Introduction
Although the prognosis of patients with heart
failure (HF) has improved considerably with the development of new
strategies, including medical therapies and advances to the
instrument used, it remains extremely poor (1,2); the
1 and 5-year mortality rates after diagnosis, have been reported to
be 20 and 53%, respectively in the Olmsted County cohort study
(3). Therefore, the prevention of
HF is of utmost importance. European Society Guidelines recommended
a healthy diet, avoiding excessive salt intake (>5 g/day, i.e.,
2 g/day sodium); however, the optimal level of sodium intake
remains unclear.
The ESPRIT study (4) (Evaluation of sodium Intake for the
prediction of cardiovascular events in Japanese high-risk patients)
revealed that a high sodium excretion ≥4.0 g/day, assessed by
repeated measurements of spot urine, was associated with composite
cardiovascular events in Japanese high-risk patients. During the
median follow-up period of 5.2 years in 520 enrolled patients, 105
(20%) experienced composite cardiovascular events, which were
predominantly driven by 60 (12%) hospitalizations due to HF.
However, the method for estimating sodium excretion
using spot urine is complex requiring age, body weight, height, and
multiplier factors for calculation (5).
There are certain reports comparing the
sodium/creatinine (Na/Cr) ratio and 24-hr sodium excretion. Mann
and Gerber (6) reported that the
Na/Cr ratio of a late afternoon/early evening urine sample highly
correlated with the actual 24-h sodium excretion (r=0.86,
P<0.001), although the correlation was weak when using AM
samples (r=0.31, P=0.06). Wan et al (7) reported that the Na/Cr ratio in spot
urine and 24-h sodium excretion weakly correlated (r=0.26,
P=0.019). A higher correlation of the Na/Cr ratio in spot urine and
24-h sodium excretion was observed (r=0.392, P<0.01) in a Korean
study using a small number of 15 subjects (8). Furthermore, blood pressure and
hypertension have been found to be associated with the Na/Cr ratio
using a large population (n=9,674) in Korea (9). However, to the best of our knowledge,
there are no reports available to date assessing the association
between the Na/Cr ratio in spot urine and hospitalizations due to
HF.
The aim of the present study was to elucidate
whether the Na/Cr ratio in spot urine, a key component in
estimating daily sodium excretion, is associated with
hospitalizations due to HF.
Patients and methods
Patient cohort
In the present study, a post hoc analysis of the
previously published ESPRIT study (4) was performed. The study protocol
conformed to the ethical guidelines of the 1975 Declaration of
Helsinki and was approved by the Institutional Ethics Committee of
Ueki Hospital, and informed written consent was obtained from all
the patients. Briefly, the ESPRIT study was a single-center,
prospective, observational study that included 520 patients who
visited the cardiology clinic with at least one of the following
cardiovascular conditions: i) Stable and compensated HF [having New
York Heart Association (NYHA) ≥2 symptoms and/or congestive sign
requiring loop diuretics, or a history of congestive heart failure
that required continued medical treatment]; ii) reduced left
ventricular ejection fraction (LVEF <50%); iii) brain
natriuretic peptide (BNP) levels ≥100 pg/ml for any reason; iv)
documented coronary artery disease; v) cerebrovascular disease; vi)
chronic kidney disease (CKD), estimated glomerular filtration rate
(eGFR) <60 ml/min/1.73 m2; and vii) atrial
fibrillation. Follow-up was commenced at the time of entry. During
the median follow-up period of 5.2 years, 105 (20%) patients
experienced composite cardiovascular events (hospitalization due to
HF, acute coronary syndrome, cerebrovascular events and
cardiovascular-related mortality), which were predominantly driven
by 60 (12%) hospitalizations due to HF.
The sodium (mEq/l) and creatinine (mmol/l)
concentrations were measured using spot urine and the Na/Cr ratio
was calculated. Sodium intake was estimated using the Tanaka method
(5). The measurements were
conducted at the time of entry and repeated at least every 6
months. An average of all data from each patient was used for the
analysis (median 14 measurements).
