1. Introduction
The co-occurrence of psychiatric disorders with
epilepsy has been long known and debated, as the relationship
between the two pathologies is complex and bidirectional (1,2). The
recent International League Against Epilepsy (ILAE) guidelines
recommend early and continued screening, diagnosis and management
for all epilepsy-associated comorbidities in every patient with
epilepsy (3). However, the
prevalence of specific psychiatric comorbidities and correlation
with other clinical characteristics of epilepsy is still a matter
of debate, reflecting different methodologies in research studies
and clinical practice (4,5) and the changing diagnostic criteria for
both epilepsy (6) and psychiatric
disorders (7).
As far as we are aware, to date there are only a few
systematic reviews concerning psychiatric disorders associated with
epilepsy. We were not able to find recent reviews that address the
prevalence of most common psychiatric disorders in patients with
epilepsy. A systematic review published in 2016 addressed the risk
factors for depression in community treated epilepsy cases (based
on research results published between 2000 and 2013) and found that
sociodemographic variables (such as patient age and sex) played the
most important role (8). Another
older systematic review focused on psychosocial predictors of
depression and anxiety in epilepsy patients (9), while more recent reviews assessed
mainly screening and/or diagnostic methods for depression (10) or anxiety (11).
The aim of this study was to describe the prevalence
of specific interictal psychiatric disorders (depressive disorders,
anxiety disorders, psychotic disorders and personality disorders)
in patients with epilepsy and to compare this to the prevalence of
psychiatric disorders in the general population and to assess
possible associations between psychiatric disorders and other
sociodemographic or clinical characteristics of epilepsy
patients.
2. Methods
This review was performed according to the
recommendations of the Preferred Reporting Items of Systematic
Reviews and Meta-Analyses (PRISMA) statement (12).
Search strategy
A systematic literature search using two electronic
databases, namely MEDLINE and ScienceDirect was conducted in
February 2021. The databases were searched using a combination of
keywords: Depression, anxiety, affective disorder, psychotic
disorder, psychosis, personality, traits, epilepsy and seizures.
The search was limited to original research conducted in humans,
published in English language between January 2015 and February
2021. We applied additional filters for age (adults, older than 18
years).
Study inclusion criteria
Only controlled studies (randomized, cohort,
cross-sectional or case-control) were included in this analysis.
Studies were selected if conducted in patients diagnosed with
epilepsy/unprovoked single seizure, if the diagnostic methods used
for epilepsy and psychiatric disorders were reported, if the
characterization of both epilepsy and psychiatric comorbidities was
considered adequate, and if methodology (including statistical
analysis) was clearly described.
Study exclusion criteria
We excluded studies assessing only ictal/peri-ictal
psychiatric manifestations, treatment response or adverse effects.
We also excluded studies assessing psychogenic non-epileptic
seizures that did not report data of psychogenic non-epileptic
seizure patient groups separately, studies using for diagnosis
questionnaires administered online/remotely, studies that evaluated
psychiatric disorders only with self-administered screening tools
and studies that did not include comparative groups. Articles that
did not meet the primary inclusion criteria were also excluded
(e.g.: Case reports, case series, reviews, abstracts, book
chapters, patents, and conference papers) due to the lack of data
for assessment and comparison.
Data extraction
The data extracted from the eligible studies
included: Study setting (including year of publication, type of
research facility and country where the study was conducted), study
type, study objectives, inclusion and exclusion criteria, total
number of subjects included, mean/median age of patients included,
information on each comparative group (description, number of
patients, mean/median age of patients), information on epilepsy
(diagnosis criteria used, epilepsy syndrome, duration of epilepsy,
current seizure frequency), information on antiepileptic and
psychiatric drugs used by patients at the time of inclusion in the
study, information on psychiatric disorders observed (screening
tools used, confirmation tests applied, raters' qualification,
diagnosis code as per Statistical Manual of Mental Disorders
IV/Diagnostic and Statistical Manual for Psychiatric Disorders-5th
edition (DSM-5, 2013), statistical methods, results (prevalence of
psychiatric disorders, statistically significant associations with
other clinical or paraclinical features of epilepsy) and
limitations of each study.
Study quality assessment
The risk of bias for the articles selected for this
review was assessed with the following quality checking
instruments: The RoB 2.0 tool for randomized trials (13), Newcastle-Ottawa Scale (NOS) for
Cohort and Case-Control Studies, respectively (14), Joanna Briggs Institute (JBI)
Critical Appraisal Checklist for analytical cross-sectional studies
(15) and Crombie's Items for
purely descriptive cross-sectional studies.
3. Results
Results of the search
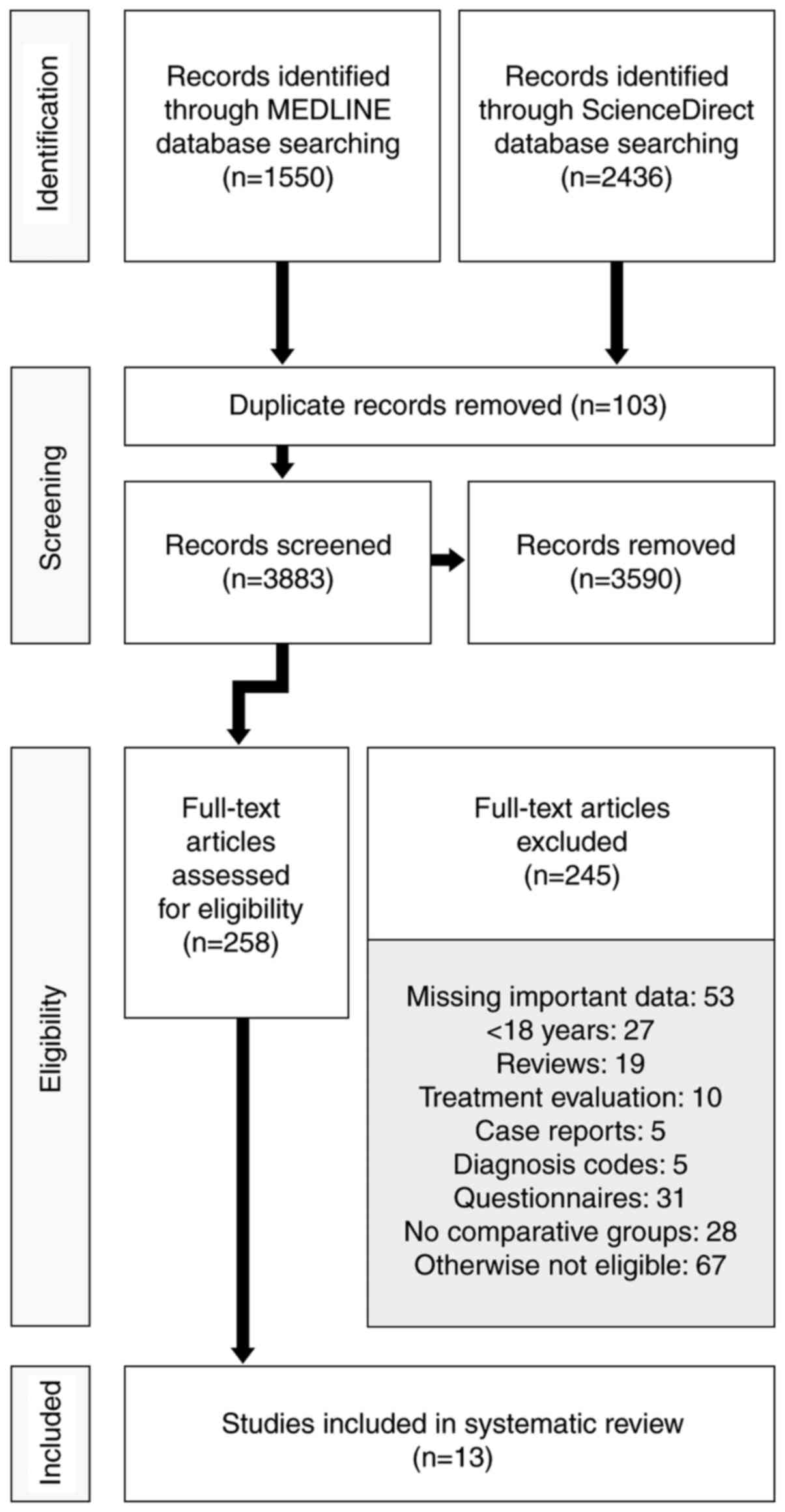
Using the search criteria described above we
identified 3,986 original articles (1,550 articles in MEDLINE
database and 2,436 articles in ScienceDirect database). We assessed
258 full articles for eligibility. Finally, we included in this
analysis 13 articles. The flowchart shown in Fig. 1 details this process.
Description of the studies. This analysis
includes 13 research studies, conducted in 7 countries (Australia,
one study; Brazil, three studies; China, two studies; Germany, two
studies; Japan, one study; Spain, one study; and USA, three
studies).
We included data obtained from one randomized controlled
trial (assessing depression and anxiety improvement in epilepsy
patients when multidisciplinary management was applied) because the
severity of the psychiatric disorders in the control group was
assessed after 12 months (16), two
cohort studies [one designed to detect depression disorders and
anxiety disorders in adult patients with childhood onset epilepsy
(17) and the other one analyzing
psychotic disorders in idiopathic focal epilepsy (18)], one case-control study that
evaluated specifically the psychiatric outcome in drug-resistant
epilepsy patients who underwent surgery vs. patients that were
considered non-eligible for the procedure (because baseline data on
psychiatric disorders diagnosed was solid and because the patients
in the control group were re-assessed by psychiatrist at 6 months,
thus providing information about the time evolution of psychiatric
disorders in people with epilepsy) (19), four studies with a cross sectional
design [first assessing interictal personality in patients with
juvenile myoclonic epilepsy (JME) and in patients with mesial
temporal lobe epilepsy related to hippocampal sclerosis (MTLE/HS)]
(20), second one analyzing
interictal dysphoric disorder and interictal personality in
drug-resistant temporal lobe epilepsy (TLE) (21), the third one evaluating depressive
symptoms and executive functions in patients with TLE (22) and the last one on white matter
changes in patients with TLE and depression (23). We selected for this analysis five
studies that assessed the relation between interictal dysphoric
disorder and other psychiatric disorders in patients with epilepsy
(24), the association between
childhood trauma and psychiatric comorbidities in epilepsy
(25), social adjustment
determinants in JME (26), possible
phenotypes of depression in epilepsy (27) and brainstem sonographic changes in
patients with idiopathic generalized epilepsy (IGE) (28). Importantly, we identified two
studies having the same first author (24,25)
and two studies performed by the same research team (22,23)
that had different research questions, but used a shared sample
population of epilepsy patients that was compared with a different
control group in the first case and with the same control group
(but fewer subjects) in the second case.
