Introduction
Branch retinal vein occlusion (BRVO) is a common
retinal vascular disease, and the secondary macular edema (ME) is
an important cause of visual impairment (1,2). The
treatment of BRVO aims to alleviate ME, inhibit angiogenesis, and
eliminate non-perfusion area, in which early alleviation of ME is
the key to improving visual acuity (3,4). At
present, the most commonly used therapeutic methods for ME include
intravitreal injection of triamcinolone acetonide, intravitreal
injection of anti-vascular endothelial growth factor (VEGF) drugs,
and fundus laser photocoagulation (5). Macular grid laser photocoagulation can
reduce vascular leakage and alleviate ME, but its improvement
effect on visual acuity is limited, with a risk of visual
impairment (6). Intravitreal
injection of anti-VEGF drugs can effectively treat RVO, and
combined with laser photocoagulation can achieve better results
(7,8).
This study retrospectively analyzed the clinical
data of 98 patients with BRVO secondary macular edema admitted to
Yantaishan Hospital (Yantai, China) from June 2017 to June 2018.
Comparative analysis of retinal photocoagulation and intravitreal
injection of Conbercept combined with retinal photocoagulation was
carried out. Therapeutic efficacy and safety of BRVO secondary
macular edema was evaluated in order to provide a more accurate
basis for the development of effective treatment options.
Patients and methods
General data
A total of 98 patients (98 eyes) diagnosed with ME
secondary to BRVO in Yantaishan Hospital from June 2017 to June
2018 were selected, including 51 males and 47 females aged 31-77
years with an average of 55.87±9.79 years. The course of disease
was 5 days to 3 months, and the best corrected visual acuity (BCVA)
before treatment and central macular thickness (CMT) were 0.4 and
351.4-731.8 µm with an average of 563.6±162.5 µm, respectively. The
patients were divided into laser group (retinal photocoagulation
alone, n=49) and combination group (intravitreal injection of
Conbercept combined with retinal photocoagulation, n=49) using a
random number Table based on the treatment order. Inclusion
criteria: i) fluorescein fundus angiography (FFA) was diagnosed as
BRVO; ii) optical coherence tomography (OCT) showed macular cystic
edema, and the retina was diffusely thickened; iii) All are
monocular, with a course of <3 months. Exclusion criteria: i)
previous exposure to intravitreal injection of anti-VEGF drugs or
subconjunctival injection of triamcinolone acetonide; ii) previous
treatment with laser photocoagulation; iii) diagnosis or suspected
shallow anterior chamber, glaucoma or ocular hypertension; iv) ME
secondary to age-related macular degeneration, diabetic
retinopathy, retinal vein inflammation, retinal vasculitis; v) eye
diseases other than BRVO; vi) history of drug allergy and bronchi
asthma, and diabetes. The general data, such as sex, age, BCVA
before treatment, CMT and intraocular pressure, had no
statistically significant differences between the two groups
(P>0.05, Table I), and they were
comparable. This study was approved by the Ethics Committee of
Yantaishan Hospital, and patients and their families agreed and
signed the informed consent.
 | Table IDemographics and general clinical data
of the studied patients. |
Table I
Demographics and general clinical data
of the studied patients.
| Parameters | Combination group
n=49 | Laser group n=49 | P-value |
|---|
| Sex
(male/female) | 27/22 | 24/25 | 0.686 |
| Age (years) | 55.13±9.62 | 56.84±9.57 | 0.380 |
| Course of the disease
(days) | 19.5±2.7 | 18.8±2.3 | 0.170 |
| BCVA (logMAR) | 0.84±0.47 | 0.89±0.49 | 0.607 |
| CMT (µm) | 559.5±152.7 | 570.3±172.6 | 0.744 |
| IOP (mmHg) | 14.8±3.9 | 15.2±3.5 | 0.594 |
| Occlusion vessel | | | 0.871 |
|
Superior
temporal branch | 23 (46.9%) | 26 (53.1%) | |
|
Inferior
temporal branch | 17 (34.7%) | 14 (28.6%) | |
|
Superior
nasal branch | 4 (8.2%) | 3 (6.1%) | |
|
Inferior
nasal branch | 5 (10.2%) | 6 (12.2%) | |
Treatment methods
In combination group, intravitreal injection of
Conbercept was performed routinely. 0.05 ml of Conbercept injection
(10.0 mg/ml) containing 0.5 mg of Conbercept was taken using a 1 ml
syringe, and the syringe was vertically inserted at 3.75 mm behind
the corneal limbus to slowly inject Conbercept. After that,
Ofloxacin eye ointment was applied and the eye was bandaged.
