Introduction
Posterior ankle pain is a multifaceted condition
that can pose a major concern among young and middle-aged patients
(1). Haglund's deformity, first
described by the Swedish physician Patrick Haglund in 1928(2), is defined as an inflammation of the
bursa in the posterior calcaneus, which can lead to repetitive
mechanical impacts between the posterior calcaneus and Achilles
tendon (3). The inflammation can
cause pain and swelling, which may affect the patient's ability to
work or exercise (4).
Both conservative and surgical methods are used for
the treatment of Haglund's deformity. Patients showing poor
response to conservative treatment can undergo surgery to remove
the abnormally prominent posterior calcaneus and the subcondylar
inflammatory bursa (5). Due to its
continual development and improvements, endoscopy is becoming
increasingly popular (6,7), which can be performed using two- and
three-portal techniques (8).
Isokinetic muscle strength test implemented on the
Biodex system (9) is a method used
for evaluating and testing muscle function that has been applied in
clinical research in sports and rehabilitation medicine (10,11).
However, to the best of our knowledge, it has not been previously
applied for evaluating Haglund's deformity. This test can be
applied to the plantar flexors and dorsiflexors of the ankle joint
to evaluate muscle strength and endurance, providing reliable
clinical evidence of patient rehabilitation after endoscopic
calcaneoplasty (12). In the present
study, Biodex system test results, American Orthopaedic Foot and
Ankle Score (AOFAS) values and visual analog scale (VAS)scores
(13,14) were all obtained from each patient to
compare muscle strength and performance before surgery, then 3 and
6 months after surgery. The aim of the present study was to assess
the effectiveness of the Biodex system in determining postoperative
recovery for treating Haglund's deformity.
Patients and methods
Patients
A retrospective (medical records), level 3 evidence
study was performed to evaluate the outcomes of patients who
underwent endoscopic surgery for Haglund's deformity. The present
study included 34 patients (age range, 15-44 years; mean age,
31.3±11.6 years; sex, 30 men and 4 women) who were diagnosed with
Haglund's deformity and were treated by the authors from June 2012
to November 2018 at the Peking University Third Hospital (Beijing,
China). All patients, 2 of whom were professional athletes,
underwent conservative therapy initially, including physical
therapy, calf and ankle muscle strength exercises and oral
anti-inflammatory analgesics. Patients aged >45 years, suffering
with diseases involving the Achilles tendon and with Achilles
tendon rupture were all excluded. The present study was approved by
the Peking University Third Hospital's ethics committee. Written
informed consent was obtained from all patients, parents or
guardians of the patients prior to the present study. The rights of
the patients were protected.
Diagnosis
Patients were diagnosed based on subjective
complaints, combined with clinical and radiological examinations.
Radiological measurements for this disease include the
Fowler-Phillip angle, calcaneal pith angle, parallel pitch lines,
Chauveaux-Liet angle and the X/Y ratio (15-19).
Haglund's deformity would be suspected in cases where the lateral
angle between the plantar and posterior borders of the calcaneus,
also known as Fowler-Phillip angle, >75˚ (15-19).
For the examinations performed in the present study, the upper part
of the calcaneal nodule (noncalcaneus nodules) exhibited obvious
tenderness at 2-3 cm and posterior protrusion of the calcaneus. MRI
confirmed the abnormal ridge of the posterior calcaneus and the
presence of collateral fluid in the Achilles tendon. Suspected peep
or partial tearing of the Achilles tendon was observed in some
patients. All patients exhibited soft tissue swelling in or around
the Achilles tendon and pain in the stretched tendon.
Surgical technique
To prepare for the endoscopic procedure, each
patient was placed in the prone position under lumbar anesthesia.
