Introduction
Ischemic heart disease (IHD) is a threat to human
health (1,2), and the key to treating IHD is to
restore blood supply to the ischemic myocardium as soon as possible
(3). However, restoration of blood
supply is inevitably accompanied by subsequent cardiac injury,
which is widely recognized as myocardial ischemia reperfusion
(MI/R) injury (1,4,5). Since
IHD became the leading cause of death in patients with type 1
diabetes (6), the MI/R injury in
diabetes has attracted widespread attention. Epidemiological data
have demonstrated that the incidence rate of ischemic
cardiomyopathy among patients with diabetes is ~4-fold higher than
that among patients without diabetes (7). Patients with diabetes are more
susceptible to MI/R injury (8,9), with
worse clinical prognosis and higher fatality rate compared with
patients without diabetes (10,11).
Therefore, it is necessary to implement new strategies to prevent
MI/R injury in patients with diabetes to improve the effectiveness
diabetic IHD treatment.
Naringenin (Nar) is a naturally occurring flavanone,
predominantly derived from citrus fruits. Nar plays a biological
role in the human body (12), and
is known to exert cardioprotective effects (13). Nar prevents doxorubicin-induced
toxicity, including apoptosis and oxidative stress in
cardiomyoblasts (14-17).
In addition, Nar antagonizes hypercholesterolemia-induced cardiac
oxidative stress and subsequent necroptosis in rats (18). Although a few studies have confirmed
that Nar is able to attenuate MI/R injury (19,20),
to the best of our knowledge, whether Nar counteracts MI/R injury
in diabetes has not yet been clarified. It has been reported that
Nar protects cardiomyocytes against hyperglycemia-induced injury
(21). Therefore, in the present
study, streptozotocin (STZ)-induced diabetic rats were exposed to
MI/R to construct a model of diabetic MI/R (D-MI/R) injury, and to
explore whether Nar has a potential therapeutic function.
The PI3K/AKT signaling pathway plays a critical
protective role in MI/R injury (22). In the myocardium, the PI3K/AKT
signaling pathway indirectly regulates the contraction of the
cardiac muscle and the function of calcium channels (23). Accumulating evidence has
demonstrated that the PI3K/AKT signaling pathway is impaired during
MI/R injury, and that MI/R injury can be ameliorated by activation
of the PI3K/AKT signaling pathway (24-26).
These previous studies provided evidence that activated PI3K/AKT
signaling may improve MI/R injury. Therefore, the present study
investigated whether the PI3K/AKT signaling pathway is involved in
the protective effect of Nar against MI/R injury in diabetes.
MicroRNA-126 (miR-126) is involved in the
pathophysiological processes of various cardiovascular diseases,
particularly MI/R injury (27-29).
It has been demonstrated that miR-126 attenuates oxidative stress
and apoptosis induced by MI/R injury in rats (27,28).
Notably, miR-126 may be a therapeutic agent for diabetes mellitus
(30). Diabetes reduces miR-126
expression and angiogenesis in the myocardium compared with healthy
rats, while enhancement of myocardial miR-126 level significantly
improves myocardial angiogenesis in diabetic rats (31). Therefore, although an association
between Nar and miR-126 has not been reported to date, the
aforementioned studies led to a hypothesis that miR-126 may be
involved in the protective effects of Nar against MI/R injury in
diabetes.
The present study aimed to explore whether Nar
antagonizes MI/R-injury in diabetic rats and whether
miR-126-PI3K/AKT are involved in this protective effect. The
results of the present study demonstrated that Nar significantly
ameliorated MI/R injury and enhanced the myocardial
miR-126-PI3K/AKT axis in rats with D-MI/R. The results suggest that
Nar alleviated MI/R injury via enhancing the myocardial
miR-126-PI3K/AKT axis in STZ-induced diabetic rats.
Materials and methods
Reagents
STZ, Nar, ketamine, xylazine and an MTT kit were
supplied by Sigma-Aldrich; Merck KGaA. The BCA protein assay kit
was obtained from Dojindo Molecular Technologies, Inc. Lactate
dehydrogenase (LDH) and creatine kinase myocardial band (CK-MB)
measurement kits were obtained from the Nanjing Jiancheng
Bioengineering Institute. The assay kits for glutathione peroxidase
(GSH-Px), superoxide dismutase (SOD), malondialdehyde (MDA),
8-hydroxy-2 deoxyguanosine (8-OHdG) and H2O2
measurement were purchased from Wuhan USCN Business Co., Ltd.
Specific monoclonal antibodies against phosphorylated (p)-PI3K
(cat. no. 4228), PI3K (cat. no. 4255), p-AKT (cat. no. 9271), AKT
(cat. no. 9272) and GAPDH (cat. no. 2118), Anti-rabbit
IgG-HRP-linked Antibody (cat. no. 7074) were supplied by Cell
Signaling Technology, Inc.
Animals
A total of 50 adult male Sprague-Dawley rats (age,
8-10 weeks; weight, 250±10 g) were supplied by Guangdong Medical
Laboratory Animal Center. Rats were raised in single cages
(individually) in a specific-pathogen-free environment under a 12-h
light/dark cycle (light exposure, 7:00 a.m.-7:00 p.m.), and
maintained at a constant temperature (22±2˚C), ventilation and
humidity (50%). Rats were provided with food and water ad
libitum, and the bedding was changed 1-2 times a week to ensure
a suitable environment for the rats.
Induction of diabetes
STZ was dissolved in 0.1 mol/l sodium citrate buffer
(pH 4.3) and used immediately after preparation, which was
performed in a cold (4-6˚C) and dark environment. After overnight
(12-h) fasting, the rats were weighed. The STZ-treated groups
received a single intraperitoneal (i.p.) injection of STZ (55
mg/kg), while the other groups received an equivalent dose of PBS
(i.p.). The rats were administered food 1 h after STZ injection. A
total of 72 h after the STZ injection, Baseline body weight and
blood glucose level were measured in all the rats. After STZ or PBS
injection, blood glucose levels at day 3 and day 30 were determined
measured using a glucometer (Roche Applied Science), and body
weights were measured once a week. Only animals with fasting blood
glucose levels >16.7 mmol/l at 3 days after STZ injection were
considered diabetic and ~80 rats used for further experiments
(32). Finally, six of the rats did
not reach their target levels of blood glucose, which were
supplemented with STZ (10-20 mg/kg) 3 days later. Failing that,
diabetic induction was repeated from scratch once blood glucose
levels had returned to normal.
Experimental protocol
After a week of adaptation to the experimental
environment, then 3 days after the STZ or PBS injection, the rats
were randomly divided into the following five groups (10 rats in
each group) and were provided with the following treatments: i)
Control-sham group (C-S), non-diabetic rats that received sham
surgery; ii) diabetes-sham group (D-S), diabetic rats that received
sham surgery; iii) D-MI/R group, diabetic rats that were orally
treated with vehicle (distilled water, 1.5 ml) for 30 days, and
then subjected to MI/R injury; iv) D-MI/R + low-dose Nar (LN)
group, diabetic rats that were orally treated with Nar (25
mg/kg/day; diluted in distilled water) for 30 days and then
subjected to I/R injury; and v) D-MI/R + high-dose Nar (HN) group,
diabetic rats that were orally treated with Nar (50 mg/kg/day;
diluted in sterile water) for 30 days and then subjected to I/R
injury.
MI/R modeling
After the aforementioned 4 weeks of treatment with
Nar or distilled water, the hearts of the rats were isolated and
perfused according to a previously described protocol (33,34).
Briefly, the each rat were heparinized (500 IU) to avoid blood
clotting during surgery and then anesthetized with ketamine (60
mg/kg; i.p.) and xylazine (10 mg/kg; i.p.). Subsequently, the
hearts were rapidly excised and immediately perfused on a
Langendorff device (ADInstruments, Ltd.) with modified
Krebs-Henseleit solution (pH 7.4; 37˚C) containing 118 mmol/l NaCl,
4.7 mmol/l KCl, 1.25 mmol/l CaCl2, 1.2 mmol/l
MgSO4, 25 mmol/l NaHCO3, 1.2 mmol/l
KH2PO4 and 11 mmol/l glucose, saturated with
95% O2 and 5% CO2. Upon stabilization, the
hearts were subjected to 30-min regional ischemia by tightening a
5-0 silk suture around the left anterior descending coronary artery
and reperfusion for 120 min. The sham groups underwent sham surgery
(the left anterior descending coronary artery was not ligated) in
which the heart was exteriorized without MI/R injury.
