Introduction
Mophea, also known as localized scleroderma (LSc) or
circumscribed scleroderma, is an inflammatory cutaneous condition,
characterized by localized sclerosis of the skin (1). Morphea presents as single or multiple
inflammatory or sclerotic plaques, which are usually active for 3-6
years (2). This skin condition
presents in several clinical forms: plaque (circumscribed),
generalized, linear (en coup de sabre) and deep morphea. Also, we
can classify morphea in: superficial (primarily dermal) or deep
(involving the deep dermis plus the subcutis, fascia, and/or bone)
(3). In most cases, the diagnosis of
morphea is clinical. Sometimes, the histopathological examination
may be useful (4). The treatment
depends on the stage and extension of morphea (5).
Case report
A case of a 60 year-old woman is presented, who was
referred to the Dermatology Clinic for an evaluation of
erythematous-violaceus, asymptomatic eruption, located on the trunk
and legs, in evolution for 2 months. Her medical history revealed
an infection with Borrelia burgdorferi (1 year previously)
(Fig. 1), and dyslipidemia. The
patient was informed of the study and written informed consent was
obtained from the patient.
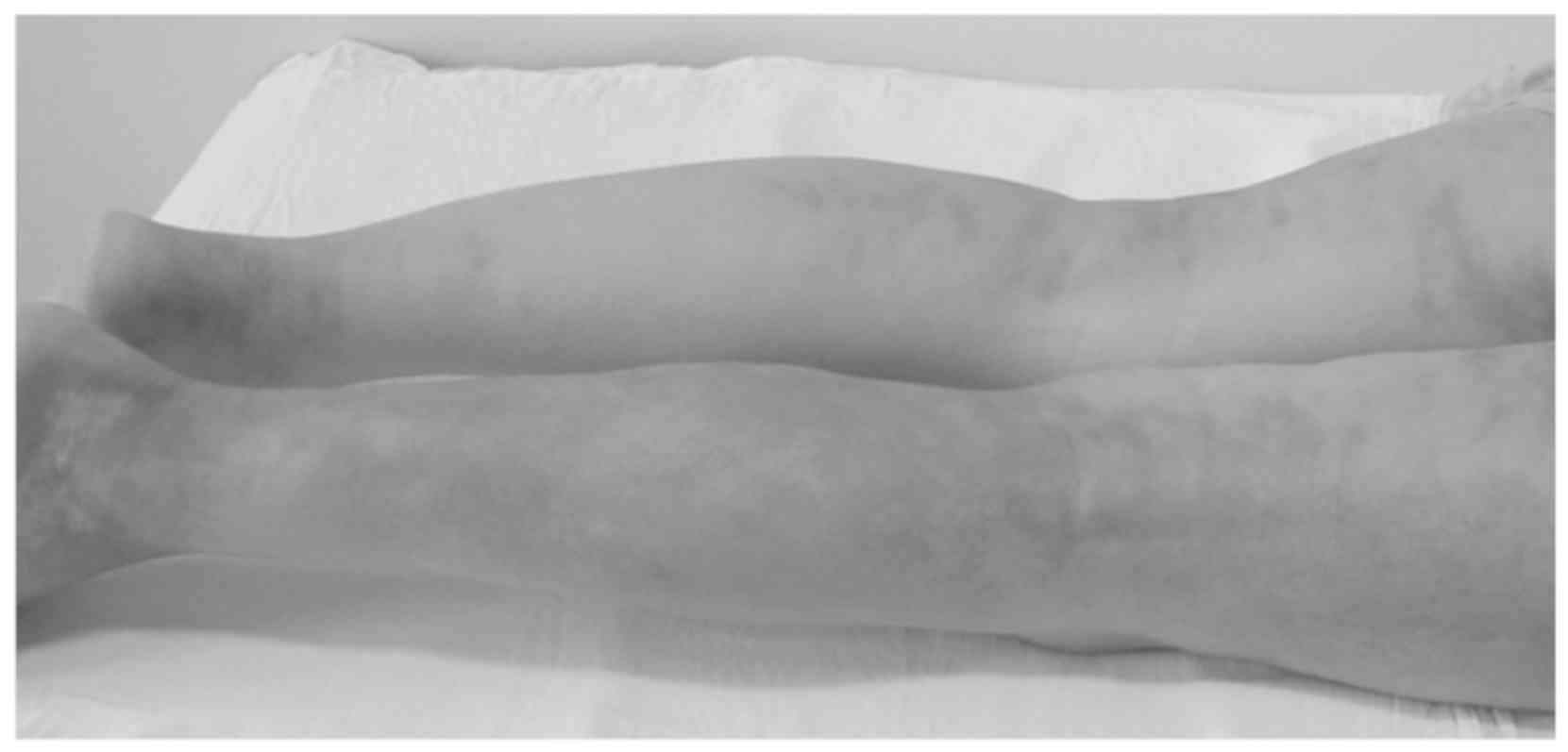
Physical examination showed grade II obesity.
