Introduction
Ptosis refers to the improper position of the upper
eyelid edge relative to the upper corneoscleral rim not due to
reasons such as poor eyesight and blepharoptosis. Such a situation
in a child at birth or in the first year after birth can be
diagnosed as congenital ptosis, and unilateral ptosis accounts for
64.7-75.0% of all types of ptosis (1-3).
Congenital ptosis can be classified into mild, moderate, or severe
ptosis (4), which is mainly caused
by the following reasons: The upper eyelid cannot lift or is in
partial or complete ptosis due to hypoplasia of levator muscle,
defects of Müller smooth muscle, or nerve defects of upper eyelid
muscle (5,6). Ptosis usually causes partial or
complete pupillary block, and thus results in visual disturbance.
If not corrected in time, it may lead to deprived amblyopia,
seriously degrading visual function (7,8).
There are many clinical treatment methods for
moderate or severe congenital ptosis, and one of the most classic
methods is frontalis muscle suspension (9). It connects the upper eyelid bone to the
frontal muscle using suspension materials to help patients to open
the eyelid with frontal muscle, so as to treat ptosis (10). However, this technology is prone to
bring a high postoperative complication rate and recurrence rate
(11). Therefore, conjoint fascial
sheath suspension, a new clinical therapy, has gained favor from
patients (12). This study focused
on comparing the conjoint fascial sheath suspension and frontalis
muscle suspension based on comparison of clinical efficacy, ocular
surface, and refractive status to find out which one is more
advantageous in the treatment of moderate or severe congenital
ptosis.
Patients and methods
General materials
A total of 75 patients with moderate or severe
congenital ptosis (108 eyes) treated in Yidu Cental Hospital
(Qingzhou, China) from June 2014 to June 2019 were enrolled in this
study, and divided into group A and group B. Group A was treated
with conjoint fascial sheath suspension (n=38, 55 eyes), while
group B was treated with frontalis muscle suspension (n=37, 53
eyes). group A consisted of 18 males (25 eyes) and 20 females (30
eyes) aged 18-34 years, with an average age of 21.5±3.3 years.
There were 17 patients (23 eyes) with moderate ptosis and 21
patients (32 eyes) with severe ptosis in group A. Group B consisted
of 16 males (24 eyes) and 21 females (29 eyes) aged 19-35 years,
with an average age of 22.3±2.7 years. There were 17 patients (22
eyes) with moderate ptosis and 20 patients (31 eyes) with severe
ptosis in group B.
The inclusion criteria were as follows: Patients
diagnosed with moderate or severe congenital ptosis, patients with
positive bell syndrome before surgery, patients who had not
received any eyelid surgery, and patients with all required
clinical data. The study was approved by the Ethics Committee of
Yidu Central Hospital. All subjects and their family members were
informed of the research purpose, and each subject provided a
written informed consent.
Exclusion criteria were as follows: Patients with
the neurosis of Marcus Gunn Jaw Winking syndrome, patients with
connective tissue diseases or immunological diseases, patients with
contraindications for eyelid surgery; patients with severe
dysfunction in heart, lung, liver or kidney or hematopoietic
failure, or patients with psychosis or family history of
psychosis.
Methods
Each patient in group A was treated using the
conjoint fascial sheath suspension as follows: i) The subcutaneous
tissue was cut off along a designed cutting line. ii) Each patient
was disinfected and draped, and then anesthetized through
subcutaneous infiltration from conjunctival epithelium and upper
eyelid. iii) The upper eyelid skin and subcutaneous tissue were cut
open along the designed incision to cut off the loose skin. iv) The
ocular anterior muscle of tarsus was cut off, and the tarsus edge
was fully exposed. v) The orbital septum was lifted, and excess fat
was removed. It was separated from the levator muscle. The exposed
diaphragm was separated from levator muscle, and the conjunctivas
were injected with 2% lidocaine, and separated from Miller muscle
with water. The upper eyelid pal muscle was separated from Miller
muscle aponeurosis at the site 5 mm above the hole, and the white
conjoint fascial sheath (CFS) thickened tissue was exposed. vi) The
CFS was pulled down, sutured with 6-0 nylon thread, and fixed at
the middle, inner, and outer upper edge of the tarsus (1/3,
respectively), so that the upper eyelid edge was 3 mm above the
pupil when the eye was opened to look straight ahead, and both
sides were basically symmetrical. vii) The incision at the upper
edge of tarsus and the side of the eyelid edge was subject to
subcutaneous mattress suture with 6-0 nylon to form double eyelid
for adhesion. The incision was sutured at the middle, inner and
outer of the eyelid (1/3, respectively). viii) From Miller muscle,
the upper eyelid muscle and muscle complex were sutured to the bone
margin, and then the skin incision due to the double eyelid surgery
was sutured. ix) The eyelid was applied with erythromycin ointment,
and bound up under pressure.