In the present study, endoscopic calcaneoplasty was performed using
the two-portal technique. A tourniquet was applied to the lower
extremity, where 5-mm-long portals were made on the inner and outer
edges of the Achilles tendon at the posterior calcaneus level to
insert the endoscopes and surgical instruments. Surgical
instruments applied in the present study were as follows: i)
Endoscope, Smith & Nephew 560P High Definition Camera System;
ii) power equipment for blades and burr, Smith & Nephew Dyonics
Power II Control System; iii) blades, Smith & Nephew Dyonics
4.5 mm Synoblator blade platinum series (cat. no. 72203523); and
iv) burr (cat. no. 7205324), Smith & Nephew Dyonics 4.0 mm
abrader burr (All from Smith & Nephew plc.). In general,
endoscopes were inserted directly into the anterior sac of the
Achilles tendon to observe the inflammation of the synovium. For
some patients in the present study, planers were required to clean
portions of the adipose tissue on the ventral side so that the
Achilles tendon and calcaneus could be revealed completely. The
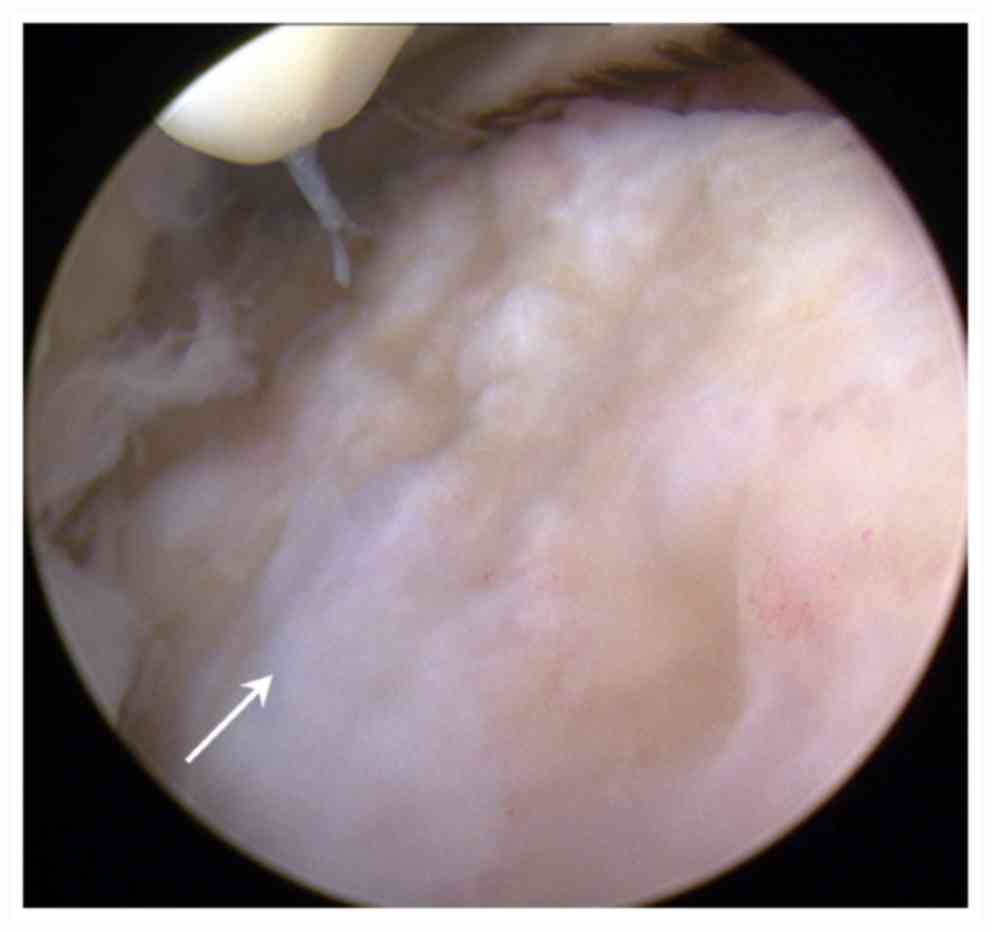
cartilage of the posterior superior calcaneus from 64.3% of the
patients was observed to be degenerated (Fig. 1). During ankle dorsiflexion,
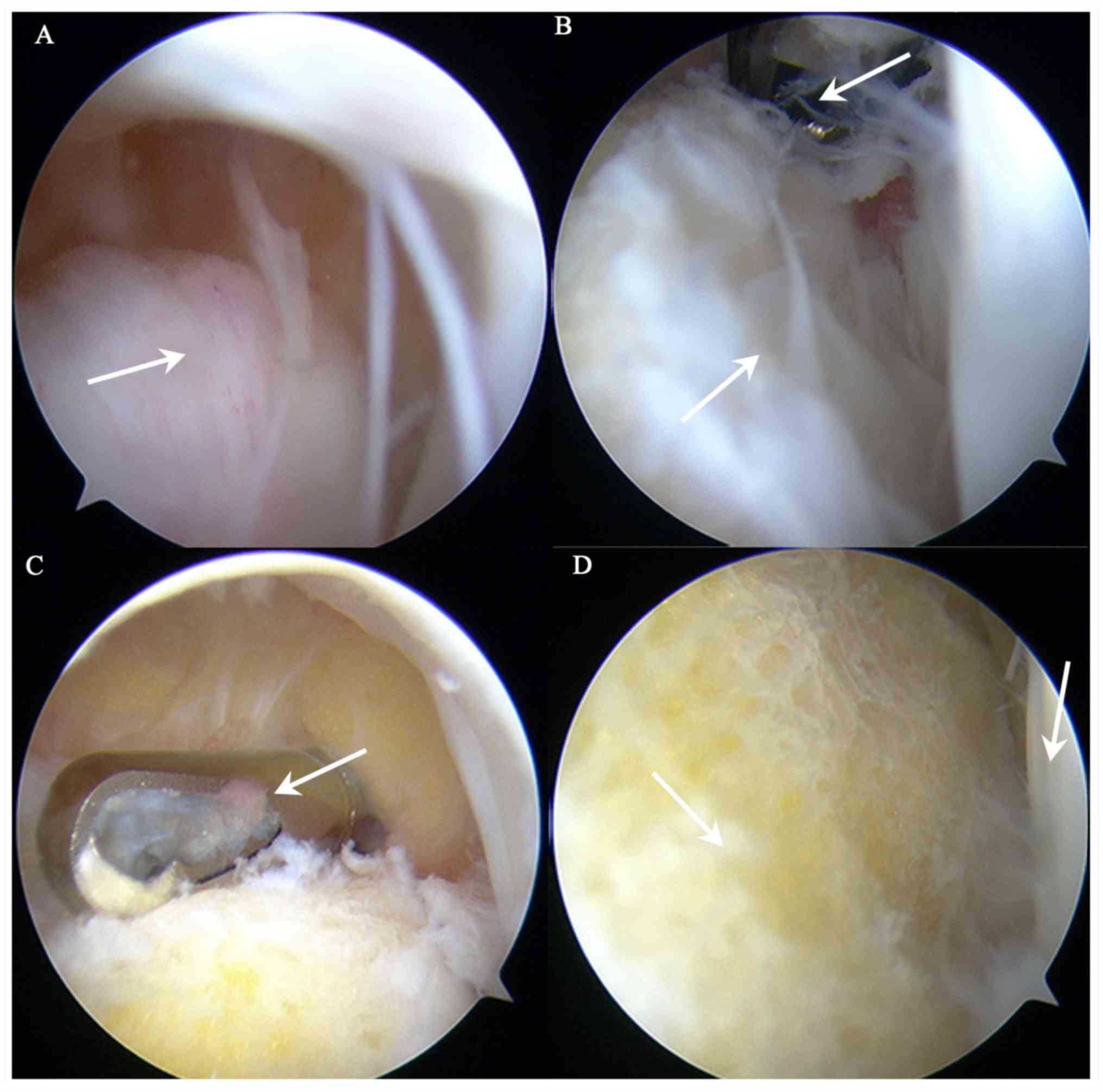
posterior calcaneus collided with the Achilles tendon in all
patients (Fig. 2). The prominent
posterior calcaneus was then polished to a flat or slightly concave
shape using a burr and the distal end of the calcaneus in front of
the Achilles tendon was resected (Figs.
3 and 4). This can completely
halt the collision action on dorsiflexion. Finally, the portals
were flushed and closed using pressure-wrapped cotton and a
splint.
Postoperative care
The plaster was removed 3 weeks after surgery. The
patients were instructed to wore shoes with a 2-cm-thick pad to
walk using their full weight for 9 weeks, whilst scheduled
activities such as lifting exercises were performed in parallel.
Recreational activities or special training was gradually resumed
after 3 months.
