Introduction
Periampullary diverticula (PAD) or peripapillary
diverticula are saccular structures of the duodenal outpouchings,
arising within a range of 2-3 cm around the ampulla of Vater
(1). Relevant studies have reported
that PAD are difficult to identify in patients aged <40 years
and the prevalence of PAD increases with advancing age (2-5).
Although the presence of PAD is usually asymptomatic, it may
increase the occurrence of diseases such as pancreatitis or
choledocholithiasis according to the specific anatomical structure
between PAD and the major duodenal papilla and pancreaticobiliary
ampulla (3,6). Age is considered to be a confounding
factor, since the prevalence of diverticula and bile duct stones
both increase along with age (7).
Previous studies have demonstrated the association between PAD and
the incidence of bile duct stones (8).
Endoscopic retrograde cholangiopancreatography
(ERCP) is one of the preferred methods for the diagnosis and
treatment of extrahepatic biliary and pancreatic diseases. With the
popularity and development of ERCP, the detection rate of PAD has
been markedly improved. The estimated occurrence of PAD in patients
undergoing ERCP is 10-20% (9), and
the prevalence and diameter of PAD increase with age (2-4).
However, the influence of PAD on ERCP for the treatment of biliary
and pancreatic diseases remains controversial. Certain studies have
indicated that the presence of PAD does not increase the risk of
failure of selective cannulation (2); however, other studies have
demonstrated that the presence of PAD increases the difficulty
associated with ERCP and the risk of complications (8,10).
Thus, further studies are required in order to fully determine the
influence of PAD on ERCP.
In the present retrospective study, clinical and
endoscopic data of patients with biliary and pancreatic diseases
treated with ERCP over the past 2 years were collected and
analyzed. The study was to evaluate the current situation of PAD
and to examine the influence of the presence of PAD in elderly
patients with bile duct stones who received ERCP treatment.
Materials and methods
Patients
The present single-center retrospective study was
performed at the First Affiliated Hospital of Bengbu Medical
College (Bengbu, China). The demographic data and details of the
ERCP procedure in patients with pancreaticobiliary disease who
underwent ERCP between January 2017 and December 2018 were obtained
from the electronic ERCP database. Patients undergoing ERCP for the
first time with complete information were included in the present
study.
Patients who met the following criteria were
excluded: i) History of choledochojejunostomy; ii) a fistula in the
major duodenal papilla; iii) incomplete records of clinical and/or
accessory examinations.
A total of 388 included cases were divided into the
PAD group (n=179) and the non-PAD (N-PAD) group (n=209). Subjects
aged ≥60 years were defined as elderly (11). All patients with complete
information from hospital records on general data, laboratory and
imaging examination were used to determine the initial diagnosis
and ERCP indications, and contraindications were excluded. This
study was approved by the Ethics Committee of the First Affiliated
Hospital of Bengbu Medical College (Bengbu, China; approval no.
2019KY030).
Collection of baseline
information
Baseline information, including sex, age and
diseases, was first retrieved for the patients of the present
study. Subsequently, the characteristics including age distribution
were analyzed in patients with cholangiolithiasis.
Procedures
All ERCP procedures were performed or supervised by
qualified physicians with >10 years of experience in ERCP. The
duodenoscope (Olympus JF-260/TJF-260), CleverCut sphincterotome
(Olympus Medical Systems Co. Ltd.), guidewire, dilation balloon,
extraction balloon, stone extractor, nasobiliary drainage, various
types of biliopancreatic stents and related instruments were
applied under X-ray fluoroscopy. The operators and patients
received standard radiation protection. Patients received oral
dimethicone 30 min prior to surgery and an intramuscular injection
of anisodamine, meperidine and/or diazepam (depending on the age
and general condition) 15 min prior to surgery for non-anesthetic
sedation and analgesia pretreatment.
