Introduction
In 2019, an estimated 463 million people worldwide
were affected by diabetes mellitus and 5 million people have
succumbed to diabetes mellitus (1).
The number of individuals with diabetes aged 20-79 years is
predicted to rise to 642 million by 2040 (2,3). This
increase will have adverse social and financial implications and
adversely affect health systems. The global healthcare expenditure
on people with diabetes was estimated to be 850 billion US dollars
in 2017(2). Diabetes results in
end-organ damage and the microvascular complications of
nephropathy, retinopathy and neuropathy (4). Diabetic neuropathy (DN), one of the
most common complications of diabetes, affects ≥50% of patients
with diabetes (5). Its most
prominent feature is nerve fiber damage and/or dysfunction, and
symptoms of DN usually include numbness, tingling, pain and
weakness (6). Although there are
numerous pharmacological methods to treat DN, they lack efficacy
and cause adverse reactions, such as neuropsychiatric nature,
peripheral edema and weight gain (7). In addition to strict glycemic control,
researchers have sought potential therapeutic targets and novel
pharmacological alternatives (8).
A previous study revealed increased oxidative stress
in the pathogenesis of experimental DN. Elevated extra- and
intracellular glucose concentrations result in the impairment of
antioxidant defense in patients with diabetes and in diabetic
animal models (9,10). Hyperglycemia has been proposed to
promote reactive oxygen species (ROS) and malondialdehyde (MDA)
accumulation and reduce the activity of superoxide dismutase (SOD)
(11). An increase in ROS and MDA
is directly neurotoxic, promotes neuronal apoptosis (12) and may inhibit mitochondrial
respiratory enzymes, resulting in insufficient neural energy
production and insufficient neurological function (13). Cyclooxygenase-2 (COX-2) mediates the
development of inflammation and is involved in oxidative stress and
ROS production (14). Short-term
selective chemical COX-2 inhibition in rats and COX-2 gene
inactivation in mice prevented functional and biochemical
peripheral nerve defects caused by diabetes (13,15).
Furthermore, nuclear factor erythroid-2-related factor 2 (Nrf2) is
involved in antioxidant stress (16). Numerous studies have indicated that
persistent hyperglycemia decreases Nrf2 expression (17-19).
This downregulation of Nrf2 causes various microvascular changes,
ultimately leading to DN (18).
Moreover, COX-2-dependent electrophilic oxygen molecules have been
demonstrated to act as anti-inflammatory agents by their activation
of Nrf2-dependent antioxidant response elements (20). Therefore, selective COX-2 inhibition
may be useful for preventing or delaying DN (21).
Celecoxib (CXB) is a nonsteroidal anti-inflammatory
drug widely used clinically to treat pain and inflammation
(22,23). It has been hypothesized that
nonsteroidal anti-inflammatory drugs relieve pain primarily by
suppressing the activity of COX proteins (COX-1, COX-2 and COX-3)
(24). Among them, COX-2 has been
described as a target of CXB (25)
and that CXB is the only COX-2 inhibitor currently in clinical use
(26). Oral administration of CXB
in experimental diabetic mice effectively relieved neuropathic DN
pain (27,28); however, the molecular mechanism
remains unclear.
MicroRNAs (miRNAs or miRs) are endogenous noncoding
single-stranded RNAs consisting of ~22 nucleotides (29). The majority of miRNAs are involved
in regulating post-transcriptional gene expression (30). It has been hypothesized that miRNAs
regulate 1/3 of human genes (31).
Furthermore, miRNAs serve a key role in numerous biological
processes. Apoptosis, differentiation and metabolism are regulated
by base-pairing with targets, causing target mRNA degradation or
inhibiting translation (32). The
regulation of miR-155 in acute and chronic inflammatory responses
has been extensively studied (33,34).
Moreover, miR-155 has been demonstrated to serve an important role
in peripheral DN (35). miR-155
protects dorsal root ganglion (DRG) neurons by downregulating the
inflammatory response (36).
However, it remains unclear whether miR-155 affects oxidative
stress in DN.
The present study aimed to investigate the molecular
mechanism by which CXB relieves DN using a cellular model of DN
generated by stimulating DRG neurons with hyperglycemic conditions.
Furthermore, the present study also researched the role of CXB in
regulating the expression of miR-155 and COX-2, thereby providing a
possible explanation for the effect of CXB on DN.
Materials and methods
Cell culture
Mouse DRG neurons were purchased from Qincheng
Biotechnology Co., Ltd. (cat. no. MIC-QC-242; Beijing Solarbio
Science & Technology Co., Ltd.). DRG neurons were cultured in
DMEM with 10% FBS, 100 µg/ml streptomycin and 100 U/ml penicillin
(all Beijing Solarbio Science & Technology Co., Ltd.) at 37˚C
with 5% CO2 in a humid atmosphere. The neurons were
cultured for a few passages prior to subsequent experiments.
Establishment of the cell damage model
and CXB treatment
To mimic diabetes and DN in vitro, DRG
neurons were cultured in complete medium supplemented with 50 mM
glucose (cat. no. G8150; Beijing Solarbio Science & Technology
Co., Ltd.). DRG neurons were maintained under high-glucose
conditions at 37˚C with 5% CO2 for 48 h (D) or 72 h
(DN). DRG neurons in the negative control (NC) group were cultured
in complete medium containing 25 mM glucose conditions at 37˚C with
5% CO2 for 48 h, which is optimal for DRG neuron
survival and growth (37).
To determine the effect of CXB (cat. no. IC0230;
Beijing Solarbio Science & Technology Co., Ltd.) on DN, DRG
neurons in the DN group were incubated with CXB at various
concentrations (0, 1, 5, 15, 30 or 50 µM) for 24 h prior to
subsequent experiments.
Cell transfection
miR-155 inhibitors (5'-ACCCCUAUCACAAUUAGCAUUAA-3'),
NC inhibitors (5'-CAGUACUUUUGUGUAGUACAA-3'), miR-155 mimics
(5'-UUAAUGCUAAUCGUGAUAGGGGU-3'), mimic NC
(5'-UCACAACCUCCUAGAAAGAGUAGA-3') and predesigned vectors expressing
siRNAs targeting COX-2 mRNAs (si-COX-2,
5'-AATGTCCGGGTACAATCGCACCCTGTCTC-3') were purchased from Cytiva.
Scrambled siRNA (si-control, 5'-AATTCTCCGAACGTGTCACGT-3'; Qiagen
GmbH) was used as the NC for si-COX-2. A total of 2x105
DRG neurons of the DN group were cultured in 24-well plates and
transfected using Lipofectamine™ 3000 (cat. no. L3000008;
Invitrogen; Thermo Fisher Scientific, Inc.), according to the
manufacturer's protocol. miR-155 inhibitors, miR-155 mimics, NC
inhibitors and mimic NC were used at a concentration of 100 nM and
si-COX-2 and si-controls were used at a concentration of 50 nM.
Cells were treated with CXB at 48 h post-transfection, after which
cell suspensions were collected for further analysis.
Cell viability
Cell viability was measured using a Cell Counting
Kit-8 (CCK-8; cat. no. C0038; Beyotime Institute of Biotechnology)
according to the manufacturer's protocol. DRG neurons were cultured
into a 96-well microplate (5x103 cells/well) and treated
with glucose, CXB and/or transfected. A total of 10 µl of CCK-8
reagent was added to the microplates and incubated at 37˚C for 2 h.
Absorbance at 450 nm (A450) was detected using a microplate reader
(Bio-Rad Laboratories, Inc.). Cell growth curves were plotted based
on the average A450 value from 3 replicate measurements.
Apoptosis analysis
Apoptosis was determined with an Annexin
V-FITC/propidium iodide (PI) Apoptosis Detection kit (cat. no.
E606336-0500; Sangon Biotech, Co. Ltd.) according to the
manufacturer's protocol. DRG neurons under various treatment
conditions were seeded into 6-well plates (5x105
cells/well) and reacted with 5 µl of Annexin V-FITC and 10 µl of PI
in the dark at a room temperature for 5 min. Flow cytometric
analysis was performed using a flow cytometer (FACSCalibur; BD
Biosciences) and FlowJo software version 7.6 (FlowJo, LLC). The
results reflect the combination of early and late apoptotic
cells.
ROS assay
ROS generation was detected using a ROS assay kit
(cat. no. S0033S; Beyotime Institute of Biotechnology) according to
the manufacturer's protocol. DRG neurons under various treatment
conditions were seeded into 6-well plates (5x105
cells/well). Then, 10 µM 2,7-dichlorodi-hydrofluorescein diacetate
(DCFH-DA) was added into each well and incubated at 37˚C for 30 min
in the dark. The fluorescence intensity at 485 and 530 nm was
examined with a flow cytometer (FACSCalibur; BD Biosciences) to
evaluate ROS generation.
ELISA
ELISAs were performed with ELISA kits for
malondialdehyde (MDA; cat. no. SBJ-M0411; SenBeiJia Biological
Technology Co., Ltd.) and superoxide dismutase (SOD; cat. no.
ml037856; Mlbio). A total of 1x105 cells under various
treatment conditions (glucose, CXB and/or transfection) added to
96-well microplates and processed according to the manufacturer's
protocol. Conditioned mediums were collected from the wells at 24 h
after processing. Finally, the absorbance at A450 was detected with
a microplate reader (Bio-Rad Laboratories, Inc.) and quantities
were calculated with standard curves.
Reverse transcription-quantitative PCR
(RT-qPCR)
A total of 5x106 DRG neurons/sample were
harvested following treatments or transfections. Total cellular RNA
was isolated using TRIzol™ Reagent (cat. no. 15596018; Invitrogen;
Thermo Fisher Scientific, Inc.). RNA concentrations were determined
using a NanoDrop spectrophotometer (Thermo Fisher Scientific,
Inc.). miR-155 expression was examined by TransScript®
Green miRNA Two-Step RT-qPCR SuperMix (cat. no. AQ202-01; Beijing
Transgen Biotech Co., Ltd.). The specific primers used were as
follows: miR-155 forward, 5'-CTGTATCAAAAGGCCAACTGAA-3' and reverse,
5'-GTGTCTATCCTTATGAATCGCCA-3'; U6 forward, 5'-AACGAGACGACGACAGAC-3'
and reverse, 5'-GCAAATTCGTGAAGCGTTCCATA-3'. PCR amplification was
then conducted using a LightCycler 480 instrument (Roche
Diagnostics). The thermocycling conditions were as follows: 95˚C
for 10 sec followed by 40 cycles of 95˚C for 10 sec and 60˚C for 30
sec. U6 was used as internal controls. Relative expression levels
were calculated using the 2-ΔΔCq method (38).