Anthropometric measurements
Isokinetic strength tests were conducted using the
Biodex system 1 week before surgery and then 3 and 6 months after
surgery. Accordingly, AOFAS values and VAS scores were also
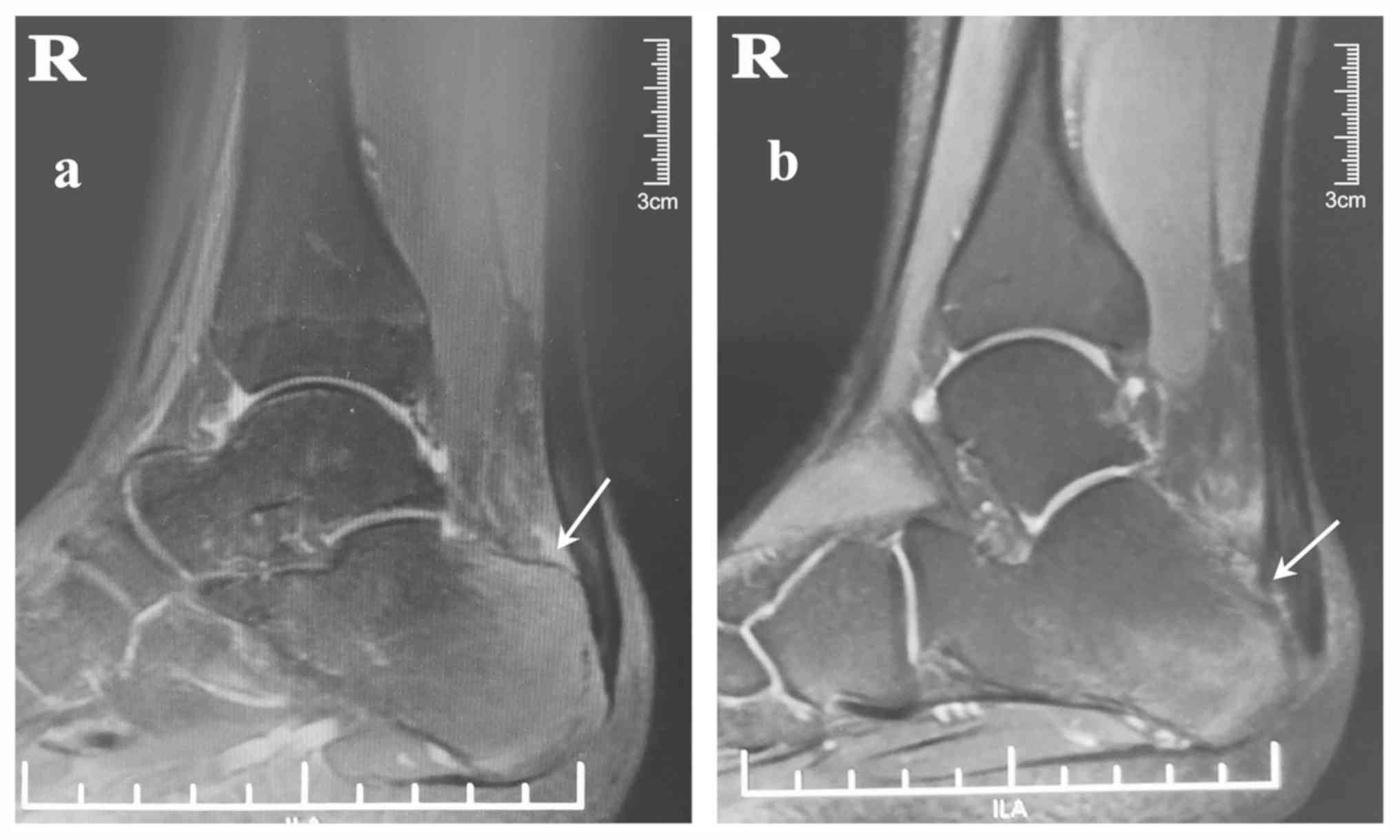
obtained preoperatively and at 3- and 6-month follow-ups. MRI and
X-ray were used to examine the patients after 5 months.
Self-evaluations of recovery were also recorded from each patient,
including the time taken for the recovery of daily life (months),
recovery of abilities to exercise (months) and work (months).
All isokinetic strength tests were performed using
the same dynamometer (Biodex System 3-Dynamometer; Biodex Medical
Systems, Inc). The dynamometer was used to measure the maximum
torque of the affected ankle at 60 and 120˚/sec before surgery and
3 and 6 months after surgery. The patients performed a
low-resistance warm-up for 5 min on a bicycle before the test.
Seated in a chair at 90˚, each patient's lower limbs were weighed
before the test, following which the results were adjusted in
accordance with the weight of the lower limbs to exclude the effect
of gravity during limb movement. The total range of motion was
120˚, set from 120˚ to 0˚ of leg flexion. Each patient performed
three submaximal contractions at 60˚/sec for warm-up, followed by a
30-sec rest before five maximal contractions at 60˚/sec. After a
1-min rest, the patients then performed three submaximal
contractions at 180˚/sec, followed by a 30-sec rest before five
maximal contractions at 180˚/sec. The uninjured side was tested
first, the results of which were used as the control. The injured
side was tested within 2 min after testing the uninjured side.