Each patient in group B was treated with frontalis
muscle suspension: i) For unilateral ptosis, the incision of the
affected double eyelid was designed according to half of the width
in the healthy double eyelid to cut off loose skin. The auxiliary
incision was designed in the lower 1/3 under the affected eyebrow,
with a length of 1.5 cm, and the frontal muscle flap was designed
to cover ~1.5x3.5 cm. ii) Each patient was disinfected and draped
conventionally, and then locally anesthetized through infiltration.
iii) The upper eyelid skin and subcutaneous upper eyelid were cut
open along the incision line to cut off the loose skin, and the
orbicularis oculi muscle was cut open along the double eyelid line
parallel to the upper edge of tarsus with a needle-shaped electric
knife to explore the anterior tarsal fascia. iv) The auxiliary
incision under the eyebrow at the affected side was cut open to the
subcutaneous site, and the range of frontal muscle flap was
designed before separation surgery at subcutaneous and periosteal
levels. The incision and forehead muscle flap were cut off
vertically to form tongue muscle flap, and its bleeding was stopped
with electrocoagulation. v) A tunnel was formed with ophthalmic
scissors by cutting it under the muscle toward the incision below
eyebrow subcutaneously, and the frontal muscle flap was pulled down
through the tunnel and sutured and fixed to the middle and upper
edge of the anterior tarsal fascia, so that the eye could be
basically symmetrical with that of the healthy side when opening to
look straight ahead. vi) The upper edge of anterior tarsal fascia
and muscle at the eyelid margin incision were sutured with 6-0
nylon thread to form double eyelid. The skin was sutured
interruptedly with 7-0 nylon thread. Film was inserted into the
incision under eyebrow for drainage, and subcutaneous skin and skin
were sutured interruptedly with 6-0 nylon thread. vii) The eyelid
was applied with erythromycin ointment, and bound up under
pressure.
Observation indexes
i) The general baseline data of the two groups were
compared. ii) The total correction efficiency of the two groups was
also compared. Evaluation criteria (13): After surgery, the width of palpebral
fissure, upper corneal mass, and cornea exposure of the patients
were evaluated. If the upper eyelid edge of one patient was located
at the site 1 mm from the corneal limbus, and the patient showed
natural upper eyelid arc and symmetrical eyelids, the result was
well corrected. If the eyelid edge of one patient was located
between the site 1 mm above the corneal limbus or the site 2 mm
below it, and the patient showed natural double-fold eyelid arc and
acceptable upper eyelid correction, the result was fairly well
corrected. The patient's upper eyelid edge should be located at the
site 2 mm from the cornea when looking straight ahead. If the site
of upper eyelid edge was 1-2 mm from the right site, the patient
was undercorrected, while if it was more than 2 mm from the right
site, the patient was overcorrected. The total correction
efficiency = (the number of well corrected patients + the number of
fairly well corrected patients)/the total number of patients x100%.
iii) The satisfaction of the two groups was compared: The patients
were investigated at three months after surgery. Satisfaction =
(the number of patients satisfied with the surgery + the number of
patients basically satisfied with the surgery)/the total number of
patients x100%. iv) The ocular surface of the two groups was
compared: The tear break-up time (BUT), Schirmer test (SIt) levels
and corneal staining score (FL) of the patients were detected
before surgery and at one week after surgery. The BUT of the
patients was determined continuously three times. If the BUT was
less than 10 sec, the tear film was judged as unstable. If the SIt
observation time was 5 min and the wet length of the filter paper
was longer than 5 mm, the secretion could be determined to be low
secretion. The corneal coloring in four quadrants need to be
observed, with 3 points for dense point or patchy coloration, 2
points for slightly dense coloration, 1 point for scattered point
coloration, and 0 points for no coloring, and a total of 12 points.
v) The refractive status of the two groups was compared: The
refraction of the two groups was determined at 1 month after
surgery. vi) The postoperative complications of the two groups were
compared at three months after surgery: The complications such as
upper eyelid entropion, exposure keratitis, conjunctival prolapse,
and blepharal hematoma of the patients were analyzed at three
months after surgery to count the complication rate.
Statistical analysis
The data were analyzed comprehensively and
statistically using SPSS 19.0 (Asia Analytics Formerly SPSS). The
enumeration data were analyzed using χ2, and measurement
data were expressed as the (mean ± SD). The inter-group comparison
in expression level before and after treatment was carried out
using the paired t-test, and the comparison between group A and
group B in expression level at the same time-point was carried out
using the independent-samples t-test. P<0.05 indicates a
significant difference.
