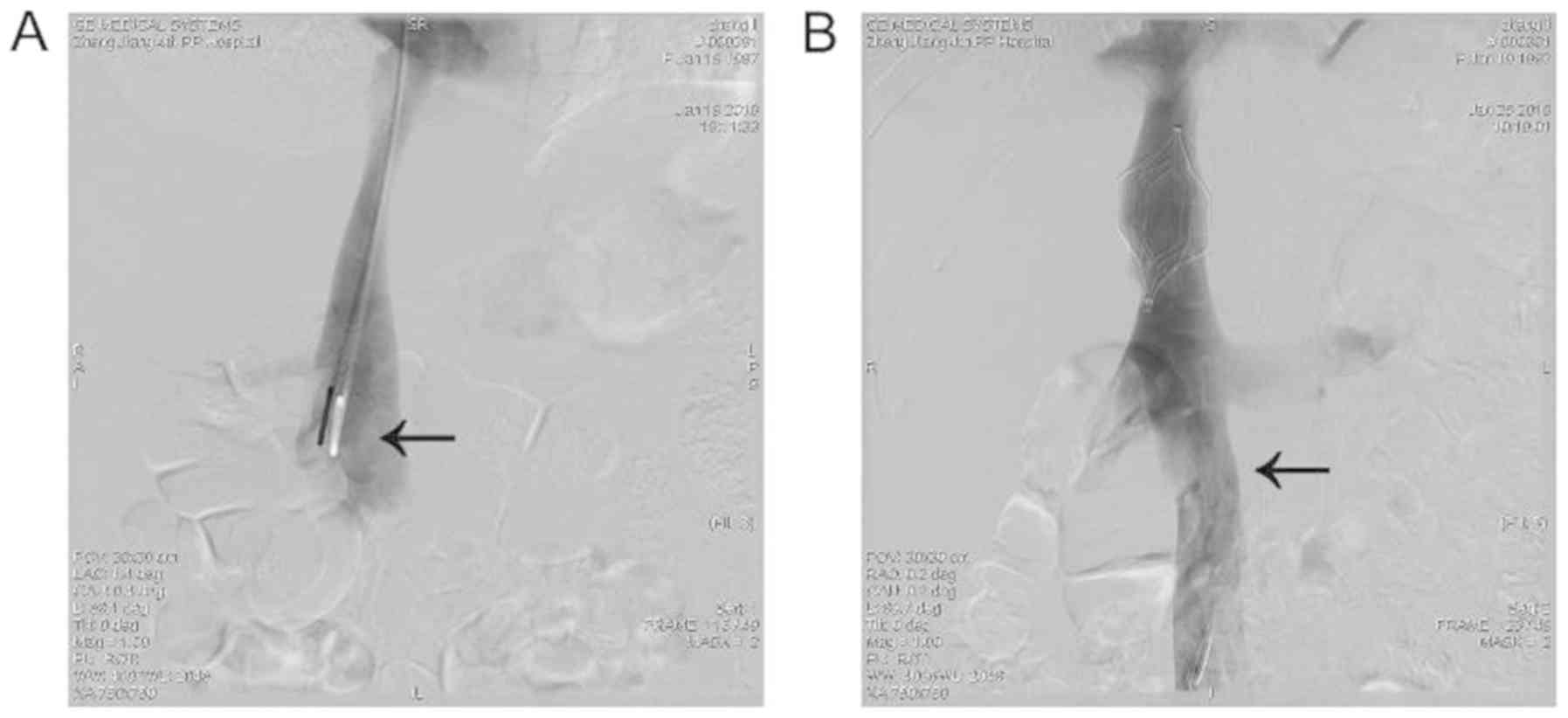
Inferior vena cava filters can be implanted for postpartum OVT to
prevent PE. A vena cava filter (Cordis) was implanted via the right
internal jugular, which was followed by recanalization of the
occluded IVC with the help of a guide wire and catheter (Fig. 2A). A trans-catheter intravenous
thrombolysis was subsequently conducted. On day 10 following
inferior vena cava filter implantation, the filter was retrieved
through the right internal jugular after thrombus was sufficiently
dissolved. This was confirmed via angiography, where the thrombus
in the inferior vena cava disappeared and recanalization of blood
flow occured (Fig. 2B). The patient
was discharged 20 days after the completion of the procedure with
no complications.
Discussion
OVT is characterized by the formation of blood clots
(thrombosis) in the ovarian veins. The pathogenesis of OVT is a
Virchow triad: Venous stasis, endothelial damage and
hypercoagulability (11). In the
current case, the increased total cholesterol and triglyceride and
low density lipoprotein in pregnancy may cause damage to the
endothelial function or increase blood viscosity, which is
beneficial for the formation of atherosclerotic plaque and the
occurrence of thrombosis (12).