Data analysis
The peak extension and flexion torques for both
ankles as obtained using the Biodex system, along with AOFAS values
and VAS scores, were evaluated for all patients. Wilcoxon signed
rank test was used to analyze the difference between the uninjured
and injured sides in terms of the AOFAS values and VAS scores
evaluated preoperatively and those evaluated at the 3 and 6 months
postoperatively. Friedman's test followed by Nemenyi's test with
Bonferroni's correction was performed for comparing the AOFAS and
VAS scores before the operation, 3 and 6 months after the
operation. P<0.05 was considered to indicate a statistically
significant difference. Statistical analysis was performed using
the SPSS software (version 23.0; IBM Corp.).
Results
Biodex system results
Isokinetic strength test conducted on both the
injured and uninjured sides of the patients using the Biodex system
before surgery, then 3 and 6 months after surgery. No significant
differences were observed between the injured and uninjured sides
in dorsiflexion torque at 60 or 120˚/sec (Tables I and II). Conversely, significant differences
were observed between the injured and uninjured sides in
plantarflexion torque at 120 and 60˚/sec before surgery (P=0.036
and P=0.040, respectively). At 3 months after surgery, a
significant difference remained between the two sides tested in
plantarflexion torque at 120˚/sec (P=0.025). However, the
difference between the two sides at 60˚/sec was not found to be
significant (P=0.459). At 6 months after surgery, no significant
differences were found between the injured and uninjured sides in
plantarflexion torque at 120 or 60˚/sec.
 | Table IComparison of torque at 120˚/sec
between the injured and uninjured sides of 34 patients before and 3
and 6 months after surgery. |
Table I
Comparison of torque at 120˚/sec
between the injured and uninjured sides of 34 patients before and 3
and 6 months after surgery.
| | Plantar flexor | | Dorsal flexor | |
|---|
| Time | Uninjured | Injured | P-value | Uninjured | Injured | P-value |
|---|
| Before surgery | 28.5±11.6 | 22.3±7.2 | 0.036 | 17.9±10.1 | 14.5±6.4 | 0.073 |
| 3 months after
surgery | 29.5±15.2 | 22.9±10.1 | 0.025 | 18.2±10.3 | 15.4±9.1 | 0.099 |
| 6 months after
surgery | 30.4±16.1 | 25.7±11.4 | 0.061 | 17.4±6.2 | 16.0±8.4 | 0.151 |
 | Table IIComparison of torque at 60˚/sec
between the injured and uninjured sides of 34 patients before and 3
and 6 months after surgery. |
Table II
Comparison of torque at 60˚/sec
between the injured and uninjured sides of 34 patients before and 3
and 6 months after surgery.
| | Plantar flexor | | Dorsal flexor | |
|---|
| Time | Uninjured | Injured | P-value | Uninjured | Injured | P-value |
|---|
| Before surgery | 26.5±9.6 | 20.8±6.0 | 0.040 | 19.8±12.0 | 16.5±8.9 | 0.579 |
| 3 months after
surgery | 27.2±11.2 | 25.6±15.1 | 0.459 | 18.7±12.2 | 7±9.6 | 0.786 |
| 6 months after
surgery | 27.7±10.6 | 26.5±16.3 | 0.827 | 20.9±9.7 | 19.4±10.7 | 0.290 |
AOFAS and VAS results
The AOFAS values and VAS results obtained at the
follow-up time points exhibited a consistent trend with the results
obtained from the Biodex system (Table
III). Significant differences were observed among in those
before surgery, 3 and 6 months after surgery (P<0.001 and
P<0.001, respectively). Specifically, compared with those before
surgery, the AOFAS values and VAS scores increased, 3 and 6 months
after surgery. At 3 months, the AOFAS values and VAS results
reached 89.0±3.8/100 (range, 79-95; P<0.001 vs. before surgery)
and 3.1±0.6/10 (range, 2-5; P=0.002 vs. before surgery),
respectively. At 6 months, the AOFAS values and VAS scores reached
93.7±3.3/100 (range, 85-100; P<0.001 vs. before surgery;
P<0.001 vs. 3 months after surgery) and 1.5±0.4/10 (range, 1-2;
P<0.001 vs. before surgery; P<0.001 vs. 3 months after
surgery), respectively. This corresponded to an improvement of 29.3
in the AOFAS value and a reduction of 3.0 points in the VAS from
the mean preoperative scores.