Western blotting
DRG neurons under various treatment conditions were
seeded into 6-well plates (5x105 cells/well). Crude cell
lysates were harvested using RIPA lysis buffer (Beijing Solarbio
Science & Technology Co., Ltd.), according to the
manufacturer's protocol. The purity of the protein in extracts was
examined by the BCA method. Proteins (100 µg/lane) were separated
by 10% SDS-PAGE and transferred to a PVDF membranes. Nonspecific
protein binding was prevented with the addition of blocking buffer
[5% milk, 20 mM Tris-HCl (pH 7.4), 150 mM NaCl and 0.1% Tween-20]
for 40 min at a room temperature. The membranes were incubated with
specific primary antibodies (1:2,000; Abcam) against nerve growth
factor (NGF; cat. no. ab52918), brain-derived neurotrophic factor
(BDNF; cat. no. ab226843), COX-2 (cat. no. ab188183), kelch-like
ECH-associated protein 1 (Keap1; cat. no. ab227828), nuclear factor
erythroid-2-related factor 2 (Nrf2; cat. no. ab137550), heme
oxygenase-1 (HO-1; cat. no. ab189491), superoxide dismutase 1
(SOD1; cat. no. ab13498), SOD2 (cat. no. ab137037) or β-actin (cat.
no. ab115777) were incubated in blocking buffer at 4˚C overnight.
The membranes were then incubated with horseradish
peroxidase-conjugated goat anti-rabbit immunoglobulin F (1:10,000;
cat. no. ab205718; Abcam) for 60 min in the dark (at room
temperature), and developed using an ECL reagent (cat. no. 32209;
Thermo Fisher Scientific, Inc.). Membranes were exposed using
chemiluminescence apparatus (Bio-Rad Laboratories, Inc.). ImageJ
software (version 1.8.0; National Institutes of Health) was used to
quantify the protein grayscale.
starBase database analysis
starBase database (http://starbase.sysu.edu.cn) provides a widely-used
noncoding RNA interaction from crosslinking-immunoprecipitation and
high-throughput sequencing (CLIP-seq) (39). The database was used to predict
potential target sequences of miR-155 and COX-2.
Dual-luciferase reporter assay
The direct binding of COX-2 and miR-155 was verified
by dual-luciferase reporter assays. Portions of the wild-type (WT)
and mutant (MUT) 3'-untranslated regions (UTRs) of COX-2 mRNA
containing the predicted miR-155-targeting regions were synthesized
and inserted into the pGL3-report luciferase reporter vector
(Sigma-Aldrich; Merck KGaA). miR-155 mimics and NC mimics were
cotransfected into cells with pGL3-3'-UTR wild-type or mutant
plasmid DNA using Lipofectamine® 3000 (cat. no.
L3000008; Invitrogen; Thermo Fisher Scientific, Inc.), according to
the manufacturer's protocol. After 24 h, relative luciferase
activity was analyzed using a dual-luciferase reporter gene
analysis system (Promega Corporation) and Renilla luciferase
reference plasmids were used for standardization.
Statistical analysis
Statistical analysis was performed using SPSS
software (version 19.0; IBM Corp.). Unpaired Student's t-test was
used to evaluate the differences between two groups. One-way ANOVA
with Tukey's Multiple Range post hoc test was used to determine
differences between multiple groups. Data are expressed as the mean
± standard deviation. P<0.05 was considered to indicate a
statistically significant difference.
Results
DRG neurons are injured by high
glucose
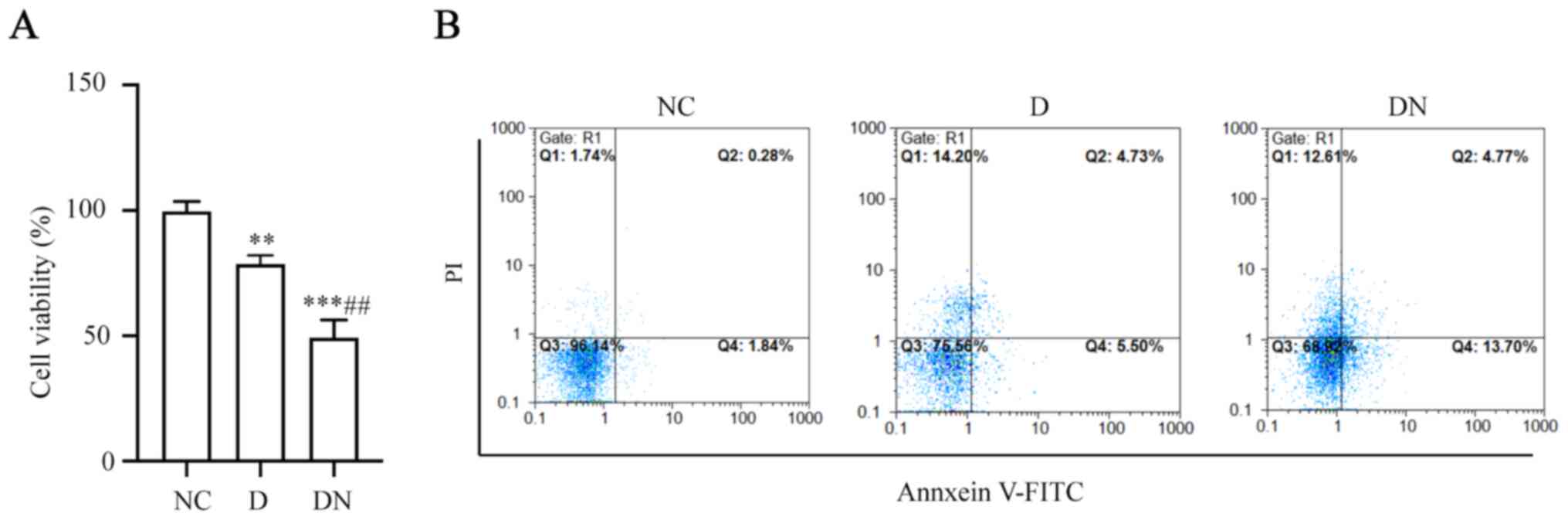
To detect the effect of glucose on DRG neurons, DRG
neurons were treated with glucose for 48 or 72 h. Cell viability
was suppressed and apoptosis was induced by 50 mM glucose for 48 h
compared with the NC group and cell survival was further inhibited
by 50 mM glucose treatment for 72 h (P<0.05; Fig. 1A and B). These results indicated that prolonged
exposure to a high glucose concentration damaged the DRG neurons.
Thus, high-glucose treatment of DRG neurons for 48 or 72 h mimicked
D or DN, respectively, in vitro.
CXB alleviates the inhibitory effect
of DN on DRG neuron survival
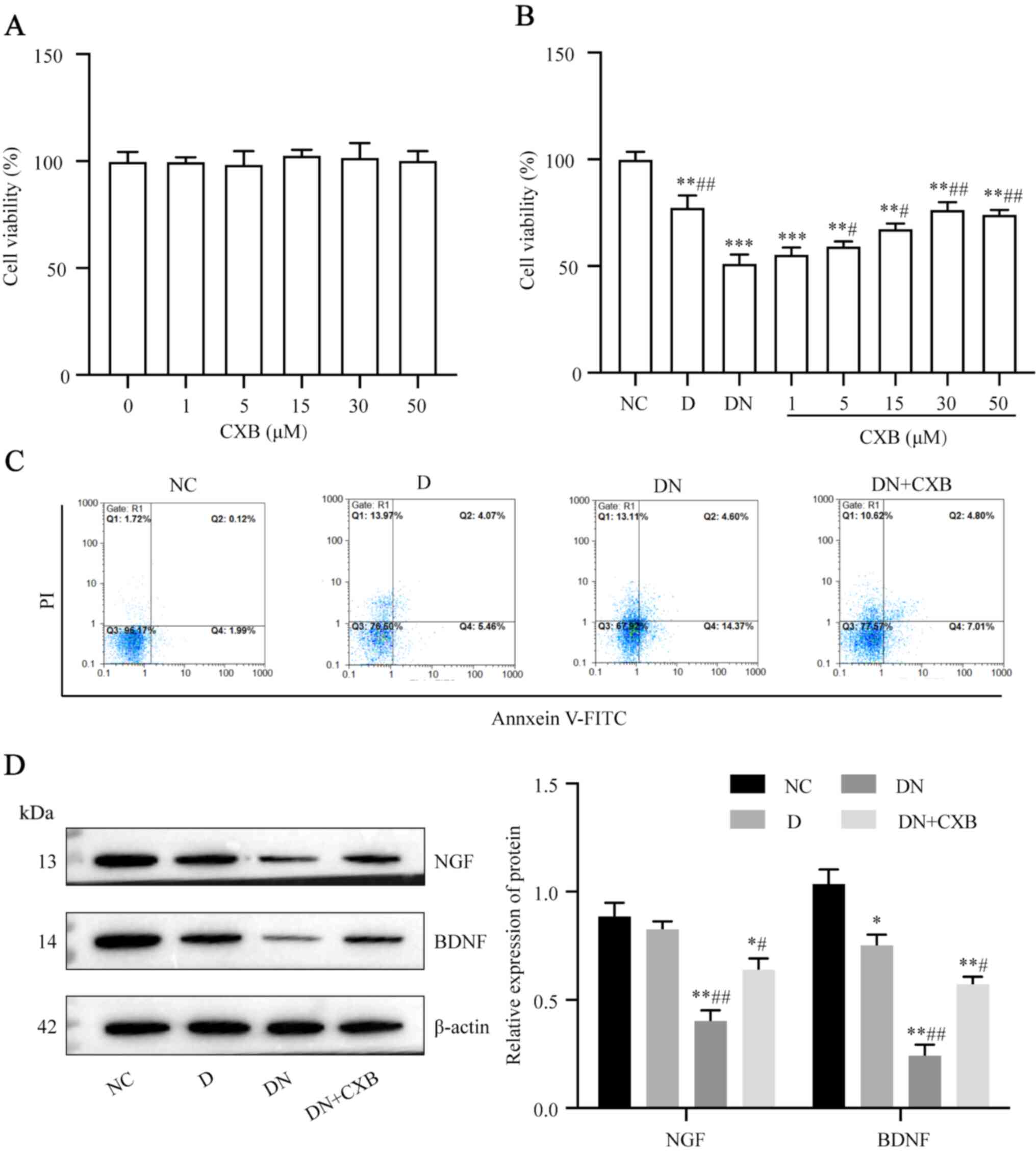
CXB (various doses, 1-50 µM) was utilized to treat
DRG neurons. Cell viability of DRG neurons was examined to evaluate
the cytotoxicity of CXB, which indicated that cell viability was
unchanged by treatment with CXB at different concentrations
(Fig. 2A). To examine the effect of
CXB on DRG neurons, DRG neurons were treated with CXB at various
concentrations. CXB increased DRG neuron viability in the DN group
to a certain extent (P<0.05; Fig.