Results
Comparison between the two groups in
general baseline data
It was necessary to compare the basic situation of
group A and group B, such as age, sex, hypertension, diabetes, and
individual preferences including smoking and drinking (all
P>0.05). Details are shown in Table
I.
 | Table IGeneral baseline data of group A and
group B [n(%)](mean ± SD). |
Table I
General baseline data of group A and
group B [n(%)](mean ± SD).
| Group | Group A (n=38; no. of
eyes, 55) | Group B (n=37; no. of
eyes, 53) | t/χ2
value | P-value |
|---|
| Sex | | | 0.129 | 0.720 |
|
Male | 18 (47.37) | 16 (43.24) | | |
|
Female | 20 (52.63) | 21 (56.76) | | |
| Age (years) | 21.5±3.3 | 22.3±2.7 | 1.147 | 0.255 |
| Upper eyelid state
(eye) | | | 0.141 | 0.708 |
|
Moderate | 25 (45.45) | 26 (49.06) | | |
|
Severe | 30 (54.55) | 27 (50.94) | | |
|
Ptosis
(mm) | 2.753±0.834 | 2.596±0.710 | 1.052 | 0.295 |
| Diabetes history | | | 0.123 | 0.725 |
|
Yes | 19 (50.00) | 17 (45.95) | | |
|
No | 19 (50.00) | 20 (54.05) | | |
| Smoking | | | 0.014 | 0.907 |
|
Yes | 19 (50.00) | 19 (51.35) | | |
|
No | 19 (50.00) | 18 (48.64) | | |
| Fond of drinking | | | 0.324 | 0.569 |
|
Yes | 16 (43.24) | 18 (48.64) | | |
|
