Introduction
The influence of nasal or oral breathing patterns on
craniofacial growth and development has been widely debated in the
orthodontic literature (1).
According to Moss's functional matrix theory, normal nasal
respiratory function is necessary for the balanced growth of
craniofacial structures. Nasal respiration along with other
functions of the craniofacial complex, e.g., mastication and
swallowing, influence the amount and direction of craniofacial
growth (2). Mouth breathing (MB) may
result in several functional transformations, including changes in
tongue position, as well as the oral and peri-oral muscular
balance. Studies on MB have also reported changes in the posture of
head and neck, which appears to facilitate oral breathing by
increasing airflow through the upper airway (3).
The etiology of MB may be multifactorial and
attributable to anatomic factors, including narrow airways,
adenotonsillar hypertrophy, nasal septal deviation, nasal polyps,
respiratory allergies, nasal turbinate hypertrophy and sleep
position (4). Irrespective of the
cause, chronic MB results in several morphological changes and is
known to cause ‘adenoid facies’ (5).
It is characterized by a narrow upper dental arch, retroclined
mandibular incisors, an incompetent lip seal, a steep mandibular
plane angle and an increased anterior facial height (6). Several studies have analyzed the facial
morphological characteristics of mouth breathers and compared them
with a cohort of nasal breathers (4,7-10).
While the majority of studies indicated the presence of significant
facial morphological changes in mouth breathers, others have failed
to elicit direct evidence of an association between respiratory
patterns and specific facial skeletal changes or malocclusions
(10-12).
Literature is also devoid of comprehensive level-1 evidence in the
form of a systematic review and meta-analysis to firmly establish
any cause-effect association. The aim of the present study was,
therefore, to perform a systematic literature search and analyze
available evidence to assess the difference in facial
characteristics of children and adolescents who are mouth breathers
or nasal breathers.
Materials and methods
Inclusion and exclusion criteria
The present systematic review was performed
following the Preferred Reporting of Items for Systematic reviews
and Meta-Analyses guidelines (13).
A search was performed for cross-sectional, case-control studies
reporting cephalometric measures of mouth-breathing individuals.
The inclusion criteria were as follows: i) Studies performed on
children and adolescents. ii) Studies comparing cephalometric data
with a control group of nasal breathers. ii) Studies not including
participants who had undergone surgery for airway obstruction or
had undergone orthodontic treatment.
Studies that were performed on syndromic individuals
or a cohort of specific malocclusion (e.g., studies performed on
class 2 division 1 malocclusion) were excluded. Studies reporting
incomplete data, uncontrolled studies, those published in a
language other than English, case reports, abstracts and review
papers were also excluded.
Search strategy and data
extraction
Two reviewers independently searched the PubMed,
Medline via OVID, Scopus, Web of Science and Google Scholar
databases for studies published from 1st January 1980 to
1st April 2019. The key-words used in various
combinations were as follows: ‘Mouth breathers’; ‘nasal breathers’;
‘facial morphology’; ‘facial characteristics’; ‘growth pattern’;
‘malocclusion’; ‘dentofacial’; ‘skeletal’ and ‘cephalometric’. The
search strategy and results are provided in Table SI. Studies were initially evaluated
at the title and abstract level. Full-text manuscripts of relevant
entries were analyzed further based on the inclusion/exclusion
criteria. Any disagreement was resolved by discussion. References
of included studies and review articles were manually searched to
identify additional articles.
Data were extracted by two authors independently and
included the following: Authors' names, country of origin, year of
publication, study design, etiology and diagnosis of MB, number of
participants, and demographic and cephalometric data. Corresponding
authors were contacted via email for missing data.
Risk of bias assessment
The assessment criteria from a previous
meta-analysis from 2013(14) on
patients with obstructive sleep apnea were modified and used for
evaluation of the quality of the studies included. Articles were
analyzed independently based on 5 criteria relevant to clinical
research in his area. Studies were rated as ‘Yes’, ‘No’ or
‘Unclear’ on the following questions: i) Was the control group
appropriately matched? ii) Were diagnostic criteria for MB
adequately defined? iii) Was the reliability of cephalometric
tracing measured? iv) Was the cephalometric evaluator masked? v)
Were the cephalometric landmarks used in the study pre-defined?
Studies were initially scored by two reviewers
independently. The scores were later matched and any disagreement
resolved by discussion.
Statistical analysis
Meta-analysis was performed only if at least 3
studies reported similar cephalometric data. Mean and standard
deviation of the scores of cephalometric values were used for
estimating the pooled effect size. Review Manager [RevMan, version
5.3; 2014; Nordic Cochrane Centre (Cochrane Collaboration)] was
used for the analysis. Heterogeneity was calculated using the
I2 statistic. I2 values <25% indicated no
heterogeneity, 25-50% represented low heterogeneity, values of
50-75% medium and >75% represented substantial heterogeneity.
However, even in cases of low or no heterogeneity, a random-effects
model was used for the meta-analysis due to heterogeneities that
exist in the samples and other geographical and methodological
variations amongst the included studies. The influence of each
study on the pooled effect size was analyzed using a sensitivity
analysis. By using the one-study-out method, it was assessed
whether deleting each individual study significantly changed the
pooled results of the meta-analysis.
Results
Search outcome
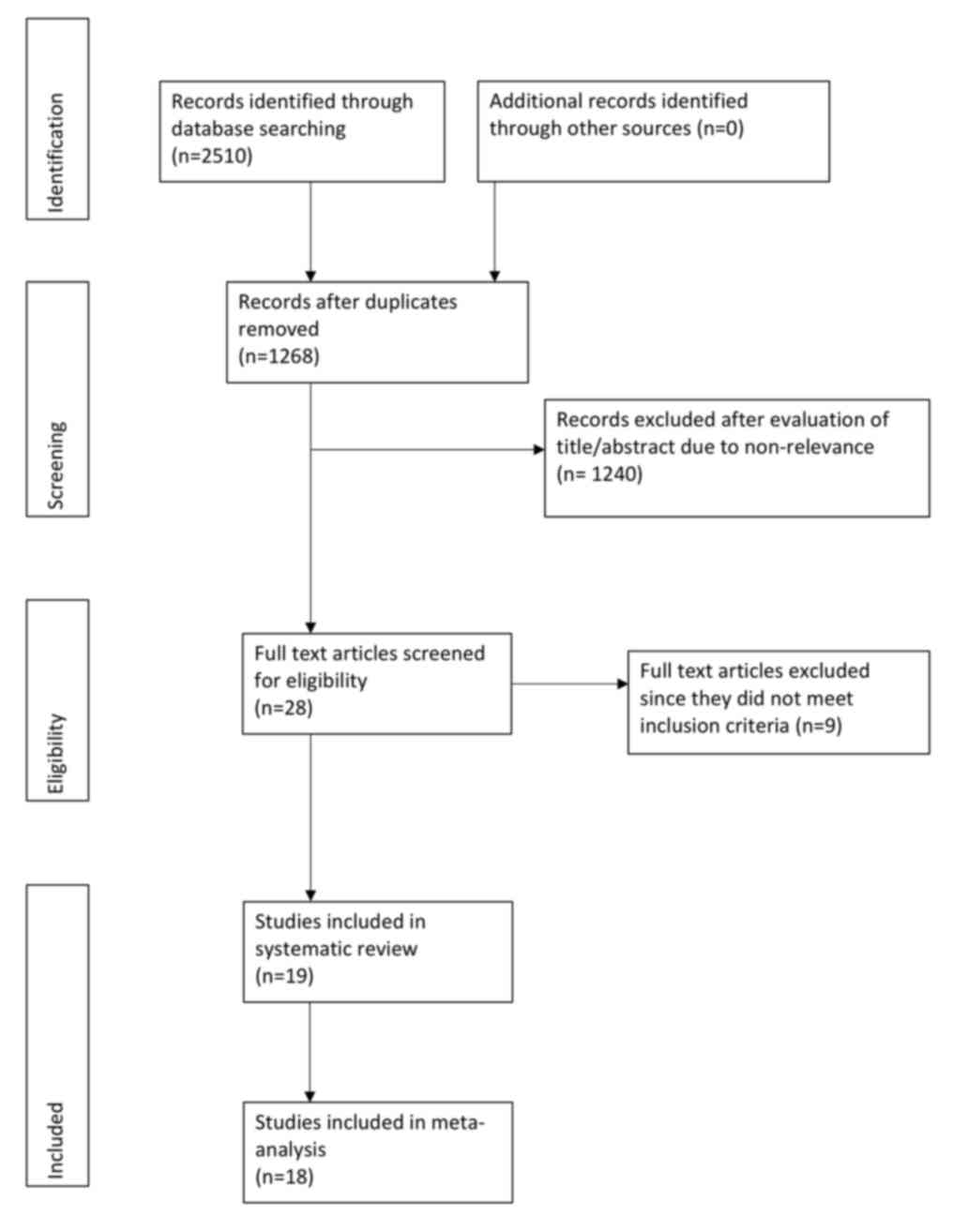
A total of 2,510 relevant entries were initially
identified using the search strategy (Fig. 1). Of these, 28 articles were eligible
for full-text review. Subsequently, 9 studies were excluded as 2
were duplicate publications (15,16), 2
studies did not report cephalometric data (17,18),
mean and SD scores of cephalometric variables were not available in
1 study (19), orthodontic treatment
was ongoing in 1 study (20), only
soft tissue cephalometric variables were studied in 1 article
(21), 1 study did not have a
control group (5) and 1 study
included adult participants as well (22). A total of 19 articles were finally
included (3,4,6-10,23-34).