The position of the papilla was determined after the
duodenoscope was moved to the descending part of the duodenum. The
shape, opening and the presence of PAD were observed. The type,
quantity and long diameter of PAD were recorded in patients with
PAD. Conventional selective cannulation was performed using a
cutting guide wire. Procedures including pancreatic guide
wire-assisted biliary cannulation, precut sphincterotomy,
needle-knife fistulosphincterotomy and clip-assisted cannulation
were performed when conventional intubation failed. After the guide
wire entered the biliary duct, the biliopancreatic duct lesion and
its position were confirmed according to the condition of contrast
agent under X-ray fluoroscopy. The methods of opening and lithotomy
included endoscopic sphincterotomy (EST), endoscopic papillary
balloon dilatation (EPBD) and EST+EPBD. One of the three options
was performed according to the number and the diameter of stones,
and the position and the side bulge length of the papilla. After
stone removal, the bile duct was examined by extraction balloon
cholangiography to confirm the absence of residual stones. After
the stone was removed, the operation of washing by noradrenaline in
iced saline solutions, balloon compression and hemostasis using a
metal clip was performed according to the papilla bleeding. The
biliary stent was simply placed when stones were not able to be
removed at one time. The types of PAD and the application of EPBD
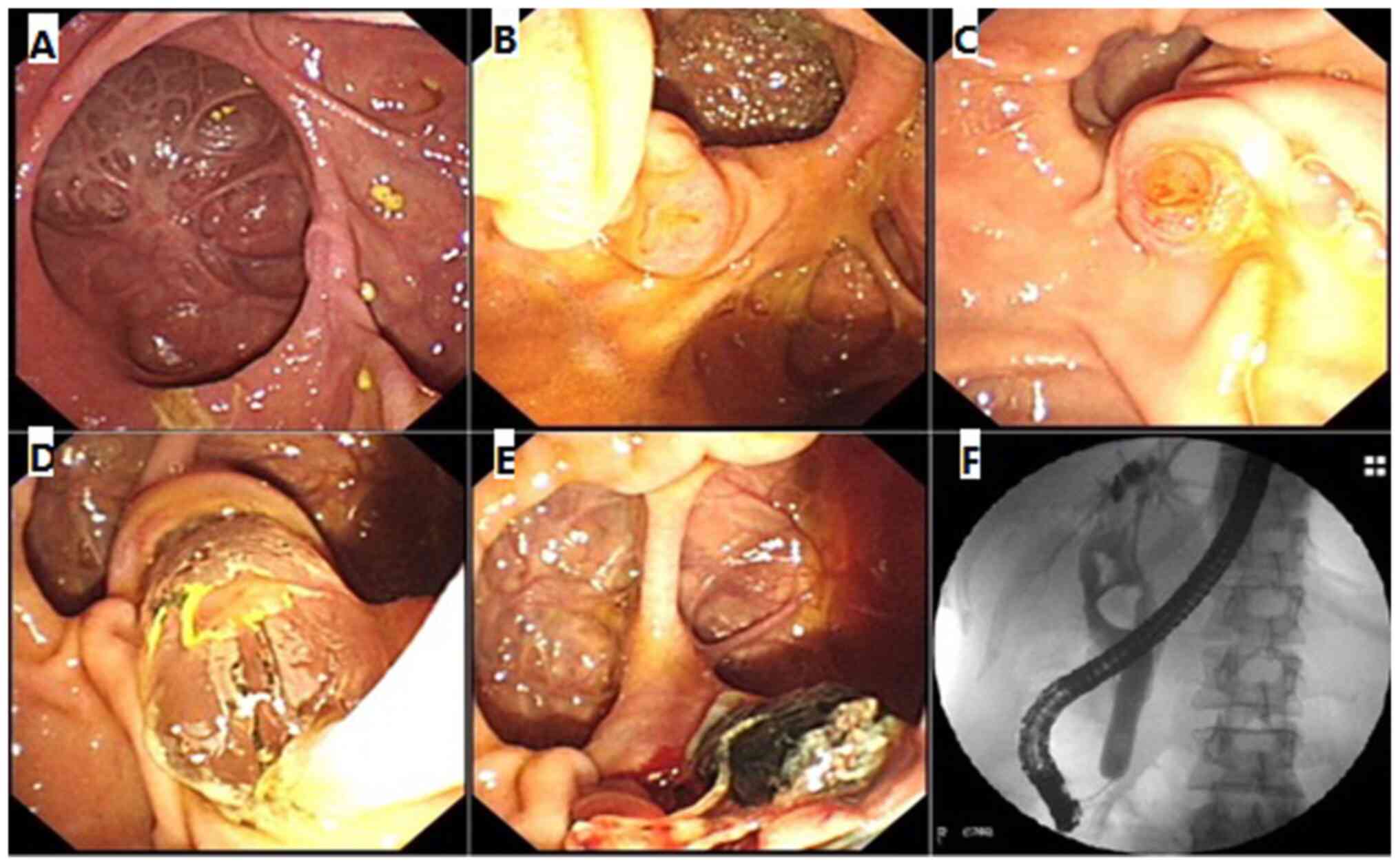
in PAD patients with bile duct stones are shown in Fig. 1. Of which, Fig. 1A is type I PAD (the duodenal papilla
is located inside the diverticulum); Fig. 1B is type II PAD (the duodenal
papilla lies at the margin of the diverticulum); Fig. 1C is type III PAD (the duodenal
papilla is located near the diverticulum); Fig. 1D shows dilated sphincter using EPBD
for type I PAD patients with bile duct stones; Fig. 1E shows the stone removal after EPBD
treatment; and Fig. 1F shows that
EPBD dilates the sphincter under the X-ray fluoroscopy.
Diagnostic criteria
The diameter of the depressed intestinal wall, which
was >5 mm within 2-3 cm of the main nipple on the descending
side of the duodenum, was defined as the PAD. The size and quantity