Evaluating myocardial systolic and
diastolic functions
For measurement of interventricular pressure
changes, a water-filled latex balloon was inserted into the left
ventricle, and the signals were delivered to the associated
transducer through a connecting pressure catheter. After
reperfusion, the cardiac function index, including left ventricular
systolic pressure (LVSP), left ventricular end-diastolic pressure
(LVEDP) and left ventricular maximal systolic/diastolic velocity
(±dP/dtmax, +dP/dtmax = the maximum rate of
pressure rise in the left ventricle; -dP/dtmax = the
maximum rate of pressure drop in the left ventricle), were recorded
using a hemodynamic monitoring system (PowerLab-PL3508;
ADInstruments, Ltd.).
Measurement of cardiac tissue
viability, and CK and LDH levels
After reperfusion, the hearts were cut into
2-mm-thick sections and incubated with MTT (3 mM) at 37˚C for 30
min to form formazan (34). Based
on previous study, cardiac tissue viability was measured by the
level of formazan using a spectrophotometer at 550 nm (34). In addition, at 5 min after
reperfusion, the coronary effluent was collected for the
determination of cardiac CK-MB and LDH activities, which are two
major indicators of MI/R injury, by spectrophotometry using the
aforementioned commercial assay kits according to a previously
described protocol (35). The
activities of these two enzymes were expressed as U/l.
Mitochondrial oxidative stress
quantification
After reperfusion, the myocardial tissue was
homogenized (10% w/v) in 0.1 mol/l PBS and centrifuged at 12,000 x
g for 10 min at 4˚C. Subsequently, the supernatant was collected,
and the protein concentration was quantified using the
aforementioned BCA protein assay. As previously described (36,37),
the activities of GSH-Px and SOD, the levels of MDA and 8-OHdG, and
H2O2 formation in the supernatant were
determined by spectrophotometry using the aforementioned
commercially available kits.
Western blot analysis
The protein levels of p-PI3K, PI3K, p-AKT and AKT
were measured by western blotting. After reperfusion, myocardial
tissue was homogenized in ice-cold homogenizing buffer [20 mM
Tris-Cl (pH 7.4), 150 mM NaCl, 1 mM EDTA, 1% Triton X-100 and 1 mM
phenylmethanesulfonyl fluoride). After centrifugation at 12,000 x g
for 30 min at 4˚C, the supernatant was collected and the protein
concentration was analyzed using a BCA protein assay kit (Beyotime
Institute of Biotechnology). Approximately 10 µg of protein for
each sample were resolved by SDS-PAGE (8-12%) and transferred onto
PVDF membranes by electroblotting. Non-specific protein binding was
blocked with TBS-Tween-20 [TBS-T; 50 mmol/l Tris-HCl (pH 7.5), 150
mmol/l NaCl and 0.05% Tween-20] containing 5% non-fat milk for 2 h
at room temperature, and the membranes were incubated overnight at
4˚C with the aforementioned primary antibodies (P-PI3K, PI3K,
P-AKT, AKT, GAPDH; dilution, 1:1,000). After the membranes were
washed three times with TBS-T buffer, the blots were incubated with
a horseradish peroxidase-conjugated anti-rabbit secondary antibody
(1:5,000) for 2 h at 4˚C. Subsequently, the membranes were washed
with TBS-T buffer (five times for 5 min each) and electrogenerated
chemiluminescence reaction solution (SuperSignal™ West Pico PLUS
Chemiluminescent Substrate-A38555; Thermo Fisher Scientific, Inc.)
was added for 30 sec. The protein bands were visualized using a
Tanon-5600 Imaging System (Tanon Science and Technology Co., Ltd.).
The semi-quantitative analysis of each blot was performed using
SigmaScan Pro 5.0 software (Systat Software, Inc) and expression
values were normalized to that of GAPDH.
Reverse transcription-quantitative PCR
(RT-qPCR)
The myocardial miR-126 level was measured by RT-qPCR
as previously described (28).
Briefly, total RNA from the myocardial tissue of rats was isolated
using the TRIzol® reagent (Thermo Fisher Scientific,
Inc.). Next, miRNA-specific stem-loop primers were reverse
transcribed to cDNA according to the instructions of the miRNA RT
kit (Takara Biotechnology Co., Ltd.). RT reaction conditions were
processed at 42˚C for 15 min, followed by 3 min at 95˚C. qPCR was
performed using SYBR Premix Ex Taq™ according to the manufacturer's
instructions (Takara Biotechnology Co., Ltd.). The following PCR
protocol was used: 95˚C for 10 min, followed by 40 cycles of 95 ˚C
for 15 sec and 60 ˚C for 1 min. The 2-ΔΔCq method
(38) was used to calculate the
relative expression levels of miR-126 and U6 was used as an
internal reference. The sequences of the primers (Beyotime
Institute of Biotechnology) used were as follows: miR-126 forward,
5'-ACTGTCACTCTCATCACAAGCGC-3' and reverse,
5'-ACGCTGGCTCAGGGATCAGAGA-3'; and U6 forward,
5'-CTCGCTTCGGCAGCACA-3' and reverse,
5'-AACGCTTCACGAATTTGCGT-3'.
Statistical analysis
All experiments were repeated ≥3 times, and
statistical analyses were performed using SPSS 20.0 software (IBM
Corp.). Data are presented as the mean ± SEM, and differences
between groups were assessed using one-way analysis of variance and
Tukey's post hoc test. Repeated measurement data were analyzed
using mixed ANOVA and a Tukey's post-hoc test for simple main
effects. Two-tailed P<0.05 was considered to indicate a
statistically significant difference.
Results
Nar does not affect blood glucose
levels or body weight in STZ-induced diabetic rats
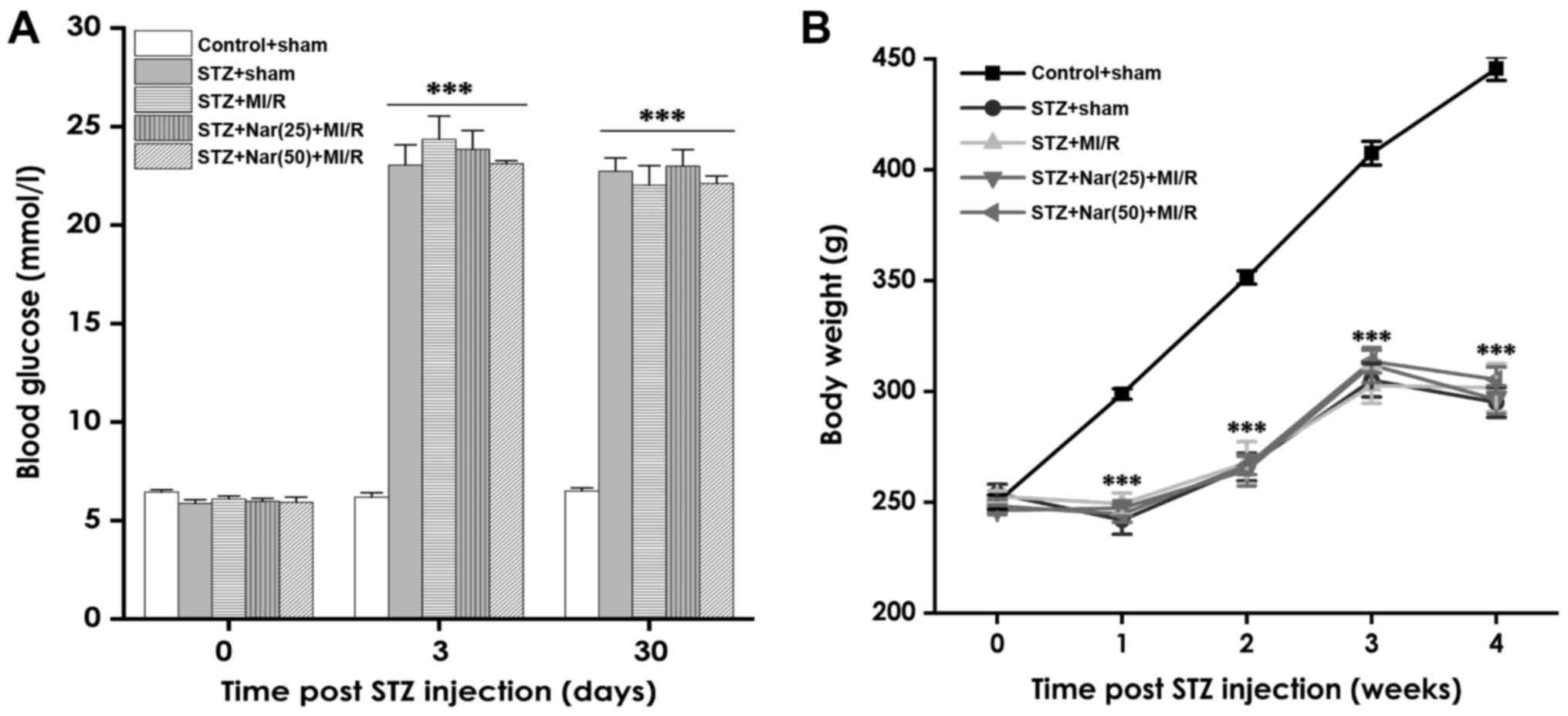
Blood sugar levels and weight were regularly
measured in diabetic rats to determine whether Nar had an effect on
these parameters. The blood glucose level of the diabetic groups
was significantly higher than that of the control group 3 days
after STZ injection (Fig. 1A). At
day 30, the blood glucose levels in the four diabetic groups
remained high, and there was no significant difference in blood
glucose levels between STZ-treated rats and rats co-treated with
STZ and Nar (Fig. 1A).