No | 22 (56.76) | 19 (51.35) | | |
| Obesity | | | 0.329 | 0.573 |
|
Yes | 21 (47.62) | 18 (50.00) | | |
|
No | 17 (52.38) | 19 (38.10) | | |
| History of
hypertension | | | 1.072 | 0.300 |
|
Yes | 16 (43.24) | 20 (54.05) | | |
|
No | 22 (56.76) | 17 (45.95) | | |
Comparison between the two groups in
ocular surface at one week after surgery
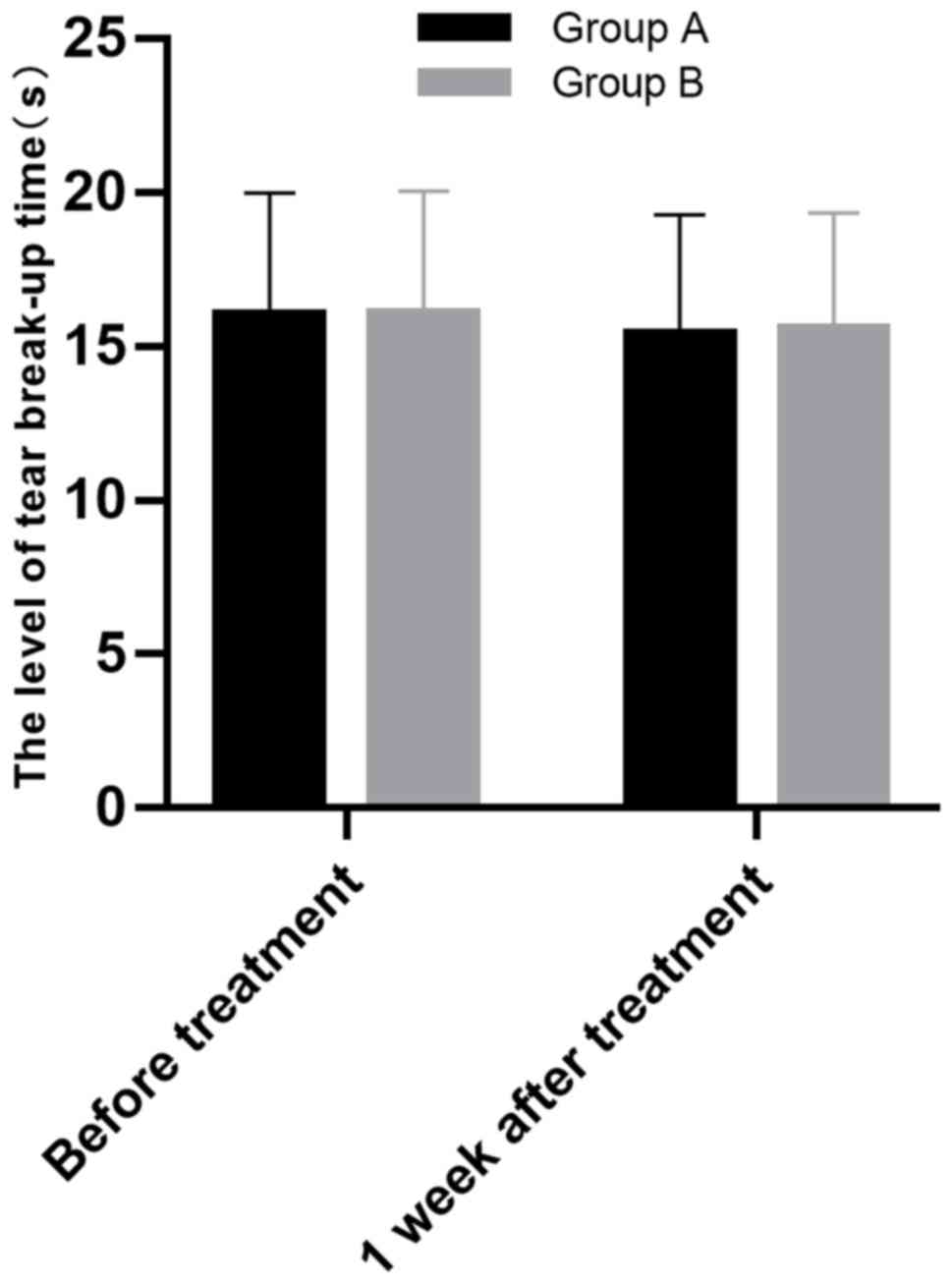
i) The BUT level of the two groups was
compared. The BUT level of group A before surgery and at one
week after surgery was 16.03±3.96 and 15.38±3.91 sec, respectively,
and that of group B before surgery and at one week after surgery
was 16.05±4.01 and 15.57±3.78 sec, respectively. Therefore, both
groups showed no significant BUT level change after surgery, and
group A was also not much different from group B in BUT level
before and after surgery (all P>0.05). More details are shown in
Fig. 1.
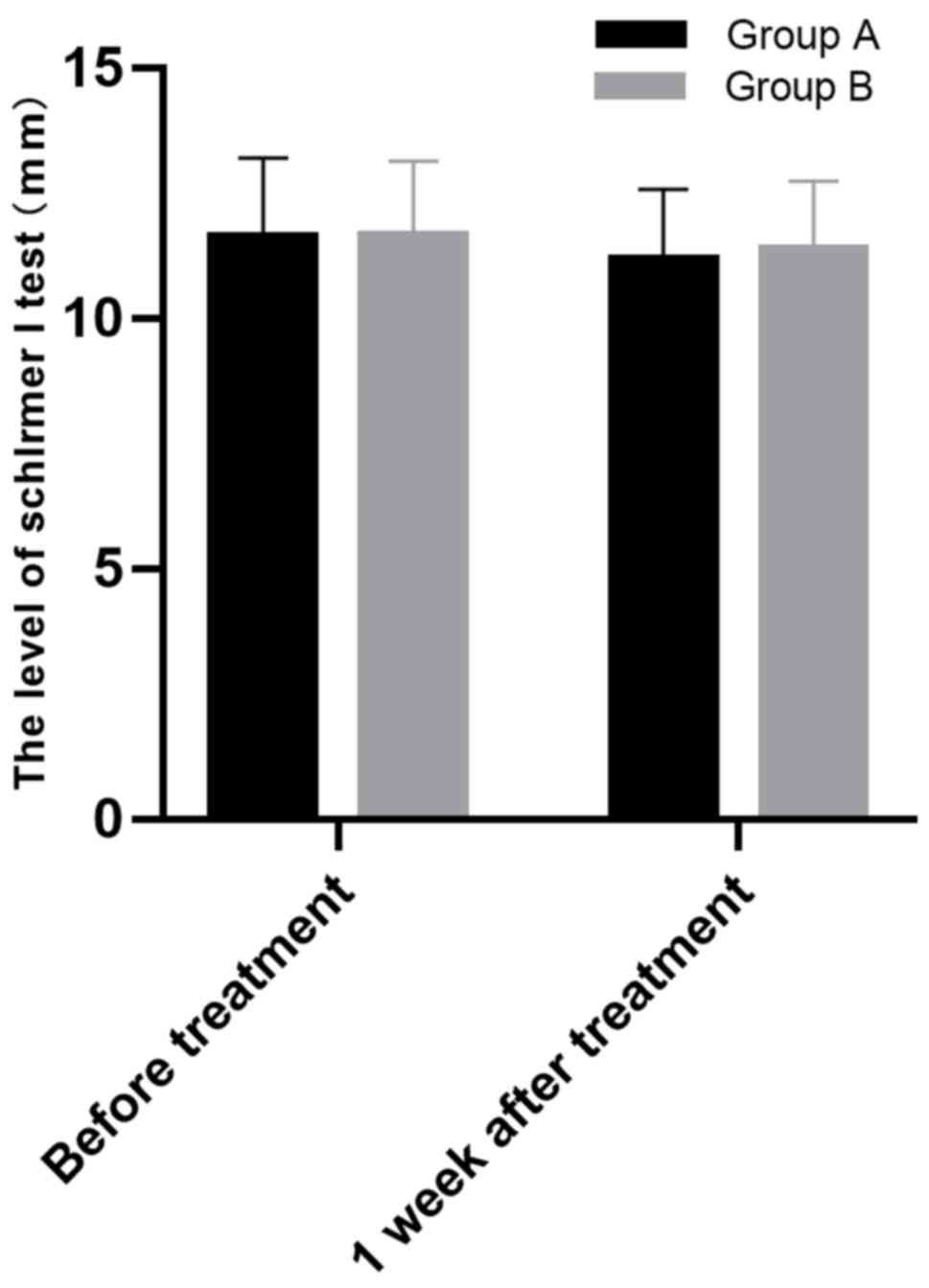
ii) The SIt level of the two groups was
compared. The wet length of the filter paper of group A before
surgery and at one week after surgery was 11.63±1.59 and 11.18±1.41
mm, respectively, and that of group B before surgery and at one
week after surgery was 11.65±1.51 and 11.37±1.38 mm, respectively.