of the diverticula were confirmed in relation to the scale of
computed tomography and magnetic resonance cholangiopancreatography
(MRCP) examination images combined with direct view images acquired
with the endoscope with reference to the dilated balloon. A
diverticulum with a length ≥3 cm was defined as a giant
diverticulum, while a quantity ≥2 was defined as multiple
diverticula (12).
Difficult biliary cannulation refers to the failure
of conventional instruments and methods to enter the bile duct
(>5 contacts with the papilla whilst attempting to cannulate or
>5 min spent attempting to cannulate following visualization of
the papilla or >1 unintended pancreatic duct cannulation or
opacification) (13).
The criteria for sphincter of Oddi dysfunction (SOD)
were as follows (14): i) Typical,
episodic biliary or pancreatic pain; ii) >1.5- to 2.0-fold
elevation in liver-associated enzymes (aminotransferases or
alkaline phosphatase levels) or pancreatic enzymes (amylase or
lipase) on at least 2 occasions during episodes of pain; iii) MRCP
and ERCP revealed dilated common bile duct (bile duct diameter ≥10
mm) or main pancreatic ducts (pancreatic duct diameter ≥6 mm in the
head and ≥5 mm in the body), and excluded other biliary and
pancreatic diseases; iv) duodenal papillary sclerosis resulted in
difficult dilatation and required high-pressure balloon sphincter
stretching; v) following EST or sphincter stretching, the clinical
symptoms improved significantly.
The definition of large balloon dilation is that the
dilation of the columnar balloon in the papillary sphincter is ≥12
mm (15). ERCP-related adverse
reactions, including pancreatitis, cholangitis, hemorrhage and
perforation, were defined according to the American Society for
Gastrointestinal Endoscopy guidelines (16).
Statistical analysis
SAS 9.4 software (SAS Institute Inc.) was used for
statistical analysis. Count data are expressed as n(%) and the
chi-squared test was used to analyze these data. Data with a normal
distribution are expressed as the mean ± standard deviation and the
Student's t-test was adopted for the comparison of these data
between groups. Univariate and multivariate logistic regression
analyses were used to assess the influencing factors of PAD.
