Introduction
Neck pain is a frequently encountered complaint in
emergency and orthopedic departments. According to statistics, ~71%
of individuals experience neck pain during their lifespan (1). Crowned dens syndrome (CDS) was first
reported by Bouvet et al (2)
in 1985, which is a rare cause of neck pain with restricted
mobility and its incidence is 2% in patients with acute neck pain
(3). Since this first case was
reported, only 88 further cases were reported in the literature
until March 2020 (1-50).
Due to its rarity, clinicians at emergency departments and
orthopedic surgeons are generally not sufficiently aware of the
disease and numerous cases with matching symptoms are not properly
diagnosed; thus, the incidence of CDS appears to be
underestimated.
The clinical manifestations of CDS include acute
neck pain, neck stiffness accompanied by restricted cervical range
of motion, fever and/or high serum C-reactive protein (CRP) levels
and erythrocyte sedimentation rate (ESR). There are reports on
cases of nerve root compression and even rare cases of spinal cord
compression (51,52); these cases have symptoms similar to
cervical spondylotic radiculopathy and myelopathy, i.e., radicular
pain in the upper extremities, difficulty in walking, paralysis of
the extremities and even progressively aggravated quadriplegia. A
CT scan reveals the presence of irregular high-density shadows at
different sizes surrounding the top and lateral sides of the
odontoid process, appearing as a crown surrounding the top of the
dens.
The present study reported on four cases of CDS who
rapidly recovered after treatment with non-steroidal
anti-inflammatory drugs (NSAIDs) at Hubei 672 Orthopaedics Hospital
of Integrated Chinese and Western Medicine (Wuhan, China).
Case report
Case 1
A 76-year-old female was admitted to the Department
of Minimally Invasive Spinal Surgery in Hubei 672 Orthopaedics
Hospital of Integrated Chinese and Western Medicine (Wuhan, China)
