Introduction
Carpal tunnel (CT) syndrome (CTS), also known as
delayed median nerve palsy, is one of the most common peripheral
nerve entrapment syndromes diagnosed in the clinic (1). CTS frequently occurs in females aged
40-60 years and the male-to-female ratio is 1:2-5. The incidence
rate in the US is 0.5-1.0% (2).
Although no definite statistical data for CTS have been reported in
China, it is clear that the morbidity rate is increasing with the
improvement of living conditions. It may be hypothesized that
carpal tunnel syndrome correlates with both an increase in the
aging population and changing working conditions. The median nerve
passes directly beneath the transverse carpal ligament and lies
superficial to the nine flexor tendons of the digits, within close
confinement of the CT; it is at this level that the median nerve is
so easily compressed by any condition that increases the volume of
the structures within the CT. The symptoms of median nerve
compression were first described by Paget during the diagnosis and
treatment of two patients with distal radius fractures in 1854, and
CTS, a term first coined by Kremer, is the term currently used to
describe the condition (3). The
diagnosis and treatment of CTS has been approached from different
perspectives and with different methods and there are currently
several therapeutic methods available, ranging from non-surgical to
surgical management. If non-surgical treatment is ineffective,
surgery should be performed to alleviate the disease. The primary
aim of the surgical treatment is to effectively remedy the
compression state of the median nerve (4-6).
To achieve this goal, surgical fasciotomy of the transverse carpal
ligament and distal forearm are necessary (7). A number of different methods for
surgical release have been reported, including traditional open
dissection and double incision cannula (8,9), a
single small incision release (10)
and endoscopic release (11).
However, there remain several controversies regarding the
advantages and disadvantages of the various surgical methods. Due
to the rapid recovery and relatively small levels of inflicted
trauma achieved with endoscopic CT release (ECTR), which was
developed in Japan by Okutsu et al (12) in 1989, ECTR has been widely applied
in the clinic. However, minimally invasive surgery via endoscopy
requires expensive special equipment and the training required to
perform the technique involves a long learning process; therefore,
its application is restricted (13).
In recent years, the functionality of a modified
endoscope for the treatment of CTS has been investigated. It is not
the first time that ECTR through a single portal was described
(14); however, in the novel method
described in the present study, a small, single surgical incision
was made without requiring the use of a special device. This method
requires a probe, hook knife and ordinary arthroscopic systems,
rather than the expensive facet endoscopic systems used in other
procedures. In addition, the learning curve to use this method was
discovered to be relatively short; therefore, this method may be
easily learned by a new surgeon. In fact, the technique may be
easily developed and practiced in areas with less advanced health
systems. Due to the novel method achieving marked therapeutic
results, a standardized operation procedure for the process is
described in the present manuscript.
Materials and methods
Patients
The experimental protocol of the present study was
approved by the Ethics Committee of Sir Run Run Hospital, Nanjing
Medical University (Nanjing, China; approval no. 2015-SR-016) and
was in accordance with the Declaration of Helsinki and
institutional guidelines. A total of 94 patients aged 25-60 years
with idiopathic CTS were randomized in the operating room into
either an experimental or a control group. Factors that may have
had a confounding effect (including age, gender, race, education
level and living conditions) were stratified first, and then
randomly grouped in each layer. Patients were seen by the same
physician between January 2015 and March 2018. All patients had the
typical symptoms in three and a half of the fingers on the radial
side, including hypoesthesia, numbness, weakness in holding and no
hyperalgesia (15). The patients
had also received regular conservative treatment (e.g. oral
non-steroidal anti-inflammatory drugs and rest) for ≥3 months prior
to the visit. Electromyography examination revealed that the
sensory nerve conduction velocity had become slow and the motor
conduction terminal latency was prolonged. The patients were
randomly divided into the open CTR (OCTR) and modified ECTR (MECTR)
groups. The OCTR group comprised 46 patients with a mean age of
48.0±5.33 years and an average disease course of 10.6±2.87 months.
The MECTR group contained 48 cases, who had a mean age of 50.8±7.97
years and an average disease course of 11.0±1.83 months. In the
OCTR group, the male to female ratio was 16:30. In MECTR group, the
male to female ratio was 18:30. This ratio was not purposefully
selected. Factors that may have had a confounding effect (including
age, sex, race, education level and living conditions) were
stratified first.