Whether the treatment should be repeated after injection once was
determined according to the return visit examination. The anti-VEGF
drugs were given if the BCVA declined by 2 lines or CMT was
increased by ≥100 µm. The injection was performed twice at an
interval of ≥4 weeks. At 1 week after injection, the patients
underwent laser photocoagulation under a retinoscope using the
multi-wavelength laser machine (Lumenis). The laser parameters are
as follows: spot diameter, 100-200 µm; power, 150-200 mW; exposure
time, 0.1-0.15 sec; level I spot, spot gap, ~1 spot diameter. The
quadrant photocoagulation was conducted for the non-perfusion area
shown in FFA. The laser parameters are as follows: spot diameter,
50-100 µm; exposure time, 0.2 sec; spot reaction, level I-II, spot
gap, ~1 spot diameter. After treatment, eye drops (non-steroidal
anti-inflammatory drugs) were used 4 times per day for 3
consecutive days. The range of photocoagulation each time was ≤1/4
quadrant, and photocoagulation was conducted twice at an interval
of 1 week. The patients who could not receive photocoagulation due
to great bleeding should undergo photocoagulation after bleeding
absorption.
In laser group, the macular grid laser
photocoagulation was directly performed. The laser parameters are
as follows: spot diameter, 100-200 µm; power, 150-200 mW; exposure
time, 0.1-0.15 sec; level I spot, spot gap: ~1 spot diameter.
Quadrant local photocoagulation was performed using the same laser
parameters for the patients with non-perfusion area or new vessels
in the peripheral retina. All operations were completed by the same
physician.
Observation indexes
The BCVA, OCT, fundus color photography, and FFA
examination were performed before treatment and 1 week and 1, 3,
and 6 months after treatment. The BCVA examination uses a standard
logarithmic visual acuity chart, which is converted to the
logarithm of the minimum angle of resolution (logMAR) visual
acuity. Nonmyd α-DIII non-mydriatic fundus camera (Kowa Co., Ltd.)
was used in fundus color photography, Spectralis HRA instrument was
used in FFA, and Spectralis OCT instrument was used in OCT. With
the central fovea of macula as the center, the horizontal linear
scanning was conducted (scanning depth, 1.9 mm; scanning area, 6x6
mm; transverse resolution, 14 µm; axial resolution, 7 µm; scanning
mode, 512x496). The distance from the internal limiting membrane of
retinal nerve epithelial layer to the lateral strong reflective
area of retinal pigment epithelial layer was measured as CMT using
the built-in range of software by two experienced technicians 3
times, and the average was taken. The integrity of ellipsoid zone
and external limiting membrane (ELM) was observed on the central
horizontal scanning line and within 500 µm in the greyscale map. We
also recorded the BCVA, mean CMT changes, intraocular pressure
changes, and complications before and 1 week after treatment and at
1, 3, and 6 months.
The correlations of long-term visual acuity of
patients in combination group with age, logMAR BCVA before
treatment, CMT before treatment, times of drug injection and
decrease value of CMT at 1 month after treatment were analyzed
using Pearson correlation analysis. The multivariate regression
analysis was adopted for the correlations of long-term visual
acuity of patients in combination group with age, logMAR BCVA
before treatment, CMT before treatment, times of drug injection,
decreased value of CMT at 1 month after treatment, and integrity of
ellipsoid zone and ELM.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
22.0 software (IBM Corp.) was used for statistical analysis.
Enumeration data were expressed as rate (%), and χ2 test
was performed for the intergroup comparison. Measurement data were
expressed as mean ± standard deviation (mean ± SD), multivariate
analysis of variance (MANOVA) with repeated measures was adopted
for the comparison of BCVA and CMT at different time points,
independent-samples t-test for the intergroup comparison, and LSD-t
test for the intragroup comparison. P<0.05 was considered to
indicate a statistically significant difference.