2B). Considering that DN DRG neurons treated with 30 µM CXB
exhibited the highest viability, 30 µM was used as the optimum CXB
dose in subsequence experiments. Additionally, apoptosis in DN
neurons was attenuated by CXB treatment (Fig. 2C). Furthermore, DN-induced
neurotrophic factors NGF and BDNF suppression was attenuated with
CXB treatment (Fig. 2D; P<0.05).
These results indicated that CXB rescued DN-mediated inhibition of
DRG neuron survival to a certain extent.
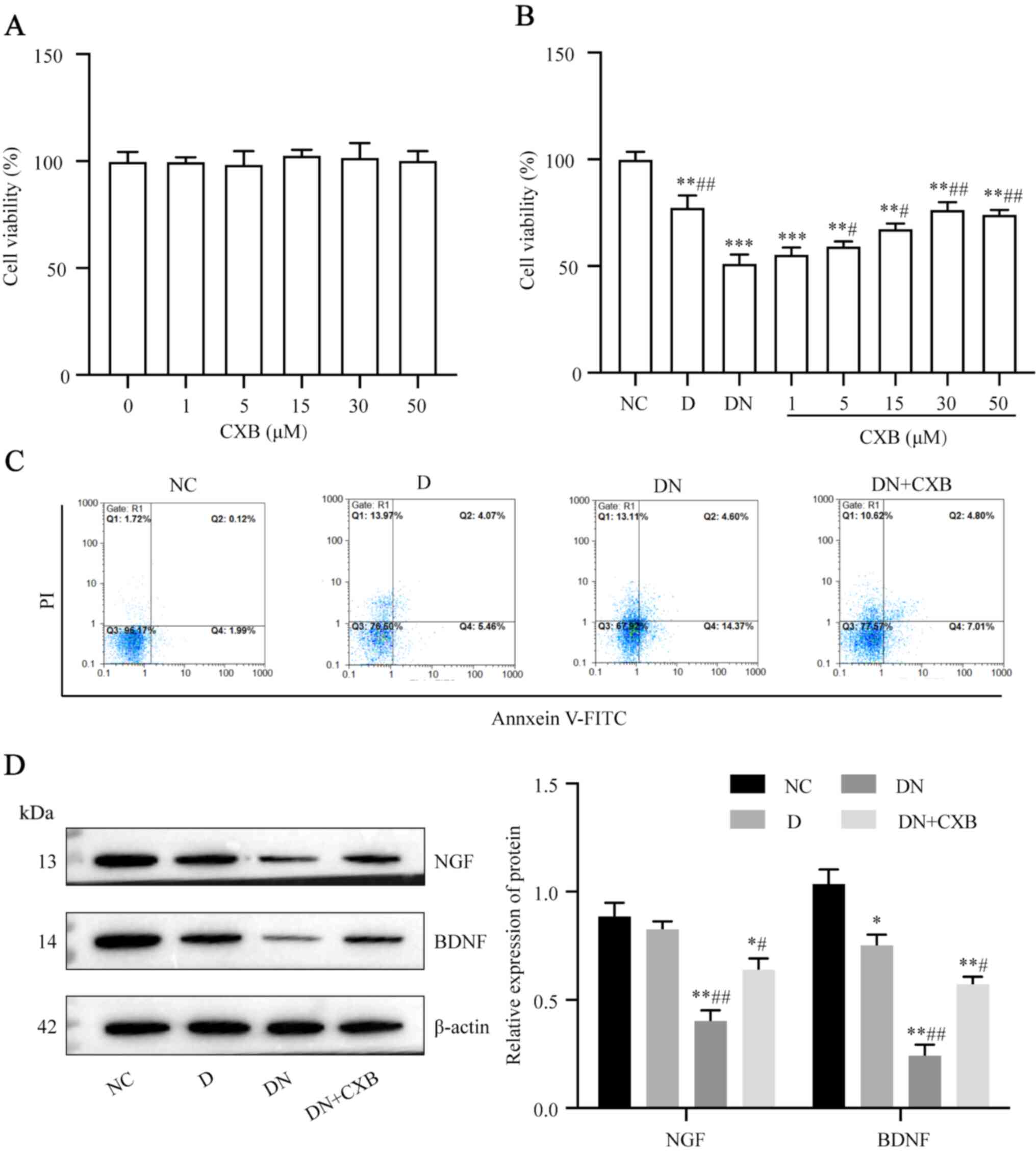 | Figure 2CXB alleviates the inhibitory effect
of DN on dorsal root ganglion neuron survival. Following treatment
on NC neurons with 0-50 µM CXB, (A) the cytotoxicity of CXB was
measured using the CCK-8 assay. Following treatment of DN neurons
with 0-50 µM CXB, (B) cell viability and (C) cell apoptosis rates
were measured using the CCK-8 assay and flow cytometry,
respectively. (D) Protein levels of NGF and BDNF were measured
using western blotting. Data are presented as the mean ± SD. In
(B), **P<0.01 and ***P<0.001 vs. NC
group, and #P<0.05 and ##P<0.01 vs. DN
group using One-way ANOVA with Tukey's post hoc test. In (D),
*P<0.05 and **P<0.01 vs. NC group, and
#P<0.05 and ##P<0.01 vs. D group, using
One-way ANOVA with Tukey's post hoc test. CXB, celecoxib; DN,
diabetic neuropathy; CCK-8, Cell Counting Kit-8; NGF, nerve growth
factor; BDNF, brain-derived neurotrophic factor; PI, propidium
iodide. |
CXB ameliorates DN-induced oxidative
stress in DRG neurons
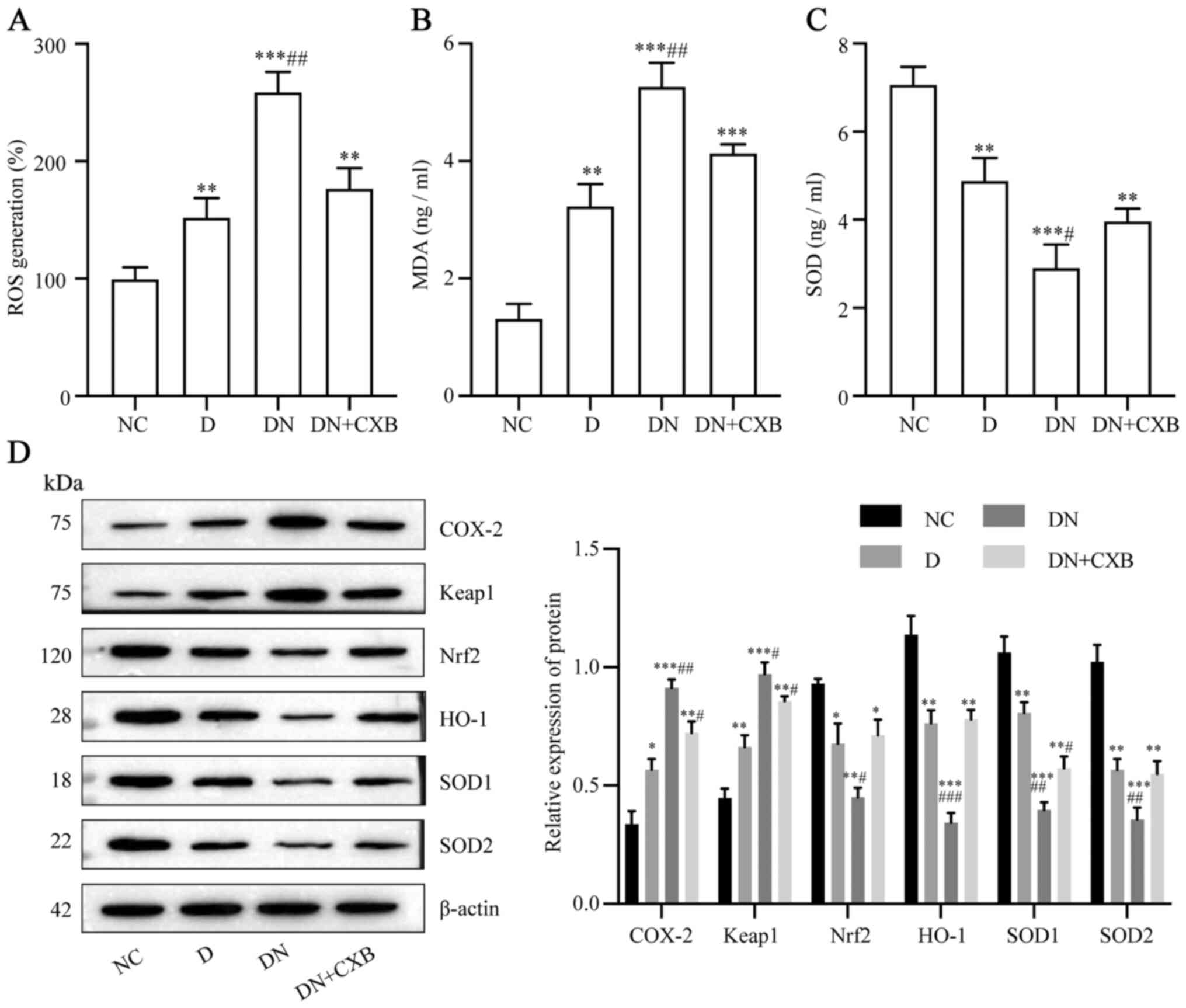
DRG neurons were treated with 30 µM CXB and the
protective effect of CXB against oxidative stress in neurons was
evaluated. The ROS and MDA levels in the DN group were decreased by
CXB treatment (P<0.05; Fig. 3A
and B). However, the SOD levels
were enhanced by CXB treatment (P<0.05; 3C). Additionally, the
levels of oxidative stress-related proteins in each group were
assessed. The levels of COX-2 and Keap1 were reduced by CXB
treatment, while the levels of Nrf2, HO-1, SOD1 and SOD2 were
partially increased by CXB treatment (P<0.05; Fig. 3D). These data indicated that CXB
effectively ameliorated oxidative stress in DRG neurons in the DN
group.
