Introduction
Cervical cerclage is used to correct cervical
insufficiency in order to prevent second-trimester loss and
premature childbirth. Traditionally, a cerclage is placed via a
vaginal approach. Placement of the cervical cerclage via an
abdominal approach is recommended in patients with a prior failed
vaginal cerclage or with extreme cervical shortening or deformity
(1,2). With the advances of minimally invasive
surgery, laparoscopic transabdominal cerclage (LTAC) appears to
become the preferred treatment option, with a success rate of
79-100% (3). To overcome the
cerclage insertion difficulties in pregnancy, a modified LTAC was
developed, where the tape is placed laterally to the uterine
vessels (4). However, there is
scarce information on the impact of this procedure on the
trajectories of the uterine arteries (UtAs) and the
uterine-placental circulation. Our experience with a successful
modified LTAC performed during the first trimester of pregnancy is
reported. The effects of the cerclage on the spatial configuration
of the UtAs and of the pulsatility index (PI) along the gestation
and fetal growth and development were assessed.
Case report
Modified laparoscopic transabdominal
cerclage
A female patient of 31 years of age, gravida 1,
presented for prenatal care to our Institution at 7-week of
gestation. The patient provided a signed informed consent agreeing
to participate in the study and consented in writing to the
anonymized use of information from medical records and the
publication of clinical images.
The medical history of the patient was relevant for
two cervical conizations for cervical dysplasia. Otherwise, she was
healthy. Speculum examination found a small size cervix, flushed to
the vagina. The cervical length measured by transvaginal ultrasound
was 16 mm. The woman was offered a laparoscopic abdominal cerclage