Results
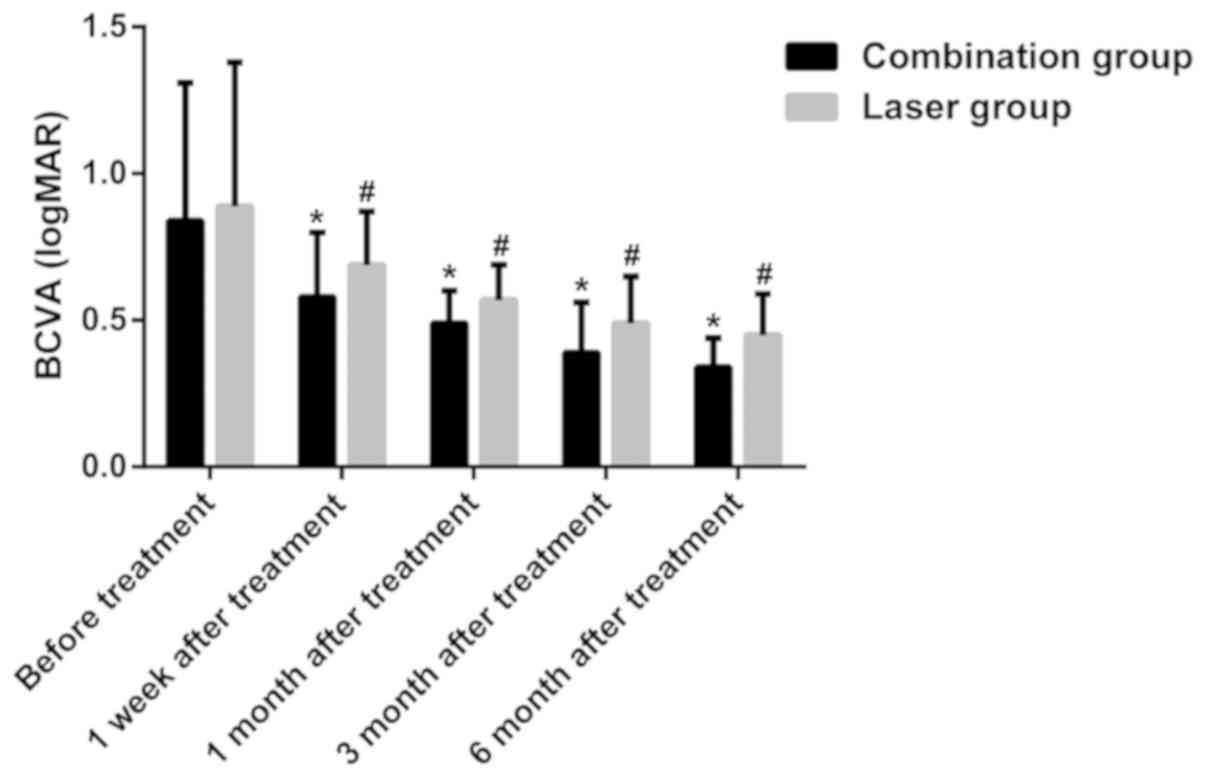
Changes in BCVA before and after
treatment in the groups
The changes in BCVA had statistically significant
differences in both groups before and after treatment (F group =
14.56, F time = 10.84, F time x group = 12.62, P<0.01). At 1
week, 1 month, 3 months and 6 months after treatment, the BCVA in
both groups was significantly superior to that before treatment
(P<0.05), and the BCVA in combination group was obviously better
than that in laser group, showing statistically significant
differences (P=0.008, P<0.001, P=0.004, P<0.001) (Fig. 1).