Therefore, both groups showed no significant SIt level change after
surgery, and group A was also not much different from group B in
SIt level before and after surgery (all P>0.05). More details
are shown in Fig. 2.
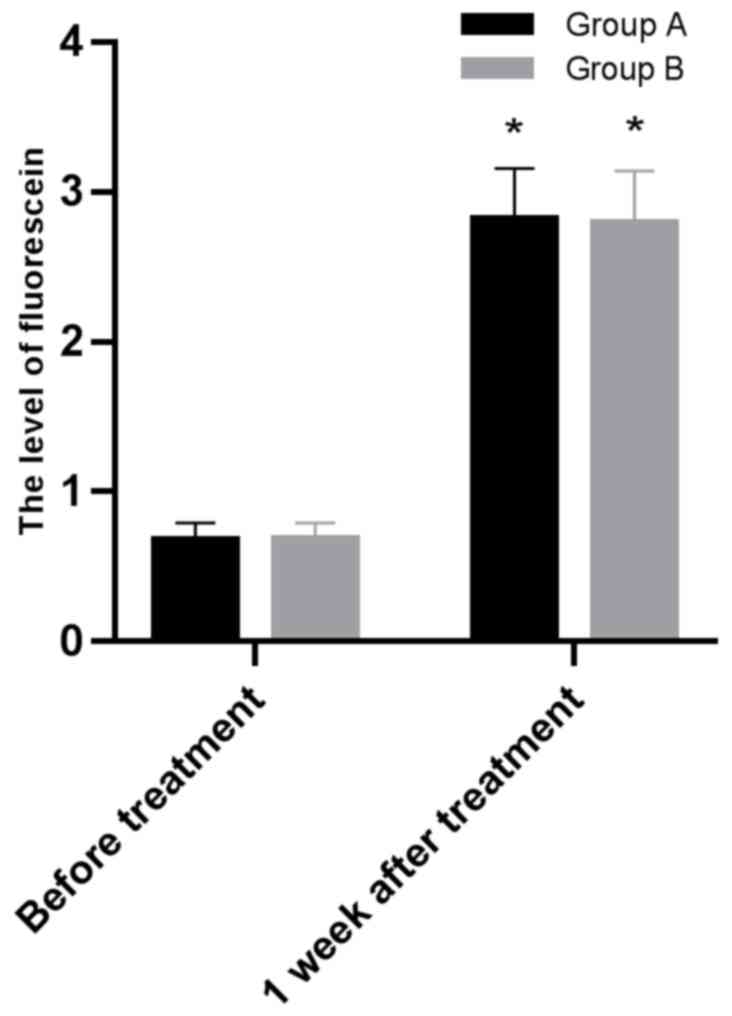
iii) Comparison of FL levels after one week of
operation between the two groups. Before surgery and one week
after surgery, the FL levels of group A were 0.67±0.12 and
2.82±0.34 mm; the FL levels of group B were 0.68±0.11 and 2.79±0.35
mm. There were significant differences in FL levels in the two
groups between before and after surgery (P<0.05). The levels of
FL in group A before and after surgery were not significantly
different from those in group B (P>0.05) (Fig. 3).