Clinical examination revelead numerous erythematous-purple plaques,
indurated, relatively well delimited, with irregular edges, with
central atrophy, diameter 2-7 cm, disseminated at the level of the
trunk and lower limbs (Fig. 2).
Routine laboratory tests revealed inflammatory
syndrome and dyslipidemia. Radiological examination and
abdominal-pelvic ultrasound were within normal limits. Because a
form of morphea was suspected, several autoantibodies were
evaluated and antinuclear antibody serum levels were elevated;
anti-single-stranded DNA (ssDNA), anti-double-stranded DNA (dsDNA),
antihistone, anti-topoisomerase IIα and antiphospholipid antibodies
were negative. The medical history of our patient revealed
infection with Borrelia, which is known as an etiologic
factor of morphea.
Generalized morphea was suspected, so a skin biopsy
from a lesion was prelevated, and the histopathological examination
revealed moderate orthokeratosis and minimal epidermal basal
pigmentation; at the dermal level, areas of fibrosis were
identified, which focally compressed the attached structures (ducts
and sweat glands); minimal inflammatory lymphocyte inflitrate,
predominantly perinaexial or perivascular; papillary dermis with
homogenized appearance and turgid capillaries. The
histopathological findings supported the clinical diagnosis of
morphea. Corroborating the clinical, paraclinical data and
histopathological examination, the final diagnosis of generalized
morphea was establised.
The patient was hospitalized, and systemic treatment
initiated with corticosteroids (prednisolone 1 mg/kg per day,
slowly decreasing), associated with gastric protection and
methotrexate 15 mg/week, administered subcutaneously. This
treatment was chosen because there were multiple, indurated, and
disseminated lesions. As local treatment, the patient applied
tacrolimus 0.1% ointment. During hospitalization, the evolution was
favorable, with improvement of lesions. Upon discharge,
continuation of prednisolone in decreasing doses, with gastric
protection, continuation of the same dose of methotrexate, and
local treatment were recommended.
Four weeks after discharge, our patient presented to
evaluation, the evolution was favorable, with improvement of
injuries and induration. Moreover, there was no more inflammation
of the lesions. The recommendations were: continuing the cortizonic
treatment, with decreasing doses as in the initial scheme, under
gastric protection; keeping the same dose of methotrexate and local
treatment.
Discussion
The etiopathogenesis of morphea is not well
understood. Drugs, local trauma, environmental toxins or infections
may be involved in the pathogenesis. There are two processes that
trigger the disease: abnormal fibroblast function and immune
dysfunction resulting in autoimmunity (6). The possible mechanism involved in
pathogenesis of morphea, also in our patient, may be the infection
with Borrelia burgdorferi. According to some authors,
increased levels of antibodies against this organism, was higher in
patients with morphea compared with controls. They also identified
Borrelia DNA in skin biopsies of patients with morphea,
using polymerase chain reaction (7-9).