Body weight was measured once a week
after STZ or PBS injection
The body weight of STZ-induced diabetic rats was
significantly reduced compared with that of the control group. In
addition, there were no significant differences in body weight
between STZ-treated rats and rats co-treated with STZ and Nar
(Fig. 1B). These data indicate that
STZ injection resulted in a diabetic status in rats, and that Nar
did not affect the blood glucose level or body weight of diabetic
rats.
Nar decreases myocardial enzyme
content and enhances cardiac tissue viability in D-MI/R rats
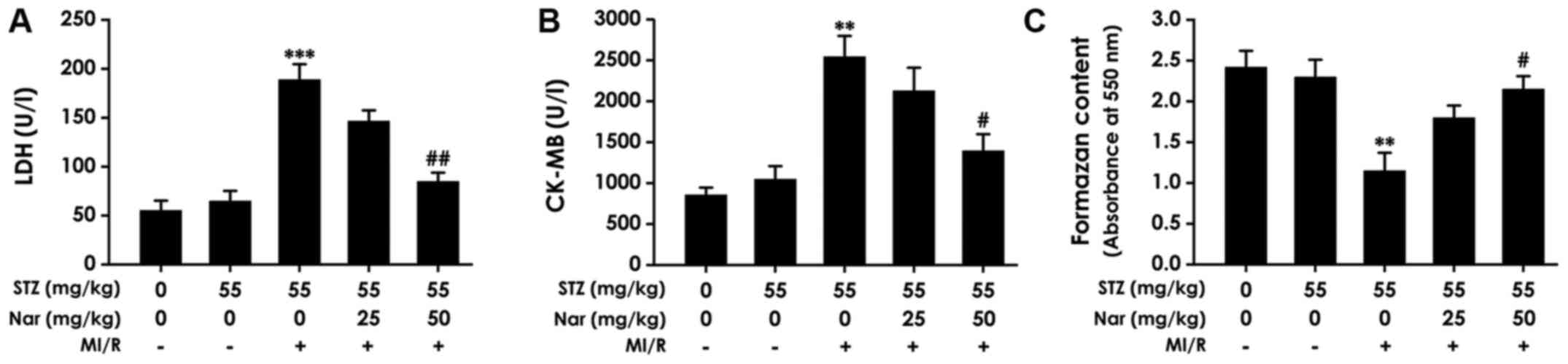
To determine if Nar alleviated MI/R injury in
diabetic rats, the present study first explored whether Nar
decreased myocardial enzyme levels and enhanced cardiac tissue
viability by observing the effects of Nar on the levels of LDH and
CK-MB in the coronary effluent, and the viability of heart tissues
in D-MI/R rats. The results showed that HN significantly
downregulated the levels of LDH and CK-MB (Fig. 2A and B) in the coronary effluent, and increased
the cardiac formazan content (Fig.
2C) in D-MI/R rats compared with that in the untreated D-MI/R
group. Moreover, there was no significant difference in the levels
of LDH, CK-MB or formazan content between the C-S and D-S groups.
These data indicate that Nar decreased the myocardial enzyme
content and increased cardiac tissue viability in D-MI/R rats.
Nar inhibits myocardial oxidative
stress in D-MI/R rats
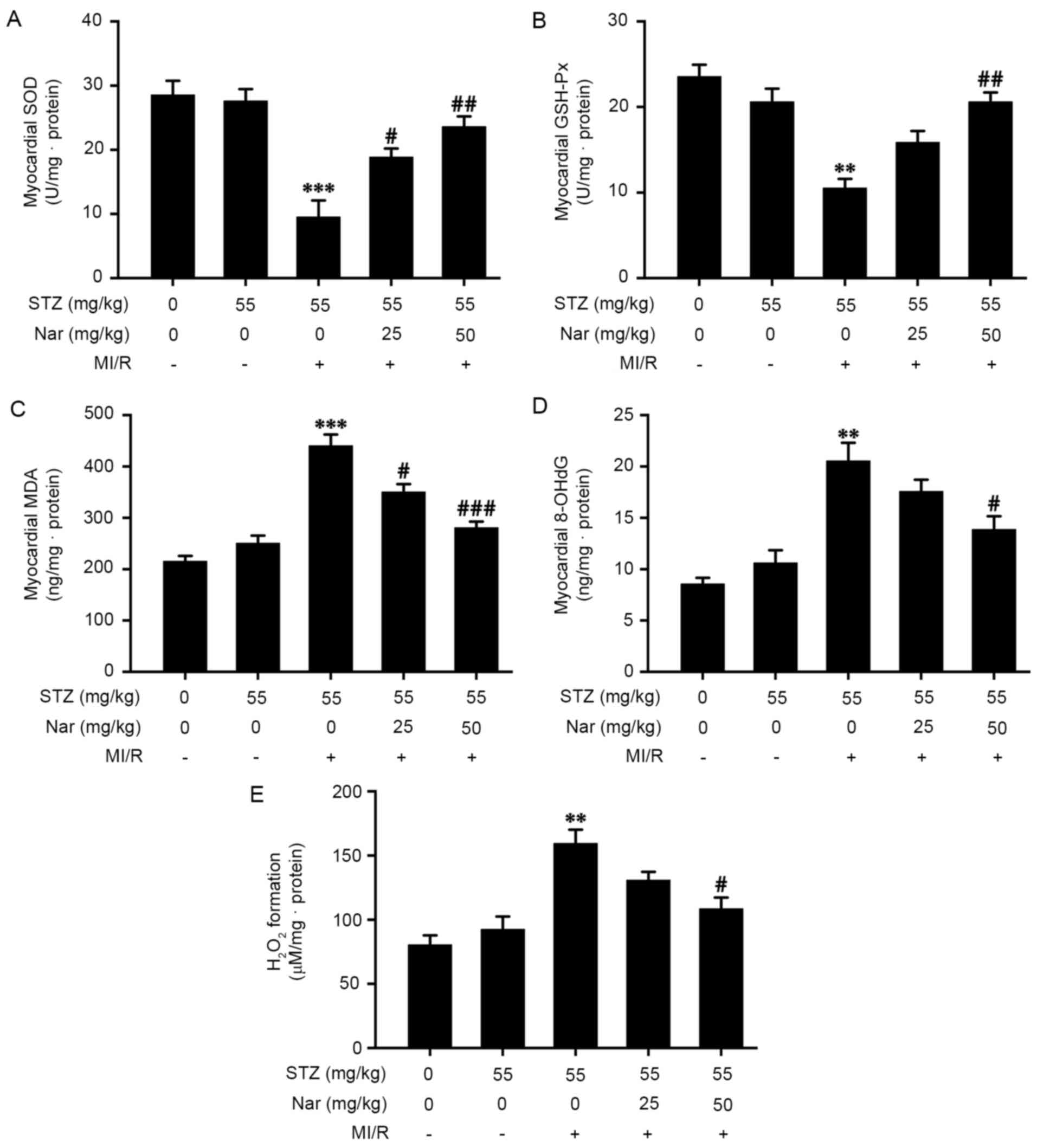
To confirm that Nar alleviates MI/R injury in
diabetic rats, the present study investigated whether Nar
antagonized myocardial oxidative stress by observing the effects of
Nar on the activity of GSH-Px and SOD, and the levels of MDA,
8-OHdG and H2O2 in the myocardium of D-MI/R
rats. In the D-MI/R group, upregulation in the content of MDA,
8-OHdG and H2O2, and downregulation in the
activities of GSH-Px and SOD in the myocardium of D-MI/R rats were
observed, compared with the D-S group, while these effects were
markedly reversed by pretreatment with Nar (Fig. 3A-E). Furthermore, there was no
significant difference in myocardial oxidative stress indexes
between the C-S and D-S groups. These data indicated that Nar
inhibited myocardial oxidative stress in D-MI/R rats (Fig. 3A-E).