in May 2018, presenting with neck pain with restricted cervical
range of motion of unknown causes for 3 days. She complained of
persistent pain but had no other type of discomfort, such as
numbness or pain in the upper limbs or unstable walking. The
patient denied a history of gout or rheumatoid arthritis. On
admission, the patient's body temperature was 36.6˚C and the neck
muscle (sternocleidomastoid) was stiff with an obviously restricted
cervical range of motion with a pain Visual Analogue Scale (VAS)
score of 8. The patient had no signs of neurological or spinal cord
injuries. Laboratory examination results revealed the following
abnormalities: White blood cells (WBC), 3.33x109/l
[normal range (NR), 4-10x109/l]; high-sensitivity CRP
(hs-CRP), 31.0 mg/l (NR, 0-10 mg/l); ESR, 49.0 mm/h (NR, 0-15
mm/h); calcium, 2.30 mmol/l (NR, 2.03-2.6 mmol/l); and magnesium,
1.00 mmol/l (NR, 0.67-1.04 mmol/l). Rheumatoid factor (RF),
anti-streptolysin O (ASO), anti-cyclic citrullinated peptide
antibody (anti-CCP antibody) and procalcitonin (PCT) levels were
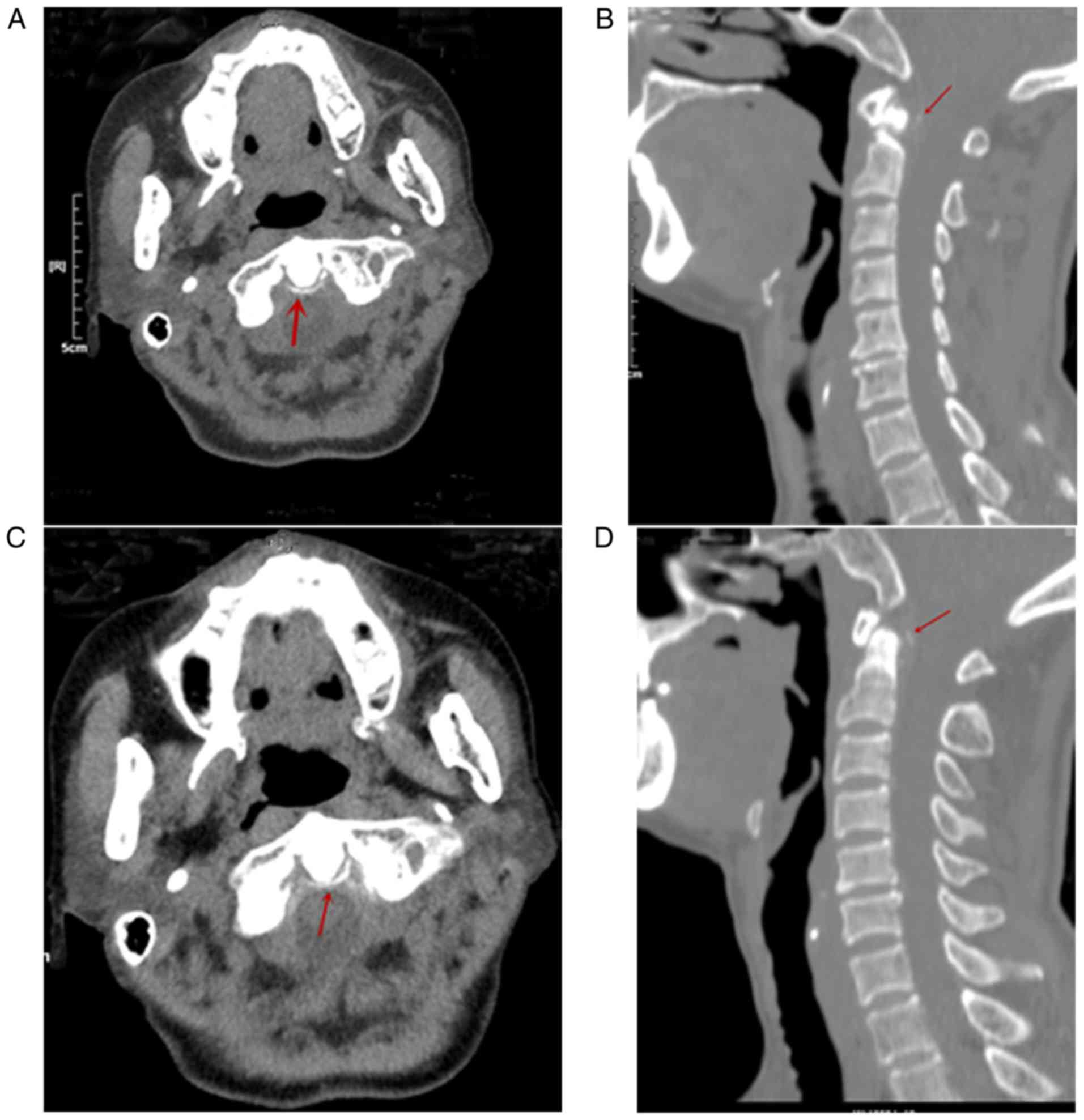
normal. After admission, CT scans revealed arc-shaped calcification
of the transverse ligament (Fig. 1A)
and vertical line-like calcification of the cruciate ligament of
the atlas in the posterior area of the odontoid process (Fig. 1B). According to the patient's medical
history, physical signs and auxiliary examination results, CDS was
diagnosed. The patient was administered nimesulide (100 mg/tablet,
orally, once in the morning and once in the evening). After 7
successive days of treatment, hs-CRP and ESR recovered to normal,
neck pain and restricted cervical range of motion were obviously
alleviated, and the pain VAS score was 1. Neck pain and restricted
cervical range of motion did not recur during the 10-month
follow-up. The follow-up CT images at 10 months are presented in
Fig. 1C and D. There was no significant difference from
the previous CT scan obtained.