 | Table IIIAOFAS values and VAS scores obtained
from the 34 patients 1 week before and 3 and 6 months after
surgery. |
Table III
AOFAS values and VAS scores obtained
from the 34 patients 1 week before and 3 and 6 months after
surgery.
| Score type | Pre-operation | 3 months after
surgery | 6 months after
surgery |
|---|
| AOFAS | 64.4±4.5 |
89.0±3.8a |
93.7±3.3c,e |
| VAS | 4.5±0.9 |
3.1±0.6b |
1.5±0.4d,f |
Patient self-assessment
The results of the patient self-assessment were also
found to be consistent with the results obtained using the Biodex
system. During the follow-up period, the patients reported that
they recovered living and athletic capacity within 2.7±1.5 and
6.6±3.0 months, respectively, on average. MRI was used to confirm
the abnormal ridge of the posterior calcaneus and the collateral
fluid in the Achilles tendon during the follow-up period (Fig. 4). Most patients reported alleviation
of pain at the final follow-up. Specifically, in terms of pain 15
patients recovered within 3 months, 17 recovered within 4-6 months,
but 2 showed no recovery.
Discussion
A number of studies have previously reported
isokinetic dynamometry to be a reliable procedure for evaluating
ankle joint function (20-22).
Although studies have been performed using isokinetic dynamometry
to evaluate ankle function in patients with other diseases,
including sciatica (23), and
rheumatoid arthritis (24), studies
applying this procedure to assess Haglund's deformity remain
insufficient. In general, torque testing at 60 and 120˚/sec are
associated with strength and power parameters, respectively
(25). In the present study
conducted on patients with Haglund's deformity, the results
revealed no significant differences between the injured and
uninjured sides in terms of dorsiflexion torque at 60 or 120˚/sec.
these findings indicate that this disease does not hinder
dorsiflexion strength but instead affects plantarflexion strength.
Before surgery, the plantarflexion torque at 60 and 120˚/sec varied
significantly between the injured and uninjured sides. At 3 months
after surgery, the plantarflexion torques at 60˚/sec were almost
identical on both sides, suggesting no significant difference.
However, torques at 120˚/sec differed significantly between the two
sides 3 months after surgery. This indicates that although patients
had recovered extensor muscle strength for slower movements, the
ability to adapt to fast movements was not yet recovered within 3
months of surgery. Although their normal day-to-day functions were
restored, difficulties remained in resuming work. The results
showed no statistically significant differences in plantarflexion
torque at 60 or 120˚/sec between the two sides 6 months after
surgery. The strength of the extensors on the injured side was
found to be almost identical compared with that on the uninjured
side, such that the patients could resume normal exercise and work.
The AOFAS values and VAS scores in addition to patient
self-assessment regarding recovery time also exhibited a consistent
trend with the Biodex results during the follow-up period, further
demonstrating the validity of the results obtained using the Biodex
system.
Conventional treatment for Haglund's deformity
involves resting, wearing modified shoes, medical therapy and in
selected cases, surgery (26). Open
surgery is no longer executed due to the trauma it causes and the
relatively high risk of infection (27). Endoscopic surgery is commonly
performed and has been reported to engender notable improvements
with limited complication rates of ankle surgeries (28-30).
Additionally, it also provides an optimal view of the pathological
posterosuperior calcaneal region using small incisions.
Results from the present study also confirmed that
the postoperative care plan was reasonable and effective. The
patients could wear shoes with 2-cm-thick pads 3 weeks after
surgery for 9 weeks, perform some exercises and walk using their
entire weight. After 3 months, the patients reported recovery of
living capacity, where they gradually resumed recreational
activities or special training. Recovery of athletic capacity was
reported after 6 months.
Limitations exist regarding the present study. The
sample size was relatively small and therefore more cases are
required to obtain more representative research findings. The
diagnosis of Haglund's deformity of the Achilles tendon remains
controversial. Recognized diagnostic criteria have yet to be
established, where physicians perform diagnoses subjectively on the
basis of their own judgment. Although the Fowler-Philip angle was
measured as a diagnostic factor, previous studies have revealed
that its correlation with clinical symptoms is low, with the false
negative rate reaching 85-100%. As a result, its accuracy as a
diagnostic and predictive indicator remains poor (31). Additionally, the Fowler-Philip angle
exceeded 75˚ in only three patients in the present study, further
suggesting its unreliability in diagnosing Haglund's deformity.