Statistical analysis
Data are presented as the mean ± standard deviation,
median (interquartile range), or percentages, as appropriate. Event
frequencies were compared using a χ2 test. Other
comparisons between two groups of data were performed using an
unpaired Student's t-test or the Mann-Whitney U test, as
appropriate. The optimal Na/Cr ratio cut-off point was determined
using receiver operating characteristic (ROC) curve analysis. The
outcomes were displayed with Kaplan-Meier event-free curves and
compared with the use of log-rank tests. The prognostic values of
Na/Cr ratio, sodium excretion ≥4.0 g/day and clinical variables
were analyzed using Cox-proportional hazard models and hazard
ratios (HRs) were described with a 95% confidence interval (CI).
For multivariate analyses, age, sex, body weight, BNP, eGFR,
diabetes mellitus, and the use of diuretics were used for
adjustments. P<0.05 was considered to indicate a statistically
significant difference. The statistical software package JMP
(version 11; SAS Institute, Inc.) was used for the analyses.
Results
Cut-off values
With ROC analysis, the optimum cut-off point for
Na/Cr ratio in spot urine using a median of 14 (interquartile
range, 10-21) measurements, yielded 24.8 to detect hospitalization
due to HF [area under the curve (AUC), 0.58, P=0.015; sensitivity,
40%, specificity, 81%]. This association was not observed when
using only a Na/Cr ratio at the time of entry alone (AUC 0.52,
P=0.81). Similarly, this association was not observed when using
the average values of first three (n=511; AUC, 0.52; P=0.22) or
first five (n=495; AUC, 0.54; P=0.10) Na/Cr ratios. However, there
were trends towards an association when using the average values of
last five Na/Cr ratios (n=495; AUC, 0.58; P=0.070).
Baseline characteristics
The Baseline characteristics of the patients, below
and above the cut-off point, are presented in Table I. In patients with a Na/Cr ratio
≥24.8, an older age, female sex, a smaller body weight and diabetes
mellitus were more prevalent, and BNP levels were higher.
Additionally, diuretics were more commonly used in patients with a
high Na/Cr ratio.
 | Table ICharacteristics of the study patients
according to the Na/Cr ratio in spot urine. |
Table I
Characteristics of the study patients
according to the Na/Cr ratio in spot urine.
| Variable | All patients | Na/Cr <24.8 | Na/Cr ≥24.8 | P-value |
|---|
| No. | 520 | 408 | 112 | |
| Event: HF
hospitalization, n (%) | 60 | 36 (8.8) | 24(22) | <0.001 |
| Sodium excretion at
entry, g/day | 3.52±0.93 | 3.36±0.84 | 4.07±1.03 | <0.001 |
| Average sodium
excretion, g/day | 3.52±0.67 | 3.35±0.57 | 4.13±0.67 | <0.001 |
| Na/Cr ratio at
entry | 18.9±13.0 | 15.5±9.5 | 31.2±16.3 | <0.001 |
| Average Na/Cr