In total, 2,192 epilepsy patients were analyzed
(1,252 as sample cases and 940 in some of the control groups). Most
studies (nine) included patients investigated or followed up in
dedicated epilepsy units (of which at least six were tertiary
referral centres, as per authors' descriptions), while only four
studies included patients from general hospitals/practice. A
summary of the selected studies is shown in Table I.
 | Table ISummary of the selected studies. |
Table I
Summary of the selected studies.
| Study
information | Sample | Control |
|---|
| Authors, year
(country) (ref.) | Design | Setting | Total size (N) | Subgroups | Age, years/months
mean (SD), median (IQR) [Range] | Description | Size (N) |
|---|
| Alonso et
al, 2019 (Brazil) (20) |
Cross-sectional | Outpatients,
Epilepsy centre | 200 | MTLE/HS 100 | 40.0 (11.46)
years | Healthy
volunteers | 100 |
| | | | | JME 100 | 30.9 (9.33)
years | | |
| Baldin et
al, 2015 (USA) (17) | Cohort | Outpatients | 257 | NA | 22.5 (3.5)
years | Siblings | 134 |
| | | | | | | External database
(randomly sampled by age at a ratio of 3:1) | 771 |
| de Araújo Filho
et al, 2017 (Brazil) (21) |
Cross-sectional | Outpatients,
Tertiary epilepsy centre | 95 | NA | 40.3 (14.6)
years | Healthy individuals
(community) | 50 |
| Galioto et
al, 2017 (USA) (22) | Cross-sectional,
prospective | Outpatients,
Neurology practice | 51 | TLE without
depression (TLE) 29 TLE with depression (TLE+DEP) 22 | 41.44 (12.18)
[22-63] years 41.32 (8.71) [27-60] years | Depression (DEP)
(hospital-based outpatient psychiatry clinics, community
advertisements) | 31 |
| Kavanaugh et
al, 2017 (USA) (23) |
Cross-sectional | Outpatients,
Neurology practice | 20 | TLE without
depression (TLE) 11 TLE with depression (TLE+DEP) 9 | 37.00 (11.79) years
46.56 (9.14) years | Depression (DEP)
(hospital-based outpatient psychiatry clinics, community
advertisements) | 11 |
| Konishi and
Kanemoto, 2020 (Japan) (18) | Cohort | Adult epilepsy
unit, Late onset PWE | 98 | NA | 66.2 (64.0-68.4)
years | Adult epilepsy
unit, early onset PWE | 775 |
| Labudda et
al, 2018 (Germany) (24) | Not specified | Epilepsy centre
(tertiary referral), PWE | 120 | NA | 35.42 (13.86)
years | Epilepsy centre
(tertiary referral), PNES | 28 |
| Labudda et
al, 2017 (Germany) (25) | Not specified | Epilepsy centre
(tertiary referral) | 120 | NA | 35.42 (13.86)
years | External (age-,
gender- and education-matched, random 1:1 selection) | 120 |
| Paiva et al,
2020 (Brazil) (26) | Not specified | Outpatients,
Epilepsy centre ambulatory (tertiary centre) | 112 | NA | 27.18 (±8.82)
years | Healthy controls
(patient acquaintances, hospital staff members, students) | 61 |
| Ramos-Perdigués
et al, 2016 (Spain) (19) | Prospective
case-control | Epilepsy centre for
presurgical evaluation, Surgical PWE | 85 | NA | 37.97 (12.307)
years | Epilepsy centre for
presurgical evaluation, Non-surgical PWE chronologically paired
with the immediately preceding surgical patient | 68 |
| Rayner et
al, 2016 (Australia) (27) | Not specified | Inpatients,
Comprehensive epilepsy programme | 91 | NA | 40.850 (12.602)
years | Healthy controls
(patient families, broader community) | 77 |
| Shen et al,
2020 (China) (28) | Not specified | Outpatients,
Department of neurology | 46 | NA | 31 (7.13)
years | Healthy subjects
(age- and gender-matched) | 45 |
| Zheng et al,
2019 (China) (16) | Randomized
controlled trial | Outpatients,
Hospital (tertiary referral centre) | 97 | NA | 28 (23.3, 38.8)
years | Outpatients,
hospital (tertiary referral centre), PWE | 97 |
The best represented epilepsy type was TLE (eight
studies included patients with this type of epilepsy), followed by
focal extratemporal lobe epilepsy (ETLE) and IGE (five studies
each). Two articles mentioned the inclusion of patients with
generalized seizures (without any reference to the actual epilepsy
diagnosis in these patients) and another three studies included
patients with other (not mentioned) types of epilepsy or presenting
unspecified or unclassifiable epilepsy/seizures.
Duration of epilepsy (mean/median) was less than 10
years in three studies (16,18,28),
between 10 and 20 years in six studies (18,20,24-27)
and longer than 20 years in three studies (20-22).
Three research articles did not contain clear information on
epilepsy duration.
Seizure frequency and antiepileptic drugs used for
treatment are difficult to summarize, because different reporting
measures were used. A summary of the epilepsy characteristics in
the selected studies is shown in Table
II.
 | Table IISummary of the epilepsy
characteristics. |
Table II
Summary of the epilepsy
characteristics.
| | Epilepsy
characteristics |
|---|
| Study information
Authors, year (country) (ref.) | Diagnosis | Duration: Mean
(SD), median (IQR), [Range] years/months | Seizure
frequency | AED |
|---|
| Alonso et
al, 2019 (Brazil) (20) | Diagnosis criteria:
ILAE Post-surgical MTLE/HS, JME | 27.0 (11.29) years,
MTLE/HS 17.1 (9.50) years, JME | MTLE/HS Controlled
35 (35%); uncontrolled 65 (65%) JME Controlled 61 (61%);
uncontrolled 39 (39%) | Not specified |
| Baldin et
al, 2015 (USA) (17) | Diagnosis criteria:
Not specified Neurotypical cases of childhood-onset epilepsy
(normal clinical and imaging examination) recruited for other
research between 1993-1997, who attained the age of majority
Epilepsy type (n, %): BECTS+ 38 (14.8%); CAE 42 (16.3%); JA/ME 19
(7.4%); Other 158 (61.5%) | Not specified (at
least 15 years after diagnosis) | Not specified | Proportion in
5-year remission, n (%): On medication 15 (23.4); off medication
181 (94.3) |
| de Araújo Filho
et al, 2017 (Brazil) (21) | Diagnosis criteria:
Not specified Pharmacoresistant TLE-MTS | 25.3 (7.4)
years | Not specified | Most frequently
used AED, n (%): Carbamazepine: 58 (61.0); phenobarbital: 41
(43.1); clonazepam: 25 (26.3); Lamotrigine: 21 (22.1), clobazam: 18
(18.9) Number of AED used, n (%): One AED 5 (5.1); two AED: 79
(83.4); three AED 11 (11.5) |
| Galioto et
al, 2017 (USA) (22) | Diagnosis criteria:
Video-EEG monitoring TLE (HS/normal imaging) Lateralization, %: TLE
group right 10.0%; left 56.7%; bilateral 13.3% Lateralization, %:
TLE+DEP group right 20.0%; left 48%; bilateral 29.2% | 20.03 (13.10)
years, TLE 25.73 (15.43) years, TLE+DEP | No. of seizures in
the past month (mean, SD): 0.90 (0.94), TLE No. of seizures in the
past month (mean, SD): 1.00 (1.23), TLE+DEP | Polytherapy: 58.6%,
TLE Polytherapy: 59.1%, TLE+DEP |
| Kavanaugh et
al, 2017 (USA) (23) | Diagnosis criteria:
video-EEG monitoring, MRI Non-lesional TLE Lateralization n/N: Left
only-8/11 and 5/9; right only-0/11 and 1/9; bilateral-3/11 and
3/9 | Not specified Age
at seizure onset, years (mean): 15.64 (15.95) for TLE 13.22 (11.23)
for (TLE+DEP) | No. of seizure in
the past month (0, 1 or 2-n): 0-5, 1-3, 2-3 (TLE) No. of seizure in
the past month (0, 1 or 2-n): 0-7/, 1-1, 2-1 (TLE+DEP) | Current AE
treatment (n): 10, TLE Current AE treatment (n): 8, TLE+DEP |
| Konishi and
Kanemoto, 2020 (Japan) (18) | Diagnosis criteria:
Ictal symptoms, interictal EEG Idiopathic focal epilepsy TLE/ETLE:
Late onset PWE 32/66; control 227/548 | 13.6 (12.4-14.8)
years, early onset PWE 3.35 (2.25-4.45) years, late onset PWE | Not specified | Not specified |
| Labudda et
al, 2018 (Germany) (24) | Diagnosis criteria:
Not specified Epilepsy type, n: Focal (TLE 34, ETLE 66);
generalized 12; unclassifiable: 8 | 18.44 (14.35)
years | Seizure frequency,
% (n): Daily 21.7(26); weekly 34.2(41); monthly 21.7(26); yearly
16.7(20); none within the last year 5.8(7) | Mean number of AED
(mean, SD): 2.19 (0.98) |
| Labudda et
al, 2017 (Germany) (25) | Diagnosis criteria:
History, MRI, seizure semiology Epilepsy Type, n: Focal (TLE 34,
ETLE 23, multi-lobar 26, unknown 17); IGE 12, unclassifiable 8 | 18.44 (14.35)
years | Seizure frequency,
% (n): Daily 21.7(26); weekly 34.2(41); monthly 21.7(26); yearly
16.7(20); none within the last year 5.8(7) | Not specified |
| Paiva et al,
2020 (Brazil) (26) | Diagnosis:
Avignon's consensus JME | 12.72 (8.84)
years | GTC seizures %, n:
None 2.7% (3); good (<1 seizure per year) 74.1% (83); moderate
(1-4 seizures per year) 11.6% (13); or poor (>4 seizures per
year) 0.9% (1) Myoclonic seizures %, n: Good (<5 single seizures
or clusters per month, rare seizures, or occasional seizures)
69.64% (78); moderate (5-14 single seizures or clusters per month,
several seizures, or frequent seizures) 16.1% (18); poor (>15
single seizures or clusters per month or daily seizures) 3.6% (4)
Absence of seizures: None 59.82(67), good (<5 seizures per
month, rare seizures, or occasional seizures) 33.92% (38); moderate
(5-14 seizures per month, several seizures, or frequent seizures)