Lipids constitute a large part of the arterial wall, as do plasma
and intracellular membranes. Therefore, lipid abnormalities may
lead to endothelial damage and vascular injury (13). Cesarean section raises the risk of
OVT compared with vaginal delivery as when veins are dilated and
blood flow velocity decreases under anesthesia, tissue trauma is
increased, bed rest is prolonged and the incidence of puerperal
infection is higher due to surgery (14).
The early identification of symptomatic OVT and the
precise treatment of OVT is important to prevent life-threatening
complications. CT scan is primarily used to diagnose OVT as it can
assess the extent of thrombosis within the IVC (15). In the current case, dilated right
ovarian vein with thrombi, extending up to the inferior vena cava,
was identified. A diagnosis of OVT and IVC thrombosis was
subsequently made. Pregnant women are at an increased risk of deep
vein thrombosis (16). The patient
in the present study exhibited increased blood FDP and D-Dimer and
fibrinogen levels after CS, further indicating the rapid
progression of blood coagulation and fibrinolysis. OVT is most
commonly treated using anticoagulation therapy (17). There are no standard guidelines for
the dose, duration or drug of choice for anticoagulation treatment.
An anticoagulant therapy was started in the current patient with a
subcutaneous injection of low molecular weight heparin calcium (0.4
ml, every 12 h for 7 days), urokinase as a thrombolytic agent
intravenous drip (25 UI/day for 3 days) and implantation of
inferior vena cava filters. This is the current recommend
anticoagulant therapy for ovarian vein and inferior vena cava
thrombosis due to the lack of high quality evidence for other
treatments. Previous studies have demonstrated that the use of
thrombolysis for OVT can break down blood clots and exhibits some
advantages, including earlier thrombus removal compared with the
use of anticoagulants alone (18-21).
At present, urokinase is one of the common thrombolytic agents
(22). Studies have reported that
urokinase agent combined with implantation of inferior vena cava
filters can aid in dissolving thrombi (23). Inferior vena cava filter has been
widely used in patients with venous thrombosis and no-pregnancy,
effectively preventing PE (24).
During pregnancy, there have been some reports of inferior vena
cava filter, however, these are controversial (25). In the current case, the treatment
received was effective. The patient was treated successively and
was discharged from the hospital after 20 days.
Ovarian vein thrombosis with inferior vena cava is a
very rare condition postpartum condition. Like any other venous
thromboembolic disease, OVT can be fatal and lead to serious
complications, including the extension of the thrombus into the
IVC. These complications can be managed using anticoagulation and
thrombolytic therapy combined with an IVC filter. In the present
case, the timely diagnosis and management of OVT successfully
prevented these potentially life-threatening complications.
Acknowledgements
Not applicable.
Funding
This study was supported by the preventive medicine
program of Jiangsu Provincial Health and Health Committee (grant
no. Y2018062) and the Project of Science and Technology Development
Research Center of National Health and Family Planning Commission
(grant no. W2016CWJS03).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
QW and YL acquired the clinical data. XN performed
the investigation. JL conceived of the methodology. WC, TC and XW
made substantial contributions to conception, and analysis and
interpretation of data. WC was involved in drafting the manuscript
and XW revised it critically for important intellectual content.
All authors produced and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the ethics
committee of the Maternity and Child Health Hospital of Zhenjiang.
Written informed consent was obtained from the patient.
Patient consent for publication
The patient who participated in the study provided
written informed consent for the publication of any associated
data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jenayah AA, Saoudi S, Boudaya F Bouriel I,
Sfar E and Chelli D: Ovarian vein thrombosis. Pan Afr Med J.
21(251)2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Plastini T, Henry D and Dunleavy K:
Ovarian vein thrombus: To treat or not to treat? Blood Advance.
1:1120–1123. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rottenstreich A, Da'as N, Kleinstern G,
Spectre G, Amsalem H and Kalish Y: Pregnancy and non-pregnancy
related ovarian vein thrombosis: Clinical course and outcome.
Thromb Res. 146:84–88. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
See A and Chern B: Contained
intra-abdominal morcellation: Is it the way forward? Gynecol Minim
Invasive Ther. 5:99–101. 2016. View Article : Google Scholar
|
|
5
|
Bates SM, Middeldorp S, Rodger M, James AH
and Greer I: Guidance for the treatment and prevention of
obstetric-associated venous thromboembolism. J Thromb Thrombolysis.
