Introduction
Cerebrovascular diseases are characterized by
systemic vascular disease and neuronal apoptosis (1-3).
Cardiovascular diseases are the most common cause of death in the
adult population in economically developed countries, accounting
for ~33% of deaths in 2017(4).
Cerebral infarction is a type of severe cerebrovascular disease,
which often occurs due to brain hypoxic-ischemic necrosis, and
leads to embolism and thrombosis (5,6). A
previous study found that endothelial cells promote survival,
proliferation and neuronal differentiation of transplanted adult
ischemia-induced neural stem/progenitor cells after cerebral
infarction (7). Maintaining
endothelial function and circulating endothelial progenitor cells
(EPCs) is associated with a functional recovery for patients with
cerebral infarctions (8). Therefore,
understanding the molecular mechanisms of action behind cerebral
infarction injuries to EPCs is essential for the prevention and
treatment of cerebrovascular disease.
Prazosin
(C19H21N5O4·HCl) is a
α-1 adrenergic receptor blocker which prevents the binding of
postsynaptic adrenaline. Postsynaptic adrenaline plays an essential
role in the progression of coronary artery diseases (9). Prazosin is widely used for treating
mild and moderate hypertension (10). The long-term effects of prazosin
showed protective effects on blood pressure, heart, carotid artery
and acetylcholine in young Wistar rats (11). Furthermore, prazosin treatment causes
enduring vulnerability to the transient reinstatement of hemiplegia
after traumatic brain injury (12).
A previous study demonstrated that nuclear filament
(NF)-κB plays an important role in cerebral ischemia (13). In addition, a previous report
indicated that inhibition of apoptosis and inflammation contributes
to the recovery folliwng cerebral ischemia/reperfusion injury
(14). Expression of Akt is
correlated with the expression of apoptosis-related molecules
caspase-3 and p38 in acute cerebral ischemia (15). These findings suggest that EPC
mobilization following traumatic brain injury may take a different
course compared to that associated with body or vascular injuries
(16). Activating the Akt signaling
pathway can protect rats against cerebral ischemia/reperfusion
injury in rat hippocampal neurons (17). This also indicates that the
Akt-mediated JNK3/caspase-3 signaling pathway protects rat
hippocampal neurons against cerebral ischemia/reperfusion injury in
the CA1 region (18). Therefore, the
present study hypothesized that prazosin may regulate cerebral
ischemia injury through targeting the Akt/NF-κB signaling
pathway.
In the present study, the therapeutic efficacy of
prazosin in a rat cerebral infarction model was analyzed. The
present study investigated the association between prazosin and the
Akt/NF-κB signal pathway in EPCs in rats with cerebral ischemia
injury. The ameliorative effects of prazosin on the cerebral
infarct volume, brain water content, cerebral edema, neurological
deficits, inflammatory response and EPC apoptosis were also
evaluated, which aimed to uncover the potential mechanisms of
action of prazosin for the treatment of cerebral infarction in
vitro and in vivo.
Materials and methods
Animal study
The protocols used in the present study were
approved by the Animals Committee of Affiliated Hospital of North
Sichuan Medical College (Nanchong City, China). A total of 30 male
SD rats (8 weeks old, 320-340 g body weight) were purchased from
Chongqing Medical University. All rats were maintained at 22±2˚C,
50-60% relative humidity and a 12 h light/dark cycle with free
access to diet and water. The cerebral ischemia injury model was
developed in these rats as described previously (19). Briefly, cerebral ischemia in the area
perfused by the middle cerebral artery was induced using an
incision in the midline of the neck, where the right carotid
bifurcation was observed. Rats were anesthetized using sodium
pentobarbital [intraperitoneal (IP), 40 mg/kg]. The internal
carotid artery was identified, ligated and then occluded, and the
branches of the external carotid artery were dissected and divided.
A 4-0 nylon suture with a silicone-coated tip was then advanced
from the external carotid artery into the lumen of the internal
carotid artery until it blocked the origin of the middle cerebral
artery. Reperfusion was accomplished and rats underwent ischemia
for 1 h and reperfusion for 4 h. The sham-operated animals were
synchronously intragastrically administrated with equal volume of
normal saline. Rat model was established and randomized into three
groups: Vehicle, prazosin and sham (n=10 per group). The animals
received prazosin (1 mg/kg; Sigma-Aldrich; Merck KGaA) treatment
once every day or the same volume of PBS by IP injection. The
treatment continued for 30 days.
The modified neurological severity
scores (mNSS) test
Neurological deficits were analyzed using the mNSS
test in the prazosin and PBS group on day 30 (n=4) as previously
reported (20). The mNSS test was
scored on a 5-point scale: 0, no neurological deficits; 1, failure
to extend right forepaw fully; 2, circling to the right; 3, falling
to the right; 4, inability to walk spontaneously combined with
depressed levels of consciousness.
Infarct volume analysis
On day 30, after IP injection of pentobarbital (40
mg/kg) for anesthesia, the brains were dissected and collected.
Brain tissues were sliced into 1.0-mm-thick coronal sections and
then frozen for 30 min at -80˚C. The tissue sections were incubated
with 1% 2,3,5-triphenyl tetrazolium chloride (Sigma-Aldrich; KGaA)
for 15 min at 25˚C and fixed in 4% paraformaldehyde for 12 h at
4˚C. The infarct region lacks staining and appears white, whereas
the normal non-infarct tissue appears red (14). The stained coronal slices were imaged
using a fluorescent microscope (x200 magnification), and the
infarction was analyzed using Image J V4.6 (National Institutes of
Health). The percentage of infarct volume was measured as follows:
(The total infarct volume of the ipsilateral structure/total volume
of the contralateral structure) x100%.
Brain water content
Brains were carefully dissected and cut alongside
the sagittal plane and the wet weight was measured. The hemispheres
were dried for 24 h at 90˚C to determine the dry weight. Based on
gravimetrical differences, water content was measured using the
following calculation: Brain water content (%)=[(wet weight-dry
weight)/wet weight] x100.
Cells cultures
EPCs were isolated from the middle cerebral artery
in experimental rats (the sham group) and cultured in DMEM
(Invitrogen; Thermo Fisher Scientific, Inc.) medium with 10% fetal
bovine serum (Invitrogen; Thermo Fisher Scientific, Inc.) and
incubated overnight at 37˚C in a humidified atmosphere of 5%
CO2. EPCs were treated with 5 mg/ml prazosin
(Sigma-Aldrich; Merck KGaA) and/or Akt inhibitor (AktIR; 1 mg/ml;
cat. no. ab14088; Abcam) and/or NF-κB inhibitor (NF-κBIR; 1 mg/ml;
cat. no. ab141588; Abcam) for 24 h at 37˚C to analyze the
therapeutic effects of prazosin.
