Introduction
Coronary heart disease (CHD) is a major contributor
to overall mortality. An estimated 3.8 million men and 3.4 million
women die from CHD every year (1-3).
Myocardial ischemia/reperfusion injury is a severe pathological
change associated with CHD, which leads to a reduction in heart
ejection fraction and causes cardiac decompensation (4). Inhibition of apoptosis to prevent
myocardial ischemia/reperfusion injury has long been a therapeutic
target (5).
Flavonoids are a class of natural secondary
metabolites produced by plants and fungi; their molecular structure
is characterized by two phenyl rings and one heterocyclic ring.
Flavonoids display antioxidant and antibacterial effects, both
in vitro and in patients with cardiovascular disease and
cancer (6-8).
Studies conducted on patients with cardiovascular
disorders have demonstrated that flavonoids reduce the risk of
atherosclerosis and hypertension via attenuation of oxidative
stress and the related signaling pathways in blood vessel cells,
and by improving endothelial and capillary function (9,10). The
main factors involved in inflammation include nuclear factor
(NF)-κB and matrix metallopeptidase-9 (MMP-9). The activity of
NF-κB is primarily regulated by interaction with inhibitor of κB
(IkB) proteins; the IkB/NF-κB interaction is a key step for
controlling NF-κB activity. Activation of NF-κB has been widely
reported in the context of several diseases including cancer,
chronic inflammatory disorders, neurodegenerative diseases, and
heart disease (11). Matrix
metalloproteinases are associated with post-myocardial infarction
left ventricular remodeling with MMP-9 identified as the only
circulating factor that predicts late onset of congestive heart
failure (12,13).
Fisetin (3,3',4',7-tetrahydroxyflavone) is present
in various drugs, fruits and vegetables, such as apples, grapes,
onions, and cucumbers (14-16).
Studies have demonstrated that fisetin displays a number of
beneficial properties, including anticancer, anticoagulatory,
anti-inflammatory and antioxidant effects (17-22).
Our previous study determined the anticoagulant and thrombolytic
effect of fisetin in vitro, using heparin as a positive
control (18). However, the
cardioprotective effect of fisetin and the underlying mechanism are
yet to be studied in vivo. Therefore, the present study
explored the potential protective effects of fisetin on ischemic
cardiomyocytes and the underlying mechanism in a rat model of
myocardial ischemia/reperfusion.
Materials and methods
Preparation of reagents and
samples
Enteric coated aspirin tablets were provided by
Luoyang Mingkang Pharmaceutical Co., Ltd (Luoyang, China).
Clopidogrel bisulfate tablets were purchased from Jinan Lekangxin
Pharmaceutical Co., Ltd. (Jinan, China). Dipyridamole injection was
purchased from Yabao Pharmaceutical Group Co., Ltd. (Ruicheng,
China). Adrenaline hydrochloride injection was provided by Tianjin
Jinyao Amino Acid Co., Ltd. (Tianjin, China). Aspirin, adenosine
5'-diphosphate disodium salt and arachidonic acid were purchased
from Sigma-Aldrich (Merck KGaA, Darmstadt, Germany). Fisetin and
quercetin (purity >98%) were purchased from Shaanxi Chang Yue
Plant Technology Co., Ltd. (Xi'an, China). Prothrombin Time kit (PT
kit), Activated Partial Thromboplastin Time kit (APTT kit) and
Thrombin Time kit (TT kit) were purchased from Shanghai Sunred
Biological Technology Co., Ltd. (Shanghai, China). NF-κB and MMP-9
detection kits and 5% bovine serum albumin were provided by Wuhan
Boster Biological Technology, Ltd. (Wuhan, China). Annexin
V-fluorescein isothiocyanate (FITC)/propidium iodide (PI) apoptosis
detection kit was purchased from Nanjing KGI Biological Technology
Development Co., Ltd. (Nanjing, China). Other reagents used in the
study were of analytical grade.
Animal experiments
Male Sprague-Dawley (SD) rats (age, 8 weeks; weight,
250-300 g) were purchased from the Animal Center of Xi'an Jiaotong
University College of Medicine (Xi'an, China). The animals were
housed under 12-h light-/dark cycle at 26±3˚C 30-70% humidity.
Ad libitum access to standard rodent chow and water was
provided. All animal experiments were approved and conducted
according to the experimental protocol authorized by the Ethical
Committee of the First Affiliated Hospital of Xi'an Medical
College.
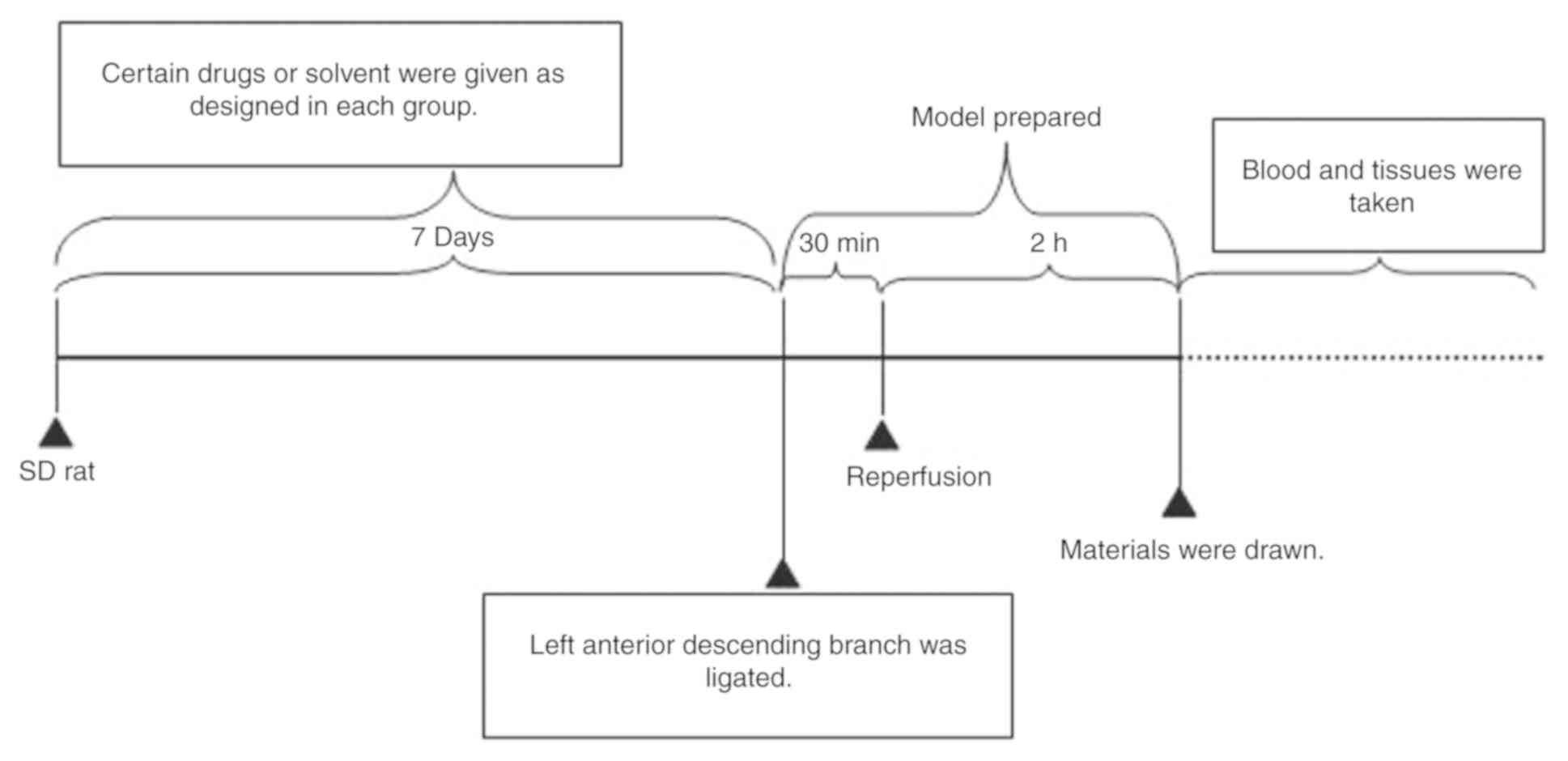
Eighty-four SD rats were randomly divided into seven
groups: Sham operation group (negative control); model group; three
fisetin-pretreated groups (5, 15 and 45 mg/kg);
quercetin-pretreated; and aspirin-pretreated groups. Rats in the
sham control and model groups were administered 0.5% sodium
carboxymethyl cellulose (CMC-Na) solution (10 ml/kg) by gavage
administration. Rats in the other groups were pretreated with
solutions containing the varying concentrations of fisetin, aspirin
or quercetin in 0.5% CMC-Na by gavage administration once per day
for 7 days. The dosage of aspirin and quercetin was determined by
preliminary experiments and through reference to published
literature (18,23,24). On
day 8, rats were anesthetized with 10% chloral hydrate (350 mg/kg,
4 ml/kg) and fixed in the dorsal position for operation. A two-lead
electrocardiogram (ECG) was connected to the depilated skin and
rats were mechanically ventilated. Tracheotomy was performed for
endotracheal intubation. The ventral thorax was incised
transversely at the level of intercostal spaces 4 to 6 to expose
the heart. The left anterior descending branch was ligated.