ratio | 19.5±10.2 | 15.4±4.8 | 34.5±10.6 | <0.001 |
| Serum sodium,
mEq/liter | 141±2.5 | 141±2.4 | 141±3.1 | 0.35 |
| Follow-up duration,
years | 5.2 (3.2-5.7) | 5.3 (3.2-5.7) | 4.8 (2.7-5.7) | 0.65 |
| Measurement,
times | 14 (10-21) | 14 (10-20) | 15 (10-22) | 0.74 |
| Age, years | 73±10 | 73±10 | 75±9 | 0.016 |
| Age >75 years, n
(%) | 254(49) | 193(47) | 61(54) | 0.18 |
| Female, n (%) | 199(38) | 126(31) | 73(65) | <0.001 |
| Body weight, kg | 60±13 | 62±13 | 55±10 | <0.001 |
| Body weight <60
kg, n (%) | 260 (50%) | 182 (45%) | 78 (70%) | <0.001 |
| Body mass index,
kg/m2 | 24±3.5 | 24±3.5 | 23±3.3 | 0.013 |
| Systolic blood
pressure, mmHg | 123±15 | 124±16 | 121±15 | 0.094 |
| Diastolic blood
pressure, mmHg | 70±11 | 70±11 | 68±12 | 0.15 |
| Hypertension, n
(%) | 384(74) | 302(74) | 82(74) | 0.86 |
| eGFR, ml/min/1.73
m2 | 64±18 | 63±18 | 65±20 | 0.23 |
| eGFR <60
ml/min/1.73 m2, n (%) | 219(42) | 174(43) | 45(40) | 0.63 |
| Cr, mg/dl | 0.87±0.28 | 0.89±0.28 | 0.79±0.24 | <0.001 |
| BNP, pg/ml | 53 (24-115) | 50 (22-105) | 67 (29-148) | 0.011 |
| BNP >100 pg/ml, n
(%) | 147(28) | 107(26) | 40(36) | 0.048 |
| Chronic HF, n
(%) | 114(22) | 70(17) | 44(39) | <0.001 |
| Permanent AF, n
(%) | 97(19) | 77(19) | 20(18) | 0.80 |
| HbA1c, % | 6.1±0.64 | 6.1±0.64 | 6.0±0.65 | 0.066 |
| Diabetes mellitus, n
(%) | 129(25) | 112(27) | 17(15) | <0.01 |
| Medications, n
(%) | | | | |
| ACEI/ARBs | 330(64) | 254(62) | 76(68) | 0.28 |
| β-blockers | 194(37) | 154(38) | 40(36) | 0.69 |
| Calcium channel
blockers | 264(51) | 205(50) | 59(53) | 0.65 |
| Diuretics | 125(24) | 76(19) | 49(44) | <0.001 |
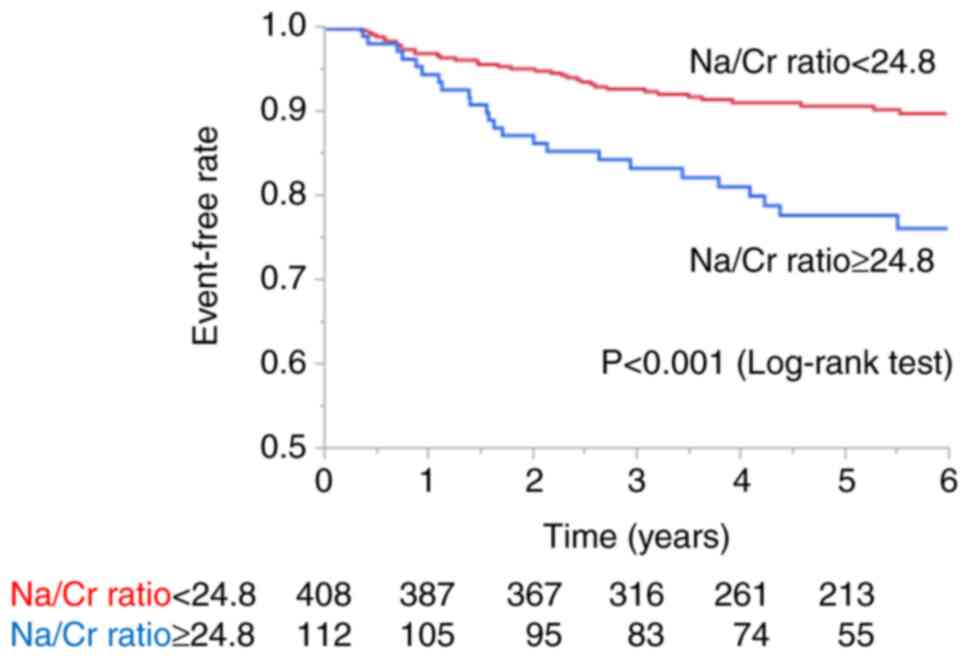
Hospitalization due to HF
The Na/Cr ratio was significantly higher in patients
who were hospitalized due to HF than that in patients without
hospitalization for HF (22.7±13.0 vs. 19.1±9.7, P<0.01). There
were 24 (22%) hospitalizations for HF observed in patients with an
average Na/Cr ratio ≥24.8 as compared with 36 (8.8%) such events in
those with an average Na/Cr ratio <24.8. Kaplan-Meier free
curves for hospitalization due to HF for the Na/Cr ratio revealed
that an elevated Na/Cr ratio was significantly associated with
hospitalization for HF (P<0.001, Fig. 1). The HRs of the Na/Cr ratio ≥24.8
for hospitalization due to HR are presented in Table II. In the univariate analysis, a
Na/Cr ratio ≥24.8 was associated with hospitalization for HF (HR,
2.49; CI, 1.47-4.16). Following adjustment for age, sex and body
weight, a Na/Cr ratio ≥24.8 was also associated with
hospitalization for HF (HR, 2.74; CI, 1.47-4.16). The association
between high Na/Cr ratio and hospitalization for HF remained
following further additional adjustments for either BNP, eGFR,
diabetes mellitus, or the use of diuretics (Table II).
