1. Introduction
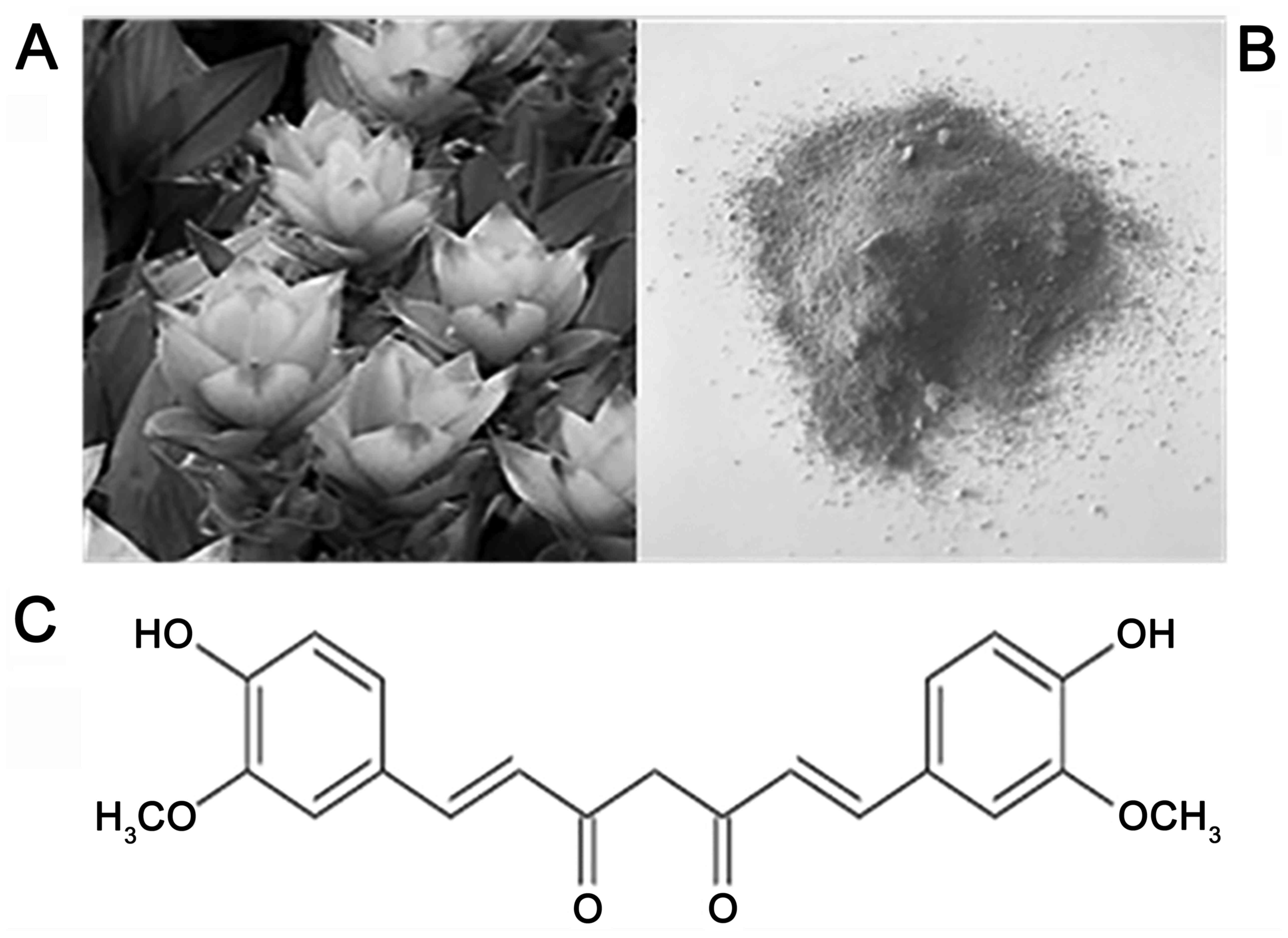
Curcumin: Chemical structure
Curcumin
(1,7-bis[4-hydroxy-3-methoxyphenyl]-1,6-heptadiene-3,5-dione) is a
hydrophobic and insoluble yellowish-orange colored polyphenol and
the major bioactive component of turmeric (Curcuma longa).
It is also known as Diferuloylmethane or E100, in relation to the
European coding of food additives (1). Another term commonly used to refer to
this substance is ‘Curcumin I’ (2).
Considering its pleiotropic action, curcumin belongs to the group
of phytocompounds, which can be defined as biologically active
molecules produced by plants with positive effects on health
(3). In 1815, more than 140 years
ago, Vogel isolated it from the Curcuma longa rhizomes, a
traditional perennial plant belonging to the Zingiberaceae family.
Later, in 1913, Lampe synthesized this molecule (4).
Owing to its anti-inflammatory, antioxidant,
antimicrobial, anti-angiogenesis, antimutagenic and neuroprotection
properties (5-9),
curcumin is considered to be a nutraceutical substance for the
treatment of several chronic diseases t such as diabetes,
atherosclerosis, rheumatism, infectious and oncological diseases
(brain, lung, breast and colon cancer) (10-12).
From a commercial point of view, the most
interesting component of the plant is represented by Curcuma
Longa's roots: Once the rhizomes are boiled and dried in the
sun, they are crushed in order to produce a yellow-orange powder,
whose biologically active compound is curcumin which accounts for
2-5% of turmeric extract (5,13)
(Fig. 1).
Apart from this molecule, demethoxycurcumin (DMC)
and bis-demethoxycurcumin (BDMC) represent the major turmeric
curcuminoids: More specifically, DMC and BDMC present biological
properties quite similar to those of curcumin, being able to
suppress the activity of enzymes such as COX-2, responsible for
nuclear factor-κB (NF-κB) activation. Conversely, the turmeric
volatile fraction includes terpene compounds, such as zingiberene,
curcumol and β-turmerone (14,15).