Reverse transcription-quantitative PCR
(RT-qPCR) analysis
Total RNA was obtained from EPCs using the RNAeasy
Mini kit (QIAGEN, Inc.). RNA was reverse transcribed to cDNA using
a reverse transcription kit (cat. no. AB4106C) with β-actin
expression as an endogenous control (Invitrogen; Thermo Fisher
Scientific, Inc.). The RT temperature protocol was as follows: 37˚C
for 1 h and then 85˚C for 5 min to terminate the reaction. Gene
expression levels of Bcl-w, Bcl-2, Bax, Bad, interleukin (IL)-1 and
tumor necrosis factor (TNF)-α in cells were measured on the iCycler
thermal cycler (Bio-Rad Laboratories, Inc.) using iQ SYBR Green
Supermix (Bio-Rad Laboratories, Inc.). The following thermocycling
conditions were used for the qPCR: Initial denaturation for 10 min
at 94˚C; 40 cycles of denaturation for 10 sec at 95˚C, annealing
for 20 sec at 56-62˚C, extension for 10 sec at 72˚C; and melt curve
analysis at 0.5˚C for 6 sec. All the forward and reverse primers
were synthesized by Invitrogen; Thermo Fisher Scientific, Inc.
(Table I). Relative mRNA expression
level changes were calculated using the 2-ΔΔCq method
(21). The results are expressed as
the n-fold expression levels, normalized to β-actin expression.
 | Table IPrimers for reverse
transcription-quantitative PCR. |
Table I
Primers for reverse
transcription-quantitative PCR.
| Gene | Forward
(5'-3') | Reverse
(5'-3') |
|---|
| TNF-α |
CCAGACCCTCACACTCAGATCA |
TCCGCTTGGTGGTTTGCTA |
| IL-1β |
GGCTGCTTCCAAACCTTTGA |
GAAGACACGGATTCCATGGT |
| Bcl-w |
GCTGGTGGTTGACTTTCTCTCC |
GGCTTCAGTCCTGTTCTCTTCG |
| Bcl-2 |
GATGAAGTACATCCATTATAAGCTGTCACA |
GCGCTCAGCCCTGTGCCACCTGTGGTCCAC |
| Bad |
GGAGCATCGTTCAGCAGCAG |
CCATCCCTTCATCTTCCTCAGTC |
| Bax |
CTTCAGGGTTTCATCCAG |
CTCCATGTTACTGTCCAG |
| β-actin |
CGGAGTCAACGGATTTGGTC |
AGCCTTCTCCATGGTCGTGA |
Overexpression of Akt or NF-κB
Expression plasmids pRK5-Akt and pRK5-NF-κB, with a
Flag tag at the C-terminus, were constructed by Invitrogen; Thermo
Fisher Scientific, Inc. EPCs (1x105) were seeded on
six-well plates (Corning, Inc.) and transiently transfected with
pRK5-Akt, pRK5-NF-κB or pRK5-vector by electrotransfection using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.) according to the manufacturer's protocol. After
72 h of transfection, mRNA expression levels of Akt and NF-κB were
analyzed. Cells were then treated with 5 mg/ml prazosin for 24 h at
37˚C for further analysis.
Activity of AKT and NF-κB
TransFactor AKT kit (cat. no. 611437; BD
Biosciences) and NF-κB TransFactor NF-κB kit (cat. no. 565446; BD
Biosciences) were used to detect relative AKT and NF-κB activity in
the treated EPCs, respectively, according to the manufacturer's
instructions. Subsequently, the activity of AKT and NF-κB was
analyzed as previously described (22,23).
Optical density was measured at 405 nm using a microplate
reader.
Western blot analysis
EPCs were isolated from experimental rats as
previously described (24) and
homogenized using RIPA Lysis Buffer (Thermo Fisher Scientific,
Inc.). Protein concentrations were measured using a BCA protein
assay kit (Thermo Fisher Scientific, Inc.). Subsequently, protein
samples (40 µg) were loaded and separated using 12% SDS-PAGE.
Protein were subsequently blotted on a nitrocellulose membrane and
labelled using the following rabbit anti-rat primary antibodies at
4˚C overnight: Akt (1:2,000; cat. no. ab185633; Abcam),
phosphorylated (p)Akt (1:2,000; cat. no. ab133458; Abcam), NF-κB
(1:1,000; cat. no. ab207297; Abcam), pNF-κB (1:1,000; cat. no.
ab222494; Abcam) and β-actin (1:1,000; Cell Signaling Technology,
Inc.) were added after blocking with 5% BSA for 1 h at 37˚C. The
membranes were then incubated with horse radish
peroxidase-conjugated goat anti-rabbit IgG mAb (1:5,000; cat. no.
PV-6001; OriGene Technologies, Inc.) at room temperature for 1 h.
Protein bands were detected using an ECL detection system and the
band intensities were analyzed using ImageJ software version 8.0
(National Institutes of Health).
TUNEL assay
EPCs were prepared and fixed with 10%
paraformaldehyde for 10 min at room temperature. Apoptosis of EPCs
as analyzed using TUNEL assays (DeadEnd™ Colorimetric Tunel System;
Promega Corporation) according to the manufacturer's instructions.
EPCs (1x105) were incubated TUNEL solution at 37˚C for 1
h. Cells were washed with PBS three times for 5 min at 37˚C
followed by incubated with 5% DAPI (Sigma-Aldrich; Merck KGaA) for
15 min at 37˚C in a dark wet box. Finally, images in three fields
were captured using a ZEISS LSM 510 confocal microscope at 488 nm.
The apoptosis rate was calculated using Developer XD 1.2 (Definiens
AG).