Successful surgery was confirmed by observing cyanosis around the
remote end of myocardium and ST-segment elevation and tall T-waves
in ECG (25-27).
After 30 min of ligation, 2 h of reperfusion was initiated by
removing the ligation line (Fig. 1).
After 2 h of reperfusion rats were euthanized. The rats were first
anesthetized with 10% chloral hydrate (350 mg/kg, 4 ml/kg) and kept
areflexive with muscular flaccidity. An ~8 ml volume of blood was
then taken from the abdominal aorta leading to rat death, which was
confirmed by respiratory and cardiac arrest.
Preparation of drug solution
To prepare 6x10-3 mol/l fisetin solution,
127 µl 1% sodium carbonate (Na2CO3) solution
was added into a mixing tube containing 1.72 mg fisetin powder.
Quercetin solution (6x10-3 mol/l) was prepared by
dissolving 1.81 mg of quercetin in 127 µl 1%
Na2CO3 solution. Dipyridamole solution
(120x10-6 mol/l) was prepared by dissolving 12.1 µl
dipyridamole (2 ml: 10 mg) in saline and adjusting the volume to 1
ml. Aspirin solution (3 mg/ml) was prepared by dissolving 3 mg
aspirin in 1% Na2CO3 solution and adjusting
the total volume to 1 ml. Clopidogrel (360 µg/ml) was prepared by
dissolving 0.36 mg clopidogrel in saline and adjusting the volume
to 1 ml. Sodium citrate solution (3.8%) was prepared by dissolving
1.9 g sodium citrate in saline and adjusting to 50 ml. Adrenaline
(120 µmol/l) was prepared by dissolving 13.2 µl adrenaline
hydrochloride injection (1 mg/ml) with saline and adjusting the
volume to 500 ml. Adenosine diphosphate (ADP) solution (3,000
µmol/l) was diluted with saline to the desired concentration before
use.
Preparation of platelets
Six healthy adult human blood specimens were
provided by the First Affiliated Hospital of Xi'an Medical
University (Xi'an, China; 3 men and 3 women; age, 33.7±8.9 years).
The anti-coagulant used was 3.8% sodium citrate (sodium citrate:
Whole blood, 1:9) and blood was drawn from the median cephalic
vein. Blood samples were centrifuged at 179 x g for 10 min to
remove the supernatant and platelet-rich plasma (PRP); the
remaining sample was centrifuged at 1016 x g for 10 min to collect
platelet-poor plasma (PPP). The platelet number in PRP was adjusted
with PPP to obtain a final platelet count of 250/nl (28). These procedures were performed at
room temperature to prevent platelet activation. All six patients
provided written informed consent for the collection and use of
their blood samples. In addition, the collection and use of the
blood samples was approved by the Research Ethics Committee of the
Affiliated Hospital of Xi'an Medical University.
Platelet aggregation
Human platelet aggregation was determined using a
four-channel platelet aggregation analyzer (SC-2000; Shanghai
Tiancheng Science and Technology Ltd, Shanghai, China). PRP samples
(300 µl; 250 platelets/nl) were pooled in the sample cup and
treated with saline, fisetin (1x10-4, 1x10-5,
1x10-6, 1x10-7, 1x10-8 or
1x10-9 mol/l), quercetin (1x10-4,
1x10-5, 1x10-6, 1x10-7,
1x10-8 or 1x10-9 mol/l), clopidogrel
(3x10-5 mol/l), dipyridamole (2x10-6 mol/l)
or aspirin (2.8x10-4 mol/l), respectively. Light
transmission was first measured following incubation of the sample
at 37˚C for 20 min, and then measured after platelet activation
with ADP (20 µmol/l) and adrenaline (20 µmol/l). Light transmission
was set as 0 and 100% for measurement of pure PPP and PRP,
respectively. Inhibition of platelet aggregation was calculated
according to the following formula: Percentage inhibition
(%)=[1-(platelet aggregation of sample/platelet aggregation of
control)] x100%. Each sample was measured in triplicate.
Coagulation indicators
Two drops of blood from the rat-tail vein were
collected in a glass tube to measure the clotting time. A total of
4 ml of blood was collected from the abdominal aorta in a vacuum
tube containing anticoagulant (3.8% sodium citrate: Whole blood,
1:9). The blood was centrifuged at 1,016 x g for 15 min to collect
plasma, at room temperature. Plasma was separated to measure the
PT, TT and APTT, according to their kit instructions. Plasma levels
of Von Willebrand factor (vWF) were assessed using a vWF ELISA kit
(cat. no. H274; Nanjing Jiancheng Biological Technology Co., Ltd.,
Nanjing, China).
Annexin V and PI staining for
cardiomyocyte apoptosis
Apoptosis of cardiomyocytes was measured using flow
cytometry. In brief, a 5 mm3 sample (~70 mg) of the left
ischemic myocardium was obtained following reperfusion. The
ischemic myocardium was then washed in D-Hanks solution and
digested in 10 ml 0.08% trypsin for 5 min at room temperature. The
suspension was filtered through a 200-micron mesh nylon filter to
collect the filtrate, then, 10 ml culture medium containing calf
serum was added to terminate the digestion. After centrifugation of
the suspension for 10 min, at 1,016 x g and room temperature, the
supernatant was discarded, and cells were resuspended in 5 ml
culture medium containing calf serum. Cells were then washed with
PBS and resuspended in a binding buffer. FITC-conjugated Annexin V
(3 µl) and PI reagent (3 µl) were added and the mixture was
incubated at room temperature for 20 min. The samples were
immediately measured by flow cytometer (FACSCalibur, BD
Biosciences, USA). Apoptosis was calculated as the percentage of
apoptotic cardiomyocytes (Annexin V+/PI-)
using CellQuest software (ver 4.0; BD Biosciences) (29-31).
Expression of NF-κB and MMP-9
NF-κB and MMP-9 expression was determined by
immunohistochemistry. A 5 mm3 sample of left ischemic
myocardium (~70 mg) was obtained from each rat after reperfusion,
fixed in 10% formalin solution for 24 h at room temperature and
embedded in paraffin. Paraffin-embedded samples were cut into 3 µm
thick slices and mounted on glass slide. The tissue sections were
immersed in 10 volumes of 3% hydrogen peroxide for 10 min at 70˚C
to block endogenous peroxidase activity, deparaffinized and then
subjected to antigen retrieval with 0.01 mmol/l citrate solution
(pH 6.0) for 50 sec at 80-90˚C. Next, the sections were washed in
PBS. After treatment with 5% bovine serum albumin (Wuhan Boster
Biological Technology. Ltd.) for 20 min at room temperature, the
sections were incubated with the following primary antibodies in a
moist chamber: Anti-NF-κB (1:100; cat. no. BM3940; Wuhan Boster
Biological Technology Ltd., China) for 180 min at 4˚C and
anti-MMP-9 (1:80; cat. no. BA0573; Wuhan Boster Biological
Technology. Ltd.) overnight at 4˚C. The sections were washed twice
in PBS and incubated with the labeled streptavidin-biotin complex
(1:1; cat. no. SA1022; Wuhan Boster Biological Engineering Co.
Ltd.) for 30 min at 37˚C. The slices were colored with
diaminobenzylamine chromogenic reagent at room temperature, stained
with hematoxylin, dehydrated, permeabilized and sealed, according
to immunohistochemical staining kit instructions (NF-κB, cat.no.
BM3940; MMP-9 cat no. BA0573; Wuhan Boster Biological Engineering
Co. Ltd.). The slides were examined under a light microscope at
x400 magnification, eight slides per group and five fields of view
per slide (32). MMP-9 and NF-κB
expression were assessed as described in the literature using an
Olympus BX51 positive position microscope for image analysis
(Olympus Corporation, Tokyo, Japan), using immunohistochemical
method and transmission method for qualitative and quantitative
analysis. Images were further analyzed with Image Pro Plus 6.0
(Media Cybernetics, Inc., Rockville, MD, USA). Using the
transmission method, gray levels of each IHC image of MMP-9 and
NF-κB staining were taken. Gray levels range from 0 to 255, where
white is 255 and black is 0. Τhrough the combination of
trichromatic color shades, a variety of colors can be formed, where
the smaller the gray scale, the deeper color, which can be used to
indicate higher expression levels. In the present study, the
expression of MMP-9 or NF-κB was calculated as=255-their respective
gray levels.