Characteristics of included
studies
Details of the studies included are presented in
Table I. A total of 7 studies were
performed in Brazil (3,10,24-26,32,34),
3 in Spain (7,28,30), 2
in the US (23,31), 2 in Italy (9,33), and 1
each in India (27), Saudi Arabia
(8), Morocco (29), Israel (4) and Turkey (6). All were cross-sectional studies
comparing cephalometric data of mouth breathers with age and a
gender-matched control group of nasal breathers. MB was diagnosed
using a questionnaire filled by parents of participants, using
clinical history and examination and/or nasopharyngoscopy. The
majority of the included studies did not specify the cause of MB.
The etiology of MB was exclusively allergic rhinitis in 3 studies
(7,23,31) and
nasal septum deviation in one study (33). The age group of the included sample
varied across studies. A total of 2 studies reported separate data
sets for two age-groups (29,30).
These sub-groups were pooled separately for quantitative analysis.
Another study used two control groups, one of the non-allergic
siblings and one historic control group (23). For the meta-analysis, data of the
non-allergic sibling group was included.
 | Table ICharacteristics of studies
included. |
Table I
Characteristics of studies
included.
| | | | | | | Age | | |
|---|
| First author
(year) | Country of
origin | Diagnosis
Etiology | Number of
method | participants | Gender | MB | NB | Study conclusions
(Based on P-values) | (Refs.) |
|---|
| Chambi-Rocha
(2018) | Spain | NS | Airflow sensor | MB: 56 NB: 42 | NS | 7-9 y & 10-16
y& | 7-9 y 10-16 y | ● Greater palatal
length in MB ● Increased LAFH in MB | (30) |
| El Aouame
(2016) | Morocco | NS | NS | MB: 23 NB: 30 | MB: (M, 12; F, 11)
NB: (M, 13; F, 17) | 16 y 8 m±NR | 14 y 4 m±NR | ● Mandibular
retrusion in MB ● Greater inclination of MP in MB ● Increased TAFH
and decreased PFH in MB | (29) |
| Agostinho
(2015) | Spain | Allergic
rhinitis | Standard
questionnaire & CE | MB: 35 NB: 35 | MB: (M, 24; F, 11)
NB: (M, 17; F, 18) | 10 y 2 m±NR | 11 y 5 m±NR | ● Increased LAFH in
MB ● Greater inclination of MP in MB ● Shorter maxillary and
mandibular length in MB | (7) |
| Chung Leng Muñoz
(2014) | Spain questionnaire
& CE | NS | Standard | MB: 53 NB: 65 | MB: (M, 33; F, 20)
NB: (M, 34; F, 31) | M: 10.06±1.5 F:
9.3±1.8 | M: 10.58±1.1 F:
10.36±1.1 | ● Mandibular
retrusion in MB ● Greater inclination of MP in MB ● Greater
inclination of OP in MB | (28) |
| Basheer (2014) | Saudi Arabia | Group 1: Enlarged
adenoids and nasopharynx obstruction of 60% Group 2: No nasal
obstruction | CE &
nasopharyngoscopy | MB1: 20 MB2: 20 NB:
10 | NS | 6-12 y | 6-12 y | ● Increase in
maxillary and mandibular incisor proclination in MB ● Convex facial
profile in MB | (8) |
| Souki (2012) | Brazil | Adeno-tonsillar
hypertrophy | CE &
nasopharyngoscopy | MB: 126 NB:
126 | MB: (M, 73; F, 53)
NB: (M, 65; F, 61) | 6 y 3 m±2 y 1
m | 6 y 9 m±1 y 11
m | ● Increase in
maxillary and mandibular incisor proclination in MB | (34) |
| Malhotra
(2012) | India | NS | CE &
nasopharyngoscopy | MB: 54 NB: 46 | M, 66 F, 34 | 6-9 y & 9-12
y | 6-9 y & 9-12
y | ● Greater TAFH and
LAFH in MB ● Greater inclination of MP in MB ● Greater inclination
of gonial angle in MB | (27) |
| Ucar (2012) | Turkey | NS | CE | MB: 34 NB: 32 | MB: (M, 16; F, 18)
NB: (M, 8; F, 24) | 12.8±1.5 y | 13.5±1.3 y | ● Retrognathic
maxilla in MB ● Greater TAFH in MB ● Greater inclination of MP in
MB ● Increase in mandibular incisor proclination in MB ● Posterior
rotation of palatal plane in MB | (6) |
| Bakor (2011) | Brazil | Allergic rhinitis,
obstructive hypertrophy of the palatine and/or pharyngeal tonsils,
and nasal septum deviation | CE &
nasopharyngoscopy | MB: 10 NB: 10 | MB: (M, 3; F, 7)
NB: (M, 7; F, 3) | 12.7±1.7 y | 13.9±2.6 y | ● Reduced facial
index in MB ● Reduced maxillary width in MB | (3) |
| D'Ascanio
(2010) | Italy | Nasal septal
deviation | CE,
nasopharyngoscopy, rhinomanometry | MB: 98 NB: 98 | MB: (M, 59; F, 39)
NB: (M, 26; F, 35) | 7-12 y | NS | ● Greater UAFH and
TAFH in MB ● Greater inclination of MP in MB ● Increased gonial
angle in MB ● Increased palatal height and overjet in MB ●
Retrognathic maxilla and mandible in MB | (33) |
| Harari (2010) | Israel | Nasal
obstruction | CE &
nasopharyngoscopy | MB: 55 NB: 61 | MB: (M, 28; F, 27)
NB: (M, 26; F, 35) | 12.49±1.94 y | 12.55±2.11 y | ● Backward and
downward rotation of mandible in MB ● Greater inclination of MP in
MB ● Higher palatal plane in MB ● Narrowing of upper and lower
arches in MB | (4) |
| Cuccia (2008) | Italy | NS | History &
parental reporting | MB: 35 NB: 35 | MB: (M,14; F, 21)
NB: (M,16; F, 19) | 8.8±2.2 y | 9.7±1.6 y | ● Hyperdivergent
growth pattern in MB | (9) |
| Juliano (2009) | Brazil | NS | History &
