Introduction
Bladder stones are a common type of urinary tract
stone (1). With the development of
medicine and the improvement of living standards, the incidence of
bladder stones has progressively decreased. Patients with bladder
stones experience a sudden interruption of urination, as well as
laborious urination and urinary retention (1). Secondary stone formation occurs in
most elderly males due to benign prostatic hyperplasia. The
incidence of bladder stones among younger patients is low and that
of large stones is rare. The formation of a large stone occurs over
a long period of time and it may be complicated by concurrent
serious infections, requiring open surgery for stone removal
(2). Although rare in Europe and
the US, giant bladder stones are frequently reported in developing
countries and tropical regions (3). The present study reported the case of
a young male with a giant bladder stone that led to acute renal
failure. This report may serve as a reference for clinicians.
Case report
A 31-year-old male patient from a rural area who
worked outdoors throughout the year had been experiencing repeated
frequent urination and urgency, which had worsened over the past
year. Difficulty in urination had gradually worsened over the
previous week, accompanied by bilateral back pain and urinary
retention; therefore, the patient sought medical treatment at the
local Gaotai Silk Road Ciren Hospital (Zhangye, China) in May 2021.
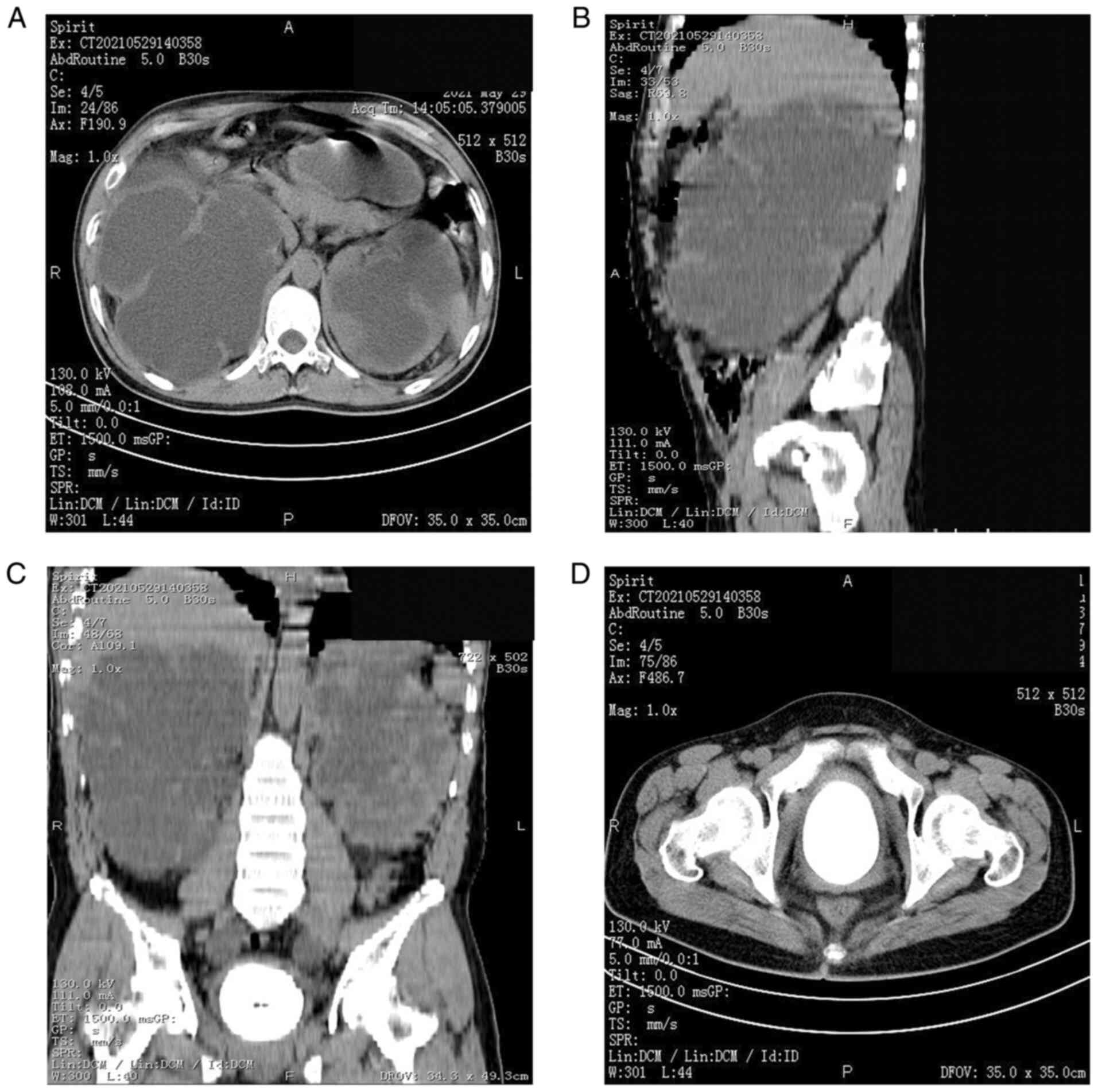
A CT scan of the patient's urinary system revealed a giant bladder
stone, giant double hydronephrosis and double ureteral dilatation
throughout the process (Fig. 1).