Evaluation of myocardial infarct size
(IS)
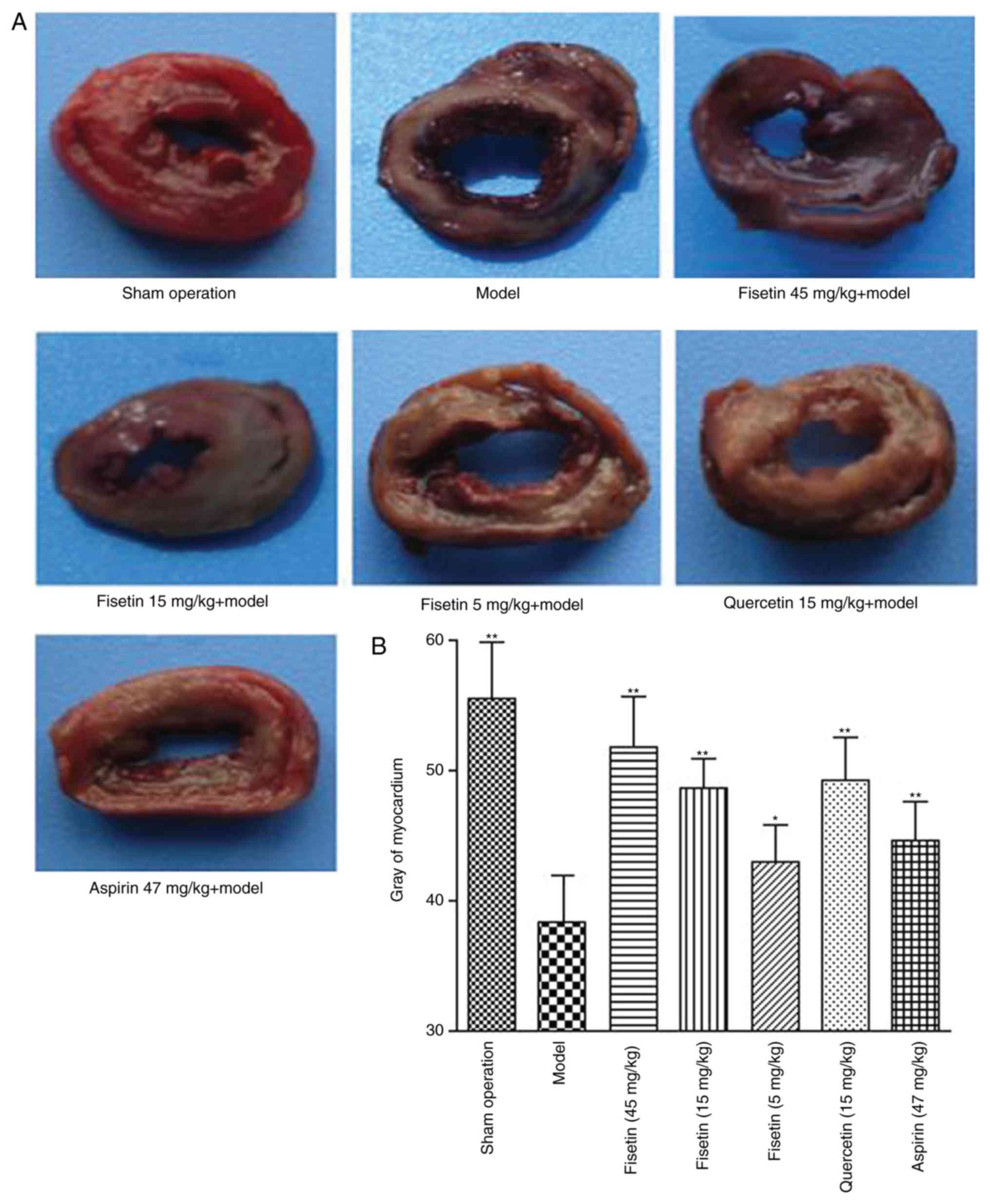
To evaluate myocardial IS,
2,3,5-triphenyltetrazolium (TTC) staining was used. After 2 h of
reperfusion, rat hearts were harvested (four samples per group) and
then immersed in 1% TTC buffer for 20 min at 37˚C. The tissues were
then incubated at -20˚C for 20 min. Subsequently, the hearts were
washed with saline and attached blood vessels and fat removed.
Serial 1 mm sections from the tip of the heart to the base of the
heart were prepared. Viable myocardium was stained deep-red,
penumbra was stained light-red and infracted/necrotic myocardium
stained pale grey or remained unstained, as previously described
(33). The sections were viewed
under a light microscope (Nikon Corporation, Tokyo, Japan;
magnification, x400). The area of the myocardium stained grey was
assessed with Image Pro Plus 6.0 (Media Cybernetics, Inc.)
(34-37).
A higher density of staining suggested that more viable myocardial
cells remained (38).
Examination of pathological changes in
myocardial cells
H&E staining was used to examine the
pathological changes in the myocardial cells. Hearts were excised,
washed with ice-cold PBS, and 1 mm thick coronal slices prepared
after the hearts were snap frozen at -20˚C for 20 min. The slices
were fixed directly in 10% neutral formalin for 24 h at room
temperature and paraffin-embedded., Sections (3 µm thickness) were
prepared from paraffin-embedded tissue blocks by dehydration
through a graded ethanol series and clearing with xylene for
H&E staining (for 12 min at room temperature). Morphological
changes in the myocardial tissues were evaluated as previously
described, using an Olympus light microscope (magnification, x400)
(39,40).
Statistical methods
Data were presented as mean ± standard error of the
mean. One-way analysis of variance followed by Dunnett's test was
used for comparisons of more than two groups. Statistical analyses
were performed using SPSS 13.0 (SPSS, Inc., Chicago, IL, USA)
statistical software package. P<0.05 was considered to indicate
statistical significance.
Results
Fisetin significantly prolongs
coagulation in rats with myocardial ischemia/reperfusion
injury
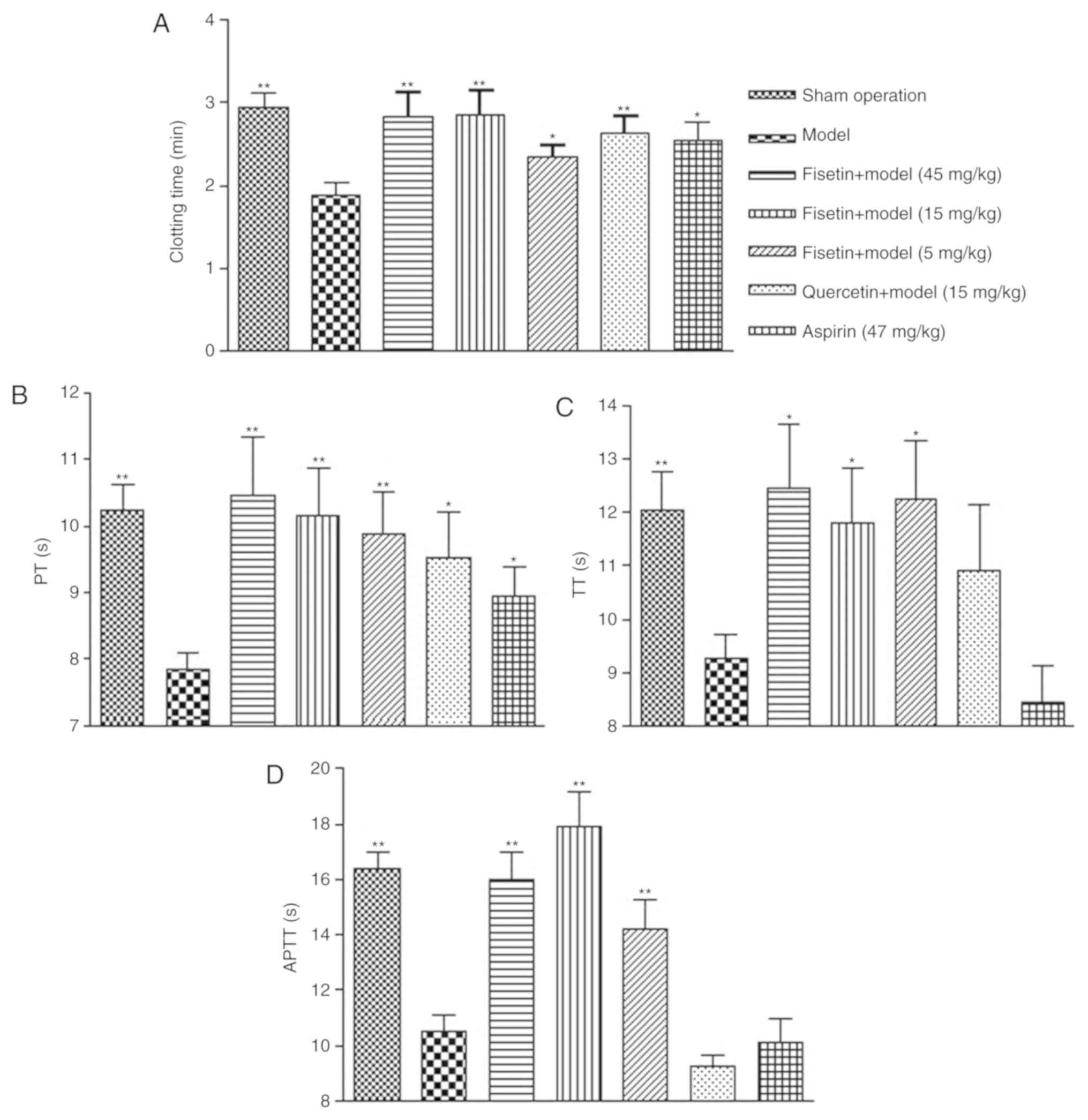
The whole blood clotting time (CT) of rats in the
group pretreated with fisetin was significantly prolonged compared
with the model group (P<0.01 for 15 and 45 mg/kg fisetin;
P<0.05 for 5 mg/kg fisetin; Fig.