Statistical analysis
All data are reported as the mean and the SD. The
mNSS test was analyzed using a Kruskal-Wallis test with post hoc
Dunn's tests for multiple comparisons. Statistical significances
between two groups were analyzed using Student's t-tests. Other
multiple groups were analyzed using one-way ANOVAs followed by
Tukey's test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Prazosin alleviates infarct volume and
improves neurological deficits in cerebral ischemia injury rat
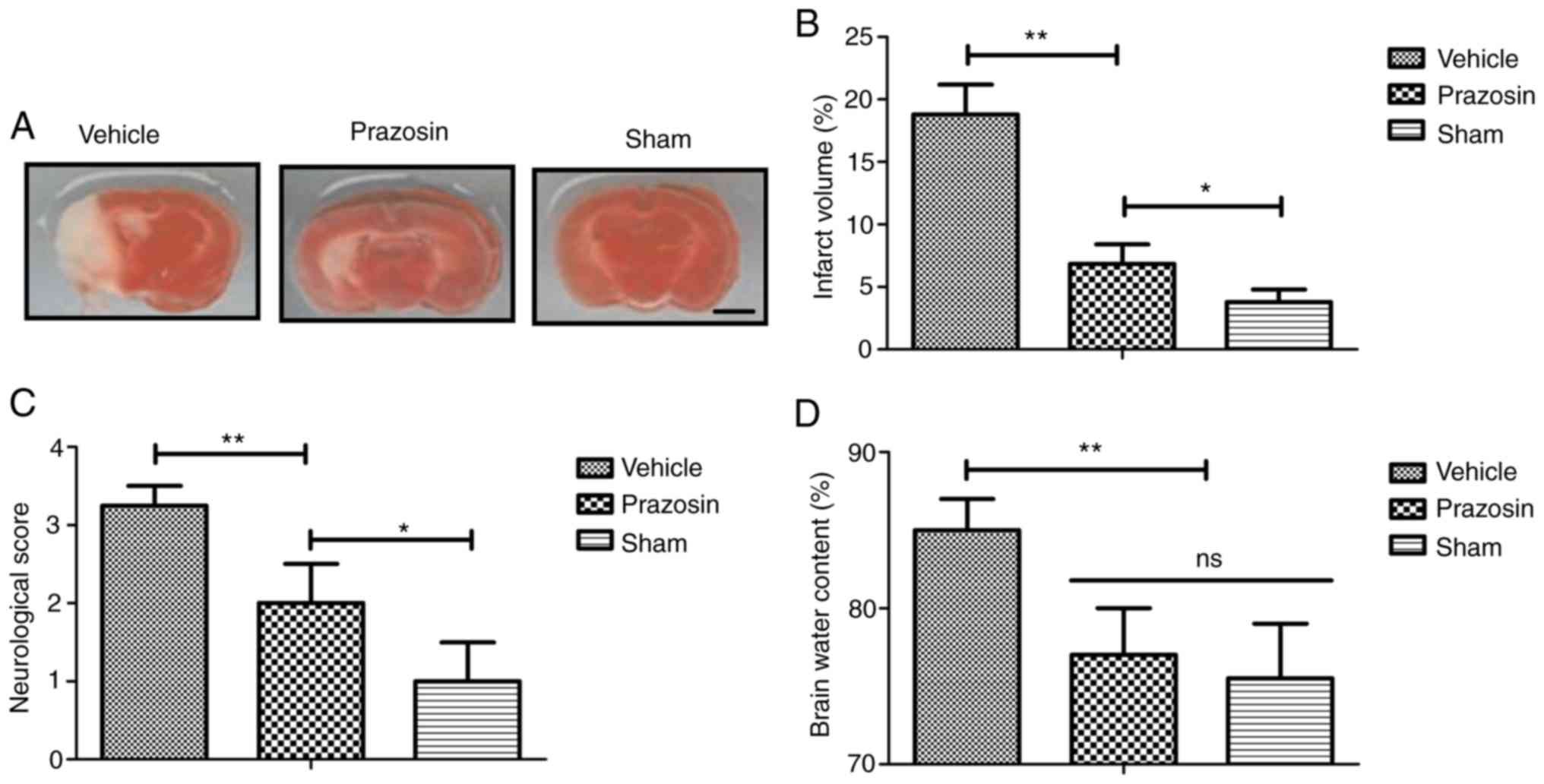
Infarct volume and functional recovery were analyzed
in experimental rats with myocardial ischemia after treatment with
prazosin. The results showed that the infarct volume was markedly
decreased following prazosin treatment compared to the vehicle
determined by the infarct volume analysis (Fig. 1A-B). Prazosin was found to improve
the neurological deficits, as determined by the mNSS test (Fig. 1C). Treatment of prazosin also
decreased brain water content compared to the vehicle group, as
determined by the brain water content assay (Fig. 1D). These results suggested that
prazosin may attenuate ischemia-induced brain injury.
Prazosin treatment inhibits apoptosis
of EPCs in vitro
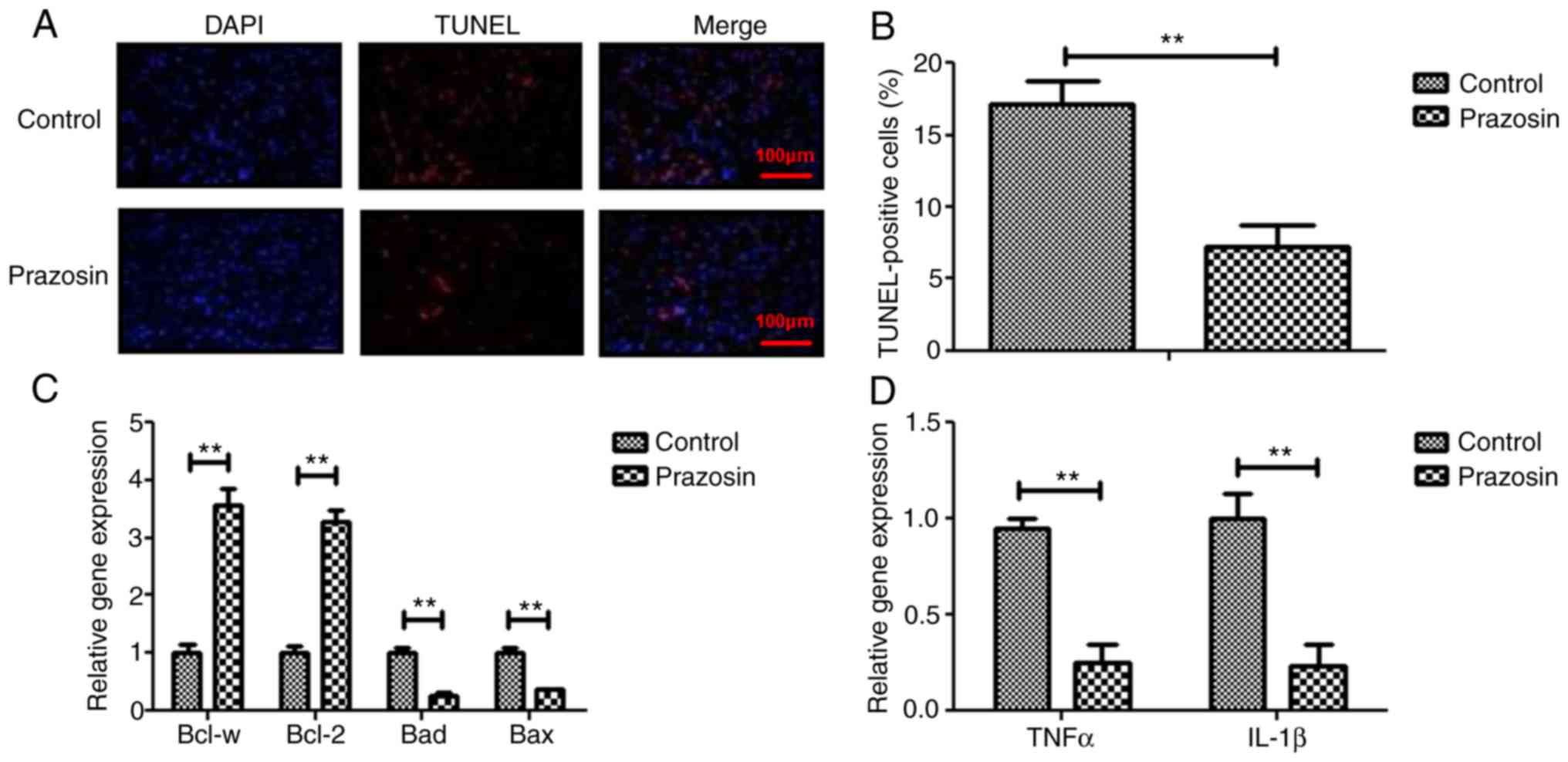
The anti-apoptotic effects of prazosin were
investigated in EPCs. The results demonstrated that prazosin
treatment decreased the numbers of apoptotic EPCs induced by TNF-α
(Fig. 2A). The number of
TUNEL-positive EPCs was higher in the control group compared with
the prazosin group (Fig. 2B).