Curcumin: Properties
The most promising feature of curcumin is its
anti-inflammatory and antioxidant activity: Normally, inflammation
represents a physiological and protective response of the body to a
series of events which can be result in organic damage. Closely
related to inflammation processes is oxidative stress, which is
commonly defined as an imbalance between reactive oxygen species
(ROS) and antioxidant defenses (16).
A situation of persistent oxidative stress can
trigger several inflammatory molecular signaling pathways: For
instance, ROS may lead to an improvement in the NF-κB and the tumor
necrosis factor α (TNF-α) (17,18).
Nowadays, it is assumed that curcumin's anti-inflammatory and
antioxidant properties are mainly related to its hydroxyl and
methoxy groups.
Curcumin leads to deregulation of TNF-α and
proinflammatory interleukins (IL-1, IL-2, IL-6, IL-8 and IL-12)
owing to its ability to down regulate the Janus kinase/signal
transducer and activator of transcription (JAK/STAT) pathway.
Despite all these positive aspects, curcumin
presents some important limitations: First of all, it has extremely
poor bio-availability, supported by evidence that the biologically
active fraction registered in the blood is minimal; secondly, the
need for high levels of the substance (>3.6 g/day in humans) in
order to achieve any therapeutic effects (19).
Curcumin: Limitations of use
Therefore, in order to overcome these strict
limitations, several approaches such as curcumin analogues,
enhancers and delivery systems have been taken into
consideration.
Regarding curcumin analogues, some of the more
promising substances appear to be the pro-drug diphosphorylated
curcumin, which is characterized by a higher molecular stability in
the aqueous media (20), the
curcumin pro-drug curcumin diethyl disuccinate (CurDD) (12) and WZ35, with stronger anti-tumoral
properties (21,22).
‘Bioavailability enhancers’ have been considered
even more encouraging: This definition refers to compounds which
improve substance availability. In the case of curcumin, there has
been a great interest in piperine owing to its ability to decrease
curcumin hepatic and intestinal glucuronidation (23) with consequent augmentation of
curcumin bioavailability. This pharmacological effect was
demonstrated by comparing serum curcumin concentration when given
alone versus administration together with piperine. In this last
case, curcumin blood levels presented a significant increase
(24).
Another field of great interest is represented by
curcumin carriers: For instance, nanoparticles, able to ameliorate
curcumin bioavailability, solubility and stability in aqueous media
(25), liposomes (26), which are spherical bilayer vesicles
with a size approximately between 25-1,000 nm, and polymeric
micelles (27-29).
One of the most encouraging delivery systems for
curcumin is an amphiphilic polymer polyvinyl caprolactam-polyvinyl
acetate-polyethylene glycol graft copolymer (Soluplus®),
which presents both a hydrophilic and a lipophilic component
(25,30).
Unfortunately, it must be clarified that most of
these strategies have not yet been tested in the eye: Nevertheless,
use of a biodegradable curcumin-loaded scleral plug for treatment
of posterior ocular diseases experimented in rabbit eyes represents
an exception, with high levels of curcumin obtained both in
vitro and in vivo (31).
In addition, a further vehicle is Meriva®, a
curcumin-phospholipid lecithin formulation, able to improve visual
acuity and reduce macular edema in DR patients when administered
twice a day as tablets (Norflo®, Eye Pharma, Genoa,
Italy) (32,33).
In ophthalmology, an initial approach with curcumin
was attempted as part of the treatment of complicated chronic
anterior uveitis: An improvement in symptoms was observed after a
12-week treatment dose of 375 mg three times a day (34).
The chemical and biological properties of curcumin
make this substance capable of exerting anti-inflammatory,
antioxidant, antimicrobial and anti-tumorigenic activity. Thanks to
these properties, curcumin has been studied in vitro and
in vivo, also in the context of many inflammatory,
autoimmune, congenital and degenerative eye diseases of both the
anterior and posterior segments, and has been used as an adjuvant
therapy (35-37).
The main problem with the oral use of curcumin is its poor
bioavailability caused by low gastrointestinal absorption and rapid
hepatic and intestinal metabolism. Considering the strong evidence
demonstrating the ‘weakness’ of isolated curcumin as a valid
therapy, the evaluation of holistic approaches that take into
account the chemistry and complexity of the
pharmacodynamics/pharmacokinetics of turmeric and its broad
nutritional basis compared to traditional drugs seems to be the
direction for future research in this field. The purpose of our
work is to identify new aspects that could guide future research on
this important traditional medicine especially in view of the fact
that it is a well-tolerated, natural product, considered safe and
economical.
2. Methodology
For this review, we searched the PubMed database
without language limitations for articles regarding curcumin. Using
the ‘Advanced Search Builder’ tool, the terms ‘curcumin’,
‘inflammation’ and ‘eye diseases’ were used with the terms
‘anti-inflammatory’, ‘retinopathy’, ‘antioxidants’, ‘extracellular
matrix remodeling’, ‘ oxidative stress ‘and’ angiogenesis ‘included
in the title or abstract of the articles. The documents published
up to December 2020 were included. All the publications have been
carefully studied, to select those most relevant to our topic. The
references reported in the selected papers were also examined.
Finally, a web search engine was also used (Google). We have not
used any exclusion criteria for this research
3. Therapeutic effects of curcumin in
retinal diseases
Nowadays, it is well-known that in a wide group of
retinal diseases an inflammatory pathogenesis can be identified:
The retina, considered as part of the central nervous system, is
characterized by the presence of different cell types, including
two types of photoreceptors: Cones, principally located in the
macula lutea, and rods, mostly placed in the retinal periphery.