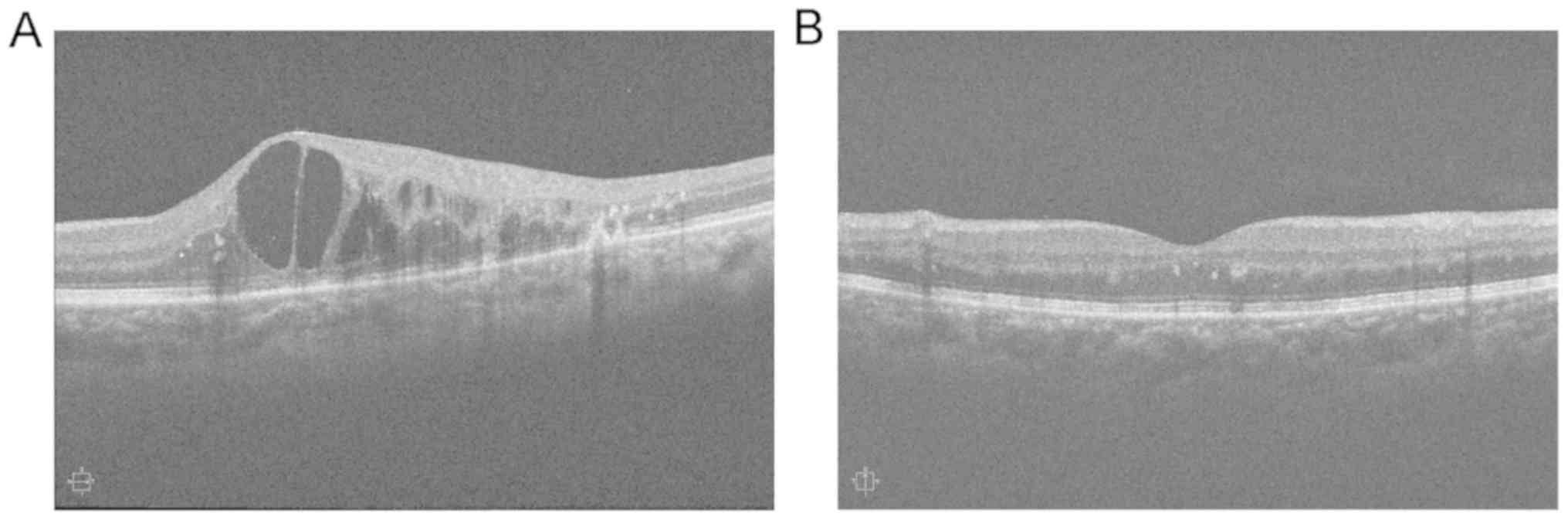
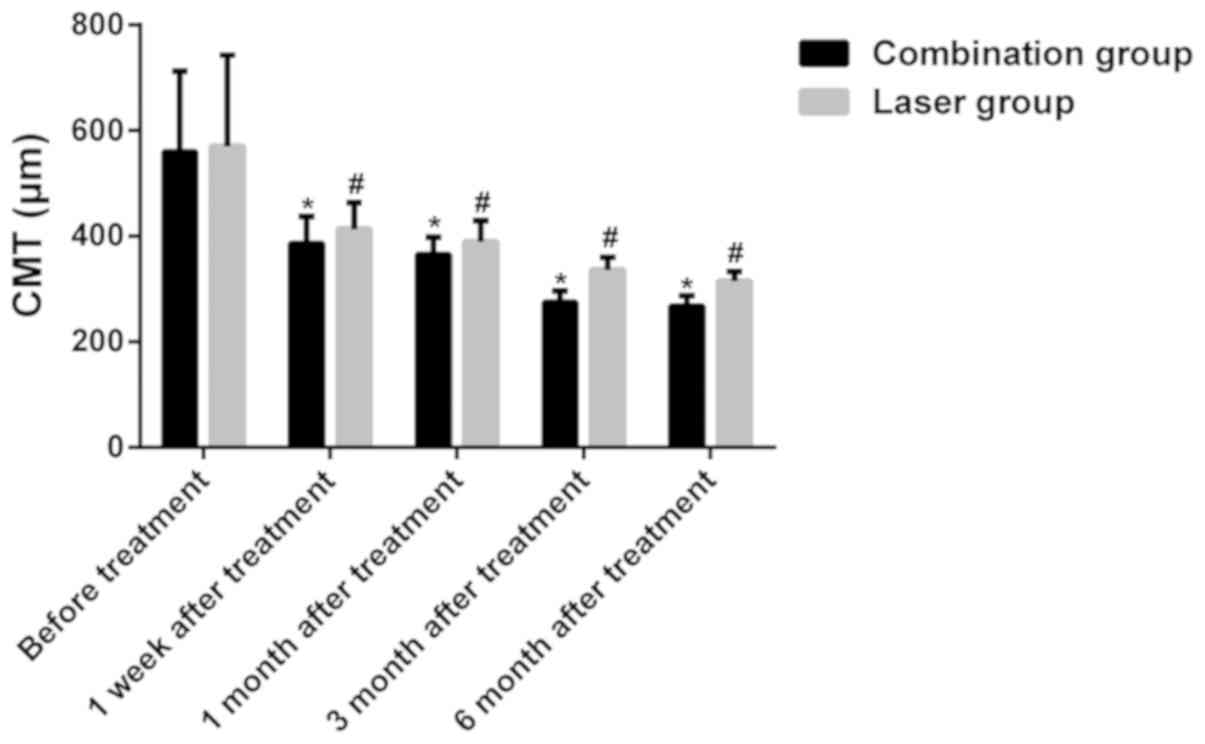
Changes in CMT before and after
treatment in the groups
The changes in CMT had statistically significant
differences in both groups before and after treatment (F group =
13.47, F time = 17.28, F time x group = 20.34, P<0.01), and ME
obviously subsided after treatment (Fig.