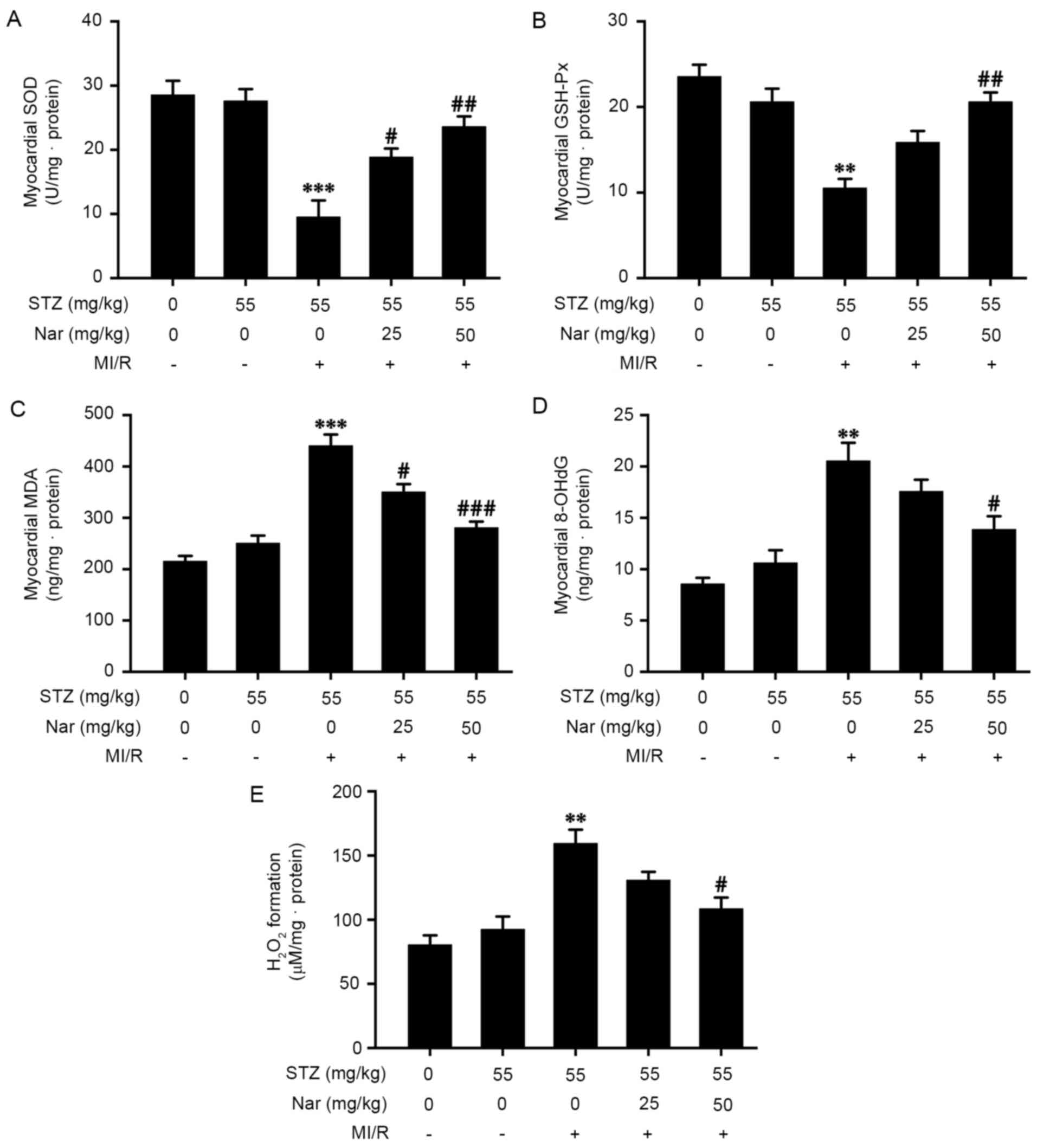 | Figure 3Effect of Nar on myocardial oxidative
stress in diabetic MI/R rats. Activities of (A) SOD and (B) GSH-Px,
and the levels of (C) MDA, (D) 8-OHdG as well as (E)
H2O2 formation in the myocardium were
determined by spectrophotometry using commercially available kits.
Data are presented as the mean ± SEM (number of repeated
measurements: n=3/group). **P<0.01 and
***P<0.001 compared with the STZ-sham group;
#P<0.05, ##P<0.01 and
###P<0.001 compared with the STZ-M/IR group. GSH-Px,
glutathione peroxidase; SOD, superoxide dismutase; MDA,
malondialdehyde; 8-OHdG, 8-hydroxy-2 deoxyguanosine; STZ,
streptozotocin; MI/R, myocardial ischemia reperfusion; Nar,
naringenin. |
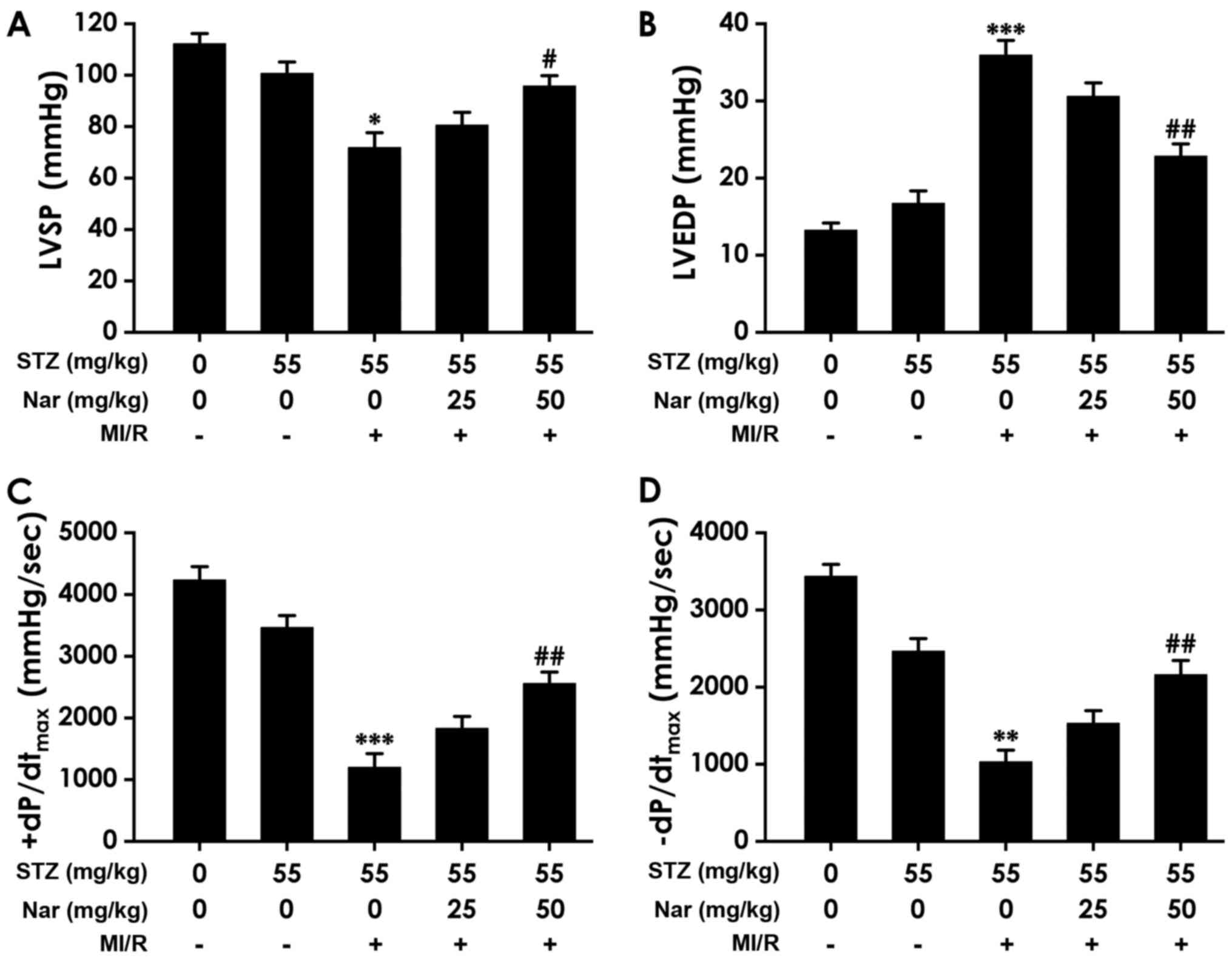
Nar improves cardiac function in
D-MI/R rats
To confirm that Nar alleviates MI/R injury in
diabetic rats, the present study sought to determine whether Nar
ameliorated cardiac function by observing the effects of Nar on
left ventricular hemodynamic parameters in D-MI/R rats. As shown in
Fig. 4, compared with the D-S
group, the D-MI/R group had lower LVSP and ±dP/dtmax, as
well as higher LVEDP. However, pretreatment with HN for 30 days
significantly increased LVSP and ±dP/dtmax, and reduced
LVEDP in D-MI/R rats (Fig. 4A-D).