These cells, along with retinal ganglion cells and retinal pigment
epithelial (RPE) cells, are particularly sensitive to oxidative
stress damage. Recent studies have shown that curcumin protects RPE
from oxidative stress and damage induced by the inflammatory
process by reducing TNF-α levels, recently Bucolo et al
(36) has shown that curcumin
provides protection against damage induced by oxidative stress in
the RPE through activation of Nrf2/HO-1 (nuclear factor erythroid
2-related factor 2/heme oxygenase 1) signaling involving modulation
of the extracellular signal-regulated kinase (ERK) pathway
suggesting that curcumin may have therapeutic value in the
treatment of retinal diseases such as diabetic retinopathy (DR) and
age-related macular degeneration (AMD) (36,37).
More in detail, this nervous tissue is largely subjected to
oxidative stress owing to its intrinsic features, such as
continuous light exposure, which leads to photooxidation mechanism
enhancement. The consequences of this are an improvement of ROS
levels, high vascularization and, finally, a high concentration of
mitochondria. Oxidative stress is the triggering mechanism in a
series of harmful processes: Cell apoptosis, angiogenesis and
inflammation leading to a wide range of retinal pathologies. As
mentioned above, thanks to its pharmacological properties, curcumin
is able to prevent the formation of ROS: Hence it can be properly
used in the prevention and treatment of distinct retinal disorders
as AMD, DR, proliferative vitreoretinopathy (PVR), retinal
ischemia-reperfusion injury (RIRI), retinitis pigmentosa (RP) and
retinal and choroid tumors (1,3,35).
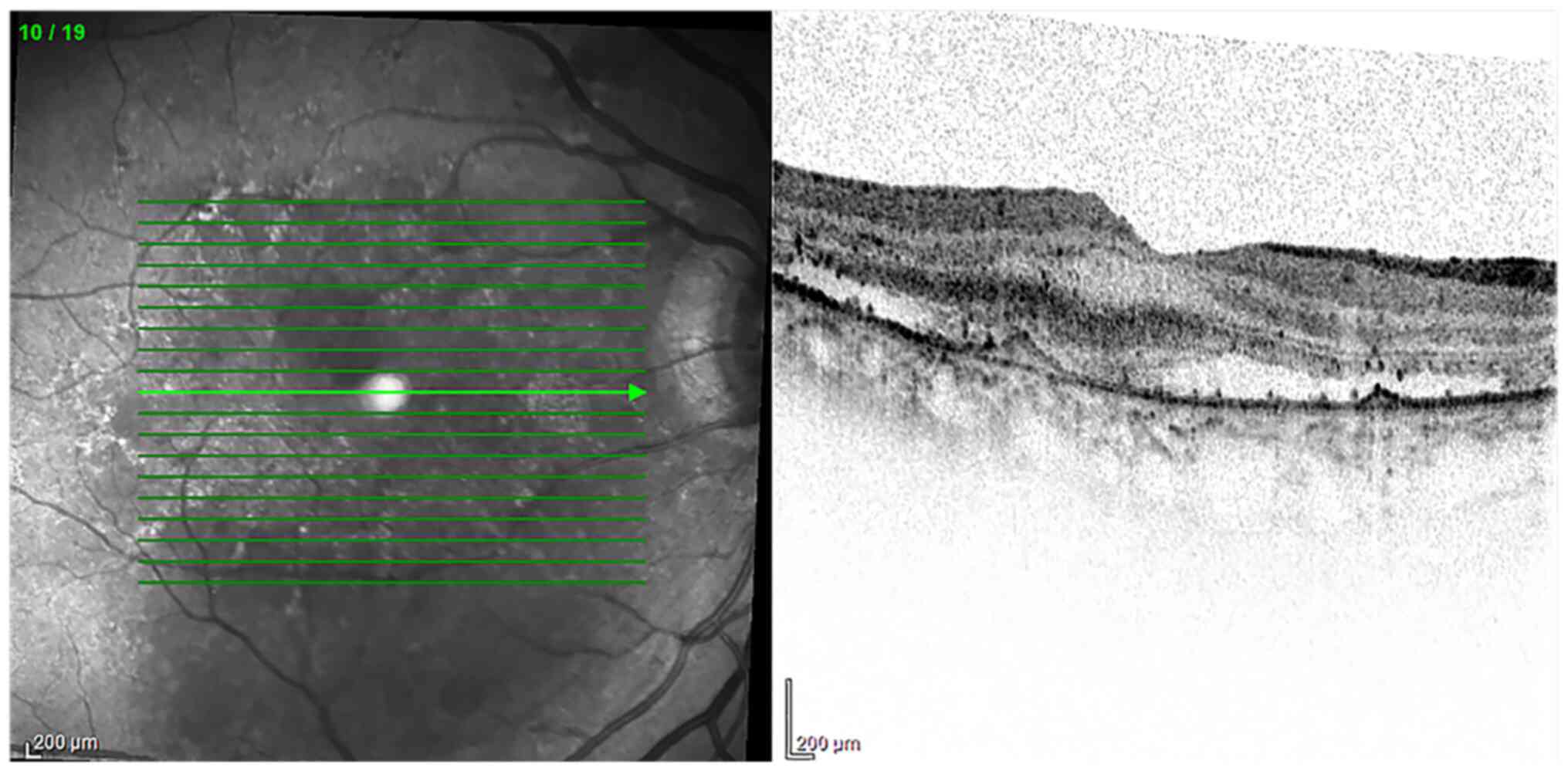
4. AMD
AMD is the most common cause of irreversible
blindness affecting elderly subjects in industrialized countries.