Renal failure was diagnosed and the patient was transferred to our
hospital (Hexi University Affiliated Zhangye People's Hospital,
Zhangye, China) for further treatment. Upon admission, physical,
biochemical and hematological examination revealed the following:
White blood cells, 41.6x109/l (normal range:
3.7-9.2x109/l); hemoglobin, 110 g/l (normal range:
131-172 g/l); neutrophil ratio, 88% (normal range: 45-77%);
creatinine, 744 µmol/l (normal range: 44-120 µmol/l); potassium,
5.4 mmol/l (normal range: 3.5-5.5 mmol/l); procalcitonin, 45.88
ng/ml (normal range: <0.5 ng/ml); routine urine test for white
blood cells, +++; and urine culture positive for Escherichia
coli. The patient's body temperature was 40˚C. Attempts to
insert an indwelling catheter were not successful, as obvious
resistance was encountered.
The patient was administered imipenem antibiotic
treatment and a retropubic cystotomy was performed under general
anesthesia to remove the stone. During the operation, pyuria in the
bladder (milky white urine accompanied by a foul odor) was
encountered. A large amount (at least 300 ml) of milky pus with
foul odor leaked out. Bacterial culture results revealed E.
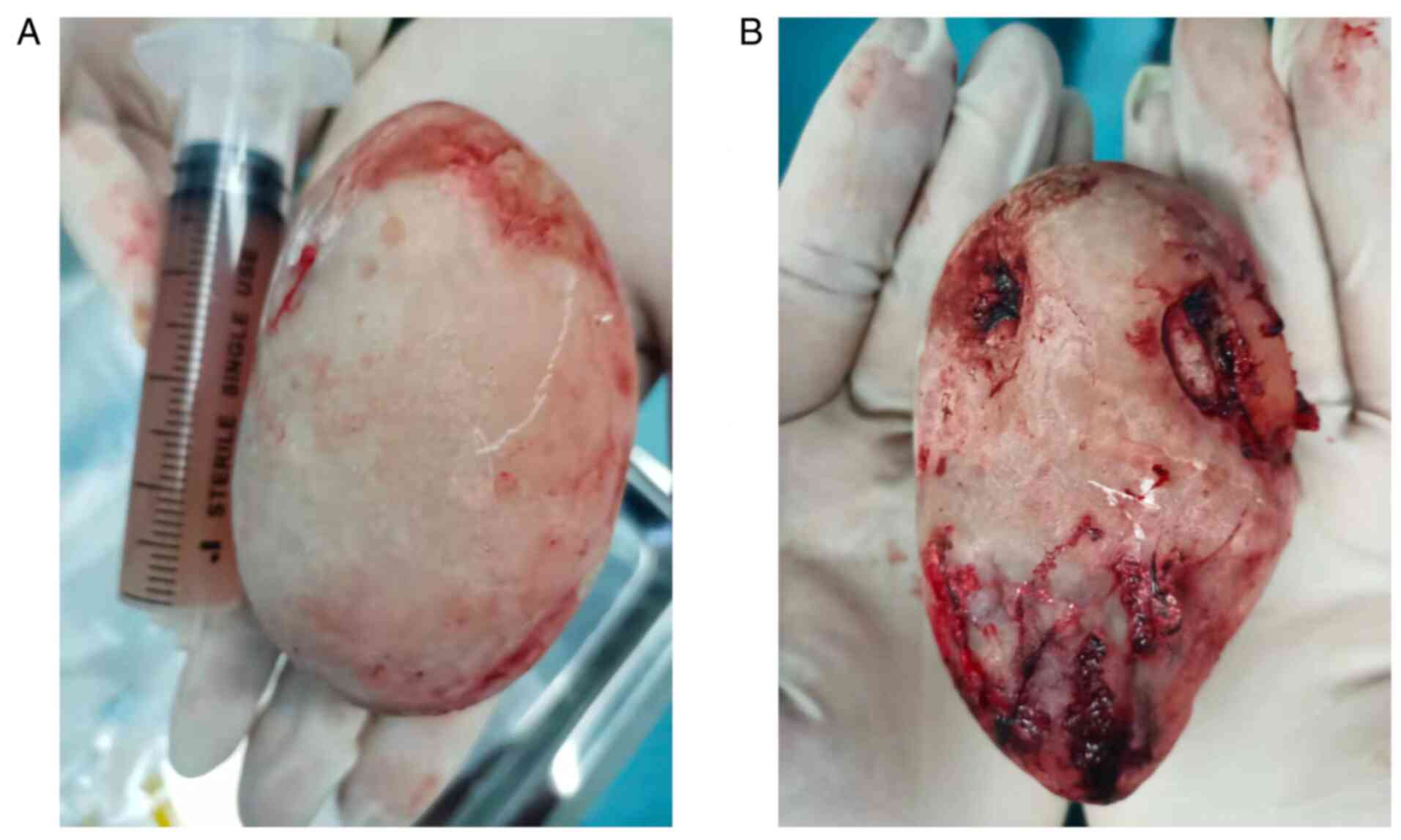
coli infection. The stone was huge and its bottom surface
closely adhered to the bladder wall, thereby complicating its
removal. The adhesion was carefully separated and the stone was
removed; the bottom surface of the stone was irregular (Fig. 2). It was planned to place a double
ureteral stent, but as the urine in the bladder was cloudy, the
mucosa in the triangular and ureteral orifice area was rough and
the visual field was poor, it was not possible to accurately locate