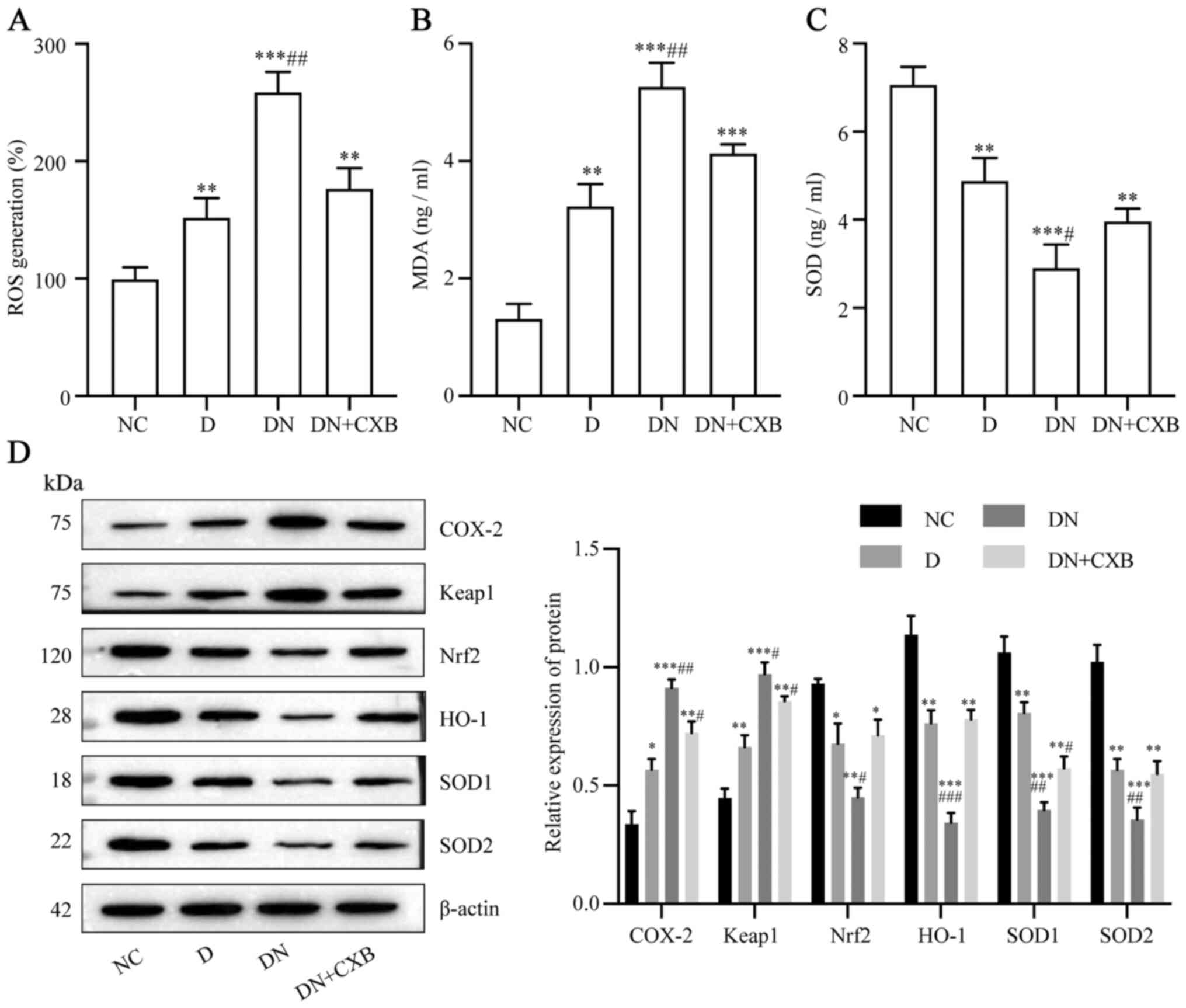 | Figure 3CXB ameliorates DN-induced oxidative
stress in dorsal root ganglion neurons. (A) ROS generation was
measured using an ROS assay kit. (B) MDA and (C) SOD levels were
measured using ELISA kits. (D) The levels of oxidative
stress-related proteins were measured using western blotting.
Values are presented as the mean ± SD. *P<0.05,
**P<0.01 and ***P<0.001 vs. NC group,
and #P<0.05, ##P<0.01 and
###P<0.001 vs. D group, using One-way ANOVA with
Tukey's post hoc test. CXB, celecoxib; DN, diabetic neuropathy;
ROS, reactive oxygen species; MDA, malondialdehyde; SOD, superoxide
dismutase; NC, negative control; D, diabetes; COX-2,
cyclooxygenase-2; Keap1, kelch-like ECH-associated protein 1; Nrf2,
nuclear factor erythroid-2-related factor 2; HO-1, heme
oxygenase-1; SOD1, superoxide dismutase 1; SOD2, superoxide
dismutase 2. |
CXB prevents DN-induced injury in DRG
neurons by upregulating miR-155
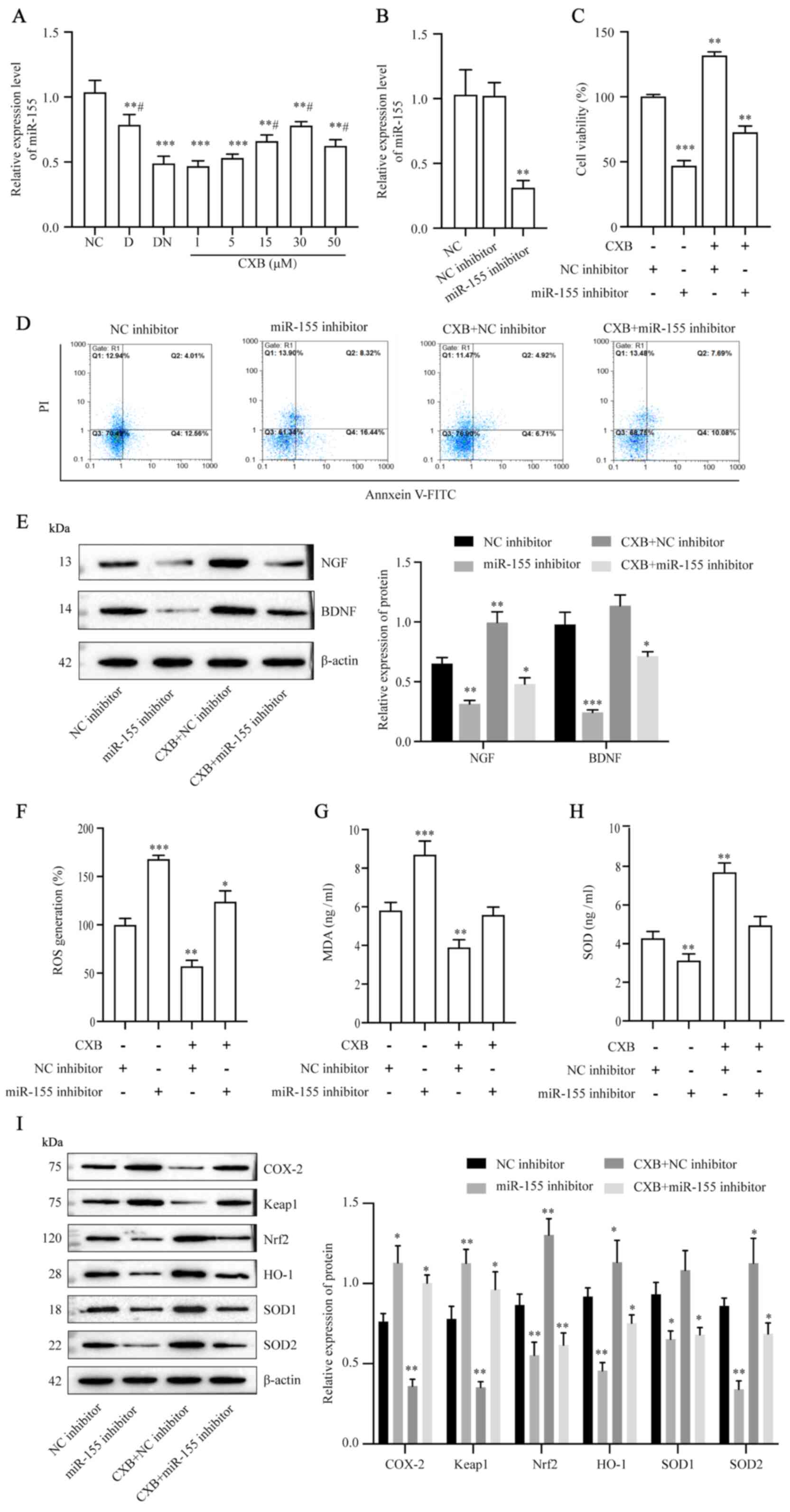
The regulatory effect of miR-155 on CXB-alleviated
DN was investigated. RT-qPCR data demonstrated that miR-155
expression was suppressed in the DN group (Fig. 4A). Furthermore, miR-155 expression
was increased in a dose-dependent manner by CXB treatment
(P<0.05). miR-155 expression in DN-treated DRG neurons was
decreased by miR-155 inhibitor transfection (P<0.05; Fig. 4B). Following this, the importance of
miR-155 in the protective function of CXB was determined. Compared
to transfection with NC inhibitor, transfection with miR-155
inhibitor significantly decreased cell viability (Fig. 4C), promoted apoptosis (Fig. 4D), suppressed NGF and BDNF
expression (Fig. 4E) and
accelerated oxidative damage (Fig.
4F-I; all, P<0.05). Moreover, the protective functions of
CXB against DN-induced damage in DRG neurons were partially
abrogated by inhibition of miR-155 expression (Fig. 4C-I). These results indicated that
miR-155 served an important role in CXB-mediated alleviation of
DN.