Diagnostic criteria
The diagnosis of CTS was considered in any patient
who had pain, hypesthesia or paresthesia in the distribution of the
median nerve in the hand or in any patient who had weakness or
paralysis of the abductor pollicis brevis or opponens pollicis. In
almost all cases, thenar atrophy was preceded by the onset of
hypesthesia in the median nerve distribution following numerous
months or years. In addition, the patients were continuously
awakened from their sleep by burning pain and numbness in the
thumb, as well as index and long fingers. The symptoms were
alleviated through wrist activity.
Physical examination included the diagnosis of
hypoesthesia in the affected fingers, atrophy of the thenar muscle
innervated by the median nerve to varying degrees and a positive
response to Tinel's sign and Phalen's maneuver. The results of the
electromyogram, which is the preferred auxiliary examination for
the diagnosis of median nerve compression, were required to
indicate that the sensory latency of the distal median nerve was
≥3.5 msec or 0.5 msec higher than that on the contralateral side.
Furthermore, the distal motor latency was required to be ≥4.5 msec
or exhibit a ≥1.0 msec difference from the healthy side (16,17).
Inclusion and exclusion criteria
The following inclusion criteria were applied: i)
Typical symptoms (pain, hypesthesia or paresthesia) on one hand,
including the thumb, index or middle finger, for ≥2 weeks; ii) the
symptoms were unrelieved, recurrent and even aggravated after
regular non-surgical treatment for >3 months; iii) Hamada Grade
I or II; iv) fulfillment of the electrodiagnostic criteria or if
they were not fulfilled, the presence of night pain that awoke the
patients and a positive flick test (shaking the wrist when the
patients were asked what they do to relieve symptoms) were
required.
The following exclusion criteria were used: i)
Presence of secondary causes, such as bone abnormalities of the
wrist, joint deformity or wrist occupations, including tumors or
masses; ii) Hamada Grade III patients (sensory disturbances, severe
thenar muscle atrophy and accompanying thumb-to-palmar
dysfunction), as the effected thumbs usually required functional
reconstruction; iii) diagnosis of inflammatory joint disease,
trauma, diabetes mellitus or thyroid disorder to the affected hand
during the preceding year, or pregnancy; iv) previous CTR surgery
in the affected hand or CTR surgery in the contralateral hand
during the preceding year; v) inability to complete questionnaires;
and vi) evidence of diffuse peripheral neuropathy or cervical