Case 2
A 70-year-old male was admitted to the Department of
Minimally Invasive Spinal Surgery in Hubei 672 Orthopaedics
Hospital of Integrated Chinese and Western Medicine in May 2019,
presenting with neck pain with restricted cervical range of motion
of unknown causes for 4 days. He complained of persistent pain but
had no other types of discomfort, such as numbness or pain in the
upper limbs or unstable walking. The patient had a history of gout.
On admission, the patient's body temperature was 36.5˚C and his
neck muscle (sternocleidomastoid) was stiff with an obviously
restricted cervical range of motion with a pain VAS score of 8. He
had no obvious signs of any neurological or spinal cord injuries.
Laboratory examination results revealed the following: WBC,
8.17x109/l; hs-CRP, 46.5 mg/l; ESR, 64 mm/h; calcium,
2.20 mmol/l; and magnesium, 0.92 mmol/l. RF, ASO, anti-CCP antibody
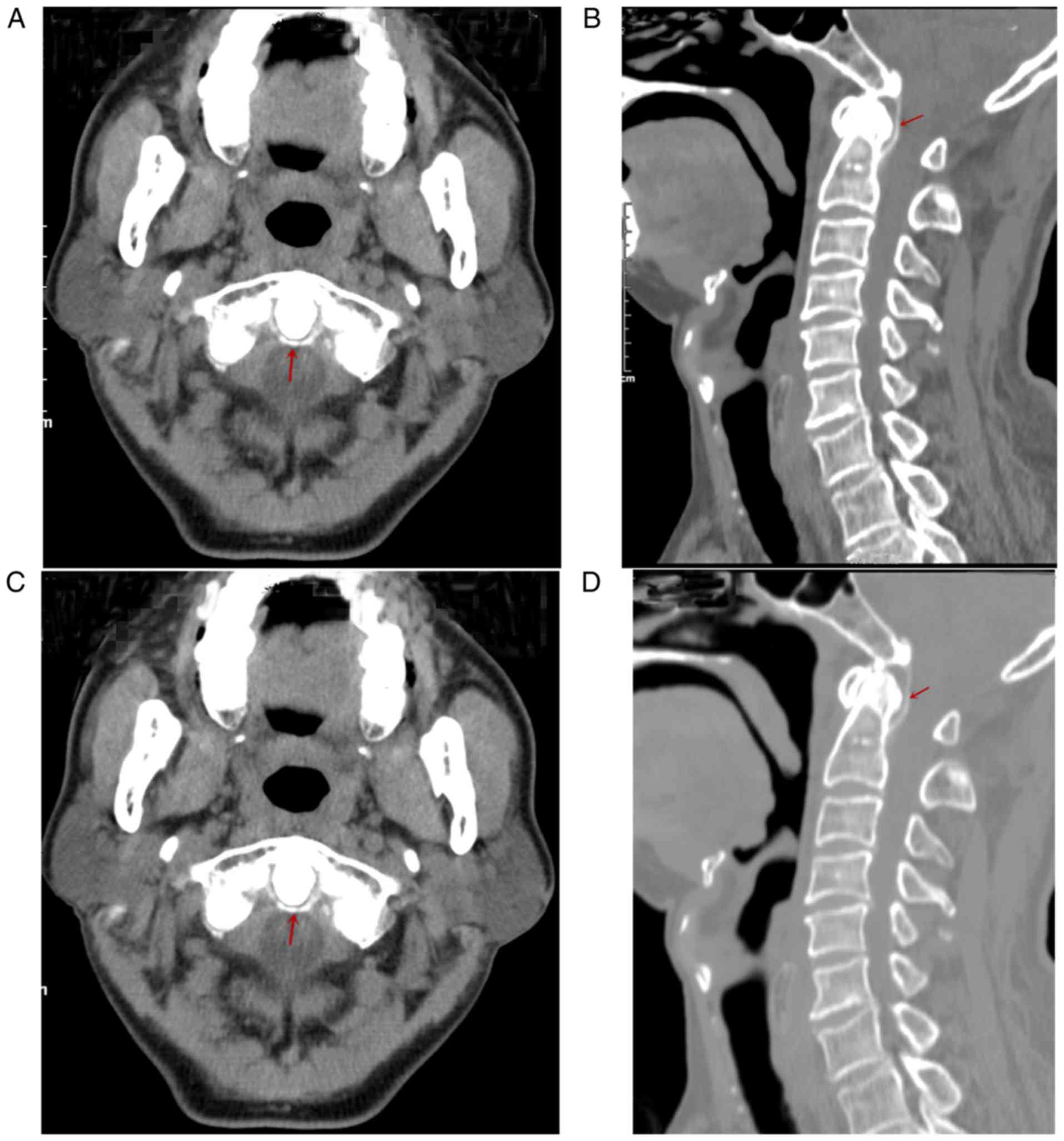
and PCT levels were normal. After admission, CT scans revealed
arc-shaped calcification of the apical ligament (Fig. 2A) and vertical line-like
calcification of the cruciate ligament in the posterior area of the
odontoid process (Fig. 1B).
According to the patient's medical history, physical signs and
auxiliary examination results, CDS was diagnosed. The patient was
administered with lappaconitine hydrobromide (8 mg/ampoule,
intravenous, once a day) and celecoxib (0.2 g/capsule, orally, once
a day). After 3 successive days of treatment, hs-CRP and ESR
recovered to normal, neck pain and restricted cervical range of
motion were obviously relieved and the pain VAS score was 2. Neck
pain and restricted cervical range of motion did not occur during
the 3-month follow-up. The follow-up CT images at 3 months are
presented in Fig. 2C and D. There was no significant difference from
the previous CT scan obtained.
Case 3
A 73-year-old female was admitted to the Department
of Minimally Invasive Spinal Surgery in Hubei 672 Orthopaedics