P<0.05 was considered to indicate a statistically significant
difference.
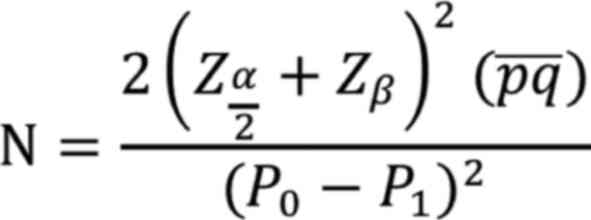
Sample size calculation was performed according to
the following formula:
where P0 is the incidence of bile duct
stones in the N-PAD group and P1 is the incidence of
bile duct stones in the PAD group. Q is the mean value of
(1-P0) and (1-P1). The sample proportion of
the two groups was 1:1 and the total sample size was n=2N. In a
previous study (17),
P1=0.47 and P0=0.16 had been calculated and
the required sample for each group was 70. The sample size in the
present study was in accordance with this.
Results
Patients
A total of 388 patients with complete information
who underwent ERCP for the first time were included, with a mean
age of 67.60±14.71 years (range, 36-93 years), and the male to
female ratio was 1.09. The mean age of the 179 patients in the PAD
group was 71.91±12.34 years and that of the 209 cases in the N-PAD
group was 63.91±15.58 years. There were statistical differences in
age and sex between the PAD and N-PAD groups (Table I).
 | Table IThe characteristics of cases who
received endoscopic retrograde cholangiopancreatography treatment
between the two groups. |
Table I
The characteristics of cases who
received endoscopic retrograde cholangiopancreatography treatment
between the two groups.
| Variables | Total | N-PAD | PAD | Statistics | P-value |
|---|
| Age, mean ± SD | 67.60±14.71 | 63.91±15.58 | 71.91±12.34 | t=-5.63 | <0.001 |
| Sex, n (%) | | | |
χ2=19.766 | <0.001 |
|
Male | 202 (52.06) | 87 (41.63) | 115 (64.25) | | |
|
Female | 186 (47.94) | 122 (58.37) | 64 (35.75) | | |
| Disease, n (%) | | | |
χ2=24.002 | 0.001 |
|
Pancreatic
diseases | 5 (1.29) | 5 (2.39) | 0 (0.00) | | |
|
SOD | 13 (3.35) | 8 (3.83) | 5 (2.79) | | |
|
Ampullary
and papillary tumors | 15 (3.87) | 14 (6.70) | 1 (0.56) | | |
|
Malignant
bile duct stricture | 85 (21.91) | 65 (31.10) | 20 (11.17) | | |
|
Bile duct
stones combined with cholecystolithiasis | 17 (4.38) | 7 (3.35) | 10 (5.59) | | |
|
Bile duct
stones combined with acute cholangitis | 26 (6.70) | 11 (5.26) | 15 (8.38) | | |
|
Benign bile
duct stricture | 11 (2.84) | 8 (3.83) | 3 (1.68) | | |
|
Bile duct
stones | 216 (55.67) | 91(43.54) | 125 (69.83) | | |
Prevalence of PAD in patients
In the present study, the prevalence of PAD was
56.93% (n=115) in males, 58.08% (n=150) in subjects with age ≥60
years and 57.87% (n=125) in cases with bile duct stones,
respectively.
Univariate regression analysis for
PAD
As shown in Table
II, the differences were discovered regarding male (OR=2.250,
95% CI: 1.670-3.801), age ≥60 years (OR=3.021, 95% CI:
1.855-4.902), ampullary and papillary tumors (OR=0.052, 95% CI:
0.007-0.403) between the PAD and N-PAD groups.
 | Table IIUnivariate and multivariate binary
logistic regression analysis for PAD. |
Table II
Univariate and multivariate binary
logistic regression analysis for PAD.