radiculopathy.
The use of all data from patients and their families
was approved by the Sir Run Run Hospital ethics committee and
written informed consent was obtained from each patient prior to
surgery.
Surgical procedures
In the traditional OCTR group, the incision was made
in the ulnar lateral of the thenar muscle crease, in order to avoid
damaging the recurrent branch of the median nerve on the radial
side of the wrist. The skin and subcutaneous tissue was incised to
reveal the forearm and palm fascia using blunt separation and the
incision of the fascia. The transverse carpal ligament was exposed
and cut off along the ulnar lateral margin to avoid injuring the
median nerve and recurrent branch. In the MECTR group, the incision
was made to the proximal region of the transverse carpal crease and
palmar longus tendon ulnar side. The length of the incision was ~1
cm, and it could be appropriately extended as required. The fascia
was bluntly separated and longitudinally incised to determine the
proximal edge of the transverse carpal ligament and the palmar
longus tendon and to decrease the risk of damage. The ulnar bursa
was separated on the ulnar side of the palmar longus tendon to
distance it from the transverse carpal ligament. Then, the wrist
joint was maintained in the dorsal position so that the nerve and
tendons could be attached to the back of the CT. The distal skin of
the incision was pulled up by a surgical hand hook and the
transverse carpal ligament was exposed. In order to ensure complete
release, the wrist joint of the patient was extended into extreme
dorsiflexion during the operation, the palmar side of the carpal
tunnel hooked from proximal to distal end 2-3 times, in order to
confirm that no ligament tissue is hooked. Ophthalmic scissors were
used to create the greatest possible longitudinal incision of the
ligament under direct vision. Subsequently, a 4.0 mm in diameter,
30˚ wide-angle common arthroscope lens without a metal sleeve was
implanted beneath the distal transverse carpal ligament. The skin
was pulled upward onto the palmar skin of the endoscopic channel by
a suspension suture with 1 or 2 stitches, without using water
perfusion. Once the smooth and white transverse carpal ligament was
visualized through the microscope, a hook knife was inserted in
front of the arthroscope to cut it off completely. Finally, the
incision was sutured and pressure-dressed prior to removing the
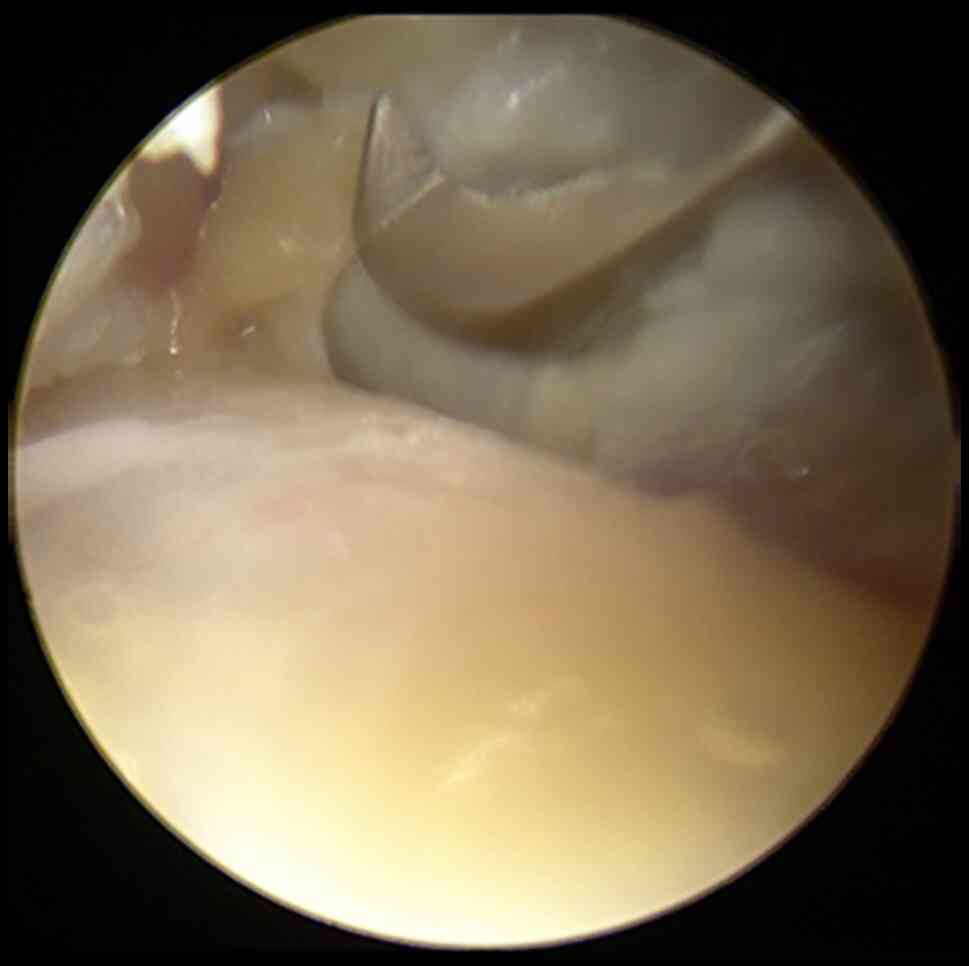
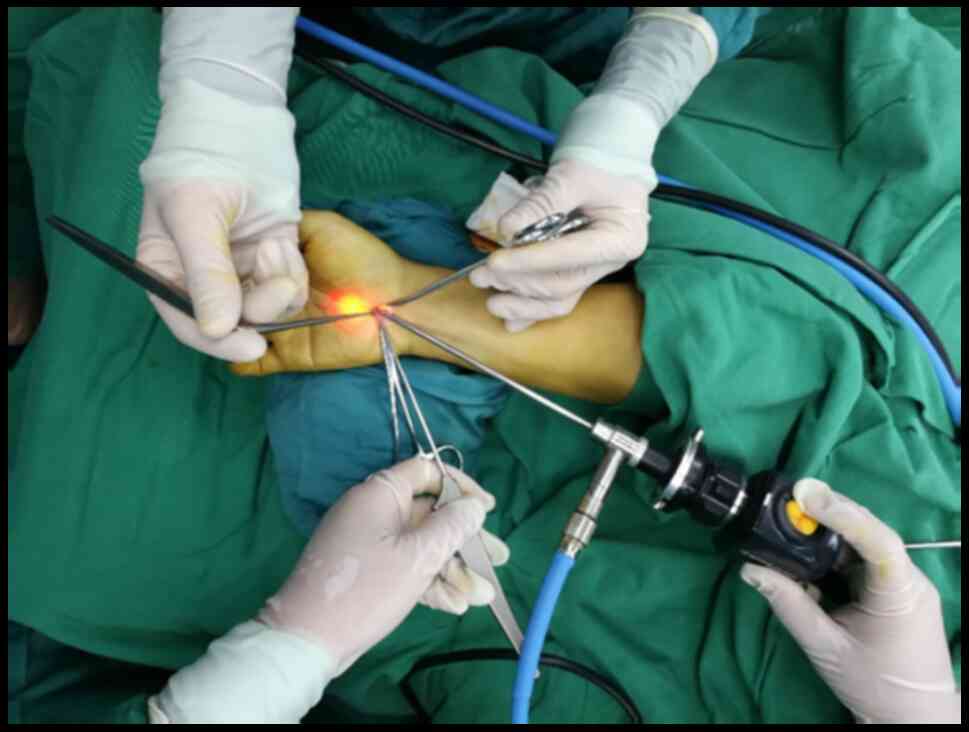
tourniquet. Intraoperative photographs are presented in Fig. 1, Fig.