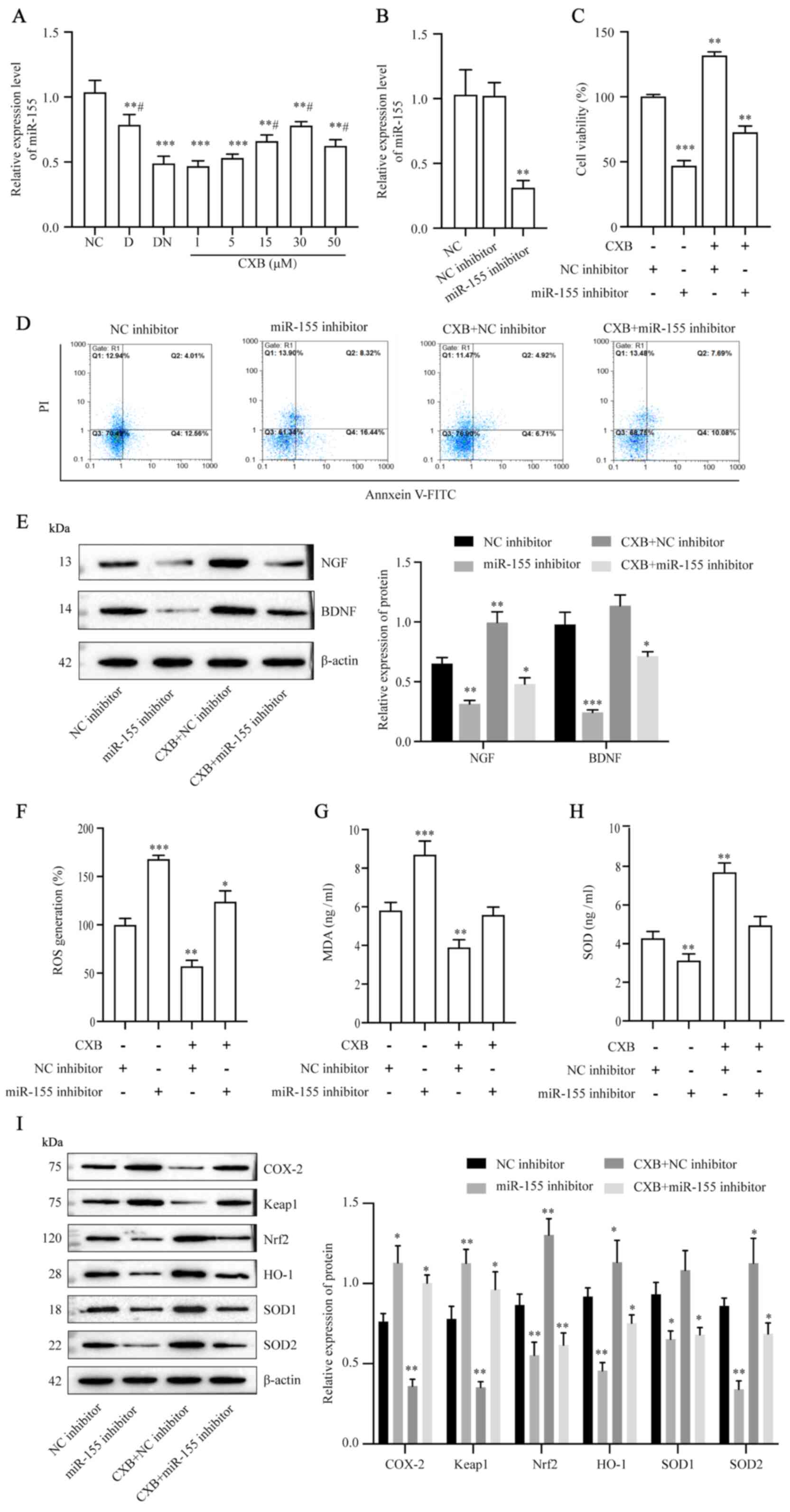 | Figure 4CXB prevents DN-induced injury in
dorsal root ganglion neurons by upregulating miR-155. Following
treatment of DN neurons with 0-50 µM CXB, (A) the expression of
miR-155 was measured using RT-qPCR. (B) Expression of miR-155 in DN
neurons following miR-155 inhibitor transfection was measured using
RT-qPCR. Following treatment with 30 µM CXB and/or miR-155
inhibitor or NC inhibitor transfection, (C) cell viability, (D) the
cell apoptosis rate and (E) protein levels of neurotrophic factors
were detected using the Cell Counting Kit-8 assay, flow cytometry
and western blotting, respectively. (F) ROS generation was measured
using an ROS assay kit, (G) MDA and (H) SOD were measured using
ELISA kits and (I) the levels of oxidative stress-related proteins
were measured using western blotting. Data are presented as the
mean ± SD. In (A), **P<0.01 and
***P<0.001 vs. NC group, and #P<0.05
vs. DN group using One-way ANOVA with Tukey's post hoc test. In
Fig. 4B-I, *P<0.05, **P<0.01 and
***P<0.001 vs. NC inhibitor group using One-way ANOVA
with Tukey's post hoc test. CXB, celecoxib; DN, diabetic
neuropathy; miR, microRNA; RT-qPCR, reverse
transcription-quantitative PCR; NC, negative control; ROS, reactive
oxygen species; MDA, malondialdehyde; SOD, superoxide dismutase; D,
diabetes; NGF, nerve growth factor; BDNF, brain-derived
neurotrophic factor; COX-2, cyclooxygenase-2; Keap1, kelch-like
ECH-associated protein 1; Nrf2, nuclear factor erythroid-2-related
factor 2; HO-1, heme oxygenase-1; SOD1, superoxide dismutase 1;
SOD2, superoxide dismutase 2; PI, propidium iodide. |
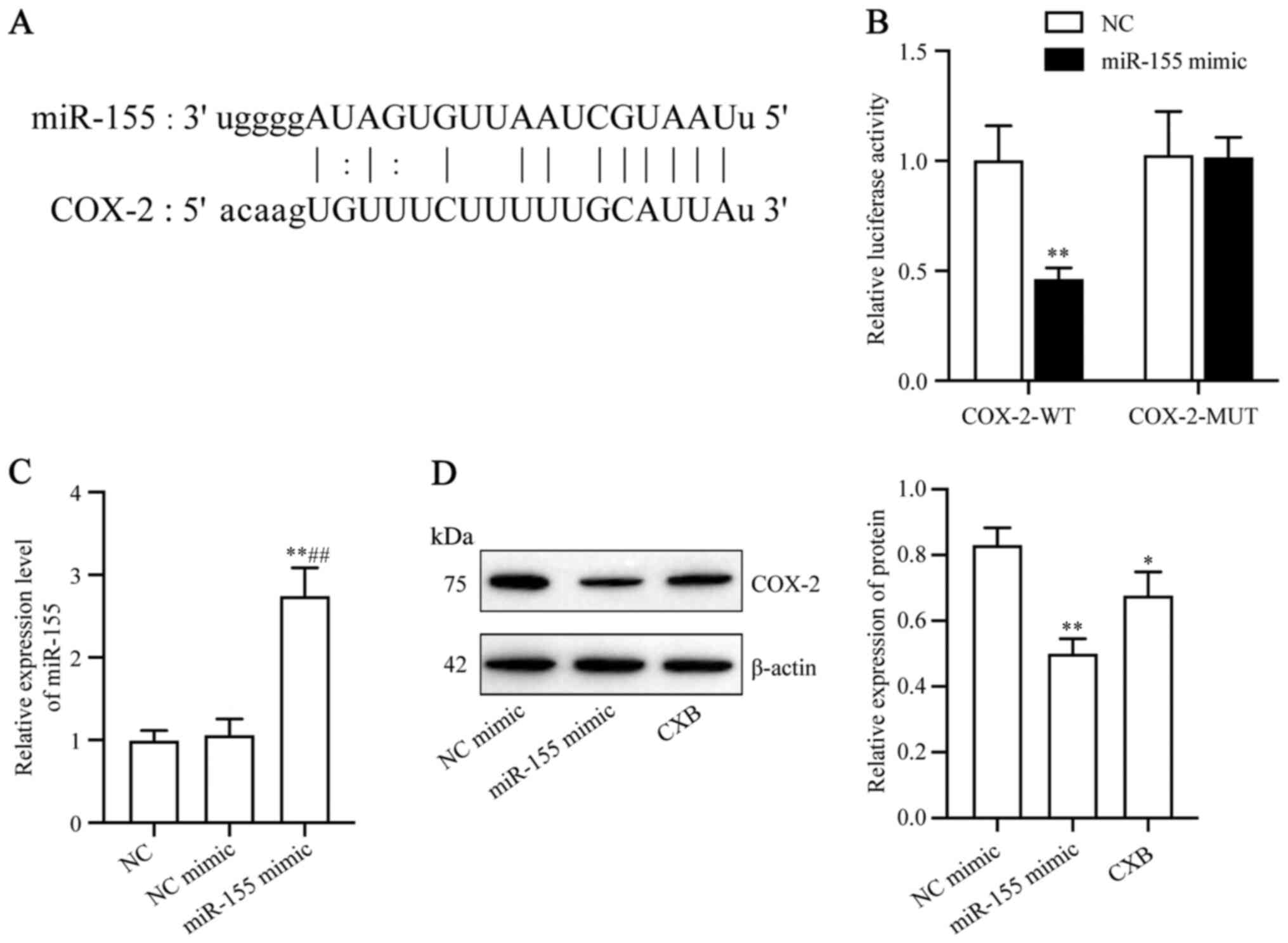
Prediction of COX-2 as a target of
miR-155
The online bioinformatics tool starBase predicted
COX-2 as a target of miR-155. The complementary binding sites of
COX-2 and miRNA-155 are presented in Fig. 5A. To further confirm the interaction
between miR-155 and COX-2, luciferase reporter gene vectors that
expressed WT or MUT 3'UTR of the downstream target luciferase gene
COX-2 were constructed. The results demonstrated a significant
decrease in luciferase activity in the COX-2 3'UTR-WT/miR-155 mimic
group compared with the COX-2 3'UTR-MUT/miR-155 mimic group
(P<0.01; Fig. 5B). miR-155 mimic
transfection efficiency was detected using RT-qPCR (P<0.05;
Fig. 5C). The regulation of COX-2
by miR-155 in DRG neurons was then investigated. The protein
expression level of COX-2 was significantly decreased after cells
were treated with miR-155 mimics compared with NC mimics
(P<0.05; Fig. 5D). These results
demonstrated that miR-155 targeted COX-2.