| Variables | OR (95% CI) | OR (95% CI) | P-value |
|---|
| Sex | | | |
|
Male | 2.250
(1.670-3.801) | 2.519
(1.586-3.999) | <0.001 |
|
Female | Reference | Reference | |
| Age, years | | | |
|
<60 | Reference | Reference | |
|
≥60 | 3.021
(1.855-4.902) | 3.066
(1.798-5.228) | <0.001 |
| Disease | | | |
|
Pancreatic
diseases | - | - | |
|
SOD | 0.455
(0.144-1.436) | 0.727
(0.217-2.433) | 0.605 |
|
Ampullary
and papillary tumors | 0.052
(0.007-0.403) | 0.054
(0.007-0.429) | 0.006 |
|
Malignant
bile duct stricture | 0.224
(0.127-0.396) | 0.181
(0.099-0.330) | <0.001 |
|
Bile duct
stones combined with cholecystolithiasis | 1.040
(0.381-2.835) | 0.841
(0.290-2.442) | 0.751 |
|
Bile duct
stones combined with acute cholangitis | 0.993
(0.436-2.262) | 1.176
(0.486-2.842) | 0.719 |
|
Benign bile
duct stricture | 0.273
(0.070-1.057) | 0.380
(0.091-1.591) | 0.006 |
|
Bile duct
stones | Reference | Reference | |
Multivariate binary logistic
regression analysis for PAD
The results of the multivariate binary logistic
regression indicated that the prevalence of PAD in males was
2.519-fold that in females (OR=2.519, 95% CI: 1.586-3.999). The
risk of PAD among the elderly was 3.066-fold that of younger
patients (OR=3.066, 95% CI: 1.798-5.228). The occurrence of PAD in
patients with malignant bile duct strictures was 0.181-fold that of
bile duct stones (OR=0.181, 95% CI: 0.099-0.330; Table II).
Risk factors of PAD in elderly
patients with bile duct stones
Among elderly patients, the constituent ratio of
males in the PAD group was significantly higher than that in the
N-PAD group (χ2=13.543, P<0.001) and the constituent
ratio of patients undergoing EST in the PAD group was lower than
that in the N-PAD group (χ2=10.800, P<0.001). No
statistically significant differences in papilla cannulation,
maximum diameter of stone, multiplicity/property of stones,
lithotomy status, mechanical lithotripsy, complications, common
bile duct diameter and repeated intervention were observed between
the two groups (P>0.05; Table
III).
 | Table IIIEffects of PAD in elderly patients
with bile duct stones who received ERCP. |
Table III
Effects of PAD in elderly patients
with bile duct stones who received ERCP.
| | Group, n (%) | |
|---|
| Variates | Total | PAD | N-PAD | χ2 | P-value |
|---|
| Sex | | | | 13.543 | <0.001 |
|
Male | 115 | 89 (68.99) | 26 (41.27) | | |
|
Female | 77 | 40 (31.01) | 37 (58.73) | | |
| Papilla
cannulation | | | | 2.694 | 0.101 |
|
Difficult
cannulation | 30 | 16 (12.90) | 14 (22.22) | | |
|
Routine
cannulation | 157 | 108 (87.10) | 49 (77.78) | | |
| Papilla
cutting | | | | 10.800 | 0.001 |
|
Simple
sphincter stretching | 49 | 42 (33.33) | 7 (11.11) | | |
|
EST | 140 | 84 (66.67) | 56 (88.89) | | |
| Maximum diameter of
stone, cm | | | | 4.240 | 0.120 |
|
1.0-1.9 | 112 | 79 (65.83) | 33 (60.00) | | |
|
<1.0 | 42 | 24 (20.00) | 18 (32.73) | | |
|
≥2 | 21 | 17 (14.17) | 4 (7.27) | | |
|
Multiplicity/property of stones | | | | 1.359 | 0.507 |
|
Single | 68 | 43 (34.13) | 25 (39.68) | | |
|
Multiple | 101 | 71 (56.35) | 30 (47.62) | | |
|
Mud-like and
not formed | 20 | 12 (9.52) | 8 (12.70) | | |
| Lithotomy
status | | | | - | 0.648 |
|
Partial
stone extraction + biliary stent | 10 | 8 (6.40) | 2 (3.17) | | |
|
Complete
stone extraction | 168 | 111 (88.80) | 57 (90.48) | | |
|
Biliary
stent inserted without stone extraction | 10 | 6 (4.80) | 4 (6.35) | | |
| Mechanical
lithotripsy | | | | 0.619 | 0.432 |
|
Unsuccessful | 166 | 109 (86.51) | 57 (90.48) | | |
|
Successful | 23 | 17 (13.49) | 6 (9.52) | | |