2). At 1 week, 1, 3 and 6 months after treatment, CMT evidently
declined in both groups compared with that before treatment
(P<0.05), while it was obviously smaller in combination group
than that in laser group (P=0.009, P=0.002, P<0.001, P<0.001)
(Fig. 3).
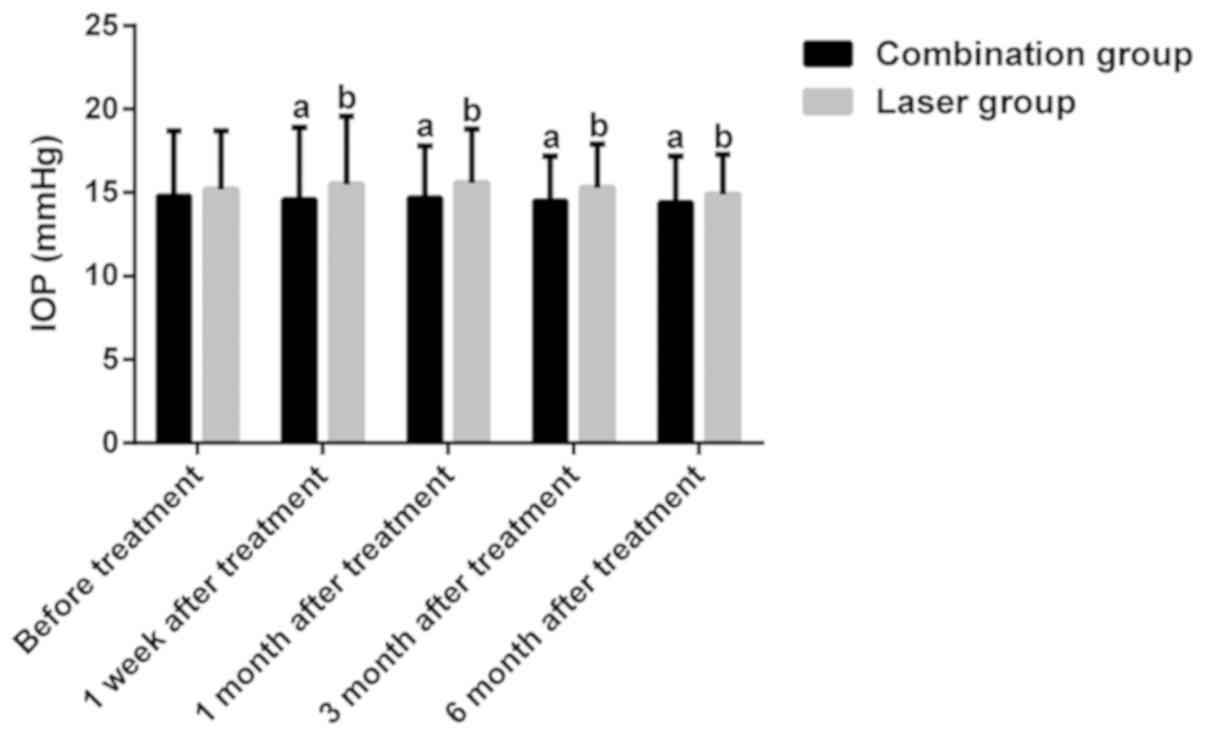
Changes in intraocular pressure before
and after treatment in the groups
No statistically significant difference was found in
intraocular pressure between and within the two groups before and
after treatment (P>0.05) (Fig.
4).
Times of drug injection and related
complications in the groups
In combination group, the average times of
intravitreal injection in affected eyes were 2.43±0.86 times, and
31 eyes received intravitreal injection 2-4 times. During treatment
and follow-up, no ocular complications (intraocular hypertension,
endophthalmitis, vitreous hemorrhage, retinal tear and iatrogenic
cataract) and systemic adverse reactions occurred.