and was counseled on the advantages and risks of the procedure. The
cerclage was placed at 11+6 week gestation, using the modified LTAC
technique described by Shin et al (4). Briefly, the woman was placed under
general anesthesia, and after the pneumoperitoneum was obtained and
the ports were placed, a fenestration was made into the posterior
leaf of the broad ligament. The peritoneum was incised at the
uterovesical fold, and the bladder was reflected downward for
complete uterine isthmus exposure. This incision was carried
laterally to expose the uterine vessels. A Mersilene tape (5 mm;
Ethicon) was passed through the broad ligament window, laterally to
the uterine vessels, with direction from posterior to anterior. The
tape was taut until it was flattened along the posterior uterine
wall and tied in a knot on the anterior aspect of the uterus. The
vesicouterine reflection was reapproximated, covering the Mersilene
knot. Placement of the laparoscopic cerclage was uncomplicated,
with minimal blood loss. The fetal heart rate was normal before and
after the procedure. The patient recovered well after the
intervention and was discharged home the following day.
The scan at 12+0 weeks of gestation found a
crown-rump length (CRL) of 56 mm and a mean UtA pulsatility index
(PI) of 2.06 (1.199 MoM). The mean arterial pressure at 12 weeks
was 88 mmHg (1.083 MoM), and PAPP-A was 2.788 IU/l (0.842 MoM). The
woman had an increased calculated risk of preeclampsia and fetal
growth restriction before 37 weeks, of 1:103 and 1:49, respectively
(5,6). Consequently, she was advised to take
150 mg daily prophylactic dose of aspirin until 35 weeks of
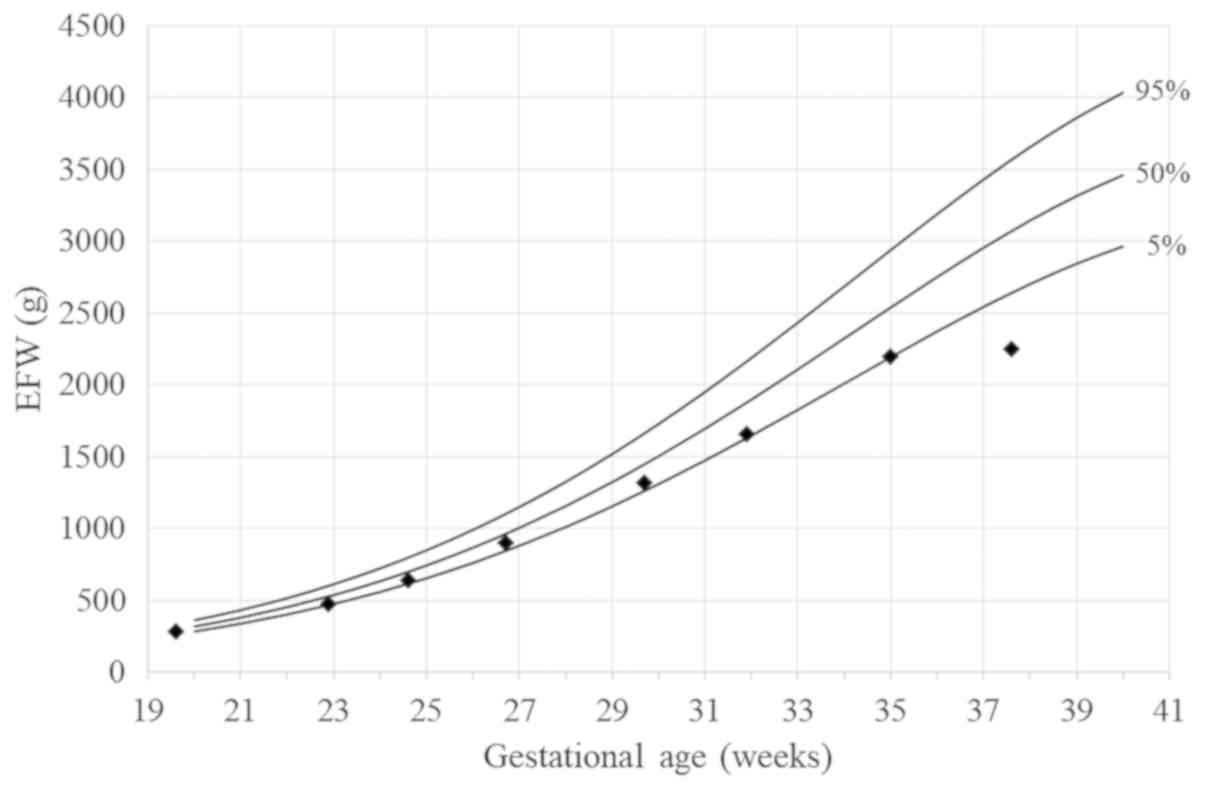
gestation. The pregnancy progressed uneventfully, with an estimated
fetal weight (EFW) in the second decile, until 32+0 gestational
weeks, when the EFW was 1,660 g, corresponding to the 8th
percentile on the fetal growth curve (Fig. 1). From here on, with a diagnostic of