parental reporting | MB: 52 NB: 90 | NS | 10.4±2.06 y | 10.83±1.8 y | ● Retrognathic
mandible in MB ● Greater inclination of MP in MB ● Greater
inclination of OP in MB | (26) |
| Frasson (2006) | Brazil | NS | Standard
questionnaire, CE & nasopharyngoscopy | MB: 25 NB: 25 | MB: (F, 25) NB: (F,
25) | 9-12 y | 9-12 y | ● No difference
between MB and NB | (10) |
| Lessa (2005) | Brazil | Severe nasal
obstruction | CE &
nasopharyngoscopy | MB: 30 NB: 30 | MB: (M, 7; F, 23)
NB: (M, 14; F, 16) | 6-10 y | 6-10 y | ● Decreased PFH and
Increased LAFH in MB ● Greater inclination of MP in MB | (32) |
| Mattar (2004) | Brazil | Severe
nasopharyngeal obstruction | CE &
nasopharyngoscopy | MB: 44 NB: 29 | NS | 3-6 y | 3-6 y | ● Greater
inclination of MP and palatal plane in MB ● Dolicocephalic pattern
in MB ● Decreased PFH in MB ● Narrow maxillary arch in molar region
in MB | (25) |
| Faria (2002) | Brazil | Severe
nasopharyngeal obstruction | CE &
nasopharyngoscopy | MB: 20 NB: 15 | NS | 7-10 y | 7-10 y | ● Greater
inclination of MP in MB ● Retrognathic maxilla and mandible in
MB | (24) |
| Trask (1987) | USA | Allergic
rhinitis | Standard
questionnaire & CE | MB: 25 NB: 25 | NS | 5 y 7 m-13 y5
m | 5 y 1 m-14 y 11
m | ● Greater
inclination of MP and palatal plane in MB ● Increased gonial angle
in MB ● Greater TAFH and LAFH in MB ● Retruded mandible in MB ●
Deeper palatal height in MB ● Retroclined mandibular incisors in
MB | (23) |
| Bresolin
(1983) | USA | Allergic
rhinitis | Standard
questionnaire & CE | MB: 30 NB: 15 | NS | 6-12 y | 6-12 y | ● Greater UAFH and
TAFH in MB ● Greater inclination of MP and palatal plane in MB ●
Increased gonial angle in MB ● Retruded maxilla and mandible in MB
● Deeper palatal height in MB ● Narrow maxillary arch in molar
region in MB | (31) |
Risk of bias assessment
A detailed risk of bias assessment of the studies
included is presented in Table II.
Only 1 study provided a statistical analysis of baseline similarity
amongst the study and control groups (26). The skeletal maturation status of nose
and mouth breathers was reported by 1 study (34). Furthermore, 2 studies diagnosed MB
based on history and parental reporting only (9,26), while
one did not specify the method of diagnosis (29). A total of 8 studies reported on the
reliability of cephalometric tracing by error analysis (6,9,10,23,30,31,33,34).
Only 2 studies performed a blinded examination of the radiograph by
the cephalometric evaluator (26,28).
Cephalometric landmarks were pre-defined in all except 1 study
(27).
 | Table IIQuality assessment of included
studies. |
Table II
Quality assessment of included
studies.
| First author
(year) | Was the control
group appropriately matched? | Were diagnostic
criteria for mouth breathing adequately defined? | Was reliability of
cephalometric tracing measured? | Was the
cephalometric evaluator masked? | Were the
cephalometric landmarks predefined? | (Refs.) |
|---|
| Chambi-Rocha
(2018) | Unclear | Yes | Yes | No | Yes | (30) |
| El Aouame
(2016) | Unclear | Unclear | No | No | Yes | (29) |
| Agostinho
(2015) | Unclear | Yes | Unclear | No | Yes | (7) |
| Chung Leng Muñoz
(2014) | Unclear | Yes | No | Yes | Yes | (25) |
| Basheer (2014) | Unclear | Yes | No | No | Yes | (8) |
| Souki (2012) | Yes | Yes | Yes | No | Yes | (34) |
| Malhotra
(2012) | Unclear | Yes | No | No | No | (27) |
| Ucar (2012) | Unclear | Yes | Yes | No | Yes | (6) |
| Bakor (2011) | Unclear | Yes | No | No | Yes | (3) |
| D'Ascanio
(2010) | Unclear | Yes | Yes | No | Yes | (33) |
| Harari (2010) | Unclear | Yes | No | No | Yes | (4) |
| Cuccia (2008) | Unclear | No | Yes | No | Yes | (9) |
| Juliano (2009) | Yes | No | No | Yes | Yes | (26) |
| Frasson (2006) | Unclear | Yes | Yes | No | Yes | (10) |
| Lessa (2005) | Unclear | Yes | No | No | Yes | (32) |
| Mattar (2004) | Unclear | Yes | No | No | Yes | (25) |
| Faria (2002) | Unclear | Yes | No | No | Yes | (24) |
| Trask (1987) | Unclear | Yes | Yes | No | Yes | (23) |
| Bresolin
(1983) | Unclear | Yes | Yes | No | Yes | (31) |
Meta-analysis
Cephalometric variables reported by individual
studies were reviewed and, based on the frequency of reporting, a
total of 11 angular and 4 linear measurements were selected for
meta-analysis. The different measurements are defined in Table III. Since the majority of studies
assessed facial characteristics on lateral cephalograms, data from
the postero-anterior cephalogram were not included in the
meta-analysis. Furthermore, 1 study did not analyze any of the 16
variables and was therefore not included in the meta-analysis
(8). Missing data of 1 study were
provided by the corresponding author via email (30).
 | Table IIIAbbreviations of cephalometric
variables used for meta-analysis. |
Table III
Abbreviations of cephalometric
variables used for meta-analysis.