the ureteral opening. After discussion, it was decided to close the
bladder and terminate the surgery. A catheter and drainage tube
were inserted and it was observed that the color of the patient's
urine was still milky white on the second day, but it gradually
turned clear later. This was the urine stored in the kidney that
entered the bladder through the ureter, as the bladder had been
removed from the place where the ureter was compressed. It was
originally planned to keep a ureteral stent to drain the huge
hydronephrosis. However, the bladder mucosa was widely damaged,
with severe infection and edema; hence, it was not possible to
locate the ureteral orifice. It was not possible to insert the
ureteral stent, and hence, the urine continued to drain and bladder
irrigation was performed. The color of the patient's urine
gradually turned normal, the renal function improved and the
drainage became smooth; no further nephrostomy was performed.
Following the surgery, the patient's body
temperature dropped. Milky-white urine continued to drain from the
catheter on the day after the operation; however, with continuous
bladder irrigation, the color of the urine turned clear. After the
operation, imipenem administration was continued as an antibiotic
for 3 days. The antibiotic was subsequently changed to ceftizoxime
for 4 days, according to the drug susceptibility test results. The
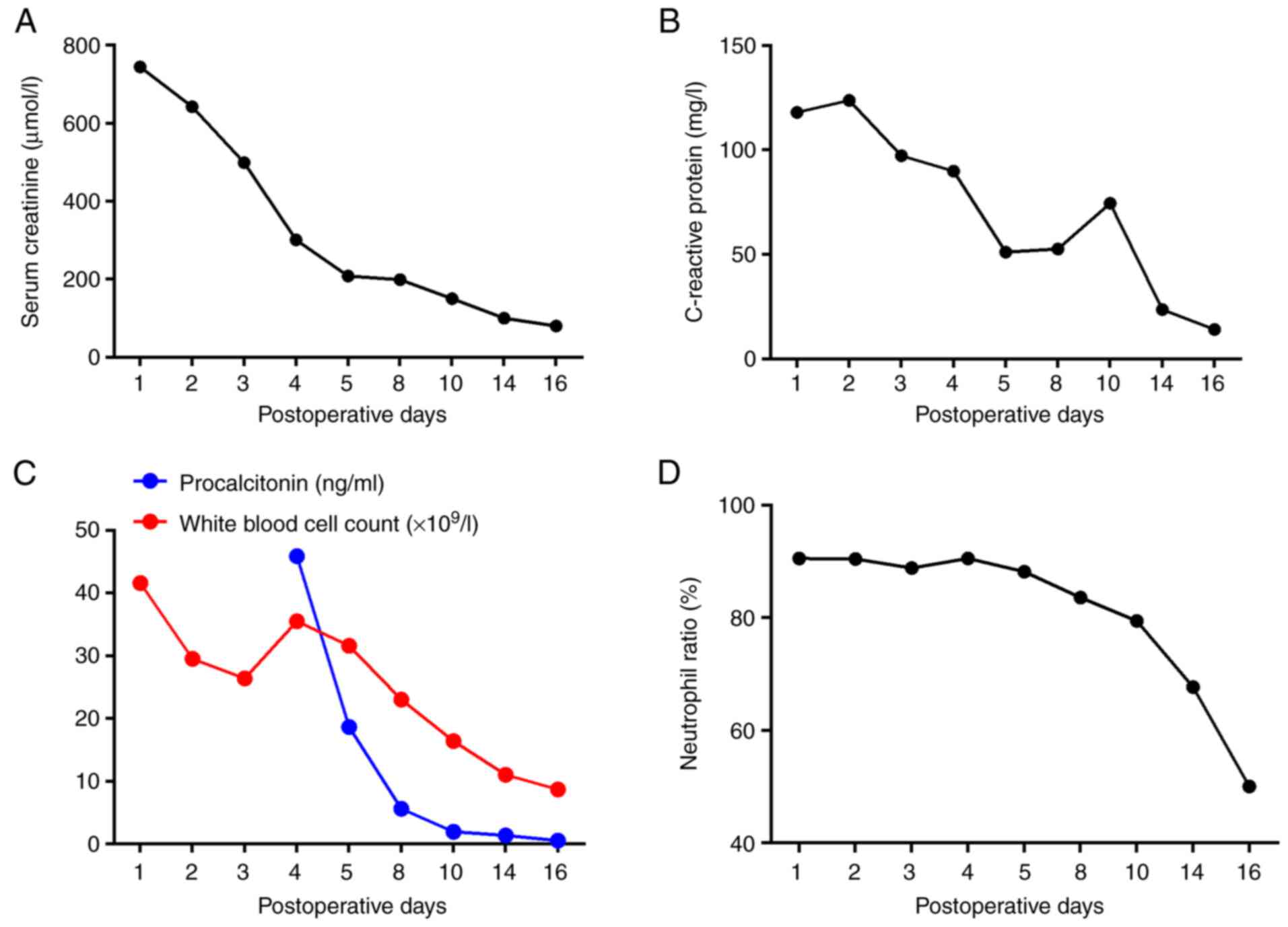
double hydronephrosis significantly improved when re-examined via
ultrasound and the patient's white blood cell count, serum
creatinine, procalcitonin, C-reactive protein and neutrophil ratio
also improved significantly (Fig.
3). The patient was discharged 2 weeks after surgery.