Pavlov et al (16) considered that the degree of bulging
of the posterior calcaneus is the most important symptom when the
parallel pitch line is used as a measurement index. The degree of
kyphosis of the calcaneus exceeded the parallel pitch line in all
patients in the present study, suggesting that the parallel pitch
line is more reliable for diagnosing Haglund's deformity. MRI can
also clearly show the degree of kyphosis, its relationship with the
Achilles tendon and the swelling of the Achilles tendon. Therefore,
Haglund's deformity was diagnosed comprehensively in the present
study by evaluating the clinical manifestations, X-ray examination
and MRI results.
To conclude, findings from the present study suggest
that using the Biodex system for isokinetic muscle testing can
dynamically reflect the postoperative recovery of patients with
Haglund's deformity after endoscopic calcaneoplasty.
Acknowledgements
The authors would like to thank Dr Zhai Wenbo
(School of Basic Medical Sciences, Peking University; Beijing,
China) for his immense effort and guidance in the statistical
analyses of this study.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YPY and YFA performed the surgical procedures. YXW,
YFA, YPY and BHL designed the study. BHL, NA, YBJ and LLL
contributed to patient data collection and follow-up. BHL, LYT and
XYP analyzed the data and performed the statistical analysis. YXW
is accountable for all aspects of the work. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Peking
University Third Hospital Medical Science Research Ethics Committee
(approval no. IRB00006761-M2018151; Beijing, China). Written
informed consent was obtained from all patients, parents or
guardians of the patients prior to the present study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ögüt T and Yontar NS: Treatment of
hindfoot and ankle pathologies with posterior arthroscopic
techniques. EFORT Open Rev. 2:230–240. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Haglund P: Beitrag zur klinik der
achillessehne. Zeitschr Orthop Chir. 49:49–58. 1928.
|
|
3
|
Wiegerinck JI, Kok AC and van Dijk CN:
Surgical treatment of chronic retrocalcaneal bursitis. Arthroscopy.
28:283–293. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ortmann FW and McBryde AM: Endoscopic bony
and soft-tissue decompression of the retrocalcaneal space for the
treatment of Haglund deformity and retrocalcaneal bursitis. Foot
Ankle Int. 28:149–153. 2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mochizuki Y, Saito Y, Tsujikawa T,
Fujiyama Y and Andoh A: Combination of endoscopic submucosal
dissection and chemoradiation therapy for superficial esophageal
squamous cell carcinoma with submucosal invasion. Exp Ther Med.
2:1065–1068. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhou XN, Li B, Wang JS and Bai LH:
Surgical treatment of popliteal cyst: A systematic review and
meta-analysis. J Orthop Surg Res. 11(22)2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Vega J, Baduell A, Malagelada F,
Allmendinger J and Dalmau-Pastor M: Endoscopic achilles tendon
augmentation with suture anchors after calcaneal exostectomy in
haglund syndrome. Foot Ankle Int. 39:551–559. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Uzümcügil O, Doğan A, Yalçinkaya M,
Mumcuoğlu E and Kabukçuoğlu Y: The three portal (including
transpatellar tendon portal) versus two portal technique in the
arthroscopic menisectomy procedure for isolated medial
bucket-handle type meniscal tears. Eklem Hastalik Cerrahisi.
21:38–43. 2010.PubMed/NCBI
|
|
9
|
Taylor NA, Sanders RH, Howick EI and
Stanley SN: Static and dynamic assessment of the biodex
dynamometer. Eur J Appl Physiol Occup Physiol. 62:180–188.
1991.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Papandreou MG, Billis EV, Antonogiannakis
EM and Papaioannou NA: Effect of cross exercise on quadriceps
acceleration reaction time and subjective scores (Lysholm
questionnaire) following anterior cruciate ligament reconstruction.
J Orthop Surg Res. 4(2)2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Müller M, Disch AC, Zabel N, Haas NP and
Schaser KD: Initial intramuscular perfusion pressure predicts early
skeletal muscle function following isolated tibial fractures. J
Orthop Surg Res. 3(14)2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sung E and Kim J: Relationship between
ankle range of motion and biodex balance system in females and
males. J Exerc Rehabil. 14:133–137. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kitaoka HB, Alexander IJ, Adelaar RS,
Nunley JA, Myerson MS and Sanders M: Clinical rating systems for
the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle
Int. 15:349–353. 1994.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hayes MH and Patterson DG: Experimental
development of the graphic rating method. Psychol Bull. 18:98–99.