| A, Angular
measurements |
|---|
| Variable | Description |
|---|
| SNA | Angle between lines
S-N and N-A |
| SNB | Angle between lines
S-N and N-B |
| ANB | Angle between lines
NA and NB |
| SN.GoGn | Angle between lines
SN and Steiner's mandibular plane (line from Go to Gn) |
| FMA | Frankfort's
mandibular plane angle. Angle between Frankfort's horizontal plane
and Downs mandibular plane |
| | (line from Me to
Go) |
| SN.MP | Angle between SN
and Downs MP |
| NSGn | Angle between SN
and Y axis (line from S to Gn) |
| SN.PP | Angle between SN
and palatal plane (line from ANS to posterior nasal spine) |
| SN.OP | Angle between SN
and occlusal plane |
| MP.PP | Angle between MP
and palatal plane |
| ArGoMe | Gonial angle of
mandible (angle from the Ar to Go to Me) |
| B, Linear
measurements |
| Variable | Description |
| N-Me | Total anterior
facial height. Linear distance between N and Me |
| ANS-Me | Lower anterior
facial height. Linear distance between ANS and Me |
| Ar-Go | Linear distance
between Ar and Go |
| S-Go | Linear distance
between S and Go |
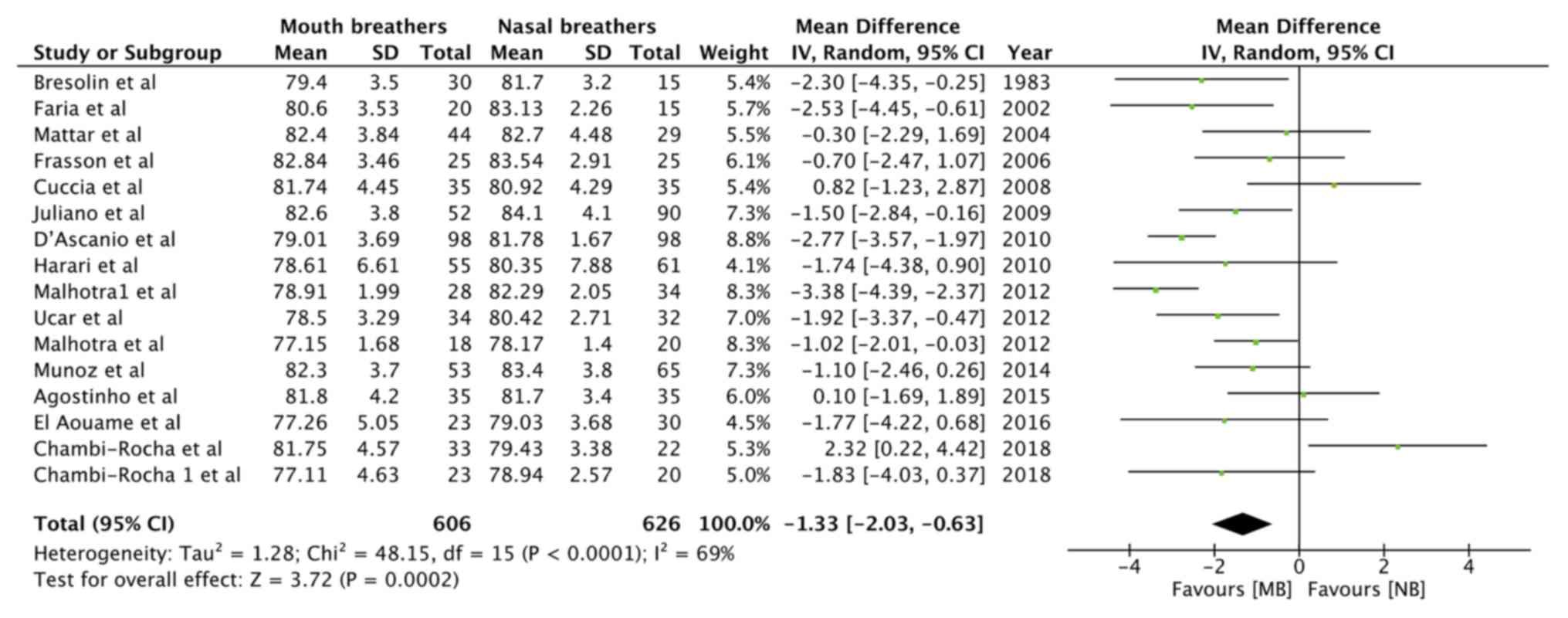
Data from 13 studies, comprising 606 mouth breathers
and 626 nasal breathers, were pooled for the angular measurement
SNA (Table III). Meta-analysis
indicated a statistically significant decrease in the SNA angle of
mouth breathers as compared with that of nasal breathers
[random-effects model: Mean difference (MD)=-1.33; 95% CI, -2.03 to
-0.63; P=0.0002; I2=69%; Fig.
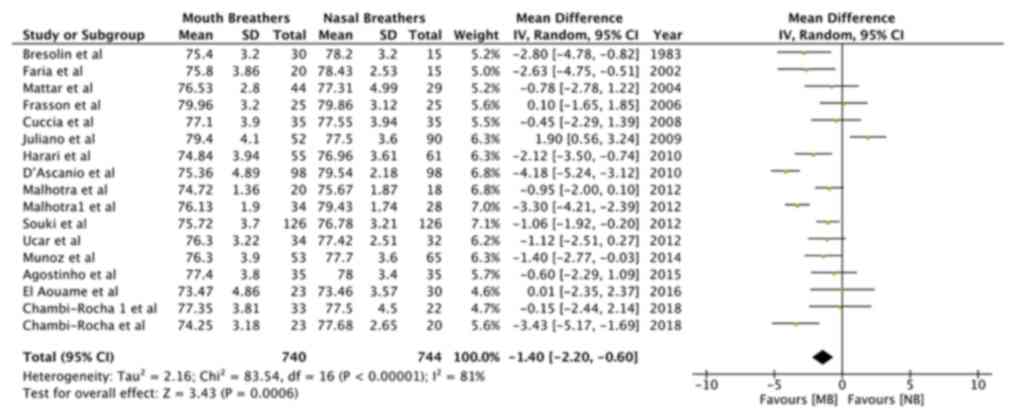
2]. Similarly, pooled data of 740 mouth breathers and 744 nasal
breathers indicated a reduced SNB angle (Table III) in mouth breathers
(random-effects model: MD=-1.40; 95% CI, -2.20 to -0.60; P=0.0006;
I2=81%; Fig. 3). A
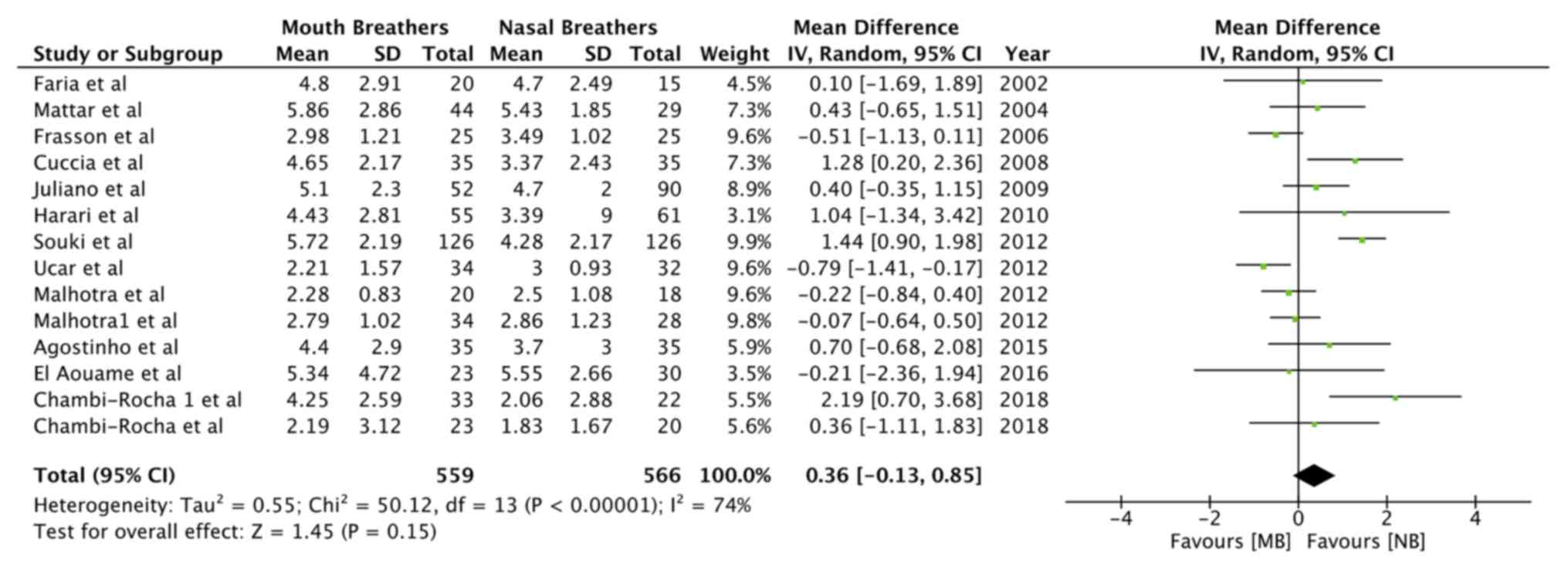
meta-analysis of data from 503 mouth breathers and 524 nasal
breathers did not indicate any significant difference in the ANB
angle (Table III) between the 2
groups (random-effects model: MD=0.36; 95% CI, -0.13 to 0.85;
P=0.15; I2=74%; Fig.