small for gestational age (SGA), a serial sonographic assessment
was carried for fetal weight, amniotic fluid index, and PI of
umbilical artery (UA), middle cerebral artery (MCA),
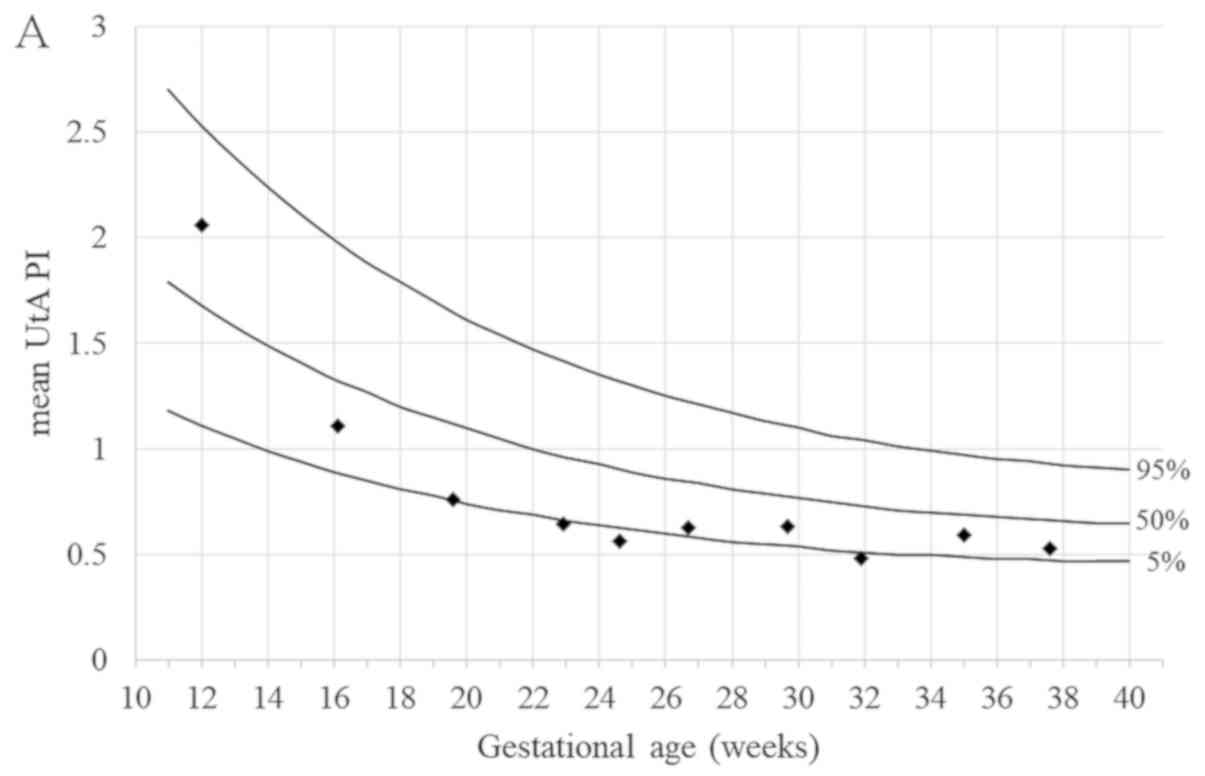
cerebroplacental ratio (CPR), and UtA. The Doppler parameters were
normal until 37+4 weeks gestation when the CPR dropped below the
5th percentile (Fig. 2).
Oligohydramnios (AFI 2.5 cm) and fetal heart rate decelerations
were also present. Therefore, emergency cesarean delivery was
performed. A female infant with a double nuchal cord, a birth
weight of 2,230 g (1st percentile on the growth curve) (7), and an Apgar score of 8/9/9 at 1/5/10
min was delivered in safe conditions. The infant was admitted to
the neonatal unit and experienced no complications. At the time of
the cesarean section, the cerclage was left in situ.
Assessment of maternal-placental-fetal
circulation
The appearance of the cerclage was assessed
throughout the pregnancy using three-dimensional (3D) ultrasound
volumes, as previously described by Ichizuka et al (8). There was no looseness of the tape
observed, the internal diameters of the cerclage ring being
constant at 26x19 mm. We found, however, that the suture ring
rotated soon after the insertion (at 12 weeks scan) to the right
such as the knot was located on the right side of the cervix. The
distance from the center of the cerclage to the external cervical
os increased from 20 to 30 mm from 12- to 37-weeks' gestation.
The PI of UA and both UtAs were measured at every
prenatal consultation until delivery. The UA PI was in the normal
ranges throughout the pregnancy. The mean UtA PI was low, varying
around the 5th percentile (0.57-0.74 MoM). Notably, the PI of the
left UtA, on the side of placental insertion, was markedly low,
below the fifth percentile, with a low-velocity flow (Fig. 2).