2, Fig. 3, Fig. 4 and Fig.
5. Fig. 1 is an intraoperative
photo highlighting that in traditional incision surgery, an ~6.0 cm
long S-shaped incision is made on the ulnar side of the thenar
muscle crease. Fig. 2 is an
intraoperative photo illustrating how the hand surgical hook is
used to incise the transverse carpal ligament. Fig. 3 is an intraoperative photo
demonstrating that after the transverse carpal ligament is incised
completely, the median nerve is exposed. Fig. 4 is an intraoperative photo
indicating that a 4 mm, 30˚ wide-angle common knee joint
arthroscope lens without a metal sleeve was implanted beneath the
distal transverse carpal ligament. Fig.
5 demonstrates that the incision is sutured after the surgery.
Fig. 6 is the surgical approach
diagram of the modified endoscope before surgery.
Post-operative treatment
Following surgery in the OCTR group, the forearm was
immobilized with plaster to maintain the wrist joint in the
functional position for 1 week. The plaster was subsequently
removed and the patients were encouraged to exercise the wrist. The
patients in the MECTR group were encouraged to exercise the wrist
joint 24 h after surgery, without immobilization.
Observational indicators
Evaluations were performed the week prior to surgery
and again at 4, 8, 12 and 52 weeks post-surgery, in addition to 4
years after surgery, with an average follow-up time of 33.6 months.
In this extended follow-up, the observations included surgical
operative time, hospitalization time, intraoperative secondary
injury rate (the incidence of nerve, vessel and tendon injury),
incision infection rate, post-operative scar pain score, the time
required to resume a normal lifestyle, recovery of grip and pinch
force, two-point discrimination 3 months following the operation,
the symptom of sympathetic dystrophy and symptom amelioration
(Kelly grading).
Post-operative efficacy
evaluation
The clinical symptom relief criteria were assessed
according to the Kelly grading system (18). The differences in treatment efficacy
were evaluated in a semi-quantitative manner (19). Semi-quantitative evaluation was
performed by rating the outcomes using certain grades to obtain
ranked data, e.g. regarding clinical efficacy, cases were rated as
cured, markedly effective, improved and invalid clinical test.
Clinical tests included wound healing grade, incision infection
rate, intraoperative complications, grip and pinch force, two-point
discrimination, symptoms of sympathetic dystrophy and clinical
symptom amelioration (Kelly). These tests were all performed by the
same physician. Clinical efficacy was divided into cured, markedly
effective, improved and invalid; clinical test results were divided
into -, +, ++, +++, and the severity of pain symptoms is divided
using 0-10 points for different levels of pain, 0 for no pain, 10
for severe pain. 0: No pain; 1-3 points: Mild pain, normal life, no
sleep disturbance; 4-6 points: Obvious pain, unbearable, analgesic
drugs required, sleep disturbed; 7-10 points: Severe pain,
intolerable, need analgesic, sleep by serious interference, can be
accompanied by autonomic nervous disorder or passive position
(20). The Kelly grading system
used was as follows: i) Excellent-following the operation, the pain
and numbness of the affected fingers had disappeared completely,
the grip strength of the fingers, thumb-to-palmar activity and the
range of joint activity had all returned to normal and the patient
had resumed their daily work, with no recurrences observed
following the operation; ii) good-symptoms were mostly relieved,
with only a few symptoms still remaining, the grip and pinch force
had returned to 3/4 of the normal level and the patients were able
to engage in light work; iii) general-symptoms were only slightly
improved and most symptoms persisted, with the grip and pinch
strength being only ≤1/2 of that of normal; and iv) bad-the
symptoms had not improved or in certain circumstances, the symptoms
were even aggravated and the patient was required to change jobs or
give up work. The rate of excellent and good Kelly grading was
calculated as follows: Rate (%)=(nexcellent +
ngood)/ntotal cases x100.