AMD exists in two forms: A non-neovascular one (also defined as
‘dry’ or ‘non-exudative’) and a neovascular one, characterized by
choroidal neovascularization (also known as ‘wet’ or ‘exudative’)
(Fig. 2). From a clinical point of
view, loss of central vision is one of the most characteristic
symptoms referred by patients and is due to progressive macular
degeneration. Currently, no treatment is reported to exist for the
dry form, while the neovascular one is commonly approached with
continued intraocular injections of anti-vascular endothelial
growth factor (anti-VEGF) (38). To
date, AMD pathogenesis remains unclear: Undoubtedly, inflammation
and oxidative stress, along with other risk factors such as aging,
smoking, sun exposure and a poor diet, play a major role in AMD
(39). As is well-known, the macula
is constantly exposed to both oxygen and light and, consequently, a
great amount of ROS is produced in this region. ROS lead to the
activation of a series of distinct pathways such as the mitogen
activated protein kinases, the ERK, the p38 mitogen-activated
protein kinase, and the c-Jun N-terminal kinase (JNK).
Specifically, the cells that are most damaged are the RPE cells,
placed between the choroid and the photoreceptors, leading to AMD
development. RPE cells are deeply involved in supporting the
retina, both being implicated in the photoreceptor outer segments
digestion and in blood-retinal barrier maintenance. Thus, Muangnoi
et al (40) investigated the
protective role of the CurDD against curcumin in relation to
oxidative stress induced in human ARPE-19 cells (Retinal Pigment
Epithelial immortalized cell line derived from Amy Aotaki-Keen
eyes), the most widely used experimental model cells. They showed
that CurDD, like curcumin, is able to downstream a fundamental
apoptotic signaling pathway, known as p44/42 (ERK), with a
consecutive reduction of their effector molecules Bax and Bcl2 in
ARPE-19 cells. Moreover, CurDD revealed a greater protective effect
than curcumin against oxidative stress, thus representing a valid
alternative option for AMD prevention and treatment (36,37,40).
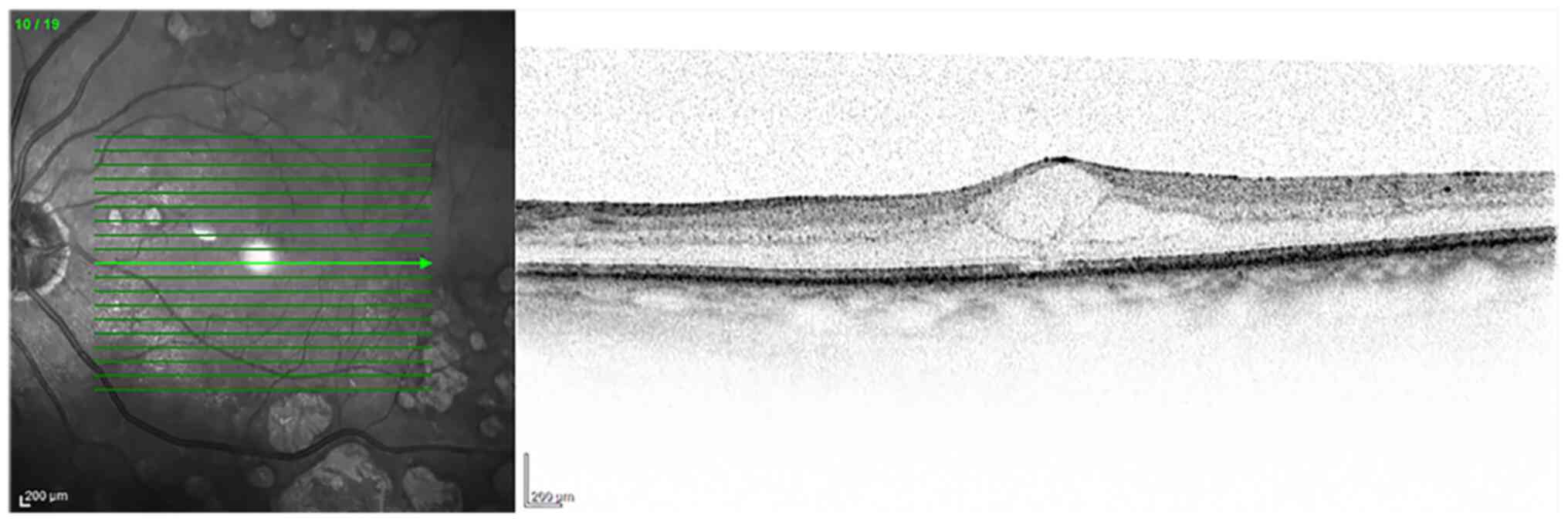
5. DR
DR is considered to be the main cause of
irreversible visual loss all over the world in the working-age
population (41). Clinically, it
can be defined as a metabolic and microvascular disease (42), characterized by a process of chronic
inflammation. Ischemia, microaneurysms, hemorrhages, retinal edema,
neuronal degeneration and neovascularization (43) represent the most indicative
manifestations of DR (Fig. 3).
Depending on neovascularization, two distinct DR
stages can be recognized: Blood flow alterations, pericyte loss and
thickening of the basement membrane define the non-proliferative
diabetic retinopathy, while a sight-threatening neovascularization
is the main feature of the proliferative diabetic retinopathy
(44).
In both cases inflammation and oxidative stress are
the underlying cause of the DR onset and progression determining
damage of photoreceptors and blood vessels with release of cellular
mediators able to stimulate angiogenesis (45). Another factor of extreme importance
in the DR pathogenesis is the oxidative stress induced by
hyperglycemia: Specifically, ROS contribute to the loss of
pericytes leading to microaneurysms and, as a consequence, to the
vascular syndrome of DR (46,47).
Moreover, free radicals favor an increase of
proinflammatory mediators such as VEGF and TNF-α (48,49).