2A). CT was comparable between groups pretreated with fisetin
(15 or 45 mg/kg) and groups pretreated with quercetin (15 mg/kg) or
aspirin (47 mg/kg). Similar results were observed for PT, TT, and
APTT. Fisetin treatment (5, 15, or 45 mg/kg) significantly
prolonged PT, TT, and APTT in a dose dependent manner (Fig. 2B-D). Similarly, quercetin (15 mg/kg)
and aspirin (47 mg/kg) significantly improved PT compared with the
model group (P<0.05). Of note, the anticoagulant effect of
fisetin was superior to quercetin and aspirin.
Fisetin significantly reduces plasma
vWF in rats with myocardial ischemia/reperfusion injury
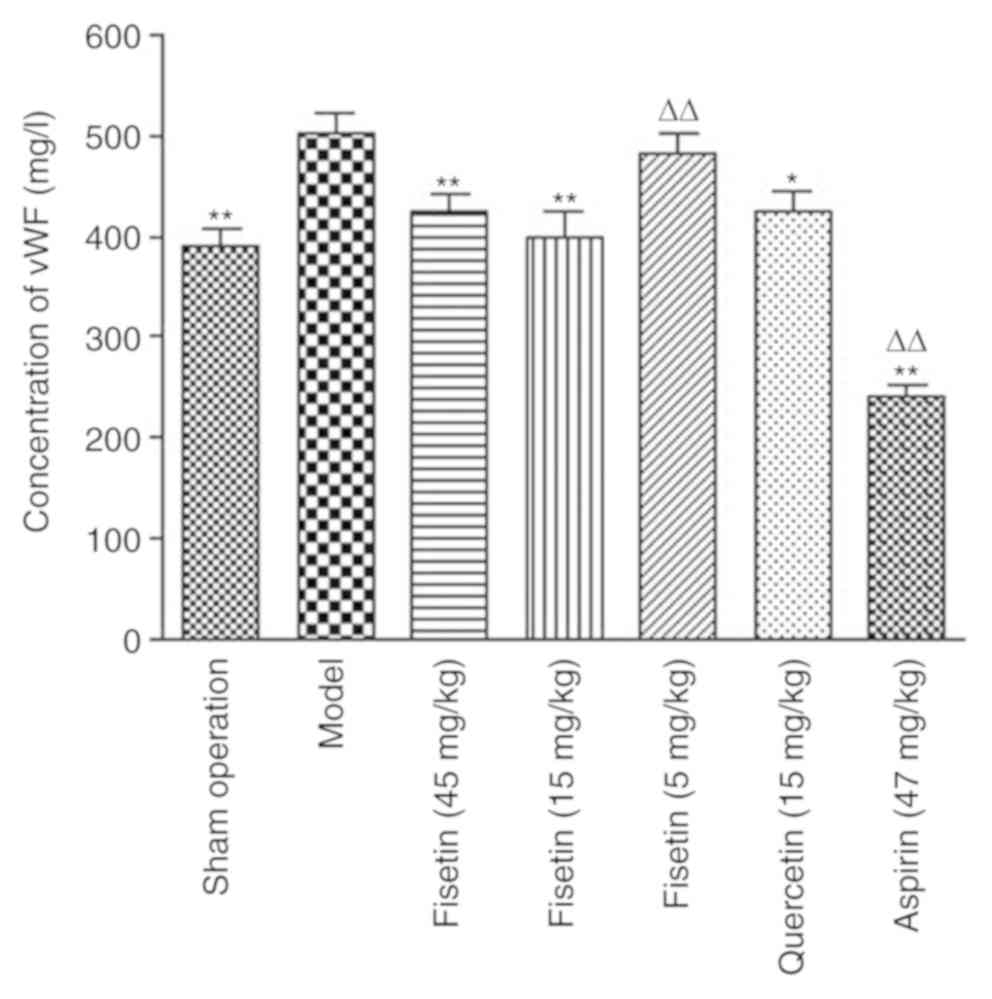
Plasma vWF levels in fisetin (15 and 45 mg/kg)
pretreated groups were significantly lower than the model group
(P<0.01; Fig. 3), which suggested
that fisetin may inhibit platelet aggregation by reducing the
levels of vWF.
Fisetin reduces acute myocardial
ischemia/reperfusion injury in rats
TTC staining was used to investigate the effects of
fisetin on acute myocardial ischemia/reperfusion injury (Fig. 4A). The infarct areas in the groups
pretreated with fisetin were significantly reduced compared with
the model group in a dose-dependent manner (P<0.01; Fig. 4B).
Fisetin alters morphological
presentation of cardiomyocytes
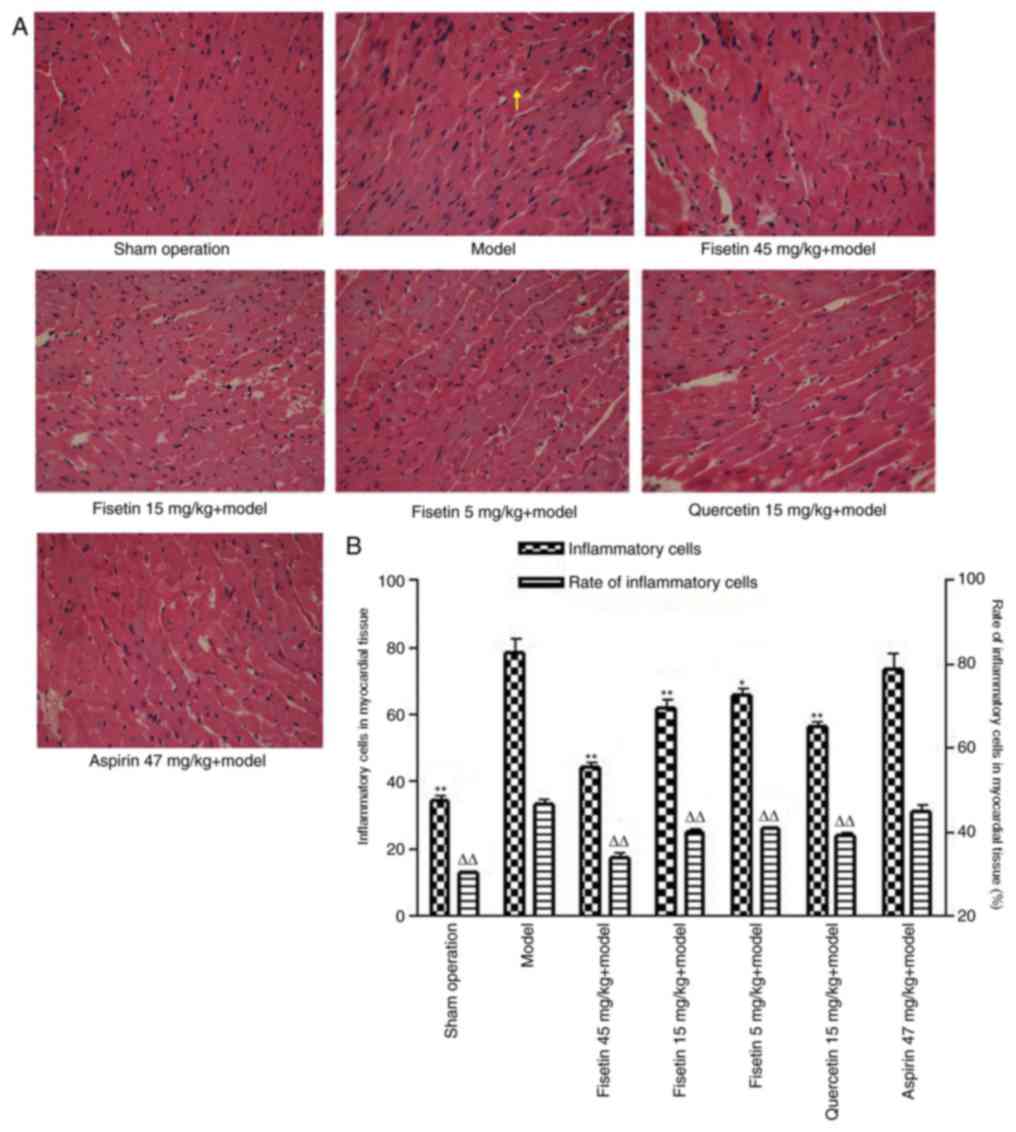
In the sham group, the myocardial fibers were
arranged in an orderly manner, the horizontal grain structure was
clear and there were almost no inflammatory cells (Fig. 5A). The presence of inflammatory cells
within myocardial fibers would indicate neutrophil infiltration, a
common occurrence in myocardial ischemia-reperfusion injury. In the
myocardial ischemia/reperfusion model group, the myocardial fibers
were arranged irregularly and their structure was disordered. Parts
of the horizontal grain structure were not clear or had
disappeared, the gaps between muscle fibers had widened, some of
the myocardial cells appeared necrotic and there were numerous
inflammatory cells in the myocardial matrix (Fig. 5A). Compared with the model group,
myocardial cells in the fisetin-pretreated group demonstrated less
notable structural changes and a reduced number of inflammatory
cells (Fig. 5A). Fisetin-pretreated
groups demonstrated less disarrangement of cardiac muscle
filaments, decreased cardiomyocyte edema or phagocytic cells,
reduced disrupted myofilaments, and less membrane rupture and
nuclear swelling when compared to the myocardial ischemia
reperfusion group (Fig. 5A). By
counting the number of infiltrative neutrophils, dividing this by
the number of cardiomyocytes in the same field of vision and
multiplying by 100 the proportion of infiltrating inflammatory
cells was estimated. Inflammatory cell counts, and the proportions
of inflammatory cells in myocardial tissue were also significantly
decreased in the fisetin-pretreated groups (Fig. 5B).