4).
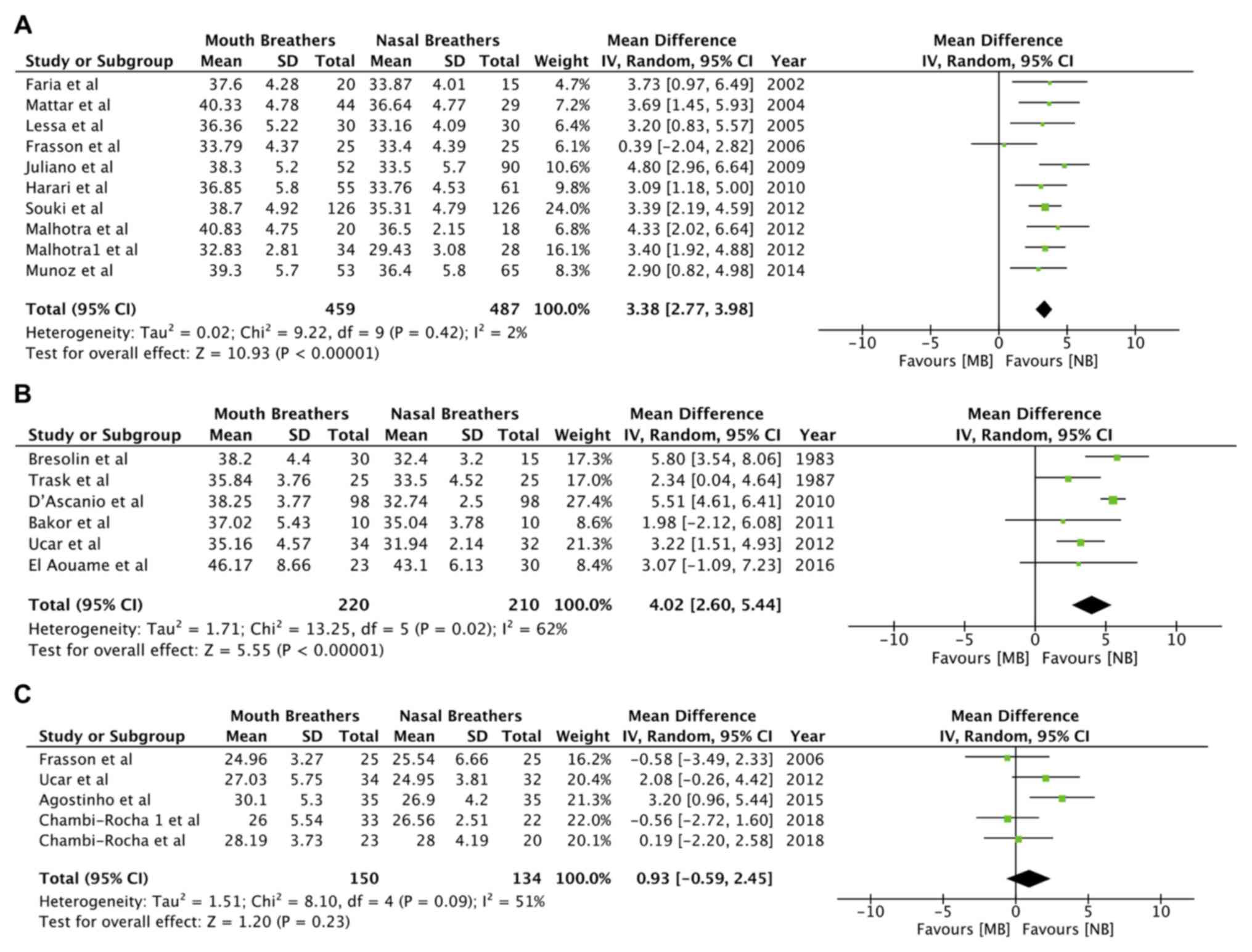
Different mandibular plane angles were pooled
separately. Mandibular plane angles of SN.GoGn (random-effects
model: MD=3.38; 95% CI, 2.77 to 3.98; P<0.00001;
I2=2%; Fig. 5A) and SN.MP
(random-effects model: MD=4.02; 95% CI, 2.60 to 5.44; P<0.00001;
I2=62%; Fig. 5B; Table III) were significantly increased in
mouth breathers. However, meta-analysis of data from 4 studies did
not reveal any significant difference in FMA (random-effects model:
MD=0.93; 95% CI, -0.59 to 2.45; P=0.23; I2=51%; Fig. 5C; Table
III).
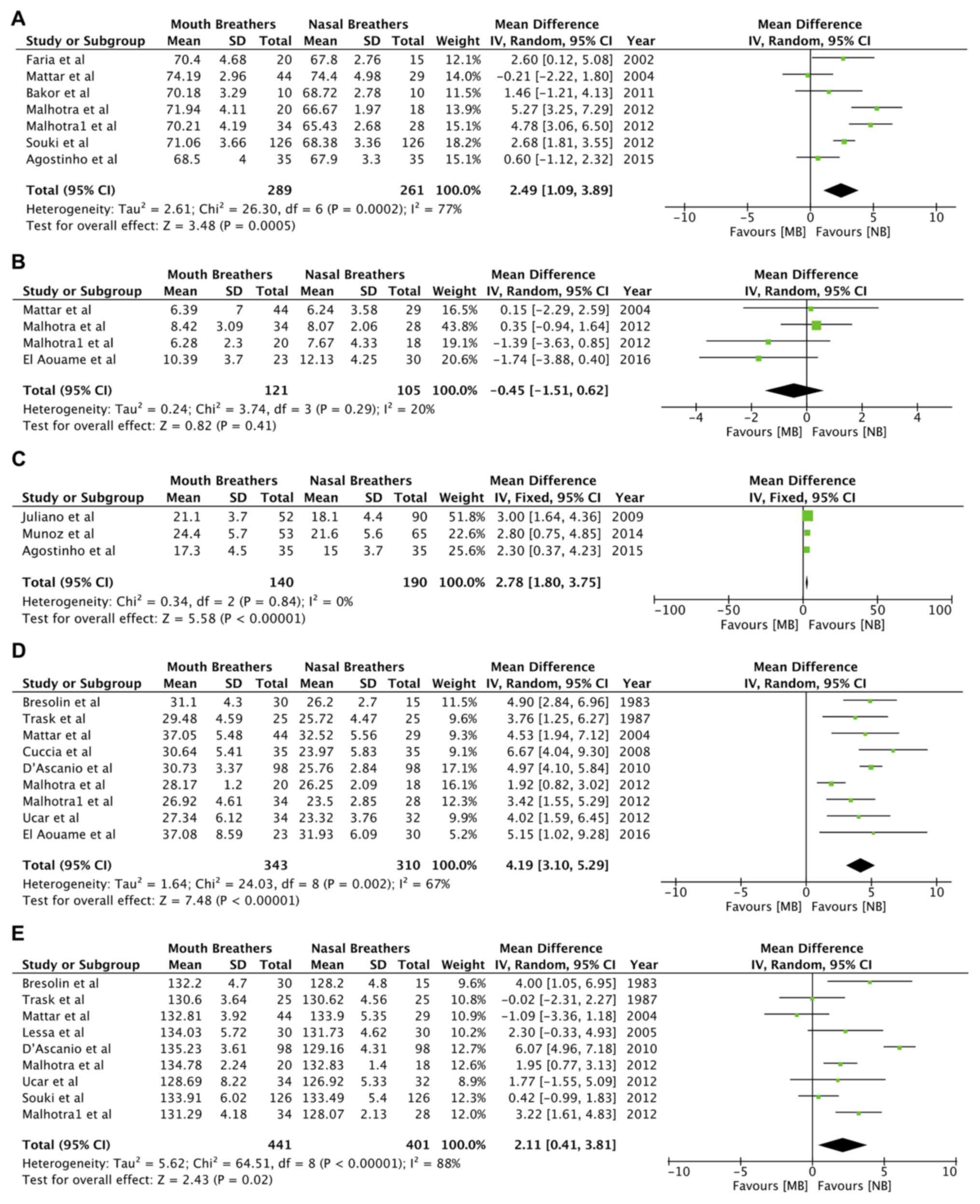
As indicated in Fig.