RT-qPCR showed that the gene expression levels of the
anti-apoptotic genes, Bcl-w and Bcl-2, were upregulated in EPCs
compared to the control (Fig. 2C).
The expression levels of pro-apoptotic genes, Bad and Bax, were
downregulated in myocardial cells compared to that of the controls
(Fig. 2C). Prazosin was also found
to downregulate TNF-α and IL-1β gene expression levels in EPCs
(Fig. 2D). These results suggested
that prazosin treatment may inhibit apoptosis and inflammation in
EPCs in vitro.
Prazosin treatment decreases apoptosis
and inflammatory factors in vivo
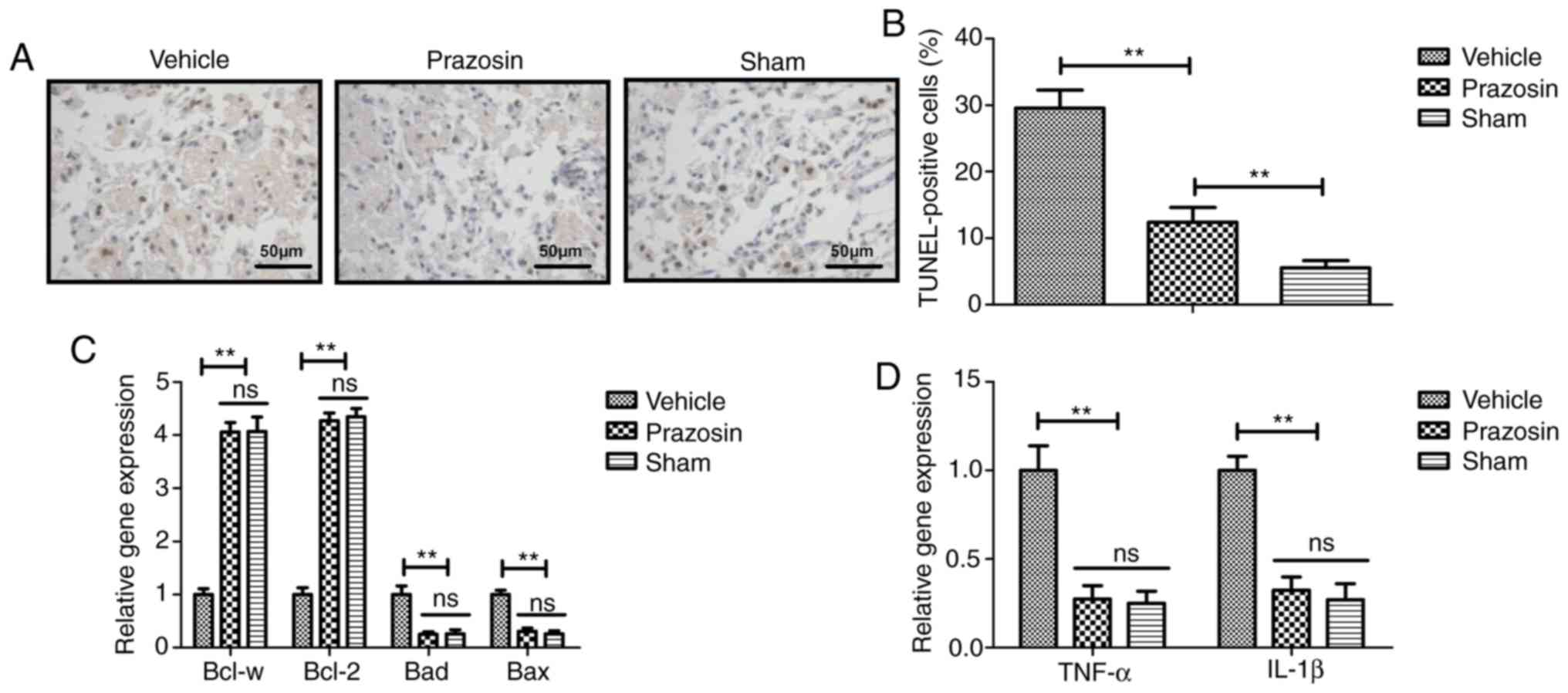
TUNEL assays showed that the number of apoptotic
EPCs significantly increased in the cerebral ischemia injury rats
compared to the vehicle controls (Fig.
3A-B). Prazosin treatment decreased the expression levels of
pro-apoptotic genes, Bad and Bax, and increased Bcl-w and Bcl-2
gene expression levels in EPCs compared to the vehicle group
(Fig. 3C). Gene expression levels of
TNF-α and IL-1 in EPCs were also decreased by prazosin treatment
compared to the vehicle (Fig. 3D).
These results suggested that prazosin treatment can decrease
apoptosis and the expression of inflammatory factors in
vivo.