3.57% (4); poor (>15 seizures per month, frequent seizures, or
daily seizures) 2.67% (3) | Monotherapy, % (n):
84.8% (95); polytherapy, % (n): 14.3% (16) Drug response % (n):
Hard-to-control 17.9(20); easy to control: 69.59(78) |
| Ramos-Perdigués
et al, 2016 (Spain) (19) | Diagnosis Criteria:
Local presurgical protocol Pharmacoresistant epilepsy Idiopathic
aetiology: 66.3% Type of seizures, %: Tonic-clonic 17.6; Partial
complex 70.6 Lateralization: Right 57%; left 35.4%; bilateral 7.6%;
unknown 0 Locus: Temporal 65.4%; extratemporal 28.4%; unestablished
6.2% | Not specified Age
of epilepsy onset, 192.38 (172.08) months for all PWE | Baseline
seizures/month (mean, SD): 16.12 (20.99) | Baseline no. of AED
(mean, SD): Whole study population 2.24 (0.81) |
| Rayner et
al, 2016 (Australia) (27) | Diagnosis criteria:
Not specified Focal epilepsy Locus, %: TLE 76 (46% left hemisphere,
60% lesion-positive); ETLE 24 (32% left hemisphere, 73%
lesion-positive). | 19.150 (12.859)
[2-52] years | Monthly seizure
frequency, mean (SD) [Range] 22.680 (52.166) [1-400] Seizure
frequency (interval, n, %): ≤1/month 21 (23%); fortnightly
(2-7-3/month) 14 (15%); weekly (4-15/month) 36 (40%); more days
than not (≥16/month) 20 (22%) | Polytherapy, n (%):
70 (77%) No. of antiepileptic drugs, mean (SD) [range]: 2.24
(0.993) [1-6] |
| Shen et al,
2020 (China) (28) | Diagnosis criteria:
ILAE guidelines IGE-TCS | 7.70 (5.72)
years | Seizures/month,
mean (SD): 1.81 (2.13) | Not specified |
| Zheng et al,
2019 (China) (16) | Diagnosis criteria:
ILAE, 2001 Seizure type (baseline), n (%): Generalized [control 11
(12.0), intervention 14 (15.2)]; Focal [control 73 (79.3),
intervention 75 (81.5)]; unclassified [control 8 (8.7),
intervention 3 (3.3)] | 78 (36, 156)
months, control 84 (36, 168) months, intervention | Control group,
Baseline seizure frequency, n (%): Low 50 (54.3); high 42 (45.7)
Intervention group, Baseline seizure frequency, n (%): Low 41
(44.6); high 51 (55.4) | Control group,
baseline, n (%): Monotherapy 43 (46.7); polytherapy 49 (53.3)
Intervention group, baseline, n (%): Monotherapy 33 (35.9);
polytherapy 59 (64.1) Control group, baseline treatment regimen, n
(%): ≤2 times daily 78 (84.8); ≥3 times daily 14 (15.2)
Intervention group, baseline treatment regimen, n (%): ≤2 times
daily 83 (90.2); ≥3 times daily 9 (9.8) |
Psychiatric disorders
The self-assessment tools used for the screening or
quantification of psychiatric symptoms in the studies we analyzed
were: Neurobehavior Inventory (NBI), Revised Personality Inventory
(NEO-PI-R) (both tools assess personality traits), Interictal
Dysphoric Disorder Inventory (IDDI) (evaluates interictal dysphoric
disorder symptoms over the last 12 months), Neurological Depression
Disorder Inventory for Epilepsy (NDDI-E) (created to detect current
depression symptoms in epilepsy patients), Beck Depression
Inventory (BDI) and Beck Depression Inventory-II (BDI-II) (for
symptoms of depression), Hospital Anxiety and Depression Scale
(HADS), State-Trait Anxiety Inventory (STAI), Patient Health
Questionnaire-Generalized Anxiety Disorder-7 Items (PHQ-GAD-7) and
Beck Depression Inventory (BAI) (the last three tools rate current
anxiety symptoms).
Psychiatric disorders were confirmed according to
the DSM IV criteria in eight studies, using different structured or
semi-structured clinical interviews such as Structured Clinical
Interview for DSM IV Axis I disorders (SCID I) (two studies)
(20,27), Structured Clinical Interview for DSM
IV Axis II disorders (SCID II) (one study) (20), SCID for DSM-IV Clinician Version
(SCID CV) (one study) (19), MINI
International Neuropsychiatric Interview (M.I.N.I.) (two studies)
(22,23), Mini International Neuropsychiatric
Interview Plus (M.I.N.I.-Plus) (two studies) (24,25),
Structured Clinical Interview for DSM-IV (SCID) (without further
details, one study) (28). DSM
IV-TR criteria were used for diagnosis in two studies: In one study
Diagnostic Interview Survey (DIS-IV) was applied by phone in
subjects and in one control group, while the Composite
International Diagnostic Interview (CIDI) was used for the second
control group (17); in the second
study SCID for Axis I and II was applied (26). Finally, DSM-5 criteria for diagnosis
were utilized in one study only (the method used for diagnosis was
standard psychiatric assessment, without a formal standardized
interview) (21). Diagnosis
criteria employed by the psychiatrist who confirmed the psychiatric
diagnoses were not specified at all in two studies (16,18).
The professional confirming the psychiatric diagnosis was a
psychiatrist in two studies (19,20)
and psychologist in two studies (22,23).
The remaining seven articles did not clearly specify the
qualifications of the person(s) who conducted the psychiatric
interview (17,21,24-28).
The prevalence of any psychiatric disorder was high
for all epilepsy types: 43 and 51%, respectively, in two
populations with JME (20,26), 33% in patients with MTLE/HS that
underwent surgery (20), 43.1% in
patients with pharmacoresistant TLE-MTS (21) and 43.3% in a sample of patients with
epilepsy from a tertiary referral centre (24,25). A
summary of the psychiatric disorders characteristics is shown in
Table III.
 | Table IIISummary of the characteristics of the
psychiatric disorders. |
Table III
Summary of the characteristics of the
psychiatric disorders.
| | Psychiatric
disorders |
|---|
| Study designation
Authors, year (country) (ref.) |
Screening/Self-assessment tests | Confirmation of
diagnosis | DSM version | Training and number
of professionals confirming the diagnosis | Lifetime
current | Diagnosis | Prevalence of
diagnosis (%, n) | Statistical
significance |
|---|
| Alonso et
al, 2019 (Brazil) (20) | NBI | SCID-I | DSM-IV | Psychiatrist
(2) | Not specified | Any psychiatric
diagnosis | | Not reported |
| | NEO-PI-R | SCID-II | | | | JME | 43% | |
| | | | | | | MTLE-HS | 33% | |
| | | | | | | Depression
disorder | | |
| | | | | | | JME | 16% | |
| | | | | | | MTLE-HS | 26% | |
| | | | | | | Anxiety
disorder | | |
| | | | | | | JME | 19% | |
| | | | | | | MTLE-HS | 7% | |
| | | | | | | Personality
disorder | | |
| | | | | | | JME | 8% | |
| | | | | | | MTLE-HS | 0 | |
| | | | | | | Psychiatric
treatment in the past | | |
| | | | | | | Controls | 6% | |
| Baldin et
al, 2015 (USA) (17) | Not applied | DIS-IV (cases,
siblings) | DSM-IV-TR | Two interviewers
with one week DIS training, by phone | NA | DIS Lifetime mood
disorder (major depressive episode, major depressive disorder
single episode, major depressive disorder recurrent, depressive
episode with melancholic features, bipolar I disorder, bipolar II
disorder, bipolar I disorder single manic episode, dysthymic
disorder, manic episode, mixed episode, hypomanic episode) | | |
| | | CIDI (external
controls) | DSM-IV-TR | Not specified | | Adults with
childhood-onset epilepsy | 20.60% | NS |
| | | DISC-IV | DSM-IV (American
Psychiatric Association) | Two interviewers
with one week DIS training, by phone | | Siblings | 23.10% | |
| | | | | | | External
controls | 23.90% | |
| | | | | | | DIS Lifetime
anxiety disorder (generalized anxiety disorder, panic disorder with
and without agoraphobia, agoraphobia, agoraphobia without panic
disorder, social phobia, and specific phobia) | | |
| | | | | | | Adults with
childhood-onset epilepsy | 15.60% | NS |
| | | | | | | Siblings | 20.20% | |
| | | | | | | External
controls | 27.80% | Unmatched adjusted
OR 0.5 (0.3-0.7), P=0.0003 |
| | | | | | | DIS Current mood
disorder (previous year: Major depressive episode, dysthymic
disorder, manic episode, hypomanic episode) | | |
| | | | | | | Adults with
childhood-onset epilepsy | 12.80% | NS |
| | | | | | | Siblings | 11.90% | |
| | | | | | | External
controls | 13.50% | |
| | | | | | | DIS Current anxiety
disorder (previous year: Anxiety disorder, panic disorder with or
without agoraphobia, agoraphobia without panic disorder, social
phobia) | | |
| | | | | | | Adults with
childhood-onset epilepsy | 6.30% | NS |
| | | | | | | Siblings | 8.40% | |
| | | | | | | External
controls | 14.50% | Unmatched adjusted
OR 0.4 (0.2-0.7),P=0.002 |
| | | | | | | DISC Suicide
ideation | | |
| | | | | | | Adults with
childhood-onset epilepsy | 16% | NS |
| | | | | | | Siblings | 13.40% | |
| | | | | | | External
controls | 13.10% | |
| | | | | | | DISC Suicide
attempt | | |
| | | | | | | Adults with
childhood-onset epilepsy | 5.10% | NS |
| | | | | | | Siblings | 2.20% | |
| | | | | | | External
controls | 3.60% | |
| de Araújo Filho
et al, 2017 (Brazil) (21) | IDDI | Standard
psychiatric assessment | DSM-5 | Not specified | Not specified | Axis I psychiatric
disorders | | |
| | NBI | | | | | | | |
| | | ILAE Diagnosis