 | Table IIHazard ratios of the urinary Na/Cr
ratio ≥24.8 for hospitalization due to heart failure. |
Table II
Hazard ratios of the urinary Na/Cr
ratio ≥24.8 for hospitalization due to heart failure.
| Analysis | Hazard ratio (95%
confidence interval) | P-value |
|---|
| Unadjusted
(univariate analysis) | 2.49 (1.47-4.16) | <0.001 |
| Adjusted for | | |
|
Age, sex and
body weight (1) | 2.74 (1.51-4.71) | <0.001 |
|
(1) + BNP
>100 pg/ml | 2.36 (1.37-4.01) | <0.01 |
|
(1) + eGFR
<60 ml/min/1.73 m2 | 2.81
(1.61-4.81) | <0.001 |
|
(1) +
Diabetes mellitus | 2.80
(1.61-4.78) | <0.001 |
|
(1) + Use of
diuretics | 1.85
(1.03-3.26) | 0.037 |
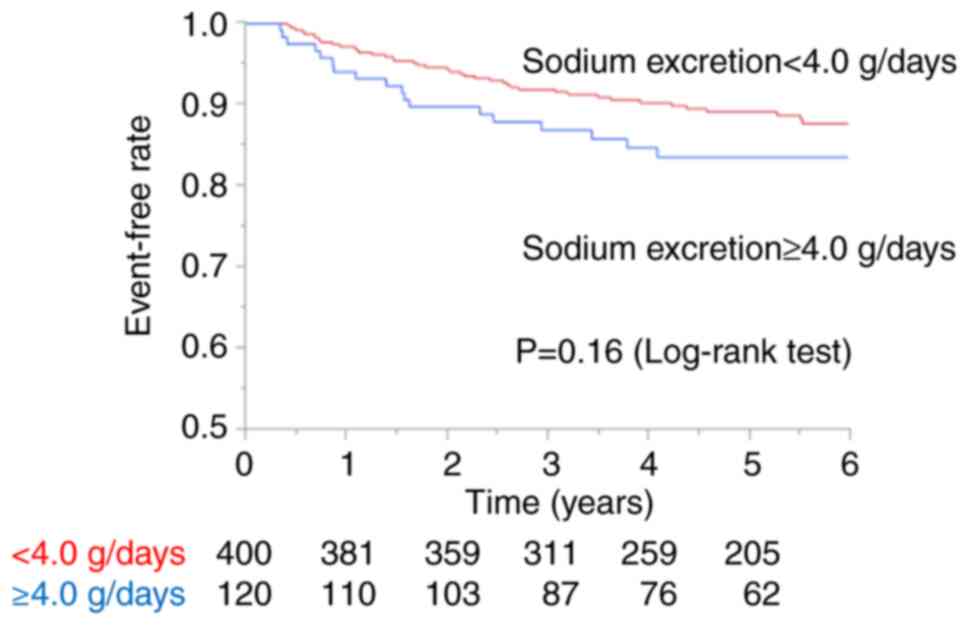
On the other hand, there were 18 (15%)
hospitalizations for HF observed in patients with a sodium
excretion ≥4.0 g/day as compared with 42 (10.5%) such events in
those with an average sodium excretion <4.0 g/day. Kaplan-Meier
free curves for hospitalization for HF for a sodium excretion ≥4.0
g/day did not reveal a significant difference (P=0.16, Fig. 2). However, Cox proportional hazard
model analysis revealed that a sodium excretion ≥4.0 g/day was
associated with hospitalization for HF following adjustment for
age, sex and body weight (HR, 2.48; CI, 1.35-4.14).