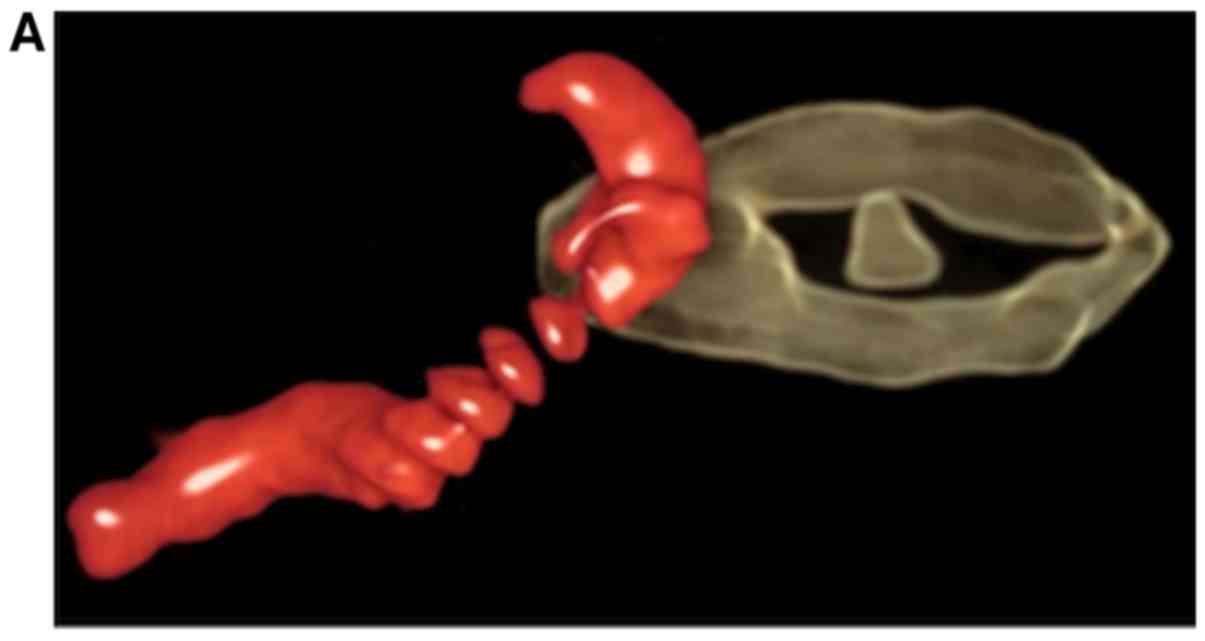
The UtAs pathway at the level of the abdominal
cerclage was evaluated using three-dimensional power Doppler
reconstruction. We acquired pelvic power Doppler ultrasound
volumes, transvaginally, with a Voluson E10 machine (GE Healthcare)
and a RIC 5-9D probe as previously described (9). Following the acquisition, the volume
was rotated and translated in a multiplanar display, to obtain an
image of the whole tape around the cervix. Then, using the magic
cut option, we deleted the gray volume component around, leaving
only a thin slice with the cerclage ring in the middle.
Additionally, we removed all color data not belonging to the UtA
from inside of the ultrasound volume. The image was analyzed by
glass body rendering in the HD live silhouette mode.
At 12 weeks gestation, 3D power Doppler showed both
UtAs passing inside the cerclage ring. The right UtA had a straight
ascending pathway, whereas the left UtA was bent, with an ascending
and descending segment, apparently pulled by the cerclage (Fig. 3A and B; Videos S1
and S2).
At 17 weeks, the right UtA still had an ascending
path, with a new branch to the uterus. The left UtA trajectory
maintained the bending at the tape, but there was a reduced view of
the ascending branch. The post-tape segment was better visualized,
with multiple, enhanced connections of the uterine vasculature
shown by the Doppler vascular signals (Fig. 3C and D; Videos S3
and S4).
The anatomy was different at 22 weeks, when the
right UtA formed a large, deep loop inferior to the cerclage ring.