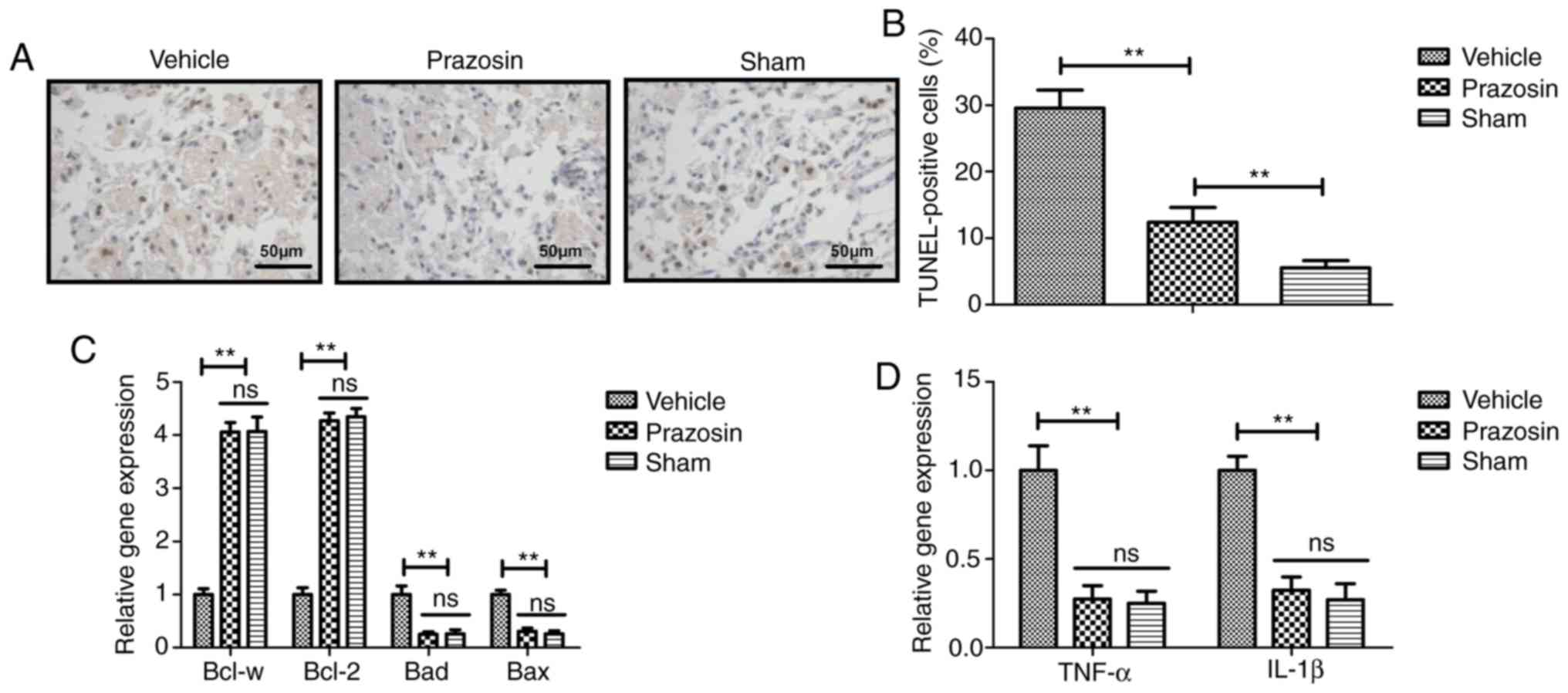 | Figure 3Effects of prazosin treatment on
apoptosis and inflammatory factors in EPCs in vivo. (A)
Representative images of apoptosis of EPCs in the cerebral ischemia
injury rats in the vehicle, prazosin and sham groups. (B)
Quantification of EPC apoptosis in the vehicle, prazosin and sham
groups. (C) Gene expression levels of Bad, Bax, Bcl-w and Bcl-2
gene expression in EPCs in the vehicle, prazosin and sham groups.
(D) Gene expression levels of TNF-α and IL-1 in EPCs in vehicle,
prazosin and sham groups. **P<0.01. EPC, endothelial
progenitor cell; IL, interleukin; ns, not significant; TNF, tumor
necrosis factor. |
Prazosin inhibits Akt/NF-κB signal
pathway and inflammation in vivo
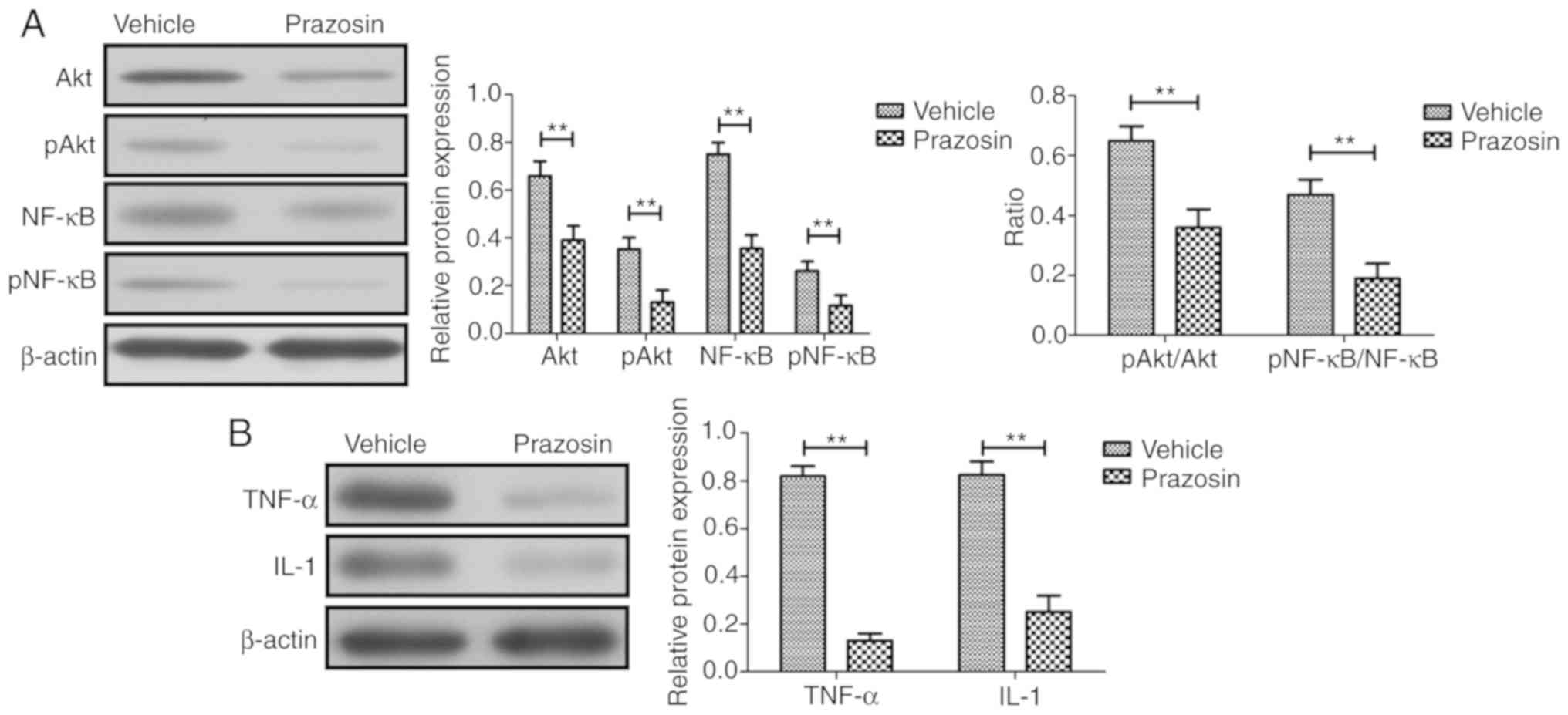
The effect of prazosin on Akt and NF-κB expression
levels was analyzed in the middle cerebral artery in vivo.
As shown in Fig. 4A, prazosin
decreased the expression and phosphorylation levels of Akt and
NF-κB in in middle cerebral artery in experimental rats compared to
that in the PBS-treated rats. Protein expression levels of TNF-α
and IL-1 in the middle cerebral artery were also decreased by
prazosin treatment compared to the vehicle in vivo (Fig. 4B). These data indicated that prazosin
may inhibit the Akt/NF-κB signaling pathway and inflammation in the
middle cerebral artery in vivo.