1921.
|
|
15
|
Fowler A and Phillip J: Abnormality of the
calcaneus as acause of painful heel: Its diagnosis and operative
treatment. Br J Surg. 132:494–498. 1945.
|
|
16
|
Pavlov H, Heneghan MA, Hersh A, Goldman AB
and Vigorita V: The Haglund syndrome: Initial and differential
diagnosis. Radiology. 144:83–88. 1982.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chauveaux D, Liet P, Le Huec JC and Midy
D: A new radiologic measurement for the diagnosis of Haglund's
deformity. Surg Radiol Anat. 13:39–44. 1991.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tourné Y, Baray AL, Barthélémy R and
Moroney P: Contribution of a new radiologic calcaneal measurement
to the treatment decision tree in Haglund syndrome. Orthop
Traumatol Surg Res. 104:1215–1219. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lu CC, Cheng YM, Fu YC, Tien YC, Chen SK
and Huang PJ: Angle analysis of Haglund syndrome and its
relationship with osseous variations and Achilles tendon
calcification. Foot Ankle Int. 28:181–185. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ryan ED, Beck TW, Herda TJ, Hull HR,
Hartman MJ, Costa PB, Defreitas JM, Stout JR and Cramer JT: The
time course of musculotendinous stiffness responses following
different durations of passive stretching. J Orthop Sports Phys
Ther. 38:632–639. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Harbo T, Brincks J and Andersen H: Maximal
isokinetic and isometric muscle strength of major muscle groups
related to age, body mass, height, and sex in 178 healthy subjects.
Eur J Appl Physiol. 112:267–275. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
de Araujo Ribeiro Alvares JB, Rodrigues R,
de Azevedo Franke R, da Silva BG, Pinto RS, Vaz MA and Baroni BM:
Inter-machine reliability of the biodex and cybex isokinetic
dynamometers for knee flexor/extensor isometric, concentric and
eccentric tests. Phys Ther Sport. 16:59–65. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ustun N, Erol O, Ozcakar L, Ceceli E,
Ciner OA and Yorgancioglu ZR: Association with isokinetic ankle
strength measurements and normal clinical muscle testing in
sciatica patients. J Back Musculoskelet Rehabil. 26:361–365.
2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Oliveira SC, Oliveira LM, Jones A and
Natour J: Isokinetic assessment of ankles in patients with
rheumatoid arthritis. Rev Bras Reumatol. 55:318–324.
2015.PubMed/NCBI View Article : Google Scholar : (In Portuguese).
|
|
25
|
Dervin GF, Taylor DE and Keene GC: Effects
of cold and compression dressings on early postoperative outcomes
for the arthroscopic anterior cruciate ligament reconstruction
patient. J Orthop Sports Phys Ther. 27:403–406. 1998.PubMed/NCBI View Article : Google Scholar
|
|
26
|
di Chio F, Cecere A, Troiano M, Mardighian
A, Parisi S and Guglielmi G: Persistent Haglund's disease after
conventional treatments: The innovative role of radiotherapy. BJR
Case Rep. 2(20150272)2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Appala RS, Rajasekhara RG, Vijayabhushanam
M, Venkateswara RM and Anil B: Comparision of open versus
endoscopic calcaneoplasty for haglunds deformity: A short term
analysis. J Evol Med Dent Sci. 4:1950–1954. 2015.
|
|
28
|
Bostick GP, Jomha NM, Suchak AA and
Beaupre LA: Factors associated with calf muscle endurance recovery
1 year after achilles tendon rupture repair. J Orthop Sports Phys
Ther. 40:345–351. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Boffeli TJ and Peterson MC: The Keck and
Kelly wedge calcaneal osteotomy for Haglund's deformity: A
technique for reproducible results. J Foot Ankle Surg. 51:398–401.
2012.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ahn JH, Ahn CY, Byun CH and Kim YC:
Operative treatment of Haglund syndrome with central achilles
tendon-splitting approach. J Foot Ankle Surg. 54:1053–1056.
2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sella EJ, Caminear DS and McLarney EA:
Haglund's syndrome. J Foot Ankle Surg. 37:110–114; discussion 173.
1998.PubMed/NCBI View Article : Google Scholar
|