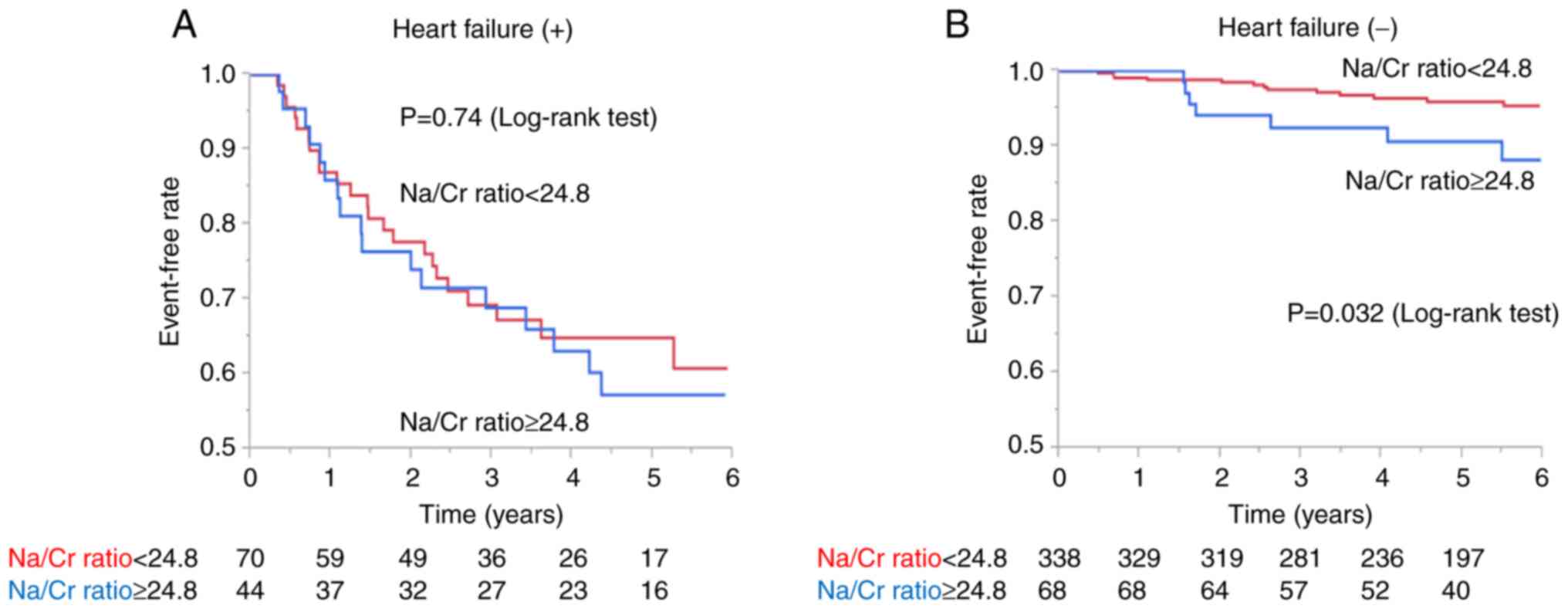
Hospitalization for HF with and
without stable HF
Stable 114 HF patients, defined as having NYHA ≥2
symptoms and/or congestive sign requiring loop diuretics, or a
history of congestive HF that required continued medical treatment
were enrolled in the present study. LVEF was preserved (≥50%) in 82
(72%) patients. There were 17 (39%) hospitalizations for HF
observed in patients with an average Na/Cr ratio ≥24.8 as compared
with 23 (33%) such events in those with an average Na/Cr ratio
<24.8. Kaplan-Meier free curves for hospitalization due to HF
for the Na/Cr ratio did not reveal any differences between the
groups (P=0.74, Fig. 3A). However,
in patients without HF (n=406), there were 7 (10%) hospitalizations
for HF observed in patients with an average Na/Cr ratio ≥24.8 as
compared with 13 (3.8%) such events in those with an average Na/Cr
ratio <24.8. Kaplan-Meier free curves for hospitalization due to
HF for Na/Cr ratio revealed that an elevated Na/Cr ratio was
significantly associated with hospitalization for HF (P=0.032,
Fig. 3B).