Discussion
Giant bladder stones >100 g in weight are rare in
modern urology, particularly in developed countries in Europe and
the US (4,5). Cases of bladder stones remain common
in developing countries and poorer areas. Numerous patients are
unable to afford medical treatment and thus delay seeking treatment
for urinary symptoms, leading to bladder stones. Bladder stones are
frequently misdiagnosed as urinary tract infections. The symptoms
improve after oral antibiotic treatment, but the stones are not
eradicated. With the improvement of the economic situation in
China, the annual incidence of bladder stones has been
progressively decreasing (6).
Secondary bladder stones are more common in older males with benign
prostatic hyperplasia (7). The
present study reported the case of a young patient with no previous
history of prostatic hyperplasia, who, at the age of 31 years,
presented with a giant bladder stone that led to severe bilateral
hydronephrosis, ureteral dilatation and renal failure. Renal
failure is rare in patients with giant bladder stone, whose most
common complaints are repeated and long-term lower urinary tract
symptoms, frequent urination, urgency and severe urinary tract
infections (8,9). The present patient reported that he
had experienced frequent urination for 5 years but had not sought
medical attention. When the symptoms worsened, the patient visited
his doctor but was not comprehensively examined, and the patient
was misdiagnosed with prostatitis. The treatment the patient
received was ineffective. After remote consultation, a giant
bladder stone was diagnosed via urinary CT evaluation and the
patient was referred to our department for surgical treatment.