Several studies have been conducted to evaluate the
beneficial effects of curcumin in the case of DR: In 2011 the role
of oral curcumin at doses of 1 g/kg body weight of
streptozotocin-induced diabetic retinopathy in Wistar albino rats
was assessed in terms of prevention and treatment. Particularly,
curcumin revealed a significant hypoglycemic activity and the
ability to positively modulate the antioxidant system, with an
increase of SOD and catalase enzymes. Moreover, a decrease of TNF-α
and VEGF levels was observed (50).
Interestingly, curcumin is able to normalize the
diabetic microvasculature: A decrease in its tortuosity, narrowing
and micro-aneurysms was observed. The beneficial effect of curcumin
treatment on the microvasculature is also demonstrated by the
regeneration and repair mechanisms observed in choroidal
microvasculature after curcumin treatment (51).
6. PVR
PVR is defined as an eye disorder generally
occurring after retinal detachment or re-attachment and often
leading to blindness. It can be defined as a form of wound healing
process induced by the epidermal growth factor and mainly
characterized by RPE cell proliferation and migration. Ren et
al (52) described a
significant reduction of RPE cell proliferation and of vitreous
opacity in the group of patients who received curcumin in
comparison with the control group.
7. RIRI
In the case of RIRI, a pathological process due to a
loss of intraocular perfusion pressure, as a consequence of ocular
hypertension, the protective role of curcumin on retinal neurons
was described by Wang et al (53). They found that curcumin is able to
inhibit both NF-κB and STAT3 (signal transducer and activator of
transcription) and the consequent over-expression of monocyte
chemoattractant protein 1 in Wistar rats (53).
The protective role of curcumin was also observed in
retinal neurons and capillaries in stroke spontaneously
hypertensive rats (SHR), where curcumin is able to down-regulate
the JNK expression (54).
8. RP
Curcumin has also been attempted as an optional
treatment in RP, a group of disorders characterized by a
progressive degeneration of photoreceptors which inexorably leads
to blindness. It can be defined as a heterogeneous disease
including both syndromic and non-syndromic forms and involving a
great number of genes, with different patterns of transmission and
distinct phenotypic presentation (55).
In this regard, a promising discovery was made by
Vasireddy et al (56): The
P23H mutation in the rhodopsin gene determines a rhodopsin
misfolding with the formation of insoluble aggregates. The
consequence of this is a form of autosomal dominant RP. They
observed that the treatment of COS-7 cells expressing mutant
rhodopsin with curcumin leads to aggregate dissociation: In light
of this, they administered curcumin to P23H-rhodopsin transgenic
rats and, in this way, were able to demonstrate the anti-protein,
aggregating activity of curcumin (56).
Curcumin is also able to prevent photoreceptor
apoptosis triggered by the ROS generator methyl-N-nitrosourea (MNU)
tested in a Sprague-Dawley rat model. As highlighted by Emoto et
al (57), the rats firstly
received MNU and were then injected with doses of 100 or 200 mg/kg
of curcumin. A reduction of central retinal damage was observed
(57).
9. Retinal and choroidal tumors
Considering that curcumin's pharmacological
activities have been studied in the treatment of various
oncological diseases, it is not surprising that its use has also
been evaluated in a form of retinal tumor, the retinoblastoma (RB).
The pathogenesis of this retinal cancer is usually due to the
biallelic loss of RB1, a tumor suppressor gene, in association with
both genetic and epigenetic modifications. In particular, one study
highlighted the ability of curcumin to determine RB cell
proliferation and migration as well as induce their apoptosis. The
pathway along which curcumin acts is the JAK/STAT with its
consequent inactivation (58).
Curcumin anti-cancer activity has even been reported in tumors not
directly originating in the retina, such as intraocular lymphoma,
able to cause ocular metastasis (59).
10. COVID and curcumin
The mechanism underlying the effect of curcuminoids
is inhibition and blocking of free radicals before they develop and
spread. Besides the anti-inflammatory and analgesic activity,
antibacterial and antiviral, hepatoprotective, cholesterol-lowering
and antithrombotic activities have also been demonstrated. In the
latter case, the antioxidant activity has proved particularly
effective in limiting oxidative damage to the vessel walls.
Oxidation of the structures of the vessel membranes is in fact one
of the main prerequisites for the formation of a thrombus. The
correlation between inflammatory diseases, such as pneumonia and
thrombosis in general (especially venous), has been known for
decades. In fact patients with any bacterial or viral form of
pneumonia, not necessarily from SARS-CoV-2, are routinely subjected
to thromboembolic prophylaxis with low molecular weight heparin. In
a recent work the authors have addressed the thrombotic
complications in the context of SARS-CoV-2(60).
11. Conclusions
Considering what has been said so far, it clearly
emerges that curcumin, the main polyphenolic compound of the food
flavoring turmeric, has gained significant interest due to its
biological anti-tumoral, antioxidant, immune-modulating,
anti-inflammatory, antiparasitic and antiviral properties (61,62).
For this reason, it has been extensively studied in different
fields of medicine, in general, and particularly, in ophthalmology,
where inflammatory cytokines are involved in the development of
many ocular diseases, such as conjunctivitis, keratitis, uveitis,
glaucoma, age-related macular degeneration and diabetic retinopathy
(63-68).
Since a wide range of beneficial properties have
been identified at different levels, much work still needs to be
done in order to overcome some important limitations inherent to
this substance, such as its bio-availability. Not least, it is
important to emphasize that curcumin is included in the food and
drug category ‘generally regarded as safe’ (69).
In the light of this, curcumin can be also
considered a promising and alternative option in several retinal
diseases: In future perspectives we can expect that from having a
niche role it could gradually assume an increasingly important
position in the treatment of a wide range of both retinal and
ocular diseases.
Acknowledgements
Not applicable.
Funding
Funding: This paper was financially supported by Ministry of
Health (grant no. RC 2765943) and Fondazione Roma.
Availability of data and materials
Not applicable.