Discussion
In the present study, a post hoc analysis of the
ESPRIT study (4) was performed and
it was found that a high Na/Cr ratio in spot urine was associated
with hospitalization for HF in high-risk Japanese patients. The
strength of this sub-analysis is that a simple marker of the Na/Cr
ratio in spot urine, when measured repeatedly, was associated with
hospitalizations for HF either in univariate analysis or following
adjustment for several factors, such as age, sex, body weight, BNP,
eGFR, diabetes mellitus, or the use of diuretics. On the other
hand, a sodium excretion ≥4.0 g/day assessed using the method of
Tanaka et al (5) was
associated with hospitalization for HF only following adjustment
for age, sex and body weight. This may be due to the fact that high
sodium excretion is associated with hospitalization for HF in
patients of an older age, of the female sex and a low body weight,
as previously reported (10). Of
note, appropriate sodium intake in these populations is not yet
well understood. Thus, it is considered that the Na/Cr ratio may be
a simple and promising marker without the need for these
adjustments.
Sodium excretion varies considerably from day to day
and hour to hour, and, therefore, spot urine results can differ
substantially from the results of 24-h collections (11-14).
It is evident that the salt intake estimation from the data of spot
urine may be too variable to examine an individual's absolute salt
intake using only a single measurement (13,14),
as may be applied to the Na/Cr ratio in spot urine. In fact, the
Na/Cr ratios at the time of entry alone, the averages of the first
three, and first five times were not associated with
hospitalization for HF in the present study. Repeated measurements
may thus be necessary. We believe this method can aid in predicting
HF hospitalization along with known clinical factors, such as an
increase in body weight, peripheral edema and HF symptoms in the
real- world practice.
With regard to hospitalization for HF in patients
with stable HF, Martens et al (15) reported that the urinary sodium
excretion remained relatively stable over time in patients with
stable and chronic HF patients, and patients who developed acute
decompensated HF exhibited a chronically lower, as opposed to a
higher urinary sodium concentration. They also demonstrated a
further decrease in the urinary sodium concentration during the
week preceding hospitalization. It was concluded that the inability
to efficiently excrete sodium, which may be due to the sustained
activation of the renin-angiotensin-aldosterone system and
sympathetic nervous system, may be a sign of worsening HF. However,
the urinary sodium excretion is also dependent on dietary sodium
intake and this hypothesis may not be validated without the
information of dietary sodium intake. Therefore, the efficacy of
urinary sodium as a biomarker of HF is more complicated than it
initially appears (16). In the
present and previous study (10),
the Na/Cr ratio and sodium excretion ≥4.0 g/day were not associated
with HF hospitalization in patients with stable HF patients
(Fig. 3A, and ref 10). The LVEF was reduced in the
majority (86%) of the patients in the study by Martens et al
(15), whereas, the LVEF was
preserved in the majority (72%) of the patients in the present
study; this may have contributed to the difference in the results.
However, these results were at least consistent at the point that a
higher urinary sodium concentration was not observed at the time of
hospitalization for HF in patients with stable HF.
The present study has several limitations. A post
hoc analysis of a single-center study was performed, and thus may
have introduced selection bias. Second, the number of included
patients and hospitalization for HF were minimal. Thus, certain
crucial factors could not be fully adjusted. Third, the AUC in ROC
analysis was relatively low (0.58); the ability of the Na/Cr to
discriminate hospitalization for HF may not be as high. However,
the results (Fig. 1) revealed
clear discriminatory ability and thus this method may be feasible.
Fourth, this method may not be used in patients with stable HF, as
aforementioned. Fifth, the original ESPRIT study was conducted
between 2011 and 2015. Thus, sacubitril/valsaltan and SGLT2
inhibitors, which were widely used in patients with HF, were not
available. Other limitations for the original ESPRIT study were
described previously (4), in
particular, the marked heterogeneity of the included patients was a
major concern.
In conclusion, the present study demonstrates that
Na/Cr ratio in spot urine is associated with hospitalization for HF
in high-risk Japanese patients. However, these findings require
further validation in the future prospective studies.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TS and SH designed the study, analyzed the data and
wrote the manuscript. TS and SH confirm the authenticity of all the
raw data. Both authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The study protocol of the Evaluation of sodium
intake for the prediction of cardiovascular events in Japanese
high-risk patients (ESPRIT) study conforms to the ethical
guidelines of the 1975 Declaration of Helsinki and was approved by
the Institutional Ethics Committee of Ueki Hospital, and informed
written consent was obtained from all of the patients. The present
study performed a post hoc analysis of the ESPRIT study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
McDonagh TA, Metra M, Adamo M, Gardner RS,
Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et
al: ESC scientific document group: 2021 ESC guidelines for the
diagnosis and treatment of acute and chronic heart failure. Eur
Heart J. 42:3599–3726. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Writing Committee, Maddox TM, Januzzi JL
Jr, Allen LA, Breathett K, Butler J, Davis LL, Fonarow GC, Ibrahim
NE, Lindenfeld J, et al: 2021 update to the 2017 ACC expert
consensus decision pathway for optimization of heart failure
treatment: Answers to 10 pivotal issues about heart failure with
reduced ejection fraction: A report of the American college of
cardiology solution set oversight committee. J Am Coll Cardiol.