This theory is quite controversial, because other studies did not
show any association between morphea and Borrelia (10). A review concluded that
Borrelia infection may not be involved in triggering
morphea, or that only some species of Borrelia that live in
few countries in Europe and Asia may lead to developing this skin
condition (11). However, this
subject remains to be further studied: some authors suggested that
Borrelia may be responsable for morphea, as they reported a
case of a patient with morphea and this infection (12).
In some cases of morphea, the diagnosis of certainty
is established by histopathological examination. A skin biopsy can
be taken from the inflammatory margin or from the central
sclerosis. It is always important to take the biopsy with
subcutaneous fat, because the changes are seen at the border
between the dermis and subcutaneous fat. At the inflammatory
border, interstitial and perivascular inflammatory cell infiltrate
is found (lymphocytes, plasma cells, eosinophils, mast cells,
macrophages). In contrast, the atrophic phase reveals loss of
inflammatory cell infiltrate, less sclerosis and absence of
appendageal structures. Some authors suggested that patients with a
histopathological pattern of sclerosis were associated with pain
more often than others (4).
The treatment of morphea varies depending on the
severity of the disease. Circumscribed lesions respond well to
low-concentration dermatocorticoids, intralesional corticosteroids,
topical tacrolimus or topical calcipotrione (13). In moderate-to-severe disease (for
example, generalized morphea), first line therapy is represented by
methotrexate, with or without corticosteroids (14). In non-responsive patients, other
systemic treatments may be beneficial: mycofenolate mofetil,
colchicine or cyclosporine (15).
Infliximab, an anti-TNF-α agent, is a human-murine chimeric drug,
composed by a constant human region and a variable mouse region
(16,17). Althought a report of a clinical case
responding to this biologic agent exists, there are not enought
data to support the efficacy of this drug (18).
Patients need to be educated on their comorbidities.
In case of our patient, who had associated dyslipidemia and
obesity, it was important to inform her of the risks of visceral
fat level (especially when treatment with methotrexate was
administered) (19).
Morphea is a chronic disorder, with periods of
exacerbations and remissions. It is important to follow up the
patients with morphea: every 2-4 months during the first year.
After the disease is under control, one visit each 6 months is
sufficient. Followed by one control per year, for clinical
evaluation should be enough. Whereas, if the disease is getting
worse, the patient should immediately present to examination
(20).
In conclusion, the etiophatogenesis of morphea is
not yet elucidated. Several mechanisms may be involved, and the
infection with Borrelia burgdorferi may be one of them. This
is why the medical history of the patient is very important. The
treatment of morphea varies depending on the severity of the
disease and follow-up of these patients is required.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
FS was involved in the writing of the manuscript and
was responsible for the patient follow up based on clinical and
paraclinical examinations. APo was involved in the conception of
the case study. APe analyzed the data from literature regarding the
etiologic role of Borrelia burgdorferi in morphea and was
involved in the writing of the manuscript. RGM was responsible for
the figures and the final aspect of the manuscript. MMC analyzed
the histological characteristics of the lesions and was responsible
for the writing of the relevant section of the manuscript. RCP
analyzed the main mechanisms involved in the etiophatogenesis of
morphea and was responsible for the writing of the relevant section
of the manuscript. TC examined the patient and wrote the section
regarding the clinical examination of the lesions. MCD was involved
in the conception and writing of the manuscript. All authors
critically revised the manuscript and approved the final version to
be published.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jablonska S: The concept of scleroderma
and its classification. In: Scleroderma and Pseudoscleroderma.
Jablonska S (ed). Polish Medical Publishers, Warsaw, pp3-10,
1975.
|
|
2
|
Provost TT, Greenberg AS and Falanga V:
Localized cutaneous sclerosis. In: Cutaneous Manifestations of
Rheumatic Diseases. 1st edition. Sontheimer RD and Provost TT
(eds). Williams & Wilkins, Baltimore, MD, p125, 1996.
|
|
3
|
Laxer RM and Zulian F: Localized
scleroderma. Curr Opin Rheumatol. 18:606–613. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jacobe H: Pathogenesis, clinical
manifestations, and diagnosis of morphea (localized scleroderma) in
adults - UpToDate. https://www.uptodate.com/contents/pathogenesis-clinical-manifestations-and-diagnosis-of-morphea-localized-scleroderma-in-adults.