| Complications | | | | - | 0.162 |
|
Hemorrhage | 1 | 0 (0.00) | 1 (1.59) | | |
|
Cholangitis | 153 | 106 (82.81) | 47 (74.60) | | |
|
Pancreatitis | 37 | 22 (17.19) | 15 (23.81) | | |
| Common bile duct
diameter, cm | | | | 0.653 | 0.419 |
|
<1.50 | 63 | 40 (31.75) | 23 (37.70) | | |
|
≥1.5 | 124 | 86 (68.25) | 38 (62.30) | | |
| Repeated
intervention | | | | - | 0.150 |
|
No | 177 | 116 (89.92) | 61 (96.83) | | |
|
Yes | 15 | 13 (10.08) | 2 (3.17) | | |
Discussion
PAD have gradually received increasing attention due
to their specific location. With the in-depth development of ERCP,
the detection rate of PAD has been greatly increased (9). The present study was performed to
explore the current situation of PAD and to analyze the influence
of the presence of PAD on the implementation of ERCP. The results
confirmed that the prevalence of PAD in elderly patients (age, ≥60
years) was higher, indicating that the presence of PAD is
significantly associated with age. The age-prone prevalence of PAD
may be related to the deterioration of the muscular wall and the
intestinal wall, the weakening of intestinal tone contraction, the
slowing of peristalsis and the abnormal retention of intestinal
contents in the elderly (5). To
date, PAD has been insufficiently studied in elderly populations
treated with ERCP. Regarding PAD in elderly patients with bile duct
stones, univariate analysis and multifactorial analysis were
performed in the present study in order to further clarify the
prevalence of PAD and the impact of PAD on ERCP.
The present study also indicated an association
between the occurrence of PAD and sex, as the prevalence of PAD in
males was higher than that in females, irrespective of the age of
the patients. To the best of our knowledge, the present study was
the first to determine that female sex may be a protective factor
against PAD. Compared with that in patients with bile duct stones,
the occurrence of PAD in patients with ampullary and papillary
tumors and malignant bile duct stricture was lower. The prevalence
of PAD in patients with bile duct stones was 57.92% and higher than
in those without stone. The present results suggested that PAD are
closely associated with the occurrence of bile duct stones and Sun
et al (18) and Hall et
al (19) also confirmed the
relationship between PAD and bile duct stones. In the current
study, analysis of patients with or without bile duct stones
indicated that the difference in age between the PAD and the N-PAD
group was mainly reflected in the population of bile duct stones
and patients with bile duct stones exhibited a higher occurrence of
PAD than other pancreatic biliary diseases.
The high prevalence of bile duct stones in patients
with PAD may be due to the following: PAD causes SOD, resulting in
inadequate drainage or regurgitation of bile and pancreatic juice;
food deposition in the diverticulum easily occurs secondary to
diverticulitis, causing constrictive papillitis, affecting the
discharge of biliary sludge and increasing the incidence of
retrograde biliary infection; exogenous glucuronidase increases the
formation of free bilirubin, which combines with calcium salts to
form the core of the stone and the pH value of the bile duct
decreases when the bile duct is infected, which may promote the
formation of pigment gallstones (20). Therefore, patients with bile duct
stones aged ≥60 years were selected as the key research subjects in
the present study in order to explore the effects of the presence
of PAD on ERCP.