Although the patient had urinary retention, it was not possible to
insert a catheter because the stone was incarcerated in the
triangular area and blocked the internal opening of the urethra.
During the operation, the giant stone was found to be closely
adherent to the bladder mucosa and to compress the double ureteral
orifice, thereby resulting in ureteral dilatation, hydronephrosis
and renal failure. Surgery was the only curative procedure
available. Several researchers argue that cystoscopy should be the
preferred method for diagnosing bladder stones (10). However, cystoscopy was not
appropriate in the present case, given the presence of severe
urinary tract infection, which is a contraindication to cystoscopy.
Furthermore, it was not possible to insert a catheter, as the giant
stone blocked the internal opening of the urethra. This was an
additional reason why it was not possible to successfully perform
cystoscopy on this patient, and it would have only resulted in
increased pain and discomfort for the patient. Abdominal
radiography, pelvic ultrasound and CT examination may diagnose most
cases of giant bladder stone (11,12).
Considering that the giant bladder stone was also associated with
lower back pain in the present case, a CT scan of the urinary
system was performed to evaluate the state of the entire urinary
system. CT scans are more accurate than other imaging modalities
and inspection methods for detecting giant bladder stones,
evaluating the state of double hydronephrosis and determining
whether these are combined with double ureteral stones (11,13).
The surgical method for removing bladder stones is either
transurethral lithotripsy or open surgery, although almost all
giant bladder stones reported in the literature are treated with
open cystotomy (14-16).
Since the bladder stones are large and most patients have
concomitant severe urinary tract infections, the efficiency of
transurethral lithotripsy is low. Furthermore, transurethral
lithotripsy increases the risk of infection and has a long
operation time, increasing the incidence of post-operative
complications. However, open surgery for removing complete stones
has shorter operation times (2,17).
In the present case, immediate relief of the obstruction caused by
the giant stone was of paramount importance and the operation time
for removing the stone was ~40 min. A large amount of turbid,
milky-white urine was removed from the bladder during the
operation. The patient's condition was further complicated by renal
failure, which required the operation time to be minimized to avoid
continuous kidney damage caused by the anesthetic drugs. Visibility
within the bladder during endoscopic exploration was poor. The
adhesion of the intravesical mucosa and the calculus had caused
extensive damage to the mucosa, leading to mucosal hemorrhage and
edema, thereby making the localization of the double ureteral
orifice difficult. Therefore, no double ureteral stent was placed
during the operation. After the operation, the patient's creatinine
level continued to decrease from 744 µmol/l on admission to 80
µmol/l at discharge. The white blood cell count, C-reactive protein
level and procalcitonin level also continued to decrease; renal
function improved, the urine color gradually cleared and the
infection was controlled. The patient was successfully treated and
was satisfied with the treatment outcome. In this patient, a stone
composition analysis should have been performed to determine the
reason for the occurrence of such a huge stone; however, the
patient's family had discarded the stone and hence, it was not
possible to perform the stone composition analysis. Such an
analysis is warranted in future cases.
We consider the present case to be of great
interest. This was a young patient with no lower urinary tract
obstruction, such as prostatic hyperplasia or urethral stricture
that causes secondary bladder stones similar to those to occur in
elderly patients. Furthermore, this case demonstrates that acute
renal failure may be a rare complication of giant bladder stone;
timely treatment prevented obvious hyperkalemia in this patient.
Finally, the present report highlights the requirement for
conducting a comprehensive physical examination and thorough
investigation of the patient's medical history during clinical
evaluation, diagnosis and treatment. The present case should not
have been misdiagnosed as prostatitis or a common urinary tract
infection, highlighting the requirement to conduct the necessary
examinations and tests to obtain a definite diagnosis. The range of
symptoms of the present case was caused by a giant bladder stone
that required timely open surgery. Any further delay in the
patient's diagnosis may have had catastrophic consequences,
highlighting the requirement for clinicians to be vigilant and take
the necessary precautions.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by Gansu Province Science
and Technology Planning Project (grant no. 20JR10RG310).