Statistical analysis
SPSS 13.0 statistical software (SPSS, Inc.) was used
for statistical analysis. Count data were expressed as n (%) and
analyzed using a χ2 test. Continuous variables were
expressed as the mean ± standard deviation and the statistical
significance of differences was analyzed using a t-test. The rank
data were analyzed using a Wilcoxon rank-sum test. P<0.01 was
considered to indicate a statistically significant difference.
Results
Patient characteristics
The data, including sex, age, surgical side,
duration of pre-operative symptoms and mean follow-up time in the
two groups were comparable (P>0.05). The severity of the disease
in each group was assessed using the Hamada classification
(21-23)
standard as follows: i) Grade I, numbness present in the radial
side of the hand; ii) Grade II, in addition to Grade I, greater
thenar muscle atrophy was also observed; and iii) Grade III, in
addition to Grade II, thumb-to-palm dysfunction was also observed.
The present study excluded Hamada Grade III patients, as these
patients have severe thenar muscle atrophy and require functional
revascularization. The remaining two groups of patients were
revealed to exhibit no significant differences in the severity of
the disease and Hamada grade (P>0.05; Table I).
 | Table IDistribution of Hamada grades among
the patients. |
Table I
Distribution of Hamada grades among
the patients.
| Group | I | II | III |
|---|
| OCTR (n=46) | 22 | 24 | 0 |
| MECTR (n=48) | 20 | 28 | 0 |
| Z | | -0.42 | |
| P-value | | 0.674 | |
Patient follow up
All of the 94 patients were followed up for 3-41
months, with an average follow-up time of 33.6 months. In the OCTR
group, one case exhibited incomplete remission of symptoms
following the operation, with finger numbness reappearing after 3.5
months. The symptom was relieved after injection with triamcinolone
acetonide and no recurrence was observed during the subsequent
6-month follow-up. The remaining 93 patients were reported to have
completely recovered. The operative time (12.5+2.3 vs. 31.5+3.3
min; P<0.01), hospitalization time (2.8+0.9 vs. 5.5+1.5 days;
P<0.01) and time required to return to normal life (11.6±2.2 vs.
26.2±2.0 days; P<0.01) in the MECTR group were significantly
shorter compared with those in the OCTR group. The visual analogue
scale score points, evaluating surgical area pain at 1 month
following surgery, were lower in the MECTR group compared with
those in the OCTR group (2.1+0.9 vs. 2.8+1.2; P<0.01).
Other indicators, including excellent and good rates
of Kelly grading (87.5 vs. 78.3%; P>0.01) and the incidence of
sympathetic dystrophy at 3 months following surgery (8.3 vs. 13.0%;
P>0.01) were similar in the MECTR and OCTR groups. The incisions
made in both groups were Class-A healing. The two-point
discrimination ability of the index finger abdomen (<5 mm) was
recovered 1 week following surgery in both groups (Tables II and III).
 | Table IIBasic information of the two
groups. |
Table II
Basic information of the two
groups.
| Characteristic | OCTR | MECTR | T (P-value) |
|---|
| Sex
(male/female) | 16/30 | 18/30 | 0.144 (0.850) |
| Age (years) | 48.0±5.33 | 50.8±7.97 | 2.159 (0.170) |
| Affected hand
(left/right) | 12/34 | 16/32 | 1.138 (0.597) |
| Course of disease
(months) | 10.6±2.86 | 11.0±1.83 | 0.196 (0.507) |
| Operative time
(min) | 31.5±3.3 | 12.5±2.3 | 2.276
(<0.001) |
| Hospitalization
time (days) | 5.5±1.5 | 2.8±0.9 | 6.844
(<0.001) |
| Return to
work/normal life (days) | 26.2±2.0 | 11.6±2.2 | 3.400
(<0.001) |
| Follow-up duration
(months) | 34.0±3.31 | 33.3±3.13 | 0.042 (0.358) |
 | Table IIIObservation indexes compared between
the two groups. |
Table III
Observation indexes compared between
the two groups.