Refraction
The refraction of group A before surgery and at one
week after surgery was -4.72±1.03 and -4.02±1.04, respectively, and
that of group B before surgery and at one week after surgery was
-4.87±1.12 and -4.33±1.02, respectively. Both groups showed
significant refraction changes at one month after surgery
(P<0.05), but group A was not significantly different from group
B in refraction before and after surgery (P>0.05). More details
are shown in Table II.
 | Table IIRefraction of group A and group B. |
Table II
Refraction of group A and group B.
| Group | Group A (n=38) | Group B (n=37) | t value | P-value |
|---|
| One day after
surgery | -4.72±1.03 | -4.87±1.12 | 0.604 | 0.548 |
| One month after
surgery | -4.02±1.04 | -4.33±1.02 | 1.308 | 0.197 |
| t value | 2.948 | 3.407 | | |
| P-value | 0.004 | 0.001 | | |
Comparison between group A and group B
in the total correction efficiency
Group A showed a total correction efficiency of
86.84%, with 19 patients well corrected, 14 patients fairly well
corrected, 5 patients undercorrected, and no patient overcorrected,
and group B showed a total correction efficiency of 63.16%, with 12
patients well corrected, 11 patients fairly well corrected, 7
patients undercorrected, and 7 patients overcorrected, so the total
correction efficiency of group A was significantly higher than that
of group B (P<0.05). Details are shown in Table III.
 | Table IIIComparison between group A and group
B in the total correction efficiency. |
Table III
Comparison between group A and group
B in the total correction efficiency.
| Group | Group A (n=38) | Group B (n=37) | χ2
value | P-value |
|---|
| Well corrected | 19 (50.00) | 12 (32.43) | - | - |
| Fairly well
corrected | 14 (36.84) | 11 (29.73) | - | - |
| Undercorrected | 5 (13.16) | 7 (18.92) | - | - |
| Overcorrected | 0 (0.00) | 7 (18.92) | - | - |
| The total
correction efficiency (%) | 33 (86.84) | 23 (63.16) | 4.756 | 0.029 |
Comparison between the two groups in
satisfaction
Group A showed a satisfaction of 94.74%, with 21
patients satisfied with the surgery, 15 patients basically
satisfied, and 2 patients dissatisfied with it, and group B showed
a satisfaction of 72.97%, with 16 patients satisfied with the
surgery, 11 patients basically satisfied, and 10 patients
dissatisfied, so the satisfaction of group A was significantly
higher than that of group B (P<0.05). Details are shown in
Table IV.
 | Table IVComparison of satisfaction between
the two groups [n(%)]. |
Table IV
Comparison of satisfaction between
the two groups [n(%)].
| Group | Group A (n=38) | Group B (n=37) | χ2
value | P-value |
|---|
| Satisfied | 21 (55.26) | 16 (43.24) | - | - |
| Basically
satisfied | 15 (39.48) | 11 (29.73) | - | - |
| Dissatisfied | 2 (5.26) | 10 (27.03) | - | - |
| Satisfaction
(%) | 36 (94.74) | 27 (72.97) | 6.607 | 0.010 |
Comparison between the two groups in
postoperative complications at three months after surgery
Group A showed a complication rate of 7.27%, with no
upper eyelid entropion, 1 patient suffering from exposure
keratitis, 1 patient suffering from conjunctival prolapse, and 2
patients suffering from blepharal hematoma, and group B showed a
complication rate of 26.43%, with 3 patients suffering from upper
eyelid entropion, 5 patients suffering from exposure keratitis, 5
patients suffering from conjunctival prolapse, and 1 patient
suffering from blepharal hematoma, so the complication rate of
group A was significantly lower than that of group B after surgery
(P<0.05). More details are shown in Table V.
 | Table VComparison between group A and group
B in postoperative complications at three months after surgery
[n(%)]. |
Table V
Comparison between group A and group
B in postoperative complications at three months after surgery
[n(%)].
| Group | Group A (55
eyes) | Group B (53
eyes) | χ2
value | P-value |
|---|
| Upper eyelid
entropion | 0 (0.00) | 3 (5.66) | - | - |
| Exposure
keratitis | 1 (1.82) | 5 (9.43) | - | - |
| Conjunctival
prolapse | 1 (1.82) | 5 (9.43) | - | - |
| Blepharal
hematoma | 2 (3.63) | 1 (1.81) | - | - |
| Complication
rate | 4 (7.27) | 14 (26.43) | 7.121 | 0.008 |
Discussion
Upper eyelid ptosis is a relatively common eye
disease requiring correction surgery (14). Common correction methods include the
frontalis muscle suspension and the emerging conjoint fascial
sheath suspension (15,16). The purpose of this study was to
compare the efficiency of the two methods in treating moderate and
severe congenital ptosis.
First we compared the efficacy of conjoint fascial
sheath suspension and that of frontalis muscle suspension based on
comparison of them in the total correction efficiency,
satisfaction, and complications. Results showed that group A had
significantly higher total correction efficiency, less
complications and higher satisfaction than group B. The joint
fascia sheath is a relatively independent connective tissue
structure between the superior rectus and upper eyelid muscles,
with a clear boundary. It is rich in elastic fibers and mainly
contains oculomotor nerves. Therefore, in terms of physiology and
anatomy, the structure of the combined fascia sheath is better than
the frontal muscle flap. Because of the principles of physiology
and anatomy, in theory, fascia sheath suspension could be combined
with frontalis flap suspension (17,18).