On the left side, the trajectory of the UtA could not be identified
with certainty within the cerclage ring, where there was no Doppler
signal. The scan was adjusted to a low threshold for the vascular
flow speed (low pulse repetition frequency), which, however,
increased the artifacts and the vascular signal around the UtA.
There was increased vascularization above the cerclage plane,
towards the uterus, but not below the plane, where there was a poor
signal from some of the vessels oriented inside of the ring.
Analysis of the ultrasound volume was not able to identify any
vascular connection between these two zones (Fig. 3E and F; Videos S5
and S6).
After 22 weeks of gestation, the characterization of
the configuration of the UtAs was not possible because of the high
segmentation of Doppler signal and chaotic vascularization.
Discussion
A case of a pregnant women who required an abdominal
cerclage at 11 weeks gestation due to a short cervix diagnosed in
the first trimester was reviewd. Our case is unique in that we
assessed the impact the cerclage had on the
maternal-placental-fetal circulation by measuring the hemodynamic
parameters of the flow of UtAs and 3D-visualisation of the
remodeling of the uterine circulation.
What is different in our case from the traditionally
reported transabdominal cerclages is the modified technique of
cerclage insertion. Very few similar cases have been reported in
the literature using the modified laparoscopic cervico-isthmic
cerclage. However, in those reports, the indication for the
modified cerclage was incompetent cervix (10), whereas we chose the method for an
early diagnosed short cervix. By placing the suture lateral of the
UtAs, one tries to overcome some of the technical challenges of the
traditional LTAC performed during pregnancy, aiming to decrease the
operational time and morbidity (11). Firstly, there is an increased risk of
bleeding due to the highly vascular area close to the UtAs and
parametrial veins. The UtAs engorgement makes their skeletonization
more difficult compared with the pre-conceptional cerclage
(12). Also, the development of UtA
windows among gravid patients is more challenging (12). Modified LTAC, in the series reported
by Shin et al (4), was
associated with lower blood loss, shorter operation time, and
postoperative recovery compared with the traditional LTAC.
Secondly, the inability to manipulate the gravid uterus poses
particular challenges in the traditional cerclage (4,12).
Gestational age is an essential factor in the manipulation of the
impregnated uterus, and Shin et al showed that no uterine
manipulation is required to perform the modified LTAC if done
between 11- and 14-weeks of gestation (4). Thirdly, the post-conception cerclage is
associated with an increased risk of spontaneous miscarriage and
fetal death. First-trimester pregnancy loss was reported as 5%
(4/80) in a modified LTAC series (4), which was similar to the 4.1% early
fetal deaths (before 20 weeks gestation) reported after traditional
LAC (13).
However, the effect of the modified LTAC on uterine
vessels and fetal development is one of the most significant
issues, although sparsely studied to date. Previous reports
suggested that this technique does not entirely block the blood
flow to the uterus because of an extensive network of collateral
connections that provides rich anastomotic communication between
different major pelvic vessel systems (4,10). The
PI measured at the level of the umbilical artery throughout the
gestation, as measured by Seo et al (10) and also reported by us in the present
study, support this concept. Furthermore, Shin et al found
that the umbilical artery S/D ratio did not vary significantly at
30 and 34 weeks of gestation between the group who underwent
modified LTAC and the healthy controls (4).
The effect of cerclage on fetal growth and
development is another issue intensely debated in the literature.
Using birthweight as a proxy to assess fetal growth and
development, Seo et al reported normal fetal growth, with
birthweight at the 19th percentile at 37 weeks in a case of
modified LTAC (10). In a cohort of
80 women who underwent modified LTAC, Shin et al found that
26% of cases (16/72) had a birth weight below 2,500 g, some of
these women also developing severe pregnancy-induced hypertension
(4). In our case, the fetus had a
relatively low, albeit normal, EFW all along gestation only to
develop an SGA status starting at 32 weeks gestation. However, the
changes in the maternal-placental-fetal circulation ensued later,
at 37 weeks gestation, when abnormal Doppler studies and fetal
heart activity, prompted urgent delivery by emergency cesarean
section. Our patient, although at risk of preeclampsia, received
prophylaxis with low dose aspirin and did not develop gestational
hypertension.