In addition, there were no significant differences in LVSP, LVEDP
or ±dP/dtmax between the C-S and D-S groups. These data
indicate that Nar alleviated cardiac dysfunction in D-MI/R rats
(Fig. 4A-D).
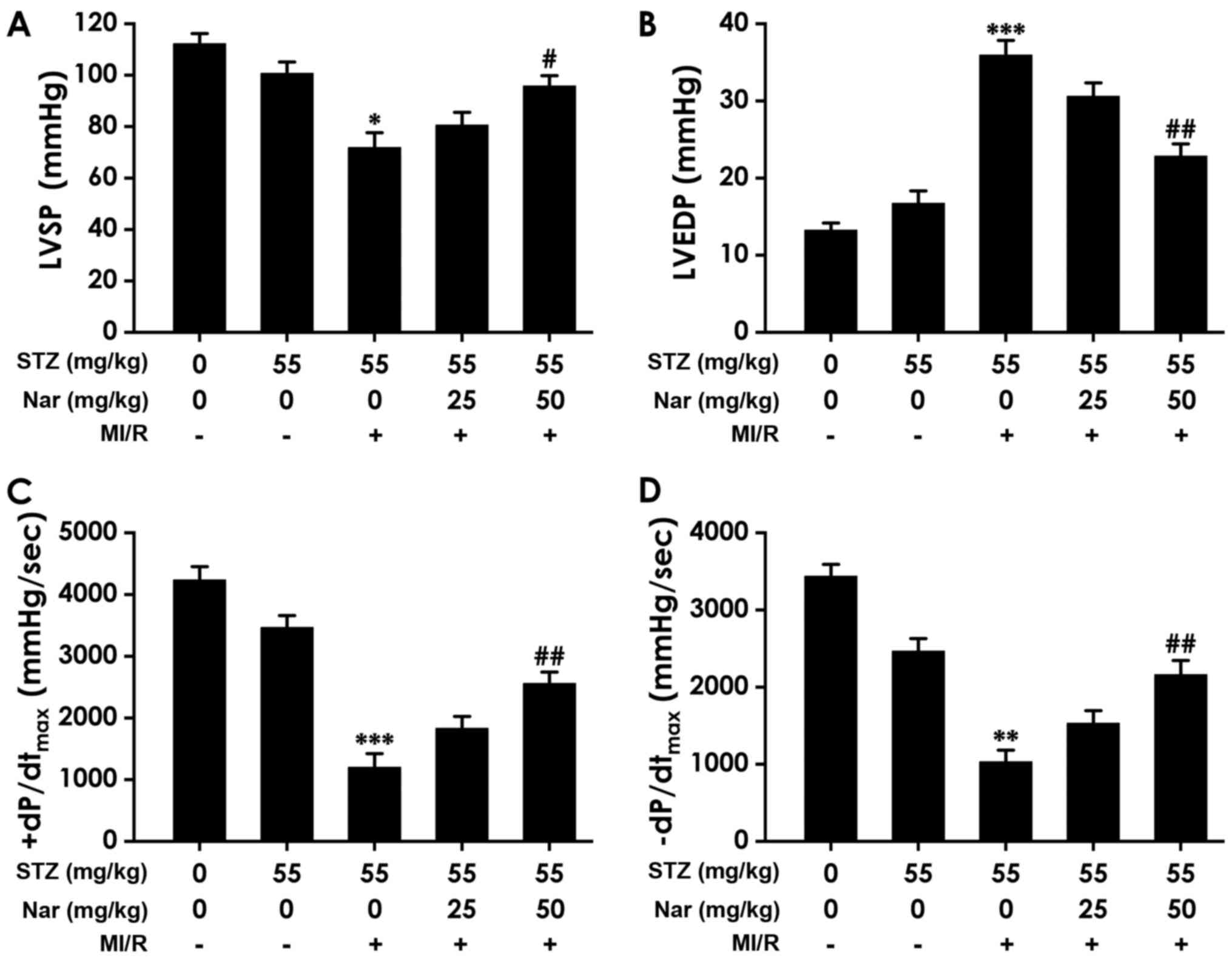 | Figure 4Effect of Nar on cardiac function in
diabetic MI/R rats. (A) LVSP, (B) LVEDP, (C) +dP/dtmax
and (D) -dP/dtmax were recorded using a hemodynamic
monitoring system. Data are presented as the mean ± SEM (number of
repeated measurements: n=6-8/group). *P<0.05,
**P<0.01 and ***P<0.001 compared with
the STZ-sham group; #P<0.05 and
##P<0.01 compared with the STZ-M/IR group. STZ,
streptozotocin; MI/R, myocardial ischemia reperfusion; Nar,
naringenin; LVSP, left ventricular systolic pressure; LVEDP, left
ventricular end-diastolic pressure; +dP/dtmax, peak rate
of left ventricular maximal systolic/diastolic velocity rise;
-dP/dtmax, peak rate of left ventricular maximal
systolic/diastolic velocity fall. |
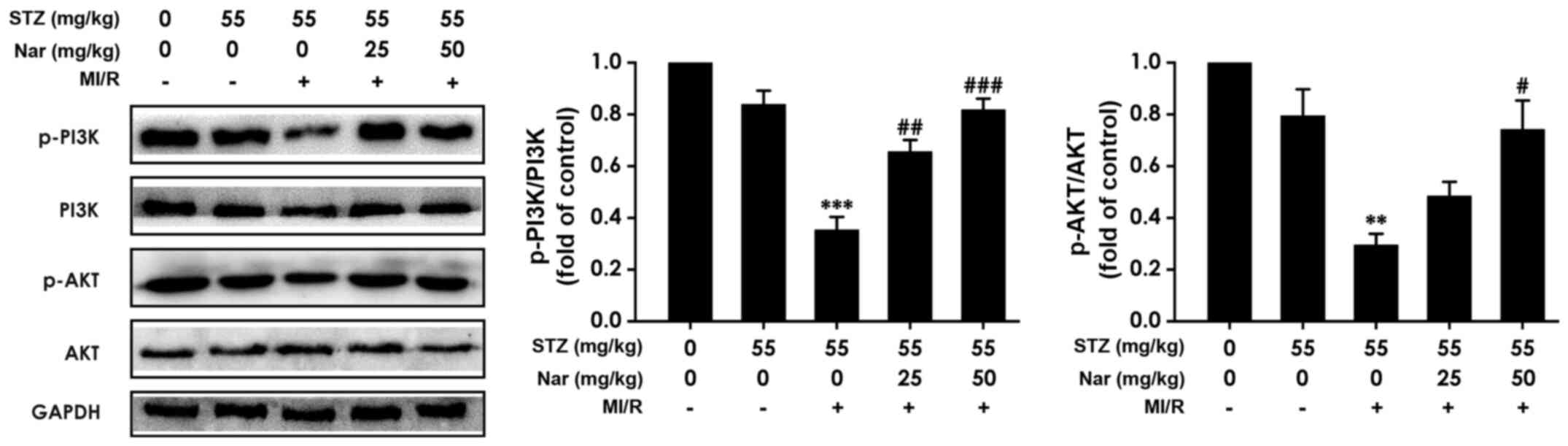
Nar upregulates myocardial PI3K/AKT
signaling in D-MI/R rats
To explore whether the PI3K/AKT signaling pathway
was involved in the Nar-mediated protection against MI/R injury in
diabetic rats, the present study determined whether Nar regulated
PI3K/AKT signaling. As represented in Fig. 5, the ratios of p-PI3K/PI3K and
p-AKT/AKT were significantly downregulated in D-MI/R rats, while
pretreatment with Nar markedly abolished this downregulation
(Fig. 5), indicating that enhanced
PI3K/AKT signaling may contribute to the Nar-mediated protection
against MI/R injury in diabetic rats.