Accessed May 31, 2019.
|
|
5
|
Jacobe H: Treatment of morphea (localized
scleroderma) in adults - UpToDate. https://www.uptodate.com/contents/treatment-of-morphea-localized-scleroderma-in-adults.
Accessed April 16, 2018.
|
|
6
|
Zulian F: Localized scleroderma in
childhood - UpToDate. https://www.uptodate.com/contents/localized-scleroderma-in-childhood.
Accessed April 3, 2019.
|
|
7
|
Aberer E, Kollegger H, Kristoferitsch W
and Stanek G: Neuroborreliosis in morphea and lichen sclerosus et
atrophicus. J Am Acad Dermatol. 19:820–825. 1988.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Aberer E, Stanek G, Ertl M and Neumann R:
Evidence for spirochetal origin of circumscribed scleroderma
(morphea). Acta Derm Venereol. 67:225–231. 1987.PubMed/NCBI
|
|
9
|
Schempp C, Bocklage H, Lange R, Kölmel HW,
Orfanos CE and Gollnick H: Further evidence for Borrelia
burgdorferi infection in morphea and lichen sclerosus et
atrophicus confirmed by DNA amplification. J Invest Dermatol.
100:717–720. 1993.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wienecke R, Schlüpen EM, Zöchling N,
Neubert U, Meurer M and Volkenandt M: No evidence for Borrelia
burgdorferi-specific DNA in lesions of localized scleroderma. J
Invest Dermatol. 104:23–26. 1995.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Weide B, Walz T and Garbe C: Is morphoea
caused by Borrelia burgdorferi? A review. Br J Dermatol.
142:636–644. 2000.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Aberer E, Neumann R and Stanek G: Is
localised scleroderma a Borrelia infection? Lancet.
2(278)1985.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cunningham BB, Landells ID, Langman C,
Sailer DE and Paller AS: Topical calcipotriene for morphea/linear
scleroderma. J Am Acad Dermatol. 39:211–215. 1998.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kreuter A, Gambichler T, Breuckmann F,
Rotterdam S, Freitag M, Stuecker M, Hoffmann K and Altmeyer P:
Pulsed high-dose corticosteroids combined with low-dose
methotrexate in severe localized scleroderma. Arch Dermatol.
141:847–852. 2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Vilela FA, Carneiro S and Ramos-e-Silva M:
Treatment of morphea or localized scleroderma: Review of the
literature. J Drugs Dermatol. 9:1213–1219. 2010.PubMed/NCBI
|
|
16
|
Constantin MM, Cristea CM, Taranu T, Bucur
S, Constantin T, Dinu A, Jinga M and Nita IE: Biosimilars in
dermatology: The wind of change. Exp Ther Med. 18:911–915.
2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Raducan A, Bucur S, Caruntu C, Constantin
T, Nita IE, Manolache N and Constantin MM: Therapeutic management
with biological anti-TNF-α agent in severe psoriasis associated
with chronic hepatitis B: A case report. Exp Ther Med. 18:895–899.
2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Diab M, Coloe JR, Magro C and Bechtel MA:
Treatment of recalcitrant generalized morphea with infliximab. Arch
Dermatol. 146:601–604. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Dumitrascu MC, Stanescu AMA, Bejan C,
Sandru F, Toader DO, Radavoi GD, Cotirlet A, Judea PCT and Diaconu
CC: Obesity and its implications on stress urinary incontinence.
Rev Chim (Bucharest). 70:3660–3662. 2019.
|
|
20
|
Mertens JS, Seyger MM, Kievit W,
Hoppenreijs EP, Jansen TL, van de Kerkhof PC, Radstake TR and de
Jong EM: Disease recurrence in localized scleroderma: A
retrospective analysis of 344 patients with paediatric- or
adult-onset disease. Br J Dermatol. 172:722–728. 2015.PubMed/NCBI View Article : Google Scholar
|