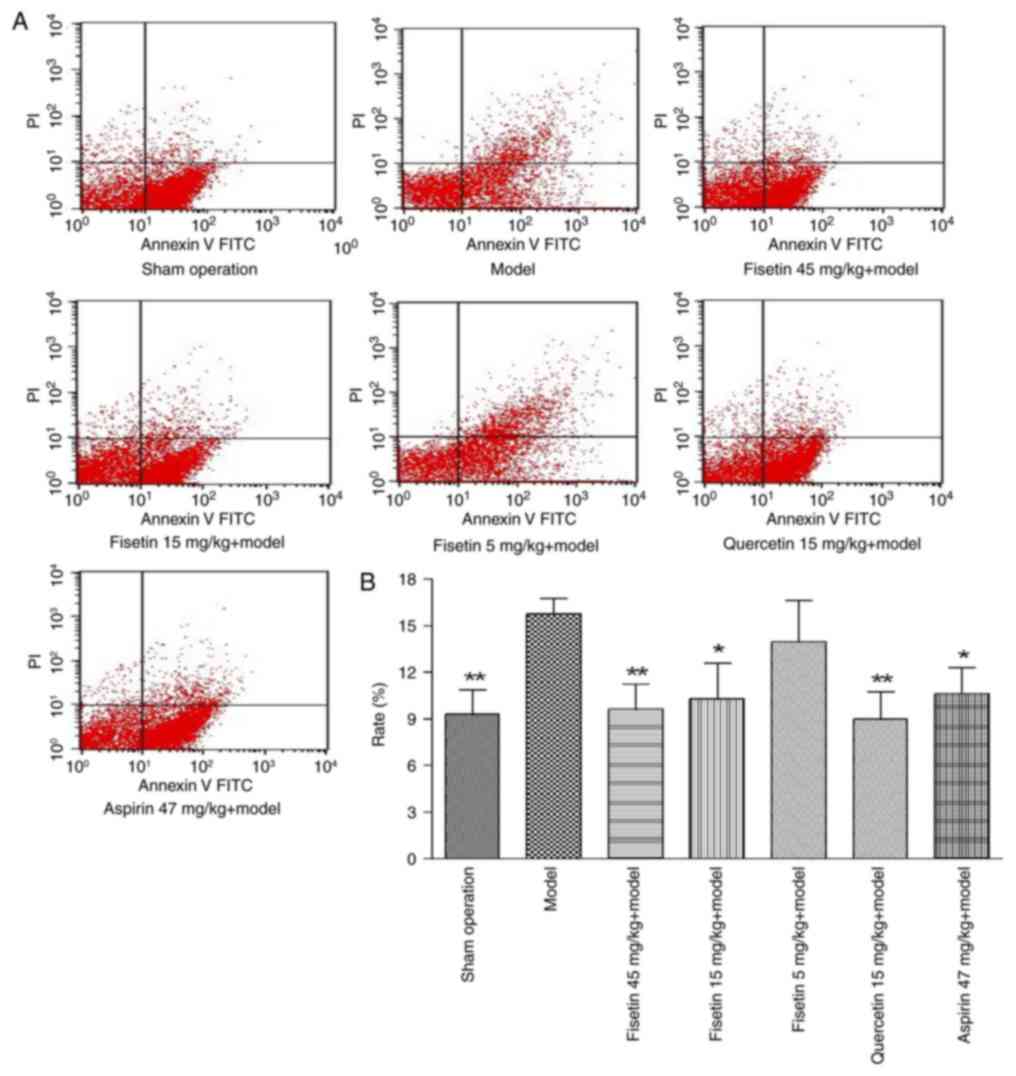
Fisetin reduces apoptosis in
cardiomyocytes
Flow cytometry analysis with annexin V/PI staining
was performed to determine the effect of fisetin on cardiomyocyte
apoptosis. Compared with the model group, fisetin treatment (15 or
45 mg/kg) significantly decreased the percentage of apoptotic
cardiomyocytes (P<0.01 or P<0.05; Fig. 6). These results indicated that
fisetin inhibited apoptosis of myocardial cells in the rat model of
ischemia/reperfusion injury in a dose dependent manner.
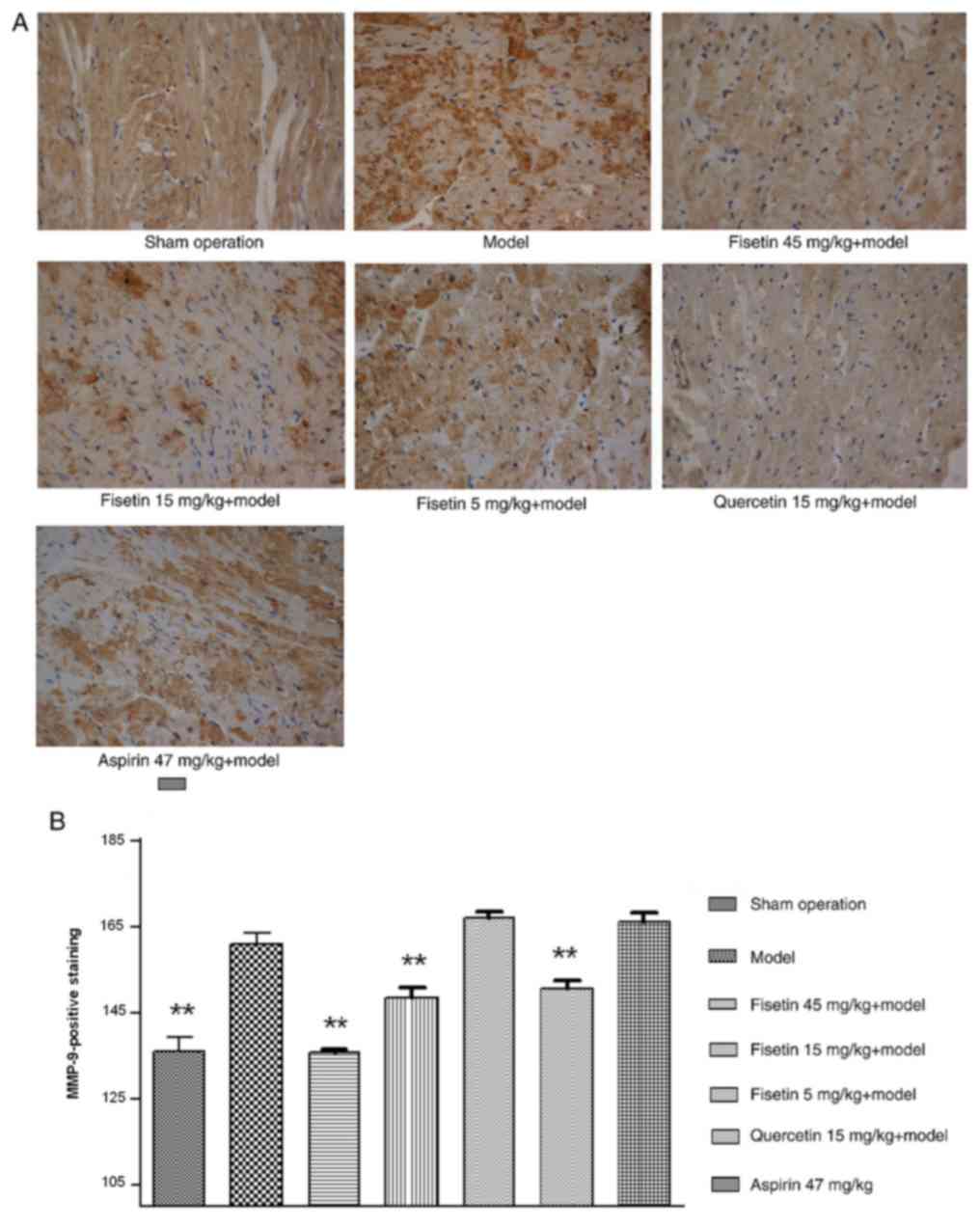
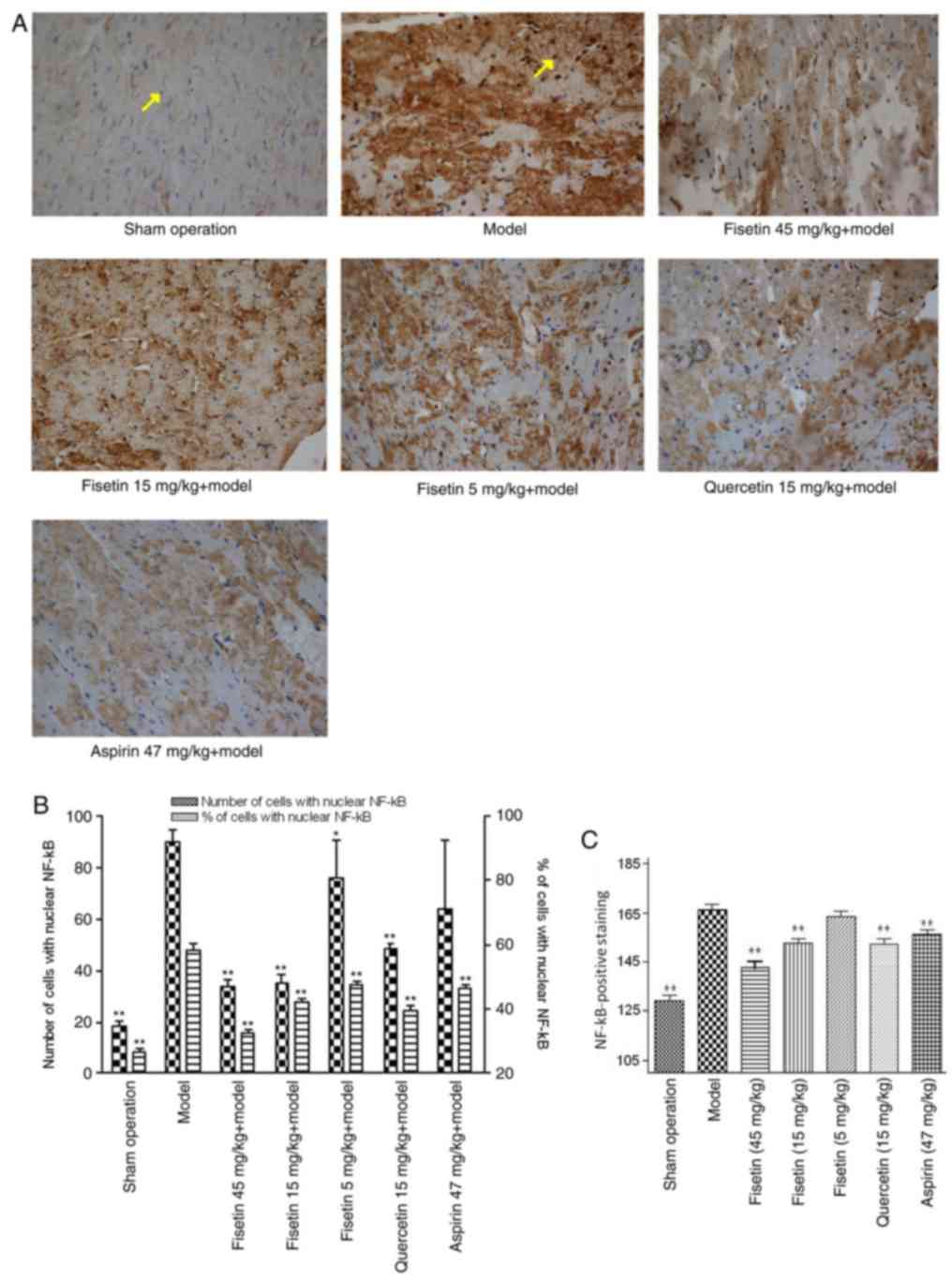
Fisetin reduces NF-κB and MMP-9
expression in ischemic myocardium
The expression of MMP-9 was significantly attenuated
in fisetin (15 and 45 mg/kg) pretreated groups compared with the
model group (P<0.01; Fig. 7A and
B). NF-κB was stained yellow/brown
and mainly appeared in the cytoplasm for the sham group. The model
group showed abundant expression of NF-κB with a significant shift
to the nucleus. NF-κB expression was significantly inhibited in
fisetin and quercetin-pretreated groups compared with the model
group, demonstrating decreased NF-κB expression with wide
cytoplasmic distribution (P<0.01; Fig. 8A-C).
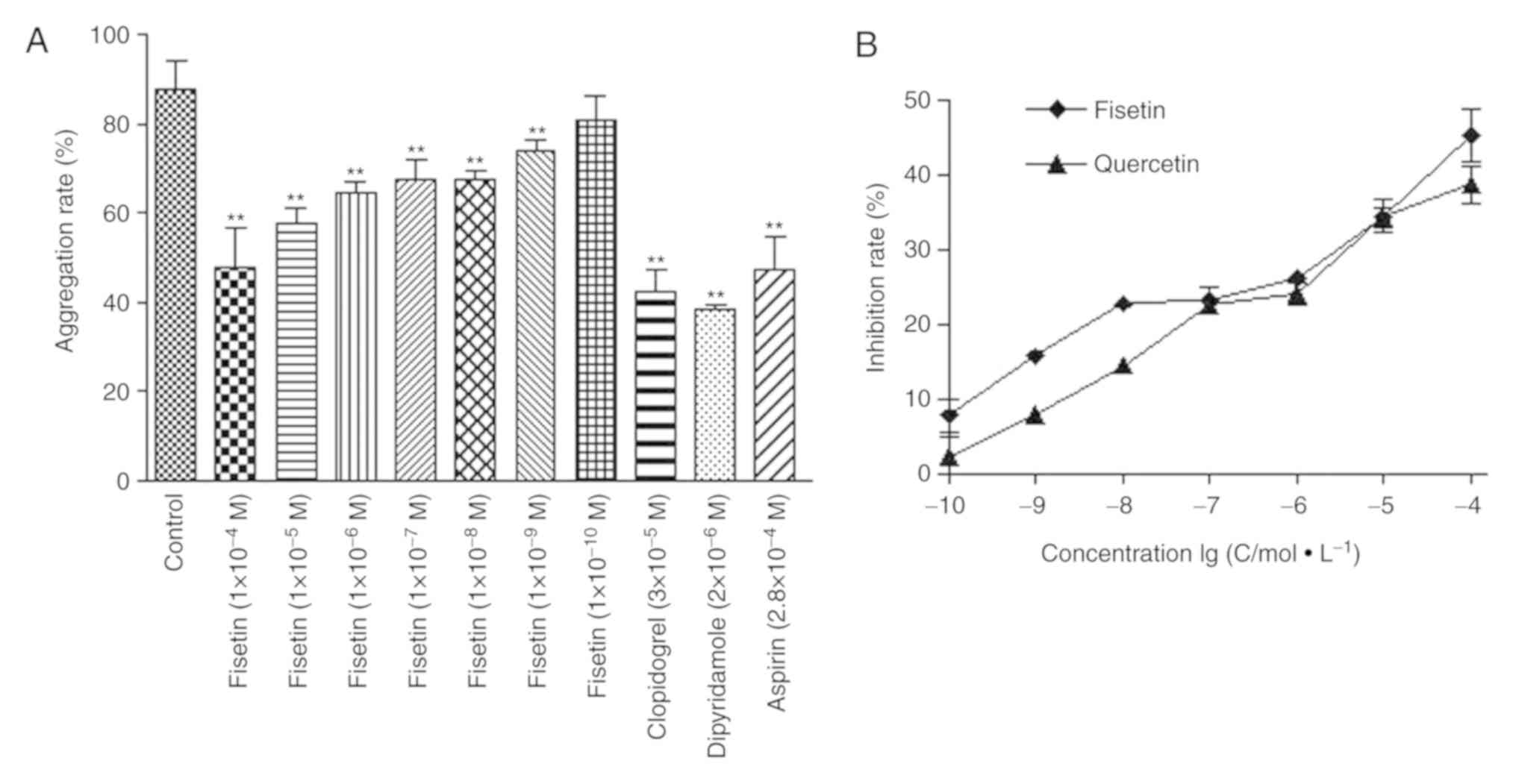
Fisetin significantly reduces platelet
aggregation rate in human blood samples
The effect of fisetin on platelet aggregation was
further tested in human blood samples in vitro. The rates of
platelet aggregation following fisetin
(1x10-9-1x10-5 M), dipyridamole
(2x10-6 mol/l), clopidogrel (3x10-5 mol/l),
and aspirin (2.8x10-4 mol/l) treatments were
significantly lower compared with the control group (P<0.01;
Fig. 9A). In addition, the
antiplatelet coagulation of fisetin and quercetin was dose
dependent with half maximal inhibitory concentration of
4.54x10-7 mol/l and 2.71x10-7 mol/l for
fisetin and quercetin, respectively (Fig. 9B).
Discussion