In this context, we believe that the course of PI
changes at the level of UtAs could be of significance. Starting
from 16 weeks of gestation, we found low values of the UtAs mean
PI, around the 5th centile. Furthermore, the PI of the UtA on the
side of placental insertion (left side in our case) was also very
low, less than the 5th centile. This finding is in agreement with
previous studies that showed the UtA PI at the placental site to be
lower than that at the nonplacental site (14), likely determined by the early
development of the uterine collateral circulation, with decreased
resistance. Also, low resistance of the uterine circulation could
be a sign of uterine congestion, enhanced by the modified placement
of the cerclage. Of note, Seo et al found normal values of
UtAs mean PI in their reported case (10).
Using three-dimensional power Doppler reconstruction
of the UtAs, we show that their appearance varies throughout the
gestation. Moderate variation in the shape and curvature could
result from the elongation of the UtAs (9) or positional changes of the entire
cervical complex within the pelvis. Once a cerclage is placed, this
would alter to a certain degree the anatomy of the uterine
circulation. Within the vicinity of the cerclage ring, we
identified both UtAs from 12 to 17 weeks of gestation. Later in
pregnancy, one of the UtAs maintained the typical pathway until
delivery, whereas on the other side, where the UtA blood flow was
limited, we found a rich vascularization, especially above the
plane of the cerclage ring and near the uterus. This
vascularization developed from 16 weeks of gestation and could be
associated with the progress of the collateral circulation. On the
placental side, the low velocity and pulsatility of the blood flow
in the left UtA complicated the viewing of the arterial pathway by
overlapping the venous flow signal from the surrounding vessels.
These characteristics of the blood flow might explain the failure
in the visualization of the UtA beyond 22 weeks gestation.
Development of varicose veins around the cerclage was recently
reported in a 28 weeks pregnancy in a patient with abdominal
cerclage inserted after a radical trachelectomy (15).
Finally, we did not find any change in the
dimensions or shape of the tape along the gestation, as previously
reported (10). We did find,
however, that the distance between the external cervical os and the
center of the ring increased with 10 mm by the time of delivery. We
speculate that this may represent mechanical modeling of the cervix
during the late gestation, the mechanism of which is uncertain.
Such cervical changes have not been described before.
In conclusion, we reviewed a successful LTAC at 12
weeks gestation that was followed up with the assessment of growth
and maternal-placental-fetal circulation throughout pregnancy. The
3D power Doppler reconstruction viewed both UtAs inside the
cerclage ring, and we were able to demonstrate that rich collateral
vascularization develops within few weeks from the insertion of the
cerclage, as early as 16 weeks of gestation. We found an adaptation
of the circulation of UtAs that aims to ensure adequate flow to the
placenta. At the same time, there was a significant increase in
cervical length during gestation. Whereas, modified LTAC allows a
safer technique, the impact of the cerclage on the pregnancy
circulation and hemodynamics and fetal growth and development
warrants further research.
Supplementary Material
Supplementary Data 1
Supplementary Data 2
Supplementary Data 3
Supplementary Data 4
Supplementary Data 5
Supplementary Data 6
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The data used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author's contributions
DN and AEV conceived and designed the study. DN,
REB, and IAT provided care to the patient. CC and EB performed the
surgery. DN and AEV drafted the manuscript. IAT, REB, CC and EB
revised critically the manuscript and made substantial intellectual
contributions to the study. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Patient consent to participate was obtained.