| Characteristic | OCTR (n=46) | MECTR (n=48) | T (P-value) |
|---|
| Grip strength
(g/mm2) | 23.2±3.7 | 23.3±1.9 | -0.039 (0.969) |
| Pinch strength
(g/mm2) | 6.3±1.6 | 6.3±1.9 | 0.021 (0.983) |
| Two-point
discrimination (mm) | 6.8±1.4 | 4.5±1.7 | 0.217 (0.829) |
| VAS (points) | 2.8±1.2 | 2.1±0.9 | 2.127 (0.039) |
| Sympathetic
dystrophy | 6 (13.0) | 4 (8.3) | -0.514 (0.610) |
| Kelly excellent or
good | 36 (78.3) | 42 (87.5) | 0.831 (0.411) |
Discussion
The CT is an inelastic fibro-osseous tunnel defined
by the carpal bones and the flexor retinaculum. CTS may be caused
by increased CT content (24-26)
or decreased CT volume. Primary CTS results from the compression of
the median nerve by the transverse carpal ligament (27). At present, the standard surgical
treatment of CTS consists of an open incision and endoscopic
release. Gurpinar et al (28) compared the clinical results and
complications between OCTR and ECTR. In recent years, traditional
open surgery has been gradually replaced by endoscopic release;
this is due to the disadvantages of traditional open surgery,
including the risk of serious injuries, a slow recovery time and
post-operative recurrence caused by adhesion, intractable pain of
the incision scar and other complications. It should be noted that
due to the limited surgical field, nerve injury in the endoscopic
group is more common compared with that in patients who receive
open surgery (29). At present, the
endoscopic treatment of CTS may be divided into two types: Those
with a single incision as part of the Agee technique (30) and Okustu technique (31), and those with a double incision as
part of the Chow technique (32).
The single-incision Okustu technique uses a special facet
endoscopic system, which is expensive and requires a special
latch-up plastic casing. Therefore, the surgery requires to be
performed outside the casing. Under these circumstances, the hook
knife is easily interfered with by the surrounding soft tissue and
may therefore deviate from the cannula when entering and operating
along the outer wall of the tube, resulting in injuries to the
blood vessels, nerve and flexor tendon, which are major causes of
complications following surgery. For the double-incision Chow
technique, the endoscope is placed in an opaque mantle tube, which
forms a relatively narrow field of vision. In addition, the
operation is vulnerable to the accumulation of subcutaneous fat and
blood after incising the transverse carpal ligament; the operative
steps are relatively complex and the learning curve to perform this
technique is long (33,34).
Compared with the single incision technique, an
additional distal incision may increase the risk of collateral
damage to the distal tissue. However, ECTR is currently, in our
experience, only performed in large regional hospitals in China.
This is firstly due to the fact that special assistive devices are
required, including transparent cannulas, special push broaches and
special facet endoscopic systems and the fact that grass-roots
hospitals, even numerous Grade IIIA hospitals, frequently do not
have the corresponding equipment and conditions. In addition, high
levels of surgical expertise are required, as an improper operation
may be prone to causing iatrogenic side injuries. Furthermore, it
is difficult for beginners to master the operating essentials.
Therefore, a long learning curve and related skills training are
required.
Compared with previous studies on ECTR (35), the procedure reported in the present
manuscript differs as the location of the incision and equipment
required is altered. The present study made a single incision at
the level of the proximal transverse carpal crease without the aid
of special auxiliary endoscopic instruments. A common endoscopic
lens (4.0-mm diameter, 30˚ wide-angle arthroscope lens) was also
used, and as the metal mantle tube was not inserted during the
operation, the working diameter of the surgical instrument was
markedly reduced. Therefore, the compression of the median nerve
during endoscopic implantation was effectively reduced, resulting
in a decreased incidence of post-operative sympathetic dystrophy
(36). In addition, the fat
suspension technique was used during this operation, which markedly
increased the operation space. No median nerve injury occurred in
the present study. The distal transverse carpal crease is the axial
point of wrist movement; therefore, choosing it as the entrance
allows the incision to be stimulated repeatedly in daily
activities, leading to more obvious scars, redness and pain
(37). In the present study, the
surgical incision was moved from the distal to the proximal
transverse carpal crease, which therefore avoided the
abovementioned problem effectively. In addition, the incision may
be appropriately expanded to increase the scope of the naked eye,
the median nerve is well exposed and the risk of median nerve
injury is further reduced by using soft glue tube and other
protective measures. This method achieved a similar curative effect
to that reported by others (28,38).
As a developing country, China has an uneven
distribution of medical care. The level of medical care in the
majority of regions is relatively low and the medical equipment is
relatively simple. With the method described in the present study,
a special endoscopic system is no longer required; therefore,
modified endoscopic surgery may be performed with the aid of an
ordinary knee arthroscopic system, which is relatively low-cost and
easy to obtain. In addition, the present method described may be
easily learned, demonstrating a short learning curve. Therefore,
the current method may be performed in areas with less advanced
medical systems.
However, the present method also has several
limitations; for instance, the lack of long palmar tendons in
certain patients had a certain impact on the location of the
incision. In addition, for Hamada Grade III patients and as the
secondary surgery for patients with CTS, this operation may not be
applicable.