Hospital of Integrated Chinese and Western Medicine in May 2019,
due to neck pain of unknown causes for 10 days. The patient
complained of persistent neck pain but had no discomfort, such as
numbness or pain in the upper limbs or unstable walking. The
patient had a history of gout. On admission, the patient's body
temperature was 36.3˚C, and the neck muscle (sternocleidomastoid)
was stiff with an obviously restricted cervical range of motion and
a pain VAS score of 6. The patient had no signs of neurological or
spinal cord injuries. Laboratory examination results indicated the
following: WBC, 9.95x109/l; hs-CRP, 19.6 mg/l; ESR, 34
mm/h; calcium, 2.31 mmol/l; and magnesium, 0.7 mmol/l. RF, ASO,
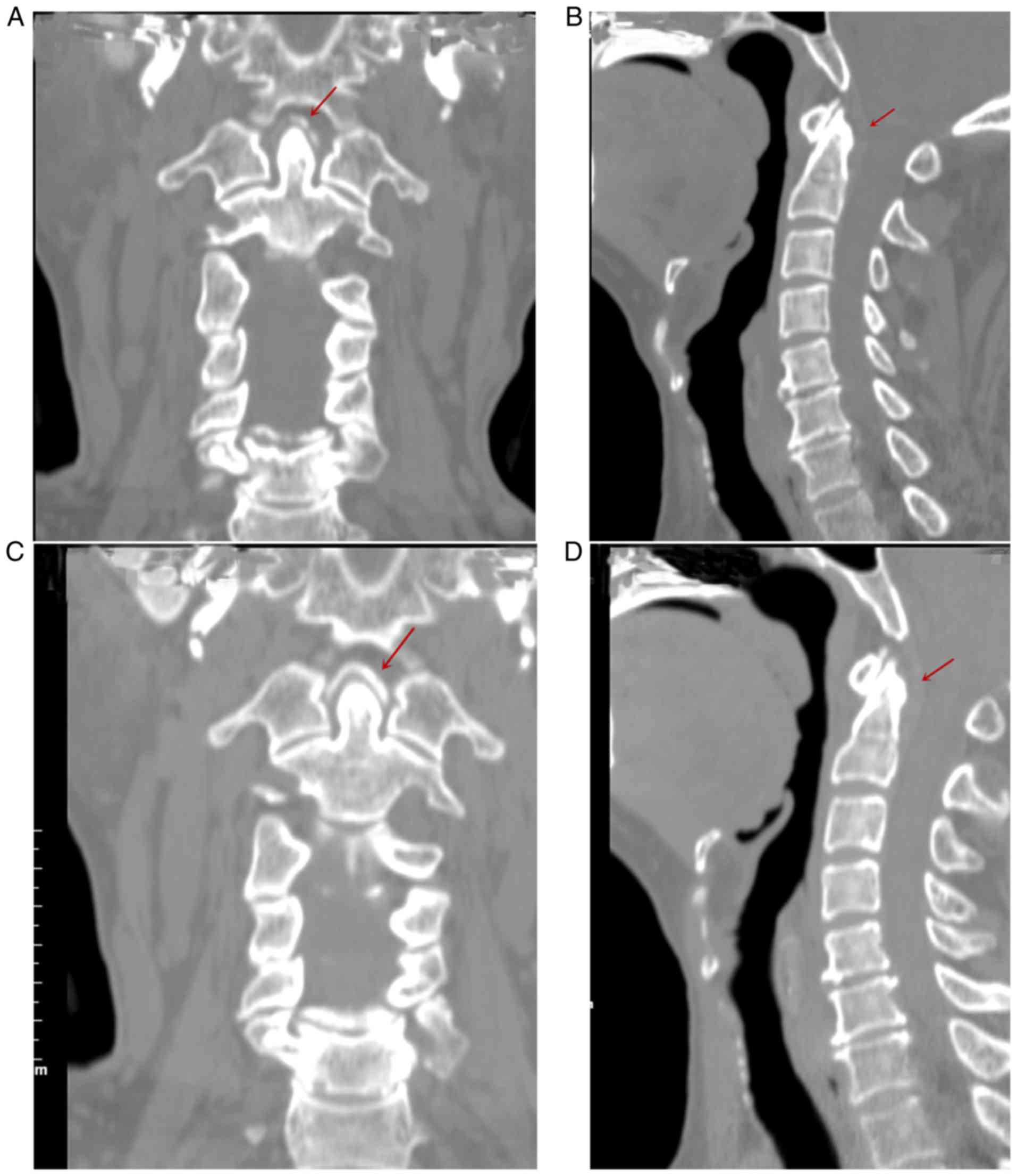
anti-CCP antibody and PCT levels were normal. After admission, CT
scans revealed arc-shaped calcification of the apical ligament in
the anterior area of the odontoid process (Fig. 3A) and vertical line-like
calcification of the cruciate ligament in the posterior area of the
odontoid process (Fig. 1B).
According to the patient's medical history, physical signs and
auxiliary examination results, CDS was diagnosed. The patient was
administered celecoxib (0.2 g/capsule, orally, once a day). After 7
successive days of treatment, hs-CRP and ESR recovered to normal,
neck pain was obviously alleviated and the pain VAS score was 1.
The neck pain did not recur during the 3-month follow-up. The
follow-up CT images at 3 months are presented in Fig. 3C and D. Calcification in the anterior area of the
odontoid process was more marked in the last follow-up.
Case 4
A 78-year-old female was admitted to the Department
of Minimally Invasive Spinal Surgery in Hubei 672 Orthopaedics
Hospital of Integrated Chinese and Western Medicine in June 2019,
due to neck pain of unknown causes for 9 days. The patient
complained of persistent pain but had no other type of discomfort,
such as numbness or pain in the upper limbs or unstable walking.