Authors' contributions
ST, EA, FF and MN designed the study. TP, GA, AM,
AG, PGL, MA, DAS and FF consulted the literature and collected
bibliographical data. ST and FF wrote the paper. EA and ST reviewed
and edited the manuscript. Data authentication is not applicable.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent for publication of images
was obtained from individuals whose data are included in this
manuscript.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
López-Malo D, Villarón-Casares CA,
Alarcón-Jiménez J, Miranda M, Díaz-Llopis M, Romero FJ and Villar
VM: Curcumin as a Therapeutic Option in Retinal Diseases.
Antioxidants. 9(48)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Anand P, Kunnumakkara AB, Newman RA and
Aggarwal BB: Bioavailability of curcumin: Problems and promises.
Mol Pharm. 4:807–818. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Peddada KV, Brown A, Verma V and Nebbioso
M: Therapeutic potential of curcumin in major retinal pathologies.
Int Ophthalmol. 39:725–734. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Noorafshan A and Ashkani-Esfahani S: A
review of therapeutic effects of curcumin. Curr Pharm Des.
19:2032–2046. 2013.PubMed/NCBI
|
|
5
|
Deogade SC and Ghate S: Curcumin:
Therapeutic applications in systemic and oral health. Int J Biol
Pharm Res. 6:281–290. 2015.
|
|
6
|
Gupta SC, Kismali G and Aggarwal BB:
Curcumin, a component of turmeric: From farm to pharmacy.
Biofactors. 39:2–13. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lestari ML and Indrayanto G: Curcumin.
Profiles Drug Subst Excip Relat Methodol. 39:113–204.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mahady GB, Pendland SL, Yun G and Lu ZZ:
Turmeric (Curcuma longa) and curcumin inhibit the growth of
Helicobacter pylori, a group 1 carcinogen. Anticancer Res.
22:4179–4181. 2002.PubMed/NCBI
|
|
9
|
Reddy DNK, Huang FY, Wang SP and Kumar R:
Synergistic antioxidant and antibacterial activity of curcumin-C3
encapsulated chitosan nanoparticles. Curr Pharm Des. 26:5021–5029.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ammon HP and Wahl MA: Pharmacology of
Curcuma longa. Planta Med. 57:1–7. 1991.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Allegra A, Innao V, Russo S, Gerace D,
Alonci A and Musolino C: Anticancer activity of curcumin and its
analogues: preclinical and clinical studies. Cancer Invest.
35:1–22. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Muangnoi C, Ratnatilaka Na Bhuket P,
Jithavech P, Supasena W, Paraoan L, Patumraj S and Rojsitthisak P:
Curcumin diethyl disuccinate, a prodrug of curcumin, enhances
anti-proliferative effect of curcumin against HepG2 cells via
apoptosis induction. Sci Rep. 9(11718)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Priyadarsini KI: The chemistry of
curcumin: From extraction to therapeutic agent. Molecules.
19:20091–20112. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Guo LY, Cai XF, Lee JJ, Kang SS, Shin EM,
Zhou HY, Jung JW and Kim YS: Comparison of suppressive effects of
demethoxycurcumin and bisdemethoxycurcumin on expressions of
inflammatory mediators in vitro and in vivo. Arch Pharm Res.
31:490–496. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pescosolido N, Giannotti R, Plateroti AM,
Pascarella A and Nebbioso M: Curcumin: Therapeutical potential in
ophthalmology. Planta Med. 80:249–254. 2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Radomska-Leśniewska DM, Osiecka-Iwan A,
Hyc A, Góźdź A, Dąbrowska AM and Skopiński P: Therapeutic potential
of curcumin in eye diseases. Cent Eur J Immunol. 44:181–189.
2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Shishodia S, Sethi G and Aggarwal BB:
Curcumin: Getting back to the roots. Ann N Y Acad Sci.
1056:206–217. 2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Singh S and Aggarwal BB: Activation of
transcription factor NF-kappa B is suppressed by curcumin
(diferuloylmethane) [corrected]. J Biol Chem. 270:24995–25000.
1995.PubMed/NCBI View Article : Google Scholar : Erratum in: J Biol
Chem 270, 30235, 1995.
|
|
19
|
Strimpakos AS and Sharma RA: Curcumin:
Preventive and therapeutic properties in laboratory studies and
clinical trials. Antioxid Redox Signal. 10:511–545. 2008.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wang J, Xiong T, Zhou J, He H, Wu D, Du X,
Li X and Xu B: Enzymatic formation of curcumin in vitro and in
vivo. Nano Res. 11:3453–3461. 2018.
|
|
21
|
Chen T, Zhao L, Chen S, Zheng B, Chen H,
Zeng T, Sun H, Zhong S, Wu W, Lin X, et al: The curcumin analogue
WZ35 affects glycolysis inhibition of gastric cancer cells through
ROS-YAP-JNK pathway. Food Chem Toxicol. 137(111131)2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wang L, Wang C, Tao Z, Zhao L, Zhu Z, Wu
W, He Y, Chen H, Zheng B, Huang X, et al: Curcumin derivative WZ35
inhibits tumor cell growth via ROS-YAP-JNK signaling pathway in
breast cancer. J Exp Clin Cancer Res. 38(460)2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ohori H, Yamakoshi H, Tomizawa M, Shibuya
M, Kakudo Y, Takahashi A, Takahashi S, Kato S, Suzuki T, Ishioka C,
et al: Synthesis and biological analysis of new curcumin analogues
bearing an enhanced potential for the medicinal treatment of
cancer. Mol Cancer Ther. 5:2563–2571. 2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Shoba G, Joy D, Joseph T, Majeed M,
Rajendran R and Srinivas PS: Influence of piperine on the
pharmacokinetics of curcumin in animals and human volunteers.