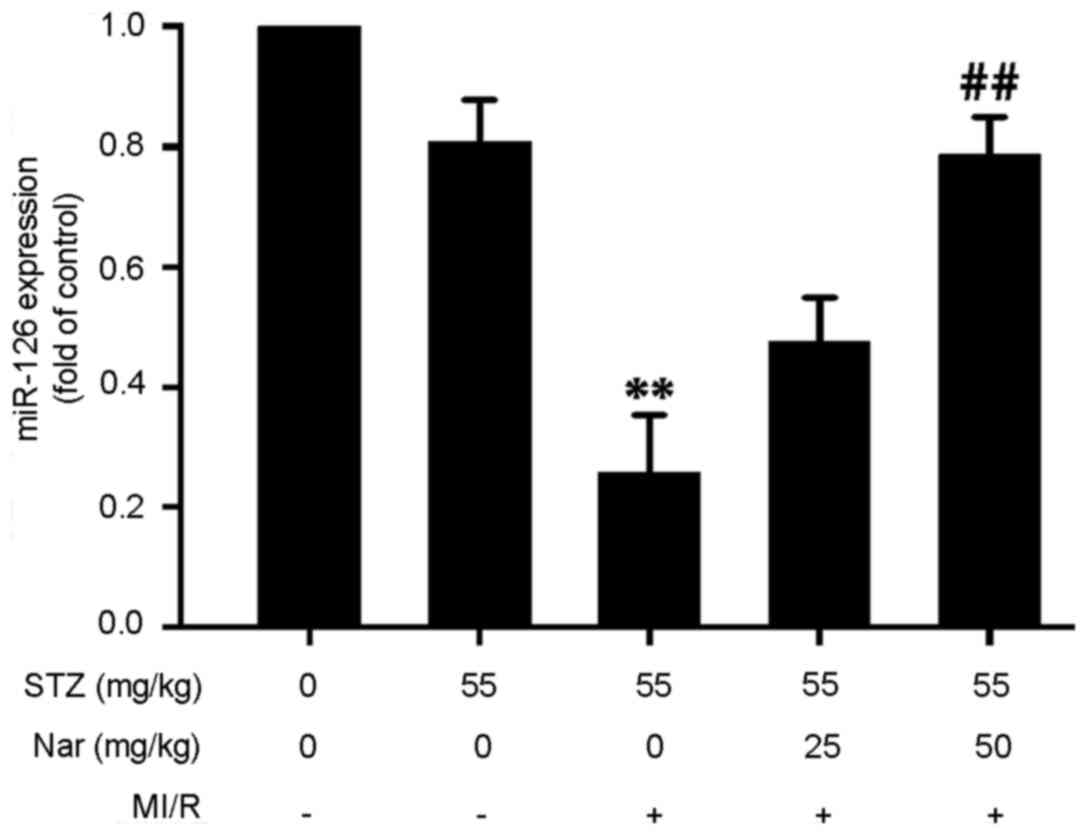
Nar upregulates myocardial miR-126
expression in D-MI/R rats
To investigate whether miR-126 was involved in the
Nar-mediated protection against MI/R injury in diabetic rats, the
present study examined the effect of Nar on myocardial miR-126
expression in D-MI/R rats. Myocardial miR-126 expression was
significantly lower in D-MI/R rats compared with that in the D-S
group, while HN significantly reversed this downregulation of
miR-126 in D-MI/R rats (Fig. 6),
indicating that the upregulation of miR-126 may participate in the
Nar-mediated protection against MI/R injury in diabetic rats.
Discussion
The anti-MI/R injury role of Nar has been previously
reported (19,20,39).
Activation of PI3K/AKT signaling alleviates MI/R injury (24-26),
and enhanced miR-126 prevents MI/R injury (27,28).
The present study used STZ-induced diabetic rats to investigate
whether Nar could ameliorate MI/R injury in diabetes, and to
explore the role of the myocardial miR-126-PI3K/AKT axis in
Nar-mediated protection. The primary findings were as follows: i)
Nar decreased myocardial enzyme content and enhanced cardiac tissue
viability in D-MI/R rats; ii) Nar inhibited myocardial oxidative
stress in D-MI/R rats; iii) Nar improved cardiac function in D-MI/R
rats; and iv) Nar upregulated the myocardial miR-126-PI3K/AKT axis
in D-MI/R rats. In summary, these findings revealed that Nar
prevented MI/R injury by upregulating the miR-126-PI3K/AKT
axis.
In the present study, STZ-induced diabetic rats were
exposed to MI/R to establish an ex vivo model of I/R injury.
Myocardial enzymes, such as CK-MB and LDH, are released into the
plasma during the I/R process due to the loss of myocardial
membrane integrity, and are regarded as indicators of MI/R damage
(40,41). The present results show that MI/R
upregulated the levels of CK-MB and LDH of the coronary effluent
following 5 min of reperfusion, and decreased cardiac viability in
diabetic rats. Moreover, the main functional manifestation of MI/R
injury is cardiac dysfunction, especially systolic and diastolic
dysfunction (42,43). The results of the present study
showed that MI/R downregulated LVSP and ±dP/dtmax, and
upregulated LVEDP in diabetic rats. Substantial evidence indicates
that oxidative stress is a major contributing factor to MI/R injury
(1,28,34,44).
It is known that the activity of SOD and GSH-Px can be used as an
objective index to evaluate the scavenging capacity of ROS
(45). MDA and 8-OHdG are
well-known biomarkers of lipid and DNA peroxidation, respectively,
indicating lipid and DNA damage caused by excessive ROS (46,47).
In the present study, compared with the D-S group, D-MI/R rats had
decreased activities of GSH-Px and SOD, and increased levels of
MDA, 8-OHdG and H2O2. These results indicate
that D-MI/R rats had upregulated levels of myocardial enzymes,
reduced cardiac tissue viability, and enhanced oxidative stress and
cardiac dysfunction, suggesting the successful establishment of the
I/R injury model.
MI/R injury can be triggered while treating IHD
(1,4,5). IHD
is a leading cause of death in patients with diabetes (6). Therefore, effective approaches against
D-MI/R injury may provide a better outcome in the management of
diabetic IHD. It has been shown that Nar prevents MI/R injury
(19,20,39,48).
Thus, the present study aimed to determine whether Nar protected
against MI/R injury in diabetic heart. The results showed that Nar
reduced the myocardial enzyme content of the coronary effluent,
increased cardiac tissue viability, alleviated the oxidative stress
level and improved cardiac function in D-MI/R rats. These data
indicate that Nar has the ability to alleviate MI/R injury in
diabetic rats. The antioxidative effect of Nar has been confirmed
in lens (49), retina (50) and renal (51) cells of diabetic rats. In addition,
Nar exhibits a protective role on cardiac hypertrophy in
STZ-induced diabetic mice (52).
These previous findings offer a reasonable explanation for the
results obtained in the present study. Therefore, it can be
suggested that Nar is an effective therapeutic drug for MI/R injury
in diabetic heart.
The present study also investigated the possible
underlying mechanism for the protective role of Nar against D-MI/R
injury. It has been shown that activation of PI3K/AKT signaling
ameliorates MI/R injury (24-26).
Notably, miR-126 may be a therapeutic agent for diabetes mellitus
(30) and MI/R injury (27,28).