The patient had a history of hyperlipidemia. On admission, the
patient's body temperature was 36.6˚C and the neck muscle
(sternocleidomastoid) was stiff with an obviously restricted
cervical range of motion and a pain VAS score of 9. The patient had
no signs of neurological or spinal cord injuries. Laboratory
examination results revealed the following: WBC,
7.52x109/l; hs-CRP, 52.25 mg/l; ESR, 64 mm/h; calcium,
2.22 mmol/l; and magnesium, 0.95 mmol/l. RF, ASO, anti-CCP antibody
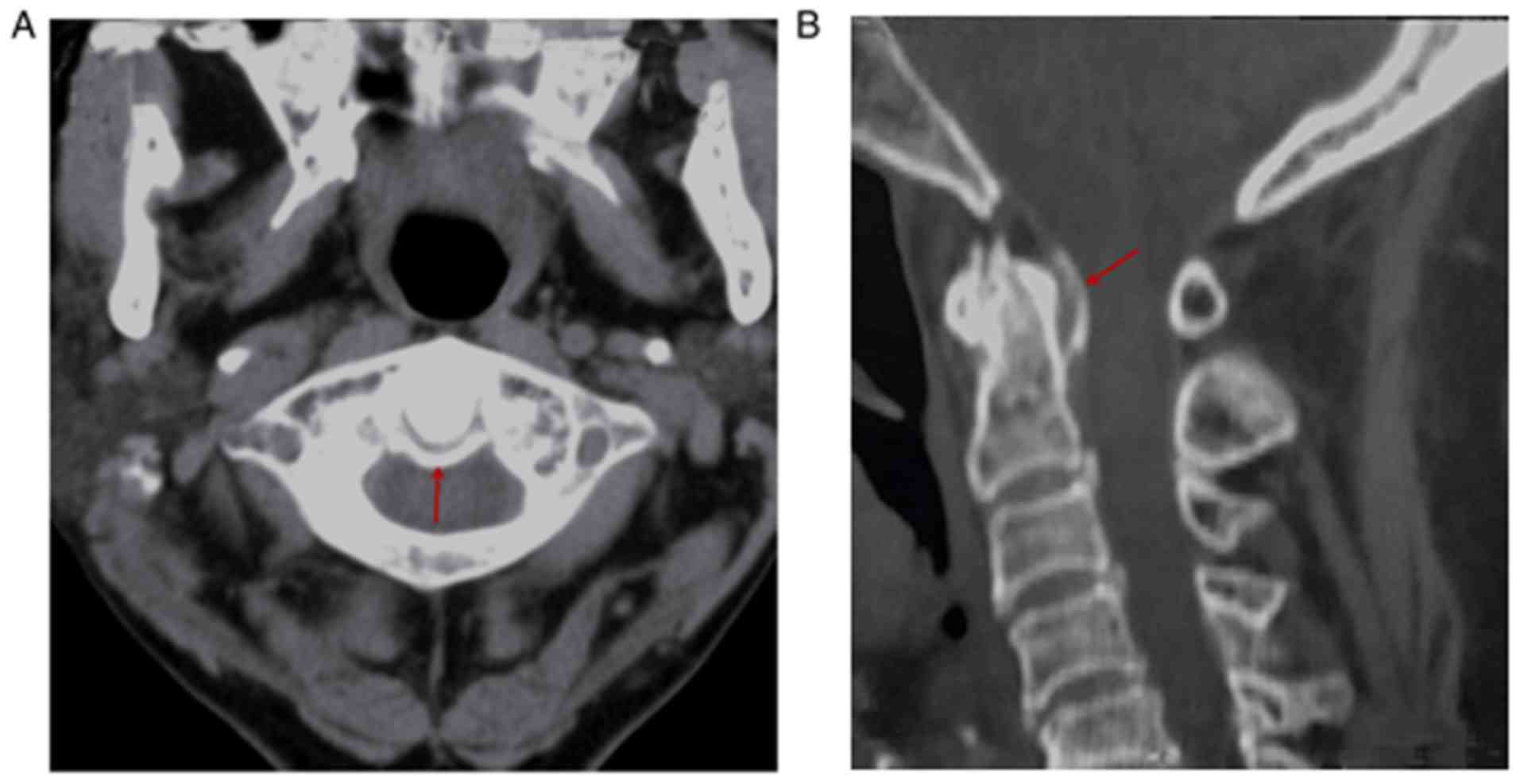
and PCT levels were normal. After admission, CT scans revealed
arc-shaped calcification of the transverse ligament (Fig. 4A) and vertical line-like
calcification of the cruciate ligament of the atlas in the
posterior area of the odontoid process (Fig. 4B). According to the patient's medical
history, physical signs and auxiliary examination results, CDS was
diagnosed. The patient was administered celecoxib (0.2 g/capsule,
by mouth, once a day). After 5 successive days of treatment, hs-CRP
and ESR recovered to normal, neck pain was obviously alleviated and
the pain VAS score was 2. The neck pain did not recur during the
3-month follow-up. However, the patient refused to undergo CT
examination again during the follow-up period.
Discussion
In 1985, Bouvet et al (2) first reported on CDS. They indicated
that CDS mainly occurred in older individuals, i.e., at least 65%
of patients with CDS were aged ≥70 years, with a male-to-female
ratio of 3:5. Therefore, the majority of patients with CDS were
female older adults. In the present study, four cases were aged ≥70
years and three out of four cases were female.
To date, the specific causes of CDS have remained
elusive. CDS may be a pseudo atlantoaxial joint disorder caused by
deposits of calcium pyrophosphate crystals (5,53,54).
Calcium pyrophosphate dihydrate crystal deposition disease occurs
mostly in articular cartilage and ligaments. It is asymptomatic in
half of the patients and it manifests as a joint inflammation
similar to gout, which is referred to as pseudogout in certain
patients. In contrast to the gout frequently occurring in older
adult males, pseudogout is more common in older adult females.
Pseudogout frequently affects the knees, hands, shoulder joints,
elbow joints and feet, and it occasionally occurs in the cervical,
thoracic and lumbar spine (55).
Pseudogout occurring around the cervical odontoid process may cause
neck pain, which usually manifests as acute or subacute moderate to
severe neck pain, even restricted cervical range of motion and
occipital pain (25). Certain
patients have a fever, but neurological examination results are
usually normal. All of the four cases reported in the present study
had only acute severe neck pain and a restricted cervical range of
motion, with no obvious fever or abnormal neurologic symptoms.