6, there was a significant increase in the angles NSGn
(random-effects model: MD=2.49; 95% CI, 1.09 to 3.89; P=0.0005;
I2=77%; Fig. 6A; Table III), SN.OP (random-effects model:
MD=2.78; 95% CI, 1.80 to 3.75; P<0.00001; I2=0%;
Fig. 6C; Table III) and MP.PP (random-effects
model: MD=4.19; 95% CI, 3.10 to 5.29; P<0.00001;
I2=67%; Fig. 6D; Table III) in the mouth-breathing group.
No significant difference was identified between the two groups for
the angular variable SN.PP (random-effects model: MD=-0.45; 95% CI,
-1.51 to 0.62; P=0.41; I2=20%; Fig. 6B; Table
III). The gonial angle (ArGoMe; Table III) was significantly increased in
mouth breathers as compared to nasal breathers (random-effects
model: MD=2.11; 95% CI, 0.41 to 3.81; P=0.02; I2=88%;
Fig. 6E).
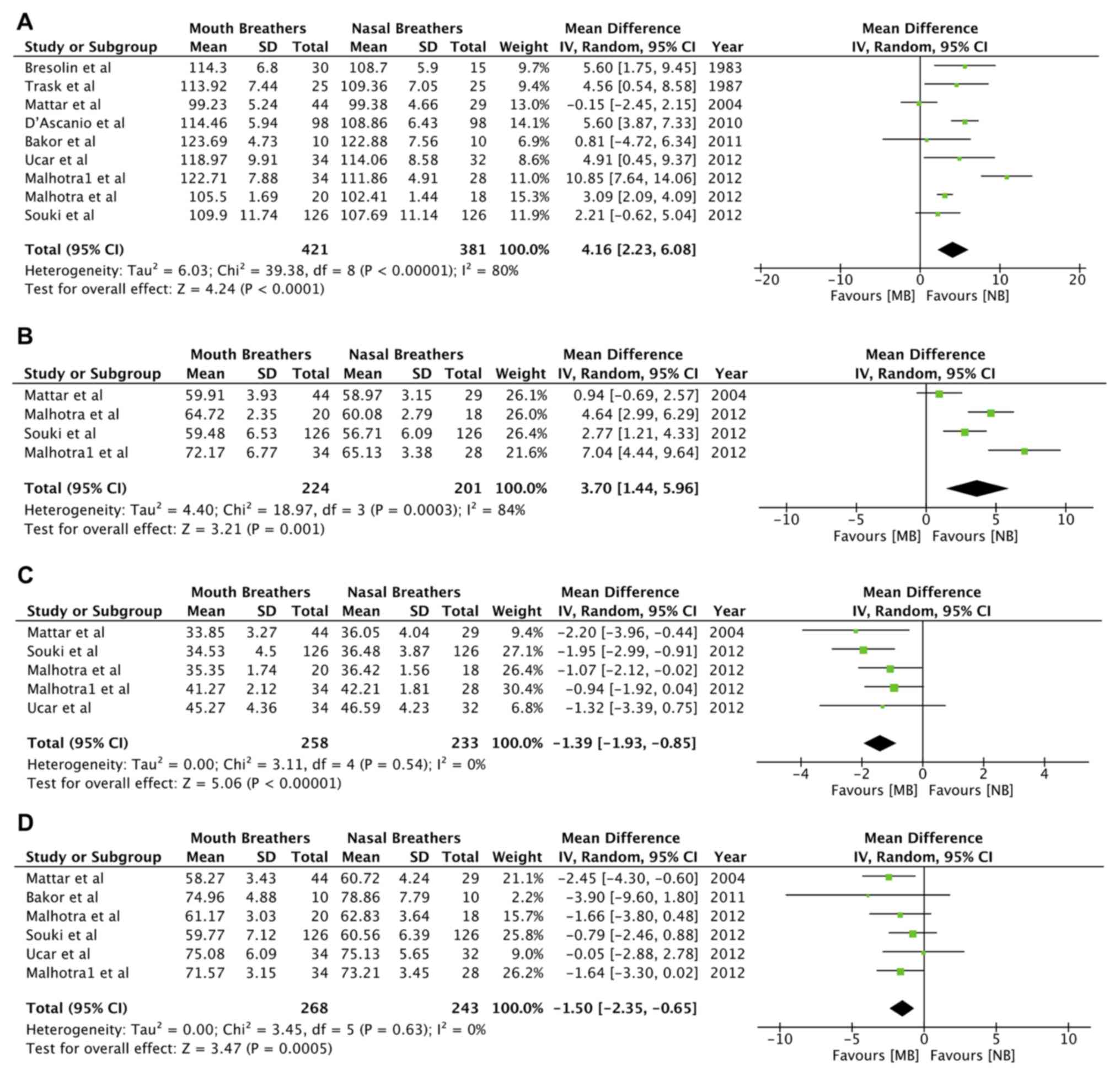
Total anterior facial height (N-Me; random-effects
model: MD=4.16; 95% CI, 2.23 to 6.08; P<0.0001;
I2=80%; Fig. 7A; Table III) and lower anterior facial
height (ANS-Me; random-effects model: MD=3.70; 95% CI, 1.44 to
5.96; P=0.001; I2=84%; Fig.
7B; Table III) were
significantly greater in mouth breathers. Linear measurements of
Ar-Go (random-effects model: MD=-1.39; 95% CI, -1.93 to -0.85;
P<0.00001; I2=0%; Fig.
7C) and S-Go (random-effects model: MD=-1.50; 95% CI, -2.35 to
-0.65; P=0.0005; I2=0%; Fig.
7D; Table III), denoting
posterior facial height, were reduced in mouth breathers as
compared to nasal breathers.
Sensitivity analysis
Sensitivity analysis was performed by removing each
study sequentially from the meta-analysis to assess any changes in
results. No change in the significance of any variable was
identified in the sensitivity analysis.
Discussion
The primary objective of the present review was to
evaluate facial morphological differences in mouth-breathing
children and adolescents as compared to age and gender-matched
control groups of nasal breathers. Considering the multiple
different angulars and linear measurements evaluated by the studies
included, it was not possible to pool all variables for a
meta-analysis. The variables used in the present meta-analysis may
be broadly divided as follows: Those measuring the association of
maxilla and mandible to the cranial base (SNA and SNB) and each
other (ANB), mandibular plane angles (SN.GoGn, FMA and SN.MP),
Y-axis angle (NSGn), association of occlusal and palatal planes to
the cranial base and mandible (SN.OP, SN.MP and MP.PP), the gonial
angle (ArGoMe) and anterior and posterior facial height
measurements (N-Me, ANS-Me, Ar-Go and S-Go).
The association of the maxilla with the cranial base
was measured in 14 studies. Of these studies, 8 individually did
not report any significant retrusion of the maxilla in their study
population (4,7,9,10,25,28-30).