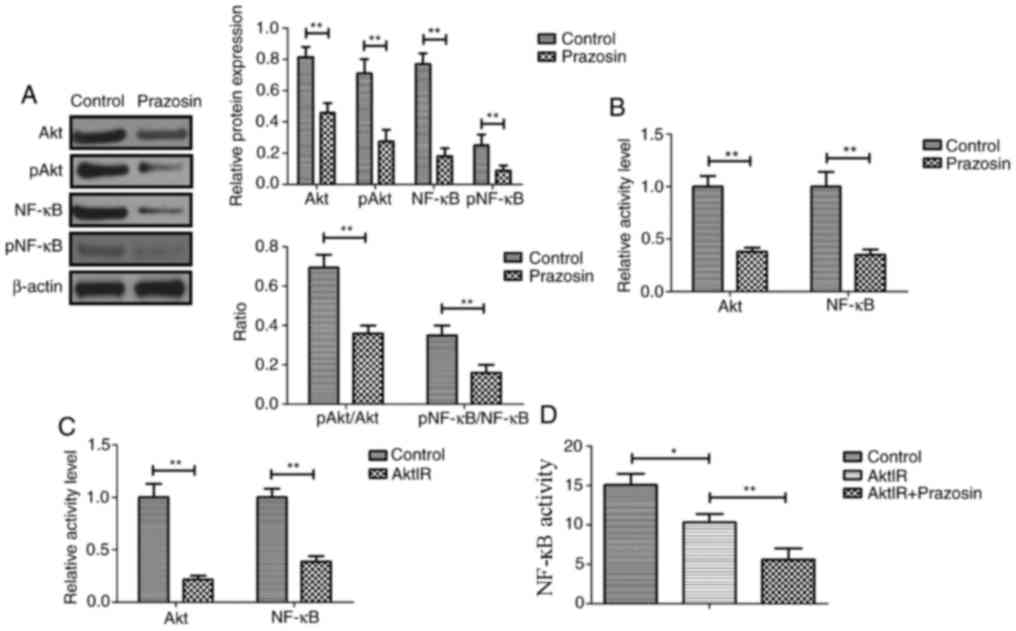
Prazosin inhibits EPC apoptosis
through targeting the Akt/NF-κB signaling pathways
Cells were transiently transfected with pRK5-Akt,
pRK5-NF-κB or pRK5-vector by electrotransfection. Fig. S1 shows that transfection was
successfully performed. The mRNA expression level of Akt and NF-κB
in pRK5-Akt and pRK5-Akt groups were significantly compared with
vector groups, respectively. The potential mechanism of action
mediated by prazosin in EPCs was further analyzed. The expression
and phosphorylation levels of Akt and NF-κB were downregulated by
prazosin treatment in EPCs (Fig.
5A). The results also demonstrated that the ratio of pAkt and
pNF-κB to total AKT and NF-κB, respectively, was decreased by
prazosin treatment in the EPCs (Fig.
5B). AktIR decreased NF-κB activity, while Akt overexpression
(AktOR) increased NF-κB activity (Fig.
5C-D). AktIR increased prazosin-inhibited apoptosis of EPCs,
while AktOR decreased prazosin-inhibited apoptosis of EPCs
(Fig. 5E-F). These results suggested
that prazosin inhibited EPC apoptosis through targeting the
Akt/NF-κB signaling pathway.
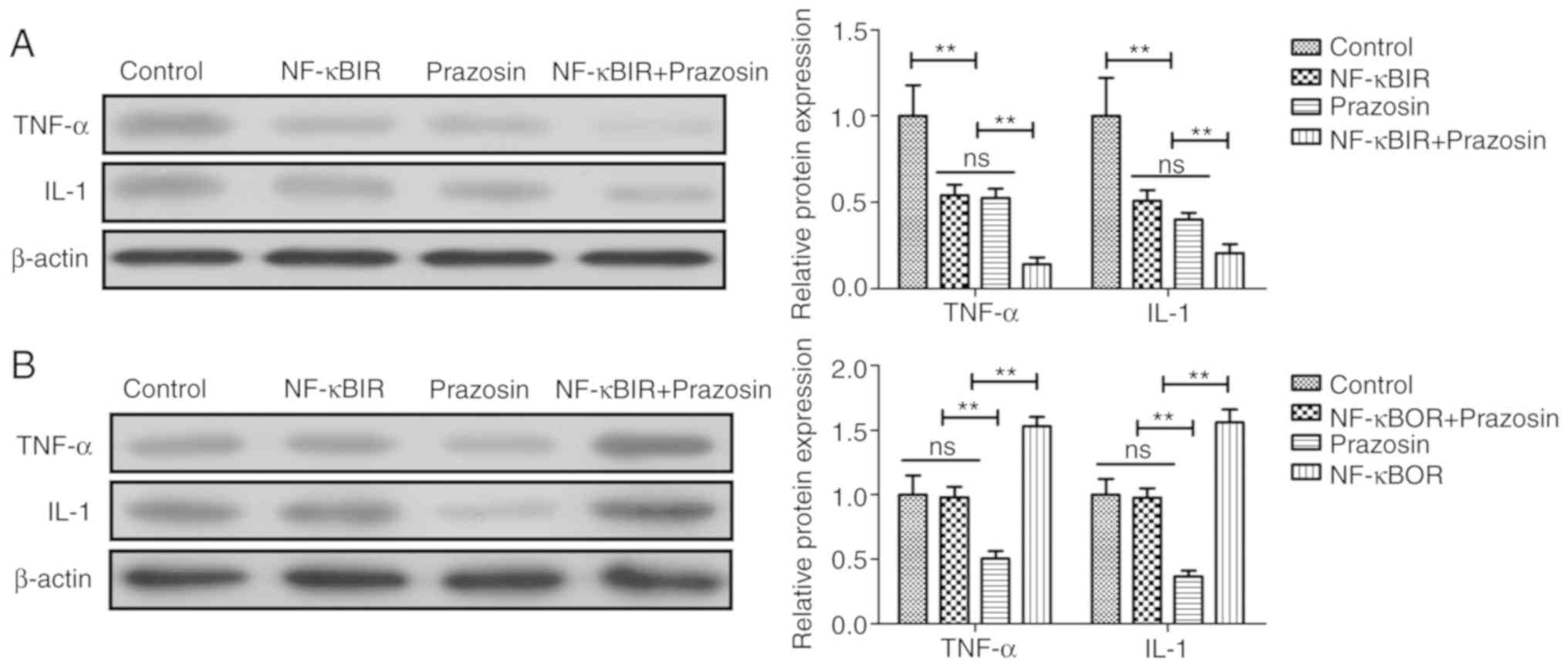
Prazosin inhibits inflammation in EPCs
through targeting the NF-κB signaling pathway
Finally, the relationship between the inhibition of
inflammatory cytokine production and NF-κB production in EPCs was
investigated. As shown in Fig. 6A,
NF-κBIR decreased TNF-α and IL-1 in EPCs and NF-κBIR increased
prazosin-inhibited TNF-α and IL-1 expression levels in EPCs. NF-κB
overexpression (NF-κBOP) increased TNF-α and IL-1 expression levels
in EPCs, and prazosin was able to prevent the NF-κBOP mediated
increase in the expression levels of these proteins (Fig. 6B). These data suggested that prazosin
inhibited inflammation in EPCs through targeting the NF-κB
signaling pathway.