Some studies have concluded that frontalis muscle suspension has
obvious defects, because it usually causes insufficient correction,
greatly impacts the appearance of eyelid, brings many postoperative
complications and even leads to exposure keratitis (19-21),
and some studies have found that conjoint fascial sheath suspension
is much more advantageous than frontalis muscle suspension, with
better efficacy and fewer complications (22,23).
Conjoint fascial sheath suspension contributes to more natural
movement of eyelid edge in blinking, and it is more biomechanical
and involves a smaller anatomical scope, so it can effectively
avoid a series of complications, and is suitable for the treatment
of patients under recurrence after frontalis muscle suspension
(24). A study by Zhang et al
found that compared with frontalis muscle suspension, conjoint
fascial sheath suspension had advantages including contributing to
beautiful and natural appearance, providing high safety, bringing
high satisfaction rate, causing fewer complications, and providing
strong physiology, which was worthy of clinical reference (25). Based on the above conclusions, we
considered conjoint fascial sheath suspension was more effective
than frontalis muscle suspension.
The two groups were compared in ocular surface at
one week after surgery, finding that after surgery, corneal
staining scores (FL) in group A and group B were significantly
increased; the groups showed few BUT and SIt level changes, and
there was no significant difference between them in the two
aspects. A similar study also revealed that both conjoint fascial
sheath suspension and frontalis muscle suspension caused only
slightly different BUT and SIt levels (26). The above results indicate that BUT
and SIt levels have scarce connection with the surgical method.
Compared with previous clinical studies on the
treatment of combined fascial sheath suspension and frontal flap
suspension, the greatest advantage of this experiment is that not
only the efficiency and the incidence of complications, but also
the diopters were compared with confirm the effect of two different
treatments on the vision of the two groups of patients. Abnormal
ptosis of the upper eyelid during primary gaze causes narrow
palpebral fissure, and increases contact area between the eyelid
and ocular surface, so upper eyelid ptosis greatly compromises the
eyesight of the patients (27,28). In
this study, the refractive status of the two groups before and
after surgery were compared with assess the role of surgery methods
in improving eyesight. We found that both groups showed significant
refraction changes at one month after surgery, but group A was not
significantly different from group B in refraction before and after
surgery. It suggested that both surgery methods could improve
refraction, thus improving the eyesight. Based on the results of
this experiment, although the differences in diopter, BUT, and SIt
levels between the two groups of patients were not obvious, it is
clear that the patients who used the combined fascial sheath
suspension had better correction effects and fewer complications.
The two treatments have obvious effects on reducing the refractive
power after operation, but combined fascia sheath suspension has
better correction effects and fewer complications, so the patient's
satisfaction is higher.
This experiment still has some shortcomings. First,
the number of samples is small, which affects the richness of the
samples. Second, conjoint fascial sheath suspension is only
compared with frontalis muscle suspension. In future, conjoint
fascial sheath suspension should also be compared with other
surgery methods besides frontalis muscle suspension, and the sample
size should be more abundant to better demonstrate the advantages
of conjoint fascial sheath suspension through comparison.
In conclusion, in terms of refractive status and
ocular surface, the two surgery methods are not very different, but
in terms of efficacy, conjoint fascial sheath suspension is more
advantageous than frontalis muscle suspension, and it brings less
complications, and enjoys a higher satisfaction, so it is worthy of
promotion.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XP and CX conceived and designed the study. XP, TW,
XW and CX were responsible for the acquisition, analysis and
interpretation of the data. TW drafted the manuscript. XP revised
the manuscript critically for important intellectual content. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yidu Central Hospital (Qingzhou, China). Signed informed consents
were obtained from the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Salman MS and Clark IH: Eyelid retraction
in isolated unilateral congenital blepharoptosis. Front Neurol.
8(190)2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lee JH and Kim YD: Surgical treatment of
unilateral severe simple congenital ptosis. Taiwan J Ophthalmol.
8:3–8. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Allard FD and Durairaj VD: Current
techniques in surgical correction of congenital ptosis. Middle East
Afr J Ophthalmol. 17:129–133. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Matayoshi S, Pereira IC and Rossato LA:
Surgical treatment of congenital blepharoptosis. Rev Bras Oftalmol.
73:202–209. 2014.
|
|
5
|
Vyas KS, Kim U, North WD and Stewart D:
Frontalis sling for the treatment of congenital ptosis. Eplasty.
16(ic12)2016.PubMed/NCBI
|
|
6
|
Quaranta-Leoni FM, Sposato S, Leonardi A,
Iacoviello L and Costanzo S: Timing of surgical correction for the
treatment of unilateral congenital ptosis: Effects on cosmetic and
functional results. Orbit. 36:382–387. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhou F, Ouyang M, Ma D, Liu G and Cheng H:
Combined surgery for simultaneous treatment of congenital ptosis
and coexisting strabismus. J Pediatr Ophthalmol Strabismus.