CT plain scan focusing on the atlantoaxial joint is
considered the gold standard for CDS diagnosis. CT scans indicate
calcification of the transverse, alar and apical ligaments around
the odontoid process, which may occur anywhere around the odontoid
process, but it most frequently occurs in the posterior and
posterolateral area. In the radiological classification of CDS
proposed by Goto et al (56),
calcification may be present posterior (50%), posterolateral
(27.5%), circular (12.5%), anterior (5%), lateral (5%) to the
odontoid process. In the present study, calcification occurred at
the posterior side of the odontoid process in all of our cases.
Regarding laboratory parameters, CRP and ESR are frequently
markedly elevated and WBC are normal or slightly increased
(53,30,43). In
the four cases of the present study, CRP and ESR were obviously
elevated, but the increase in WBC was not obvious, and it was
decreased in one case.
CDS should be differentiated from meningitis,
epidural abscess, rheumatoid arthritis, rheumatoid polymyalgia,
giant cell arteritis, cervical spondylosis or metastatic bone tumor
(1,43,44,53). All
of the above diseases may manifest as neck pain, fever and
restricted cervical range of motion. Neck pain in CDS radiates from
the bilateral suboccipital area to the neck part, with no specific
tender point or obvious neck rotation limitation. It may be clearly
determined from CT scans of the atlantoaxial joint. This avoids
unnecessary invasive treatments (such as lumbar puncture, tissue
biopsy), inappropriate medication (such as antibiotics, antiviral
drugs) and long-term hospitalization. CDS should also be
differentiated from atlantoaxial synovial cysts, which represent a
rare disease entity and may also cause neck pain. The development
of atlantoaxial synovial cysts has been linked to spinal
instability and trauma. Imaging with CT and MRI scans is crucial
for the diagnosis and characterization of synovial cysts (56,57).
In general, patients with CDS have a good prognosis
and their symptoms usually resolve within a few weeks. However, the
current treatment of CDS remains controversial. NSAIDs are usually
recommended. In most cases reported in the literature, oral NSAIDs
alone may improve symptoms within a few days. Although severe
neurological complications are rare, extensive deposits may result
in myelopathy or cervical stenosis, for which surgical
decompression may be necessary (14). Surgical decompression and
stabilization may alleviate the compression on the cervical spinal
cord, but the potential for neurological recovery remains to be
further elucidated (23). In the
cases of the present study, the symptoms rapidly resolved after
oral administration of NSAIDs. In certain refractory cases,
colchicine or a small amount of corticosteroids may be
administered, but since CDS occurs mainly in older individuals,
steroid therapy should be considered with caution to avoid any
fatal side effects (30,43,44,53,58).
In summary, due to the rare and non-specific
manifestations of CDS, its diagnosis is frequently missed, which
delays its treatment and CDS is easy to treat. Therefore, when
patients have acute neck pain accompanied by a restricted cervical
range of motion, as well as fever, particularly in older
individuals, CDS should be considered.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JT and JL made substantial contributions to the
study conception and design, the acquisition of data and the
analysis and interpretation of data. CW, XL, YL, QL, WX and TZ
contributed to drafting the manuscript and critically revising the
manuscript for important intellectual content. JT prepared the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Hubei 672 Orthopaedics Hospital of Integrated Chinese
and Western Medicine (Wuhan, China; permit no. HB6720121) and was
in conformity with the guidelines of the National Institute of
Health.
Patient consent for publication
The four patients provided written informed consent
for the publication of their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Oka A, Okazaki K, Takeno A, Kumanomido S,
Kusunoki R, Sato S, Ishihara S, Kinoshita Y and Nishina M: Crowned
dens syndrome: Report of three cases and a review of the
literature. J Emerg Med. 49:e9–e13. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bouvet JP, le Parc JM, Michalski B,
Benlahrache C and Auquier L: Acute neck pain due to calcifications
surrounding the odontoid process: The crowned dens syndrome.
Arthritis Rheum. 28:1417–1420. 1985.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Siau K, Lee M and Laversuch CJ: Acute
pseudogout of the neck-the crowned dens syndrome: 2 case reports
and review of the literature. Rheumatol Int. 31:85–88.
2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Malca SA, Roche PH, Pellet W and
Combalbert A: Crowned dens syndrome: A manifestation of
Hydroxy-apatite rheumatism. Acta Neurochir (Wien). 135:126–130.
1995.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Godfrin-Valnet M, Godfrin G, Godard J,
Prati C, Toussirot E, Michel F and Wendling D: Eighteen cases of
crowned dens syndrome: Presentation and diagnosis. Neurochirurgie.
59:115–120. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Baysal T, Baysal O, Kutlu R, Karaman I and
Mizrak B: The Crowned dens syndrome: A rare form of calcium
pyrophosphate deposition disease. Eur Radiol. 10:1003–1005.
2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Aouba A, Vuillemin-Bodaghi V, Mutschler C
and De Bandt M: Crowned dens syndrome misdiagnosed as polymyalgia
rheumatica, giant cell arteritis, meningitis or spondylitis: An
analysis of eight cases. Rheumatology (Oxford). 43:1508–1512.