Influencing factors for visual
recovery in combination group after treatment
According to the Pearson correlation analysis, the
visual recovery of patients in combination group was positively
correlated with the logMAR BCVA before treatment, decrease value of
CMT at 1 month after treatment and times of drug injection
(P<0.05), while it was not correlated with the age or CMT before
treatment (P>0.05). The results of multivariate regression
analysis revealed that the visual recovery of patients in
combination group was associated with the logMAR BCVA before
treatment, decreased value of CMT at 1 month after treatment,
integrity of ELM and times of drug injection (P<0.05), while it
was not associated with the age, CMT before treatment or integrity
of ellipsoid zone (P>0.05) (Table
II).
 | Table IIPearson correlation analysis and
multiple regression analysis of the studied patients in combination
treatment group. |
Table II
Pearson correlation analysis and
multiple regression analysis of the studied patients in combination
treatment group.
| Factors | r-value | P-value |
|---|
| Pearson correlation
analysis |
|
Age | 0.087 | 0.695 |
|
Pretreatment
logMAR BCVA | 0.434 | 0.001 |
|
Pretreatment
CMT (µm) | -0.172 | 0.506 |
|
Injection
times | 0.348 | 0.001 |
|
One month
posttreatment CMT (µm) | 0.593 | 0.001 |
| Multiple regression
analysis |
|
Age | -0.310 | 0.784 |
|
Pretreatment
logMAR BCVA | 5.525 | 0.001 |
|
Pretreatment
CMT (µm) | 2.103 | 0.074 |
|
Injection
times | 0.418 | 0.570 |
|
1 month
posttreatment CMT (µm) | 6.763 | 0.001 |
|
ELM
completeness | -0.425 | 0.001 |
|
EZ
completeness | -1.790 | 0.181 |
Discussion
Secondary ME is the major cause of diminution of
vision in BRVO patients, and its pathogenesis is mainly retinal
circulatory disorder and venous circuity and distention, in which
the local ischemia and hypoxia lead to the destruction of the
retinal blood-oxygen barrier and the damage of retinal pigment
epithelial cells, and the fundus microangiopathy results in
leakage, thus causing retinal tissue edema and ME when involving
macula (9). It has been found in
recent studies that the level of VEGF in the vitreous body of BRVO
patients is higher, and the high expression of VEGF leads to
exudation of serum protein, and promotes angiogenesis and ME.
Therefore, anti-VEGF can alleviate and treat ME secondary to BRVO
(10,11). Conbercept, a kind of fully humanized
recombinant fusion protein, can block all VEGF-A subtypes, VEGF-B
and placental growth factor, reduce vascular leakage, and inhibit
vascular endothelial cell proliferation and angiogenesis, thereby
treating ME (12). Multiple studies
have shown that intravitreal injection of Conbercept can rapidly
improve the visual acuity of patients with ME secondary to RVO, but
the duration of action of this drug is limited, and multiple
injections are required, which causes a certain economic burden for
patients (13-15).
Laser photocoagulation is a conventional treatment
means for BRVO, its mechanism is that due to the destruction of
photoreceptor cells and retinal pigment epithelial cells, the
oxygen content in the inner retina relatively increases, the
contraction of arterioles is caused, and the pressure of capillary
network and vein relatively declines, thereby reducing vascular
leakage and alleviating ME (16).
However, it is difficult to perform laser photocoagulation in the
case of severe ME and retinal edema, and great bleeding, and it has
been confirmed that the affected eyes often suffer from visual
field defect and decline in contrast sensitivity after laser
photocoagulation, affecting the recovery of visual function
(17). Therefore, some scholars have
proposed that combining laser photocoagulation and anti-VEGF drugs
can not only improve the efficacy on ME, but also facilitate the
recovery of visual function of patients, which has high clinical
application value.
Our study compared the efficacy and safety of simple
retinal photocoagulation with intravitreal injection of Conbercept
combined with retinal photocoagulation for the treatment of macular
edema secondary to BRVO. It was found that CMT was significantly
smaller in combination group than that in laser group at each time
point after treatment, and the possible reason is that Conbercept
inhibits pathological neovascularization, induces differentiation,
increase migration of vascular endothelial cells, improves vascular
endothelial cell function, reduces the elimination of retinal
endothelial system on granular antigens, and repairs the structure
and function of blood-retinal barrier, thereby alleviating fluid
exudation and inflammatory response (18). Moreover, the scar tissues produced by
retinal photocoagulation maintain the blood-retinal barrier,
promote the absorption of diffuse ME, and reduce the lesions, thus
decreasing CMT (19). In addition,
the BCVA was also remarkably improved in combination group compared
with that in laser group at each time point after treatment, and
the possible reason is that Conbercept was used to alleviate ME
before retinal photocoagulation, providing an optimal opportunity
for photocoagulation. In the case of RVO secondary to macular
edema, the Conbercept is given via intravitreal injection. Because
of the rapid onset and strong effect of anti-VEGF treatment, it can
quickly and significantly reduce macular edema, and can make the
cornea-like photocoagulation in the macular area. Low energy is
more efficiently accomplished, achieving better therapeutic results
with smaller lesions, thereby reducing the frequency of treatment,
avoiding recurrence and improving vision in patients with RVO
macular edema (20).