Flavonoids are 2-phenyl chromone natural compounds
found in plants, which promote growth, development, flowering,
fruition, and prevent bacterial diseases. Flavonoids have been
demonstrated to protect against multiple liver and cardiovascular
disorders by virtue of their antibacterial, antiviral, antitumor,
antioxidant, anti-inflammatory, and analgesic properties (6,7). The
present study tested the antiplatelet coagulation effect of fisetin
in a rat model of myocardial ischemia/reperfusion injury, and
compared the effect with that of quercetin and aspirin (positive
controls). The aim was to demonstrate the antiplatelet effect of
fisetin against ischemia/reperfusion injury and to confirm the
effect of fisetin on MMP-9 and NF-κB expression.
Coagulation parameters, CT, APTT, PT and TT, are
typically used to assess anticoagulation. CT and APTT reflect the
functional status of the intrinsic coagulation system, PT reflects
the functional status of the extrinsic coagulation system and TT is
used to determine the presence or absence of excess anticoagulant
in circulation (41,42). The present study demonstrated that
fisetin significantly increased CT, PT, APTT and TT in rats due to
its remarkable antithrombotic effects (43).
vWF is involved in postvascular injury platelet
activation following subendothelial damage leading to collagen
exposure (44). Platelet activation
induced by vWF and collagen allows platelets to adhere to
subendothelial matrix (45), which
induces coagulation and the release of ADP from platelet dense
granules (46,47). Additionally, vWF has been suggested
to be causally involved in the pathogenesis of myocardial
infarction (48). Therefore, the
present study tested the effect of fisetin on vWF levels, and
identified that vWF levels were significantly reduced in
fisetin-pretreated groups. These findings suggested that vWF was
also involved in fisetin-triggered antiplatelet coagulation.