54:288–294. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Paik JS, Kim SA, Park SH and Yang SW:
Refractive error characteristics in patients with congenital
blepharoptosis before and after ptosis repair surgery. BMC
Ophthalmol. 16(177)2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mokashi AA, Stead RE and Abercrombie LC:
Brow suspension using 3-0 Prolene. Eye (Lond).
25(819)2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Arajy ZY: Open loop fascial sling for
severe congenital blepharoptosis. J Craniomaxillofac Surg.
40:129–133. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Farahat HG, Badawi NM, Mandour SS and Nage
SA: Comparison of fasica lata and prolene suture in frontalis
suspension surgery: Frontalis muscle suspension. Menoufia Med J.
30(502)2017.
|
|
12
|
Ahn TJ, Kim JH, Lee EI, Lew DH, Kim NH,
Park RH, Kim KT and Song SH: Nonincisional conjoint fascial sheath
suspension: A novel technique for minimally invasive blepharoptosis
correction. Ann Plast Surg. 79:334–340. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pan E, Yu J, Zhang S, Nie Y and Li Q:
Retrospective analysis of the effect of Hering's law on outcomes of
surgical correction of ptosis. Ann Plast Surg. 80:242–244.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hwang K, Shin YH and Kim DJ: Conjoint
fascial sheath of the levator and superior rectus attached to the
conjunctival fornix. J Craniofac Surg. 19:241–245. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sokol JA, Thornton IL, Lee HB and Nunery
WR: Modified frontalis suspension technique with review of large
series. Ophthalmic Plast Reconstr Surg. 27:211–215. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Holmström H and Santanelli F: Suspension
of the eyelid to the check ligament of the superior fornix for
congenital blepharoptosis. Scand J Plast Reconstr Surg Hand Surg.
36:149–156. 2002.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zuo L, Wang XX, Huang XY, Zhang JL and Du
YY: A modified levator resection technique involving retention of
the levator palpebrae superioris muscle suspension system for
treatment of congenital ptosis. Aesthetic Plast Surg. 41:856–862.
2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yadav C, Saini A and Maji PK: Energy
efficient facile extraction process of cellulose nanofibres and
their dimensional characterization using light scattering
techniques. Carbohydr Polym. 165:276–284. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Farooq SM and Wani EA: Frontalis sling
surgery: Silicon rod versus autogenous fascia lata in congenital
ptosis. Int J Med Sci Public Health. 5(6)2016.
|
|
20
|
Lee YJ and Park DD: Frontalis transfer and
closed silicone rod frontalis suspension. Aesthetic Plast Surg.
22:3–9. 2016.
|
|
21
|
Wilson ME and Johnson RW: Congenital
ptosis. Long-term results of treatment using lyophilized fascia
lata for frontalis suspensions. Ophthalmology. 98:1234–1237.
1991.PubMed/NCBI
|
|
22
|
Lin W, Xu Y and Ye FL: Comparative study
on conjoint fascial sheath suspension and levator muscle resection
for moderate or severe congenital ptosis. Int Eye Sci.
16:1193–1195. 2016.
|
|
23
|
Zhao YN, Ge HG and Shen QL: Comparative
study on conjoint fascial sheath suspension and the simple
frontalis muscle suspension for moderate or severe ptosis. Int Eye
Sci. 17:1790–1792. 2017.
|
|
24
|
Xin LI, Lu MT, Jiang Y, Zhou WK, Zheng YM,
Wu HY and Zhang L: Clinical study on conjoint fascial sheath
suspension in the treatment of moderate and severe ptosis. J Reg
Anat Operative Surg. 27:333–336. 2018.
|
|
25
|
Zhang F, Sun Y and Liu L: Clinical
efficacy of conjoint fascial sheath of the levator and superior
rectus attached to conjunctival fornix suspension surgery in
treatment of severe blepharoptosis. Chin J Med Aesthet Cosmetology.
23:399–401. 2017.
|
|
26
|
Zhang D, Guo B and Cai W: Effect of
frontal muscle aponeurosis flap suspension surgery for severe
congenital ptosis in children. Minerva Pediatr. 71:358–361.
2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ma L, Mu X, Wang J and Liu H: Conjoint
fascia sheath suspension for treatment of moderate to severe ptosis
of the upper eyelid and observation of postoperative upper eyelid
movement. Int J Clin Exp Med. 11:12531–12538. 2018.
|
|
28
|
Zhu T, Ye X, Xu P, Wang J, Zhang H, Ni H,
Su Z and Ye J: Changes of corneal tomography in patients with
congenital blepharoptosis. Sci Rep. 7(6580)2017.PubMed/NCBI View Article : Google Scholar
|