Similarly, data on the association of the mandible to the cranial
base were reported by 15 studies. Individually, the results of
these studies were divided, with 7 reporting a significant
difference in SNB angles as compared to controls (4,6,24,27,28,31,34) and
8 studies indicating no such difference (3,7,9,23,25,26,29).
Concerning etiology, while Bresolin et al (31), in a cohort of patients with allergic
rhinitis, revealed retrusion of maxilla and mandible, Agostinho
et al (7) did not identify
any significant change in anteroposterior maxilla-mandibular
position in mouth breathers with the same etiology. There were also
no apparent differences between different age groups in the samples
of studies reporting positive results as compared to those
reporting no difference. However, studies by Mattar et al
(25), which had the youngest sample
amongst all studies included (3-6 years) and El Aouame et al
(29), which had the oldest sample
(mean: 16 years 8 months), reported no difference in maxillary and
mandibular positions between study and control groups. Similar
results have been reported by other authors (35). However, the present quantitative
analysis indicated a statistically significant reduction in SNA and
SNB angles in mouth breathers.
The retracted position of the maxilla in mouth
breathers has been explained with the functional matrix theory of
Moss and Salentijn (2). It has been
postulated that, in the absence of nasal respiration, there is a
hypoplasia of the maxillary sinus and narrowing of nasal cavities
with resultant maxillary retrognathism (24). Ricketts (36) has attributed a reduction in SNB
angles in cases of nasal obstructions to a more forward and
downward tongue posture to facilitate oral breathing. This tongue
posture possibly causes downward and backward positioning of the
mandible. Souki et al (34)
reported smaller mandibular corpus lengths in mouth breathers,
which the authors suggest is responsible for smaller SNB angles in
mouth breathers. Studies have also reported a greater incidence of
skeletal class 2 malocclusion in mouth breathers (33,34).
However, the same was not corroborated in the present
meta-analysis. The present analysis of the ANB angle indicates no
difference between mouth breathers and nasal breathers. The
variation amongst studies on SNA, SNB and ANB angles may be due to
geographical, gender and age variations amongst study samples. In
addition, only certain studies (6,30)
restricted the study sample to individuals with only skeletal class
1 malocclusion, whilst all others included a mixed population of
patients, which may have influenced the results.
In terms of facial morphology, mouth breathers are
expected to have a vertical growth pattern. The results of the
present analysis tend to support this assumption. Comparisons of
mandibular plane angles between mouth breathers and nasal breathers
were provided by 17 studies. Since 3 different angular measurements
(SN.GoGn, FMA and SN.MP) were utilized, data were pooled separately
for each variable. The meta-analysis indicated a statistically
significant increase in mandibular plane angles (SN.GoGn and SN.MP)
in mouth breathers. Only 4 studies, namely those of Frasson et
al (10), Bakor et al
(3), Chambi-Rocha et al
(30) and El Aouame et al
(29), did not obtain any difference
in the mandibular plane angle between the two groups. In the study
by Bakor et al (3), the
non-significant result was probably due to the small sample size of
the study. The study by El Aouame et al (29), despite no significant difference in
mandibular plane angles, concluded that a hyperdivergent growth
pattern prevails in mouth breathers as compared to nasal
breathers.
An increase in the Y-axis angle is also indicative
of a vertical growth pattern. Analysis of data from 6 studies
(3,7,24,25,27,34)
demonstrated increased NSGn angles in mouth breathers. The present
results also revealed a significant increase in the occlusal plane
angle in mouth breathers but without any difference in palatal
plane angle. The mandibular plane angle was increased in
association with the palatal plane in mouth breathers. Thus, the
present results indicate a counterclockwise rotation of the
mandible to the cranial base in mouth breathers, but without any
concomitant rotation of the maxilla.
Linear variables in the present study were
restricted to facial height measurements. The present results
indicated a significant increase in total anterior facial height
and lower anterior facial height in mouth breathers, accompanied by
a decrease in posterior facial height. While data on total anterior
facial height were reported by 8 studies (3,6,23,25,27,31,33,34),
values of lower anterior facial height were only available from 3
studies (25,27,34).
Souki et al (34) have
pointed out the difference in lower anterior facial height in
children with primary dentition as compared to those in the mixed
dentition phase. It is contended that facial height may be
influenced by the skeletal maturation stage and not by the
breathing mode alone. Therefore, the ratio of posterior facial
height to total anterior facial height is regarded as a better tool
to understand facial morphology. In their study, no difference with
regard to age groups was identified when comparing this ratio
between study and control groups. The posterior-to-anterior facial
height ratio was reported by a small number of studies included in
the present review (3,32,34). All
reported values were decreased in mouth breathers as compared to
nasal breathers. The variance in facial height tends to support the
theory that mouth breathers exhibit clockwise rotation of the
mandible with increased vertical growth of the anterior portion of
the face relative to the posterior portion of the face.
Certain limitations of the present study require to
be elaborated on and considered while interpreting the results.
Firstly, the strength of evidence of any review and meta-analysis
is measured by the quality of the included studies. Based on the
present assessment, the quality of the included studies was not
high. The biggest drawback is the baseline similarity assessment
between study and control groups. Statistical analysis and skeletal
maturity indicators were not used by the majority of studies to
establish baseline similarity amongst the study groups. Not all
studies utilized sufficient diagnostic tools, including
nasopharyngoscopy and/or rhinomanometry, to confirm the MB habit.
Furthermore, the present analysis only included data from
cross-sectional studies. Long-term longitudinal studies are
required to establish the exact role of MB in craniofacial
development. In addition, the large variance in the age groups of
individual studies combined with insufficient data precluded a
sub-group analysis based on the age of participants. The studies
also reported data of individuals from diverse geographical regions
and ethnic backgrounds. This may have introduced bias in the
results of the present review. As another limitation, only lateral
cephalometric data were analyzed, as sufficient studies on
posteroanterior cephalogram were not available. Similarly, the lack
of sufficient studies on soft tissue data precluded a meta-analysis
for soft-tissue variables. Finally, cephalometric data are prone to
errors through several factors, including radiographic
magnification, patient position and observer variance. Such errors
across a large number of studies may have influenced the
results.
However, since the present study was a study-level
meta-analysis and not a patient-level study, it may be assumed that
cephalometric errors were equally distributed amongst the study and
control groups. Despite the drawbacks, the consistency of size and
directionality of the overall effect, as well as the stability of
the results after sensitivity analysis, support the reliability of
the results of the present meta-analysis.
The present results indicated that mouth breathers
had a tendency of retrognathic maxilla and mandible as compared to
nasal breathers. The association of the maxilla with the mandible
appears to be normal. Mouth breathers tend to have a high
mandibular plane angle and an increased gonial angle. The tendency
of downward and backward rotation of the mandible is observed in
mouth breathers without a similar angular change in the maxilla.
Total anterior facial height and lower anterior facial height
appear to be increased while posterior facial height appears to be
decreased in mouth breathers.
However, the quality of evidence is not high. More
high-quality studies with longitudinal assessment of growth are
required to help strengthen the evidence on this subject.
Supplementary Material
Table SI. Search strategy used for
electronic search.
Acknowledgements
Not applicable.
Funding
This study was supported by Contract for Science and
Technology Projects in Jiaxing City (community; grant no.
2018AD32035). The subject of the project is ‘The Effect of Muscle
Functional Appliance on Malocclusion of Tooth Collar Caused by MB
in Mixed Teeth’.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WZ conceived and designed the study. XZ, JD and JH
collected the data and performed the literature search. WZ was
involved in the writing of the manuscript. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Warren DW: Effect of airway obstruction
upon facial growth. Otolaryngol Clin North Am. 23:699–712.