Planta Med. 64:353–356. 1998.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Li M, Xin M, Guo C, Lin G and Wu X: New
nanomicelle curcumin formulation for ocular delivery: Improved
stability, solubility, and ocular anti-inflammatory treatment. Drug
Dev Ind Pharm. 43:1846–1857. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Barenholz Y: Doxil® - the first
FDA-approved nano-drug: Lessons learned. J Control Release.
160:117–134. 2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Zhang W, Ma W, Zhang J, Song X, Sun W and
Fan Y: The immunoregulatory activities of astragalus polysaccharide
liposome on macrophages and dendritic cells. Int J Biol Macromol.
105:852–861. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Cabral H and Kataoka K: Progress of
drug-loaded polymeric micelles into clinical studies. J Control
Release. 190:465–476. 2014.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sai N, Dong X, Huang P, You L, Yang C, Liu
Y, Wang W, Wu H, Yu Y, Du Y, et al: A novel gel-forming solution
based on PEG-DSPE/Solutol HS 15 mixed micelles and Gellan gum for
ophthalmic delivery of curcumin. Molecules. 25(25)2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chen Y, Lu Y, Lee RJ and Xiang G: Nano
encapsulated curcumin: and its potential for biomedical
applications. Int J Nanomedicine. 15:3099–3120. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Zhang J, Sun H, Zhou N, Zhang B and Ma J:
Preparation and evaluation of biodegradable scleral plug containing
curcumin in rabbit eye. Curr Eye Res. 42:1597–1603. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Mazzolani F, Togni S, Giacomelli L,
Eggenhoffner R and Franceschi F: Oral administration of a
curcumin-phospholipid formulation (Meriva®) for
treatment of chronic diabetic macular edema: A pilot study. Eur Rev
Med Pharmacol Sci. 22:3617–3625. 2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Steigerwalt R, Nebbioso M, Appendino G,
Belcaro G, Ciammaichella G, Cornelli U, Luzzi R, Togni S, Dugall M,
Cesarone MR, et al: Meriva®, a lecithinized curcumin
delivery system, in diabetic microangiopathy and retinopathy.
Panminerva Med. 54 (Suppl 4):11–16. 2012.PubMed/NCBI
|
|
34
|
Lal B, Kapoor AK, Asthana OP, Agrawal PK,
Prasad R, Kumar P and Srimal RC: Efficacy of curcumin in the
management of chronic anterior uveitis. Phytother Res. 13:318–322.
1999.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Wang LL, Sun Y, Huang K and Zheng L:
Curcumin, a potential therapeutic candidate for retinal diseases.
Mol Nutr Food Res. 57:1557–1568. 2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Bucolo C, Drago F, Maisto R, Romano GL,
D'Agata V, Maugeri G and Giunta S: Curcumin prevents high glucose
damage in retinal pigment epithelial cells through ERK1/2-mediated
activation of the Nrf2/HO-1 pathway. J Cell Physiol.
234:17295–17304. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Pittalà V, Fidilio A, Lazzara F, Platania
CBM, Salerno L, Foresti R, Drago F and Bucolo C: Effects of novel
nitric oxide-releasing molecules against oxidative stress on
retinal pigmented epithelial cells. Oxid Med Cell Longev.
2017(1420892)2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Yonekawa Y, Miller JW and Kim IK:
Age-related macular degeneration: advances in management and
diagnosis. J Clin Med. 4:343–359. 2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ulańczyk Z, Grabowicz A, Cecerska-Heryć E,
Śleboda-Taront D, Krytkowska E, Mozolewska-Piotrowska K, Safranow
K, Kawa MP, Dołęgowska B and Machalińska A: Dietary and lifestyle
factors modulate the activity of the endogenous antioxidant system
in patients with age-related macular degeneration: correlations
with disease severity. Antioxidants. 9(9)2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Muangnoi C, Sharif U, Ratnatilaka Na
Bhuket P, Rojsitthisak P and Paraoan L: Protective effects of
curcumin ester prodrug, curcumin diethyl disuccinate against
H2O2-induced oxidative stress in human
retinal pigment epithelial cells: potential therapeutic avenues for
age-related macular degeneration. Int J Mol Sci.
20(20)2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Yau JW, Rogers SL, Kawasaki R, Lamoureux
EL, Kowalski JW, Bek T, Chen SJ, Dekker JM, Fletcher A, Grauslund
J, et al: Meta-Analysis for Eye Disease (META-EYE) Study Group:
Global prevalence and major risk factors of diabetic retinopathy.
Diabetes Care. 35:556–564. 2012.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Antonetti DA, Klein R and Gardner TW:
Diabetic retinopathy. N Engl J Med. 366:1227–1239. 2012.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Platania CBM, Fidilio A, Lazzara F, Piazza
C, Geraci F, Giurdanella G, Leggio GM, Salomone S, Drago F and
Bucolo C: Retinal protection and distribution of curcumin in vitro
and in vivo. Front Pharmacol. 9(670)2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Roy S, Maiello M and Lorenzi M: Increased
expression of basement membrane collagen in human diabetic
retinopathy. J Clin Invest. 93:438–442. 1994.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Barber AJ: Diabetic retinopathy: Recent
advances towards understanding neurodegeneration and vision loss.
Sci China Life Sci. 58:541–549. 2015.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Wan TT, Li XF, Sun YM, Li YB and Su Y:
Recent advances in understanding the biochemical and molecular
mechanism of diabetic retinopathy. Biomed Pharmacother. 74:145–147.
2015.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Wu Y, Tang L and Chen B: Oxidative stress:
Implications for the development of diabetic retinopathy and
antioxidant therapeutic perspectives. Oxid Med Cell Longev.
2014(752387)2014.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Aiello LP, Pierce EA, Foley ED, Takagi H,
Chen H, Riddle L, Ferrara N, King GL and Smith LE: Suppression of
retinal neovascularization in vivo by inhibition of vascular
endothelial growth factor (VEGF) using soluble VEGF-receptor
chimeric proteins. Proc Natl Acad Sci USA. 92:10457–10461.