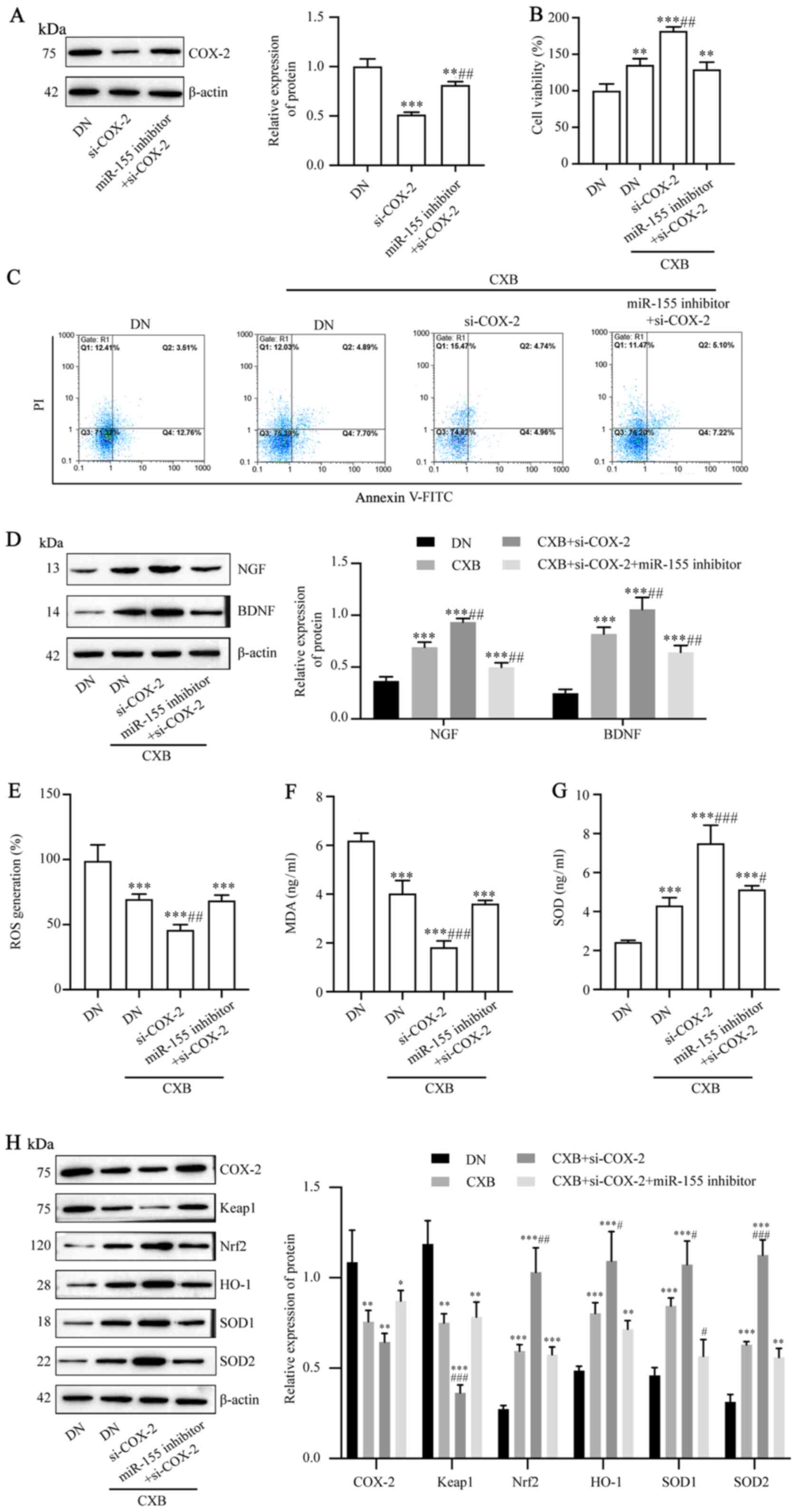
CXB prevents DN-induced injury to DRG
neurons by regulating the miR-155/COX-2 axis
The mechanism by which miR-155 and COX-2 are
involved in CXB-mediated alleviation of DN was investigated.
Vectors that expressed si-COX-2 or si-COX-2 plus miR-155 inhibitor
were transfected into DRG neurons in the DN group. The protein
expression of COX-2 was decreased by si-COX-2 transfection
(P<0.05; Fig. 6A). Following
this, the association between miR-155 and COX-2 with CXB-mediated
alleviation of DN was investigated. Compared to the cell viability
in the DN group and CXB treatment group, transfection with si-COX-2
plus CXB treatment increased cell viability (P<0.05; Fig. 6B), decreased apoptosis (Fig. 6C), upregulated NGF and BDNF
expression (P<0.05; Fig. 6D) and
reduced oxidative damage (P<0.05; Fig. 6E-H). Furthermore, the protective
functions of CXB against DN-induced damage in DRG neurons were
partially reduced by si-COX-2 and miR-155 inhibitor transfection
plus CXB treatment (P<0.05; Fig.
6B-H). In summary, these results indicated that CXB attenuated
DN-induced DRG neuron damage and oxidative stress by regulating the
miR-155/COX-2 axis.
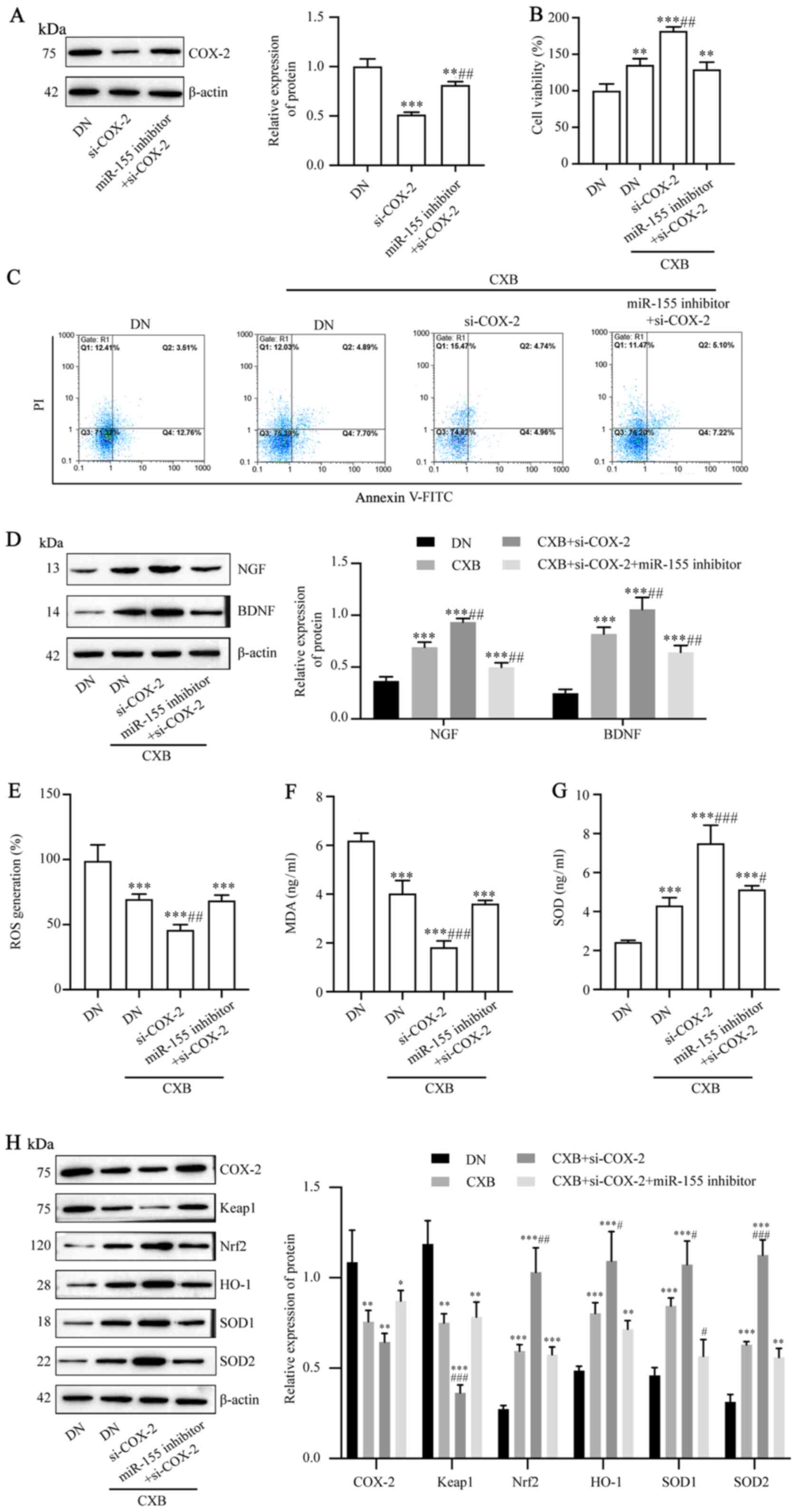 | Figure 6CXB prevents DN-induced injury in
dorsal root ganglion neurons by regulating the miR-155/COX-2 axis.
(A) The protein levels of COX-2 following transfection with
si-COX-2 or si-COX-2 plus miR-155 inhibitor were assessed using
western blotting. Following treatment with 30 µM CXB and
transfection with si-COX-2 or si-COX-2 plus miR-155 inhibitor, (B)
cell viability, (C) cell apoptosis rate and (D) protein levels of
neurotrophic factors were detected using a Cell Counting Kit-8
assay, flow cytometry and western blotting, respectively. (E) ROS
generation was measured using an ROS assay kit, (F) MDA and (G) SOD
were measured using ELISA kits and (H) the levels of oxidative
stress-related proteins were measured using western blotting. In
(A), **P<0.01 and ***P<0.001 vs. DN
group, and ##P<0.01 vs. si-COX-2 group using One-way
ANOVA with Tukey's post hoc test. In (B-H), *P<0.05,
**P<0.01 and ***P<0.001 vs. DN group,
and #P<0.05, ##P<0.01 and
###P<0.001 vs. DN+CXB group using One-way ANOVA with
Tukey's post hoc test. CXB, celecoxib; DN, diabetic neuropathy;
miR, microRNA; COX-2, cyclooxygenase-2; si-COX, siRNAs targeting
COX-2 mRNAs; ROS, reactive oxygen species; MDA, malondialdehyde;
SOD, superoxide dismutase; PI, propidium iodide; NGF, nerve growth
factor; BDNF, brain-derived neurotrophic factor; Keap1, kelch-like
ECH-associated protein 1; Nrf2, nuclear factor erythroid-2-related
factor 2; HO-1, heme oxygenase-1; SOD1, superoxide dismutase 1;
SOD2, superoxide dismutase 2. |
Discussion
In the present study, DRG neurons were stimulated
with high glucose to mimic DN in vitro and the therapeutic
effect of CXB on DN was evaluated. High-glucose conditions led to
reduced cell viability and increased apoptosis and ROS generation,
indicating that DRG neurons were damaged. Additionally, the
function of DRG neurons may have been disturbed, as evidenced by
the decreased expression of NGF and BDNF. CXB treatment
significantly protected DRG neurons against DN-induced damage. The
neuroprotective properties of CXB may be due to the upregulated
expression of miR-155, which was inversely associated with
expression of COX-2. These in vitro data provided evidence
that CXB attenuated DN-induced damage and oxidative stress in DRG
neurons by regulating the miR-155/COX-2 axis.
During the progression of diabetes, long-term
hyperglycemic exposure induces neuronal apoptosis, which leads to
nerve dysfunction and, ultimately, DN (40). Hyperglycemic conditions increase
oxidative stress. Hyperglycemia induces free radicals and produces
ROS and MDA, which reduces protein and unsaturated fatty acids
synthesis (11,41,42).
Furthermore, hyperglycemia impairs the endogenous antioxidant
defense system in patients with diabetes (9). SOD is the most potent antioxidant
in vivo (43). SOD catalyzes
superoxide into oxygen and hydrogen peroxide (44). However, persistent hyperglycemic
stimulation decreases SOD activity, which subsequently aggravates
damage to DRG neurons by oxidative stress (45,46).