Therefore, it was hypothesized that the miR-126-PI3K/AKT axis may
be involved in Nar-mediated protection against D-MI/R injury. The
present study evaluated the role of Nar on myocardial miR-126 and
PI3K/AKT signaling in D-MI/R rats. It was revealed that Nar
reversed the MI/R-reduced miR-126 expression level, as well as the
ratios of p-PI3K/PI3K and p-AKT/AKT in D-MI/R rats, which suggested
that the upregulation of the miR-126-PI3K/AKT axis contributed to
the beneficial effect of Nar on D-MI/R injury. It has previously
been confirmed that the antidiabetic effect of Nar is exerted by
activation of the PI3K/AKT signaling pathway (53). In addition, the activation the
PI3K/AKT signaling pathway is involved in in the protection
mediated by dexmedetomidine (54)
and eplerenone (55) against I/R
injury in the heart of diabetic rats. Furthermore, long non-coding
RNA cardiac hypertrophy-related factor modulates the progression of
cerebral I/R injury via the miR-126/SOX6 signaling pathway
(56). These previous findings
offer a reasonable explanation for the results obtained in the
present study.
In conclusion, the present study demonstrated that
Nar was able to prevent MI/R injury and upregulate the
miR-126-PI3K/AKT axis in D-MI/R rats. These results indicated that
Nar ameliorated MI/R injury by upregulating the miR-126-PI3K/AKT
axis in diabetic heart, and suggest that Nar may act as a potential
preventive agent for MI/R injury in diabetes, which is important
for improving the therapeutic effect of diabetic IHD including
antioxidant, improvement of myocardial enzyme level and enhancement
of cardiac activity and function.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the Guangdong Medical
Science and Technology Research Fund Project (grant nos. A2017494
and A2016267).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SHL and MSW performed the experiments and data
analysis. MRW was a contributor in analyzing the data and writing
the manuscript. WLK contributed to the experimental design and
manuscript revision. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the University
Animal Care and Use Committee of Affiliated Hospital of Guangdong
Medical (Zhanjiang, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yellon DM and Hausenloy DJ: Myocardial
reperfusion injury. N Engl J Med. 357:1121–1135. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pell VR, Chouchani ET, Frezza C, Murphy MP
and Krieg T: Succinate metabolism: A new therapeutic target for
myocardial reperfusion injury. Cardiovasc Res. 111:134–141.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Whayne TF Jr: Ischemic heart disease and
the Mediterranean diet. Curr Cardiol Rep. 16(491)2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Nordlie MA, Wold LE, Simkhovich BZ, Sesti
C and Kloner RA: Molecular aspects of ischemic heart disease:
Ischemia/reperfusion-induced genetic changes and potential
applications of gene and RNA interference therapy. J Cardiovasc
Pharmacol Ther. 11:17–30. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Feyzizadeh S and Badalzadeh R: Application
of ischemic postconditioning's algorithms in tissues protection:
Response to methodological gaps in preclinical and clinical
studies. J Cell Mol Med. 21:2257–2267. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Orchard TJ and Costacou T: When are type 1
diabetic patients at risk for cardiovascular disease? Curr Diab
Rep. 10:48–54. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Gharravi AM, Jafar A, Ebrahimi M, Mahmodi
A, Pourhashemi E, Haseli N, Talaie N and Hajiasgarli P: Current
status of stem cell therapy, scaffolds for the treatment of
diabetes mellitus. Diabetes Metab Syndr. 12:1133–1139.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Whittington HJ, Babu GG, Mocanu MM, Yellon
DM and Hausenloy DJ: The diabetic heart: Too sweet for its own
good? Cardiol Res Pract. 2012(845698)2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li N, Yang YG and Chen MH: Comparing the
adverse clinical outcomes in patients with non-insulin treated type
2 diabetes mellitus and patients without type 2 diabetes mellitus
following percutaneous coronary intervention: A systematic review
and meta-analysis. BMC Cardiovasc Disord. 16(238)2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lejay A, Fang F, John R, Van JA, Barr M,
Thaveau F, Chakfe N, Geny B and Scholey JW: Ischemia reperfusion
injury, ischemic conditioning and diabetes mellitus. J Mol Cell
Cardiol. 91:11–22. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Jha JC, Ho F, Dan C and Jandeleit-Dahm K:
A causal link between oxidative stress and inflammation in
cardiovascular and renal complications of diabetes. Clin Sci
(Lond). 132:1811–1836. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Salehi B, Fokou PV, Sharifi-Rad M, Zucca
P, Pezzani R, Martins N and Sharifi-Rad J: The therapeutic
potential of naringenin: A review of clinical trials.
Pharmaceuticals (Basel). 12(E11)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Testai L, Da Pozzo E, Piano I, Pistelli L,
Gargini C, Breschi MC, Braca A, Martini C, Martelli A and Calderone
V: The citrus flavanone naringenin produces cardioprotective
effects in hearts from 1 year old rat, through activation of mitoBK
channels. Front Pharmacol. 8(71)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Han X, Pan J, Ren D, Cheng Y, Fan P and
Lou H: Naringenin-7-O-glucoside protects against
doxorubicin-induced toxicity in H9c2 cardiomyocytes by induction of
endogenous antioxidant enzymes. Food Chem Toxicol. 46:3140–3146.
2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Han X, Ren D, Fan P, Shen T and Lou H:
Protective effects of naringenin-7-O-glucoside on
doxorubicin-induced apoptosis in H9C2 cells. Eur J Pharmacol.
581:47–53. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Han XZ, Gao S, Cheng YN, Sun YZ, Liu W,
Tang LL and Ren DM: Protective effect of naringenin-7-O-glucoside
against oxidative stress induced by doxorubicin in H9c2
cardiomyocytes. Biosci Trends. 6:19–25. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Arafa HM, Abd-Ellah MF and Hafez HF:
Abatement by naringenin of doxorubicin-induced cardiac toxicity in
rats. J Egypt Natl Canc Inst. 17:291–300. 2005.PubMed/NCBI
|
|
18
|
Chtourou Y, Slima AB, Makni M, Gdoura R
and Fetoui H: Naringenin protects cardiac
hypercholesterolemia-induced oxidative stress and subsequent
necroptosis in rats. Pharmacol Rep. 67:1090–1097. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yu LM, Dong X, Zhang J, Li Z, Xue XD, Wu
HJ, Yang ZL, Yang Y and Wang HS: Naringenin attenuates myocardial
ischemia-reperfusion injury via cGMP-PKGIα signaling and in vivo
and in vitro studies. Oxid Med Cell Longev.
2019(7670854)2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yu LM, Dong X, Xue XD, Zhang J, Li Z, Wu
HJ, Yang ZL, Yang Y and Wang HS: Naringenin improves mitochondrial
function and reduces cardiac damage following ischemia-reperfusion
injury: The role of the AMPK-SIRT3 signaling pathway. Food Funct.
10:2752–2765. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
You Q, Wu Z, Wu B, Liu C, Huang R, Yang L,
Guo R, Wu K and Chen J: Naringin protects cardiomyocytes against
hyperglycemia-induced injuries in vitro and in vivo. J Endocrinol.
230:197–214. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Yao H and Han X and Han X: The
cardioprotection of the insulin-mediated PI3K/Akt/mTOR signaling
pathway. Am J Cardiovasc Drugs. 14:433–442. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Viard P, Butcher AJ, Halet G, Davies A,
Nürnberg B, Heblich F and Dolphin AC: PI3K promotes
voltage-dependent calcium channel trafficking to the plasma
membrane. Nat Neurosci. 7:939–946. 2004.PubMed/NCBI View
Article : Google Scholar
|
|
24
|
Shen D, Chen R, Zhang L, Rao Z, Ruan Y, Li
L, Chu M and Zhang Y: Sulodexide attenuates endoplasmic reticulum
stress induced by myocardial ischaemia/reperfusion by activating
the PI3K/Akt pathway. J Cell Mol Med. 23:5063–5075. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhang BF, Jiang H, Chen J, Guo X, Li Y, Hu
Q and Yang S: Nobiletin ameliorates myocardial ischemia and
reperfusion injury by attenuating endoplasmic reticulum
stress-associated apoptosis through regulation of the PI3K/AKT
signal pathway. Int Immunopharmacol. 73:98–107. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Deng T, Wang Y, Wang C and Yan H: FABP4
silencing ameliorates hypoxia reoxygenation injury through the
attenuation of endoplasmic reticulum stress-mediated apoptosis by
activating PI3K/Akt pathway. Life Sci. 224:149–156. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Jiang C, Ji N, Luo G, Ni S, Zong J, Chen
Z, Bao D, Gong X and Fu T: The effects and mechanism of miR-92a and
miR-126 on myocardial apoptosis in mouse ischemia-reperfusion
model. Cell Biochem Biophys. 70:1901–1906. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Wang W, Zheng Y, Wang M, Yan M, Jiang J
and Li Z: Exosomes derived miR-126 attenuates oxidative stress and
apoptosis from ischemia and reperfusion injury by targeting ERRFI1.