2004.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sato Y, Yasuda T, Konno S, Kuwayama A and
Komatsu K: Pseudogout showing meningoencephalitic symptoms: Crowned
dens syndrome. Intern Med. 43:865–868. 2004.PubMed/NCBI View Article : Google Scholar
|
|
9
|
De Geeter F, Goethals L, Piette Y, De Neve
J and Ghekiere J: Correlative imaging in crowned dens syndrome.
Clin Nucl Med. 32:854–857. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Frey ME, Dery FJ Jr and Cifu DX: C1-2
Steroid injection for crowned dens syndrome. PM R. 1:379–382.
2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Taniguchi A, Ogita K, Murata T, Kuzuhara S
and Tomimoto H: Painful neck on rotation: Diagnostic significance
for crowned dens syndrome. J Neurol. 257:132–135. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Unlu Z, Tarhan S and Ozmen EM: An
idiopathic case of calcium pyrophosphate dihydrate crystal
deposition disease with crowned dens syndrome in a Young patient.
South Med J. 102:949–951. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ishikawa K, Furuya T, Noda K and Okuma Y:
Crowned dens syndrome mimicking meningitis. Intern Med.
49(2023)2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ali S, Hoch M, Dadhania V and Khurana JS:
CPPD crowned dens syndrome with clivus destruction: A case report.
J Radiol Case Rep. 5:30–37. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Arauz-Rivera R and Garcia-Porrua C:
Crowned dens syndrome resembling meningitis as the first
manifestation of calcium crystal deposition disease. J Am Geriatr
Soc. 60:374–375. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Oda Y, Ooi S, Urushidani Y and Endo A:
Crowned dens syndrome. Intern Med. 51(231)2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Garcia-Gonzalez E, Baldi C, Guidelli GM
and Selvi E: Crowned dens syndrome and cervical interspinous
bursitis mimicking acute meningitis. J Clin Rheumatol. 19:357–358.
2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Morita T, Tanimoto T, Kaji S and Fukutake
T: Poststroke crowned dens syndrome. Spine J. 13:1161–1162.
2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Takahashi T, Minakata Y, Tamura M, Takasu
T and Murakami M: A rare case of crowned dens syndrome mimicking
aseptic meningitis. Case Rep Neurol. 5:40–46. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Uh M, Dewar C, Spouge D and Blocka K:
Crowned dens syndrome: A rare cause of acute neck pain. Clin
Rheumatol. 32:711–714. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yamazaki Y, Kanaya Y, Naka H and Tokinobu
H: Severe occipital pain caused by periodontoid calcifications:
Crowned dens syndrome. Cephalalgia. 33(425)2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kuriyama A: Crowned dens syndrome. CMAJ.
186(293)2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Aichmair A, Herzog RJ, Perino G and Lebl
DR: Recovery after cervical decompression surgery for the treatment
of crowned dens syndrome causing progressive neurological decline:
A case report. HSSJ. 10:83–87. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Koyfman A and Yaffe D: Crowned dens
syndrome a case report. Neuroradiol J. 27:495–497. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ledingham D, Cappelen-Smith C and Cordato
D: Crowned dens syndrome. Pract Neurol. 18:57–59. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Monet A, Massonnat R, Merino B, Riviere A
and Richez C: Crowned dens syndrome diagnosed on 18F-FDG
PET/CT. Clin Nucl Med. 39:1041–1042. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Takahashi T, Tamura M, Osabe K, Tamiya T,
Miki K, Yamaguchi M, Akira K, Kamei S and Takasu T: A rare case of
Parkinson's disease with severe neck pain owing to crowned dens
syndrome. Case Rep Neurol. 6:149–155. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chang WJ, Hamm B, Williams T and Mitra R:
Chronic axial neck pain with underlying crowned dens syndrome. Am J
Phys Med Rehabil. 94:e128–e129. 2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Inokuchi R, Ohshima K, Yamamoto M, Fukuda
T and Nakamura K: Crowned dens syndrome. Spine J. 15:1499–1500.
2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lee GS, Kim RS, Park HK and Chang JC:
Crowned dens syndrome: A case report and review of the literature.
Korean J Spine. 11:15–17. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Moses V, Parmar HA and Sawalha AH:
Magnetic resonance imaging and computed tomography in the
evaluation of crowned dens syndrome secondary to calcium
pyrophosphate dihydrate. J Clin Rheumatol. 21:368–369.
2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Tamura T, Suzuki M and Hori S: Crowned
dens syndrome. Intern Med. 54(545)2015.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yamada T, Saitoh T, Hozumi H, Takahashi Y,
Nozawa M, Mochizuki T and Yoshino A: Crowned dens syndrome. Acute
Med Surg. 2(273)2015.PubMed/NCBI View
Article : Google Scholar
|
|
34
|
Zhang H, Jin D and Sun E: The early and
late stages of crowned dens syndrome: Two case reports. Spine J.
15:e65–e68. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cozzani E, Basso D, Cimmino MA, Larosa M,
Burlando M, Rongioletti F, Drago F and Parodi A: Generalized
annular granuloma associated with crowned dens syndrome, which
resolved with colchicine treatment. Clin Exp Dermatol. 41:640–642.
2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Fung CS and Tam GK: Crowned dens syndrome:
An uncommon cause of cord compression. Hong Kong Med J.