41:92–128. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Assal A, Kaner JD, Danda N, Cohen HW and
Billett HH: Risk factors and prognosis of ovarian vein thrombosis.
Blood Coagul Fibrinolysis. 28:468–474. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cassinelli G and Naggi A: Old and new
applications of non-anticoagulant heparin. Int J Cardiol. 212
(Suppl)(S14-S21)2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Bos AS, Tullius T, Patel M, Leef JA,
Navuluri R, Lorenz JM and Van Ha TG: Indwelling and retrieval
complications of Denali and celect infrarenal vena cavafilters. J
Vasc Interv Radiol. 27:1021–1026. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Iliodromiti S, Mackay DF, Smith GC, Pell
JP and Nelson SM: Apgar score and the risk of cause-specific infant
mortality: A population-based cohort study. Lancet. 384:1749–1755.
2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Murphy EH, Johns B, Varney E and Raju S:
Endovascular management of chronic total occlusions of the inferior
vena cava and iliac veins. J Vasc Surg Venous Lymphat Disord.
5:47–59. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dargaud Y, Rugeri L, Fleury C Battie C,
Gaucherand P, Huissoud C, Rudigoz RC, Desmurs-Clavel H, Ninet J and
Trzeciak MC: Personalized thromboprophylaxis using a risk score for
the management of pregnancies with high risk of thrombosis: A
prospective clinical study. J Thromb Haemost. 15:897–906.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Streiff MB, Agnelli G, Connors JM Crowther
M, Eichinger S, Lopes R, McBane RD, Moll S and Ansell J: Guidance
for the treatment of deep vein thrombosis and pulmonary embolism. J
Thromb Thrombolysis. 41:32–67. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Morelli VM, Lijfering WM, Bos MHA,
Rosendaal FR and Cannegieter SC: Lipid levels and risk of venous
thrombosis: Results from the MEGA-study. Eur J Epidemiol.
32:669–681. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wendelboe AM and Raskob GE: Global burden
of thrombosis: Epidemiologic aspects. Circ Res. 118:1340–1347.
2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kearon C, Akl EA, Ornelas J, Blaivas A,
Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, et
al: Antithrombotic therapy for VTE disease: CHEST guideline and
expert panel report. Chest. 149:315–352. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Farge D and Frere C: Clinical practice
guidelines for prophylaxis of venous thromboembolism in cancer
patients. Thromb Haemost. 116:618–625. 2016.
|
|
17
|
Djakovic I, Mustapic M, Marleku F, Grgic
O, Djakovic Z and Kosec V: Ovarian vein thrombosis-a case report.
Acta Clinica Belg. 70:445–446. 2015. View Article : Google Scholar
|
|
18
|
Hong-Kee N, Mei-Fong C, Azhany Y and
Zunaina E: Antiphospholipid syndrome in lupus retinopathy. Clin
Ophthalmo. 8:2359–2363. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Girolami A, Treleani M, Bonamigo E,
Tasinato V and Girolami B: Venous thrombosis in rare or unusual
sites: A diagnostic challenge. Semin Thromb Haemost. 40:81–87.
2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Liu M and Zhang F: Administration routes
affect thrombolytic effect of catheter-directed thrombolysis with
pro-urokinase in treating deep vein thrombosis. Ann Transl Med.
6(322)2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Harris SA, Velineni R and Davies AH:
Inferior vena cava filters in pregnancy: A systematic review. J
Vasc Interv Radio. 27(354-360.e8)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Angelini M, Barillari G, Londero AP,
Bertozzi S, Bernardi S, Petri R, Driul L and Marchesoni D:
Puerperal ovarian vein thrombosis: Two case reports. J
ThrombThrombolysis. 35:286–289. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wan Z, Xiang R, Wang H, Zhong Q and Tu B:
Comparative efficacy and safety of local and peripheral venous
thrombolytic therapy with urokinase for thrombosed hemodialysis
arteriovenous fistulas. Exp Ther Med. 17:4279–4284. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Bikdeli B, Chatterjee S, Desai NR, Kirtane
AJ, Desai MM, Bracken MB, Spencer FA, Monreal M, Goldhaber SZ and
Krumholz HM: Inferior vena cava filters to prevent pulmonary
embolism: Systematic review and meta-analysis. J Am Coll Cardiol.
70:1587–1597. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Watson L, Broderick C and Armon MP:
Thrombolysis for acute deep vein thrombosis. Cochrane Database Syst
Rev. 11(CD002783)2016.PubMed/NCBI View Article : Google Scholar
|