Criteria for Interictal Personality | | Not specified | Pharmacoresistant
TLE-MTS | 43.1% (41) | | |
| | | ILAE Diagnosis
Criteria for Interictal Dysphoric Disorder | Not specified | Major depressive
disorder | | | | |
| | | | | | | Pharmacoresistant
TLE-MTS | 21 | P=0.001 |
| | | | | | | Controls | 6 | |
| | | | | | | Generalized anxiety
disorder | | |
| | | | | | | Pharmacoresistant
TLE-MTS | 15 | P=0.001 |
| | | | | | | Controls | 5 | |
| | | | | | | Conversion
disorder | | |
| | | | | | | Pharmacoresistant
TLE-MTS | 9 | P=0.001 |
| | | | | | | Controls | 0 | |
| | | | | | | Interictal
psychosis | | |
| | | | | | | Pharmacoresistant
TLE-MTS | 5 | NS |
| | | | | | | Controls | 0 | |
| | | | | | | Interictal
dysphoric disorder (IDDI) | | |
| | | | | | | Pharmacoresistant
TLE-MTS | 18.4% (18) | P=0.001 |
| | | | | | | Controls | 8% (4) | |
| | | | | | | Interictal
personality (NBI) | | |
| | | | | | | Pharmacoresistant
TLE-MTS | 37.9% (36) | P=0.001 |
| | | | | | | Controls | 8% (4) | |
| Galioto et
al, 2017 (USA) (22) | Not applied | M.I.N.I. | DSM-IV | Neuropsychologist
(1, blinded to other procedures) | Not specified | Major depressive
disorder | Not specified | Not assessed |
| | | HAM-D | | Neuropsychologist
(1, blinded to other procedures) | Not specified | Dysthymic
disorder | Not specified | |
| | | | | | Current | Current major
depressive episode | | |
| | | | | | | TLE (HS/normal
imaging) with depression | 18.20% | |
| | | | | | | Depression | 22.60% | |
| Kavanaugh et
al, 2017 (USA) (23) | Not applied | M.I.N.I. | DSM-IV | Neuropsychologist
(1, blinded to other procedures) | Not specified | Major depressive
disorder | Not specified | Not assessed |
| | | HAM-D | Neuropsychologist
(1, blinded to other procedures) | Not specified | Dysthymic
disorder | | | |
| Konishi and
Kanemoto, 2020 (Japan) (18) | Not applied | Interview: Clinical
criteria for psychosis (no differentiation between
ictal/interictal) | Not specified | Psychiatrist,
number not specified | Lifetime | History of
psychosis (first visit) | | |
| | | | | | | PWE screened
(2568) | 2.5% (54) | NA |
| | | | | | | Focal idiopathic
epilepsy | 4.3% (38) | |
| | | | | | | Early onset focal
idiopathic epilepsy | 38.77% (38) | P=0.016 |
| | | | | | | Late onset focal
idiopathic epilepsy | 0 | |
| | | | | | | TLE | 8.50% | NA |
| | | | | | | Type of
psychosis | | |
| | | | | | | Interictal | 32 | |
| | | | | | | Predominantly
postictal | 6 | |
| | | | | | | Both, interictal
and postictal | 2 | |
| Labudda et
al, 2018 (Germany) (24) | IDDI | M.I.N.I.-Plus | DSM-IV | The interviews were
carried out by 2 authors (affiliated to a Psychology Department),
videotaped and re-evaluated by at least 1/2 further interviewers
experienced in this procedure when diagnostic uncertainty | Current | At least 1 current
axis I psychiatric disorder | | |
| | NDDI-E | | | | | | | |
| | STAI | | | | | | | |
| | SCL-90-R | | | | | | | |
| | | PDS | | The interviews were
carried out by 2 authors (affiliated to a Psychology Department),
videotaped and re-evaluated by at least 1/2 further interviewers
experienced in this procedure when diagnostic uncertainty | | PWE | 43.3% (52) | (χ2
>5.47, |
| | | | | | | PNES | 67.9 % (19) | P<0.022) |
| | | | | | | At least 1
affective disorder | | NS |
| | | | | | | PWE | 21.7% (26) | |
| | | | | | | PNES | 28.6% (8) | |
| | | | | | | Major depressive
episode | | |
| | | | | | | PWE | 5% (6) | |
| | | | | | | PNES | 17.9% (5) | |
| | | | | | | Recurrent
depressive disorder (with recent episode) | | |
| | | | | | | PWE | 9.2% (11) | |
| | | | | | | PNES | 10.7% (3) | |
| | | | | | | Dysthymia | | |
| | | | | | | PWE | 7.5% (9) | |
| | | | | | | PNES | 0 | |
| | | | | | | Bipolar
disorder | 0 | |
| | | | | | | At least 1 anxiety
disorder | | (χ2
>5.47, |
| | | | | | | PWE | 30.8% (37) | P<0.022) |
| | | | | | | PNES | 64.3% (18) | |
| | | | | | | Social phobia | | |
| | | | | | | PWE | 9.2% (11) | |
| | | | | | | PNES | 10.7% (3) | |
| | | | | | | Specific
phobia | | |
| | | | | | | PWE | 2.5% (3) | |
| | | | | | | PNES | 7.1% (2) | |
| | | | | | | Panic disorder
alone | | |
| | | | | | | PWE | 0.8% (1) | |
| | | | | | | PNES | 0 | |
| | | | | | | Agoraphobia
alone | | |
| | | | | | | PWE | 5% (6) | |
| | | | | | | PNES | 14.3% (4) | |
| | | | | | | Panic disorder with
agoraphobia | | |
| | | | | | | PWE | 3.3% (4) | |
| | | | | | | PNES | 21.4% (6) | |
| | | | | | | Generalized anxiety
disorder | | |
| | | | | | | PWE | 4.2% (5) | |
| | | | | | | PNES | 10.7% (3) | |
| | | | | | |
Obsessive-compulsive disorder | | |
| | | | | | | PWE | 2.5% (3) | |
| | | | | | | PNES | 3.6% (1) | |
| | | | | | | Adjustment
disorder | | |
| | | | | | | PWE | 5.8% (8) | |
| | | | | | | PNES | 3.6% (1) | |
| | | | | | | Substance
dependence | | |
| | | | | | | PWE | 1.7% (2) | Not reported |
| | | | | | | PNES | 3.6% (1) | |
| | | | | | | Eating
disorder | | |
| | | | | | | PWE | 0.8% (1) | Not reported |
| | | | | | | PNES | 0 | |
| | | | | | | Psychotic
episode | | |
| | | | | | | PWE | 3.3% (4) | Not reported |
| | | | | | | PNES | 0 | |
| | | | | | | Posttraumatic
stress disorder | | |
| | | | | | | PWE | 9.2% (11) | Not reported |
| | | | | | | PNES | 32.1% (9) | |
| | | | | | | Interictal
dysphoric disorder | | |
| | | | | | | PWE | 35% (42) | NS |
| | | | | | | PNES | 39% (11) | |
| | | | | | | Interictal
dysphoric disorder + other current psychiatric disorder | | |
| | | | | | | PWE | 27.5% (33) | Not assessed |
| Labudda et
al, 2017 (Germany) (25) | CTQ | M.I.N.I.-Plus
(Mini, version 5.0.0) | DSM IV | Interviews were
carried out by 4 authors with experience and training in clinical
interviews (affiliated to a Psychology department), videotaped and
re-evaluated by at least 1 further interviewer experienced in this
procedure when diagnostic uncertainty | Current | At least 1
diagnosis | | |
| | FBS | | | | | | | |
| | | PDS | | Interviews were
carried out by 4 authors with experience and training in clinical
interviews (affiliated to a Psychology department), videotaped and
re-evaluated by at least 1 further interviewer experienced in this
procedure when diagnostic uncertainty | | PWE | 43.3% (52) | Not assessed |
| | | The Epilepsy
Addendum for Psychiatric Assessment | Interviews were
carried out by 4 authors with experience and training in clinical
interviews (affiliated to a Psychology department), videotaped and
re-evaluated by at least 1 further interviewer experienced in this
procedure when diagnostic uncertainty | | At least 1
affective disorder | | | |
| | | | | | | PWE | 21.7% (26) | Not assessed |
| | | | | | | At least 1 anxiety
disorder | 30.8% (37) | |
| | | | | | | PWE | | Not assessed |
| Paiva et al,
2020 (Brazil) (26) | STAI | SCID for Axis I and
II (89.3% of PWE) | DSM-IV-TR | Not specified (all
authors affiliated to a Psychiatry department) | Not specified | Psychiatric
disorders | | Not assessed |
| | SAS | | | | | ME | 51% | |
| | | | | | | Anxiety
disorder | | |
| | | | | | | ME | 31% | |
| | | | | | | Personality
disorder | | |
| | | | | | | JME | 11% | |
| | | | | | | Depressive
disorder | | |
| | | | | | | JME | 9% | |
| | | | | | | Overlap | | |
| | | | | | | ME | 8% (3 patients with
an anxiety disorder and substance abuse; 2 patients with depressive
disorder and substance abuse; and 3 patients with depressive
disorder and personality disorder) | |
| Ramos-Perdigués
et al, 2016 (Spain) (19) | HADS | SCID-CV | DSM-IV | Psychiatrist
(1) | Not specified | Baseline affective
disorder (major depressive episodes, recurrent depression,
dysthymic disorder, affective disorder due to a medical condition
or substance disorder, adjustment disorder and bipolar
disorder) | | |
| | SCL-90-R | | | | | | | |
| | | | | ILAE Classification
Proposal for Interictal Dysphoric Disorder and Interictal
Personality | | Pharmacoresistant
epilepsy | 22% | NS |
| | | | | | | Surgical group | 23.20% | |
| | | | | | | Non-surgical
group | 20.60% | |
| | | | | | | Baseline psychotic
disorder (schizophrenia or schizoaffective disorder and other
psychosis) | | |
| | | | | | | Pharmacoresistant
epilepsy | 4% | NS |
| | | | | | | Surgical group | 4.90% | |
| | | | | | | Non-surgical
group | 2.90% | |
| | | | | | | Baseline anxiety
disorder (panic disorder, phobia, obsessive compulsive disorder,
posttraumatic stress disorder, and other anxiety disorders) | | |
| | | | | | | Pharmacoresistant
epilepsy | 15.30% | NS |
| | | | | | | Surgical group | 15.90% | |
| | | | | | | Non-surgical
group | 14.70% | |
| | | | | | | Baseline eating
disorder | 0 | NA |
| | | | | | | Baseline drug
use | | |
| | | | | | | Pharmacoresistant
epilepsy | 2% | NS |
| | | | | | | Surgical group | 1.20% | |
| | | | | | | Non-surgical
group | 2.90% | |