77:772–810. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gerber Y, Weston SA, Redfield MM,
Chamberlain AM, Manemann SM, Jiang R, Killian JM and Roger VL: A
contemporary appraisal of the heart failure epidemic in Olmsted
County, Minnesota, 2000 to 2010. JAMA Intern Med. 175:996–1004.
2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sadanaga T, Hirota S, Enomoto K, Kohsaka
S, Tsujita K, Ito M, Mitamura H and Fukuda K: Evaluation of sodium
intake for the prediction of cardiovascular events in Japanese
high-risk patients: the ESPRIT study. Hypertens Res. 42:233–240.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tanaka T, Okamura T, Miura K, Kadowaki T,
Ueshima H, Nakagawa H and Hashimoto T: A simple method to estimate
populational 24-h urinary sodium and potassium excretion using a
casual urine specimen. J Hum Hypertens. 16:97–103. 2002.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mann SJ and Gerber LM: Estimation of
24-hour sodium excretion from spot urine samples. J Clin Hypertens
(Greenwich). 12:174–180. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wan ER, Cross J, Sofat R and Walsh SB:
24-hour vs. spot urinary sodium and potassium measurements in adult
hypertensive patients: A cohort validation study. Am J Hypertens.
32:983–991. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lee SG, Lee W, Kwon OH and Kim JH:
Association of urinary sodium/creatinine ratio and urinary
sodium/specific gravity unit ratio with blood pressure and
hypertension: KNHANES 2009-2010. Clin Chim Acta. 424:168–173.
2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kim JG, Han SW, Yi JH, Park HC and Han SY:
Development of objective indicators for quantitative analysis of
sodium intake: the sodium to potassium ratio of second-void urine
is correlated with 24-hour urinary sodium excretion. Nutr Res
Pract. 14:25–31. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sadanaga T, Hirota S and Mitamura H:
Factors associated with heart failure hospitalization in patients
with high sodium excretion: subanalysis of the ESPRIT, evaluation
of sodium intake for the prediction of cardiovascular events in
Japanese high-risk patients, cohort study. Heart Vessels. 36:85–91.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kawano Y, Tsuchihashi T, Matsuura H, Ando
K, Fujita T and Ueshima H: Working Group for Dietary Salt Reduction
of the Japanese Society of Hypertension. Report of the working
group for dietary salt reduction of the Japanese society of
hypertension: (2) assessment of salt intake in the management of
hypertension. Hypertens Res. 30:887–893. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Umemura S, Arima H, Arima S, Asayama K,
Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, et al:
The Japanese society of hypertension guidelines for the management
of hypertension (JSH 2019). Hypertens Res. 42:1235–1481.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rhee MY, Kim JH, Shin SJ, Gu N, Nah DY,
Park JH, Kim SW, Kim HJ, Oh KW, Kim JH and Lee SY: Estimating
24-hour urine sodium from multiple spot urine samples. J Clin
Hypertens (Greenwich). 19:431–438. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rhee MY, Kim JH, Shin SJ, Gu N, Nah DY,
Hong KS, Cho EJ and Sung KC: Estimation of 24-hour urinary sodium
excretion using spot urine samples. Nutrients. 6:2360–2375.
2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Martens P, Dupont M, Verbrugge FH, Damman
K, Degryse N, Nijst P, Reynders C, Penders J, Tang WHW, Testani J
and Mullens W: Urinary sodium profiling in chronic heart failure to
detect development of acute decompensated heart failure. JACC Heart
Fail. 7:404–414. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Desai AS and Mc Causland FR: Urinary
sodium as a heart failure biomarker: More complicated than it
seems. JACC Heart Fail. 7:415–417. 2019.PubMed/NCBI View Article : Google Scholar
|