In this study, the results showed that the visual
recovery was not associated with age and CMT before treatment, but
positively correlated with BCVA before treatment. A study has
proved that the course of disease is associated with the degree of
visual recovery, so only those patients with a course <3 months
were enrolled in this study (21).
Besides, research has revealed that the simple fracture of
ellipsoid zone can repair autonomously, but beyond recovery if it
is combined with ELM damage, suggesting that ELM plays an important
role in the damage repair of ellipsoid zone (22). In this study, the results manifested
that the integrity of ellipsoid zone had no correlation with visual
recovery after treatment. However, Inoue et al (23) found that there are still repair of
ellipsoid zone and visual recovery at 12 months after treatment.
The reason may be related to the short observation time in this
study. Moreover, it was observed that the integrity of ELM may play
a significant role in the recovery of visual function, and the
changes in CMT and the structural integrity of ELM at 1 month after
the first treatment are of certain value in the prognosis
evaluation of visual acuity.
However, the results in this study need to be
further verified using large numer of samples in multi-center
randomized controlled trials.
In conclusion, intravitreal injection of Conbercept
combined with retinal photocoagulation can effectively improve the
visual acuity and reduce the CMT of patients. The visual recovery
of patients after treatment is correlated with the BCVA before
treatment, decreased value of CMT at 1 month after treatment and
integrity of ELM.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
BW and LC designed the study and performed the
experiments, SF and LC collected the data, BW and SF analyzed the
data, BW and LC prepared the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Yantaishan Hospital (Yantai, China). Signed informed consents were
obtained from all participants before the study.
Patient consent for publication
Patients or their guardians provided written
informed consent for publication.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
Yau JW, Lee P, Wong TY, Best J and Jenkins
A: Retinal vein occlusion: An approach to diagnosis, systemic risk
factors and management. Intern Med J. 38:904–910. 2008.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pierru A, Girmens JF, Héron E and Paques
M: Retinal vein occlusions. J Fr Ophtalmol. 40:696–705.
2017.PubMed/NCBI View Article : Google Scholar : (In French).
|
|
3
|
Jaulim A, Ahmed B, Khanam T and
Chatziralli IP: Branch retinal vein occlusion: Epidemiology,
pathogenesis, risk factors, clinical features, diagnosis, and
complications. An update of the literature. Retina. 33:901–910.
2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Feltgen N and Pielen A: [Retinal vein
occlusion: Epidemiology, classification and clinical findings].
Ophthalmologe. 112:607–618; quiz 619-620. 2015.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
5
|
Ehlers JP, Kim SJ, Yeh S, Thorne JE,
Mruthyunjaya P, Schoenberger SD and Bakri SJ: Therapies for macular
edema associated with branch retinal vein occlusion: A report by
the American Academy of Ophthalmology. Ophthalmology.
124:1412–1423. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Spaide RF: Retinal vascular cystoid
macular edema: Review and new theory. Retina. 36:1823–1842.
2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Campochiaro PA, Heier JS, Feiner L, Gray
S, Saroj N, Rundle AC, Murahashi WY and Rubio RG: BRAVO
Investigators. ranibizumab for macular edema following branch
retinal vein occlusion: Six-month primary end point results of a
phase III study. Ophthalmology. 117:1102–1112.e1. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tadayoni R, Waldstein SM, Boscia F,
Gerding H, Gekkieva M, Barnes E, Das Gupta A, Wenzel A and Pearce
I: BRIGHTER Study Group. Sustained benefits of ranibizumab with or
without laser in branch retinal vein occlusion: 24-month results of
the BRIGHTER Study. Ophthalmology. 124:1778–1787. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Daruich A, Matet A, Moulin A, Kowalczuk L,
Nicolas M, Sellam A, Rothschild PR, Omri S, Gélizé E, Jonet L, et
al: Mechanisms of macular edema: Beyond the surface. Prog Retin Eye
Res. 63:20–68. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chen CH, Chen YH, Wu PC, Chen YJ, Lee JJ,
Liu YC and Kuo HK: Treatment of branch retinal vein occlusion
induced macular edema in treatment-naïve cases with a single
intravitreal triamcinolone or bevacizumab injection. Chang Gung Med
J. 33:424–435. 2010.PubMed/NCBI
|
|
11
|
Feng J, Zhao T, Zhang Y, Ma Y and Jiang Y:
Differences in aqueous concentrations of cytokines in macular edema
secondary to branch and central retinal vein occlusion. PLoS One.