Consistently, the results of the present study indicated that the
exposure of DRG neurons to high glucose led to an increase in ROS
and MDA and a decrease in SOD activity. CXB, the only clinically
used COX-2 inhibitor, is involved in regulating apoptosis and ROS
production in a variety of cells, such as myocardia cells and
neurons (47-49).
The present study showed that CXB has neuroprotective functions in
a DN cell model. As revealed by in vitro experiments, CXB
protected DRG neurons from the high glucose-induced loss of
viability, apoptosis and ROS production. DRG neurons are the
primary neurons of the sensory pathway (50). The unique structure of the stem
axons of DRG neurons, which bifurcate into peripheral and central
axon branches, may have important implications for their function
in health and disease (51).
Additionally, NGF and BDNF serve crucial roles in the survival of
human DRG neurons (52). CXB was
revealed to reduce memory impairment by regulating the
BDNF-tropomyosin receptor kinase B signaling pathway in diabetic
rat models (53). The data in the
present study demonstrated that CXB increased BDNF and NGF
expression in DRG neurons, thereby increasing DRG neuron
survival.
Glucose-mediated oxidative stress and alterations in
COX pathway activities have been implicated in the pathogenesis of
experimental DN (15,54). Several DN treatments targeting COX-2
have been reported, including rutin in combination with nimesulide
(55), Juglans regia L. leaf
extract (56) and curcumin
(57). As a known inhibitor of
COX-2, CXB has been demonstrated to reduce neuropathic pain caused
by DN in rats (27,58). However, to the best of our
knowledge, the present study is the first to reveal a possible
mechanism for CXB in the treatment of DN. COX-2, also known as
prostaglandin H synthase 2, is a key enzyme that oxidizes
arachidonic acid (59) and the
products of COX-2 activity participate in various physiological and
pathophysiological processes, including pain (60), inflammation, oxidative stress
(61) and cancer (62). Groeger et al (63) demonstrated that COX-2 activates Nrf2
expression by forming a heterodimer with a small Maf protein and
binding to the ARE upstream promoter region and that COX-2
regulates the expression of various antioxidant and
anti-inflammatory genes, such as Nrf2 and HO-1. The Nrf2/HO-1
signaling pathway is involved in the oxidative stress response
(64). In the present study, CXB
impacted the levels of Nrf2 and HO-1 by regulating the expression
of COX-2. These results indicated that COX-2-mediated oxidative
stress may play a role through the Nrf2/HO-1 signaling pathway.
As CXB is a drug for pain and inflammation (22,23),
the underlying mechanisms of the function of CXB have been
preliminarily investigated. Several studies have indicated that CXB
exerts its functions by regulating miRNA expression patterns. For
example, CXB inhibited breast cancer by increasing miR-222(65) and miRNA-145 was reported to be
involved in CXB-mediated inhibition of the
epithelial-to-mesenchymal transition in bladder cancer (66). The results of the present study
demonstrated that miR-155 is a target of CXB, as its expression was
positively regulated by CXB. miR-155 has been widely studied for
its reported functions in proliferation (67), apoptosis (68) and lipid metabolism (69). In DN, miR-155 was revealed to
protect DRG neurons by downregulating the expression of tumour
necrosis factor-associated factor 2, Notch receptor 2 and sortillin
1(36). The present study
demonstrated that miR-155 was involved in regulating oxidative
stress by targeting COX-2. Furthermore, miR-155 may be a key
molecular target for the diagnosis and treatment of DN.
This study preliminarily demonstrated the potential
therapeutic effect of CXB in DN cell model. In order to better
clarify the therapeutic effect of CXB on DN, the protective effect
of CXB on DN in vivo will be further explored, and the
underlying molecular mechanisms investigated. In conclusion, the
results of the present study may be beneficial for research in
related fields for the development of novel treatment strategies
for DN.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Basic Research
Program of Yunnan Province of China [Joint Project of Kunming
Medical University; grant no. 2018FE001(-241)] and the Scientific
Research Foundation of Yunnan Province Educational Committee (grant
no. 2018JS220).
Availability of data and materials
The datasets used and/or analyzed in the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WR contributed substantially to the study conception
and drafting the manuscript. XC and LZ were involved in the study
conception and design. XC, LZ, TK and XW performed literature
research and the experimental studies. XC, LZ and LC acquired data
and edited the manuscript. SL and JH performed data and statistical
analyses. WR, XC and LZ were involved in critically revising the
manuscript for important intellectual content. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Saeedi P, Petersohn I, Salpea P, Malanda
B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA,
Ogurtsova K, et al: Global and regional diabetes prevalence
estimates for 2019 and projections for 2030 and 2045: Results from
the International Diabetes Federation Diabetes Atlas, 9th edition.
Diabetes Res Clin Pract. 157(107843)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ogurtsova K, da Rocha Fernandes JD, Huang
Y, Linnenkamp U, Guariguata L, Cho NH, Cavan D, Shaw JE and
Makaroff LE: IDF diabetes atlas: Global estimates for the
prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract.
128:40–50. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Harding JL, Pavkov ME, Magliano DJ, Shaw
JE and Gregg EW: Global trends in diabetes complications: A review
of current evidence. Diabetologia. 62:3–16. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Javed S, Alam U and Malik RA: Burning
through the pain: Treatments for diabetic neuropathy. Diabetes Obes
Metab. 17:1115–1125. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Callaghan BC, Cheng HT, Stables CL, Smith
AL and Feldman EL: Diabetic neuropathy: Clinical manifestations and
current treatments. Lancet Neurol. 11:521–534. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pasnoor M, Dimachkie MM, Kluding P and
Barohn RJ: Diabetic neuropathy part 1: Overview and symmetric
phenotypes. Neurol Clin. 31:425–445. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Calandre EP, Rico-Villademoros F and Slim
M: Alpha2 delta ligands, gabapentin, pregabalin and
mirogabalin: A review of their clinical pharmacology and
therapeutic use. Expert Rev Neurother. 16:1263–1277.
2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nawroth PP, Bendszus M, Pham M, Jende J,
Heiland S, Ries S, Schumann C, Schmelz M, Schuh-Hofer S, Treede RD,
et al: The quest for more research on painful diabetic neuropathy.
Neuroscience. 387:28–37. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Matough FA, Budin SB, Hamid ZA, Alwahaibi
N and Mohamed J: The role of oxidative stress and antioxidants in
diabetic complications. Sultan Qaboos Univ Med J. 12:5–18.
2012.PubMed/NCBI View
Article : Google Scholar
|
|
10
|
Piwkowska A, Rogacka D, Audzeyenka I,
Jankowski M and Angielski S: High glucose concentration affects the
oxidant-antioxidant balance in cultured mouse podocytes. J Cell
Biochem. 112:1661–1672. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Piconi L, Quagliaro L and Ceriello A:
Oxidative stress in diabetes. Clin Chem Lab Med. 41:1144–1149.
2003.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yang H, Jin X, Kei Lam CW and Yan SK:
Oxidative stress and diabetes mellitus. Clin Chem Lab Med.
49:1773–1782. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pop-Busui R, Marinescu V, Van Huysen C, Li
F, Sullivan K, Greene DA, Larkin D and Stevens MJ: Dissection of
metabolic, vascular, and nerve conduction interrelationships in
experimental diabetic neuropathy by cyclooxygenase inhibition and
acetyl-L-carnitine administration. Diabetes. 51:2619–2628.
2002.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Smith WL, DeWitt DL and Garavito RM:
Cyclooxygenases: Structural, cellular, and molecular biology. Annu
Rev Biochem. 69:145–182. 2000.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kellogg AP and Pop-Busui R: Peripheral
nerve dysfunction in experimental diabetes is mediated by
cyclooxygenase-2 and oxidative stress. Antioxid Redox Signal.
7:1521–1529. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sies H, Berndt C and Jones DP: Oxidative
stress. Annu Rev Biochem. 86:715–748. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Li M, Yu H, Pan H, Zhou X, Ruan Q, Kong D,
Chu Z, Li H, Huang J, Huang X, et al: Nrf2 Suppression delays
diabetic wound healing through sustained oxidative stress and
inflammation. Front Pharmacol. 10(1099)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kumar A and Mittal R: Nrf2: A potential
therapeutic target for diabetic neuropathy. Inflammopharmacology.
25:393–402. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chen JY, Wang FB, Xu H, Xu LF, Chen D, Liu
WH, Mu X and Wen YQ: High glucose promotes prostate cancer cells
apoptosis via Nrf2/ARE signaling pathway. Eur Rev Med Pharmacol
Sci. 23 (Suppl 3):S192–S200. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Luo C, Urgard E, Vooder T and Metspalu A:
The role of COX-2 and Nrf2/ARE in anti-inflammation and
antioxidative stress: Aging and anti-aging. Med Hypotheses.
77:174–178. 2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kellogg AP, Cheng HT and Pop-Busui R:
Cyclooxygenase-2 pathway as a potential therapeutic target in
diabetic peripheral neuropathy. Curr Drug Targets. 9:68–76.
2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Saxena P, Sharma PK and Purohit P: A
journey of celecoxib from pain to cancer. Prostaglandins Other
Lipid Mediat. 147(106379)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Tindall E: Celecoxib for the treatment of
pain and inflammation: The preclinical and clinical results. J Am
Osteopath Assoc. 99 (Suppl 11):S13–S17. 1999.PubMed/NCBI
|
|
24
|
Vane JR, Mitchell JA, Appleton I,
Tomlinson A, Bishop-Bailey D, Croxtall J and Willoughby DA:
Inducible isoforms of cyclooxygenase and nitric-oxide synthase in
inflammation. Proc Natl Acad Sci USA. 91:2046–2050. 1994.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hawkey CJ: COX-2 inhibitors. Lancet.
353:307–314. 1999.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mi Y, Zhang X, Zhang F, Qi J, Gao H, Huang
D, Li L, Zhang H and Du X: The role of potassium channel activation
in celecoxib-induced analgesic action. PLoS One.
8(e54797)2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Suarez-Mendez S, Tovilla-Zarate CA,
Ortega-Varela LF, Bermudez-Ocaña DY, Blé-Castillo JL,
González-Castro TB, Zetina-Esquivel AM, Diaz-Zagoya JC and Esther
Juárez-Rojop I: Isobolographic analyses of proglumide-celecoxib
interaction in rats with painful diabetic neuropathy. Drug Dev Res.