In conclusion, the results of the present study
suggested the use of MECTR as a novel endoscopic technology for CTS
treatment. The MECTR technique exhibited several advantages,
including a small risk of trauma, improved safety and effectiveness
and feasibility of being performed in grass-roots hospitals with
relative ease, which suggested that this method should be more
widespread for the clinical treatment of CTS.
Acknowledgements
Not applicable.
Funding
Funding: The work was financed by a grant from Nanjing Science
and Technology Development Plan Project in 2016 (grant no.
201605066) and Key Projects of the Science and Technology
Development Fund of Nanjing Medical University in 2016 (grant no.
2016NJMUZD036).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZC, JL, XXW and TBY were responsible for data
acquisition and interpretation. ZC, DWC and XXW were responsible
for formal data analysis. TBY and DWC carried out the
investigation. ZC and DWC wrote the original draft. JQ designed
this study and edited the manuscript. JQ and JL confirm the
authenticity of the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
This study protocol was approved by the Ethics
Committee of Sir Run Run Hospital, Nanjing Medical University
(Nanjing, China) and was performed in accordance with the
Declaration of Helsinki and institutional guidelines. Written
informed consent was obtained from all individuals or their family
members.
Patient consent for publication
The patients provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sharief F, Kanmani J and Kumar S: Risk
factors, symptom severity and functional status among patients with
carpal tunnel syndrome. Neurol India. 66:743–746. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gelfman R, Melton LJ, Yawn BP, Wollan PC,
Amadio PC and Stevens JC: Long-term trends in carpal tunnel
syndrome. Neurology. 72:33–41. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Patterson JD and Simmons BP: Outcome
assessment in carpel tunnel syndrome. Hand Clin. 18:359–363.
2002.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Akelman E and Weiss AP: Carpal tunnel
syndrome. Etiology and endoscopic treatment. Orthop Clin North Am.
26:769–778. 1995.PubMed/NCBI
|
|
5
|
Zyluk A and Strychar J: A comparison of
two limited open techniques for carpal tunnel release. J Hand Surg
Br. 31:466–472. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kiymaz N, Cirak B, Tuncay I and Demir O:
Comparing open surgery with endoscopic releasing in the treatment
of carpal tunnel syndrome. Minim Invasive Neurosurg. 45:228–230.
2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Means KR, Parks BG, Lee SK and Segalman
KA: Release of the transverse carpal ligament alone is associated
with elevated pressure beneath the distal volar forearm fascia in a
cadaver model of carpal tunnel syndrome. J Hand Surg Am.
32:1533–1537. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Papachristos A and Chow JCY: Endoscopic
carpal tunnel release: Seventeen years' experience with the chow
technique and specific anatomic considerations regarding the volar
aspect of the wrist (SS-61). Arthroscopy. 22(E31)2006.
|
|
9
|
Uchiyama S, Yasutomi T, Fukuzawa T,
Nakagawa H, Kamimura M and Kato H: Reducing neurologic and vascular
complications of endoscopic carpal tunnel release using a modified
chow technique. Arthroscopy. 23:816–821. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kawee P, Pravit K and Adisorn P: Carpal
tunnel release by mini palmar incision. Asian Biomed. 5:139–142.
2011.
|
|
11
|
Nagle DJ: Endoscopic carpal tunnel
release. Hand Clin. 18:307–313. 2002.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Okutsu I, Hamanaka I, Chiyokura Y,
Miyauchi Y and Sugiyama K: Intraneural median nerve pressure in
carpal tunnel syndrome. J Hand Surg Br. 26:155–156. 2001.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sayegh ET and Strauch RJ: Open versus
endoscopic carpal tunnel release: A meta-analysis of randomized
controlled trials. Clin Orthop Relat Res. 473:1120–1132.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Trumble TE, Diao E, Abrams RA and
Gilbert-Anderson MM: Single portal endoscopic carpal tunnel release
compared with open release: A prospective, randomized trial. J Bone
Joint Surg Am. 84:1107–1115. 2002.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Graham B, Regehr G, Naglie G and Wright
JG: Development and validation of diagnostic criteria for carpal
tunnel syndrome. J Hand Surg Am. 31:919–924. 2006.PubMed/NCBI
|
|
16
|
Gilliatt RW and Meer J: The refractory
period of transmission in patients with carpal tunnel syndrome.
Muscle Nerve. 13:445–450. 1990.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Atroshi I, Gummesson C, Johnsson R,
Ornstein E and Rosén I: Median nerve latency measurement agreement
between portable and conventional methods. J Hand Surg Br.