| | | | | | | Baseline conduct
disorder | 0 | NA |
| | | | | | | Interictal
dysphoric disorder | | |
| | | | | | | Pharmacoresistant
epilepsy | 27.10% | NS |
| | | | | | | Surgical group | 22.80% | |
| | | | | | | Non-surgical
group | 25% | |
| | | | | | | Interictal
psychotic disorder | 0 | NS |
| Rayner et
al, 2016 (Australia) (27) | NDDI- E | SCID-I | DSM-IV | Not specified | Lifetime | Lifetime history of
depressive disorder | | |
| | PHQ-GAD-7 | | | | | | | |
| | ESI-55 | | | | | Focal epilepsy | 40% (36) | Not assessed |
| | FACES-IV | | | | | | | |
| | AMI | | | | Current | Current major
depressive episode or Depressive disorder not otherwise
specified | | |
| | | | | | | Focal epilepsy | 23% (21) | Not assessed |
| | | | | | | Current major
depressive disorder | | |
| | | | | | | Focal epilepsy | 10 | Not assessed |
| | | | | | | Current dysthymic
disorder | | |
| | | | | | | Focal epilepsy | 4 | Not assessed |
| | | | | | | Current minor
depressive disorder | | |
| | | | | | | Focal epilepsy | 7 | Not assessed |
| Shen et al,
2020 (China) (28) | NDDI-E | SCID | DSM-IV | Not specified | Not specified | Depression | | |
| | BDI-II | | | | | I GE-TCS | 34.78% (16) | NA |
| | | | | | | Without
depression | | |
| | | | | | | IGE-TCS | 65.21% (30) | NA |
| Zheng et al,
2019 (China) (16) | BDI | Not Specified | Not specified | Psychiatrist | Not specified | Not specified | Not specified | Not specified |
| | BAI | | | | | | | |
Mood/affective disorders
Prevalence of current mood disorders (major
depressive episode, dysthymic disorder, manic episode, hypomanic
episode during the previous year) was 12.8% in adults with
neurotypical childhood onset epilepsy (comparison with both control
groups-siblings and external controls-was not statistically
significant) (17). Current major
depressive episode was present in 18.2% of the patients from a
population with TLE and depression (22). In a general population of epilepsy
patients from a third referral centre, 21.7% were diagnosed with at
least one affective disorder (24,25)
(5% presented major depressive episode, 9.2% recurrent depressive
disorder and 7.5% dysthymia, while none of these patients was
diagnosed with bipolar disorder), without statistical significance
when prevalence was compared with psychogenic non-epileptic
seizures patients in the control group (24). In focal epilepsy (mostly
pharmacoresistant) current major depressive episode or other
depressive disorders (major depressive disorder, minor depressive
disorder, dysthymia) had a prevalence of 23% (27).
Lifetime mood disorders (major depressive episode,
major depressive disorder single episode, major depressive disorder
recurrent, depressive episode with melancholic features, bipolar I
disorder, bipolar II disorder, bipolar I disorder single manic
episode, dysthymic disorder, manic episode, mixed episode,
hypomanic episode) had a prevalence of 20.6% in adults with
childhood-onset epilepsy, statistically not significant when
compared with the prevalence of lifetime mood disorders in both
control groups (sibling and external controls) (17). The prevalence of lifetime history of
depression in focal epilepsy (mostly pharmacoresistant) was 40%
(27).
Prevalence of depressive disorder (not specified if
lifetime/current) was 16 and 9%, respectively, in two populations
of patients with juvenile myoclonic epilepsy (20,26)
and 26% in patients with MTLE/HS, late post-surgically (20). Prevalence of major depressive
disorder was 22.1% in patients with pharmacoresistant TLE-MTS,
significantly higher than in healthy individuals from the community
(21). Prevalence of affective
disorders (including major depressive episodes, recurrent
depression, dysthymic disorder, affective disorder due to a medical
condition or substance disorder, adjustment disorder and bipolar
disorder, but not specified if lifetime/current) was 22% in
pharmacoresistant epilepsy patients assessed for epilepsy surgery
(19). Finally, the incidence of
depression (no further details regarding the exact DSM IV diagnosis
or if current/lifetime) was 34.78% in patients with idiopathic
generalized epilepsy (with tonic-clonic seizures) (IGE TCS)
(28).
Suicidal risk and suicidal attempt, evaluated by
Diagnostic Interview Survey for Children (DISC-IV), in adults with
childhood-onset epilepsy had a prevalence of 16 and 5.1%,
respectively, and statistical analysis (including comparison with
siblings and external controls) showed no relation between suicidal
thoughts and behaviors and epilepsy (17).
In a study that examined the relationship between
white matter integrity [assessed by Diffusion Tensor Imaging (DTI)]
and depression in a small group of patients with TLE and depression
(major depressive disorder or dysthymic disorder, as per DSM-IV
criteria) (23), the severity of
the depression [The 17-item Hamilton Depression Rating Scale
(HAM-D) score] was significantly and negatively correlated with the
matter integrity in non-fronto-temporo-limbic areas
[non-fronto-temporo-limbic fractional anisotropy (non-FTL-FA)
composite score, P<0.05] and showed a similar trend for
fronto-temporo-limbic areas (P=0.06), while in the control group
(patients with depression, without epilepsy) the correlation was
not statistically significant.
When the contribution of depression (major
depressive disorder, dysthymic disorder) to executive functioning
was assessed in TLE patients, it was observed that epilepsy
patients with depression (not specified if current or lifetime)
performed worse than epilepsy patients without depression in verbal
fluency test for category switching (P=0.04) (22).
One study investigated two possible symptom-based
phenotypes of depression (named by authors cognitive and somatic,
respectively) in focal epilepsy (27). For the cognitive depression group,
the authors described higher rates of parasuicidal or suicidal
thoughts, feelings of worthlessness, delusions of guilt, dysphoric
mood than in the somatic depression (but the intergroup comparison
showed no statistical significance for these DSM-IV symptoms). When
these patients were compared with non-depressed epilepsy patients;
they were more likely to have a left-lateralized seizure focus
(P=0.034), but there were no other differences in any other
epileptological variables or in anticonvulsant or psychotropic
pharmacotherapy. Compared with healthy subjects, patients with
cognitive depression exhibited significantly reduced semantic and
episodic autobiographic memory across all life periods (including
significantly worse overall semantic and episodic recollection) and
significantly reduced delayed recall across auditory-verbal
(P=0.032) and visual domains (P=0.002) on the Wechsler Memory
Scale-IV (WMS-IV) subtests, in the context of intact immediate
learning (P>0.050). Instead, somatic depression patients
presented significant higher rates of somatic symptoms (appetite
changes, sleep changes) and anhedonia (for all P<0.01) and there
were no differences when compared with epilepsy patients without
depression in any other epileptological variables or in
anticonvulsant or psychotropic pharmacotherapy. Somatic depression
patients had more seizures and greater variability in seizure
frequency than the cognitive phenotype (monthly average seizure
frequency 17.5 and 4, respectively) and performed worse than
healthy subjects in childhood episodic, early adulthood semantic,
overall episodic, and delayed visual recall, but these inter-group
differences were not statistically significant. Odds ratio (OR)
analysis suggested that, compared with patients with somatic
depression, depressed patients with the cognitive phenotype were
more likely to have semantic autobiographic memory deficit (i.e.,
Autobiographical Memory Interview (AMI) subscale score b 50; 95%
CI=0.162-81.705), episodic autobiographic memory deficit (i.e., AMI
subscale score b 16; 95% CI=0.316-16.512) and impaired immediate
verbal learning (i.e., WMS-IV score ≤8; 95%). Psychosocial and
demographic features of the two phenotypes of depression [age,
relationship status, level of depressive symptoms (NDDI-E), level
of family satisfaction (The Family Adaptability and Cohesion
Scale-Fourth edition (FACES-IV), symptoms of anxiety (PHQ-GAD-7),
quality of life (The Epilepsy Surgery Inventory-55 Items (ESI-55)
or psychotropic medications] were not significantly different
between groups (P>0.05 for all comparisons) (27).
In a study assessing brainstem echogenicity in
depressed patients with IGE-TCS there was no significant difference
in third ventricle width between epilepsy patients with and without
depression (P=0.293), but more epilepsy patients with depression
exhibited hypoechogenic brainstem raphe (P=0.000) (28).