1995.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Limb GA, Soomro H, Janikoun S, Hollifield
RD and Shilling J: Evidence for control of tumour necrosis
factor-alpha (TNF-alpha) activity by TNF receptors in patients with
proliferative diabetic retinopathy. Clin Exp Immunol. 115:409–414.
1999.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Gupta SK, Kumar B, Nag TC, Agrawal SS,
Agrawal R, Agrawal P, Saxena R and Srivastava S: Curcumin prevents
experimental diabetic retinopathy in rats through its hypoglycemic,
antioxidant, and anti-inflammatory mechanisms. J Ocul Pharmacol
Ther. 27:123–130. 2011.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Khimmaktong W, Petpiboolthai H, Sriya P
and Anupunpisit V: Effects of curcumin on restoration and
improvement of microvasculature characteristic in diabetic rat's
choroid of eye. J Med Assoc Thai. 97 (Suppl 2):S39–S46.
2014.PubMed/NCBI
|
|
52
|
Ren YX, Ma JX, Zhao F, An JB, Geng YX and
Liu LY: Effects of Curcumin on Epidermal Growth Factor in
Proliferative Vitreoretinopathy. Cell Physiol Biochem.
47:2136–2146. 2018.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Wang L, Li C, Guo H, Kern TS, Huang K and
Zheng L: Curcumin inhibits neuronal and vascular degeneration in
retina after ischemia and reperfusion injury. PLoS One.
6(e23194)2011.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Wang S, Ye Q, Tu J, Zhang M and Ji B:
Curcumin protects against hypertension aggravated retinal
ischemia/reperfusion in a rat stroke model. Clin Exp Hypertens.
39:711–717. 2017.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Limoli PG, Vingolo EM, Limoli C and
Nebbioso M: stem cell surgery and growth factors in retinitis
pigmentosa patients: Pilot study after literature review.
Biomedicines. 7(7)2019.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Vasireddy V, Chavali VR, Joseph VT, Kadam
R, Lin JH, Jamison JA, Kompella UB, Reddy GB and Ayyagari R: Rescue
of photoreceptor degeneration by curcumin in transgenic rats with
P23H rhodopsin mutation. PLoS One. 6(e21193)2011.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Emoto Y, Yoshizawa K, Uehara N, Kinoshita
Y, Yuri T, Shikata N and Tsubura A: Curcumin suppresses
N-methyl-N-nitrosourea-induced photoreceptor apoptosis in
Sprague-Dawley rats. In Vivo. 27:583–590. 2013.PubMed/NCBI
|
|
58
|
Li Y, Sun W, Han N, Zou Y and Yin D:
Curcumin inhibits proliferation, migration, invasion and promotes
apoptosis of retinoblastoma cell lines through modulation of
miR-99a and JAK/STAT pathway. BMC Cancer. 18(1230)2018.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Bar-Sela G, Epelbaum R and Schaffer M:
Curcumin as an anti-cancer agent: Review of the gap between basic
and clinical applications. Curr Med Chem. 17:190–197.
2010.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Burlacu A, Genovesi S, Popa IV and
Crisan-Dabija R: Unpuzzling COVID-19 prothrombotic state: are
preexisting thrombophilic risk profiles responsible for
heterogenous thrombotic events? Clin Appl Thromb Hemost.
26(1076029620952884)2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Moghadamtousi SZ, Kadir HA, Hassandarvish
P, Tajik H, Abubakar S and Zandi K: A review on antibacterial,
antiviral, and antifungal activity of curcumin. Biomed Res Int.
2014(186864)2014.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Praditya D, Kirchhoff L, Brüning J,
Rachmawati H, Steinmann J and Steinmann E: Anti-infective
properties of the golden spice curcumin. Front Microbiol.
10(912)2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Taurone S, Ripandelli G, Pacella E,
Bianchi E, Plateroti AM, De Vito S, Plateroti P, Grippaudo FR,
Cavallotti C and Artico M: Potential regulatory molecules in the
human trabecular meshwork of patients with glaucoma:
Immunohistochemical profile of a number of inflammatory cytokines.
Mol Med Rep. 11:1384–1390. 2015.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Stanton CM and Wright AF: Inflammatory
biomarkers for AMD. Adv Exp Med Biol. 801:251–257. 2014.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Abcouwer SF: Angiogenic factors and
cytokinesin diabetic retinopathy. J Clin Cell Immunol Suppl.
1:1–12. 2013.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Chua J, Vania M, Cheung CM, Ang M, Chee
SP, Yang H, Li J and Wong TT: Expression profile of inflammatory
cytokines in aqueous from glaucomatous eyes. Mol Vis. 18:431–438.
2012.PubMed/NCBI
|
|
67
|
Bianchi E, Ripandelli G, Feher J,
Plateroti AM, Plateroti R, Kovacs I, Plateroti P, Taurone S and
Artico M: Occlusion of retinal capillaries caused by glial cell
proliferation in chronic ocular inflammation. Folia Morphol
(Warsz). 74:33–41. 2015.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Taurone S, Ralli M, Nebbioso M, Greco A,
Artico M, Attanasio G, Gharbiya M, Plateroti AM, Zamai L and Micera
A: The role of inflammation in diabetic retinopathy: A review. Eur
Rev Med Pharmacol Sci. 24:10319–10329. 2020.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Aggarwal BB and Harikumar KB: Potential
therapeutic effects of curcumin, the anti-inflammatory agent,
against neurodegenerative, cardiovascular, pulmonary, metabolic,
autoimmune and neoplastic diseases. Int J Biochem Cell Biol.
41:40–59. 2009.PubMed/NCBI View Article : Google Scholar
|