Platelet adhesion, aggregation and release are vital
steps of thrombosis induced by platelet activation due to factors
such as ADP, collagen, thrombin and 5-hydroxytyptamine receptors
(49-51).
In vitro experiments demonstrated that fisetin strongly
inhibited ADP-induced platelet aggregation in blood samples, which
suggested that fisetin may be a potential antiplatelet
aggregator.
Furthermore, it was also observed that fisetin
treatment reduced cardiomyocyte apoptosis in rats. Flow cytometry
determined the rate of myocardial apoptosis, whilst morphological
changes were observed with H&E staining. Cardiomyocyte
apoptosis has long been reported to serve an important role in
exacerbating myocardial ischemia/reperfusion injury and is known to
be limited to the infarct zone. Considering that apoptosis is
regulated by multiple factors including inflammatory proteins, the
expressions of NF-κB and MMP-9 in myocardial tissues was
investigated. NF-κB and MMP-9 expression in fisetin-pretreated
groups was significantly downregulated compared with the model
group. Tissue expression of MMP-9 in myocardial
ischemia-reperfusion is the mechanism of myocardial small blood
vessel wall injury, cell edema and white blood cell infiltration
(51,52). Early selective inhibition of MMP-9
can significantly reduce the myocardial infarct area (52). Wang et al (53) demonstrated that MMP expression was
reduced in rats with myocardial ischemia-reperfusion injury
following total flavones of Hippophae rhamnoides
pre-treatment. Lee et al identified (54) that fisetin decreases apoptotic cell
death and intracellular reactive oxygen species by enhancing the
expression of Cu/Zn-superoxide dismutase as well as phosphorylation
of protein kinase B and extracellular regulated kinase (ERK) 1/2.
Fisetin significantly decreases apoptosis through inhibition of
cleaved caspase-3 and BCL2 associated X protein expression, and by
enhancing the expression of antiapoptotic enzyme as well as Bcl-2
in H2O2-stimulated H9c2 cells (54). Previous studies have determined that
fisetin induces cancer cell apoptosis via the mitogen-activated
protein kinase signaling pathway, mitochondria-mediated pathway, or
inhibiting heat shock transcription factor 1 activity (55-57).
In summary, the present study was the first to
evaluate the antiplatelet and antithrombotic effects of fisetin,
both in vitro and in vivo. These findings suggested
that fisetin protected against myocardial ischemia/reperfusion
injury by inhibiting apoptosis and by regulating the signaling
pathways involved in the inflammatory and coagulation reaction.
Acknowledgements
Not applicable.
Funding
The study was supported by the Key Research Project
of Shaanxi Science and Technology Agency (grant no. 2017SF-345) and
the Third Batch Key Construction Projects of Xi'an Medical
University (grant no. 2015-97).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LHL and HLY designed the study. LHL, XMM, LJL, XLH,
BQ, HLY, KLZ, JND, KL and KY performed the experiments. Data were
collated by XMM and LL and the results of data were discussed by
KL, KLZ, BQ and LHL. LHL, XMM and XLH prepared the figures. XM,
LJL, KY, HLY and LHL wrote the first draft of the manuscript. All
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
All animal and healthy human blood experiments were
approved and conducted according to the experimental protocol
authorized by the Ethical Committee of the First Affiliated
Hospital of Xi'an Medical College.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wong CX, Sun MT, Lau DH, Brooks AG,
Sullivan T, Worthley MI, Roberts-Thomson KC and Sanders P:
Nationwide trends in the incidence of acute myocardial infarction
in Australia, 1993-2010. Am J Cardiol. 112:169–173. 2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kramarow E, Lubitz J and Francis R Jr:
Trends in the coronary heart disease risk profile of middle-aged
adults. Ann Epidemiol. 23:31–34. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Braga JR, Tu JV, Austin PC, Chong A, You
JJ, Farkouh ME, Ross HJ and Lee DS: Outcomes and care of patients
with acute heart failure syndromes and cardiac troponin elevation.
Circ Heart Fail. 6:193–202. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Neri M, Riezzo I, Pascale N, Pomara C and
Turillazzi E: Ischemia/reperfusion injury following acute
myocardial infarction: A critical issue for clinicians and forensic
pathologists. Mediators Inflamm. 4(7018393)2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Portt L, Norman G, Clapp C, Greenwood M
and Greenwood MT: Anti-apoptosis and cell survival: A review.
Biochim Biophys Acta. 1813:238–259. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wei Q, Yin Y, Xi M, Zhou D, Zhu Y, Guan Y,
Guo C, Wang Y, Duan J and Wen A: Antioxidant properties of
magnesium lithospermate B contribute to the cardioprotection
against myocardial ischemia/reperfusion injury in vivo and in
vitro. J Tradit Chin Med. 33:85–91. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wang Y, Zhang ZZ, Wu Y, Zhan J, He XH and
Wang YL: Honokiol protects rat hearts against myocardial ischemia
reperfusion injury by reducing oxidative stress and inflammation.
Exp Ther Med. 5:315–319. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wang L, Ma YT, Xie X, Yang YN, Fu ZY, Li
XM, Liu F, Huang Y, Ma X, Chen BD, et al: Interaction between MMP-9
gene polymorphisms and smoking in relation to myocardial infarction
in a Uighur population. Clin Appl Thromb Hemost. 18:72–78.
2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sinha R, Srivastava S, Joshi A, Joshi UJ
and Govil G: In-vitro anti-proliferative and anti-oxidant activity
of galangin, fisetin and quercet in: Role of localization and
intermolecular interaction in model membrane. Eur J Med Chem.
79:102–109. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chen PY, Ho YR, Wu MJ, Huang SP, Chen PK,
Tai MH, Ho CT and Yen JH: Cytoprotective effects of fisetin against
hypoxia-induced cell death in PC12 cells. Food Funct. 6:287–296.
2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pasparakis M: Regulation of tissue
homeostasis by NF-kappaB signalling: Implications for inflammatory
diseases. Nat Rev Immunol. 9:778–788. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
12
|
Li JL, Chen XL and Sheng LP: Research of
the latest brain injury and MMP-9. J Gen Pract. 271–272. 2011.
|
|
13
|
Wagner DR, Delagardelle C, Ernens I, Rouy
D, Vaillant M and Beissel J: Matrix metalloproteinase-9 is a marker
of heart failure after acute myocardial infarction. J Card Fail.
12:66–72. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Nićiforović N, Mihailović V, Masković P,
Solujić S, Stojković A and Pavlović Muratspahić D: Antioxidant
activity of selected plant species; potential new sources of
natural antioxidants. Food Chem Toxicol. 48:3125–3130.
2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Valianou L, Stathopoulou K, Karapanagiotis
I, Magiatis P, Pavlidou E, Skaltsounis AL and Chryssoulakis Y:
Phytochemical analysis of young fustic (Cotinus coggygria
heartwood) and identification of isolated colourants in historical
textiles. Anal Bioanal Chem. 394:871–882. 2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Savikin K, Zdunic G, Jankovic T,
Stanojkovic T, Juranic Z and Menkovic N: In vitro cytotoxic and
antioxidative activity of Cornus mas and Cotinus coggygria. Nat
Prod Res. 23:1731–1739. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tripathi R, Samadder T, Gupta S, Surolia A
and Shaha C: Anticancer activity of a combination of Cisplatin and
fisetin in embryonal carcinoma cells and xenograft tumors. Mol
Cancer Ther. 10:255–268. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cui EX, Long LH, Zhang JQ, Shao HY and Liu
LL: Extracorporeal anticoagulant and dissolving thrombus effects of
Fisetin and Quercetin. J Chin Med Mat. 32:1111–1113. 2009.(In
Chinese).
|
|
19
|
Park HH, Lee S, Oh JM, Lee MS, Yoon KH,
Park BH, Kim JW, Song H and Kim SH: Anti-inflammatory activity of
fisetin in human mast cells (HMC-1). Pharmacol Res. 55:31–37.
2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sengupta B, Banerjee A and Sengupta PK:
Interactions of the plant flavonoid fisetin with macromolecular
targets: Insights from fluorescence spectroscopic studies. J
Photochem Photobiol B. 80:79–86. 2005.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ivanova D, Gerova D, Chervenkov T and
Yankova T: Polyphenols and antioxidant capacity of Bulgarian
medicinal plants. J Ethnopharmacol. 96:145–150. 2005.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sengupta B, Banerjee A and Sengupta PK:
Investigations on the binding and antioxidant properties of the
plant flavonoid fisetin in model biomembranes. FEBS Lett.
570:77–81. 2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yang Y and Qian ZY: Effect of crocetin on
platelet aggregation in rats. Chin J Nat Med. 5:374–378. 2007.
|
|
24
|
Cui EX, Long LH, Liu J and Cao YX:
Anti-coagulation of cotinus coggygria scop. J Chin Med Mat.