Discussion
Currently, ischemia-induced brain injury presents an
extremely high mortality rate worldwide, that closely associates
with metabolic disorders of endogenous substances, such as
acetylcholine and histamine (25-27).
Prazosin can protect myocardial cells against anoxia-reoxygenation
injury through the extracellular signal-regulated kinase signaling
pathway (28). However, the role of
prazosin in EPCs has not reported previously. In the present study,
the ameliorative effects of prazosin were investigated in a rat
cerebral infarction model. The present study found that prazosin
decreased infarct volume, brain water content and attenuated
neurological deficits in ischemia-induced brain injury. These
findings indicated that prazosin inhibited apoptosis of EPCs
through targeting the Akt/NF-κB signal pathway in EPCs.
Inflammation plays an essential role in the
occurrence and development of cerebral infarction (29). A previous study reported that the
levels of TNF-α in the serum is associated with the severity of
acute cerebral infarctions (30). It
has also been found that IL-1β expression is upregulated in the
brain tissue and sera of focal cerebral ischemia/reperfusion injury
model rats (31). The present study
found that prazosin decreased TNF-α and IL-1β gene expression
levels in EPCs, and also reduced serum levels of TNF-α and IL-1β in
the rat cerebral infarction model. Administration of prazosin also
decreased the brain water content and reduced neurological deficits
in the cerebral infarction rat model compared to the control group,
which suggested that prazosin may be a potential drug for the
treatment of cerebral infarction.
Inhibition of apoptosis and proliferation of EPCs
may repair the blood-brain barrier and improve the cognitive
function of amyloid precursor protein/presenilin 1 in transgenic
Alzheimer's disease mice following the development of cerebral
infarction (32). To the best of our
knowledge, this is the first study which has analyzed the
anti-apoptotic effects of prazosin in EPCs both in vitro and
in vivo. Prazosin treatment was found to decrease the
pro-apoptotic gene expression levels of Bad and Bax, and increase
Bcl-w and Bcl-2 gene expression levels in EPCs both in vitro
and in vivo. Previously, it has been indicated that EPCs and
neural progenitor cells synergistically protect cerebral
endothelial cells from hypoxia/reoxygenation-induced injury through
activating the Akt pathway (33).
Notably, inhibition of NF-κB activation decreases TNF-α-induced
inflammation and atherosclerotic activity in EPCs (34). Mechanistically, prazosin inhibited
the Akt signaling cascade, which prevented the apoptosis of EPCs.
The results demonstrated the protective effects of prazosin through
inhibition of apoptosis mediated by the Akt/NF-κB signaling pathway
in animals with cerebral infarctions.
In conclusion, the present study indicated that
prazosin protects EPCs against apoptosis by downregulating the
activity of the Akt/NF-κB signaling pathway in the rat cerebral
infarction model. The present findings provided evidence of the
anti-apoptotic efficacy of prazosin in the progression of cerebral
infarction, which illustrated a possible mechanistic pathway for
the treatment of ischemia-induced brain injury.
Supplementary Material
mRNA expression levels after
transfection with expression plasmid pRK5-Akt or pRK5-NF-κB in EPCs
after 72 h of transfection. (A) Akt mRNA expression levels in EPCs
after transfection with expression plasmid pRK5-Akt. (B) NF.κB mRNA
expression levels in EPCs after transfection with expression
plasmid pRK5-Akt. **P<0.01. EPC, endothelial
progenitor cell; NF, nuclear filament; p, phosphorylated.
Acknowledgements
Not applicable.
Funding
This study was supported by the Chongqing Science
and Health Joint Medical Research Project (grant no. 2019QNXM014)
and Yongchuan District Jointly Funded Science and Technology
Project (grant no. 2019nb0206).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SL and WL were responsible for guaranteeing
integrity of the entire study, study concepts and design,
definition of intellectual content, literature research,
experimental studies, data acquisition, manuscript preparation and
editing and review. WL was responsible for the experimental studies
and manuscript editing. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethical Committees of
Affiliated Hospital of North Sichuan Medical College.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lammy S, Fivey P and Sangra M:
Decompressive craniectomy for malignant middle cerebral artery
infarction in a 16-year old boy: A case report. J Med Case Rep.
10(368)2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mijiti M, Mijiti P, Axier A, Amuti M,
Guohua Z, Xiaojiang C, Kadeer K, Xixian W, Geng D and Maimaitili A:
Incidence and predictors of angiographic vasospasm, symptomatic
vasospasm and cerebral infarction in Chinese patients with
aneurysmal subarachnoid hemorrhage. PLoS One.
11(e0168657)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tai MS, Viswanathan S, Rahmat K, Nor HM,
Kadir KAA, Goh KJ, Ramli N, Bakar FKA, Zain NRM, Yap JF, et al:
Cerebral infarction pattern in tuberculous meningitis. Sci Rep.
6(38802)2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zang RS, Zhang H, Xu Y, Zhang SM, Liu X,
Wang J, Gao YZ, Shu M, Mei B and Li HG: Serum C-reactive protein,
fibrinogen and D-dimer in patients with progressive cerebral
infarction. Transl Neurosci. 7:84–88. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Xiu J, Chen G, Zheng H, Wang Y, Chen H,
Liu X, Wu J and Bin J: Comparing treatment outcomes of fractional
flow reserve-guided and angiography-guided percutaneous coronary
intervention in patients with multi-vessel coronary artery
diseases: A systematic review and meta-analysis. Clin Invest Med.
39:E25–E36. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Su C, Liao LZ, Song Y, Xu ZW and Mei WY:
The role of red blood cell distribution width in mortality and
cardiovascular risk among patients with coronary artery diseases: A
systematic review and meta-analysis. J Thorac Dis. 6:1429–1440.
2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Nakagomi N, Nakagomi T, Kubo S, Nakano-Doi
A, Saino O, Takata M, Yoshikawa H, Stern DM, Matsuyama T and
Taguchi A: Endothelial cells support survival, proliferation, and
neuronal differentiation of transplanted adult ischemia-induced
neural stem/progenitor cells after cerebral infarction. Stem Cells.
27:2185–2195. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Lee S, Kim W, Park J, Jang HH, Lee SM, Woo
JS, Kim HS, Lee KH, Kwon YJ, Lee U, et al: Effects of
electroacupuncture on endothelial function and circulating
endothelial progenitor cells in patients with cerebral infarction.
Clin Exp Pharmacol Physiol. 42:822–827. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Al-Asmari AK, Al-Seif AA, Hassen MA and
Abdulmaksood NA: Role of prazosin on cardiovascular manifestations
and pulmonary edema following severe scorpion stings in Saudi
Arabia. Saudi Medical J. 29:299–302. 2008.PubMed/NCBI
|
|
10
|
Hanon O, Giacomino A, Troy S, Bernaud C,
Girerd X and Weber S: Efficacy of and tolerance to prolonged
release prazosin in patients with hypertension and non-insulin
dependent diabetes. Ann Cardiol Angeiol (Paris). 49:390–396.