Availability of data and materials
All data generated in the present study are included
in the article and figures.
Authors' contributions
XYW and YQ contributed to the conceptualization and
design of the study, and the drafting of the manuscript. XHW, JQ
and SN contributed to the conceptualization and design of the
study. XHW, ST and JY collected clinical information and assisted
with drafting the manuscript. ST and JY contributed to critical
revisions of the intellectual content and confirm the authenticity
of all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the Ethics Committee
of Hexi University affiliated Zhangye People's Hospital (Zhangye,
China).
Patient consent for publication
Consent was obtained from the patient for the
publication of the patient's data/images included in this case
report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cicione A, DE Nunzio C, Manno S, Damiano
R, Posti A, Lima E, Tubaro A and Balloni F: Bladder stone
management: An update. Minerva Urol Nefrol. 70:53–65.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kalathia J, Patel K and Agrawal S: Giant
prostatic and bladder calculi: Endoscopic management and review of
the literature. Urol Case Rep. 35(101529)2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fu L: The use of lithotomy by missionary
surgeons in nineteenth-century China. J R Coll Physicians Edinb.
41:264–269. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ouattara Y and Koné J: Giant bladder
stone. Pan Afr Med J. 29(28)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gallego Vilar D, Beltran Persiva J, Pérez
Mestre M, Povo Martin IJ, Miralles Aguado J, Garau Perelló C and De
Francia JA: Giant bladder lithiasis: Case report and bibliographic
review. Arch Esp. 64:383–387. 2011.PubMed/NCBI
|
|
6
|
Ye Z, Zeng G, Yang H, Li J, Tang K, Wang
G, Wang S, Yu Y, Wang Y, Zhang T, et al: The status and
characteristics of urinary stone composition in China. BJU Int.
125:801–809. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kang J: Bladder stone secondary to
prostatic urethral lift (PUL) for benign prostatic hyperplasia
(BPH). Urol Case Rep. 39(101777)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sullivan AE and Sata SS: Giant uric acid
stone in the bladder. Cleve Clin J Med. 87:14–15. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pattiiha AM, Hadi AF, Rokhimah S and Hafiq
HM: Giant bladder uric acid stone with a history of prolonged sun
exposure and high protein diet in North Moluccas: Case series. Int
J Surg Case Rep. 73:328–331. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Julian AS and Agil A: Hanging bladder
stone due to misplaced surgical suture several years after
hysterectomy: A case report. Int J Surg Case Rep.
89(106586)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
O'Kane D, Papa N, Manning T, Quinn J,
Hawes A, Smith N, McClintock S, Lawrentschuk N and Bolton DM:
Contemporary accuracy of digital abdominal X-ray for follow-Up of
pure calcium urolithiasis: Is there still a role? J Endourol.
30:844–849. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liu S, Wang H, Feng W, Hu X, Guo J, Shang
Q, Li Z and Yu H: The value of X-ray digital tomosynthesis in the
diagnosis of urinary calculi. Exp Ther Med. 15:1749–1753.
2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Avanesov M, Togmat J, Solmaz M, Kaul MG,
Laqmani A, Guerreiro H, Keller S, Weisbach L, Adam G and Yamamura
J: Increased urinary bladder volume improves the detectability of
urinary stones at the ureterovesical junction in non-enhanced
computed tomography (NECT). Eur Radiol. 29:6953–6964.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tan YK, Gupta DM, Weinberg A, Matteis AJ,
Kotwal S and Gupta M: Minimally invasive percutaneous management of
large bladder stones with a laparoscopic entrapment bag. J
Endourol. 28:61–64. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Aboulela W, ElSheemy MS, Shoukry AI,
Shouman AM, ElShenoufy A, Daw K, Morsi HA and Badawy H:
Transurethral holmium laser cystolithotripsy in children: Single
center experience. J Endourol. 29:661–665. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Jia Q, Jin T, Wang K, Zheng Z, Deng J and
Wang H: Comparison of 2 kinds of methods for the treatment of
bladder calculi. Urology. 114:233–235. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Alshayyah RWA, Yu Y, Lv H, Liu W and Yang
B: Bipolar transurethral enucleation of the prostate combined with
open cystolithotomy in the treatment of large and giant prostate
with bladder stones: Case series. Urologia. 89:195–202.
2022.PubMed/NCBI View Article : Google Scholar
|