Gene. 690:75–80. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Moghaddam AS, Afshari JT, Esmaeili SA,
Saburi E, Joneidi Z and Momtazi-Borojeni AA: Cardioprotective
microRNAs: Lessons from stem cell-derived exosomal microRNAs to
treat cardiovascular disease. Atherosclerosis. 285:1–9.
2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Pishavar E and Behravan J: miR-126 as a
Therapeutic Agent for Diabetes Mellitus. Curr Pharm Des.
23:3309–3314. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Naderi R, Mohaddes G, Mohammadi M,
Alihemmati A, Khamaneh A, Ghyasi R and Ghaznavi R: The effect of
garlic and voluntary exercise on cardiac angiogenesis in diabetes:
The role of miR-126 and miR-210. Arq Bras Cardiol. 112:154–162.
2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Bhutada P, Mundhada Y, Bansod K, Bhutada
C, Tawari S, Dixit P and Mundhada D: Ameliorative effect of
quercetin on memory dysfunction in streptozotocin-induced diabetic
rats. Neurobiol Learn Mem. 94:293–302. 2010.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Bayrami G, Alihemmati A, Karimi P, Javadi
A, Keyhanmanesh R, Mohammadi M, Zadi-Heydarabad M and Badalzadeh R:
Combination of vildagliptin and ischemic postconditioning in
diabetic hearts as a working strategy to reduce myocardial
reperfusion injury by restoring mitochondrial function and
autophagic activity. Adv Pharm Bull. 8:319–329. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Xiao C, Xia ML, Wang J, Zhou XR, Lou YY,
Tang LH, Zhang FJ, Yang JT and Qian LB: Luteolin attenuates cardiac
ischemia/reperfusion injury in diabetic rats by modulating Nrf2
antioxidative function. Oxid Med Cell Longev.
2019(2719252)2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Yu L, Liang H, Dong X, Zhao G, Jin Z, Zhai
M, Yang Y, Chen W, Liu J, Yi W, et al: Reduced silent information
regulator 1 signaling exacerbates myocardial ischemia-reperfusion
injury in type 2 diabetic rats and the protective effect of
melatonin. J Pineal Res. 59:376–390. 2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Yang JT, Qian LB, Zhang FJ, Wang J, Ai H,
Tang LH and Wang HP: Cardioprotective effects of luteolin on
ischemia/reperfusion injury in diabetic rats are modulated by eNOS
and the mitochondrial permeability transition pathway. J Cardiovasc
Pharmacol. 65:349–356. 2015.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Yang Y, Duan W, Jin Z, Yi W, Yan J, Zhang
S, Wang N, Liang Z, Li Y, Chen W, et al: JAK2/STAT3 activation by
melatonin attenuates the mitochondrial oxidative damage induced by
myocardial ischemia/reperfusion injury. J Pineal Res. 55:275–286.
2013.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-ΔΔC(T)) method. Methods. 25:402–408. 2001.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Meng LM, Ma HJ, Guo H, Kong QQ and Zhang
Y: The cardioprotective effect of naringenin against
ischemia-reperfusion injury through activation of ATP-sensitive
potassium channel in rat. Can J Physiol Pharmacol. 94:973–978.
2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Kumar A, Kaur H, Devi P and Mohan V: Role
of coenzyme Q10 (CoQ10) in cardiac disease, hypertension and
Meniere-like syndrome. Pharmacol Ther. 124:259–268. 2009.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Du L, Zhang H, Zhao H, Cheng X, Qin J,
Teng T, Yang Q and Xu Z: The critical role of the zinc transporter
Zip2 (SLC39A2) in ischemia/reperfusion injury in mouse hearts. J
Mol Cell Cardiol. 132:136–145. 2019.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Yang M, Kong DY and Chen JC: Inhibition of
miR-148b ameliorates myocardial ischemia/reperfusion injury via
regulation of Wnt/β-catenin signaling pathway. J Cell Physiol.
234:17757–17766. 2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Mamamtavrishvili ND, Sharashidze NS,
Abashidze RI and Kvirkveliia AA: Metabolic issues of ischemia
induced myocardial dysfunction. Georgian Med News. 195:40–43.
2011.PubMed/NCBI(In Russian).
|
|
44
|
Sinning C, Westermann D and Clemmensen P:
Oxidative stress in ischemia and reperfusion: Current concepts,
novel ideas and future perspectives. Biomarkers Med.
11:11031–11040. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Taysi S, Tascan AS, Ugur MG and Demir M:
Radicals, oxidative/nitrosative stress and preeclampsia. Mini Rev
Med Chem. 19:178–193. 2019.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Kołodziej U, Maciejczyk M, Miąsko A,
Matczuk J, Knaś M, Żukowski P, Żendzian-Piotrowska M, Borys J and
Zalewska A: Oxidative modification in the salivary glands of high
fat-diet induced insulin resistant rats. Front Physiol.
8(20)2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Zhao H, Zhao M, Wang Y, Li F and Zhang Z:
Glycyrrhizic acid prevents sepsis-induced acute lung injury and
mortality in rats. J Histochem Cytochem. 64:125–137.
2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Kara S, Gencer B, Karaca T, Tufan HA,
Arikan S, Ersan I, Karaboga I and Hanci V: Protective effect of
hesperetin and naringenin against apoptosis in
ischemia/reperfusion-induced retinal injury in rats.
ScientificWorldJournal. 2014(797824)2014.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Wojnar W, Zych M and Kaczmarczyk-Sedlak I:
Antioxidative effect of flavonoid naringenin in the lenses of type
1 diabetic rats. Biomed Pharmacother. 108:974–984. 2018.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Al-Dosari DI, Ahmed MM, Al-Rejaie SS,
Alhomida AS and Ola MS: Flavonoid naringenin attenuates oxidative
stress, apoptosis and improves neurotrophic effects in the diabetic
rat retina. Nutrients. 9(E1161)2017.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Roy S, Ahmed F, Banerjee S and Saha U:
Naringenin ameliorates streptozotocin-induced diabetic rat renal
impairment by downregulation of TGF-β1 and IL-1 via modulation of
oxidative stress correlates with decreased apoptotic events. Pharm
Biol. 54:1616–1627. 2016.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Zhang J, Qiu H, Huang J, Ding S, Huang B,
Wu Q and Jiang Q: Naringenin exhibits the protective effect on
cardiac hypertrophy via EETs-PPARs activation in
streptozocin-induced diabetic mice. Biochem Biophys Res Commun.
502:55–61. 2018.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Nishina A, Sato D, Yamamoto J,
Kobayashi-Hattori K, Hirai Y and Kimura H: Antidiabetic-like
effects of naringenin-7-O-glucoside from edible chrysanthemum
‘Kotobuki’ and naringenin by activation of the PI3K/Akt pathway and
PPARγ. Chem Biodivers. 16(e1800434)2019.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Cheng X, Hu J, Wang Y, Ye H, Li X, Gao Q
and Li Z: Effects of dexmedetomidine postconditioning on myocardial
ischemia/reperfusion injury in diabetic rats: Role of the
PI3K/Akt-dependent signaling pathway. J Diabetes Res.
2018(3071959)2018.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Mahajan UB, Patil PD, Chandrayan G, Patil
CR, Agrawal YO, Ojha S and Goyal SN: Eplerenone pretreatment
protects the myocardium against ischaemia/reperfusion injury
through the phosphatidylinositol 3-kinase/Akt-dependent pathway in
diabetic rats. Mol Cell Biochem. 446:91–103. 2018.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Gai HY, Wu C, Zhang Y and Wang D: Long
non-coding RNA CHRF modulates the progression of cerebral
ischemia/reperfusion injury via miR-126/SOX6 signaling pathway.
Biochem Biophys Res Commun. 514:550–557. 2019.PubMed/NCBI View Article : Google Scholar
|