Selective cannulation of the bile duct through the
main papilla is the primary method for ERCP lithotomy and the time
and the route of cannulation influence the risk of post-ERCP
pancreatitis (21). PAD has been
reported to increase the difficulty and operating time of deep
cannulation (19). However, the
presence of PAD has also been determined to improve the success
rate of intubation and to be an independent factor for easier
cannulation (22). There was no
significant effect on selective bile duct cannulation, even with
stricter requirements and time limits for ERCP in elderly patients,
and these results are supported by previous studies (22,23).
In the present study, multivariate binary logistic regression
analysis revealed that the risk of PAD in males was 2.519 times
that of females among the elderly. The means of papilla cutting
were different in elderly patients with bile duct stones. The
prevalence of elderly patients aged ≥60 years who were subjected to
simple sphincter stretching was 4.593 times that of those who
underwent EST. This result suggested that the presence of PAD may
be associated with a decreased usage rate of EST.
Considering the difficulty associated with ERCP, the
present study provided suggestions which may be used to circumvent
the difficulties associated with ERCP and the following steps may
be suggested: i) Careful and complete examination prior to ERCP;
ii) risk assessment and implementation of preventive measures for
complications prior to ERCP; iii) comprehensive evaluation of
indications for ERCP with a strict control of indications; iv)
standardization of ERCP surgery; v) adequate preparation of ERCP
operating consumables and instruments.
There are certain limitations to the present study
that require to be mentioned: i) this was a retrospective single
center study; ii) the conservative attitude of the physicians
regarding subjective sphincter incision in patients with PAD. A
larger sample size and a well-designed prospective randomized
controlled trial are required to further confirm the results of the
present study.
In conclusion, the present study indicated that the
prevalence of patients with PAD was high among the elderly who
received ERCP treatment, males exhibited a higher prevalence of PAD
than females.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the Key Research Project of
Anhui Provincial University Natural Science Fund (grant no.
KJ2019A0336) and the Anhui Provincial University Natural Science
Fund Project (grant no. 1808085MH240).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HZ and XD designed the study. HZ wrote the
manuscript. SY and YX contributed to data collection. HZ and DL
analyzed and interpreted the data. YX contributed to the literature
search. XD critically reviewed the manuscript for important
intellectual content. HZ, SY, YX and DL confirmed the authenticity
of all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The research protocol was examined and approved by
the Ethics Committee of the First Affiliated Hospital of Bengbu
Medical College (approval no. 2019KY030).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lobo DN, Balfour TW, Iftikhar SY and
Rowlands BJ: Periampullary diverticula and pancreaticobiliary
disease. Br J Surg. 86:588–597. 1999.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zippi M, Traversa G, Pica R, De Felici I,
Cassieri C, Marzano C, Occhigrossi G and Paoluzi P: Efficacy and
safety of endoscopic retrograde cholangiopancreatography (ERCP)
performed in patients with Periampullary duodenal diverticula
(PAD). Clin Ter. 165:e291–e294. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chen L, Xia L, Lu Y, Bie L and Gong B:
Influence of periampullary diverticulum on the occurrence of
pancreaticobiliary diseases and outcomes of endoscopic retrograde
cholangiopancreatography. Eur J Gastroenterol Hepatol. 29:105–111.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Örmeci N, Deda X, Kalkan Ç, Tüzün AE,
Karakaya F, Dökmeci A, Bahar DK, Özkan H, İdilman R and Çınar K:
Impact of periampullary diverticula on bile duct stones and
ampullary carcinoma. Euroasian J Hepatogastroenterol. 6:31–34.
2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tyagi P, Sharma P, Sharma BC and Puri AS:
Periampullary diverticula and technical success of endoscopic
retrograde cholangiopancreatography. Surg Endosc. 23:1342–1345.
2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Li X, Zhu K, Zhang L, Meng W, Zhou W, Zhu
X and Li B: Periampullary diverticulum may be an important factor
for the occurrence and recurrence of bile duct stones. World J
Surg. 36:2666–2669. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Neoptolemos JP: Endoscopic sphincterotomy
in acute gallstone pancreatitis. Br J Surg. 80:547–549.