Patient consent for publication
The patient provided a signed informed consent
agreeing to participate in the study. The patient consented in
writing to the anonymized use of information from medical records
and the publication of clinical images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Clark NV and Einarsson JI: Laparoscopic
abdominal cerclage: A highly effective option for refractory
cervical insufficiency. Fertil Steril. 113:717–722. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Shennan A, Chandiramani M, Bennett P,
David AL, Girling J, Ridout A, Seed PT, Simpson N, Thornton S,
Tydeman G, et al: MAVRIC: A multicenter randomized controlled trial
of transabdominal vs transvaginal cervical cerclage. Am J Obstet
Gynecol. 222:261.e1–261.e9. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ades A, Dobromilsky KC, Cheung KT and
Umstad MP: Transabdominal cervical cerclage: Laparoscopy versus
laparotomy. J Minim Invasive Gynecol. 22:968–973. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Shin SJ, Chung H, Kwon SH, Cha SD, Lee HJ,
Kim AR, Hwang I and Cho CH: The feasibility of a modified method of
laparoscopic transabdominal cervicoisthmic cerclage during
pregnancy. J Laparoendosc Adv Surg Tech A. 25:651–656.
2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Karagiannis G, Akolekar R, Sarquis R,
Wright D and Nicolaides KH: Prediction of small-for-gestation
neonates from biophysical and biochemical markers at 11-13 weeks.
Fetal Diagn Ther. 29:148–154. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
O'Gorman N, Wright D, Syngelaki A,
Akolekar R, Wright A, Poon LC and Nicolaides KH: Competing risks
model in screening for preeclampsia by maternal factors and
biomarkers at 11-13 weeks gestation. Am J Obstet Gynecol.
214:103.e101–103.e112. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Nicolaides KH, Wright D, Syngelaki A,
Wright A and Akolekar R: Fetal Medicine Foundation fetal and
neonatal population weight charts. Ultrasound Obstet Gynecol.
52:44–51. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ichizuka K, Seo K, Dohi S, Ishikawa T,
Sekizawa A and Nagatsuka M: Three-dimensional ultrasound imaging of
intra-abdominal cervical-isthmus cerclage. Ultrasound Obstet
Gynecol. 51:704–705. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nemescu D, Navolan DB and Veduta A:
Spatial configuration of the uterine artery cervical segment in
3-dimensional reconstruction at 11 to 14 weeks' gestation. J
Ultrasound Med. 37:2717–2720. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Seo K, Dohi S, Ishikawa T, Ichizuka K,
Sekizawa A and Nagatsuka M: Modified laparoscopic cervicoisthmic
cerclage in early pregnancy for refractory cervical incompetence: A
case report. J Obstet Gynaecol Res. 45:1597–1602. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Whittle WL, Singh SS, Allen L, Glaude L,
Thomas J, Windrim R and Leyland N: Laparoscopic cervico-isthmic
cerclage: Surgical technique and obstetric outcomes. Am J Obstet
Gynecol. 201:364.e361–367. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Moawad GN, Tyan P, Awad C and Abi Khalil
ED: Surgical variance between postconceptional and preconceptional
minimally invasive transabdominal cerclage placement. Am J Obstet
Gynecol. 219:414.e411–414.e412. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Foster TL, Moore ES and Sumners JE:
Operative complications and fetal morbidity encountered in 300
prophylactic transabdominal cervical cerclage procedures by one
obstetric surgeon. J Obstet Gynaecol. 31:713–717. 2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kofinas AD, Penry M, Greiss FC Jr, Meis PJ
and Nelson LH: The effect of placental location on uterine artery
flow velocity waveforms. Am J Obstet Gynecol. 159:1504–1508.
1988.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tamada S, Masuyama H, Hayata K, Eto E,
Mitsui T, Eguchi T, Maki J and Tani K: Successful delivery after
abdominal radical trachelectomy, using transabdominal cerclage in
early pregnancy. Acta Med Okayama. 73:173–176. 2019.PubMed/NCBI View Article : Google Scholar
|