2000.PubMed/NCBI(In French).
|
|
11
|
Kristek F, Malekova M and Cacanyiova S:
Long-term effect of prazosin and losartan administration on blood
pressure, heart, carotid artery, and acetylcholine induced dilation
of cardiovascular system of young Wistar rats and SHR. Gen Physiol
Biophys. 32:235–243. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Stibick DL and Feeney DM: Enduring
vulnerability to transient reinstatement of hemiplegia by prazosin
after traumatic brain injury. J Neurotrauma. 18:303–312.
2001.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang Y, Li L, Deng S, Liu F and He Z:
Ursolic acid ameliorates inflammation in cerebral ischemia and
reperfusion injury possibly via high mobility group Box 1/Toll-like
receptor 4/NFkB pathway. Front Neurol. 9(253)2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Li M, Peng J, Song Y, Liang H, Mei Y and
Fang Y: Electro-acupuncture combined with transcranial magnetic
stimulation improves learning and memory function of rats with
cerebral infarction by inhibiting neuron cell apoptosis. J Huazhong
Univ Sci Technology Med Sci. 32:746–749. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chang J, Yao X, Zou H, Wang L, Lu Y, Zhang
Q and Zhao H: BDNF/PI3K/Akt and Nogo-A/RhoA/ROCK signaling pathways
contribute to neurorestorative effect of Houshiheisan against
cerebral ischemia injury in rats. J Ethnopharmacol. 194:1032–1042.
2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Liu L, Liu H, Jiao J, Bergeron A, Dong JF
and Zhang J: Changes in circulating human endothelial progenitor
cells after brain injury. J Neurotrauma. 24:936–943.
2007.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jiao S, Zhu H, He P and Teng J: Betulinic
acid protects against cerebral ischemia/reperfusion injury by
activating the PI3K/Akt signaling pathway. Biomed Pharmacother.
84:1533–1537. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zhang M, Yan H, Li S and Yang J:
Rosmarinic acid protects rat hippocampal neurons from cerebral
ischemia/reperfusion injury via the Akt/JNK3/caspase-3 signaling
pathway. Brain Res. 1657:9–15. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kato N, Yanaka K, Hyodo K, Homma K, Nagase
S and Nose T: Stable nitroxide Tempol ameliorates brain injury by
inhibiting lipid peroxidation in a rat model of transient focal
cerebral ischemia. Brain Res. 979:188–193. 2003.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Patel N, Rao VA, Heilman-Espinoza ER, Lai
R, Quesada RA and Flint AC: Simple and reliable determination of
the modified rankin scale score in neurosurgical and neurological
patients: The mRS-9Q. Neurosurgery. 71:971–975; discussion 975.
2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Jia YS, Hu XQ, Gabriella H, Qin LJ and
Meggyeshazi N: Antitumor activity of Tenacissoside H on esophageal
cancer through arresting cell cycle and regulating PI3K/Akt-NF-kB
transduction cascade. Evid Based Complement Alternat Med.
2015(464937)2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zhu G, Song M, Wang H, Zhao G, Yu Z, Yin
Y, Zhao X and Huang L: Young environment reverses the declined
activity of aged rat-derived endothelial progenitor cells:
Involvement of the phosphatidylinositol 3-kinase/Akt signaling
pathway. Ann Vasc Surg. 23:519–534. 2009.PubMed/NCBI View Article : Google Scholar
|
|
24
|
She Q, Xia S, Deng SB, Du JL, Li YQ, He L,
Xiao J and Xiang YL: Angiogenesis in a rat model following
myocardial infarction induced by hypoxic regulation of
VEGF165 gene-transfected EPCs. Mol Med Rep. 6:1281–1287.
2012.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Carloni S, Buonocore G and Balduini W:
Protective role of autophagy in neonatal hypoxia-ischemia induced
brain injury. Neurobiol Dis. 32:329–339. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lee JJ, Li L, Jung HH and Zuo Z:
Postconditioning with isoflurane reduced ischemia-induced brain
injury in rats. Anesthesiology. 108:1055–1062. 2008.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Nishioku T, Takata F, Yamauchi A, Sumi N,
Yamamoto I, Fujino A, Naito M, Tsuruo T, Shuto H and Kataoka Y:
Protective action of indapamide, a thiazide-like diuretic, on
ischemia-induced injury and barrier dysfunction in mouse brain
microvascular endothelial cells. J Pharmacol Sci. 103:323–327.
2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Wang L, Xue Y, Ma H, Shi H, Wang L and Cui
X: Prazosin protects myocardial cells against anoxia-reoxygenation
injury via the extracellular signalregulated kinase signaling
pathway. Mol Med Rep. 17:2145–2152. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Cuenca-López MD, Brea D, Segura T, Galindo
MF, Antón-Martínez D, Agulla J, Castillo J and Jordán J:
Inflammation as a therapeutic agent in cerebral infarction:
Cellular inflammatory response and inflammatory mediators. Rev
Neurol. 50:349–359. 2010.PubMed/NCBI(In Spanish).
|
|
30
|
Lin JZ, Miao KQ, Zhang HX, Kong QZ, Yuan
RM, Wang ZW and Liu SX: Change of early serum TNF-alpha and IL-6
levels in acute cerebral infarction and its significances. Zhejiang
Da Xue Xue Bao Yi Xue Ban. 39:415–418. 2010.PubMed/NCBI(In Chinese).
|
|
31
|
Liu JW, Ren YL, Liu XL, Xia HL, Zhang HL,
Jin SH, Dai QX and Wang JL: Effect of ginsenoside Rb1 on cerebral
infarction volume and IL-1 beta in the brain tissue and sera of
focal cerebral ischemia/reperfusion injury model rats. Zhongguo
Zhong Xi Yi Jie He Za Zhi. 33:1696–1700. 2013.PubMed/NCBI(In Chinese).
|
|
32
|
Zhang S, Zhi Y, Li F, Huang S, Gao H, Han
Z, Ge X, Li D, Chen F, Kong X and Lei P: Transplantation of in
vitro cultured endothelial progenitor cells repairs the blood-brain
barrier and improves cognitive function of APP/PS1 transgenic AD
mice. J Neurol Sci. 387:6–15. 2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wang J and Chen Y, Yang Y, Xiao X, Chen S,
Zhang C, Jacobs B, Zhao B, Bihl J and Chen Y: Endothelial
progenitor cells and neural progenitor cells synergistically
protect cerebral endothelial cells from
Hypoxia/reoxygenation-induced injury via activating the PI3K/Akt
pathway. Mol Brain. 9(12)2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Yang JX, Pan YY, Ge JH, Chen B, Mao W, Qiu
YG and Wang XX: Tanshinone II A Attenuates TNF-α-induced expression
of VCAM-1 and ICAM-1 in endothelial progenitor cells by blocking
activation of NF-kB. Cell Physiol Biochem. 40:195–206.
2016.PubMed/NCBI View Article : Google Scholar
|