78:116–123. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Juárez-Rojop IE, Morales-Hernández PE,
Tovilla-Zárate CA, Bermúdez-Ocaña DY, Torres-Lopez JE, Ble-Castillo
JL, Díaz-Zagoya JC and Granados-Soto V: Celecoxib reduces
hyperalgesia and tactile allodynia in diabetic rats. Pharmacol Rep.
67:545–552. 2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bartel DP: Metazoan microRNAs. Cell.
173:20–51. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Correia de Sousa M, Gjorgjieva M, Dolicka
D, Sobolewski C and Foti M: Deciphering miRNAs' Action through
miRNA editing. Int J Mol Sci. 20(6249)2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Hammond SM: An overview of microRNAs. Adv
Drug Deliv Rev. 87:3–14. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Huntzinger E and Izaurralde E: Gene
silencing by microRNAs: Contributions of translational repression
and mRNA decay. Nat Rev Genet. 12:99–110. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Mann M, Mehta A, Zhao JL, Lee K, Marinov
GK, Garcia-Flores Y, Lu LF, Rudensky AY and Baltimore D: An
NF-κB-microRNA regulatory network tunes macrophage inflammatory
responses. Nat Commun. 8(851)2017.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Worm J, Stenvang J, Petri A, Frederiksen
KS, Obad S, Elmén J, Hedtjärn M, Straarup EM, Hansen JB and
Kauppinen S: Silencing of microRNA-155 in mice during acute
inflammatory response leads to derepression of c/ebp Beta and
down-regulation of G-CSF. Nucleic Acids Res. 37:5784–5792.
2009.PubMed/NCBI View Article : Google Scholar
|
|
35
|
El-Lithy GM, El-Bakly WM, Matboli M,
Abd-Alkhalek HA, Masoud SI and Hamza M: Prophylactic L-arginine and
ibuprofen delay the development of tactile allodynia and suppress
spinal miR-155 in a rat model of diabetic neuropathy. Transl Res.
177:85–97. 2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Chen J, Liu W, Yi H, Hu X, Peng L and Yang
F: MicroRNA-155 mimics ameliorates nerve conduction velocities and
suppresses hyperglycemia-induced pro-inflammatory genes in diabetic
peripheral neuropathic mice. Am J Transl Res. 11:3905–3918.
2019.PubMed/NCBI
|
|
37
|
Chen T, Li H, Yin Y, Zhang Y, Liu Z and
Liu H: Interactions of Notch1 and TLR4 signaling pathways in DRG
neurons of in vivo and in vitro models of diabetic neuropathy. Sci
Rep. 7(14923)2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Li JH, Liu S, Zhou H, Qu LH and Yang JH:
starBase v2.0: Decoding miRNA-ceRNA, miRNA-ncRNA and protein-RNA
interaction networks from large-scale CLIP-Seq data. Nucleic Acids
Res. 42 (Database Issue):D92–D97. 2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Guo C, Quobatari A, Shangguan Y, Hong S
and Wiley JW: Diabetic autonomic neuropathy: Evidence for apoptosis
in situ in the rat. Neurogastroenterol Motil. 16:335–345.
2004.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Suzuki N, Sawada K, Takahashi I, Matsuda
M, Fukui S, Tokuyasu H, Shimizu H, Yokoyama J, Akaike A and Nakaji
S: Association between polyunsaturated fatty acid and reactive
oxygen species production of neutrophils in the general population.
Nutrients. 12(3222)2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Gehrmann W, Würdemann W, Plötz T, Jörns A,
Lenzen S and Elsner M: Antagonism between saturated and unsaturated
fatty acids in ROS mediated lipotoxicity in rat insulin-producing
cells. Cell Physiol Biochem. 36:852–865. 2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Valko M, Rhodes CJ, Moncol J, Izakovic M
and Mazur M: Free radicals, metals and antioxidants in oxidative
stress-induced cancer. Chem Biol Interact. 160:1–40.
2006.PubMed/NCBI View Article : Google Scholar
|
|
44
|
He L, He T, Farrar S, Ji L, Liu T and Ma
X: Antioxidants maintain cellular redox homeostasis by elimination
of reactive oxygen species. Cell Physiol Biochem. 44:532–553.
2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Liu D, Zhang H, Gu W and Zhang M: Effects
of exposure to high glucose on primary cultured hippocampal
neurons: Involvement of intracellular ROS accumulation. Neurol Sci.
35:831–837. 2014.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Russell JW, Berent-Spillson A, Vincent AM,
Freimann CL, Sullivan KA and Feldman EL: Oxidative injury and
neuropathy in diabetes and impaired glucose tolerance. Neurobiol
Dis. 30:420–429. 2008.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Zhang C, Wang F, Zhang Y, Kang Y, Wang H,
Si M, Su L, Xin X, Xue F, Hao F, et al: Celecoxib prevents pressure
overload-induced cardiac hypertrophy and dysfunction by inhibiting
inflammation, apoptosis and oxidative stress. J Cell Mol Med.
20:116–127. 2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Crivelli B, Bari E, Perteghella S,
Catenacci L, Sorrenti M, Mocchi M, Faragò S, Tripodo G, Prina-Mello
A and Torre ML: Silk fibroin nanoparticles for celecoxib and
curcumin delivery: ROS-scavenging and anti-inflammatory activities
in an in vitro model of osteoarthritis. Eur J Pharm Biopharm.
137:37–45. 2019.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Huang Y, Liu J, Wang LZ, Zhang WY and Zhu
XZ: Neuroprotective effects of cyclooxygenase-2 inhibitor celecoxib
against toxicity of LPS-stimulated macrophages toward motor
neurons. Acta Pharmacol Sin. 26:952–958. 2005.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Griso O and Puccio H: Primary cultures of
pure embryonic dorsal root ganglia sensory neurons as a new
cellular model for Friedreich's Ataxia. Methods Mol Biol.
2056:241–253. 2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Nascimento AI, Mar FM and Sousa MM: The
intriguing nature of dorsal root ganglion neurons: Linking
structure with polarity and function. Prog Neurobiol. 168:86–103.
2018.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Kaval Oğuz E: Neuronal survival of DRG
neurons after neurite transection in vitro promotes by nerve growth
factor and brain derived neurotrophic factor. Cell Mol Biol
(Noisy-le-Grand). 64:41–46. 2018.PubMed/NCBI
|
|
53
|
Yang Y and Gao L: Celecoxib alleviates
memory deficits by downregulation of COX-2 expression and
upregulation of the BDNF-TrkB signaling pathway in a diabetic rat
model. J Mol Neurosci. 62:188–198. 2017.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Sztanek F, Molnárné Molnár Á and Balogh Z:
The role of oxidative stress in the development of diabetic
neuropathy. Orv Hetil. 157:1939–1946. 2016.PubMed/NCBI View Article : Google Scholar : (In Hu).
|
|
55
|
Mittal R, Kumar A, Singh DP, Bishnoi M and
Nag TC: Ameliorative potential of rutin in combination with
nimesulide in STZ model of diabetic neuropathy: Targeting
Nrf2/HO-1/NF-kB and COX signalling pathway. Inflammopharmacology.
26:755–768. 2018.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Nasiry D, Khalatbary AR, Ahmadvand H,
Talebpour Amiri F and Akbari E: Protective effects of methanolic
extract of Juglans regia L. leaf on streptozotocin-induced
diabetic peripheral neuropathy in rats. BMC Complement Altern Med.
17(476)2017.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Joshi RP, Negi G, Kumar A, Pawar YB,
Munjal B, Bansal AK and Sharma SS: SNEDDS curcumin formulation
leads to enhanced protection from pain and functional deficits
associated with diabetic neuropathy: An insight into its mechanism
for neuroprotection. Nanomedicine. 9:776–785. 2013.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Bujalska-Zadrożny M, de Cordé A and Pawlik
K: Influence of nitric oxide synthase or cyclooxygenase inhibitors
on cannabinoids activity in streptozotocin-induced neuropathy.
Pharmacol Rep. 67:209–216. 2015.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Smith WL, Garavito RM and DeWitt DL:
Prostaglandin endoperoxide H synthases (cyclooxygenases)-1 and -2.
J Biol Chem. 271:33157–33160. 1996.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Lin J, Zhang L and Yang H: Perioperative
administration of selective cyclooxygenase-2 inhibitors for
postoperative pain management in patients after total knee
arthroplasty. J Arthroplasty. 28:207–213. 2013.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Uchida K: A lipid-derived endogenous
inducer of COX-2: A bridge between inflammation and oxidative
stress. Mol Cells. 25:347–351. 2008.PubMed/NCBI
|
|
62
|
Vosooghi M and Amini M: The discovery and
development of cyclooxygenase-2 inhibitors as potential anticancer
therapies. Expert Opin Drug Discov. 9:255–267. 2014.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Groeger AL, Cipollina C, Cole MP, Woodcock
SR, Bonacci G, Rudolph TK, Rudolph V, Freeman BA and Schopfer FJ:
Cyclooxygenase-2 generates anti-inflammatory mediators from omega-3
fatty acids. Nat Chem Biol. 6:433–441. 2010.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Loboda A, Damulewicz M, Pyza E, Jozkowicz
A and Dulak J: Role of Nrf2/HO-1 system in development, oxidative
stress response and diseases: An evolutionarily conserved
mechanism. Cell Mol Life Sci. 73:3221–3247. 2016.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Wong TY, Li F, Lin SM, Chan FL, Chen S and
Leung LK: Celecoxib increases miR-222 while deterring
aromatase-expressing breast tumor growth in mice. BMC Cancer.
14(426)2014.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Liu X, Wu Y, Zhou Z, Huang M, Deng W, Wang
Y, Zhou X, Chen L, Li Y, Zeng T, et al: Celecoxib inhibits the
epithelial-to-mesenchymal transition in bladder cancer via the
miRNA-145/TGFBR2/Smad3 axis. Int J Mol Med. 44:683–693.
2019.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Woeller CF, Roztocil E, Hammond C and
Feldon SE: TSHR signaling stimulates proliferation through PI3K/Akt
and induction of miR-146a and miR-155 in thyroid eye disease
orbital fibroblasts. Invest Ophthalmol Vis Sci. 60:4336–4345.
2019.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Xu L and Leng H, Shi X, Ji J, Fu J and
Leng H: miR-155 promotes cell proliferation and inhibits apoptosis
by PTEN signaling pathway in the psoriasis. Biomed Pharmacother.
90:524–530. 2017.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Lin X, Jia J, Du T, Li W, Wang X, Wei J,
Lin X, Zeng H, Yao L, Chen X, et al: Overexpression of miR-155 in
the liver of transgenic mice alters the expression profiling of
hepatic genes associated with lipid metabolism. PLoS One.
10(e0118417)2015.PubMed/NCBI View Article : Google Scholar
|