1990.PubMed/NCBI
|
|
2
|
Moss ML and Salentijn L: The primary role
of functional matrices in facial growth. Am J Orthod. 55:566–577.
1969.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bakor SF, Enlow DH, Pontes P and De Biase
NG: Craniofacial growth variations in nasal-breathing,
oral-breathing, and tracheotomized children. Am J Orthod
Dentofacial Orthop. 140:486–492. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Harari D, Redlich M, Miri S, Hamud T and
Gross M: The effect of mouth breathing versus nasal breathing on
dentofacial and craniofacial development in orthodontic patients.
Laryngoscope. 120:2089–2093. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sousa JB, Anselmo-Lima WT, Valera FC,
Gallego AJ and Matsumoto MA: Cephalometric assessment of the
mandibular growth pattern in mouth-breathing children. Int J
Pediatr Otorhinolaryngol. 69:311–317. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ucar FI, Ekizer A and Uysal T: Comparison
of craniofacial morphology, head posture and hyoid bone position
with different breathing patterns. Saudi Dent J. 24:135–141.
2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Agostinho HA, Furtado IÃ, Silva FS and
Ustrell Torrent J: Cephalometric evaluation of children with
allergic rhinitis and mouth breathing. Acta Med Port. 28:316–21.
2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Basheer B, Hegde KS, Bhat SS, Umar D and
Baroudi K: Influence of mouth breathing on the dentofacial growth
of children: A cephalometric study. J Int Oral Health. 6:50–55.
2014.PubMed/NCBI
|
|
9
|
Cuccia AM, Lotti M and Caradonna D: Oral
breathing and head posture. Angle Orthod. 78:77–82. 2008.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Frasson JM, Magnani MB, Nouer DF, de
Siqueira VC and Lunardi N: Comparative cephalometric study between
nasal and predominantly mouth breathers. Braz J Otorhinolaryngol.
72:72–81. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fields HW, Warren DW, Black K and Phillips
CL: Relationship between vertical dentofacial morphology and
respiration in adolescents. Am J Orthod Dentofacial Orthop.
99:147–154. 1991.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Vig KW: Nasal obstruction and facial
growth: The strength of evidence for clinical assumptions. Am J
Orthod Dentofacial Orthop. 113:603–611. 1998.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Welch V, Petticrew M, Tugwell P, Moher D,
O'Neill J, Waters E and White H: PRISMA-Equity Bellagio group:
PRISMA-equity 2012 extension: Reporting guidelines for systematic
reviews with a focus on health equity. PLoS Medicine.
9(e1001333)2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Flores-Mir C, Korayem M, Heo G, Witmans M,
Major MP and Major PW: Craniofacial morphological characteristics
in children with obstructive sleep apnea syndrome: A systematic
review and meta-analysis. J Am Dent Assoc. 144:269–277.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Franco LP, Souki BQ, Pereira TB, Meyge de
Brito G, Gonçalves Becker HM and Pinto JA: Is the growth pattern in
mouth breathers comparable with the counterclockwise mandibular
rotation of nasal breathers? Am J Orthod Dentofacial Orthop.
144:341–348. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Valera FC, Travitzki LV, Mattar SE,
Matsumoto MA, Elias AM and Anselmo-Lima WT: Muscular, functional
and orthodontic changes in pre school children with enlarged
adenoids and tonsils. Int J Pediatr Otorhinolaryngol. 67:761–770.
2003.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zicari AM, Albani F, Ntrekou P, Rugiano A,
Duse M, Mattei A and Marzo G: Oral breathing and dental
malocclusions. Eur J Paediatr Dent. 10:59–64. 2009.PubMed/NCBI
|
|
18
|
Lione R, Buongiorno M, Franchi L and Cozza
P: Evaluation of maxillary arch dimensions and palatal morphology
in mouth-breathing children by using digital dental casts. Int J
Pediatr Otorhinolaryngol. 78:91–95. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rossi RC, Rossi NJ, Rossi NJ, Yamashita HK
and Pignatari SS: Dentofacial characteristics of oral breathers in
different ages: A retrospective case-control study. Prog Orthod.
16(23)2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ung N, Koenig J, Shapiro PA, Shapiro G and
Trask G: A quantitative assessment of respiratory patterns and
their effects on dentofacial development. Am J Orthod Dentofacial
Orthop. 98:523–532. 1990.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Jakobsone G, Urtane I and Terauds I: Soft
tissue profile of children with impaired nasal breathing.
Stomatologija. 8:39–43. 2006.PubMed/NCBI
|
|
22
|
Cheng MC, Enlow DH, Papsidero M, Broadbent
BH Jr, Oyen O and Sabat M: Developmental effects of impaired
breathing in the face of the growing child. Angle Orthod.
58:309–320. 1988.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Trask GM, Shapiro GG and Shapiro PA: The
effects of perennial allergic rhinitis on dental and skeletal
development: A comparison of sibling pairs. Am J Orthod Dentofacial
Orthop. 92:286–293. 1987.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Faria PT, de Oliveira Ruellas AC,
Matsumoto MA, Anselmo-Lima WT and Pereira FC: Dentofacial
morphology of mouth breathing children. Braz Den J. 13:129–132.
2002.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mattar SE, Anselmo-Lima WT, Valera FC and
Matsumoto MA: Skeletal and occlusal characteristics in
mouth-breathing pre-school children. J Clin Pediatr Dent.
28:315–318. 2004.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Juliano ML, Machado MA, Carvalho LB, Prado
LB and do Prado GF: Mouth breathing children have cephalometric
patterns similar to those of adult patients with obstructive sleep
apnea syndrome. Arq Neuropsiquiatr. 67:860–865. 2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Malhotra S, Pandey RK, Nagar A, Agarwal SP
and Gupta VK: The effect of mouth breathing on dentofacial
morphology of growing child. J Indian Soc Pedod Prev Dent.
30:27–31. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chung Leng Muñoz I and Beltri Orta P:
Comparison of cephalometric patterns in mouth breathing and nose
breathing children. Int J Pediatr Otorhinolaryngol. 78:1167–1172.
2014.PubMed/NCBI View Article : Google Scholar
|
|
29
|
El Aouame A, Daoui A and El Quars F: Nasal
breathing and the vertical dimension: A cephalometric study. Int
Orthod. 14:491–502. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chambi-Rocha A, Cabrera-Domínguez ME and
Domínguez-Reyes A: Breathing mode influence on craniofacial
development and head posture. J Pediatr (Rio J). 94:123–130.
2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Bresolin D, Shapiro PA, Shapiro GG, Chapko
MK and Dassel S: Mouth breathing in allergic children: Its
relationship to dentofacial development. Am J Orthod. 83:334–340.
1983.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Lessa FC, Enoki C, Feres MF, Valera FC,
Lima WT and Matsumoto MA: Breathing mode influence in craniofacial
development. Braz J Otorhinolaryngol. 71:156–160. 2005.PubMed/NCBI View Article : Google Scholar
|
|
33
|
D'Ascanio L, Lancione C, Pompa G,
Rebuffini E, Mansi N and Manzini M: Craniofacial growth in children
with nasal septum deviation: A cephalometric comparative study. Int
J Pediatr Otorhinolaryngol. 74:1180–1183. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Souki BQ, Lopes PB, Pereira TB, Franco LP,
Becker HM and Oliveira DD: Mouth breathing children and
cephalometric pattern: Does the stage of dental development matter?
Int J Pediatr Otorhinolaryngol. 76:837–841. 2012.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Linder-Aronson S: Respiratory function in
relation to facial morphology and the dentition. Br J Orthod.
6:59–71. 1979.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Ricketts RM: Forum on the tonsil and
adenoid problem in orthodontics respiratory obstruction syndrome.
Am J Orthod. 54:495–507. 1968.PubMed/NCBI
|