Interictal dysphoric disorder is a psychiatric
disorder assumed to be specific for epilepsy patients. Prevalence
of interictal dysphoric disorder was 35% in a general population of
epilepsy patients (associated in 27% of the total cases with mood
disorder, anxiety disorder, both mood and anxiety disorder,
substance abuse), 39% in a population with psychogenic
non-epileptic seizure (both epilepsy patients and psychogenic
non-epileptic seizure patients were assessed in a tertiary centre
and comparison between the two groups did not show a statistical
difference) (24), 18.4% in
resistant TLE-MTS (significantly higher than in healthy subjects
from the control group) (21) and
27.1% in a group of patients with pharmacoresistant epilepsy (also
significantly higher than in the control group) (19). In a study of prevalence of
interictal dysphoric disorder in epilepsy patients it was
demonstrated that epilepsy patients with interictal dysphoric
disorder had more frequently than epilepsy patients without
interictal dysphoric disorder at least one current psychiatric
disorder (χ2=32.68, P<0.001), at least one current
affective disorder [major depressive episode, recurrent depressive
disorder, dysthymia (χ2=25.64, P<0.001)] and at least
one current anxiety disorder [social phobia, specific phobia, panic
disorder alone, agoraphobia alone, panic disorder with agoraphobia,
generalized anxiety disorder (GAD), obsessive compulsive disorder,
adjustment disorder (χ2=17.35, P<0.001)], and that
66% of epilepsy patients without a current psychiatric comorbidity
had a diagnosis of a past psychiatric disorder (recurrent
depressive disorder currently remitted and substance addiction)
(24). Also, epilepsy patients with
interictal dysphoric disorder and other psychiatric disorders had
similar symptoms with epilepsy patients with interictal dysphoric
disorder alone (euphoria, Fisher's exact test: P=1.0; irritability,
Fisher's exact test: P=0.698) (24). In patients with drug-resistant
epilepsy assessed for surgery, the presence of interictal dysphoric
disorder was correlated with epilepsy location: 33.3% of patients
had no loci established, 8.3% had extratemporal loci, and 58.3% had
temporal loci (P=0.002) (19).
Analysis of the diagnostic superposition between interictal
dysphoric disorder and DSM Axis I psychiatric disorders in patients
with TLE-MTS showed that none of the interictal dysphoric disorder
patients and none of the healthy subjects in the control group had
a DSM Axis I psychiatric disorder (21). Multivariate logistic regression
analysis revealed that the significant risk factors for interictal
dysphoric disorder in patients with pharmacoresistant TLE-MTS were
the presence of left-sided mesial temporal sclerosis (OR=3.22;
P=0.008), previous psychiatric treatment (OR=4.29; P=0.007) and the
use of more than one antiepileptic drug (OR=2.73; P=0.02) (21).
Anxiety disorders
Current anxiety disorders (anxiety disorder, panic
disorder with or without agoraphobia, agoraphobia without panic
disorder, social phobia during the previous year) had a prevalence
of 6.3% among adult patients with childhood onset epilepsy. In this
case the prevalence of current anxiety disorders was not
statistically significant different between cases and siblings, but
when cases were compared with external controls, current anxiety
disorders were associated with a significantly decreased odds of
epilepsy (17). At least one
anxiety disorder was present in 30.8% of a sample of epilepsy
patients from a tertiary referral centre (social phobia in 9.2%,
specific phobia in 2.5%, panic disorder alone in 0.8%, agoraphobia
alone in 5%, panic disorder with agoraphobia in 3.3%, GAD in 4.2%
and adjustment disorder in 5.8%). The overall comparison with a
group of patients with psychogenic non-epileptic seizures showed
that for all disorders mentioned above (except adjustment
disorder), the prevalence was higher in the psychogenic
non-epileptic seizures group (24).
Lifetime anxiety disorders (generalized anxiety
disorder, panic disorder with and without agoraphobia, agoraphobia,
agoraphobia without panic disorder, social phobia, and specific
phobia) were present in 15.6% of adults with childhood onset
epilepsy. As in the case of current anxiety disorders, in this
study the prevalence of lifetime anxiety disorders was not
significantly different between cases and siblings, but was
significantly higher in the external controls than in epilepsy
patients (17).
Where lifetime or current was not specified, anxiety
disorder was present in 19 and 31%, respectively in two populations
of patients with JME (20, 26), in 7% of the post-surgical patients
with MTLE/HS (20) and in 15.3% of
patients with pharmacoresistant epilepsy (diagnosed with panic
disorder, phobia, obsessive compulsive disorder, posttraumatic
stress disorder, and other anxiety disorders) (19). Prevalence of generalized anxiety
disorder in pharmacoresistant TLE-MTS was 15.78% (significantly
higher than in healthy controls, P=0.001) (21).
In patients with JME, the presence of anxiety
disorder (not specified if current or lifetime) was moderately
correlated with a higher frequency of generalized tonico-clonic
seizures (GTCS) (τ=-0.320; P=0.008) and with worse familiar
relationship adjustment [Social Adjustment Scale (SAS) family
score, (τ=0.241; P=0.025)]. There was no other significant
correlation between the presence of anxiety disorder and other
social adjustment domains (SAS scores for work, leisure/social,
economic or total) (26).
Psychotic disorders
Only four studies reported the prevalence of
psychotic disorders in epilepsy patients. The prevalence of
lifetime psychosis (ictal or interictal), as reported historically
by patients during their first psychiatric assessment in epilepsy
centre was 2.5% in a general epilepsy patient population (2,568
epilepsy patients screened), 4.3% in focal idiopathic epilepsy and
even higher in TLE (8.5%). In this specific study, interictal
psychosis was retrospectively diagnosed in 4.12% of the focal
idiopathic epilepsy cases (18).
When DSM criteria were used, 3.3% of the epilepsy
patients from a tertiary epilepsy centre were diagnosed with
current psychotic episode (24).
Psychotic disorders (schizophrenia, schizoaffective disorder, other
psychosis) had a prevalence of 4% in pharmacoresistant epilepsy
(19) and interictal psychosis had
a prevalence of 5% in pharmacoresistant TLE-MTS (not significant in
comparison with controls) (21).
Interictal psychotic disorder (as per ILAE proposed criteria) was
not diagnosed in any of the patients with drug resistant epilepsy
assessed for surgery eligibility (19).
The only study that specifically investigated the
presence of psychosis in focal epilepsy without central nervous
system diseases found a significant difference between the
prevalence of psychosis (predominantly interictal, but also
peri-ictal) between patients with late-onset epilepsy (at >49
years) and patients with early onset epilepsy (at <49 years),
basically with no cases in the old-onset group (P=0.016).
Significant determinants associated with psychosis in this study
were duration of illness (P=0.000001) and presence of temporal lobe
epilepsy (P=0.000343), while sex and age at examination were not
contributory to psychosis (18).
Personality disorders
Personality disorders (assessed using DSM criteria)
were present in 8% and respectively 11% of the JME patients
assessed in two studies (20,26)
and in none of the post-surgical MTLE/HS cases assessed in one
study (20).
A study that specifically investigated personality
profile in JME and post-surgical MTLE/HS patients using NBI and
NEO-PI-R found a positive correlation between the neuroticism
domain of NEO-PI-R and psychiatric symptoms in both MTLE/HS
(r=0.201; P=0.003) and JME (r=0.145; P=0.010) groups. Also,
post-surgical MTLE-HS patients with psychiatric diagnoses
(depressive disorders, anxiety disorders and personality
disorders), had higher total NBI scores than those with no
psychiatric symptoms (P<0.001) and JME patients with psychiatric
diagnoses and uncontrolled GTCS had higher total NBI scores than
those with no psychiatric symptoms/controlled GTCS (P=0.001 and
P=0.032, respectively). In patients with psychiatric symptoms,
13/20 NBI traits (65%) were higher in the MTLE/HS group than in the
JME group (9/20, 45%) (P=0.05) (20).
Interictal personality, a behavioral condition that
could be associated with epilepsy (assessed with NBI) had a
prevalence of 37.9% in pharmacoresistant TLE (significantly higher
than in controls) (21). When
analysis of the diagnostic superposition between interictal
personality and DSM Axis I psychiatric disorders was conducted, 15
(41.6%) of the epilepsy patients with interictal personality had a
DSM Axis I psychiatric disorder (major depressive disorder 66.6%,
interictal psychosis 18.7%, conversion disorder 13.4%), while none
of the subjects in the control group with DSM Axis I psychiatric
disorders demonstrated superposition with interictal personality.
Multivariate logistic regression models showed that significant
risk factors for interictal personality are the presence of
bilateral mesial temporal sclerosis (OR=3.27; P=0.008), longer
disease duration (OR=3.39; P=0.006) and the presence of major
depressive disorder (21).
Other important associations
In a study assessing the prevalence of interictal
dysphoric disorder and interictal personality, significantly more
patients with drug-resistant TLE-MTS had a history of previous
psychiatric treatment (P=0.001), family history of epilepsy
(P=0.001), and family history of psychiatric disorders (P=0.001)
(21).
Current psychiatric disorders in a general
population of epilepsy patients are associated with childhood
maltreatment experiences (25).
Patients with current psychiatric disorders [major depressive
episode, recurrent depressive disorder, dysthymia, social phobia,
specific phobia, panic disorder alone, agoraphobia alone, panic
disorder with agoraphobia, generalized anxiety disorder,
obsessive-compulsive disorder, adjustment disorder, substance
dependence, eating disorder, psychotic episode-diagnosed as per DSM
IV criteria or posttraumatic stress disorders-diagnosed with
Posttraumatic Diagnostic Scale (PDS)] had suffered significantly
more childhood maltreatment experiences [higher Childhood Trauma
Questionnaire (CTQ) scores-total score (t=3.41, P=0.001), emotional
abuse (t=2.83, P=0.006) and emotional neglect (t=3.47, P=0.001)];
had higher Fragebogen zu Belastenden Sozialerfahrungen (FBS) scores
(t=3.75, P<0.001) and significantly more reported severe
emotional abuse (χ2=13.72, P≤0.001), emotional neglect
(χ2=12.28, P≤0.001), and physical abuse
(χ2=3.98, P=0.046). Age at epilepsy onset, epilepsy
duration, number of different seizure types and number of patients
in each seizure frequency category did not differ between epilepsy
patients with psychiatric disorders and epilepsy patients without
psychiatric disorders. Direct logistic regression showed that CTQ
total score, FBS score and epilepsy-related variables, i.e., age of
epilepsy onset, epilepsy duration, number of seizure types and
seizure frequency, were all predictors for a current psychiatric
disorder [χ2 (9, 120)=27.13, P<0.001, Nagelkerke
R2=0.28) (25).