8(e68149)2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Xia JP, Wang S and Zhang JS: The
anti-inflammatory and anti-oxidative effects of conbercept in
treatment of macular edema secondary to retinal vein occlusion.
Biochem Biophys Res Commun. 508:1264–1270. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sun Z, Zhou H, Lin B, Jiao X, Luo Y, Zhang
F, Tao S, Wu Q, Ke Z and Liu X: Efficacy and safety of intravitreal
Conbercept injections in macular edema secondary to retinal vein
occlusion. Retina. 37:1723–1730. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tang F, Qin X, Lu J, Song P, Li M and Ma
X: Optical coherence tomography predictors of short-term visual
acuity in eyes with macular edema secondary to retinal vein
occlusion treated with intravitreal conbercept. Retina: Jan 10,
2019 (Epub ahead of print).
|
|
15
|
Luo W, Jia F, Liu M, Wang Y and Zhang T:
The analysis of correlative factors of visual acuity with
intravitreal Conbercept injection in macular edema associated with
branch retinal vein occlusion. J Ophthalmol.
2018(7348153)2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tadayoni R, Waldstein SM, Boscia F,
Gerding H, Pearce I, Priglinger S, Wenzel A, Barnes E, Gekkieva M,
Pilz S, et al: BRIGHTER study group: Individualized stabilization
criteria-driven ranibizumab versus laser in branch retinal vein
occlusion: Six-month results of BRIGHTER. Ophthalmology.
123:1332–1344. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Brown DM, Ou WC, Wong TP, Kim RY, Croft DE
and Wykoff CC: DAVE Study Group. Targeted retinal photocoagulation
for diabetic macular edema with peripheral retinal nonperfusion:
Three-year randomized DAVE trial. Ophthalmology. 125:683–690.
2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yan M, Huang Z, Lian HY, Song YP and Chen
X: Conbercept for treatment of choroidal neovascularization
secondary to pathologic myopia. Acta Ophthalmol. 97:e813–e814.
2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lang GE, Liakopoulos S, Vögeler J, Weiß C,
Spital G, Gamulescu MA, Lohmann C and Wiedemann P: The RELATION
study: Efficacy and safety of ranibizumab combined with laser
photocoagulation treatment versus laser monotherapy in NPDR and PDR
patients with diabetic macular oedema. Acta Ophthalmol.
96:e377–e385. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ishibashi T, Li X, Koh A, Lai TY, Lee FL,
Lee WK, Ma Z, Ohji M, Tan N, Cha SB, et al: REVEAL Study Group: The
REVEAL Study: Ranibizumab monotherapy or combined with laser versus
laser monotherapy in Asian patients with diabetic macular edema.
Ophthalmology. 122:1402–1415. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Januschowski K, Feltgen N, Pielen A,
Spitzer B, Rehak M, Spital G, Dimopoulos S, Meyer CH and Szurman
GB: Bevacizumab Study Group Venous Occlusion. Predictive factors
for functional improvement following intravitreal bevacizumab
injections after central retinal vein occlusion. Graefes Arch Clin
Exp Ophthalmol. 255:457–462. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Theodossiadis PG, Grigoropoulos VG and
Theodossiadis GP: The significance of the external limiting
membrane in the recovery of photoreceptor layer after successful
macular hole closure: A study by spectral domain optical coherence
tomography. Ophthalmologica. 225:176–184. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Inoue M, Watanabe Y, Arakawa A, Sato S,
Kobayashi S and Kadonosono K: Spectral-domain optical coherence
tomography images of inner/outer segment junctions and macular hole
surgery outcomes. Graefes Arch Clin Exp Ophthalmol. 247:325–330.
2009.PubMed/NCBI View Article : Google Scholar
|