1993.PubMed/NCBI
|
|
8
|
Kim KH and Kim TN: Endoscopic papillary
large balloon dilation in patients with periampullary diverticula.
World J Gastroenterol. 19:7168–7176. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Egawa N, Anjiki H, Takuma K and Kamisawa
T: Juxtapapillary duodenal diverticula and pancreatobiliary
disease. Dig Surg. 27:105–109. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Karaahmet F and Kekilli M: The presence of
periampullary diverticulum increased the complications of
endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol
Hepatol. 30:1009–1012. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liang K: Differential associations between
subjective age and depressive symptoms among urban and rural
Chinese older adults. Aging Ment Health. 24:1271–1277.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kim CW, Chang JH, Kim JH, Kim TH, Lee IS
and Han SW: Size and type of periampullary duodenal diverticula are
associated with bile duct diameter and recurrence of bile duct
stones. J Gastroenterol Hepatol. 28:893–898. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Testoni PA, Mariani A, Aabakken L,
Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M,
Dumonceau JM, Giovannini M, et al: Papillary cannulation and
sphincterotomy techniques at ERCP: European Society of
Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy.
48:657–683. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Nakeeb A: Sphincter of Oddi dysfunction:
How is it diagnosed? How is it classified? How do we treat it
medically, endoscopically, and surgically? J Gastrointest Surg.
17:1557–1558. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zulli C, Grande G, Tontini GE, Labianca O,
Geraci G, Sciumè C, Antypas P, Fiocca F, Manes G, Devani M, et al:
Endoscopic papillary large balloon dilation in patients with large
biliary stones and periampullary diverticula: Results of a
multicentric series. Dig Liver Dis. 50:828–832. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chandrasekhara V, Khashab MA, Muthusamy
VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD,
Faulx AL, Gurudu SR, et al: ASGE Standards of Practice Committee:
Adverse events associated with ERCP. Gastrointest Endosc. 85:32–47.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tazuma S, Unno M, Igarashi Y, Inui K,
Uchiyama K, Kai M, Tsuyuguchi T, Maguchi H, Mori T, Yamaguchi K, et
al: Evidence-based clinical practice guidelines for cholelithiasis
2016. J Gastroenterol. 52:276–300. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sun Z, Bo W, Jiang P and Sun Q: Different
types of periampullary duodenal diverticula are associated with
occurrence and recurrence of bile duct stones: A case-control study
from a Chinese center. Gastroenterol Res Pract.
2016(9381759)2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hall RI, Ingoldby CJ and Denyer ME:
Periampullary diverticula predispose to primary rather than
secondary stones in the common bile duct. Endoscopy. 22:127–128.
1990.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Miyazaki S, Sakamoto T, Miyata M, Yamasaki
Y, Yamasaki H and Kuwata K: Function of the sphincter of Oddi in
patients with juxtapapillary duodenal diverticula: Evaluation by
intraoperative biliary manometry under a duodenal pressure load.
World J Surg. 19:307–312. 1995.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lawrence C, Romagnuolo J, Cotton PB, Payne
KM and Hawes RH: Post-ERCP pancreatitis rates do not differ between
needle-knife and pull-type pancreatic sphincterotomy techniques: A
multiendoscopist 13-year experience. Gastrointest Endosc.
69:1271–1275. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Panteris V, Vezakis A, Filippou G,
Filippou D, Karamanolis D and Rizos S: Influence of juxtapapillary
diverticula on the success or difficulty of cannulation and
complication rate. Gastrointest Endosc. 68:903–910. 2008.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Tham TC and Kelly M: Association of
periampullary duodenal diverticula with bile duct stones and with
technical success of endoscopic retrograde
cholangiopancreatography. Endoscopy. 36:1050–1053. 2004.PubMed/NCBI View Article : Google Scholar
|