30:202–205. 2007.(In Chinese).
|
|
25
|
Mennander AA, Vuohelainen V, Aanismaa RS,
Narkilahti S, Paavonen T and Tarkka M: Sildenafil after cardiac
arrest and infarction; an experimental rat model. Scand Cardiovasc
J Suppl. 47:58–64. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Jin J, Chen F, Wang Q, Qiu Y, Zhao L and
Guo Z: Inhibition of TNF-α by cyclophosphamide reduces myocardial
injury after ischemia-reperfusion. Ann Thorac Cardiovasc Surg.
19:24–29. 2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ding YF, Zhang MM and He RR: Ischemic
preconditioning reduces cardiomyocytic apoptosis in rabbit heart in
vivo. Sheng Li Xue Bao. 52:220–224. 2000.PubMed/NCBI(In Chinese).
|
|
28
|
Long LH, Cao YX, Ma Z and Liu J:
Anticoagulant, anti-aggregation and antithrombotic effects of a
novel hexapeptide. J Pharm Pharmacol. 63:1454–1461. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Maulik N, Sasaki H, Addya S and Das DK:
Regulation of cardiomyocyte apoptosis by redox-sensitive
transcription factors. FEBS Lett. 485:7–12. 2000.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Galang N, Sasaki H and Maulik N: Apoptotic
cell death during ischemia/reperfusion and its attenuation by
antioxidant therapy. Toxicol. 148:111–118. 2000.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gabai VL, Meriin AB, Yaglom JA, Wei JY,
Mosser DD and Sherman MY: Suppression of stress kinase JNK is
involved in HSP72-mediated protection of myogenic cells from
transient energy deprivation HSP72 alleviates the stewss-induced
inhibition of JNK dephosphorylation. J Biol Chem. 275:38088–38094.
2000.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yu-hui H, Yun F, Fen J and Xing L: Study
about cardiomyocyte apoptosis in myocardial ischemic-reperfusion
injury of rats and NF-κB p65, iNOS expression. Xi Bao Yu Fen Zi
Mian Yi Xue Za Zhi. 26:868–870. 2010.PubMed/NCBI(In Chinese).
|
|
33
|
Yang F, Zhao WL, Mi QY, Xie LP, Liu Z,
Zhang W, Li XZ, Huang Y and Ji Y: Assessment of myocardial
ischemia-reperfusion injury with two different staining methods.
Acta Univ Med Nanjing (Nat Sci). 29:1055–1058. 2009.
|
|
34
|
Fantinelli JC, Gonzalez Arbelaez LF, Perez
Nunez IA and Mosca SM: Protective effects of
N-(2-mercaptopropionyl)-glycine against ischemia-reperfusion injury
in hypertrophied hearts. Exp Mol Pathol. 94:277–284.
2013.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chen J, Petrov A, Yaniz-Galende E, Liang
L, de Haas HJ, Narula J and Hajjar RJ: The impact of pressure
overload on coronary vascular changes following myocardial
infarction in rats. Am J Physiol Heart Circ Physiol. 304:H719–H728.
2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Cao Z, Ren D, Ha T, Liu L, Wang X,
Kalbfleisch J, Gao X, Kao R, Williams D and Li C: CpG-ODN, the TLR9
agonist, attenuates myocardial ischemia/reperfusion injury:
Involving activation of PI3K/Akt signaling. Biochim Biophys Acta.
1832:96–104. 2013.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Bacaksiz A, Teker ME, Buyukpinarbasili N,
Inan O, Tasal A, Sonmez O, Erdogan E, Turfan M, Akdemir OC and
Ertas G: Does pantoprazole protect against reperfusion injury
following myocardial ischemia in rats? Eur Rev Med Pharmacol Sci.
17:269–275. 2013.PubMed/NCBI
|
|
38
|
Yu YP, Xu QQ, Zheng MZ and Wei EQ: Light
transmission measurement of focal ischemic cerebral infarction in
mice. Zhejiang Da Xue Xue Bao Yi Xue Ban. 31:91–93. 2002.PubMed/NCBI(In Chinese).
|
|
39
|
Kou YY, Zha XD, Li YF and Ge RL: The
antioxidative effect of Sanwei Tanxiang powder on rats' hearts
against myocardial ischemia and reperfusion injury. Zhong Yao Cai.
31:1013–1015. 2008.PubMed/NCBI(In Chinese).
|
|
40
|
Zhang Q, Rui X and Cai D: Protective
effect of Ginaton on rat liver microcirculation disturbance
following liver xenotransplantation. Zhonghua Yi Xue Za Zhi.
80:706–708. 2000.PubMed/NCBI(In Chinese).
|
|
41
|
Ashraf HS, Hussain I, Siddiqui AA, Ibrahim
MN and Khan MU: The outcome of living related kidney
transplantation with multiple renal arteries. Saudi J Kidney Dis
Transpl. 24:615–619. 2013.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Burton TM, Lacey M, Liu F, Yu Y, Monsalvo
ML, Lang K and Sander S: One-year follow-up healthcare costs of
patients hospitalized for transient ischemic attack or ischemic
stroke and discharged with aspirin plus extended-release
dipyridamole or clopidogrel. J Med Econ. 15:1217–1225.
2012.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Violi F, Basili S, Berger JS and Hiatt WR:
Antiplatelet therapy in peripheral artery disease. Handb Exp
Pharmacol. 547–563. 2012.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Weber R, Brenck J and Diener HC:
Antiplatelet therapy in cerebrovascular disorders. Handb Exp
Pharmacol. 519–546. 2012.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Horton S and Augustin S: Activated
clotting time (ACT). Methods Mol Biol. 992:155–167. 2013.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Papayannis AC, Abdel-Karim AR, Mahmood A,
Rangan BV, Makke LB, Banerjee S and Brilakis ES: Association of
coronary lipid core plaque with intrastent thrombus formation: A
near-infrared spectroscopy and optical coherence tomography study.
Catheter Cardiovasc Interv. 81:488–493. 2013.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Lv Y, Ren Y, Sun L, Wang S, Wei M and Jia
D: Protective effect of Na(+)/Ca (2+) exchange blocker KB-R7943 on
myocardial ischemia-reperfusion injury in hypercholesterolemic
rats. Cell Biochem Biophys. 66:357–363. 2013.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Ueno H and Harrington WF:
Temperature-dependence of local melting in the myosin subfragment-2
region of the rigor cross-bridge. J Mol Biol. 190:59–68.
1986.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Manchikanti L, Falco FJ, Benyamin RM,
Caraway DL, Kaye AD, Helm S II, Wargo BW, Hansen H, Parr AT, Singh
V, et al: Assessment of bleeding risk of interventional techniques:
A best evidence synthesis of practice patterns and perioperative
management of anticoagulant and antithrombotic therapy. Pain
Physician. 16 (2 Suppl):SE261–SE318. 2013.PubMed/NCBI
|
|
50
|
Vanstreels L, Molenberghs G and Voigt JU:
Secondary stroke prevention: Misguided by guidelines? Acta Cardiol.
67:431–438. 2012.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Torres-Urrutia C, Guzmán L,
Schmeda-Hirschmann G, Moore-Carrasco R, Alarcón M, Astudillo L,
Gutierrez M, Carrasco G, Yuri JA, Aranda E and Palomo I:
Antiplatelet, anticoagulant, and fibrinolytic activity in vitro of
extracts from selected fruits and vegetables. Blood Coagul
Fibrinolysis. 22:197–205. 2011.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Joffs C, Gunasinghe HR, Multani MM, Dorman
BH, Kratz JM, Crumbley AJ III, Crawford FA Jr and Spinale FG:
Cardiopulmonary bypass induces the synthesis and release of matrix
metalloproteinases. Ann Thorac Surg. 71:1518–1523. 2001.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Wang HT, Wang SM, Yun TTS, G. H and Wang
ZZ: Effects of sindacom on the expressions of MMP-9 and myocardial
ischemia reperfusion injury of rats. J Chin Gerontol. 30:2619–2621.
2010.(In Chinese).
|
|
54
|
Lee JS, Lee JS, Cha KJ, Kim DE, Lee D,
Jung SY, Park ES and Kim IS: Fisetin protects H9c2 cardiomyoblast
cells against H2O2-induced apoptosis through
Akt and ERK1/2 signaling pathways. Mol Cell Toxicol. 14:183–192.
2018.
|
|
55
|
Kang KA, Piao MJ, Madduma Hewage SR, Ryu
YS, Oh MC, Kwon TK, Chae S and Hyun JW: Fisetin induces apoptosis
and endoplasmic reticulum stress in human non-small cell lung
cancer through inhibition of the MARK signaling pathway. Tumour
Biol. 37:9615–9624. 2016.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Kim JA, Lee S, Kim DE, Kim M, Kwon BM and
Han CH: Fisetin, a dietary flavonoid, induces apoptosis of cancer
cells by inhibiting HSF1 activity through blocking its binding to
the hsp70 promoter. Carcinogenesis. 36:696–706. 2015.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Kang KA, Piao MJ and Hyun JW: Fisetin
induces apoptosis in human nonsmall lung cancer cells via a
mitochondria-mediated pathway. In Vitro Cell Dev Biol Anim.
51:300–309. 2015.PubMed/NCBI View Article : Google Scholar
|