In a prospective case-control study, designed to
evaluate the psychiatric outcome in drug-resistant epilepsy
patients that underwent surgery, compared with those who did not,
existing differences in baseline affective disorders (major
depressive episodes, recurrent depression, dysthymic disorder,
affective disorder due to a medical condition or substance
disorder, adjustment disorder and bipolar disorder), psychotic
disorders (schizophrenia or schizoaffective disorder and other
psychosis), anxiety disorders (panic disorder, phobia, obsessive
compulsive disorder, posttraumatic stress disorder, and other
anxiety disorders), eating disorder, drug use, conduct disorder
(diagnosed as per DSM-IV, not specified if current or lifetime),
interictal dysphoric disorder and interictal psychotic disorder
(diagnosed as per ILAE Classification Proposal) did not depended on
the presence vs. absence of complex partial seizures (CPS), the
cerebral hemisphere involved (left vs. right), and seizure
localization (temporal vs. extratemporal vs. unestablished). Paired
comparisons between baseline and 6 months after surgery showed no
statistical change in all psychiatric disorders mentioned above in
any group (19).
4. Discussion and limitations
This systematic review examined whether current
literature provides quality information on the prevalence and risk
factors for psychiatric disorders in epilepsy patients. In order to
properly treat epilepsy patients with psychiatric comorbidities, it
is very important to have an accurate psychiatric diagnosis, in
patients who are usually attended by neurologists or
epileptologists. Although in recent years numerous screening tools
have been developed and validated for the screening of anxiety
disorders (29) and depressive
disorders (30-33),
in epilepsy patients, these instruments cannot replace a formal
psychiatric assessment (34).
Unfortunately, most recent studies reporting data on psychiatric
comorbidities in epilepsy used these type of instruments and, as a
result, only psychiatric symptoms associated with epilepsy were
reported and analyzed.
The overall reported prevalence of mood/affective
disorders was 12.8 to 34.78%, while the prevalence of specific
diagnoses as per DSM-IV is difficult to assess. In general, a
higher prevalence of mood/affective disorders was reported when the
temporal characteristics (lifetime vs. current) were not specified.
Current and lifetime mood disorders appear to be less frequently
encountered in IGE and more prevalent in focal drug-resistant
epilepsy (mainly TLE). In TLE, the severity of depression was found
to be associated with white matter anomalies in
non-fronto-temporo-limbic areas and with cognitive impairment
(executive function). In focal epilepsies, cognitive depression was
found to be associated with a left-lateralized seizure focus (no
other associations were found between depression and
epileptological variables, antiepileptic drugs or psychotropic
treatments in epilepsy patients with or without depression) and
with cognitive impairment (semantic and autobiographic memory,
delayed auditory-verbal and visual recall). In IGE, depression was
associated with hypoechogenic brainstem raphe (without any
difference on third ventricle width between epilepsy patients with
or without depression).
Suicidal risk was reported only for adults with
childhood onset epilepsy and in this population, it beared no
significant relation with epilepsy. This risk was lower than
previously reported (35), but the
childhood onset epilepsies often have a more favorable course, with
remission in adulthood.
Interictal dysphoric disorder is a highly
controversial epilepsy-specific psychiatric disorder, that is not
recognized by DSM but has specific diagnosis criteria developed by
epileptologists (36). Its
prevalence ranged between 18.4% in resistant TLE-MTS to 35% in a
general population of patients with epilepsy. The results of two
studies are contrasting: In a general sample of epilepsy patients,
interictal dysphoric disorder was more frequently present when
other psychiatric disorders were present and interictal dysphoric
disorder symptoms frequencies were similar in patients with or
without interictal dysphoric disorder, while in resistant TLE-MTS
none of the patients with interictal dysphoric disorders had an DSM
Axis I psychiatric disorder (21,24).
In drug-resistant TLE, the risk factors for interictal dysphoric
disorder were left-sided MTS, previous psychiatric treatment and
the use of more than one antiepileptic drug. In drug-resistant
epilepsies assessed for surgery, the prevalence of interictal
dysphoric disorder was higher in TLE patients as well.
Prevalence of anxiety disorders was between 5.6% in
adults with childhood onset epilepsy and 30.8% in a sample from a
general population of epilepsy patients. As in the case of
mood/affective disorders, the prevalence of specific diagnoses and
temporal characteristics were hard to systemize, but current
anxiety disorders appeared to have a higher prevalence. We
speculate that this trend is related to the long duration of
epilepsy and to the higher severity of seizures in selected
studies. In JME, the presence of anxiety disorders was correlated
with a higher frequency of GTCS and with worse familial adjustment
(no other correlations were found between the presence of anxiety
disorder and other social adjustments domains such as work,
leisure/social or economic).
Psychotic disorders were found to have a low
prevalence across all epilepsy types (2.5-5%), but only four
studies reported data on this psychiatric disorder (18,19,21,24).
Prevalence of psychosis (ictal, interictal) was significantly
higher in patients with early-onset focal epilepsy and its presence
was corelated with longer disease duration and presence of TLE (sex
and age at examination were not contributory to psychosis).
Prevalence of personality disorders was assessed in
three studies (20,21,26).
Personality disorders, under these circumstances, appear to be a
characteristic of JME (but only one study assessed patients with
post-surgical MTLE/HS). When JME, MTLE/HS and control patients were
compared, no significant differences were found regarding normal
personality traits or supposed interictal personality
characteristics between groups.
Interictal personality (also known as
Gastaut-Geschwind Syndrome) (37),
another disorder described only by epileptologists, had a high
prevalence in pharmacoresistant TLE (37.9%), but was not confirmed
when DSM-IV criteria were used. Instead significant correlations
were found between presence of interictal personality and presence
of bilateral MTS, longer disease duration and presence of major
depressive disorder.
Another interesting correlation that was made in
epilepsy patients is the association between childhood maltreatment
experiences, age at epilepsy onset, epilepsy duration, seizure
types, seizure frequency and the presence of any current DSM Axis I
psychiatric disorder. Another study showed that the presence of DSM
Axis I psychiatric disorders, interictal dysphoric disorder and
interictal psychotic disorder in pharmaco-resistant epilepsy do not
depend on the presence vs. absence of complex partial seizures,
lateralization or localization of seizures.
The last study was the only study that assessed the
presence of psychiatric disorders diagnosed per DSM-IV in
pharmacoresistant epilepsies that did not undergo surgery at
baseline and at six months and found that there were no significant
diagnosis changes over a period of 6 months (19).
The prevalence of psychiatric disorders in our
analysis resemble to some extent the prevalence reported in a
non-systematic review of literature published in 2004(38), but direct comparison is not possible
because both epilepsy and psychiatric disorder classifications have
changed since its publication.
Our analysis is subject to many limitations. Some
important gaps are present in recent literature. We were not able
to find eligible studies on psychiatric disorders in patients with
single unprovoked seizures or in patients with a recent diagnosis
of epilepsy. Methodology used in the studies selected for this
analysis was highly heterogenous and this did not allow us to
perform a meta-analysis. Most studies included small samples of
epilepsy patients and were conducted in epilepsy units, thus
introducing biases such as exclusion of patients with severe
neurological pathologies, over-representation of TLE,
over-representation of pharmacoresistant epilepsy and exclusion of
patients with less severe epilepsy. Control groups were smaller
than patient samples in eight studies and six studies used control
groups with other pathologies. Formal psychiatric assessment was
not performed in controls in 7 studies. In almost 40% of the
studies, the epilepsy diagnosis was not formulated very clearly.
Epilepsy duration was not specified in three articles, seizure
frequency was not specified in three articles and antiepileptic
drug treatment was not specified in four articles. Even if most
studies included epileptic subtypes in their general sample, the
authors did not stratify the results by subtype. Only four studies
report that psychiatric assessment was performed by qualified
professionals. Three versions of the DSM and nine versions of
structured or semi-structured clinical interviews were used to
diagnose the psychiatric disorders. Finally, in eight studies we
are not sure if the psychiatric disorders reported are current or
lifetime disorders. Specific psychiatric disorder diagnoses are not
mentioned in five studies (only DSM broader category is provided).
As is the case for epilepsy subtypes, even when specific
psychiatric disorders are reported, the authors did not stratify
results by subtype in many cases.
5. Conclusions
The studies included in our analysis are
heterogenous. Objectives, methodology and result reporting were
found to be different in all studies. Psychiatric disorders are
present in a high proportion of epilepsy patients, at least at some
time point in the disease evolution.
Prevalence of any psychiatric disorder observed was
up to 51% in IGE, up to 43.1% in TLE, up to 43.3% in a general
population of patients with epilepsy. The most frequent psychiatric
comorbidities of epilepsy are mood/affective disorders (up to 40%
for lifetime occurrence and up to 23% for current occurrence),
anxiety disorders (up to 30.8% for lifetime occurrence and up to
15.6% for current occurrence), personality disorders (up to 11% in
JME) and psychotic disorders (up to 4% of patients with epilepsy).
Personality disorders and anxiety disorders are more frequently
described (and studied) in IGE patients, while depressive disorders
and psychotic disorders are more frequently described in focal
epilepsy (mainly TLE) and pharmacoresistant epilepsy. Evidence
regarding the presence and prevalence of interictal dysphoric
disorder and interictal personality is contradictory.
Depressive disorders might be associated with
specific brain imaging findings and with cognitive impairment in
focal epilepsy. Anxiety disorders are associated with higher
frequency of generalized tonico-clonic seizures and with worse
social functioning. Psychotic disorders are associated with longer
duration of epilepsy. Childhood maltreatment experiences are a
powerful predictor for the occurrence of psychiatric comorbidities
in epilepsy patients, while data regarding association of other
epilepsy characteristics (age at epilepsy onset, epilepsy duration,
seizure type, seizure localization and lateralization, seizure
frequency) with the presence of psychiatric disorders are
conflicting.
Future research in this area should assess the
presence of psychiatric disorders in newly diagnosed epilepsy/after
a single unprovoked seizure, should include a detailed
sociodemographic description for all patients/controls, should use
standardized assessment tools (including standardized epilepsy and
seizure classification, standardized reporting for seizure
frequency-as recommended by ILAE for clinical practice,
standardized structured clinical interview for diagnosis of
psychiatric disorders) and should stratify data according to the
specific epilepsy and psychiatric diagnosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All information provided in this review is
documented by relevant references.