22:399.e4–e5. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Nakano H, Nakahara K, Michikawa Y, Suetani
K, Morita R, Matsumoto N and Itoh F: Crowned dens syndrome
developed after an endoscopic retrograde cholangiopancreatography
procedure. World J Gastroenterol. 22:8849–8852. 2016.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Tagami S, Inokuchi R, Awaji K, Maehara H,
Yamaguchi Y and Nakajima S: Crowned dens syndrome and interspinous
ligament inflammation due to calcium pyrophosphate deposition in an
elderly man. Spine J. 16:e453–e454. 2016.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Inoue A, Kohno K, Ninomiya S, Tomita H,
Iwata S, Ohue S, Kamogawa K, Okamoto K, Fukumoto S, Ichikawa H, et
al: Usefulness of cervical computed tomography and magnetic
resonance imaging for rapid diagnosis of crowned dens syndrome: A
case report and review of the literature. Int J Surg Case Rep.
30:50–54. 2017.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Shikino K, Ota T and Ikusaka M: Crowned
dens syndrome. Am J Med. 130:e111–e112. 2017.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Sifuentes-Giraldo WA, Larena-Grijalba C
and García-Villanueva MJ: Crowned dens syndrome. Rev Clin Esp.
217:302–303. 2017.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Heck A, Nolan N and Rojas-Moreno C:
Crowned dens syndrome: Calcium pyrophosphate deposition disease
masquerading as osteomyelitis. J Rheumatol. 45:1422–1423.
2018.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Bansal A and Gupta M: Crowned dens
syndrome presenting as pyrexia of unknown origin (PUO). Rom J
Intern Med. 57:266–269. 2019.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Koda R, Tsuchida Y, Yoshizawa K, Suzuki K,
Kasai A, Takeda T, Kazama JJ, Narita I and Yoshida K: Crowned dens
syndrome as an initial manifestation of crystalline deposition
disease. Intern Med. 54:2405–2408. 2015.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Conticini E, Di Martino V, De Stefano R,
Frediani B, Volterrani L and Mazzei MA: Crowned dens syndrome
presenting as hemiplegia and hypoesthesia. J Clin Rheumatol: Oct
22, 2019 (Epub ahead of print).
|
|
46
|
Cox TH, Gentle SV and Rees DHE: Crowned
dens syndrome; a diagnostic thorn. Rheumatology (Oxford).
59(694)2019.
|
|
47
|
De Silva T and Rischin A: Crowned dens
syndrome Illustrated by dual energy computed tomography scan. J
Clin Rheumatol: Sep 12, 2019 (Epub ahead of print).
|
|
48
|
Scheldeman L, Van Hoydonck M, Vanheste R,
Theys T and Cypers G: Crowned dens syndrome: A neurologist's
perspective. Acta Neurol Belg. 119:561–565. 2019.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Urits I, Peck J, Chesteen G, Orhurhu V and
Viswanath O: An acute presentation of cervical pain: Crowned dens
syndrome. J Clin Anesth. 58:117–118. 2019.PubMed/NCBI View Article : Google Scholar
|
|
50
|
McCarron EP, Wilson J, Galkin S, Clarke G,
Valley S and Sreenivasan S: Crowned dens syndrome: An easily
overlooked cause of fever and neck stiffness. QJM. 113:52–53.
2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Feydy A, Lioté F, Carlier R, Chevrot A and
Drapé JL: Cervical spine and crystal-associated diseases: Imaging
findings. Eur Radiol. 16:459–468. 2006.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Fenoy AJ, Menezes AH, Donovan KA and
Kralik SF: Calcium pyrophosphate dihydrate crystal deposition in
the craniovertebral junction. J Neurosurg Spine. 8:22–29.
2008.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Sekijima Y, Yoshida T and Ikeda S: CPPD
crystal deposition disease of the cervical spine: A common cause of
acute neck pain encountered in the neurology department. J Neurol
Sci. 296:79–82. 2010.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Zhang W, Doherty M, Bardin T, Barskova V,
Guerne PA, Jansen TL, Leeb BF, Perez-Ruiz F, Pimentao J, Punzi L,
et al: European league against rheumatism recommendations for
calcium pyrophosphate deposition Part I: Terminology and diagnosis.
Ann Rheum Dis. 70:563–570. 2011.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Soma T, Asoda S, Kimura M, Munakata K,
Miyashita H, Nakagawa T and Kawana H: Acute odontogenic infection
combined with crowned dens syndrome: A case report. J Med Case Rep.
13(143)2019.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Goto S, Umehara J, Aizawa T and Kokubun S:
Crowned dens syndrome. J Bone Joint Surg Am. 89:2732–2736.
2007.PubMed/NCBI View Article : Google Scholar
|
|
57
|
D'Aliberti GA, Talamonti G, Villa FG and
Crisà FM: A rare case of cervical junction ligamentous cyst. Acta
Neurochir (Wien). 161:1385–1388. 2019.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Slostad JA, Wild EM, Anderson CM and
Ingram C: Intractable neck pain in a patient with newly diagnosed
AML: An underrecognized cause of a treatable syndrome. J Pain
Symptom Manage. 57:e3–e5. 2019.PubMed/NCBI View Article : Google Scholar
|