25:73–77. 2000.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Shinoda J, Hashizume H, McCown C, Senda M,
Nishida K, Doi T and Inoue H: Carpal tunnel syndrome grading system
in rheumatoid arthritis. J Orthop Sci. 7:188–193. 2002.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Macdermid JC, Richards RS, Roth JH, Ross
DC and King GJ: Endoscopic versus open carpal tunnel release: A
randomized trial. J Hand Surg Am. 28:475–480. 2003.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wewers ME and Lowe NK: A critical review
of visual analogue scales in the measurement of clinical phenomena.
Res Nurs Health. 13:227–236. 1990.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ciccone W II: Editorial Commentary: What's
Hamada with partial rotator cuff repair? Arthroscopy. 35:351–352.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Takayama K, Yamada S and Kobori Y:
Clinical effectiveness of mini open superior capsular
reconstruction using autologous tensor fascia lata graft. J
Shoulder Elbow Surg: Sep 30, 2020 (Epub ahead of print). doi:
10.1016/j.jse.2020.09.005.
|
|
23
|
Hamada K, Fukuda H, Mikasa M and Kobayashi
Y: Roentgenographic findings in massive rotator cuff tears. A
long-term observation. Clin Orthop Relat Res. 92–96.
1990.PubMed/NCBI
|
|
24
|
Zamora CA, Zamora MA, Soto JD and Garcés
MA: Myoepithelioma of the hand and carpal tunnel: An unusual cause
of median nerve compression. J Clin Ultrasound. 39:44–47.
2010.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mohamed A, Rosalie S, Taylor K, Fink M,
Coombs C, Ryan M and Kornberg A: Carpal tunnel syndrome secondary
to ganglion cyst in a child. J Child Neurol. 26:630–633.
2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Robinson AJ, Haj Basheer M and Herbert K:
An unusual cause of carpal tunnel syndrome. J Plast Reconstr
Aesthet Surg. 63:e788–e791. 2010.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yücetaş SC and Yildirim A: Comparative
results of standard open and mini open, knifelight
instrument-assisted carpal tunnel release. J Neurol Surg A Cent Eur
Neurosurg. 74:392–399. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Gurpinar T, Polat B, Polat AE, Carkci E,
Kalyenci AS and Ozturkmen Y: Comparison of open and endoscopic
carpal tunnel surgery regarding clinical outcomes, complication and
return to daily life: A prospective comparative study. Pak J Med
Sci. 35:1532–1537. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Trehan SK, Lyman S, Ge Y, Do HT and
Daluiski A: Incidence of nerve repair following endoscopic carpal
tunnel release is higher compared to open release in New York
State. HSS J. 15:143–146. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Worseg AP, Kuzbari R, Korak K, Höcker K,
Wiederer C, Tschabitscher M and Holle J: Endoscopic carpal tunnel
release using a single-portal system. Brit J Plast Surg. 49:1–10.
1996.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Okutsu I, Ninomiya S, Takatori Y and Ugawa
Y: Endoscopic management of carpal tunnel syndrome. Arthroscopy.
5:11–18. 1989.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Chow JC and Hantes ME: Endoscopic carpal
tunnel release: Thirteen years' experience with the Chow technique.
J Hand Surg Am. 27:1011–1018. 2002.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Chow JC: Endoscopic release of the carpal
ligament for carpal tunnel syndrome: 22-month clinical result.
Arthroscopy. 6:288–296. 1990.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Okutsu I, Ninomiya S, Natsuyama M,
Takatori Y, Inanami H, Kuroshima N and Hiraki S: Subcutaneous
operation and examination under nuiversal endoscope. Nihon
Seikeigeka Gakkai Zasshi. 61:491–498. 1987.PubMed/NCBI(In Japanese).
|
|
35
|
Hansen TB and Majeed HG: Endoscopic carpal
tunnel release. Hand Clin. 30:47–53. 2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Tuzuner S, Sherman GM, Ozkaynak S and
Ozcanli H: Endoscopic carpal tunnel release: Modification of
Menon's technique and data from 191 cases. Arthroscopy. 20:721–727.
2004.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Agee JM, Peimer CA, Pyrek JD and Walsh WE:
Endoscopic carpal tunnel release: A prospective study of
complications and surgical experience. J Hand Surg Am. 20:165–172.
1995.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Michelotti B, Romanowsky D and Hauck RM:
Prospective, randomized evaluation of endoscopic versus open carpal
tunnel release in bilateral carpal tunnel syndrome: An interim
analysis. Ann Plast Surg. 73 (Suppl 2):S157–S160. 2014.PubMed/NCBI View Article : Google Scholar
|