Authors' contributions
RSG conceived the research protocol (including
search strategy and study inclusion/exclusion criteria),
cross-checked all full articles reviewed and selected by RID,
cross-checked data extracted from the selected studies, performed
the quality assessment of studies included, prepared the manuscript
and modified the manuscript as per the feedback received from AMC
and CAP. AMC reviewed the methodology and the manuscript, provided
feedback, submitted the manuscript and the cover letter. RID
searched the databases, screened title and abstracts, identified
and excluded duplicate titles, assessed the full text articles for
eligibility, excluded articles that did not meet inclusion criteria
or meet the exclusion criteria and extracted relevant data from
selected studies. CAP reviewed the methodology and the manuscript
and provided feedback. All authors read and approved the final
manuscript for publication.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
Adela Magdalena Ciobanu: ORCID: ID
0000-0003-2520-5486.
References
|
1
|
World Health Organization (WHO): The
ICD-10 classification of mental and behavioural disorders: Clinical
descriptions and diagnostic guidelines. World Health Organization,
1992.
|
|
2
|
Salpekar JA and Mula M: Common psychiatric
comorbidities in epilepsy: How big of a problem is it? Epilepsy
Behav. 98:293–297. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Michaelis R, Tang V, Goldstein LH, Reuber
M, LaFrance WC Jr, Lundgren T, Modi AC and Wagner JL: Psychological
treatments for adults and children with epilepsy: Evidence-based
recommendations by the international league against epilepsy
psychology task force. Epilepsia. 59:1282–1302. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Vogt VL, Äikiä M, Del Barrio A, Boon P,
Borbély C, Bran E, Braun K, Carette E, Clark M, Cross JH, et al:
Current standards of neuropsychological assessment in epilepsy
surgery centers across Europe. Epilepsia. 58:343–355.
2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wilson SJ, Baxendale S, Barr W, Hamed S,
Langfitt J, Samson S, Watanabe M, Baker GA, Helmstaedter C, Hermann
BP and Smith ML: Indications and expectations for
neuropsychological assessment in routine epilepsy care: Report of
the ILAE neuropsychology task force, diagnostic methods commission,
2013-2017. Epilepsia. 56:674–681. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Scheffer IE, Berkovic S, Capovilla G,
Connolly MB, French J, Guilhoto L, Hirsch E, Jain S, Mathern GW,
Moshé SL, et al: ILAE classification of the epilepsies: Position
paper of the ILAE commission for classification and terminology.
Epilepsia. 58:512–521. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fabiano F and Haslam N: Diagnostic
inflation in the DSM: A meta-analysis of changes in the stringency
of psychiatric diagnosis from DSM-III to DSM-5. Clin Psychol Rev.
80(101889)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lacey CJ, Salzberg MR and D'Souza WJ: Risk
factors for depression in community-treated epilepsy: Systematic
review. Epilepsy Behav. 43:1–7. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gandy M, Sharpe L and Perry KN:
Psychosocial predictors of depression and anxiety in patients with
epilepsy: A systematic review. J Affect Disord. 140:222–232.
2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mula M: Developments in depression in
epilepsy: Screening, diagnosis, and treatment. Expert Rev
Neurother. 19:269–276. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wang Z, Luo Z, Li S, Luo Z and Wang Z:
Anxiety screening tools in people with epilepsy: A systematic
review of validated tools. Epilepsy Behav.
99(106392)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. PLoS Med.
6(e1000097)2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sterne JAC, Savović J, Page MJ, Elbers RG,
Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge
SM, et al: RoB 2: A revised tool for assessing risk of bias in
randomised trials. BMJ. 366(l4898)2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wells GA, Shea B, O'Connell D, Peterson J,
Welch V, Losos M and Tugwell P: The Newcastle-Ottawa Scale (NOS)
for assessing the quality if nonrandomized studies in
meta-analyses. 2015. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Accessed March 14, 2021.
|
|
15
|
The Joanna briggs institute critical
appraisal tools for use in JBI systematic reviews: Checklist for
analytical cross-sectional studies. 2017. https://jbi.global/critical-appraisal-tools.
Accessed March 14, 2021.
|
|
16
|
Zheng Y, Ding X, Guo Y, Chen Q, Wang W,
Zheng Y, Wang S, Ding Y and Ding M: Multidisciplinary management
improves anxiety, depression, medication adherence, and quality of
life among patients with epilepsy in eastern China: A prospective
study. Epilepsy Behav. 100(106400)2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Baldin E, Hesdorffer DC, Caplan R and Berg
AT: Psychiatric disorders and suicidal behavior in neurotypical
young adults with childhood-onset epilepsy. Epilepsia.
56:1623–1628. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Konishi R and Kanemoto K: Psychosis rarely
occurs in patients with late-onset focal epilepsy. Epilepsy Behav.
111(107295)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ramos-Perdigués S, Baillés E, Mané A,
Carreño M, Donaire A, Rumia J, Bargalló N, Boget T, Setoain X,
Valdes M and Pintor L: A prospective study contrasting the
psychiatric outcome in drug-resistant epilepsy between patients who
underwent surgery and a control group. Epilepsia. 57:1680–1690.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Alonso NB, de Albuquerque M, Vidal-Dourado
M, Cavicchioli LH, Mazetto L, de Araújo Filho GM, de Figueiredo
Ferreira Guilhoto LM, Centeno RS and Yacubian EMT: Revisiting
personality in epilepsy: Differentiation of personality in two
epilepsies starting in adolescence. Epilepsy Behav. 97:75–82.
2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
de Araújo Filho GM, Tarifa B, Santos RE,
de Oliveira Dias AL, Ulliano JRL and Marques LHN: Clinical and
sociodemographic variables associated with interictal dysphoric
disorder and interictal personality in patients with drug-resistant
temporal lobe epilepsy: A controlled study. Epilepsy Behav.
69:100–103. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Galioto R, Tremont G, Blum AS, LaFrance WC
Jr, Crook CL and Davis JD: Depressive symptoms contribute to
executive deficits in temporal lobe epilepsy. J Neuropsychiatry
Clin Neurosci. 29:135–141. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kavanaugh B, Correia S, Jones J, Blum A,
LaFrance WC Jr and Davis JD: White matter integrity correlates with
depressive symptomatology in temporal lobe epilepsy. Epilepsy
Behav. 77:99–105. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Labudda K, Illies D, Bien CG and Neuner F:
Interictal dysphoric disorder: Further doubts about its
epilepsy-specificity and its independency from common psychiatric
disorders. Epilepsy Res. 141:13–18. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Labudda K, Illies D, Herzig C, Schröder K,
Bien CG and Neuner F: Current psychiatric disorders in patients
with epilepsy are predicted by maltreatment experiences during
childhood. Epilepsy Res. 135:43–49. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Paiva ML, Lima EM, Siqueira IB, Rzezak P,
Koike C, Moschetta SP, Vincentiis S, Alessi R, Khafif TC, Mendoza M
and Valente KD: Seizure control and anxiety: Which factor plays a
major role in social adjustment in patients with Juvenile myoclonic
epilepsy? Seizure. 80:234–239. 2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Rayner G, Jackson GD and Wilson SJ: Two
distinct symptom-based phenotypes of depression in epilepsy yield
specific clinical and etiological insights. Epilepsy Behav.
64:336–344. 2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Shen J, Li DL, Tan XX, Tao WW, Xie CJ, Shi
XG and Wang Y: A transcranial sonography study of brainstem and its
association with depression in idiopathic generalized epilepsy with
tonic-clonic seizures. Epilepsy Behav. 102(106589)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Micoulaud-Franchi JA, Lagarde S, Barkate
G, Dufournet B, Besancon C, Trébuchon-Da Fonseca A, Gavaret M,
Bartolomei F, Bonini F and McGonigal A: Rapid detection of
generalized anxiety disorder and major depression in epilepsy:
Validation of the GAD-7 as a complementary tool to the NDDI-E in a
French sample. Epilepsy Behav. 57:211–216. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lin CY and Pakpour AH: Using hospital
anxiety and depression scale (HADS) on patients with epilepsy:
Confirmatory factor analysis and rasch models. Seizure. 45:42–46.
2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gur-Ozmen S, Leibetseder A, Cock HR,
Agrawal N and von Oertzen TJ: Screening of anxiety and quality of
life in people with epilepsy. Seizure. 45:107–113. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Rampling J, Mitchell AJ, Von Oertzen T,
Docker J, Jackson J, Cock H and Agrawal N: Screening for depression
in epilepsy clinics. A comparison of conventional and visual-analog
methods. Epilepsia. 53:1713–1721. 2012.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ciobanu AM, Roşca T, Vlădescu CM, Tihoan
C, Popa C, Boer MC and Cergan R: Frontal epidural empyema (Pott's
puffy tumor) associated with Mycoplasma and depression. Rom J
Morphol Embryol. 55 (Suppl 3):S1203–S1207. 2014.PubMed/NCBI
|
|
34
|
Hesdorffer DC, Baldin E, Caplan R and Berg
AT: How do we measure psychiatric diagnoses? Implications of the
choice of instruments in epilepsy. Epilepsy Behav. 31:351–355.
2014.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Mula M, Kanner AM, Schmitz B and Schachter
S: Antiepileptic drugs and suicidality: An expert consensus
statement from the task force on therapeutic strategies of the ILAE
commission on neuropsychobiology. Epilepsia. 54:199–203.
2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Amiri M and Hansen CP: The interictal
dysphoric disorder in patients with epilepsy: A doubtful disorder
lacking diagnostic tools. Seizure. 24:70–76. 2015.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Trimble M and Freeman A: An investigation
of religiosity and the gastaut-geschwind syndrome in patients with
temporal lobe epilepsy. Epilepsy Behav. 9:407–414. 2006.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Gaitatzis A, Trimble MR and Sander JW: The
psychiatric comorbidity of epilepsy. Acta Neurol Scand.
110:207–220. 2004.PubMed/NCBI View Article : Google Scholar
|